Abstract
On 30 October 2017, an outbreak of measles started in the Nouvelle-Aquitaine (NA) region in France among Bordeaux University students before spreading to other regions. Until 1 July 2018, 1,101 cases were reported in NA, including 98 complications and two deaths. Cases were related to clusters (e.g. students, healthcare workers) in 16%; 81% of cases were not vaccinated against measles as recommended. Vaccination coverage above herd immunity threshold remains the main preventative outbreak measure.
Keywords: measles, measles-mumps-rubella (MMR) vaccine, outbreaks, Air-borne infections, Students, Healthcare facilities
On 30 October 2017, a measles outbreak started among students attending Bordeaux University in the southwest of France. It rapidly spread into the general population of Bordeaux’s Gironde district, into Nouvelle-Aquitaine region (NA) and then onto other regions. We conducted an investigation to describe the outbreak, identify clusters and stop further transmission.
Case definitions
In France, measles became a notifiable disease in 2005 to improve the detection of active transmission and increase the specificity of the diagnosis through laboratory confirmation of clinical cases. Clinicians and microbiologists are requested to report suspected and confirmed measles cases immediately to the Regional Health Agencies (ARS) responsible for implementing control measures.
We included all cases reported in the mandatory notification system (possible, probable and confirmed) who lived in NA and developed rash onset between 30 October 2017 and 1 July 2018 (Box). We interviewed cases to identify contacts at risk and detect clusters in high risk groups.
Box. Definition of cases and other categories followed-up during the measles outbreak, Nouvelle-Aquitaine region, France, 30 October 2017–1 July 2018.
Measles cases
Possible case
Person presenting with fever ≥ 38.5 °C, maculopapular rash and at least one of the following symptoms: conjunctivitis, coryza, cough or Koplik’s spots
Probable case
Person meeting the clinical criteria and with an epidemiological link to a laboratory-confirmed case
Confirmed case
Person meeting the clinical criteria and with laboratory-confirmed measles infection detected by serology or RT-PCR in serum or oral fluid and not recently vaccinated
Other categories
Cluster
At least three cases including one confirmed case in high-risk groups
High-risk groups
Groups with high number of susceptibles and/or people at risk to develop complications
Outbreak description
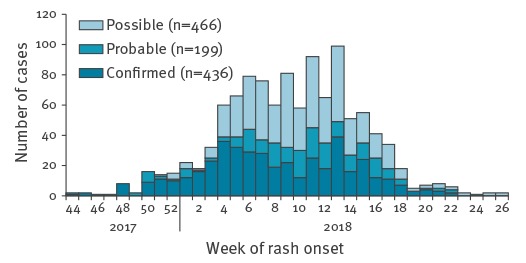
In total, 1,101 cases (466 possible, 199 probable, 436 confirmed) were reported in NA which represented 41% of the cases reported in France. Following the start of the measles outbreak on 30 October 2017, cases increased from week 50 2017 and peaked during week 13 2018 (Figure 1). Five hundred and eighty-one cases (53%) were male, and 646 (59%) cases were older than 15 years. The highest cumulative incidence rate was observed in children < 1 year of age (160.8/100,000). The incidence rate was 40.7 per 100,000 in children of 1–14 years, 41.7 in young adults of 15–29 years and 4.1 in adult’s ≥ 30 years. Of the 1,101 cases, 248 cases (23%) were hospitalised, 98 cases (9%) had complications and two died – one of respiratory complications (in their mid-30s, with underlying risk factors: morbid obesity and heavy smoking) and the second of neurologic complications (teenager, with an immunodeficiency).
Figure 1.
Notified measles cases by week of rash onset, Nouvelle-Aquitaine region, France, 30 October 2017–1 July 2018 (n = 1,101)
Source: Notification data-Santé publique France.
