Abstract
Objective
To assess the impact of assignment to a Medicaid‐focused versus mixed managed care plan on continuity of Medicaid coverage.
Data Sources
2011–2016 Medicaid claims from a Northeastern state.
Study Design
Following the exit of a Medicaid managed care insurer, Medicaid administrators prioritized provider networks in reassigning enrollees, but randomly assigned beneficiaries whose providers were equally represented in the two plans. We leveraged the natural experiment created by random plan assignment and conducted an instrumental variable analysis.
Data Collection
We analyzed Medicaid claims for 12,083 beneficiaries who were members of the exiting Blue Cross Blue Shield plan prior to January 1, 2011.
Principal Findings
Managed care plan type did not significantly impact continuous enrollment in the Medicaid program. Greater outpatient utilization and the presence of a special need among children were associated with longer enrollment in Medicaid.
Conclusions
Managed care plans did not differ in their capacity to keep Medicaid beneficiaries continuously enrolled in coverage, despite differences in plan features.
Keywords: Medicaid, managed care, continuity of coverage, natural experiment
Discontinuous Medicaid enrollment has been shown to negatively impact health outcomes and impose substantial costs on patients and state Medicaid budgets. Lapses in continuous Medicaid enrollment can lead to foregone care that exacerbates existing conditions and delays screening and detection of new illnesses (Gill et al. 2003; Koroukian 2004; Gold et al. 2009). Enrollees who use care while uninsured can face serious financial consequences (Duchon et al. 2001). Spells of disenrollment are associated with higher spending for potentially preventable conditions through greater emergency room and psychiatric facility use (Harman et al. 2003; Bindman, Chattopadhyay, and Auerback 2008; Hall, Harman, and Zhang 2008). Even brief interruptions in Medicaid coverage pose financial burdens to state Medicaid programs. Prior research demonstrates that on average, a single episode of “churning” off and on Medicaid coverage comprises 10–15 percent of total annual Medicaid expenditures for a healthy, nondisabled adult (Swartz et al. 2015). For these reasons, average monthly Medicaid expenditures generally decline as the length of time beneficiaries are enrolled increases (Ku and Ross 2002).
In 2014, nearly 80 percent of the over 70 million Americans with Medicaid coverage were enrolled in a managed care plan (Kaiser Family Foundation 2014). Medicaid managed care plans have distinct characteristics that can influence Medicaid beneficiary retention. Some plans exclusively or primarily serve Medicaid populations, while others are mixed, serving both Medicaid and commercial markets. Plans can be local or national, can vary on whether they are publicly traded companies, and can have for‐profit or nonprofit tax status. National plans that provide Medicaid managed care are more likely to be for‐profit “mixed” plans that serve multiple markets, while local plans tend to be nonprofit and primarily serve Medicaid populations. As of 2010, 63 percent of Medicaid managed care plans were Medicaid focused, 53 percent of plans were for‐profit, 42 percent were publicly traded, and 51 percent of plans were national (Kaiser Family Foundation 2011). By 2015, 52 percent of the largest managed care organizations served both the Medicaid and commercial markets and 72 percent of the largest Medicaid‐focused managed care organizations held for‐profit status (Milliman 2016).
Distinct features of managed care plan may influence continuity of Medicaid enrollment through various pathways. Managed care companies with for‐profit tax status may face greater incentives to increase profits by maintaining a healthier pool of Medicaid enrollees, leading to practices that discourage the enrollment and retention of complex patients. Medicaid‐focused plans may benefit from experience serving the specific needs of the Medicaid population, building on strong relationships with safety‐net providers who are familiar with the barriers to care for vulnerable populations and are experienced in coordinating care for complex patients. Compared to plans that also serve commercial enrollees, Medicaid‐focused plans may also have stronger relationships with community health centers that facilitate Medicaid enrollment and renewals. However, plans that operate in commercial markets may be able to draw on national administrative infrastructure that could help identify and engage complex patients. These plans may also be able to encourage access to care through more extensive provider networks.
Few studies have assessed the impact of distinct types of Medicaid managed care plans on provision of Medicaid services, and none have addressed the impact of managed care plan type on Medicaid enrollee retention. Studies have shown that Medicaid enrollees in for‐profit plans were more likely to report unmet medical needs compared to Medicaid enrollees in nonprofit plans, and Medicaid enrollees in publicly traded plans were more likely to experience worse preventive and chronic illness care (Long and Yemane 2005; McCue and Bailit 2011). Research that has examined the staggered rollout of Medicaid managed care across counties in California found improvements in perinatal hospital quality metrics and greater increases in medical expenditures in counties with a public, county‐run managed care organization compared to counties with private managed care organizations, but found equal or nonsignificant declines in infant health outcomes between the two types of counties (Duggan 2004; Aizer, Currie, and Moretti 2007). Poor outcomes may discourage enrollees from maintaining continuous coverage in a given managed care plan either due to dissatisfaction or low engagement with providers who are often the frontline connection between the Medicaid‐eligible population and the Medicaid program.
This study examines the impact of managed care plan type on continuous enrollment in Medicaid. We leverage randomization of Medicaid enrollees to two managed care plans following the exit of an insurer in the Medicaid managed care market in a Northeastern state. Enrollees were randomized to either a national, for‐profit plan that serves both Medicaid and commercial populations, or a local, non‐profit plan that predominantly serves Medicaid beneficiaries. Medicaid plan exits are concerning because they pose a risk for major care disruptions if beneficiaries do not understand their new plan or network or if treatment plans are altered due to differences across plans in approaches to care, obtaining specialty services, or population management strategies (Long and Yemane 2005). It is an open policy question as to how to reassign beneficiaries while minimizing disruptions in care. The purpose of this study was to assess whether there are differences in continuity of coverage across distinct features of managed care plans and to highlight lessons from one state's randomization strategy for reassigning enrollees following a market exit.
