Abstract
Objective
To quantify the impact of multiyear utilization of preventive dental services on downstream dental care utilization and expenditures for children.
Data Sources/Study Setting
We followed 0.93 million Medicaid‐enrolled children who were 3–6 years old in 2005 from 2005 to 2011. We used Medicaid claims data of Alabama, Georgia, Mississippi, North Carolina, South Carolina, and Texas.
Study Design
We clustered each state's study population into four groups based on utilization of topical fluoride and dental sealants before caries‐related treatment using machine learning algorithms. We evaluated utilization rates and expenditures across the four groups and quantified cost savings of preventive care for different levels of penetration.
Data Extraction Method
We extracted all dental‐related claims using CDT codes.
Principal Findings
In all states, Medicaid expenditures were much lower for children who received topical fluoride and dental sealants before caries development than for all other children, with a per‐member per‐year difference ranging from $88 for Alabama to $156 for Mississippi.
Conclusions
The cost savings from topical fluoride and sealants across the six states ranged from $1.1M/year in Mississippi to $12.9M/year in Texas at a 10 percent penetration level. Preventive dental care for children not only improves oral health outcomes but is also cost saving.
Keywords: Dental care, prevention policy, Medicaid, cost savings, pediatrics
Although preventable, dental caries (tooth decay) is among the most prevalent chronic conditions in U.S. children (Griffin et al. 2014). Untreated caries can lead to pain, infection, problems with eating and speaking, and missed school days (Jackson et al. 2011; Seirawan, Faust, and Mulligan 2012; Agaku et al. 2015).
Basic pediatric dental preventive services include dental prophylaxis (teeth cleaning), topical fluoride application, and dental sealants. There is no evidence that dental prophylaxis is effective in preventing dental caries (Badersten, Egelberg, and Koch 1975; Azarpazhooh and Main 2009; Sampson 2010). In contrast, there is strong evidence that the application of dental sealants (Werner, Pereira, and Eklund 2000; Beauchamp et al. 2008; Bertrand et al. 2011; Ahovuo‐Saloranta et al. 2013) and topical fluoride (Weintraub et al. 2006; Lawrence et al. 2008; Slade et al. 2011; Hendrix et al. 2013; Biordi et al. 2015) are effective prevention services. The American Academy of Pediatric Dentistry recommends application of dental sealants and topical fluoride as part of a comprehensive prevention strategy (American Academy of Pediatric Dentistry 2013). Further, several studies have found that fluoride varnish applied in medical settings prevents caries and is cost‐effective (Pahel et al. 2011; Stearns et al. 2012; Kranz et al. 2014).
While there is evidence for the prevention effectiveness of topical fluoride and dental sealants, there is no consensus on how those prevention services impact downstream dental care expenditures and outcomes (Kuo et al. 2015). For insured children, one study found that placing sealants resulted in reduced expenditures and an increase in the average number of caries‐free months per tooth (Quinonez et al. 2005) and that the reduction in expenditures was greater for at‐risk children. Other studies also suggested that targeting at‐risk children, such as those that are Medicaid‐enrolled, may be an effective strategy (Dennison, Straffon, and Smith 2000; Leskinen et al. 2008).
Among a cohort of 15,438 Medicaid‐enrolled children in North Carolina followed during 1985–1992, sealants were found to be cost saving within 2 years if children were at high risk for caries (Weintraub et al. 2001). In a cohort of 9,549 Medicaid‐enrolled children in Alabama followed during 1990–1997, those who did not have sealant claims were four times more likely than those with at least one sealant claim to have subsequent restorative care (Dasanayake et al. 2003). A cohort study of 14,972 CHIP‐enrolled children aged < 8 years in Alabama found that more dental preventive visits were associated with fewer nonpreventive dental visits, although they were not found to be cost saving (Sen et al. 2013). For primary teeth, a tooth‐level Markov model based on claims from children enrolled in Iowa Medicaid from 2008 to 2011 found that sealing primary molars helped prevent restorations and extractions, but it was more costly than not sealing (Chi, van der Goes, and Ney 2014). Fluoride varnish may improve health outcomes in Medicaid‐enrolled children, but it has not always been found to be cost saving (Quinonez et al. 2006). The Into the Mouths of Babes program in North Carolina, in which fluoride varnish was regularly applied to Medicaid‐enrolled children, found a 32 percent probability of being cost saving at its current reimbursement rate. However, at a lower reimbursement rate, the probability of being cost saving was nearly 100 percent (Stearns et al. 2012).
In this study, we assessed how topical fluoride treatments and dental sealants (either primary or permanent molars) together impacted overall downstream dental care expenditures and outcomes in six states using multiyear longitudinal utilization for dental care derived from patient‐level claims. Those six states—Alabama, Georgia, Mississippi, North Carolina, South Carolina, and Texas—were selected because of their differences in the level of utilization of preventive dental care (American Dental Association Health Policy Institute 2015) and variations in state‐level oral health policies (Government Accountability Office 2010; Centers for Medicare & Medicaid Services 2013, 2014). The study population consisted of young children who were 3–6 years old in 2005, relatively healthy, and enrolled in Medicaid for at least five of seven consecutive years (2005–2011).
To estimate the impact of utilization behaviors on associated costs, we clustered patient‐level data derived from the Medicaid Analytic Extract (MAX) claims files based on the utilization of topical fluoride and sealants before restorative care treatment was provided. We used only the child's preventive care events before any caries‐related treatment event because children who had not utilized preventive care commonly received preventive services shortly after their first caries‐related treatment. Outcome measures were compared across the patient clusters.
Using patient‐level detailed utilization data over multiple years for a large population of young children, we were able to longitudinally determine the temporal relationship between preventive and restorative dental care.
Methods
Data Source
We used Medicaid Analytic Extract (MAX) claims data for 7 years (2005–2011) acquired from the Centers for Medicare and Medicaid Services (CMS). The data consisted of patient‐level claims for all Medicaid‐enrolled beneficiaries in Alabama, Georgia, Mississippi, North Carolina, South Carolina, and Texas. The data extraction process is detailed in Appendix SA2. This study was approved by our institution's Institutional Review Board (protocol number H11287) and by CMS (Data Use Agreement #23621).
Study Population
We estimated the costs of varying utilization behaviors for the study population that consisted of children who were 3–6 years old in 2005, enrolled in Medicaid for at least 60 of 84 months, and utilized dental care at least once for the 7 years. The age range of 3–6 years was chosen to ensure covering the age range 6–7 years, when the application of sealants is recommended, and the immediate years following. To avoid bias due to complex health conditions (Herndon et al. 2015), we excluded children whose Clinical Risk Grouping (CRG), derived using the 3M CRG Software, were not among Healthy, Recent History of Significant Acute Disease, Single or Multiple Minor Chronic Disease, or Single Moderate Chronic Disease (CRGs 1–4 or 5a). Table 1 shows the numbers of children in each state excluded due to these criteria.
Table 1.
