Abstract
Background:
A rectus abdominis–adductor longus (RA-AL) aponeurotic plate injury, commonly associated with athletic pubalgia, sports hernia, or a core muscle injury, causes significant dysfunction in athletes. Increased recognition of this specific injury distinct from inguinal hernia abnormalities has led to better management of this debilitating condition.
Hypothesis:
Surgical repair of RA-AL aponeurotic plate injuries will result in decreased symptoms and high rates of return to play.
Study Design:
Case series; Level of evidence, 4.
Methods:
Using our billing and clinical database, patients who underwent RA-AL aponeurotic plate repair by a single surgeon at a single institution were contacted for Hip Outcome Score (HOS) and return-to-play data. Patients with a confirmed diagnosis by history, physical examination, and magnetic resonance imaging who failed 6 to 12 weeks of appropriate conservative treatment were indicated for surgery. Surgical repair involved adductor longus fractional lengthening, limited adductor longus tenotomy, and a turn-up flap of the released adductor tendon and aponeurosis onto the rectus abdominis for imbrication reinforcement.
Results:
Of 100 patients who met the inclusion criteria, 85 (85%) were contacted. A total of 82 (96%) patients were able to return to play at a mean of 4.1 months after repair. Hip function was rated as 98% of normal and sports function as 92% of normal. Factors associated with negative outcomes were multiple procedures, prior inguinal hernia repair, and female sex. Negative outcomes were demonstrated by decreased HOS scores and decreased sports function. The overall complication rate was 7%.
Conclusion:
RA-AL aponeurotic plate repair by the method of an adductor-to–rectus abdominis turn-up flap is a safe procedure with high return-to-play success. Patients who had previously undergone inguinal hernia repair or other hip/pelvic-related surgery and female patients had worse outcomes.
Keywords: groin, athletic pubalgia, sports hernia, core muscle
Athletic pubalgia can be a very debilitating injury in athletes, particularly in explosive and rotationally demanding sports. This entity commonly includes “sports hernia” or core muscle injuries, pubic arthropathy/osteitis pubis, entrapment neuropathies, and rectus abdominis–adductor longus (RA-AL) aponeurotic plate injuries. Many careers have been affected because of hip or groin injuries.10 Athletic competition that involves hyperextension of the hip and trunk with twisting motions such as kicking or a hockey slap shot generates tremendous forces across the common tendon attachment of the rectus abdominis and adductor longus tendons.6,22 Repetitive trauma or single episodes can result in strain or avulsion at this attachment, leading to significant dysfunction in twisting, cutting, or pivoting sports. Historically, this was felt to be symptomatic inguinal canal insufficiency without true herniation, and treatment was based on standard hernia repair techniques.4,7,8,11,23 In addition to other sources of groin pain, this specific injury to the aponeurotic plate is becoming more recognized as a distinct tendinous injury, thus requiring more specific structural repair.
In several previously published reports using varying techniques, return to play was good, with rates ranging from 80% to 97%, but some athletes experienced failure of treatment.13,17,21,26 As more attention was drawn to this condition, advanced imaging and specialized evaluations uncovered the injury to the common aponeurosis of the rectus abdominis and adductor longus as a cause of athletic pubalgia (Figure 1). Several authors began to recognize the involvement of the adductor tendon and began performing adductor tenotomy along with standard herniorrhaphy.1,2,7,17,18,26 Both laparoscopic and open techniques have been used, and techniques include plication of the inguinal canal structures, suturing of the conjoint tendon to the inguinal ligament, and even the use of mesh for inguinal canal or pelvic floor reconstruction. A “minimal repair” technique with primary neurolysis and/or neurectomy of the genital branch of the genitofemoral nerve has also been described.20 There remains a lack of consensus on the definitive lesion and appropriate treatment.
Figure 1.
The relationship of the common aponeurosis of the rectus abdominis and adductor longus demonstrated in the coronal and sagittal planes. Image courtesy of OBERD. Reproduced with permission.