Methods
Random Assignment to Managed Care Plans
In 2010, the state Medicaid office solicited bids for managed care contracts for the 2011 calendar year. In the summer of 2010, one of the three operating insurers (a large Blue Cross Blue Shield [BCBS] plan) informed the state that it opted not to renew its Medicaid contract, and it was agreed that all current plan enrollees would be disenrolled by 12/31/10 and assigned to the remaining two insurers. In planning how to accommodate BCBS enrollees, Medicaid administrators prioritized provider networks in reassigning enrollees, such that if one of the two remaining plans included more of the enrollees’ regular providers in its network, they were directly assigned to that plan. However, for 56.9 percent of BCBS enrollees, provider network fit was equal between the two plans. Therefore, the state decided to randomly assign the remaining enrollees in a 3 : 2 fashion to either the local, not‐for‐profit plan (hereafter referred to as the “Medicaid‐focused plan”) or the national, for‐profit plan (hereafter referred to as the “mixed plan”). In other words, for the sample of enrollees for whom provider fit was equivalent across the plans, the state prioritized balancing enrollment through random assignment. The unit of randomization was the family.
Enrollees were notified of their auto‐assigned plan in four mailings between 15 October 2010 and 1 December 2010. Enrollees received a letter and fact sheet informing them of their change in coverage and encouraging them to contact the Medicaid program with any questions or concerns. In the letter, enrollees were informed that they could “opt‐out” of their assigned plan without penalty either before enrolling in their new plan or in a 90‐day open enrollment period after their transition. Less than 3 percent opted out of their assigned plan prior to 1 January 2011.
Data and Sample
We obtained Medicaid claims for beneficiaries who were members of the exiting BCBS plan prior to 1 January 2011 and were reassigned to the remaining Medicaid focused or mixed managed care plans. We used claims from two years prior to plan reassignment to ascertain baseline utilization, comorbidities, and demographics, and used five years following plan reassignment on 1 January 2011 to measure continuity of coverage. Data from 1 January 2011 to 31 December 2013 contain information about the type of managed care plan beneficiaries were enrolled in, whereas data from 1 January 2014 to 31 December 2016 records only whether an enrollee was in the Medicaid program or not.
Of the 14,083 members of the exiting BCBS plan, 6,073 were directly, nonrandomly assigned to either the Medicaid‐focused plan or the mixed plan because their primary care providers only participated in one of the plan's networks. Our analyses focused on the remaining 8,010 enrollees who were randomized to the two plan options after the exit of BCBS. We excluded 332 individuals from the analysis because they disenrolled from Medicaid prior to the start of follow‐up on 1 January 2011, 133 individuals who delayed enrollment for six or more months after the randomization date, and 715 with missing address or eligibility information. Our final study sample included 6,830 individuals and 2,876 families. A total of 4,051 individuals (59.3 percent) and 1,667 families (58.0 percent) were randomly assigned to the Medicaid‐focused plan, and 2,779 (40.7 percent) individuals and 1,209 families (43.5 percent) were randomly assigned to the mixed plan. All the same exclusions were applied to the nonrandomized population. Secondary analyses compared the randomized population of 6,830 beneficiaries to 5,253 directly assigned beneficiaries who met the aforementioned inclusion and exclusion criteria.
Outcomes and Measures
In order to understand the effect of randomization to managed care plan type on continuous Medicaid coverage, the primary outcome measure was a binary measure of 12 months of continuous Medicaid coverage, defined as enrollment in any type of Medicaid coverage where a code of 1 indicated 12 months of continuous coverage and a code of 0 indicated disenrollment, gaps in coverage, or within‐Medicaid switches in plan type prior to the end of the year. Because gaps in the enrollment record may reflect administrative lags as opposed to coverage lapses, a sensitivity analysis varied the definition of a gap to include a minimum gap length of 28, 45, and 90 days. These restrictions did not substantially change the findings, and thus, no minimum gap length requirement was imposed. The outcome was assessed annually starting from 1 January 2011, but our results focus on the three‐year measure as results did not vary meaningfully across years (see Table S3). The primary independent variable of interest was random assignment to type of managed care plan as of 1 January 2011. We also examined the impact of a secondary independent variable comparing whether beneficiaries were randomized or directly assigned to their plan. In our instrumental variable analysis, the instrument was random assignment and the independent variable was plan enrollment.
Baseline covariates included sex, age, reason for Medicaid eligibility, primary language, prior health care utilization, comorbid medical conditions, imputed race/ethnicity, and an Area Deprivation Index (ADI). Reasons for eligibility were grouped into five categories: child, pregnancy, disability, caretaker/parent, and low‐income adults. To assess whether patterns of disenrollment across plans differed by health status, we counted the number of admissions, emergency department visits, and outpatient doctor visits. Utilization measures compared the sample with the highest 10 percent of utilization to the rest of the distribution for each type of utilization. Comorbidities were measured using the Charlson Comorbidity Index among adults and the Children's Special Health Care Services measure among those under 18, as described in Charlson et al. (1987) and Pollack et al. (2004).