Number of Children Excluded in the Cost Estimation
| Alabama | Georgia | Mississippi | North Carolina | South Carolina | Texas | |
|---|---|---|---|---|---|---|
| Medicaid‐enrolled children aged 3–6 years in 2005 | 115,912 | 277,052 | 83,065 | 208,854 | 105,875 | 682,908 |
| Excluded due to health conditions (CRG 5b or 6–9) | −4,423 | −7,028 | −2,784 | −8,788 | −3,970 | −18,750 |
| Excluded as enrolled less than 5 years | −35,379 | −92,601 | −24,926 | −44,132 | −25,775 | −227,580 |
| Excluded as having no utilization event | −4,701 | −13,238 | −3,017 | −12,269 | −1,800 | −10,702 |
| Total subject population | 71,409 | 164,185 | 52,338 | 143,665 | 74,330 | 425,876 |
Based on the costs estimated, we projected the potential cost savings from providing preventive care. The target population for quantifying the future cost savings consisted of children aged 3–6 years in 2011 and CRGs 1–4 and 5a. That is, the future cost‐savings analysis included children regardless of whether they utilized dental care.
Translating Claims into Patient‐Level Longitudinal Utilization
We extracted all dental‐related claims and translated the claims into utilization events. An event was a summary of care provided to a child within a day, obtained by aggregating dental care claims by service date. Based on the Code on Dental Procedures and Nomenclature (CDT), we categorized utilization events as evaluation (“EV”), preventive care, or restorative care.
Preventive care included “FL” (topical fluoride, applied in either a dental or medical setting), “SE” (pit and fissure sealants), and “FL_SE” (both FL and SE in one visit). In all six states, Medicaid reimbursed physicians for providing fluoride varnish. For three of the six states (Georgia, North Carolina, and South Carolina), CDT was used in the claims during our study period. In the other three states (Alabama, Mississippi, and Texas), Medicaid reimbursed physicians only for fluoride varnish provided to children younger than 3 years of age. Those children were not included in our analysis. Regarding sealants, three of the six states (Alabama, Mississippi, and South Carolina) did not reimburse sealants on primary teeth. For the other three (Georgia, North Carolina, and Texas), our study included sealants on both primary and permanent molars as they were not distinguished in claims data.
Restorative care included “OV” (office visit for less severe caries‐related treatment), “SevOV” (office visit for severe caries‐related treatment), and “Out” (outpatient hospital visit for caries‐related treatment). Restorative care events were categorized based on the place of service and caries‐related CDT codes into “severe” and “less severe” treatments.
We also extracted monthly enrollment records to account for lapses in enrollment across the seven‐year period. Data censoring events, “LC” (left censoring) and “RC” (right censoring), were added for the entry and exit points, respectively.
For each child in the study population, we used dental care events and their chronologically ordered time stamps to define the child's longitudinal utilization sequence during the enrollment years. To simplify the presentation, we included EV as one of the services that would define a preventive care visit. Details regarding the derivation of the utilization sequences are in Appendix SA2.
Outcome Measures
The primary outcome measure was the Medicaid expenditures per member per year (PMPY), stratified by event type. We computed Medicaid PMPY expenditures of an event type for a given population as the total amount paid by Medicaid due to the event type for the population divided by the total enrollment years of the population. All dollar amounts were converted to 2015 U.S. dollars using the medical cost inflation (Bureau of Labor Statistics 2013).
Medicaid expenditures were derived from Medicaid payments, which were available for all claims and for all states except Georgia. In Georgia, claims for those children whose care was delivered under Dental Managed Organizations did not have information about the Medicaid payments. To impute the payments for these claims, we used the Medicaid fee schedule for Georgia (Georgia Department of Public Health 2013).
Additional outcome measures included the following:
The average PMPY rate for an event computed as the total number of events the population had over the study period divided by the total enrollment years of the population. Outcome measures in this category were the average PMPY rate for dental visits, for preventive services, for FL, and for caries‐related treatments. The average PMPY rate for FL before any caries was computed as the total number of FL events before the first caries treatment divided by the total enrollment years before the first caries treatment for the population.
The proportion of children that had an event for a given population was computed as the total number of children in the population who had the event at least once during the study period divided by the size of the population. Outcome measures in this category were the proportion of children that received SE, received SE before any caries, and received any caries treatment.
The use of claims data prevented us from observing caries in children who did not receive caries‐related treatments, which may have been due to access barriers (Government Accountability Office 2010). To address this limitation, we also estimated the proportion of children that experienced caries among the Medicaid population from the National Health and Nutrition Examination Survey (NHANES; Centers for Disease Control and Prevention [CDC] 2016). We first fitted logistic regression models (Cao et al. 2017) using NHANES participants insured by Medicaid or their state Children's Health Insurance Program (CHIP). For each state, we simulated the Medicaid‐eligible population at the census tract level and estimated caries prevalence for all census tracts using the regression model. We then aggregated the census tract‐level prevalence into a state‐level estimate. Details of the regression model for estimation of caries prevalence are provided in Appendix SA3. We compared the proportion of children that experienced caries estimated using NHANES to the proportion of children that had any caries‐related claim.
Cost‐Savings Analysis
In order to quantify the impact of preventive care, we classified the utilization sequences based on whether the child received repeated FL and/or SE before his or her first caries treatment event: Group 1 did not receive either FL or SE; Group 2 received SE only; Group 3 received FL only; and Group 4 received both FL and SE. For this classification, we used preventive events before any caries‐related treatment in order to avoid any bias introduced by children who saw a dentist due to dental caries and then received preventive care. The clustering approach for dividing children into the four groups used a Markov renewal process (MRP) (Foufoula‐Georgiou and Lettenmaier 1987), along with an (unsupervised) classification algorithm.
We used the MRP to represent utilization behavior because it accounted for the order of events and elapsed time between events. For each pair of event types, a transition probability was estimated along with an interevent time distribution. For example, the transition probability from EV to SE was the probability that a child had an SE applied after an oral examination, where the interevent time between EV and SE was an exponential random variable.
Figure 1 illustrates the MRP representations of utilization behaviors. For example, children with a utilization pattern shown in Figure 1a received FL with probability equal to 0.97, at an average of 2 years after entry. FL was repeated with probability 0.44 with an average interevent time between FL applications of 0.9 years. The other possibility after FL was that there was no other receipt of services until the end of the study (RC). Thus, the children in the first pattern received FL one or more times but did not receive any caries‐related treatment. Children in Figure 1b had an OV with probability 0.53 after an EV, with an average transition time estimated at 0.20 years. The probability of a repeating OV was 0.19. They received FL with probability 0.34 after an EV, without repeating it.
Figure 1.
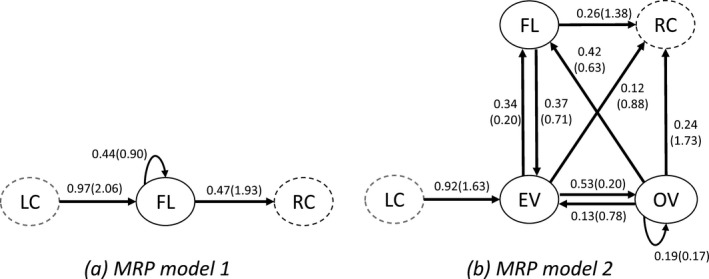
Illustrative Utilization Patterns Represented as Markov Renewal Process
Note. The numbers on each arrow are the transition probability and the average interevent time in years in parentheses. The network graph summarizes 90 percent of the volume of encounters; edges with transition probabilities <.1 were omitted for ease of interpretation.