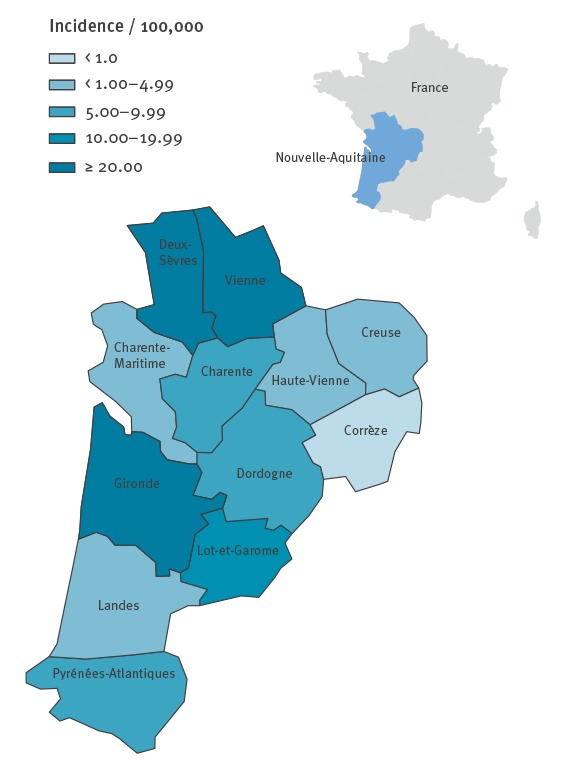
The majority of the 1,101 cases (n = 617; 56%) lived in Gironde, which is NA’s biggest district; all districts reported cases (Figure 2). In NA, the cumulative crude incidence rate was 18.5 per 100,000 population (vs 4.0/100,000 in France during the same period), and reached 39.4 per 100,000 population in Gironde.
Figure 2.
Crude incidence rate of measles, by district, Nouvelle-Aquitaine region, France, 30 October 2017–1 July 2018 (n = 1,101)
Source: Notification data-Santé publique France, extracted on 23 July 2018.
Number of cases: Charente (n = 18), Charente-Maritime (n = 25), Corrèze (n = 2), Creuse (n = 3), Deux-Sèvres (n = 89), Dordogne (n = 31), Gironde (n = 617), Haute-Vienne (n = 14), Landes (n = 19), Lot-et-Garonne (n = 41), Pyrénées-Atlantiques (n = 39), Vienne (n = 203).
A total of 594 (69%) of 860 cases with a known vaccination status were unvaccinated, 128 (15%) had received one dose, 118 (14%) two doses and 20 (2%) had been vaccinated with an unspecified number of doses.
Between 30 October 2017 and 1 July 2018 (study period) genotyping was conducted on 125 specimens by the French National Reference Laboratory for Measles in Caen, leading to the identification of genotype D8 in 105 cases (84%) and genotype B3 in 12 cases (10%). For six specimens the sequencing test was in failure due to limited material.
A total of 176 cases (16%) were related to clusters (n = 19) (Table 1).
Table 1. Characteristics of clusters identified in Nouvelle-Aquitaine region, France, 30 October 2017–1 July 2018, (n = 176).
| Clusters | Number of cases | Week of rash onset of the first case | Number of weeks between the first and the last case | Median age (range) | Number of non-vaccinateda | Number of hospitalisations | |
|---|---|---|---|---|---|---|---|
| N | % | ||||||
| Hospital | |||||||
| University of Bordeauxb | 40 | 46–2017 | 19 | 20 (17–31) | 33 | 100 | 8 |
| University of Poitiers | 21 | 09–2018 | 7 | 20 (18–55) | 11 | 65 | 2 |
| Healthcare facilities | |||||||
| Hospital in Bordeauxc | 26 | 48–2017 | 20 | 26 (0–72) | 10 | 62 | 7 |
| Hospital in Poitiers | 6 | 05–2017 | 1 | 31.5 (28–36) | 4 | 80 | 2 |
| Place assigned for France’s nomadic minorities | |||||||
| Area 1 in Gironde | 8 | 52–2017 | 12 | 18.5 (1–29) | 7 | 100 | 4 |
| Area 2 in Gironde | 3 | 06–2018 | 2 | 3 (1–21) | 3 | 100 | 1 |
| Area 3 in Gironde | 10 | 08–2018 | 7 | 20 (0–28) | 5 | 83 | 2 |
| Area 4 in Gironde | 3 | 07–2018 | 3 | 10 (0–26) | 3 | 100 | 0 |
| Area 1 in Vienneb | 9 | 03–2018 | 3 | 16 (1–49) | 5 | 100 | 7 |
| Area 2 in Vienne | 7 | 04–2018 | 4 | 29 (10–35) | 2 | 100 | 3 |
| Area 1 in Deux-Sèvres | 3 | 05–2018 | 4 | 7 (2–8) | NA | NA | 2 |
| Area 2 in Deux-Sèvresb | 6 | 07–2018 | 6 | 2 (1–24) | 5 | 100 | 0 |
| Area 3 in Deux-Sèvres | 3 | 04–2018 | 2 | 2 (0–6) | 2 | 100 | 0 |
| Private school | |||||||
| Private school of Bordeaux | 5 | 01–2018 | 1 | 5 (4–8) | 5 | 100 | 0 |
| Private school of Vienned | 9 | 11–2018 | 3 | 5 (1–38) | 9 | 100 | 1 |
| Private school of Deux-Sèvres | 5 | 12–2018 | 5 | 11 (7–34) | 4 | 80 | 1 |
| Socially vulnerable people | |||||||
| Migrants | 3 | 12–2018 | 2 | 27 (26–45) | 2 | 100 | 1 |
| Prisoners | 6 | 13–2018 | 6 | 36 (30–43) | 2 | 100 | 0 |
| Childcare centre | |||||||
| Childcare centre in Bordeaux | 3 | 09–2018 | 6 | 0 (0–1) | 3 | 100 | 1 |
NA: not available.