In 2012, the senior author (B.A.E.) began performing a technique for RA-AL aponeurotic plate injuries with an adductor-to–rectus abdominis turn-up flap. The purpose of this article is to present our current surgical technique and outcomes with this repair in the first consecutive 100 patients.
Methods
This study was approved by the institutional review board of St Vincent’s Health System. Patients were identified in our clinical and billing records based on Current Procedural Terminology codes 27299 and 27299SH. Operative notes were reviewed, and patients were selected if they underwent our standard repair of the RA-AL aponeurotic plate. A minimum 6-month follow-up was required, and there were no exclusions. Patient sex, age, and unilateral versus bilateral involvement were all recorded. Patients were then contacted for a telephone interview and inclusion in the study. Verbal consent for inclusion was obtained before conducting the telephone interview. The Hip Outcome Score (HOS) was used as a standardized metric. The HOS was selected as the most commonly used outcome measure with athletic-related hip injuries, and it includes a sport subscale (HOS-Sport). Subjective scores assessing overall hip function (normal, nearly normal, abnormal) and sports function (≥90% or <90%) were also obtained. Additional information gathered included prior surgery, additional surgeries, previous invasive treatment, time to return to full competition, sexual or urinary dysfunction, and highest postoperative level of competition.
Subgroup analysis was completed to evaluate the small subset of patients who were either unable to return to competition or felt a significant loss of function after surgery. A complication was defined as the need for a second surgical procedure at the same location, a localized infection, or an anesthetic-related complication.
Patient Evaluation
Our history and examination followed an organized progression. History was taken in detail and often pointed quickly toward the correct diagnosis. The majority of patients experienced an acute “sentinel” groin injury that progressed subacutely to pain in the lower abdomen; however, many experienced an insidious onset. An inability to perform explosive movements, perform lateral or rotational changes in direction, or sustain peak performance was most commonly reported. Injury date, sport, level of play, prior surgery, and a comprehensive review of systems were recorded. The physical examination began with a general assessment of the patient's overall condition. A complete evaluation of hip range of motion along with impingement testing were performed because of the high incidence of femoroacetabular impingement (FAI) associated with athletic pubalgia.5 Pain or loss of motion with flexion, adduction, and internal rotation or flexion, abduction, and internal rotation indicated FAI as a potential concomitant diagnosis.
The examination of the pubic symphysis and groin began with visualization. Bruising or swelling could indicate an acute injury, and prior incisions might be recognized, which were critical in this patient population because of the incidence of prior surgeries. Palpation was critical to assessing the location of the abnormality. Tenderness directly over the midline indicated potential osteitis pubis. Other entities such as symphyseal arthritis or infection would also be tender to palpation at the midline. Lateral compression of the pelvis could also cause pain at the midline. Tenderness immediately lateral to the symphysis, where the common aponeurosis of the adductor longus and rectus abdominis attaches to the pubis, indicated a common site for pain with an RA-AL aponeurotic plate injury. Specific to the RA-AL aponeurotic plate evaluation was pain at the same location with resisted sit-ups and simultaneous resisted adduction. These reliably produced pain directly over the pubic tubercle or slightly distal over the adductor tendon.