In the enrollment claims file, race was not reported for 52 percent of the randomized sample. For those with missing race information, we used multiple imputation to predict individual race using a combination of race/ethnicity data sources: Census block geocoding from the 2011 American Community Survey and surname analysis from the Census Bureau Spanish Surname List and Lauderdale‐Kestenbaum Asian Surname List. Probabilities of a given race/ethnicity that were used in the imputation process were computed following Adjaye‐Gbewonyo et al.'s Bayesian Improved Surname Geocoding (BISG) approach and validated through comparison to the recorded race/ethnicity values in claims (Adjaye‐Gbewonyo et al. 2014). To capture neighborhood socioeconomic contextual disadvantage, we used the ADI. This measure aggregates 17 different census block‐group level indicators of education, income, poverty, housing, and employment drawn from the 2009 to 2013 American Community Survey data available through the University of Wisconsin (Kind et al. 2014). The ADI is constructed to have a national index mean of 100 with a standard deviation of 20. We constructed quintiles of relative neighborhood disadvantage, with higher values indicating greater disadvantage.
Statistical Analysis
For our primary analysis of the impact of random plan assignment on continuity of coverage, we used an intention‐to‐treat analysis, which assessed the causal effect of random managed care plan assignment on continuity of coverage. One hundred and twenty‐two beneficiaries who delayed enrollment for fewer than 6 months of assignment were treated as enrolled as of randomization. Baseline differences between the two groups were assessed using chi‐square tests for categorical variables, two‐sample t tests for continuous variables, and t tests for differences in proportions. We used logistic regression models to estimate the conditional effect of managed care plan assignment on annual rates of continuity of coverage. We stratified by age groups ≤14 and ≥18 at baseline, excluding 15–17 year olds from the stratified analyses to avoid including adolescents who lost coverage over the 5 years of follow‐up due to aging out of Medicaid eligibility at 18. In models that included enrollees of all ages, age was removed from the model due to collinearity with reason for eligibility. We also tested two interaction terms between plan assignment and the top 10 percent of outpatient utilization and between plan assignment and children with special health care needs. These interactions were not statistically significant and were not included in the final model. Standard errors were clustered at the family level in all models.
Because some individuals did not enroll in the plan to which they were assigned, we also estimated a two‐stage least square regression that used random plan assignment as an instrument to assess the impact of plan type enrollment on continuity of coverage. We used the same modeling approach and covariates in this secondary analysis and our assessment of the impact of random versus direct assignment on continuity of Medicaid enrollment. All analyses were conducted using STATA version 14.2 (STATA version 14.0: College Station, Texas, USA).
Results
Table 1 displays baseline characteristics of each group randomized to the mixed and Medicaid‐focused plans. The majority of the randomized population was female, white, English‐speaking, and under 18. The most common eligibility pathways were through child and parental/caretaker status, while pregnancy and disability‐based eligibility pathways composed a smaller share of the overall sample (~10 percent in each assigned plan). There were no significant differences between the two groups with respect to age, sex, neighborhood disadvantage, reason for eligibility, language, utilization, or comorbidities at baseline. However, a chi‐square test of the imputed race/ethnicity categories across plan indicated that the proportions were not balanced across the two groups (p = .008).
Table 1.
2011 Baseline Characteristics of Randomized Sample by Assigned Plan, N = 6,830
| Variable | Medicaid‐Focused Plan N = 4,051 Families = 1,667 | Mixed Health Plan N = 2,779 Families = 1,209 | p‐Value |
|---|---|---|---|
| Female, % | 58.2 | 58.6 | .780 |
| Age, % | |||
| <18 | 60.5 | 61.2 | |
| 18–45 | 33.7 | 32.9 | |
| 46–64 | 5.9 | 5.9 | .809 |
| Race/ethnicity, % | |||
| White | 71.1 | 68.2 | |
| Black | 10.8 | 10.7 | |
| Asian/Pacific Islander | 3.0 | 3.6 | |
| Hispanic | 14.1 | 16.9 | |
| Native American | 0.9 | 0.6 | .008 |
| Enrollment pathway, % | |||
| Pregnancy | 4.9 | 5.7 | |
| Disability | 3.5 | 3.4 | |
| Child | 61.8 | 62 | |
| Parent/caretaker | 20.4 | 20.2 | |
| Adult other | 9.4 | 8.7 | .618 |
| Language, % | |||
| English | 92.7 | 91.2 | |
| Spanish | 6.6 | 8.2 | |
| Other | 0.7 | .7 | .042 |
| Residing in highest quintile of neighborhood disadvantage, % | 9.8 | 10.2 | .525 |
| Utilization counts, mean | |||
| Admissions | 1.2 | 1.2 | .255 |
| ED visits | 1.8 | 1.9 | .161 |
| Doctor visits | 6.5 | 6.3 | .333 |
| Charlson comorbidity index, % (over 18, N = 2,593) | |||
| 0 | 91.0 | 89.9 | |
| 1 | 7.2 | 8.3 | |
| 2+ | 1.7 | 1.8 | .605 |
| Pollack children with special needs among <18 years old, % | 27.3 | 29.7 | .120 |
Notes. Race/ethnicity estimates are imputed. Not all numbers may sum to 100 due to rounding. p‐Values were computed using chi‐square tests for categorical variables, two‐sample t tests for continuous variables, and two‐sample t tests for differences between proportions.