In the classification process, we used the expectation‐maximization (EM), a standard method for parameter estimation in model‐based clustering (Do and Batzoglou 2008). We determined the number of clusters using the Bayesian information criterion (BIC) (Schwarz 1978; Jones 2011), which balances the trade‐off between identifying heterogeneous patterns within a population and keeping the number of clusters small. Output of the algorithm is an optimal classification of utilization sequences into clusters so that children in the same cluster behave similarly, while children in different clusters exhibit heterogeneous behaviors. We regrouped the clusters into the four utilization groups (Groups 1–4) based on a priori rules on the probabilities they received SE before caries, received FL before caries, and received repeated FL. Further details about the clustering are provided in Appendix SA4.
We used the PMPY rate of caries‐related treatments and PMPY Medicaid expenditures of the four utilization groups to estimate the potential impact of preventive care utilization on the downstream utilization of restorative dental care and resulting Medicaid expenditures. Again, the target population of this cost‐savings projection was children who were enrolled in Medicaid in 2011, aged 3–6 years, and in CRGs 1–5a. The baseline number of caries‐related treatments per year and the baseline Medicaid expenditures per year were computed as POP · r and POP · M, respectively, where POP denotes the size of the target population, and r and M represent the population PMPY caries rate and the population PMPY Medicaid expenditures computed as reported previously.
We assumed a constant marginal change for the different levels of penetration when computing the changes of the number of caries‐related treatments and Medicaid expenditures. For a change of utilization behavior from Group i to Group j and a given penetration percentage p, the resulting change of caries‐related treatments per year was computed as p · POP · (r i – r j), where r i is the PMPY caries rate of Group i. The corresponding change of Medicaid expenditures per year was computed as p · POP · (M i – M j), where M i denotes the PMPY Medicaid expenditures of Group i.
Results
Outcome Measures
Table 2 summarizes dental care utilization and expenditures for the study population by state. South Carolina had the highest rate of preventive visits (1.01 PMPY) and Georgia had the lowest rate (0.69 PMPY). The average rate of FL PMPY ranged from 0.56 in Mississippi to 0.87 in South Carolina. Texas and North Carolina had higher proportions of children that received SE (53.1 and 49.6 percent, respectively) than the other four states. Of the children who received SE, fewer than half received SE before any caries treatment during the entire study period in each state except North Carolina.
Table 2.
Dental Care Utilization and Expenditures Outcome Measures for Medicaid Children Aged 3–6 years in 2005 in the Six States, 2005–2011a
| Outcome Measure | State | |||||
|---|---|---|---|---|---|---|
| Alabama | Georgia | Mississippi | North Carolina | South Carolina | Texas | |
| Number of Children | 71,409 | 164,185 | 52,338 | 143,665 | 74,330 | 425,876 |
| Gender % (Female) | 49.7 | 49.6 | 49.3 | 49.8 | 49.1 | 49.2 |
| Age % (3/4/5/6) | 26.4/25.7/25.1/22.8 | 26.1/25.9/25.1/22.9 | 26.5/26.0/25.4/22.0 | 26.2/26.0/25.2/22.5 | 25.0/25.8/25.4/23.8 | 28.4/25.8/24.2/21.6 |
| Years Enrolled | 6.70 | 6.71 | 6.67 | 6.80 | 6.75 | 6.65 |
| Preventive/Caries Visitsb PMPYc | 1.35 | 1.06 | 1.15 | 1.18 | 1.54 | 1.33 |
| Preventive Visits PMPY | 0.84 | 0.69 | 0.75 | 0.74 | 1.01 | 0.82 |
| Fluoride PMPY | 0.71 | 0.61 | 0.56 | 0.61 | 0.87 | 0.62 |
| Fluoride before Caries PMPY | 0.59 | 0.56 | 0.50 | 0.52 | 0.76 | 0.57 |
| Received Sealant (%) | 25,290 (35.4) | 57,568 (35.1) | 20,843 (39.8) | 71,321 (49.6) | 33,394 (44.9) | 226,317 (53.1) |
| Received Sealant before Caries (%) | 10,003 (14.0) | 27,339 (16.7) | 9,151 (17.5) | 40,201 (28.0) | 12,805 (17.2) | 92,048 (21.6) |
| Medicaid Expenditure PMPY ($) | 150.94 | 170.07 | 211.58 | 219.06 | 211.47 | 269.01 |
| Caries Treatment Visits PMPY | 0.51 | 0.37 | 0.39 | 0.44 | 0.53 | 0.51 |
| Received Caries Treatment (%) | 60,616 (84.9) | 126,687 (77.2) | 41,723 (79.7) | 116,060 (80.8) | 64,029 (86.1) | 382,121 (89.7) |
| Had Caries in the Past 2 years (%)d | 67.0 | 64.6 | 62.6 | 66.4 | 64.9 | 66.7 |
Children aged 3–6 years in 2005, enrolled in Medicaid for at least 60 months of 84, utilized dental care at least once, and in CRGs 1–5a.
Preventive visits include only topical fluoride, sealant, and evaluation. Caries visits are visits including any caries‐related procedure, listed in eTable 1 of Appendix SA2.
Per member per year.
Not estimated from the MAX claims data, but obtained from the regression model.
The average Medicaid expenditure PMPY was highest in Texas ($269.01) and lowest in Alabama ($150.94). The proportion of children who received any caries‐related treatment during the 7 years was highest in Texas (89.7 percent) and lowest in Georgia (77.2 percent).
For all six states, the treated prevalence of caries for the study population was consistently higher when estimated for the entire study period (ranging from 77.2 percent for Georgia to 89.7 percent for Texas) as compared to the prevalence of caries for Medicaid‐enrolled children estimated over 2 years using the external data (ranging from 62.6 percent for Mississippi to 67.0 percent for Alabama). The utilization PMPY for restorative care ranged from 0.37 for Georgia to 0.53 for South Carolina.
Cost‐Savings Analysis
Table 3 shows the outcome measures of the four utilization groups in each state. Groups 1 and 2 had distinctively lower rates of FL before any caries compared with those in Groups 3 and 4, and Groups 1 and 3 had distinctively lower proportions of children receiving SE before any caries, compared with Groups 2 and 4. The visit rates (including preventive or caries treatment visits) of Group 2 consistently were lower than that of the other groups across all states. However, Groups 1, 3, and 4 had relatively similar rates of visits in each state. A graphical representation of their utilization patterns is in Appendix SA5.
Table 3.