Imaging results were also critically evaluated. A standard anteroposterior radiograph was obtained in patients with groin pain toward the midline. If patients had 1 or both hips involved in their reported symptoms, anteroposterior and frog-leg lateral radiographs were obtained. Plain radiography assists in the evaluation of bony abnormalities such as heterotopic ossification, osteophytes, or FAI. Magnetic resonance imaging (MRI) is our preferred technique for an RA-AL aponeurotic plate evaluation. Plain pelvic MRI is used unless concomitant intra-articular hip abnormalities are suspected, in which case a magnetic resonance arthrogram is obtained. Other intra-abdominal abnormalities can be identified, and the rectus and adductor tendons are best visualized on MRI. Tendon avulsions or tendinitis could be seen, as increased signal and frank detachment might be visible. Our most common finding, shown in Figures 2 and 3, was a partial tendon avulsion from the inferior edge of the superior pubic ramus. This has been termed a “superior cleft sign.”19
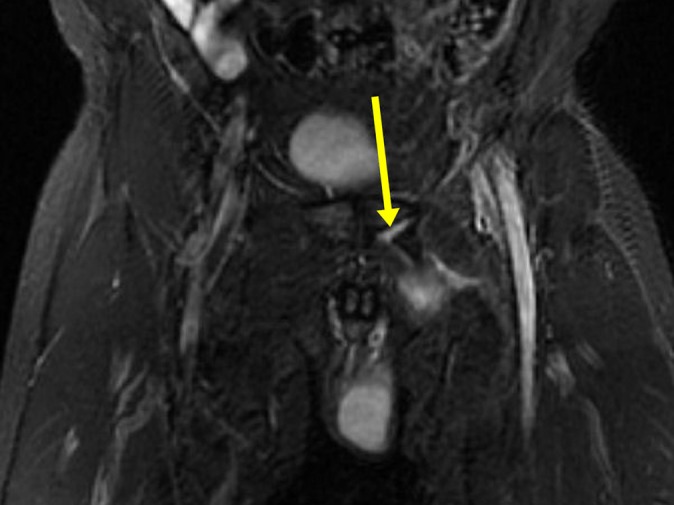
Figure 2.

Coronal STIR (short tau inversion recovery) magnetic resonance imaging of the pelvis in a 21-year-old male patient with left-sided groin pain. There is a defect in the common aponeurosis of the rectus abdominis and adductor longus tendon, as indicated by the larger yellow arrow. Also, a subtle area of edema along the inferior edge of the superior pubic ramus is seen along the muscular attachment (smaller green arrow).
Figure 3.
Coronal T2-weighted magnetic resonance imaging of the pelvis in a 19-year-old male patient with left-sided groin pain demonstrates a more significant defect in the common aponeurosis of the rectus abdominis and adductor longus tendon (arrow).
Surgical Indications
Surgery was considered only after conservative treatment had failed. All patients underwent an attempt with a combination of active rest, nonsteroidal anti-inflammatory drugs if able, physical therapy, and at times local corticosteroid injections. Six to 12 weeks was our standard duration of conservative treatment. If symptoms were tolerable, in-season athletes were allowed to return to sport if able. When symptoms still persisted, surgery was indicated.
Surgical Technique
Patients were placed supine on the operating table, and their hair was clipped before the area was prepped and draped in a typical fashion. Bony landmarks were palpated and marked. The patient’s legs were placed in the frog-leg position. A 4-cm horizontal incision was made on the injured side along the superior pubic ramus in the upper one-third of the bone. This was then carried down with scissor dissection spreading in the cephalad-to-caudad direction to protect superficial neural structures. In male patients, the spermatic cord was palpated and retracted medially for protection. The common aponeurosis of the adductor longus and rectus abdominis was identified (Figure 4). Needle-tip electrocautery was used to perform fractional lengthening and incomplete adductor longus tenotomy anteriorly (from medial to lateral) approximately 1 cm off the pubic origin, leaving a 1-cm flap of the adductor tendon at the pelvic attachment (Figure 5). This tendon flap was then folded back and turned up onto the rectus aponeurosis, and 3 nonabsorbable figure-of-8 sutures were used to join the rectus, underlying periosteum, and adductor flap (Figure 6). Early in the series, a deep drain was placed and removed at the physical therapy recheck on the first postoperative day. During the series, the change was made to placing thrombin-soaked Gelfoam (Pfizer) in the fractionated adductor site in lieu of a deep drain (Figure 7). After irrigation, the wound was closed with buried 3-0 Monocryl (Ethicon) and running 3-0 Monocryl, and island dressings were placed.
Figure 4.
