Abstract
Combined lesions of the glenoid labrum are a relatively common finding in shoulder instability patients. Even so, relatively few studies have been published evaluating outcomes after repair of these complex labral detachments. To achieve a successful outcome, accurate identification of all pathologic lesions in the shoulder combined with an organized, stepwise approach to sometimes circumferential labral fixation is required. Repair of 360° labral tears can be effectively and efficiently achieved by implementing the reproducible steps and sequence described to reconstruct these circumferential labral tears.
Shoulder instability patients can have a wide variety of symptoms ranging from isolated pain complaints to recurrent dislocations. Likewise, some patients present with unidirectional instability, while others are found to have a multidirectional instability pattern. Traumatically induced lesions, most often seen in patients with unidirectional anterior instability, usually occur at the anterior glenoid rim and were initially described by Bankart.1 Lesions of the superior labrum, as described by Andrews et al.2 and later called SLAP tears as well as posterior and inferior labral tears, can all be present in the same symptomatic shoulder. In fact, these complex combined lesions, which include detachments of the anterior, inferior, posterior, and superior labrum, have been termed “360° tears” because they involve the full circumferential attachment of the glenoid labrum.
Multidirectional instability can be thought of as a spectrum of pathology consisting of both traumatic and atraumatic components.3 Atraumatic multidirectional instability is most often successfully managed nonoperatively using organized rehabilitation techniques. For those patients with atraumatic etiologies that fail conservative management, surgical stabilization of the glenohumeral joint has been described by many investigators with successful results.4, 5, 6 In contrast to this type of multidirectional instability patient, there exists a subset of patients with instability in multiple directions for which their symptoms are initiated or exacerbated by specific, traumatic events that often result in distinct labral disruptions. The pathologic lesions seen in such patients have been described by Lo and Burkhart7 as “triple labral lesions” in their report of 7 patients with combined anterior, posterior, and superior labral lesions following a specific, traumatic inciting event. Combined lesions of the glenoid labrum have been further investigated by Tokish et al.8 and Ricchetti et al.,9 who described circumferential (360°) lesions of the glenoid labrum. The study by Tokish et al. reported on 41 shoulders, and the Ricchetti et al. study evaluated the outcomes of 48 shoulders. All patients in both of these studies underwent arthroscopic repair of their circumferential labral tears using a mean of 7.1 and 7.9 points of suture anchor fixation, respectively.
The described technique is the preferred surgical approach by the senior author (M.R.W.) and is commonly used in such patients when these complex 360° labral lesions are encountered. In addition, the authors often carry out a supplemental, concomitant capsular plication when significant, residual capsular patulousness is identified after the 360° labral repair has been completed. The sequence for reattachment of these complex labral tears is important and is described.
Surgical Technique
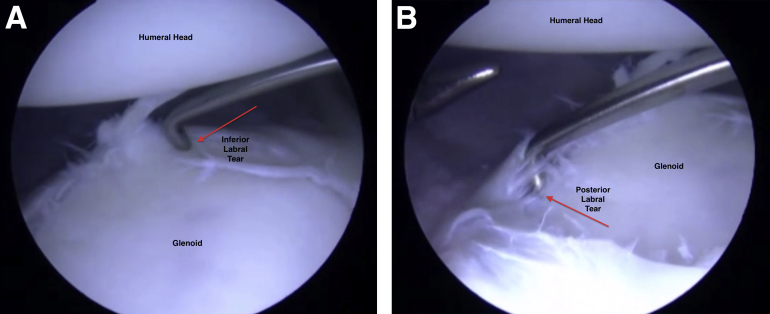
Following induction of anesthesia and after careful examination under anesthesia comparing both shoulders, the patient is positioned in the lateral decubitus position. The operative arm is then prepared and draped in a sterile fashion. Ten pounds of balanced suspension is applied to the shoulder, and a diagnostic shoulder arthroscopy using a 30° arthroscope is performed using standard posterior and anterior-inferior viewing portals. Once the diagnosis of a 360° labral disruption is confirmed, an anterior-superior portal is also established. A more thorough assessment of the degree and extent of the labral disruptions is then carried out by visualizing the labrum circumferentially using all of these portals as well as by probing the labrum circumferentially (Fig 1 A and B).
Fig 1.