Outcome Measures of the Four Utilization Groups from the Six States, 2005–2011a
| State | Alabama | Georgia | Mississippi | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Groupb | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 |
| Number of Children (%) | 42,567 (59.6) | 2,265 (3.2) | 21,217 (29.7) | 5,360 (7.5) | 90,903 (55.4) | 6,474 (3.9) | 50,057 (30.5) | 16,751 (10.2) | 29,683 (56.7) | 2,526 (4.8) | 16,085 (30.7) | 4,044 (7.7) |
| Fluoride before Caries PMPYc | 0.31 | 0.33 | 0.83 | 0.91 | 0.32 | 0.30 | 0.73 | 0.78 | 0.27 | 0.31 | 0.71 | 0.67 |
| Received Sealant before Caries (%) | 282 (0.7) | 2,123 (93.7) | 2,377 (11.2) | 5,221 (97.4) | 1,480 (1.6) | 6,470 (99.9) | 3,824 (7.6) | 15,565 (92.9) | 775 (2.6) | 2,526 (100.0) | 2,046 (12.7) | 3,804 (94.1) |
| Preventive/Caries Visitsd PMPY | 1.38 | 0.77 | 1.38 | 1.26 | 1.07 | 0.62 | 1.12 | 1.00 | 1.16 | 0.72 | 1.24 | 0.93 |
| Medicaid Expenditure PMPY ($) | 177.41 | 87.52 | 120.36 | 89.14 | 209.23 | 95.50 | 134.93 | 93.46 | 253.47 | 111.10 | 179.23 | 97.56 |
| Expenditure Reduction from Group 1 | 50.7% | 32.2% | 49.8% | 54.4% | 35.5% | 55.3% | 56.2% | 29.3% | 61.5% | |||
| Expenditure for Preventive Services PMPY ($) | 35.25 | 38.19 | 47.33 | 59.59 | 37.39 | 41.76 | 50.61 | 63.82 | 44.23 | 47.90 | 57.66 | 64.82 |
| Expenditure for Caries Treatment PMPY ($) | 142.16 | 49.33 | 73.03 | 29.55 | 171.84 | 53.74 | 84.31 | 29.64 | 209.24 | 63.20 | 121.56 | 32.74 |
| Expenditure for OVe Event PMPY ($) | 83.79 | 35.88 | 51.21 | 24.66 | 80.40 | 37.72 | 52.23 | 22.54 | 66.50 | 38.20 | 46.05 | 19.73 |
| Expenditure for SevOVf Event PMPY ($) | 51.68 | 13.28 | 20.01 | 4.89 | 55.81 | 14.83 | 23.98 | 6.42 | 28.23 | 15.02 | 18.49 | 5.83 |
| Expenditure for Outg Event PMPY ($) | 6.68 | 0.17 | 1.82 | 0.00 | 35.64 | 1.19 | 8.11 | 0.69 | 114.51 | 9.98 | 57.02 | 7.18 |
| Caries Treatment Visits PMPY | 0.63 | 0.25 | 0.38 | 0.19 | 0.46 | 0.20 | 0.30 | 0.12 | 0.48 | 0.26 | 0.32 | 0.12 |
| Reduction from Group 1 | 60.4% | 40.0% | 70.7% | 57.8% | 35.8% | 73.6% | 45.6% | 34.2% | 74.9% | |||
| Received Caries Treatment (%) | 40,140 (94.3) | 1,236 (54.6) | 16,588 (78.2) | 2,652 (49.5) | 79,832 (87.8) | 3,489 (53.9) | 36,662 (73.2) | 6,704 (40.0) | 26,833 (90.4) | 1,637 (64.8) | 11,769 (73.2) | 1,484 (36.7) |
| State | North Carolina | South Carolina | Texas | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 |
| Number of Children (%) | 78,142 (54.4) | 16,039 (11.2) | 27,627 (19.2) | 21,857 (15.2) | 38,576 (51.9) | 1,931 (2.6) | 24,233 (32.6) | 9,590 (12.9) | 249,058 (58.5) | 23,699 (5.6) | 102,797 (24.1) | 50,322 (11.8) |
| Fluoride before Caries PMPY | 0.31 | 0.36 | 0.73 | 0.72 | 0.43 | 0.36 | 0.94 | 0.95 | 0.28 | 0.41 | 0.85 | 0.77 |
| Received Sealant before Caries (%) | 1,160 (1.5) | 16,039 (100.0) | 3,123 (11.3) | 19,879 (91.0) | 240 (0.6) | 1,734 (89.8) | 1,536 (6.3) | 9,295 (96.9) | 6,886 (2.8) | 23,541 (99.3) | 15,651 (15.2) | 45,970 (91.4) |
| Preventive/Caries Visits PMPY | 1.24 | 0.95 | 1.26 | 1.07 | 1.61 | 0.96 | 1.57 | 1.29 | 1.31 | 1.07 | 1.49 | 1.19 |
| Medicaid Expenditure PMPY ($) | 266.77 | 168.01 | 183.73 | 131.31 | 263.18 | 124.45 | 177.93 | 106.67 | 302.88 | 232.77 | 250.34 | 156.70 |
| Expenditure Reduction from Group 1 | 37.0% | 31.1% | 50.8% | 52.7% | 32.4% | 59.5% | 23.1% | 17.3% | 48.3% | |||
| Expenditure for Preventive Services PMPY ($) | 44.27 | 67.60 | 57.11 | 81.54 | 47.91 | 45.25 | 57.18 | 66.40 | 46.48 | 70.83 | 62.63 | 84.92 |
| Expenditure for Caries Treatment PMPY ($) | 222.50 | 100.42 | 126.62 | 49.77 | 215.27 | 79.20 | 120.75 | 40.27 | 256.40 | 161.94 | 187.71 | 71.79 |
| Expenditure for OV Event PMPY ($) | 103.14 | 71.82 | 70.69 | 35.30 | 111.15 | 51.32 | 73.59 | 29.77 | 127.40 | 107.55 | 101.91 | 47.90 |
| Expenditure for SevOV Event PMPY ($) | 67.37 | 24.59 | 32.31 | 9.91 | 89.22 | 26.08 | 39.49 | 9.81 | 96.60 | 49.74 | 64.69 | 20.73 |
| Expenditure for Out Event PMPY ($) | 51.99 | 4.01 | 23.62 | 4.57 | 14.90 | 1.79 | 7.67 | 0.69 | 32.39 | 4.65 | 21.12 | 3.15 |
| Caries Treatment Visits PMPY | 0.56 | 0.36 | 0.37 | 0.18 | 0.68 | 0.31 | 0.44 | 0.18 | 0.59 | 0.42 | 0.47 | 0.20 |
| Reduction from Group 1 | 35.6% | 32.8% | 66.9% | 55.0% | 35.5% | 74.3% | 29.7% | 21.3% | 66.3% | |||
| Received Caries Treatment (%) | 71,534 (91.5) | 12,354 (77.0) | 21,898 (79.3) | 10,274 (47.0) | 37,496 (97.2) | 1,264 (65.5) | 20,688 (85.4) | 4,581 (47.8) | 241,184 (96.8) | 20,652 (87.1) | 95,834 (93.2) | 24,451 (48.6) |
Children aged 3–6 years in 2005, enrolled in Medicaid for at least 60 months of 84, utilized dental care at least once, and in CRGs 1–5a.
Group definition—1: receiving none, 2: receiving sealant only, 3: receiving repeated fluoride only, 4: receiving both (all before caries).
Per member per year.
Preventive visits include only topical fluoride, sealant, and evaluation. Caries visits are visits including any caries‐related procedure, listed in eTable 1 of Appendix SA2.
Dentist office visit for less severe caries‐related treatment. For details of the categorization of less severe and severe caries‐related treatment, see Appendix SA2.
Dentist office visit for severe caries‐related treatment.
Outpatient hospital visit for caries‐related treatment.
Medicaid expenditures for groups that utilized either repeated FL, SE, or both (Groups 2, 3, and 4) consistently were lower than expenditures of the group with neither repeated FL nor SE (Group 1) across all states. Further, the group that received both services (Group 4) had lower expenditures than the group receiving only repeated FL (Group 3), across all states. Children that received both (Group 4) had lower expenditures than those receiving only SE (Group 2) in all states except Alabama. The reduction of expenditures from utilizing no preventive service (Group 1) to utilizing SE (Group 2) ranged from 23.1 to 56.2 percent, from none (Group 1) to repeated FL (Group 3) was 17.3 to 35.5 percent, and from none (Group 1) to both (Group 4) was 48.3 to 61.5 percent.