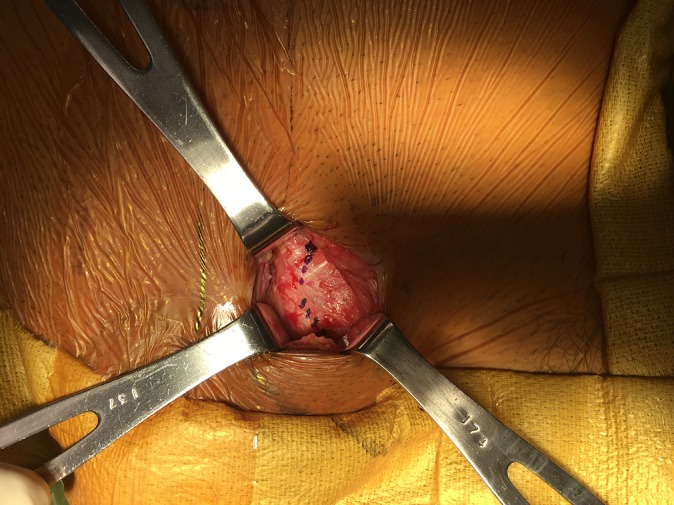
The deep investing fascial layer is exposed. A surgical marking pen has been used to outline the lateral border of the rectus abdominis and adductor longus at their common attachment points of the pubis.
Figure 5.
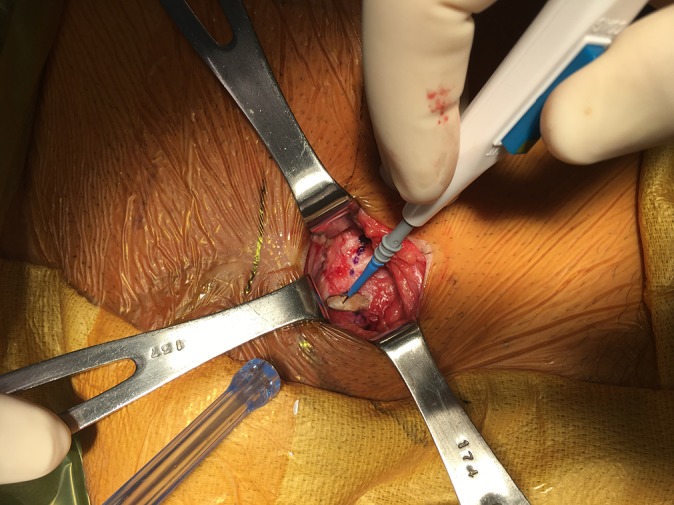
Needle-tip electrocautery is utilized to perform limited adductor longus tenotomy and generate a soft tissue sleeve to turn up, repair, and reinforce the rectus abdominis to the pubis.
Figure 6.

Nonabsorbable suture is used for repair.
Figure 7.

Gelfoam is used for hemostasis and a void filler to facilitate reconstitution of the fractionated adductor longus tendon.
Physical therapy began on postoperative day 1. Phase 1, consisting of weeks 1 and 2, was focused on decreasing pain and inflammation by stretching, walking, and cryotherapy. Recruitment of the transversus abdominis with controlled isometrics was initiated. Week 2 comprised more active hip and core exercises including hip strengthening, mini-squats, lunges, pelvic tilts, and continued stretching. Phase 2, consisting of weeks 3 and 4, began when the patient had minimal pain, improved hip and spine range of motion, an ability to achieve a neutral spine, and recruitment of the transversus abdominis. Core activity was significantly increased in weeks 3 and 4. The single-leg stance and perturbations improved hip and core strength. More aggressive stretching was permitted, and jogging was initiated. Phase 3, the advanced exercise phase, was centered around returning to light sport activity and the ability to initiate the single-leg stance with good stabilization of the spine and pelvis. Core and hip strengthening was increased, plyometric training was initiated, and light sport activity was started but without cutting or lateral movements. Cutting, agility, pivoting, and speed training began around week 6. Return to play was allowed once certain criteria were met: full range of motion without pain, equal hip strength, sport-specific drills without pain, and satisfactory physical examination findings by the physician.