Table 2 depicts summary continuity of coverage measures. There were significant differences in compliance rates across the two plan types. About 83.7 percent of those randomly assigned to the Medicaid‐focused plan enrolled in the Medicaid‐focused plan, while 89.2 percent of those randomly assigned to the mixed plan enrolled in the mixed plan (p < .001). We observed a significant difference in the switch rates between those who initially enrolled in their assigned plan, but subsequently switched to the other plan. About 11.1 percent of enrollees assigned to the Medicaid‐focused plan enrolled in the mixed plan, compared to 5.8 percent of those assigned to the mixed plan who enrolled in the Medicaid‐focused plan (p < .001). Approximately 4 percent of those assigned to each plan were initially enrolled in fee‐for‐service instead of their assigned managed care plan due to administrative enrollment delays, but these rates did not vary across plan type.
Table 2.
Summary Continuity of Coverage Statistics by Assigned Plan, (N = 6,830)
| Variable | Medicaid‐Focused Plan (N = 4,051) | Mixed Health Plan (N = 2,779) | p‐Value |
|---|---|---|---|
| Enrolled in assigned plan, N (%) | 3,390 (83.7) | 2,485 (89.4) | <.001 |
| Enrolled in non‐assigned plan, N (%) | 448 (11.1) | 162 (5.8) | <.001 |
| Enrolled in fee‐for‐service, N (%) | 179 (4.4) | 112 (4.0) | .435 |
| Switched from assigned plan after index enrollment, N (%) | 235 (5.8) | 95 (3.4) | <.001 |
| No. of months enrolled, mean (SE) | 33.3 (.35) | 33.3 (.41) | .943 |
| Years of continuous Medicaid, N (%) | |||
| 1 year | 2,935 (72.5) | 2,062 (74.2) | .109 |
| 2 years | 2,565 (63.3) | 1,794 (64.6) | .296 |
| 3 years | 1,895 (46.8) | 1,282 (46.1) | .599 |
| 4 years | 1,506 (37.2) | 1,012 (36.4) | .522 |
| 5 years | 714 (17.6) | 455 (16.4) | .177 |
| Gaps, N (%) | |||
| 0 gaps | 2,632 (65.0) | 1,789 (64.4) | |
| 1 gap | 1,127 (27.8) | 786 (28.3) | |
| 2+ gaps | 292 (7.2) | 204 (7.3) | .880 |
| Mean duration of gap in days, mean (SE) | 274.2 (7.9) | 290.1 (10.1) | .214 |
Note. Percentages may add to over 100 due to rounding.
In Table 3, we explored the differences between the populations that opted out of each plan to ascertain whether their exit conferred any advantages or disadvantages to either plan in terms of the health status, expenditures, or complexity of their enrollee pools. Overall, more enrollees switched out of the Medicaid‐focused plan and into the mixed than vice versa (11.1 percent compared to 5.8 percent, respectively, p < .001). Those who did so were, on average, less complex patients with comparatively better health and higher socioeconomic status. Those who were assigned to the mixed plan but opted to enroll in the Medicaid focused plan were more likely to speak Spanish as a primary language and to be eligible because of pregnancy or disability status.
Table 3.
Descriptive Characteristics of Enrollees Who Defied Original Plan Assignment
| Variable | Assigned to Medicaid‐Focused Plan, Enrolled or Switched to Mixed Plan/FFS (N = 848) | Assigned to Mixed Plan, Enrolled or Switched to Medicaid‐Focused/FFS (N = 366) | p‐Value | Complied with Plan Assignment (N = 5,614) |
|---|---|---|---|---|
| Age | ||||
| <18 | 58.0 | 63.8 | 61.0 | |
| 18–45 | 34.6 | 32.2 | 33.2 | |
| 46–64 | 7.4 | 4.1 | .042 | 5.8 |
| Race/ethnicity | ||||
| White | 82 | 62 | 69 | |
| Black | 8 | 10 | 11 | |
| Asian/Pacific Islander | 2 | 2 | 4 | |
| Hispanic/Latino | 8 | 26 | 16 | |
| Native American | 0 | 0 | <.001 | 1 |
| Enrollment pathway | ||||
| Pregnancy | 2.8 | 6.0 | 5.6 | |
| Disability | 2.2 | 4.1 | 3.4 | |
| Child | 60.9 | 62.4 | 62.0 | |
| Parent/caretaker | 23.2 | 18.0 | 20.0 | |
| Adult other | 10.9 | 9.5 | .008 | 8.8 |
| Language | ||||
| English | 96.0 | 85.0 | 92.0 | |
| Spanish | 3.7 | 15.0 | 7.3 | |
| Other | .35 | .00 | <.000 | 0.80 |
| Residing in highest quintile of neighborhood disadvantage | 5.7 | 13.4 | <.000 | 10.4 |
| Historical utilization | ||||
| Any admission | 7.1 | 13.4 | <.001 | 9.8 |
| Any ED visits | 26.1 | 32.7 | .018 | 29.4 |
| >2 Doctor visits | 76.4 | 79.8 | .190 | 75.1 |
| Utilization prior to switch* | ||||
| Any admission | 1.2 | 5.4 | <.001 | |
| Any ED visit | 12.7 | 20.7 | .012 | |
| Any office visit | 59.4 | 79.9 | <.001 | |
| Health status | ||||
| Charlson comorbidity index (kids included) | ||||
| 1 | 4.6 | 7.9 | 4.9 | |
| 2 | 0.83 | 0.27 | 0.041 | 0.77 |
| Pollack children with special needs (<18 years old) | 27.0 | 31.7 | 0.233 | 28.9 |
Notes. This sample includes all enrollees who opted to enroll in the plan they were not assigned to at the time of randomization or switched after a period of enrollment in their originally assigned plan. It also includes those who were enrolled in fee‐for‐service as opposed to managed care, which means they were not covered by either managed care plan. p‐Value refers to the differences between the two plans. Nonswitchers’ demographics provided for comparison. p‐Values were computed using chi‐square tests for categorical variables, two‐sample t tests for continuous variables, and two‐sample t tests for differences between proportions.