Medicaid expenditures due to caries treatments were much lower for those who used a preventive service (Groups 2 and 3) than for children utilizing none (Group 1). Across all states, children who received both preventive services (Group 4) had lower restorative care expenditures than those who utilized only one (Groups 2 and 3). Caries treatment expenditures were stratified by the types of caries treatment events (OV, SevOV, Out), and the difference in expenditure between Groups was the greatest (percentage wise) for Out event, followed by SevOV, and then OV.
The rates of caries‐related treatments for those receiving only one service (Groups 2 and 3) were lower than those receiving none (Group 1), and the rate for utilizing both (Group 4) was lower than for utilizing only one service (Groups 2 and 3), across all states. Relative to the rate of utilizing none (Group 1), the reduction in caries treatment rate of utilizing sealant (Group 2) ranged from 29.7 to 60.4 percent, utilizing repeated FL (Group 3) was 21.3 to 40.0 percent, and utilizing both (Group 4) was 66.3 to 73.9 percent.
Table 4 shows the projected reductions in the number of caries‐related treatments and Medicaid expenditures from changing utilization behavior before any caries develops from receiving none (Group 1) to receiving FL repeatedly (Group 3) and from receiving none (Group 1) to receiving both (Group 4). The second column shows the size of the subject population of the six states. For example, in Texas, there were 882,878 children in the subject population, the baseline number of caries‐related treatments of the population was 447.0 (in thousands) per year, and the Medicaid expenditures were $237.5 million per year. If 10, 20, or 30 percent of the population switched their utilization behavior from Groups 1 to 3 throughout the study period, then the total number of caries‐related treatments per year would be reduced by 11.1, 22.3, and 33.4 (in thousands), respectively, and the Medicaid expenditures per year would be reduced by $4.6M, $9.3M, and $13.9M, respectively. If 10, 20, or 30 percent of the population switched their utilization behavior from utilizing none (Group 1) to utilizing both (Group 4) throughout the study period, then the total number of caries‐related treatments per year would be decreased by 34.7, 69.4, and 104.1 (thousands), respectively, and the Medicaid expenditures per year would be reduced by $12.9M, $25.8M, and $38.7M, respectively.
Table 4.
Projected Caries Reduction and Medicaid Cost Savings Associated with Changes in Utilization of Dental Preventive Services
| State | N a | Baseline Cariesb (per year) | Baseline Medicaid Cost (per year) | Caries Reduction/Cost Savings (per year) | |||||
|---|---|---|---|---|---|---|---|---|---|
| If the Percentage Starts Utilizing Fluoride Repeatedly | If the Percentage Starts Utilizing Fluoride and Dental Sealants | ||||||||
| 10% | 20% | 30% | 10% | 20% | 30% | ||||
| Alabama | 140,086 | 71.9k | $21.1M | 3.6k/$0.8M | 7.1k/$1.6M | 10.7k/$2.4M | 6.3k/$1.2M | 12.6k/$2.5M | 18.9k/$3.7M |
| Georgia | 301,469 | 110.8k | $51.3M | 5.0k/$2.2M | 10.0k/$4.5M | 15.0k/$6.7M | 10.3k/$3.5M | 20.6k/$7.0M | 30.9k/$10.5M |
| Mississippi | 70,879 | 27.9k | $15.0M | 1.2k/$0.5M | 2.3k/$1.1M | 3.5k/$1.6M | 2.6k/$1.1M | 5.1k/$2.2M | 7.7k/$3.3M |
| North Carolina | 297,397 | 131.6k | $65.1M | 5.4k/$2.5M | 10.9k/$4.9M | 16.3k/$7.4M | 11.1k/$4.0M | 22.1k/$8.1M | 33.2k/$12.1M |
| South Carolina | 142,113 | 75.2k | $30.1M | 3.5k/$1.2M | 6.9k/$2.4M | 10.4k/$3.6M | 7.2k/$2.2M | 14.4k/$4.4M | 21.7k/$6.7M |
| Texas | 882,878 | 447.0k | $237.5M | 11.1k/$4.6M | 22.3k/$9.3M | 33.4k/$13.9M | 34.7k/$12.9M | 69.4k/$25.8M | 104.1k/$38.7M |
Children enrolled in Medicaid in 2011, 3–6 years of age in 2011, and in CRGs 1–5a.
The total number of caries‐related treatments per year.
Discussion
Overall, we found that preventive dental care including topical fluoride, sealants, or both was cost saving for relatively healthy young children enrolled in Medicaid. In all states except Alabama, utilizing sealants alone was cost saving according to our analysis, but one caveat is that this group had low dental care utilization overall.
Cost savings were substantial at a 10 percent penetration of preventive care, as recommended by the Oral Health Initiative (Centers for Medicare & Medicaid Services 2011). The cost savings across the six states ranged from $1.1M/year in Mississippi to $12.9M/year in Texas at the 10 percent penetration level, within a 7‐year period. That is, if 10 percent of young children within the state would have received FL once per year and SE at the appropriate age, the cost savings would amount to $7.7M for Mississippi and $90.3M for Texas over 7 years.
The level of cost savings differed among the states due to differences in child population size, utilization rates, and state fee scales for dental procedures. Texas had more than 850,000 children in the target population and also had the highest per‐member spending among the six states. Georgia, with the next largest target population (about 300,000 children), spent less than 80 percent of what other states (except Alabama) spent during the study period. That difference is because Georgia had the lowest utilization rates for preventive or restorative care among all states in the study, and it had a lower fee scale for restorative services than several other states (SC Department of Health and Human Services 2011; Georgia Department of Public Health 2013; Alabama Medicaid Agency 2016; NC Division of Medical Assistance 2016; Texas Medicaid & Healthcare Partnership 2016; The Mississippi Division of Medicaid 2016).
Several previous studies of Medicaid‐enrolled children have not found as high a level of cost savings for dental sealants and topical fluoride as our estimates. One recent study showed that preventive oral health care provided in a primary care setting significantly reduced the likelihood of having a caries‐related hospital episode but had only a 32 percent chance of being cost saving (Stearns et al. 2012). There are several possible reasons for this difference. First, we used a larger study population and controlled for bias through the initial clustering procedure. Second, the study population was enrolled in Medicaid for at least 5 years over a 7‐year horizon, which is a longer time period than was used in most previous studies (Weintraub et al. 2001; Pahel et al. 2011; Beil et al. 2012; Stearns et al. 2012; Sen et al. 2013; Kranz et al. 2014). Because dental caries often takes many months to progress to a point at which restorative care is required, studies that used a shorter length may not capture as much downstream treatment costs. Third, previous studies have been limited to measuring the impact of preventive dental care for a single utilization event, such as the timing of the first dental visit or whether a child received a sealant (Weintraub et al. 2001; Kleinman 2002; Savage et al. 2004; Beil et al. 2012, 2014; Marinho et al. 2013; Griffin, Jones, and Crespin 2014).
Our methodology is rather general and can therefore be applied beyond the present study population. It may be applicable for projecting cost savings associated with various state Medicaid interventions such as “Into the Mouths of Babes” in North Carolina (Rozier et al. 2003, 2010) along with those of Connecticut and Maryland that led to an increase in Medicaid reimbursement rates (Nasseh and Vujicic 2015).
Limitations
There are several limitations of this study. First, utilization and associated expenditures may have been affected by factors other than clinical preventive services, such as the availability of community water fluoridation.