(A) The glenohumeral joint of a left shoulder with patient in the lateral decubitus position is viewed from the anterior-superior portal with a probe revealing an anterior labral tear, a posterior labral tear, and an inferior labral tear after labral debridement and mobilization have been performed. As described in the technique, an opposite joint–sided approach is helpful to mobilize the labrum prior to fixation being placed. This is performed circumferentially in the case of a 360° labral tear. (B) Again, in this left shoulder in the lateral decubitus position, the posterior labrum is probed, revealing the extent of the labral pathology in this case. The labrum has been mobilized circumferentially.
Prior to placing anchors around the circumferential perimeter of the glenoid as indicated, standard technical steps are important to understand and follow (Video 1). Extensive mobilization of the labrum circumferentially, often using an opposite joint–sided approach, is carried out. This opposite joint–sided approach technique to mobilize the labrum is accomplished by inserting a labral elevator into the portal cannula that is opposite the side of the glenoid labrum to be elevated and mobilized. For example, to detach the anterior labrum, the arthroscopic labral elevator is passed into the glenohumeral joint through the posterior portal cannula. This approach often provides the most effective angle for mobilization of the labral detachment.
A concurrent, significant capsular insufficiency may also be present in combination with a 360° labral lesions in some of these patients. In such circumstances, supplemental capsular plication can also be accomplished at the time of labral repair by incorporating this additional patulous capsule within the labral reattachment suture loops.
Once adequate mobilization of this circumferential labral detachment is completed, it is imperative to develop and execute a stepwise plan for reattaching the labrum. Each 360° disruption is unique regarding the specific degree and location of the various components of the pathologic lesions, making broad generalizations related to the most appropriate sequence for reattachment of this complex labral detachment unwise.
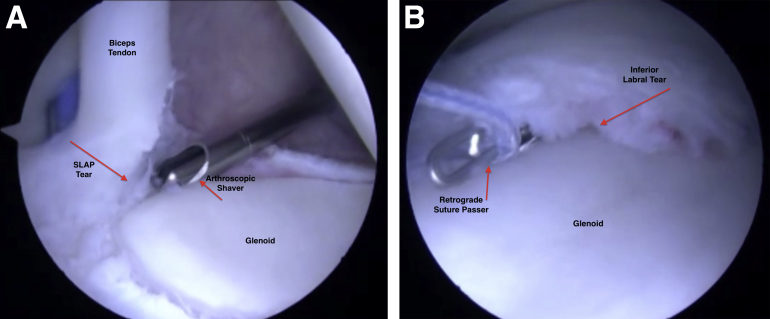
Deciding on the most appropriate sequence for repair of a 360° labral detachment in an individual patient begins before the surgical procedure is initiated. Carefully examination of the patient preoperatively in the clinic setting to identify the primary direction and degree of instability should be carried out. Once the instability pattern is confirmed and correlated with preoperative objective testing such as radiographs and magnetic resonance imaging, examination under anesthesia at the time of surgery, along with a thorough diagnostic arthroscopic assessment, should be done (Fig 2A).
Fig 2.
(A) Thorough evaluation of the biceps anchor should also be performed prior to fixation. In this left shoulder in the lateral decubitus position, a shaver is used to debride the biceps anchor, which reveals its attachment is intact. This completes the diagnostic portion of the procedure, and attention can then be turned to fixation. (B) A left shoulder with patient in the lateral decubitus position is shown as a labral anchor is placed at the 6 o’clock position. The anchor is placed using a posterior portal, while viewing is performed from anterior-superior. This image shows sutures that are passed through the labrum using a retrograde suture passer that is introduced into the glenohumeral joint through a posterior portal, and sutures are retrieved in retrograde fashion.
The inferior component of the instability pattern and labral pathology is most often addressed as an initial step with placement of an anchor or anchors (Arthrex 2.5 mm double loaded labral anchor; Naples, FL) at the 6 o’clock position on the glenoid face (Fig 2B). Sutures are typically retrieved through the most inferior labrum using a 60° retrograde suture retriever (IDEAL suture grasper, Depuy Mitek, Raynham, MA) that is advanced into the glenohumeral joint through either the posterior portal or the anterior-inferior portal (or both portals) depending on the specifics of the inferior labral pathology. Almost always, additional inferior capsule is also incorporated into these suture passes most inferiorly in an effort to diminish any pathologic inferior capsular laxity that is present (Video 1). However, once the 6 o’clock anchor(s) has been placed and sutures passed through both the inferior labrum and capsule, suture tying of these inferiorly placed suture anchor sutures is usually delayed until later in the procedure. This delay is felt by the authors to be important in some situations to avoid unintentionally constraining the degree of superior labro-ligamentous translation that might otherwise be possible compared with these 6 o’clock sutures being tied immediately.