Statistical Analysis
Descriptive and inferential calculations were made using SAS 9.4 (SAS Institute). Subgroups were defined, and comparisons were made using the Student t test and chi-square test. Statistically significant differences in HOS scores were considered clinically nonsignificant if they did not exceed the minimal clinically important difference (MCID) of 9 points for the HOS–Activities of Daily Living or 6 points for the HOS-Sport.16 Mixed stepwise logistic and generalized linear regression was used to determine the best predictors for positive outcomes as measured by return to sport, return to sport in less than 6 months, sports function >90%, normal hip function, and absence of complications or sexual/genitourinary dysfunction. Predictors included patient sex, concomitant procedures, previous inguinal hernia repair, laterality (unilateral vs bilateral), number of procedures performed, and age at surgery. Variables with a P value <.25 were entered into the model, and variables with a P value >.15 were removed. Second-level interactions were considered for all predictors. Differences with P < .05 were considered significant.
Results
In total, 100 patients were identified, and 85 patients were interviewed, resulting in an 85% follow-up rate. The mean follow-up time was 25.8 ± 13.2 months (range, 6.9-53.8 months). There were no significant baseline demographic or intraoperative differences between those who were successfully followed up via telephone and those who were not able to be contacted. The mean age at surgery was 26.0 ± 10.9 years (range, 15-65 years). Male patients were the majority (86%), and the most commonly reported sport played was football (34%). Most patients competed at the collegiate level at the time of surgery (49%), although 29% were recreational athletes. The vast majority of repairs were performed unilaterally (92%). Thirty-one patients (38%) had undergone some prior medical treatment for abdominal/groin pain, of whom 9 had a prior inguinal hernia that was surgically repaired. Full baseline demographics and intraoperative information can be found in Table 1. Six patients experienced a surgical complication, for an overall complication rate of 7%. Complications included 2 unconfirmed retears, 2 superficial wound infections, 1 hematoma, and 1 reoperation for heterotopic ossification. Eight patients experienced transient sexual dysfunction, and no patients experienced urinary dysfunction. The majority of patients (87%) rated their hip function after surgery as normal.
TABLE 1.
Patient Demographicsa
| Female (n = 12) | Male (n = 73) | Total (N = 85) | P Value | |
|---|---|---|---|---|
| Age, mean ± SD, y | 28.8 ± 9.7 | 25.5 ± 11.1 | 26.0 ± 10.9 | .35 |
| Sport played | .073 | |||
| Baseball | 0 (0) | 9 (13) | 9 (11) | |
| Basketball | 0 (0) | 3 (4) | 3 (4) | |
| Football | 0 (0) | 29 (41) | 29 (34) | |
| Running/track & field | 3 (25) | 10 (14) | 13 (16) | |
| Soccer | 2 (17) | 6 (8) | 8 (10) | |
| Softball | 1 (8) | 3 (4) | 4 (5) | |
| Tennis | 2 (17) | 4 (6) | 6 (7) | |
| Weight lifting/exercise | 3 (25) | 5 (7) | 8 (10) | |
| Other | 1 (8) | 4 (6) | 5 (6) | |
| Level of play | .28 | |||
| Recreational | 6 (50) | 19 (27) | 25 (29) | |
| High school | 2 (17) | 10 (14) | 12 (14) | |
| Collegiate | 3 (25) | 39 (55) | 42 (49) | |
| Professional/Olympic | 1 (8) | 5 (7) | 6 (7) | |
| Bilateral repair | 1 (7) | 6 (8) | 7 (8) | .99 |
| Previous inguinal hernia repair | 2 (14) | 7 (10) | 9 (11) | .61 |
aData are expressed as n (%) unless otherwise indicated.