Second, claims data do not capture all dental care utilization or demand of Medicaid‐enrolled children. In some health care settings, dental care is reimbursed based on the number of visits rather than by services provided, as is often the case in federally qualified health centers (FQHCs). For the claims under such settings, we could not distinguish between preventive versus restorative care. However, because only a small proportion of FQHCs provide dental care in the states included in this study (with the exception of Texas) and because their capacity is dedicated primarily to adults, this should not significantly bias our results. We also may not observe overall oral health demand due to potential barriers to care for Medicaid enrollees. In addition, the original MAX data for the study population did not have any inpatient claims with either a CDT code or a caries‐related diagnosis code. Therefore, our analysis did not incorporate caries‐related hospitalizations, possibly underestimating the cost savings of prevention.
Third, some children could have received fluoride varnish in a medical setting or sealants in a community‐based setting such as a school but did not have access to restorative care. In such a situation, the benefits of preventive services may be overestimated.
Finally, there may be limitations on the completeness of Medicaid MAX files, especially for states with large populations served by managed care (Byrd and Dodd 2013). Among the states included in this study, Georgia and Texas were the only states with managed dental care during the study period. Both states have been shown to have usable, quality data for managed care for children during the study period (Byrd and Dodd 2012, 2015).
Findings from this study may not be generalizable to all Medicaid‐enrolled children, those with private dental insurance, or those who pay directly for dental care. There are other factors that affect dental care expenditures such as public insurance reimbursing at lower rates than private insurance, and demographic, socioeconomic, environmental, and familiar characteristics that influence oral health behaviors and status.
Conclusion
Findings from this study suggest that delivery of two evidence‐based preventive dental services for children results in cost savings to state Medicaid programs. Differences in how different state Medicaid programs are administered may affect actual penetration and cost‐savings rates. However, our sensitivity analyses showed that these services remain cost saving over a fairly wide range of penetration levels. Quantifying the potential cost savings of the provision of preventive care for young children can help improve the allocation of resources, resulting in high‐value care (Rouse and Serban 2014). Further, Medicaid‐enrolled children may have limited access to dental care (Cao et al. 2017). Hence, community‐based interventions such as school‐based sealant programs could be a cost‐saving approach for this population (Griffin et al. 2016), although that would depend on the relative effectiveness of sealants applied in school‐based settings compared with dental office settings. Access to care also could be potentially improved by increasing dentist participation by raising Medicaid reimbursement rates (Beazoglou et al. 2015). Some studies, however, have found that the size of the effect is modest (Decker 2011; Buchmueller, Orzol, and Shore‐Sheppard 2015). In addition, changing reimbursement rates would significantly reduce the cost savings of preventive services if reimbursements for preventive services were increased by a higher percentage than fees for restorative services.
The publicly funded health care insurance landscape is changing, and many states have recently moved to a Medicaid block grant rather than a fee‐for‐service model, or they are considering such a change (Sanders et al. 2016). Such changes have the potential to impact the delivery of preventive dental services. Accurately quantifying expenditures of those block grant states is a challenging and important future research direction. Other important directions include the examination of how caries experience and preventive dental exposure in the primary dentition translate into caries experience in the permanent dentition with or without continuity of preventive dental care. Similarly, estimation of the lifetime costs of caries experience would provide better estimates of cost savings of preventive care rather than limiting the analysis to the study time horizon over which data are available.
Supporting information
Appendix SA1: Author Matrix.
Appendix SA2: Data Translation from Claims to Utilization Sequence.
Appendix SA3: Model‐Based Estimation of Caries Prevalence.
Appendix SA4: Clustering Process.
Appendix SA5: Graphical Representation of the Four Utilization Patterns of the Six States.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: We are grateful that Pravara M. Harati and Pratik Khairnar at Georgia Tech computed CRGs and obtained the caries prevalence from regression model. We thank Carol Smith, Director of the Oral Health Program at the Georgia Department of Public Health, for her support with data and policy guidance. The research of Dr. Lee was supported by a Health Analytics Research Gift provided by Andrea Laliberte and Mr. Monahan was supported by Children's Healthcare of Atlanta and the Petit Undergraduate Research Scholars Program of Georgia Tech. Other support includes the Coca Cola Early Professorship Chair (Dr. Serban) and the Virginia C. and Joseph C. Mello Professorship Chair (Dr. Griffin) of Georgia Tech.
Disclosures: None.
Disclaimer: None.
Work of this study was done while Ilbin Lee, Sean Monahan, and Paul M. Griffin were at Georgia Institute of Technology, School of Industrial and Systems Engineering.
References
- Agaku, I. T. , Olutola B. G., Adisa A. O., Obadan E. M., and Vardavas C. I.. 2015. “Association between Unmet Dental Needs and School Absenteeism Because of Illness or Injury among US School Children and Adolescents Aged 6–17 Years, 2011–2012.” Preventive Medicine 72: 83–8. [DOI] [PubMed] [Google Scholar]
- Ahovuo‐Saloranta, A. , Forss H., Walsh T., Hiiri A., Nordblad A., Makela M., and Worthington H. V.. 2013. “Sealants for Preventing Dental Decay in the Permanent Teeth.” Cochrane Database of Systematic Reviews (3): CD001830. [DOI] [PubMed] [Google Scholar]
- Alabama Medicaid Agency . 2016. “Alabama Medicaid Fee Schedule – Dental” [accessed on August 9, 2016]. Available at http://medicaid.alabama.gov/documents/6.0_Providers/6.6_Fee_Schedules/6.6_Dental_Fee_Schedule_8-8-16.xlsx
- American Academy of Pediatric Dentistry . 2013. “Guideline on Caries‐Risk Assessment and Management for Infants, Children, and Adolescents.” Pediatric Dentistry 35 (5): E157–64. [PubMed] [Google Scholar]
- American Dental Association Health Policy Institute . 2015. “The Oral Health Care System: A State by State Analysis.”
- Azarpazhooh, A. , and Main P. A.. 2009. “Efficacy of Dental Prophylaxis (Rubber Cup) for the Prevention of Caries and Gingivitis: A Systematic Review of Literature.” British Dental Journal 207 (7): E14; discussion 328–329. [DOI] [PubMed] [Google Scholar]
- Badersten, A. , Egelberg J., and Koch G.. 1975. “Effect of Monthly Prophylaxis on Caries and Gingivitis in Schoolchildren.” Community Dentistry and Oral Epidemiology 3 (1): 1–4. [DOI] [PubMed] [Google Scholar]
- Beauchamp, J. , Caufield P. W., Crall J. J., Donly K., Feigal R., Gooch B., Ismail A., Kohn W., Siegal M., Simonsen R., and Frantsve‐Hawley J.. 2008. “Evidence‐Based Clinical Recommendations for the Use of Pit‐and‐Fissure Sealants – A Report of the American Dental Association Council on Scientific Affairs.” Journal of the American Dental Association 139 (3): 257–68. [DOI] [PubMed] [Google Scholar]
- Beazoglou, T. , Douglass J., Myne‐Joslin V., Baker P., and Bailit H.. 2015. “Impact of Fee Increases on Dental Utilization Rates for Children Living in Connecticut and Enrolled in Medicaid.” The Journal of the American Dental Association 146 (1): 52–60. [DOI] [PubMed] [Google Scholar]
- Beil, H. , Rozier R. G., Preisser J. S., Stearns S., and Lee J. Y.. 2012. “Effect of Early Preventive Dental Visits on Subsequent Dental Treatment and Expenditures.” Medical Care 50 (9): 749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beil, H. , Rozier R. G., Preisser J. S., Stearns S. C., and Lee J. Y.. 2014. “Effects of Early Dental Office Visits on Dental Caries Experience.” American Journal of Public Health 104 (10): 1979–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertrand, E. , Mallis M., Bui N. M., and Reinharz D.. 2011. “Cost‐Effectiveness Simulation of a Universal Publicly Funded Sealants Application Program.” Journal of Public Health Dentistry 71 (1): 38–45. [DOI] [PubMed] [Google Scholar]
- Biordi, D. L. , Heitzer M., Mundy E., DiMarco M., Thacker S., Taylor E., Huff M., Marino D., and Fitzgerald K.. 2015. “Improving Access and Provision of Preventive Oral Health Care for Very Young, Poor, and Low‐Income Children Through a New Interdisciplinary Partnership.” American Journal of Public Health 105: E23–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmueller, T. C. , Orzol S., and Shore‐Sheppard L. D.. 2015. “The Effect of Medicaid Payment Rates on Access to Dental Care Among Children.” American Journal of Health Economics 1 (2): 194–223. [Google Scholar]
- Bureau of Labor Statistics . 2013. “Consumer Price Index” [accessed on June 21, 2016]. Available at http://www.bls.gov/cpi/
- Byrd, V. L. , and Dodd A. H.. 2012. “Assessing the Usability of Encounter Data for Enrollees in Comprehensive Managed Care across MAX 20072009.” Mathematica Policy Research.