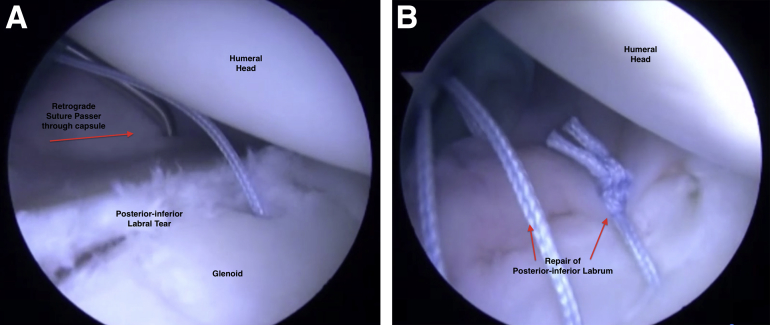
Following passage of these 6 o’clock anchor sutures, and for a patient who is identified clinically as possessing a primarily posterior inferior instability pattern, viewing is then accomplished from the anterior superior portal while posterior labral anchors are sequentially placed and sutures are tied from inferior to superior on the glenoid face. The number and location of these glenoid anchors depend on the pathology identified at the time of surgical intervention. Again, a pinch-and-tuck technique incorporating posterior capsular tissue (Fig 3A) is also carried out prior to knot tying as necessitated by the degree of posterior inferior capsular patulousness (Fig 3B).
Fig 3.
(A) Suture passage and anchor placement are performed, beginning inferior and working superiorly along the glenoid. In this left shoulder in the lateral decubitus position, a retrograde suture passer is placed in the posterior portal and passed through the patulous posterior capsule in addition to the labrum to address both the labral tear and capsular patulousness. (B) Knot tying is performed to address the posterior-inferior labral tear and capsular patulousness.
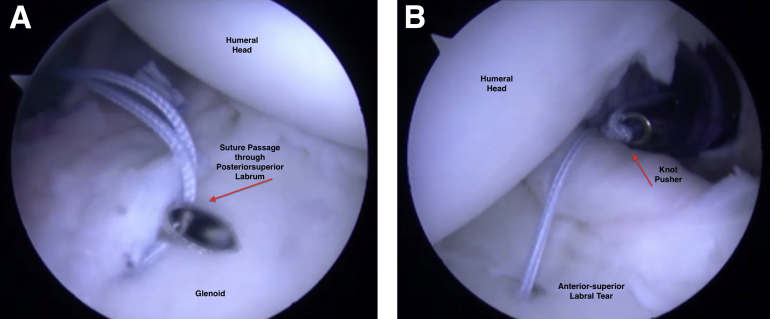
After passage of the inferior sutures and tying of the posterior-inferior sutures (Fig 4A), attention is then turned to the anterior labrum. Typically, the arthroscope is placed in the posterior viewing portal. Multiple suture anchors are generally used anteriorly with suture passage and knot tying proceeding sequentially from inferior to superior on the anterior glenoid face. Simultaneous capsular plication is also performed anteriorly as necessary to adequately reduce anterior and inferior capsular volume (Fig 4B). Surgical management of the superior labral disruption is usually carried out last in the repair sequence due, in part, to the relative ease of accessibility of the superior glenoid labrum. Following completion of all suture tying, the glenohumeral joint volume is significantly reduced, and the humeral head usually remains centered on the glenoid face (Fig 5).
Fig 4.
(A) Anchor placement and knot tying are advanced from inferior to superior along the posterior glenoid face first. This image of a left shoulder in the lateral decubitus position again shows suture passage in retrograde fashion through the posterior-superior labrum. (B) The glenohumeral joint of a left shoulder in the lateral decubitus position is now viewed from the posterior portal, and knot tying is performed to address the anterior labral tear. Incorporation of anterior and inferior capsule can be seen as well.
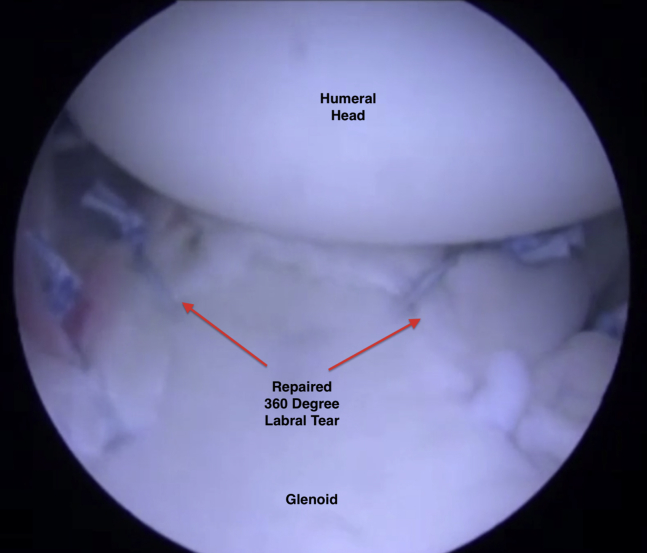
Fig 5.