Source: Santé publique France.
a Number of unvaccinated or vaccinated with one dose MMR among with a known vaccination status.
b One epidemiologically linked case lived in another region (not included).
c Vaccination coverage survey conducted among medical staff in Bordeaux University Hospital during the outbreak (in units with high-risk of transmission as emergency, paediatrics, infectious diseases, etc.) estimated a vaccination coverage of 14% for one MMR dose and 34% for two MMR doses.
d Eight epidemiologically linked cases lived in another region (not included).
French vaccination schedule
Measles-containing vaccines have been included in the French vaccination schedule since 1983 with the first dose administered at 12 months of age. In 1996, a second dose was introduced and initially administered at 11 years of age, but changed to 3 to 6 years of age in 1997. This led to a decrease in the number of estimated measles cases (clinical case definition) from 331,000 cases in 1986 to 4,448 cases in 2004 [1]. Despite its increase, vaccination coverage in 2000 remained under the target of 85% for the first dose. A large outbreak occurred between 2008 and 2011, leading to more than 22,000 reported cases [2]. Since 2005, two doses of measles, mumps and rubella (MMR) vaccine has been recommended in France; the first dose administered at 12 months of age and the second dose between 16 and 18 months. A two-dose catch-up measles vaccination is recommended for people born in 1980 and after [3].
Control measures
Specific control measures targeting populations affected by the outbreak were implemented by ARS according to national guidelines, including catch-up and post-exposure vaccination and/or prophylaxis with immunoglobulin for people at high-risk of severe disease [4].
Since December 2017, information regarding the recommended vaccination schedule has been disseminated to the population in NA via various means e.g. newspapers and social media, as well as to health workers (HCWs) and specific at-risk populations such as France nomadic minorities.
Infection control measures such as isolation of cases and airborne precautions were implemented in healthcare facilities and susceptible individuals (unvaccinated HCWs and patients’ contacts without history of measles) were vaccinated to reach two doses of MMR vaccine. MMR catch-up campaigns were undertaken targeting the population around several clusters: University students (Bordeaux and Poitiers), HCWs in Bordeaux hospital, places of France’s nomadic minorities in Gironde and Vienne districts and the prison in Vienne. The outbreak control team established mobile vaccination teams to increase vaccination uptake among these groups.
Discussion
Since May 2017, there has been an increase in measles incidence in several Europe countries [5]. France has been experiencing a large measles outbreak that started in NA, rapidly spread to other regions and resulted in a total of 2,663 cases in France between 30 October 2017 to 1 July 2018 [6]; among which 1,101 occurred in NA (41%) where clusters among under-vaccinated groups were documented.
We also observed cases among fully vaccinated people and the proportion of fully vaccinated among cases was higher than what was observed in France during the 2008–11 epidemic (14% vs 3–4%, respectively). This may be linked to the waning immunity over time among vaccinated people and to a higher proportion of vaccinated cases in a population where the level of vaccination coverage becomes optimal [2,7,8]. But this finding should nevertheless be further investigated.