- Byrd, V. L. , and Dodd A. H.. 2013. “Assessing the Usability of MAX 2008 Encounter Data for Comprehensive Managed Care.” Medicare Medicaid Res Rev 3 (1): E1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrd, V. L. , and Dodd A. H.. 2015. “Assessing the Usability of Encounter Data for Enrollees in Comprehensive Managed Care 2010–2011.” Mathematica Policy Research. [DOI] [PMC free article] [PubMed]
- Cao, S. , Gentili M., Griffin P., Griffin S., Harati P., Johnson B., Serban N., and Tomar S.. 2017. “Identifying Shortage Areas for Preventive Dental Care for Children Using High Geographic Granularity Estimates of Need and Supply.” Public Health Reports, in press. [DOI] [PMC free article] [PubMed]
- Centers for Disease Control and Prevention (CDC) . 2016. “National Health and Nutrition Examination Survey Data” [accessed on October 20, 2016]. Available at http://www.cdc.gov/nchs/nhanes.htm
- Centers for Medicare & Medicaid Services . 2011. “Improving Access to and Utilization of Oral Health Services for Children in Medicaid and CHIP Programs: CMS Oral Health Strategy.”
- Centers for Medicare & Medicaid Services . 2013. “CMS Analysis of FFY 2011 CMS‐416 Reports (Annual EPSDT Report), Lines 1b and 12b.”
- Centers for Medicare & Medicaid Services . 2014. Updates on CMCS Informational Bulletin: CMS Oral Health Initiative and Other Dental‐Related Items. Baltimore, MD: U.S. Department of Health and Human Services. [Google Scholar]
- Chi, D. L. , van der Goes D. N., and Ney J. P.. 2014. “Cost‐Effectiveness of Pit‐and‐Fissure Sealants on Primary Molars in Medicaid‐Enrolled Children.” American Journal of Public Health 104 (3): 555–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasanayake, A. P. , Li Y., Kirk K., Bronstein J., and Childers N. K.. 2003. “Restorative Cost Savings Related to Dental Sealants in Alabama Medicaid Children.” Pediatric Dentistry 25 (6): 572–86. [PubMed] [Google Scholar]
- Decker, S. L. 2011. “Medicaid Payment Levels to Dentists and Access to Dental Care among Children and Adolescents.” Journal of the American Medical Association 306 (2): 187–93. [DOI] [PubMed] [Google Scholar]
- Dennison, J. B. , Straffon L. H., and Smith R. C.. 2000. “Effectiveness of Sealant Treatment over Five Years in an Insured Population.” Journal of the American Dental Association 131 (5): 597–605. [DOI] [PubMed] [Google Scholar]
- Do, C. B. , and Batzoglou S.. 2008. “What is the Expectation Maximization Algorithm?” Nature Biotechnology 26 (8): 897–9. [DOI] [PubMed] [Google Scholar]
- Foufoula‐Georgiou, E. , and Lettenmaier D. P.. 1987. “A Markov Renewal Model for Rainfall Occurrences.” Water Resources Research 23 (5): 875–84. [Google Scholar]
- Georgia Department of Public Health . 2013. “Billing Resource Manual.”
- Government Accountability Office . 2010. “Oral Health: Efforts Under Way to Improve Children's Access to Dental Services, but Sustained Attention Needed to Address Ongoing Concerns.” Washington, DC.
- Griffin, S. O. , Jones K., and Crespin M.. 2014. “Calculating Averted Caries Attributable to School‐Based Sealant Programs with a Minimal Data Set.” Journal of Public Health Dentistry 74 (3): 202–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin, S. O. , Barker L. K., Wei L., Li C. H., Albuquerque M. S., Gooch B. F., and Centers for Disease Control and Prevention (CDC) . 2014. “Use of Dental Care and Effective Preventive Services in Preventing Tooth Decay among U.S. Children and Adolescents–Medical Expenditure Panel Survey, United States, 2003–2009 and National Health and Nutrition Examination Survey, United States, 2005–2010.” MMWR Supplements 63 (2): 54–60. [PubMed] [Google Scholar]
- Griffin, S. O. , Naavaal S., Scherrer C., Griffin P. M., Harris K., and Chattopadhyay S.. 2016. “School‐Based Dental Sealant Programs Prevent Cavities and Are Cost‐Effective.” Health Affairs 35 (12): 2233‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrix, K. S. , Downs S. M., Brophy G., Carney Doebbeling C., and Swigonski N. L.. 2013. “Threshold Analysis of Reimbursing Physicians for the Application of Fluoride Varnish in Young Children.” Journal of Public Health Dentistry 73 (4): 297–303. [DOI] [PubMed] [Google Scholar]
- Herndon, J. B. , Tomar S. L., Catalanotto F. A., Vogel W. B., and Shenkman E. A.. 2015. “The Effect of Medicaid Primary Care Provider Reimbursement on Access to Early Childhood Caries Preventive Services.” Health Services Research 50 (1): 136–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson, S. L. , Vann W. F. Jr, Kotch J. B., Pahel B. T., and Lee J. Y.. 2011. “Impact of Poor Oral Health on Children's School Attendance and Performance.” American Journal of Public Health 101 (10): 1900–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, R. H. 2011. “Bayesian Information Criterion for Longitudinal and Clustered Data.” Statistics in Medicine 30 (25): 3050–6. [DOI] [PubMed] [Google Scholar]
- Kleinman, D. V. 2002. “The Guide to Community Preventive Services – Oral Health.” American Journal of Preventive Medicine 23: 1–2. [DOI] [PubMed] [Google Scholar]
- Kranz, A. , Rozier R., Preisser J., Stearns S., Weinberger M., and Lee J.. 2014. “Preventive Services by Medical and Dental Providers and Treatment Outcomes.” Journal of Dental Research 93: 633–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo, D. Z. , Hall M., Agrawal R., Cohen E., Feudtner C., Goodman D. M., Neff J. M., and Berry J. G.. 2015. “Comparison of Health Care Spending and Utilization Among Children with Medicaid Insurance.” Pediatrics 136 (6): E1521–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence, H. P. , Binguis D., Douglas J., McKeown L., Switzer B., Figueiredo R., and Laporte A.. 2008. “A 2‐Year Community‐Randomized Controlled Trial of Fluoride Varnish to Prevent Early Childhood Caries in Aboriginal Children.” Community Dentistry and Oral Epidemiology 36 (6): 503–16. [DOI] [PubMed] [Google Scholar]