As viewed from the anterior-superior portal, the 360° labral repair can be seen along with a centered humeral head and decreased intra-articular capsular volume.
Postoperatively, patients are immobilized in a shoulder sling for approximately 4 to 6 weeks. Patients are allowed and encouraged to perform pendulum exercises, shoulder shrugs, and elbow and hand range-of-motion activities from the first postoperative day. Organized physical therapy is usually initiated at 3 weeks postoperatively and includes passive and active assisted range of motion exercises limiting external and internal rotation as dictated by the direction and degree of the individual patient’s instability pattern as well as by the stability and security that the surgical procedure achieved. Six weeks after surgical intervention, progressive active range of motion and strengthening begin and are usually continued until approximately 4 months following surgery.
Discussion
A stepwise approach to the repair of these complex 360° labral detachments is very important and helps to maximize the stability of the reconstruction. This described approach and sequence to repairing these 360° lesions and concurrent capsular insufficiency provides a reproducible, safe, and efficient way to address these complex labral disruptions.
This 360° labral reconstruction surgical technique is dependent on the effective execution of several important sequential steps (Table 1). First, thorough and circumferential labral mobilization must be carried out prior to reapproximation of any of the labral detachments. Mobilizing the labrum using an opposite joint–sided approach can be helpful in this task. For example, when mobilizing the anterior labrum, it is sometimes helpful to insert the metal elevator through the posterior cannula portal because the angle for mobilization may be improved for anterior labral mobilization. This opposite joint–sided access may be valuable when mobilizing the inferior labral tear as well. Next, attention should be paid to recognizing and addressing excessive capsular volume when pathologic capsular patulousness is present. Suture passage can easily be accomplished through this patulous capsular tissue at the time of labral repair. Finally, determining a specific sequence for securing the various components of the labral disruption in an individual patient, based on the pathology identified arthroscopically along with the surgeon’s assessment of the primary instability direction and degree, is critical in these complex cases. In addition, the authors emphasize the importance of delaying inferior knot tying, when appropriate, to avoid inadvertently constraining subsequent posterior and anterior labral and ligamentous translations as labral fixation ultimately progresses from inferior to superior. In fact, knot tying for the 6 o’clock labral and capsule sutures is routinely delayed by the authors until the posterior inferior glenohumeral ligament and the anterior inferior glenohumeral ligament tension has been restored more superiorly. Lastly, the superior labral disruption is generally managed as necessary after all other repairs have been completed since it is most easily accessed with the arthroscopic instruments.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Mobilizing the labrum using an opposite of joint technique prior to fixation. | Difficulty visualizing and placing inferior glenoid anchors. |
| Follow sequential process of fixation beginning with inferior labrum and working superior. | |
| Abduction with neutral rotation moves the axillary nerve maximally away from the glenoid rim. |
This 360° labral repair technique has few potential, inherent risks (Table 2). As with any inferior glenohumeral arthroscopic or open procedure, care must be taken to avoid iatrogenic injury to the axillary nerve. Caution should be used when placing instrumentation inferiorly as the axillary nerve is in close proximity to the glenoid rim especially during suture passage through the inferior labrum and capsule. Abduction with neutral rotation allows the axillary nerve to translate maximally away from the glenoid rim.10, 11 Another potential risk is related to suture anchor placement. Because of the extent of these circumferential labral lesions, very inferior suture anchors are often deployed. The angle for safe, intracortical insertion of these 6 o’clock anchors may be difficult to achieve so care should be taken during this important step. Lim et al.12 showed that the most inferior anchors (5:30 and 6 o’clock positions in a right shoulder) carried a higher risk of perforating the inferior cortex of the glenoid when inserted from an anterior-inferior portal in the lateral decubitus position.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Capsular volume closure performed concomitantly when patulous capsule present. | Risk of iatrogenic injury to axillary nerve. |
| Working from inferior to superior allows room to work as fixation is moved up the glenoid face. | Suture anchor failure or malposition. |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: L.D.F. receives support from AANA, Smith & Nephew, Arthrex, and Mitek. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
A standard arthroscopic view with a 30o arthroscope from the anterior-superior portal in the lateral position is seen, revealing an inferior, anterior, posterior, and superior combined labral tear. A type IV SLAP lesion is identified superiorly and debrided. Viewing from the same anterior-superior portal, attention is turned to the inferior labrum with sutures passed at the 6 o’clock position to repair the inferior labral lesion. Labral repair is then performed in a stepwise fashion beginning with the posterior-inferior labrum and anterior-inferior labrum. Concomitant capsular-plication is performed. Labral repair is then performed posterior-superiorly and anterior-superiorly, resulting in a significant reduction in capsular volume and reapproximation of the extensive labral tear.
