INTRODUCTION
There is uncertainty about the magnitude of infectious endocarditis (IE), with a wide range in reported incidence (3.5 to 10 cases per 100,000 persons-year), and mortality (29 to 40%).1–5 Discrepancies may be due to clinical and methodological differences between studies. The aging of the population, more aggressive interventions, and the increase of poverty are potentials and are possible epidemiological factors affecting IE over the last decades, particularly in Europe. The Spanish public health system is free and covers nearly all population (46.5 million inhabitants in 2017). Our aim was to assess evolution of incidence, mortality, length of hospital stay, and costs related to IE between 1997 and 2014.
METHODS
We used the Basic Minimum Data Set (BMDS) of the National Surveillance System for Hospital Data in Spain (Spanish Ministry of Health) to obtain retrospective data in all admissions for IE with hospital discharge from January 1, 1997 to December 31, 2014. Diagnoses and comorbidities were available in ICD-9 CM codes. IE was considered (421, acute and subacute endocarditis) regardless of whether it was a primary or secondary diagnosis. An anonymized dataset with demographic data (sex, age), comorbidities, associated organ dysfunction(s), Charlson’s index, and mortality information was generated.
RESULTS
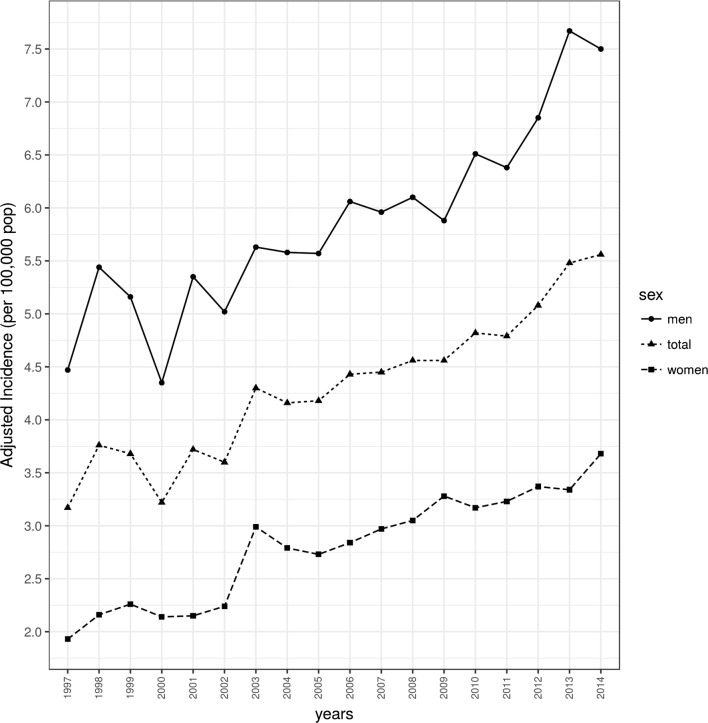
Overall, 34,399 patients were diagnosed with IE. The adjusted IE incidence (events per 100,000 persons) was 4.3%, ranging from 3.2% in 1997 to 5.6% in 2014 (Fig. 1). Age-adjusted incidence was higher in the 75–79 age group. Higher rates were observed in males than in females (67 v. 33%).
Figure 1.
Population-adjusted incidence of infective endocarditis by gender in Spain between 1997 and 2014.
The Charlson Index increased from (mean ± SD) 0.7 ± 1.1 in 1997 to 1.3 ± 1.4 in 2014. The percentage of IE patients with one, two, or three or more with organ dysfunction increased dramatically between 1997 and 2014, rising from 10.5, 1.8, and 0.2%, respectively, to 25.5, 6.1, and 1.3% (Table 1).
Table 1.