The second MMR dose vaccination coverage administered at 2 years of age increased from 45–64% in 2010 to 71–81% in 2015 among the districts of NA; yet it remained insufficient to reach the herd immunity threshold of 95% to achieve a high level of population immunity and measles elimination [9,10]. Vaccination coverage is most likely lower among minority groups such as nomadic minorities or confessional groups, but it would not alone account for the low vaccination coverage of the region; further studies are ongoing to estimate vaccination coverage among France's nomadic minorities.
The main circulating genotypes reported in NA were B3 and D8, as observed in the rest of the country and Europe [11].
Two clusters started among university students, which belong to large cohorts with increasing numbers of under-vaccinated (susceptible) people. Crowded environments with close-contact situations such as those observed in students’ communities can greatly contribute to the emergence of outbreaks. Moreover complications are often more frequent and more severe for these age groups [12].
Two of the clusters occurred in healthcare facilities involving HCWs and hospitalised patients, also described in others recent outbreaks [2,13,14]. Despite the existing recommendations for HCWs to be vaccinated against measles, we found among clusters in NA that vaccination coverage of HCWs remained insufficient. Systematic checks and updating of the vaccination status of HCWs and implementation of other control measures are needed to avoid nosocomial measles transmissions, which may have been a main transmission route in this outbreak.
The high proportion of hospitalised cases could suggest that severe cases are more likely to be reported than less severe cases diagnosed by general practitioners (GPs). During the 2008–11 epidemic, a cross-sectional survey conducted among blood donors 18–32 years old in the south-east of France found that only 45% of cases had been notified [15]. Further, during the first weeks of this outbreak, investigations indicated that some of the GPs waited for a laboratory confirmation before notifying the cases. This delay in reporting might have led to a delay in the implementation of control measures and further transmission of disease.
Conclusion
This measles outbreak was the consequence of a suboptimal vaccination coverage in children and insufficient catch-up vaccinations in young adults, resulting in a large reservoir of susceptible individuals. There is an urgent need to improve vaccination coverage with two doses of MMR in NA and France, especially among young adults and in hard-to-reach populations. In 2018, a new law has been enacted that makes MMR vaccination mandatory for the new birth cohorts, which should help reaching the vaccination target of 95% in the future [16]. Prevention of measles transmission in healthcare settings should be strengthened by implementing effective infection control practices and ensuring that all HCWs are immune against measles.
Acknowledgements
We thank the clinicians, biologists, and public health professionals who contributed to the development of this surveillance and the implementation of control measures; and Christian Winter for his careful reading of this manuscript.
Conflict of interest: None declared.
Authors’ contributions: Anne Bernadou was the primary investigator and drafted of the manuscript; Cyril Astrugue, Fatima Aït-Belghiti, Denise Antona and Stéphanie Vandentorren provided epidemiological support during the outbreaks; Julia Dina conducted microbiology investigation; Matthieu Méchain, Valérie Le Galliard, Catherine Verdun-Esquer and France Dupuy were responsible for management of patients. All authors reviewed and approved the final version of the manuscript.
References
- 1.Houssin D, Brücker G. Rougeole: déclaration obligatoire et nouvelles mesures vaccinales. Bull Epidemiol Hebd 2005; 41-42:205-12. [Google Scholar]
- 2.Antona D, Lévy-Bruhl D, Baudon C, Freymuth F, Lamy M, Maine C, et al. Measles elimination efforts and 2008-2011 outbreak, France. Emerg Infect Dis. 2013;19(3):357-64. 10.3201/eid1903.121360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haut Conseil de la Santé publique (HCSP). Calendrier des vaccinations et recommandations vaccinales 2018 [Schedule of vaccinations and vaccination recommendations 2018]. Paris: HCSP; 2018. French. Available from: http://solidarites-sante.gouv.fr/IMG/pdf/calendrier_vaccinations_2018.pdf