References
- 1.Bankart A.S.B. The pathology and treatment of recurrent dislocation of the shoulder joint. Br J Surg. 1938;26:23–29. [Google Scholar]
- 2.Andrews J.R., Carson W., Jr., McLeod W. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13:337–341. doi: 10.1177/036354658501300508. [DOI] [PubMed] [Google Scholar]
- 3.Alpert J.M., Verma N., Wysocki R., Yanke A.B., Romeo A.A. Arthroscopic treatment of multidirectional shoulder instability with minimum 270o labral repair: Minimum 2-year follow-up. Arthroscopy. 2008;24:704–711. doi: 10.1016/j.arthro.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Duncan R., Savoie F.H., 3rd Arthroscopic inferior capsular shift for multidirectional instability of the shoulder: A preliminary report. Arthroscopy. 1993;9:24–27. doi: 10.1016/s0749-8063(05)80340-8. [DOI] [PubMed] [Google Scholar]
- 5.Treacy S.H., Savoie F.H., 3rd, Field L.D. Arthroscopic treatment of multidirectional instability. J Shoulder Elbow Surg. 1999;8:345–350. doi: 10.1016/s1058-2746(99)90158-1. [DOI] [PubMed] [Google Scholar]
- 6.McIntyre L.F., Caspari R.B., Savoie F.H., 3rd The arthroscopic treatment of multidirectional shoulder instability: Two-year results of a multiple suture technique. Arthroscopy. 1997;13:418–425. doi: 10.1016/s0749-8063(97)90118-3. [DOI] [PubMed] [Google Scholar]
- 7.Lo I.K., Burkhart S.S. Triple labral lesions: Pathology and surgical repair technique-report of seven cases. Arthroscopy. 2005;21:186–193. doi: 10.1016/j.arthro.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 8.Tokish J.M., McBrantney C.M., Solomon D.J., LeClere L., Dewing C.B., Provencher M.T. Arthroscopic repair of circumferential lesions of the glenoid labrum. J Bone Joint Surg Am. 2009;91:2795–2802. doi: 10.2106/JBJS.H.01241. [DOI] [PubMed] [Google Scholar]
- 9.Ricchetti E.T., Ciccotti M.C., O’Brien D.F. Outcomes of arthroscopic repair of the panlabral tears of the glenohumeral joint. Am J Sports Med. 2012;40:2561–2568. doi: 10.1177/0363546512460834. [DOI] [PubMed] [Google Scholar]
- 10.Powell S.E., Nord K.D., Ryu R.K.N. The diagnosis, classification, and treatment of SLAP lesions. Oper Tech Sports Med. 2004;12:99–110. [Google Scholar]
- 11.Yoo J.C., Kim J.H., Ahn J.H., Lee S.H. Arthroscopic perspective of the axillary nerve in relation to the glenoid and arm position: A cadaveric study. Arthroscopy. 2007;23:1271–1277. doi: 10.1016/j.arthro.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 12.Lim T.K., Koh K.H., Lee S.H. Inferior anchor cortical perforation with arthroscopic Bankart repair: A cadaveric study. Arthroscopy. 2013;29:31–36. doi: 10.1016/j.arthro.2012.08.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A standard arthroscopic view with a 30o arthroscope from the anterior-superior portal in the lateral position is seen, revealing an inferior, anterior, posterior, and superior combined labral tear. A type IV SLAP lesion is identified superiorly and debrided. Viewing from the same anterior-superior portal, attention is turned to the inferior labrum with sutures passed at the 6 o’clock position to repair the inferior labral lesion. Labral repair is then performed in a stepwise fashion beginning with the posterior-inferior labrum and anterior-inferior labrum. Concomitant capsular-plication is performed. Labral repair is then performed posterior-superiorly and anterior-superiorly, resulting in a significant reduction in capsular volume and reapproximation of the extensive labral tear.