- Leskinen, K. , Salo S., Suni J., and Larmas M.. 2008. “Comparison of Dental Health in Sealed and Non‐Sealed First Permanent Molars: 7 Years Follow‐up in Practice‐Based Dentistry.” Journal of Dentistry 36 (1): 27–32. [DOI] [PubMed] [Google Scholar]
- Marinho, V. C. C. , Worthington H. V., Walsh T., and Clarkson J. E.. 2013. “Fluoride Varnishes for Preventing Dental Caries in Children and Adolescents.” Cochrane Database of Systematic Reviews (7): CD002279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Mississippi Division of Medicaid . 2016. “Dental Fees – Professional Services.” [accessed on August 9, 2016]. Available at https://medicaid.ms.gov/wp-content/uploads/2014/03/Dental.xlsx
- Nasseh, K. , and Vujicic M.. 2015. “The Impact of Medicaid Reform on Children's Dental Care Utilization in Connecticut, Maryland, and Texas.” Health Services Research 50 (4): 1236–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NC Division of Medical Assistance . 2016. “NC Medicaid Dental Reimbursement Rates” [accessed on August 9, 2016]. Available at https://ncdma.s3.amazonaws.com/s3fs-public/documents/files/Dentalfee_general_2016_01.xls
- Pahel, B. T. , Rozier R. G., Stearns S. C., and Quinonez R. B.. 2011. “Effectiveness of Preventive Dental Treatments by Physicians for Young Medicaid Enrollees.” Pediatrics 127 (3): E682–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinonez, R. B. , Downs S. M., Shugars D., Christensen J., and Vann W. F. Jr. 2005. “Assessing Cost‐Effectiveness of Sealant Placement in Children.” Journal of Public Health Dentistry 65 (2): 82–9. [DOI] [PubMed] [Google Scholar]
- Quinonez, R. B. , Stearns S. C., Talekar B. S., Rozier R. G., and Downs S. M.. 2006. “Simulating Cost‐Effectiveness of Fluoride Varnish during Well‐Child Visits for Medicaid‐Enrolled Children.” Archives of Pediatrics and Adolescent Medicine 160 (2): 164–70. [DOI] [PubMed] [Google Scholar]
- Rouse, W. B. , and Serban N.. 2014. Understanding and Managing the Complexity of Healthcare. Cambridge, MA: MIT Press. [Google Scholar]
- Rozier, R. G. , Sutton B. K., Bawden J. W., Haupt K., Slade G. D., and King R. S.. 2003. “Prevention of Early Childhood Caries in North Carolina Medical Practices: Implications for Research and Practice.” Journal of Dental Education 67 (8): 876–85. [PubMed] [Google Scholar]
- Rozier, R. G. , Stearns S. C., Pahel B. T., Quinonez R. B., and Park J.. 2010. “How a North Carolina Program Boosted Preventive Oral Health Services for Low‐Income Children.” Health Affairs 29 (12): 2278–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson, C. 2010. “Is Routine Dental Prophylaxis Effective?” Evidence‐Based Dentistry 11 (1): 16–7. [DOI] [PubMed] [Google Scholar]
- Sanders, G. D. , Neumann P. J., Basu A., Brock D. W., Feeny D., Krahn M., Kuntz K. M., Meltzer D. O., Owens D. K., and Prosser L. A.. 2016. “Recommendations for Conduct, Methodological Practices, and Reporting of Cost‐Effectiveness Analyses: Second Panel on Cost‐Effectiveness in Health and Medicine.” Journal of the American Medical Association 316 (10): 1093–103. [DOI] [PubMed] [Google Scholar]
- Savage, M. F. , Lee J. Y., Kotch J. B., and Vann W. F.. 2004. “Early Preventive Dental Visits: Effects on Subsequent Utilization and Costs.” Pediatrics 114 (4): E418–23. [DOI] [PubMed] [Google Scholar]
- SC Department of Health and Human Services . 2011. “Dental Medicaid Fee Schedule – CDT” [accessed on August 9, 2016]. Available at https://www.scdhhs.gov/internet/pdf/FeeScheduals/CDT_CPT%20proc%20codes.xls
- Schwarz, G. 1978. “Estimating the Dimension of a Model.” The Annals of Statistics 6 (2): 461–4. [Google Scholar]
- Seirawan, H. , Faust S., and Mulligan R.. 2012. “The Impact of Oral Health on the Academic Performance of Disadvantaged Children.” American Journal of Public Health 102 (9): 1729–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen, B. , Blackburn J., Morrisey M. A., Kilgore M. L., Becker D. J., Caldwell C., and Menachemi N.. 2013. “Effectiveness of Preventive Dental Visits in Reducing Nonpreventive Dental Visits and Expenditures.” Pediatrics 131 (6): 1107–13. [DOI] [PubMed] [Google Scholar]
- Slade, G. D. , Bailie R. S., Roberts‐Thomson K., Leach A. J., Raye I., Endean C., Simmons B., and Morris P.. 2011. “Effect of Health Promotion and Fluoride Varnish on Dental Caries among Australian Aboriginal Children: Results from a Community‐Randomized Controlled Trial.” Community Dentistry and Oral Epidemiology 39 (1): 29–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stearns, S. C. , Rozier R. G., Kranz A. M., Pahel B. T., and Quinonez R. B.. 2012. “Cost‐Effectiveness of Preventive Oral Health Care in Medical Offices for Young Medicaid Enrollees.” Archives of Pediatrics and Adolescent Medicine 166 (10): 945–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Texas Medicaid & Healthcare Partnership . 2016. “Texas Medicaid Static Fee Schedules – Dental” [accessed on August 9, 2016]. Available at http://public.tmhp.com/FeeSchedules/StaticFeeSchedule/FeeSchedules.aspx?fn=%5c%5cAUSCIFSFeeSchedule01.tmhp.net%5cFeeSchedule%5cPROD%5cStatic%5cTexas_Medicaid_Fee_Schedule_PRCR496C.xls
- Weintraub, J. A. , Stearns S. C., Rozier R. G., and Huang C. C.. 2001. “Treatment Outcomes and Costs of Dental Sealants among Children Enrolled in Medicaid.” American Journal of Public Health 91 (11): 1877–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weintraub, J. A. , Ramos‐Gomez F., Jue B., Shain S., Hoover C. I., Featherstone J. D. B., and Gansky S. A.. 2006. “Fluoride Varnish Efficacy in Preventing Early Childhood Caries.” Journal of Dental Research 85 (2): 172–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner, C. W. , Pereira A. C., and Eklund S. A.. 2000. “Cost‐Effectiveness Study of a School‐Based Sealant Program.” ASDC Journal of Dentistry for Children 67 (2): 93–7, 82. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Data Translation from Claims to Utilization Sequence.
Appendix SA3: Model‐Based Estimation of Caries Prevalence.
Appendix SA4: Clustering Process.
Appendix SA5: Graphical Representation of the Four Utilization Patterns of the Six States.