- 4.Ministère de la santé et des sports. CIRCULAIRE N°DGS/RI1/2009/334 du 4 novembre 2009 relative à la transmission obligatoire de données individuelles à l’autorité sanitaire en cas de rougeole et la mise en œuvre de mesures préventives autour d’un cas ou de cas groupés. [CIRCULAR N ° DGS / RI1 / 2009/334 of 4 November 2009 on the compulsory transmission of individual data to the health authority in case of measles and the implementation of preventive measures around a case or a cluster]. Code de la santé publique (04/11/2009). French. Available from: http://solidarites-sante.gouv.fr/IMG/pdf/09_334t0pdf.pdf
- 5.European Centre for Disease Prevention and Control (ECDC). Monthly measles and rubella monitoring report July 2018. Stockholm: ECDC; 2018. Available from: https://ecdc.europa.eu/sites/portal/files/documents/Monthly-Measles-Rubella-monitoring-report-July-2018-1.pdf
- 6.Santé Publique France(ANSP). Bulletin épidémiologique rougeole. Données de surveillance au 27 juin 2018[Epidemiological Bulletin Measles. Monitoring Data as of June 27, 2018]. Saint-Maurice: ANSP; 2018. French. Available from: http://invs.santepubliquefrance.fr/Dossiers-thematiques/Maladies-infectieuses/Maladies-a-prevention-vaccinale/Rougeole/Points-d-actualites/Bulletin-epidemiologique-rougeole.-Donnees-de-surveillance-au-27-juin-2018
- 7.Sá Machado R, Perez Duque M, Almeida S, Cruz I, Sottomayor A, Almeida I, et al. Measles outbreak in a tertiary level hospital, Porto, Portugal, 2018: challenges in the post-elimination era. Euro Surveill. 2018;23(20):18-00224. 10.2807/1560-7917.ES.2018.23.20.18-00224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hahné SJM, Nic Lochlainn LM, van Burgel ND, Kerkhof J, Sane J, Yap KB, et al. Measles Outbreak Among Previously Immunized Healthcare Workers, the Netherlands, 2014. J Infect Dis. 2016;214(12):1980-6. 10.1093/infdis/jiw480 [DOI] [PubMed] [Google Scholar]
- 9.Santé publique France (ANSP). Bulletin de santé publique Nouvelle-Aquitaine. Vaccination [Nouvelle-Aquitaine Public Health Bulletin. Vaccination]. Bordeaux: ANSP; 2018.French. Available from: http://invs.santepubliquefrance.fr/fr/Publications-et-outils/Bulletin-de-veille-sanitaire/Tous-les-numeros/Nouvelle-Aquitaine/Bulletin-de-sante-publique-Nouvelle-Aquitaine.-Avril-2018
- 10.World Health Organization (WHO). Global measles and rubella strategic plan: 2012. Geneva: WHO; 2012. Available from: http://apps.who.int/iris/bitstream/handle/10665/44855/9789241503396_eng.pdf?sequence=1
- 11.European Centre for Disease Prevention and Control (ECDC). Risk of measles transmission in the EU/EEA, 21 March 2018. Stockholm: ECDC; 2018.Available from: https://ecdc.europa.eu/sites/portal/files/documents/Measles-rapid-risk-assessment-European-Union-countries.pdf
- 12.Béraud G, Abrams S, Beutels P, Dervaux B, Hens N. Resurgence risk for measles, mumps and rubella in France in 2018 and 2020. Euro Surveill. 2018;23(25):1700796. 10.2807/1560-7917.ES.2018.23.25.1700796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Filia A, Bella A, Del Manso M, Baggieri M, Magurano F, Rota MC. Ongoing outbreak with well over 4,000 measles cases in Italy from January to end August 2017 - what is making elimination so difficult? Euro Surveill. 2017;22(37):30614. 10.2807/1560-7917.ES.2017.22.37.30614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grammens T, Schirvel C, Leenen S, Shodu N, Hutse V, Mendes da Costa E, et al. Ongoing measles outbreak in Wallonia, Belgium, December 2016 to March 2017: characteristics and challenges. Euro Surveill. 2017;22(17):30524. 10.2807/1560-7917.ES.2017.22.17.30524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Antona D, Gallian P, Gimeno L, Fonteneau L, Jacquot C, Morel P, et al. Enquête de séroprévalence rougeole-rubéole chez les donneurs de sang, France, 2013 [Measles-rubella seroprevalence survey in blood donors, France, 2013]. Jounées nationales infectieuses; 2015 June 10-12, Nancy.French. Available from: http://www.infectiologie.com/UserFiles/File/medias/JNI/JNI15/posters/2015-poster-JNI-PADS01-07.pdf
- 16.Ministère des solidarités et de la santé. Article L3111-2, L3111-2. Code de la santé publique (01/01/2018) [public health code (01/01/2018)]. French. Available from: https://www.legifrance.gouv.fr/affichCodeArticle.do?cidTexte=LEGITEXT000006072665&idArticle=LEGIARTI000006687781