*Captures utilization that occurred after random assignment but before the switch or opt out date or before 6 months had elapsed, whichever occurred first.
There were no significant differences in the mean number of months beneficiaries remained continuously enrolled; both groups were enrolled for an average of 33 months (~2.8 years) of undisrupted coverage. The proportion of enrollees who experienced 12 months of continuous coverage each year of follow‐up did not vary significantly between the two plans. These findings are displayed graphically in Figure 1, stratified by adults 18 and over versus children and adolescents 14 and under. While children exhibited higher rates of continuous coverage compared to adults overall, these rates did not vary by plan assignment. There were also no significant differences between the proportions of enrollees who experienced gaps in Medicaid coverage across the two plans, nor a significant difference in the duration of those gaps.
Figure 1.
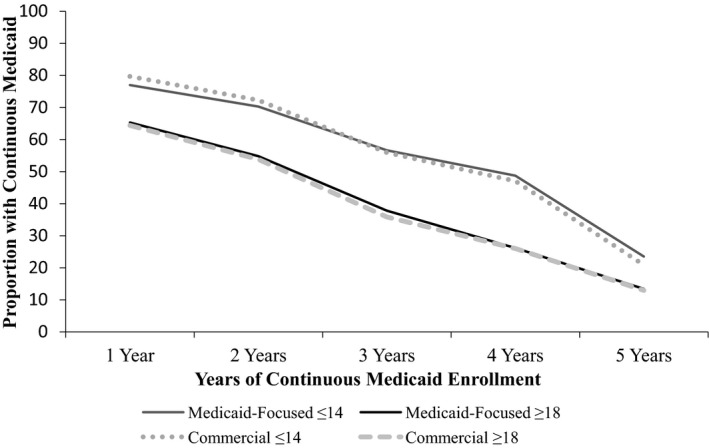
Proportion of Adults and Children with 1–5 Years of Continuous Medicaid Enrollment
Table 4 presents the adjusted results among the full sample at 3 years. We only present results for the 3‐year model because findings at other timepoints in the 5 years of follow‐up did not vary meaningfully (see Table S3). Conditional on all model covariates, those enrolled in the mixed plan did not have significantly different odds of staying continuously enrolled at 3 years of follow‐up, compared to those enrolled in the Medicaid‐focused plan. Enrollees’ sex, race/ethnicity, and neighborhood disadvantage did not increase or decrease the odds of continuous enrollment significantly. Stratified analyses of children and adults yielded similar findings (see Table S4). Excluding the imputed race/ethnicity variables did not alter these results.
Table 4.
Adjusted Impact of Medicaid Managed Care Plan Type on 3 Years of Continuous Medicaid Coverage
| Three Years of Continuous Medicaid Coverage | Full Sample, N = 6,830 |
|---|---|
| Mixed plan assignment | 0.97 (.075) |
| Eligibility | |
| Child | Ref |
| Pregnant | 0.63*** (.073) |
| Disabled | 1.18 (.168) |
| Parents/caretaker | 0.72*** (.047) |
| Low‐income adults | 0.64*** (.636) |
| Female | 0.98 (.048) |
| Language | |
| English | Ref |
| Spanish | 1.45** (.226) |
| Other | 0.37* (.167) |
| Charlson comorbidity index | |
| 0 | Ref |
| 1 | 1.10 (.132) |
| 2+ | 0.89 (.272) |
| Area deprivation index (quintiles) | 1.01 (.015) |
| Children with special needs | 1.30*** (.097) |
| Top quintile of admissions | 0.96 (.102) |
| Top quintile of ED visits | 0.94 (.083) |
| Top quintile outpatient visits | 1.69*** (.163) |
| Race/ethnicity | |
| White | Ref |
| Black | 0.90 (.111) |
| Asian | 1.19 (.253) |
| Hispanic | 0.87 (.987) |
| Native American | 0.99 (.417) |
Note. Exponentiated coefficients; Standard errors in parentheses.
*p < .05, **p < .01, ***p < .001.
Children had significantly higher odds of continuous enrollment compared to pregnant women, parents/caretakers, and low‐income adults. Spanish‐speaking enrollees had higher odds of continuous enrollment compared to English‐speaking enrollees. While the number of existing comorbidities at baseline was not associated with continuous coverage, children with special health care needs had significantly higher odds of continuous enrollment compared to children who did not have special health care needs (OR = 1.30; 95% CI: 1.13–1.51). The top 10 percent of utilizers of outpatient visits had significantly higher odds of continuous Medicaid enrollment compared to those who used fewer outpatient services (OR = 1.69; 95% CI: 1.40–2.04), although this trend did not follow for admissions and emergency department utilizations.
Our instrumental variable analysis revealed that those enrolled in the mixed plan gained 29 additional days of Medicaid enrollment compared to those enrolled in the Medicaid‐focused plan over the first two years of follow‐up (p = .029; see Table S5). Given the small magnitude of this effect, this result does not substantively alter our central findings.
The results from our secondary analysis comparing the randomized cohort to the directly assigned cohort are displayed in Table S1 (Table S1 compares baseline covariates between the randomized and directly assigned groups). Because plan administrators deliberately assigned the nonrandomized enrollees based on their providers, we observe systematic differences between the randomized and nonrandomized populations across several of the covariates at baseline, including age, race/ethnicity, reason for eligibility, primary language, and neighborhood disadvantage. Table S2 reports adjusted odds ratios for 3 years of continuous Medicaid coverage. Conditional on all covariates, we did not observe a significant association between randomization and continuity of Medicaid enrollment.