Overall, 82 athletes (96%) were able to return to sport, with a mean recovery time of 4.1 ± 2.3 months (range, 1-12 months) (Table 2). Of those who returned, the majority did so in less than 6 months (87%). The mean HOS score for all patients was 99.1 ± 3.7 (range, 76-100), and the mean HOS-Sport subscore was 96.4 ± 9.7 (range, 42-100). In addition to the HOS, patients subjectively rated their hip function as 98% of normal and their sports function as 92% of normal, and 78% of athletes reported sports function of at least 90% of normal (Table 3).
TABLE 2.
Return-to-Play Outcomesa
| Returned to Play | Time to Return to Play, mo | HOS Score | HOS-Sport Subscore | |||||
|---|---|---|---|---|---|---|---|---|
| n (%) | P Value | Mean ± SD | P Value | Mean ± SD | P Value | Mean ± SD | P Value | |
| Overall | 82/85 (96) | 4.1 ± 2.3 | 99.1 ± 3.7 | 96.4 ± 9.7 | ||||
| Sex | .37 | .26 | .015 | .028 | ||||
| Female | 11/12 (92) | 4.9 ± 3.3 | 99.5 ± 2.9 | 90.8 ± 17.2 | ||||
| Male | 71/73 (97) | 4.0 ± 2.1 | 96.7 ± 6.7 | 97.3 ± 7.6 | ||||
| Age | >.99 | .82 | .87 | .99 | ||||
| ≤25 y | 57/59 (97) | 4.2 ± 2.2 | 99.1 ± 3.6 | 96.4 ± 9.8 | ||||
| >25 y | 25/26 (96) | 4.1 ± 2.5 | 99.0 ± 4.2 | 96.4 ± 9.7 | ||||
| Prior procedures | .008 | .039 | <.001 | <.001 | ||||
| Yes | 15/18 (83) | 5.2 ± 2.9 | 95.9 ± 7.4 | 89.3 ± 18.6 | ||||
| No | 67/67 (100) | 3.9 ± 2.1 | 99.9 ± 0.4 | 98.3 ± 3.7 | ||||
| Repair laterality | >.99 | .34 | .56 | .84 | ||||
| Unilateral | 75/78 (96) | 4.2 ± 2.3 | 100.0 ± 3.9 | 96.4 ± 10.1 | ||||
| Bilateral | 7/7 (100) | 3.4 ± 1.9 | 99.9 ± 0.4 | 97.1 ± 3.2 | ||||
| Previous inguinal hernia | .29 | .027 | .067 | .030 | ||||
| Yes | 8/9 (89) | 5.8 ± 3.6 | 95.9 ± 8.1 | 89.8 ± 18.6 | ||||
| No | 73/75 (97) | 3.9 ± 2.0 | 99.4 ± 2.7 | 97.2 ± 8.0 | ||||
aHOS, Hip Outcome Score.
TABLE 3.
Functional Outcomesa
| Hip Function | Sports Functionb | ||||||
|---|---|---|---|---|---|---|---|
| Normal | Nearly Normal | Abnormal | P Value | ≥90% | <90% | P Value | |
| Overall | 74/85 (87) | 7/85 (8) | 4/85 (5) | 65/83 (78) | 18/83 (22) | ||
| Sex | .047 | .28 | |||||
| Female | 8/12 (67) | 2/12 (17) | 2/12 (17) | 8/12 (67) | 4/12 (33) | ||
| Male | 66/73 (90) | 5/73 (7) | 2/73 (3) | 57/71 (80) | 14/71 (20) | ||
| Age | .96 | >.99 | |||||
| ≤25 y | 51/59 (86) | 5/59 (8) | 3/59 (5) | 46/59 (78) | 13/59 (22) | ||
| >25 y | 23/26 (88) | 2/26 (8) | 1/26 (4) | 19/24 (79) | 5/24 (21) | ||
| Prior procedures | .007 | <.001 | |||||
| Yes | 12/18 (67) | 3/18 (17) | 3/18 (17) | 59/66 (89) | 7/66 (11) | ||
| No | 62/67 (93) | 4/67 (6) | 1/67 (1) | 6/17 (35) | 11/17 (65) | ||
| Repair laterality | .57 | .11 | |||||
| Unilateral | 67/78 (86) | 7/78 (9) | 4/78 (5) | 62/77 (81) | 15/77 (19) | ||
| Bilateral | 7/7 (100) | 0/7 (0) | 0/7 (0) | 3/6 (50) | 3/6 (50) | ||
| Previous inguinal hernia | .16 | .011 | |||||
| Yes | 6/9 (67) | 2/9 (22) | 1/9 (11) | 3/8 (38) | 5/8 (63) | ||
| No | 67/75 (89) | 5/75 (7) | 3/75 (4) | 61/74 (82) | 13/74 (18) | ||
aData are expressed as n (%).