Clinical and Epidemiological Characteristics of the Patients Diagnosed with Endocarditis Between 1997 and 2014
| All periods | 1997–1999 | 2000–2004 | 2005–2009 | 2010–2014 | |
|---|---|---|---|---|---|
| No. of patients | 34,399 (100%) | 4239 (12.32%) | 7975 (23.18%) | 10,074 (29.28%) | 12,111 (35.20%) |
| Gender | |||||
| Male | 23,045 (66.99%) | 2943 (69.42%) | 5345 (67.02%) | 6656 (66.07%) | 8101 (66.88%) |
| Female | 11,353 (33.00%) | 1296 (30.57%) | 2629 (32.96) | 3418 (33.92%) | 4010 (33.11%) |
| Unknown | 1 (0.00%) | 0 (0.00%) | 1 (0.01%) | 0 (0.00%) | 0 (0.00%) |
| Age (years) | 61.83 ± 18.44 | 53.10 ± 19.96 | 59.24 ± 18.43 | 62.37 ± 17.91 | 66.13 ± 16.90 |
| Comorbid condition | |||||
| Ischemic heart disease | 1625 (4.72%) | 117 (2.70%) | 390 (4.89%) | 549 (5.44%) | 569 (4.69%) |
| Heart failure | 8571 (24.92%) | 693 (16.34%) | 1737 (21.78%) | 2520 (25.01%) | 3621 (29.89%) |
| Peripheral vascular disease | 1694 (4.92%) | 91 (2.15%) | 343 (4.31%) | 513 (5.09%) | 747 (6.17%) |
| Stroke | 1412 (4.10%) | 145 (3.42%) | 348 (4.36%) | 366 (3.63%) | 553 (4.56%) |
| Chronic lung disease | 4798 (13.95%) | 318 (7.50%) | 906 (11.36%) | 1496 (14.85%) | 2078 (17.16%) |
| Rheumatic disease | 554 (1.61%) | 35 (0.82%) | 105 (1.32%) | 195 (1.93%) | 219 (1.80%) |
| Mild liver disease | 1522 (4.42%) | 131 (0.32%) | 301 (3.77%) | 488 (4.84%) | 602 (4.97%) |
| Moderate-to-severe liver disease | 844 (2.45%) | 71 (1.67%) | 166 (2.08%) | 256 (2.54%) | 351 (2.89%) |
| Mild-to-moderate mellitus diabetes | 4685 (13.62%) | 302 (7.12%) | 924 (11.58%) | 1493 (14.82%) | 1966 (16.23%) |
| DM with chronic complications | 1227 (3.56%) | 59 (1.39%) | 212 (2.66%) | 378 (3.75%) | 578 (4.77%) |
| Chronic renal disease | 1901 (5.53%) | 286 (6.75%) | 642 (8.05%) | 702 (6.97%) | 271 (2.24%) |
| Hemiplegia | 608 (1.76%) | 55 (1.29%) | 124 (1.55%) | 138 (1.37%) | 291 (2.41%) |
| Dementia | 463 (1.34%) | 33 (0.78%) | 110 (1.38%) | 124 (1.23%) | 196 (1.62%) |
| Charlson Index | 1.12 ± 1.37 | 0.71 ± 1.09 | 1.04 ± 1.34 | 1.18 ± 1.39 | 1.27 ± 1.42 |
| Acute organ dysfunction | |||||
| Cardiovascular | 577 (1.67%) | 54 (1.27%) | 114 (1.43%) | 169 (1.67%) | 240 (1.98%) |
| Hematologic | 1512 (4.39%) | 125 (2.95%) | 306 (3.84%) | 452 (4.48%) | 629 (5.19%) |
| Hepatic | 637 (1.85%) | 40 (1.06%) | 105 (1.32%) | 188 (1.86%) | 304 (2.51%) |
| Neurologic | 453 (1.31%) | 43 (1.01%) | 113 (1.41%) | 123 (1.22%) | 174 (1.44%) |
| Renal | 6123 (17.80%) | 378 (8.92%) | 1081 (13.55%) | 1851 (18.37%) | 2813 (23.22%) |
| Respiratory | 584 (1.69%) | 47 (1.11%) | 122 (1.53%) | 213 (2.11%) | 202 (1.67%) |
| Metabolic | 487 (1.41%) | 18 (0.42%) | 63 (0.79%) | 134 (1.33%) | 272 (2.24%) |
| Heart valve surgery | 5414 (15.74%) | 515 (12.14%) | 1190 (14.92%) | 1658 (16.46%) | 2051 (16.93%) |
| Sepsis | 4350 (12.64%) | 326 (7.69%) | 910 (11.41%) | 1391 (13.80%) | 1723 (14.23%) |
| Microorganism isolated | |||||
| Gram + | 2651 (7.71%) | 206 (4.86%) | 627 (7.86%) | 881 (8.74%) | 937 (7.73%) |
| Gram − | 1766 (5.13%) | 123 (2.90%) | 297 (3.72%) | 528 (5.24%) | 818 (6.75%) |
| Anaerobes | 27 (0.08%) | 2 (0.05%) | 5 (0.06%) | 7 (0.07%) | 13 (0.11%) |
| Fungi | 195 (0.56%) | 19 (0.45%) | 47 (0.59%) | 54 (0.54%) | 75 (0.62%) |
| Emergency admission | 28,306 (82.29%) | 3549 (83.72%) | 6571 (82.39%) | 8274 (82.13%) | 9912 (81.84%) |
| Re-admission | 6355 (18.47%) | 671 (15.83%) | 1342 (16.83%) | 1854 (18.40%) | 2488 (20.54%) |
Values were expressed as absolute numbers (percentage) and means (standard deviation)
DM diabetes mellitus
Adjusted IE mortality (deaths per 100,000 persons) was 0.9%, ranging from 0.5% in 1997 to 1.2% in 2014. Age-adjusted mortality was higher in older male patients, peaking at 4.8% in the 80–84 age group. Higher figures were observed in males than in females.