Discussion
We evaluated a novel natural experiment to assess whether assignment to two different types of Medicaid managed care plans impacted Medicaid retention. In our intention‐to‐treat analysis, we observed no significant differences in continuity of Medicaid coverage between Medicaid enrollees who were randomized to a mixed plan versus a Medicaid‐focused plan. These findings held across 5 years of follow‐up and among subsamples of adults and children.
Our instrumental variable analysis indicated that on average, enrollment in the mixed plan was associated with 2 weeks of additional coverage per year. For the vast majority of Medicaid enrollees, 2 weeks of coverage would not be expected to measurably affect health or well‐being. It is for this reason that we conclude that the practical significance of our instrumental variable findings is limited, particularly when considered in conjunction with the results of our intention‐to‐treat analysis. Taken together, these results suggest that in this setting, enrollment in either of the two Medicaid managed care plan types did not cause a meaningful impact on the duration of Medicaid beneficiaries’ enrollment.
In fully adjusted models, reason for Medicaid eligibility was strongly associated with duration of continuous Medicaid enrollment. Children had greater odds of continuous enrollment compared to all other eligibility groups. Children who had diagnoses of special needs had consistently longer spans of continuous Medicaid enrollment, and those in the highest quintile of outpatient care utilization had significantly lower odds of disrupted coverage, although these effects did not vary by plan assignment. We also observed no difference in continuous Medicaid enrollment rates between the population that was randomly assigned and the population that was directly assigned based on provider networks.
Prior studies have explored individual and regulatory predictors of churning, but to our knowledge, our study is the first to explore the role of managed care plans in determining Medicaid retention outcomes (Sommers 2009; Sommers et al. 2014). The finding that managed care plan type does not influence continuity of care is encouraging because it demonstrates that despite features that have the potential to affect enrollment, these features do not cause plans to push beneficiaries off their rolls or beneficiaries to disenroll earlier. One reason we may have observed no difference in continuity of coverage across plan type is that Medicaid managed care companies are highly regulated in the products they deliver to their beneficiaries and may ultimately have few levers through which to impact enrollee retention. The two plans may have provided a similar level of outreach and enrollment resources to beneficiaries to facilitate continuous coverage, had significant overlap in provider networks, and offered comparable quality of care.
Rates of 12 months of continuous Medicaid enrollment in this managed care population are approximately 10 percentage points lower than national averages over the same time period, but they followed similar patterns with children and the disabled population retaining coverage for longer periods (Ku and Steinmetz 2013). Our finding on the relationship between greater outpatient utilization and improved continuity of Medicaid coverage is consistent with studies of the Children's Health Insurance Program (CHIP), which showed that sustained contact with office‐based providers is an important pathway to continuous Medicaid enrollment (Davidoff and Garrett 2001; Phillips et al. 2004; Sommers 2006). This finding may be robust because providers and staff in clinics that serve low‐income populations are valuable sources of information about enrollment and renewal procedures or because greater contact with the health care system underscores the value of maintaining insurance (Feinberg et al. 2002). In contrast to prior work using national data, we did not find race/ethnicity, neighborhood disadvantage, or sex to be independent predictors of Medicaid retention in our study population (Klein, Glied, and Ferry 2005; Satchell and Pati 2005; Hill and Shaefer 2011). We also did not find disability‐based eligibility to be associated with greater odds of continuous enrollment compared to children, although this was likely due to the small number of persons with disabilities in the dataset or because children with special needs were not captured in the disability eligibility category.
Recent evidence has also shown that exits from the Medicaid managed care market occur frequently, with nearly 5 million Medicaid beneficiaries affected by market exits between 2006 and 2014 (Ndumele et al. 2017). As of March 2017, approximately half of state Medicaid programs contract with five or fewer managed care plans. This suggests that the exit of a single plan in these states can lead to disrupted coverage for a substantial portion of the market (Kaiser Family Foundation 2017). When this occurs, Medicaid officials in that region must decide the best approach for reenrolling the beneficiaries of that plan. In this study, Medicaid officials used a combination strategy of reassignment based on provider networks and random assignment. Our finding that the randomized cohort did not experience worse enrollment outcomes compared to the cohort assigned based on provider networks suggests these two approaches may be comparable in terms of Medicaid retention.
Other states employ similar approaches when beneficiaries do not select a plan within the required timeframe for initial enrollment. Medicaid departments have used beneficiary‐focused approaches such as assignment based on geography or the plan of a family member, or approaches that meet programmatic goals, such as assignment based on the plan's ability to achieve specified quality metrics or balancing the number of enrollees across plans (Kaiser Family Foundation 2011). Our results highlight one strategy for policymakers to implement in the case of plan turnover in the Medicaid managed care market that maintains equity, achieves balance across plan enrollment, and is not associated with worse Medicaid retention. Randomization also facilitates the study of important outcomes across plans because it generally ensures the comparison of demographically and clinically similar populations.
This study has several limitations. There were significant differences across plan assignment in the number of beneficiaries who enrolled in the plan to which they were assigned and in the number of beneficiaries who, after enrolling in their assigned plan initially, switched plans. Both of these patterns favor beneficiaries leaving the Medicaid‐focused plan in favor of the mixed plan, perhaps due to perceived superiority of a national plan with name recognition, or because these enrollees were previously enrolled in a mixed Medicaid managed care plan (BCBS).