Between 1997 and 2014, the length of hospital stay was (mean ± SD) 28.1 ± 24.6 days. Hospital stay peaked (31.2 days) in 2008 and progressively declined to 26.2 days by 2014. The expenditure in the care of IE per patient increased from 6759.3 in 1997 to 15,489.6 euros in 2008, remaining stable from that year (15,097.5 euros in 2014).
DISCUSSION
The 1997 to 2014 series data from Spain shows a marked increase of incidence and more than doubled mortality due to IE. The incidence rate observed coincides with that reported in a Danish study (3.93 and 7.55 cases per 100,000 persons-year in 1994 and 2011, respectively).4
Despite medical and technological advances, IE incidence and mortality increased between 1997 and 2014 due to the older age, increased comorbidities, higher Charlson’s index, and frequent multiple organ dysfunction. These results are in concordance with other reported by different authors.5
Length of hospital stay and cost per patient increased from 1997 to 2008, slightly decreasing from that year until 2014. These results are consistent with those reported in France between 2007 and 2009, where the mean length of hospital stay was 30 days, with a mean cost per patient of 15,281 euros.2
In Spain, there was not an increase of health spending consumption in terms of gross domestic product (GDP) during the covered period, and even it drop from 6.7 to 6.0% of GDP during the economic crisis (2009 to 2014).6
This study suggests that epidemiological characteristics of IE have changed in Spain over the last two decades. Results of our study should encourage health authorities to reconsider preventive strategies implemented so far, with a special focus on elder patients with previous diseases, who are hospitalized and/or subjected to invasive diagnostic or therapeutic procedures.
Acknowledgements
We would like to thank the “Subdirección General del Instituto de Información Sanitaria (Ministerio de Sanidad, Servicios Sociales e Igualdad)” for providing the information on which this study was based.
Funding Information
This study was funded by the Carlos III Health Institute (PI15/01451) and the Regional Department of Health of the Autonomous Community of Castilla y León (“Gerencia de Salud, Consejería de Sanidad, Junta de Castilla y Leon”) [grant number GRS: GRS 1270/A/16 and GRS 1255/A/16 to ET].
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
REFERENCES
- 1.Muñoz P, Kestler M, De Alarcon A, Miro JM, Bermejo J, Rodríguez-Abella H, et al. Current epidemiology and outcome of infective endocarditis: a multicenter, prospective, cohort study. Medicine (Baltimore). 2015;94:e1816. doi: 10.1097/MD.0000000000001816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sunder S, Grammatico-Guillon L, Baron S, Gaborit C, Bernard-Brunet A, Garot D, et al. Clinical and economic outcomes of infective endocarditis. Infect Dis (Lond). 2015;47:80–7. doi: 10.3109/00365548.2014.968608. [DOI] [PubMed] [Google Scholar]
- 3.Federspiel JJ, Stearns SC, Peppercorn AF, Chu VH, Fowler VG. Increasing US rates of endocarditis with Staphylococcus aureus: 1999-2008. Arch Intern Med. 2012;172:363–5. doi: 10.1001/archinternmed.2011.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erichsen P, Gislason GH, Bruun NE. The increasing incidence of infective endocarditis in Denmark, 1994-2011. Eur J Intern Med. 2016;35:95–9. doi: 10.1016/j.ejim.2016.05.021. [DOI] [PubMed] [Google Scholar]
- 5.Fedeli U, Schievano E, Buonfrate D, Pellizzer G, Spolaore P. Increasing incidence and mortality of infective endocarditis: a population-based study through a record-linkage system. BMC Infect Dis. 2011;11:48. doi: 10.1186/1471-2334-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Estadística de Gasto Sanitario Público (EGSP). Ministerio de Sanidad, Servicios Sociales e Igualdad. Gobierno de España. https://www.msssi.gob.es/estadEstudios/estadisticas/inforRecopilaciones/gastoSanitario2005/home.htm (accessed 14.02.18.)