Because of this, our intention‐to‐treat approach, which analyzed enrollees in the plan to which they were randomly assigned, may be biased toward the null in estimating the effect of the plan type on continuous coverage. However, because noncompliance in the overall sample was low (<10 percent), this bias is not expected to be large. To address this source of potential bias, we also conducted an instrumental variables analysis that examined the causal effect of plan enrollment (rather than plan assignment) on enrollee retention. The intention‐to‐treat analysis, which examined the effect of plan assignment, and the instrumental variable analysis, which assessed the effect of plan enrollment, yielded qualitatively similar findings.
Information on race/ethnicity was imputed for some enrollees due to missing race/ethnicity data in the claims. However, we used a validated approach that combined geographic and surname data to predict the race/ethnicity of those individuals with missing values. Despite random assignment, significant baseline differences in race/ethnicity persisted. We addressed this by including baseline covariates, including race/ethnicity, in all adjusted models. Plan‐specific determinants of continuity of coverage were not available to us, such as provider network information and outreach efforts. The data also lacked income and employment information that could distinguish Medicaid disenrollment from transitioning to other sources of coverage. In addition, we cannot infer a causal relationship from our analysis of the randomized versus directly assigned groups. Finally, our findings may not generalize to other states and managed care programs.
Random assignment has the potential to balance insurance enrollment across managed care plans and is one equitable strategy for policymakers to implement when auto‐assigning enrollees. We found that managed care plans did not differ considerably in their capacity to keep Medicaid beneficiaries continuously enrolled, despite differences in the features of the plans.
Supporting information
Appendix SA1: Author Matrix.
Table S1. 2011 Baseline Characteristics of Randomized and Non‐Randomized Samples.
Table S2. Adjusted Impact of Randomization on Three Years of Continuous Medicaid Coverage.
Table S3. Adjusted Impact of Medicaid Managed Care Plan Type on Annual Continuous Coverage among the Full Sample, 2011–2015.
Table S4. Adjusted Impact of Medicaid Managed Care Plan Type on Three Years of Continuous Medicaid Coverage among Adults 18 and Over and Children 14 and Under.
Table S5. Instrumental Variable Analysis of Impact of Plan Enrollment on Number of Days Continuously Enrolled in Medicaid.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was funded by the U.S. Department of Health and Human Services Health Resources and Service Administration Maternal and Child Health Bureau, and by the National Institutes of Health National Institute on Minority Health and Health Disparities. We would like to acknowledge Bill McQuade for his data assistance and Medicaid expertise.
Disclosure: None.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
- Adjaye‐Gbewonyo, D. , Bednarczyk R. A., Davis R. L., and Omer S. B.. 2014. “Using the Bayesian Improved Surname Geocoding Method (BISG) to Create a Working Classification of Race and Ethnicity in a Diverse Managed Care Population: A Validation Study.” Health Services Research 49 (1): 268–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aizer, A. , Currie J., and Moretti E.. 2007. “Does Managed Care Hurt Health? Evidence from Medicaid Mothers.” The Review of Economics and Statistics 89 (3): 385–99. [Google Scholar]
- Bindman, A. B. , Chattopadhyay A., and Auerback G. M.. 2008. “Interruptions in Medicaid Coverage and Risk for Hospitalization for Ambulatory Care‐Sensitive Conditions.” Annals of Internal Medicine 149 (12): 854–60. [DOI] [PubMed] [Google Scholar]
- Charlson, M. E. , Pompei P., Ales K. L., and MacKenzie C. R.. 1987. “A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation.” Journal of Chronic Diseases 40 (5): 373–83. [DOI] [PubMed] [Google Scholar]
- Davidoff, A. J. , and Garrett B.. 2001. “Determinants of Public and Private Insurance Enrollment among Medicaid‐Eligible Children.” Medical Care 39 (6): 523–35. [DOI] [PubMed] [Google Scholar]
- Duchon, L. , Schoen C., Doty M. M., Davis K., Strumpf E., and Bruegman S.. 2001. “Security Matters: How Instability in Health Insurance Puts US Workers at Risk” [accessed on August 28, 2017]. The Commonwealth Fund. Available at http://www.academia.edu/download/38369626/duchon_securitymatters_512_pdf
- Duggan, M. 2004. “Does Contracting out Increase the Efficiency of Government Programs? Evidence from Medicaid HMOs.” Journal of Public Economics 88 (12): 2549–72. [Google Scholar]
- Feinberg, E. , Swartz K., Zaslavsky A. M., Gardner J., and Walker D. K.. 2002. “Language Proficiency and the Enrollment of Medicaid‐Eligible Children in Publicly Funded Health Insurance Programs.” Maternal and Child Health Journal 6 (1): 5–18. [DOI] [PubMed] [Google Scholar]
- Gill, J. M. , Mainous A. G., Diamond J. J., and Lenhard M. J.. 2003. “Impact of Provider Continuity on Quality of Care for Persons with Diabetes Mellitus.” Annals of Family Medicine 1 (3): 162–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold, R. , DeVoe J., Shah A., and Chauvie S.. 2009. “Insurance Continuity and Receipt of Diabetes Preventive Care in a Network of Federally Qualified Health Centers.” Medical Care 47 (4): 431–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall, A. G. , Harman J. S., and Zhang J.. 2008. “Lapses in Medicaid Coverage: Impact on Cost and Utilization among Individuals with Diabetes Enrolled in Medicaid.” Medical Care 46 (12): 1219–25. [DOI] [PubMed] [Google Scholar]
- Harman, J. S. , Manning W. G., Lurie N., and Christianson J. B.. 2003. “Association between Interruptions in Medicaid Coverage and Use of Inpatient Psychiatric Services.” Psychiatric Services 54 (7): 999–1005. [DOI] [PubMed] [Google Scholar]
- Hill, H. D. , and Shaefer H. L.. 2011. “Covered Today, Sick Tomorrow? Trends and Correlates of Children's Health Insurance Instability.” Medical Care Research and Review 68 (5): 523–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation . 2011. “A Profile of Medicaid Managed Care Programs in 2010: Findings from a 50‐State Survey” [accessed on August 28, 2017]. Available at https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8220.pdf
- Kaiser Family Foundation . 2014. “Total Medicaid Managed Care Enrollment“ [accessed on August 28, 2017]. Available at http://www.kff.org/medicaid/state-indicator/totalmedicaid-mc-enrollment/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%2sort%22:%22asc%22%7D
- Kaiser Family Foundation . 2017. “Total Medicaid MCOs by State” [accessed on August 28, 2017]. Available at http://www.kff.org/medicaid/state-indicator/total-medicaid-mcos
- Kind, A. J. H. , Jencks S., Brock J., Yu M., Bartels C., Ehlenbach W., Greenberg C., and Smith M.. 2014. “Neighborhood Socioeconomic Disadvantage and 30‐Day Rehospitalization: A Retrospective Cohort Study.” Annals of Internal Medicine 161 (11): 765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein, K. , Glied S., and Ferry D.. 2005. “Entrances and Exits: Health Insurance Churning, 1998–2000.” Commonwealth Fund Issue Brief 855: 1–12. [PubMed] [Google Scholar]
- Koroukian, S. M. 2004. “Screening Mammography Was Used More, and More Frequently, by Longer Than Shorter Term Medicaid Enrollees.” Journal of Clinical Epidemiology 57 (8): 824–31. [DOI] [PubMed] [Google Scholar]
- Ku, L. , and Ross D. C.. 2002. “Staying Covered: The Importance of Retaining Health Insurance for Low‐Income Families.” Commonwealth Fund.
- Ku, L. , and Steinmetz E.. 2013. “Bridging the Gap: Continuity and Quality of Coverage in Medicaid” [accessed on August 28, 2017]. Available at http://ccf.georgetown.edu/wpcontent/uploads/2013/09/GW-Continuity-Report-9-10-13.pdf
- Long, S. K. , and Yemane A.. 2005. “Commercial Plans in Medicaid Managed Care: Understanding Who Stays and Who Leaves.” Health Affairs 24 (4): 1084–94. [DOI] [PubMed] [Google Scholar]
- McCue, M. J. , and Bailit M. H.. 2011. “Assessing the Financial Health of Medicaid Managed Care Plans and the Quality of Patient Care They Provide.” Commonwealth Fund. [PubMed]
- Milliman . 2016. “Medicaid Risk‐Based Managed Care: Analysis of Administrative Costs for 2015” [accessed on August 28, 2017]. Available at http://www.milliman.com/insight/2016/Medicaid-risk-based-managed-care-Analysis-of-administrative-costs-for-2015/
- Ndumele, C. D. , Schpero W. L., Schlesinger M. J., and Trivedi A. N.. 2017. “Association between Health Plan Exit from Medicaid Managed Care and Quality of Care, 2006–2014.” Journal of the American Medical Association 317 (24): 2524–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips, J. A. , Miller J. E., Cantor J. C., and Gaboda D.. 2004. “Context or Composition: What Explains Variation in SCHIP Disenrollment?” Health Services Research 39 (4p1): 865–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack, H. A. , Dombkowski K. J., Zimmerman J. B., Davis M. M., Cowan A. E., Wheeler J. R., Hillemeier A. C., and Freed G. L.. 2004. “Emergency Department Use among Michigan Children with Special Health Care Needs: An Introductory Study.” Health Services Research 39 (3): 665–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satchell, M. , and Pati S.. 2005. “Insurance Gaps among Vulnerable Children in the United States, 1999–2001.” Pediatrics 116 (5): 1155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommers, B. D. 2006. “Protecting Low‐Income Children's Access to Care: Are Physician Visits Associated with Reduced Patient Dropout from Medicaid and the Children's Health Insurance Program?” Pediatrics 118 (1): 36–42. [DOI] [PubMed] [Google Scholar]
- Sommers, B. D. . 2009. “Loss of Health Insurance among Non‐Elderly Adults in Medicaid.” Journal of General Internal Medicine 24 (1): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommers, B. D. , Graves J. A., Swartz K., and Rosenbaum S.. 2014. “Medicaid and Marketplace Eligibility Changes Will Occur Often in All States; Policy Options Can Ease Impact.” Health Affairs 33 (4): 700–7. [DOI] [PubMed] [Google Scholar]
- Swartz, K. , Short P. F., Graefe D. R., and Uberoi N.. 2015. “Evaluating State Options for Reducing Medicaid Churning.” Health Affairs 34 (7): 1180–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1. 2011 Baseline Characteristics of Randomized and Non‐Randomized Samples.
Table S2. Adjusted Impact of Randomization on Three Years of Continuous Medicaid Coverage.
Table S3. Adjusted Impact of Medicaid Managed Care Plan Type on Annual Continuous Coverage among the Full Sample, 2011–2015.
Table S4. Adjusted Impact of Medicaid Managed Care Plan Type on Three Years of Continuous Medicaid Coverage among Adults 18 and Over and Children 14 and Under.
Table S5. Instrumental Variable Analysis of Impact of Plan Enrollment on Number of Days Continuously Enrolled in Medicaid.