bTwo male patients did not provide their estimated sports function.
Male patients reported statistically significantly higher HOS scores (P = .015) compared with female patients, although this difference did not exceed the MCID for the HOS. However, male patients also had significantly higher HOS-Sport subscores (P = .028) that were greater than the MCID for the HOS-Sport. Male patients also reported their hip function as 8.7 percentage points higher than female patients (P < .001) and their sports function as 12.1 percentage points higher than female patients (P = .009) and were more likely to report normal hip function (P = .047). Patients who had undergone prior procedures were less likely to return to play (P < .001), were less likely to report their hip function as normal (P = .007), were less likely to report their sports function as ≥90% (P < .001), scored 9.0 points lower on the HOS-Sport (P < .001), and were more likely to experience sexual dysfunction (P = .038) when compared with patients having undergone isolated sports hernia repair. Of those who returned to sport, athletes who had undergone prior procedures required 1.3 additional months to be able to return (P = .039). Athletes who had undergone previous inguinal hernia repair were less likely to report their sports function as ≥90% (P = .011), required 1.8 additional months to return to play (P = .027), and scored 7.4 points lower on the HOS-Sport (P = .030). Patients undergoing bilateral repair did not fare differently compared with patients undergoing unilateral RA-AL aponeurotic plate repair, nor did age have any significant effect.
Stepwise logistic regression analysis revealed predictive models that identified a number of significant markers of surgical success. Patients undergoing isolated RA-AL aponeurotic plate repair were 6.2 times (95% CI, 1.6-23.6) more likely to report normal hip function (P = .008) and 15.5 times (95% CI, 4.4-54.8) more likely to report sports function ≥90% (P < .001) compared with patients who underwent prior procedures. Each additional procedure performed resulted in a 3.0-fold likelihood (95% CI, 1.3-7.2) of being unable to return to sport in less than 6 months (P = .014). A significant interaction between patient sex and prior procedures was also found with respect to the HOS-Sport (P = .011): female patients who underwent at least 1 additional procedure scored significantly lower on the HOS-Sport than female patients who underwent isolated RA-AL aponeurotic plate repair (P < .001). Male patients experienced no such significant change in the HOS with respect to prior procedures performed (P = .95).
Discussion
Our rationale for this technique is derived from understanding the pathoanatomy of the RA-AL aponeurotic plate injury. Structurally, the common aponeurosis of the rectus and adductor is compromised chronically because of repetitive microtrauma and/or acutely because of disruption. Performing fractional lengthening of the adductor longus allows excessive tension to be relieved from the tendon and muscular compartment. Subsequently, limited tenotomy allows a structural layer to be turned up to reinforce the terminal insertion of the rectus while imbricating the injured region of the aponeurotic plate.
Our results compare favorably with previously reported findings of the outcomes for surgical repair of structurally related injuries across multiple subsets in the setting of “athletic pubalgia” (Table 4). In the current study, 96% of patients were able to return to sport at a mean 4.1 months (17.8 weeks) after surgical repair, compared with previous studies, in which 79% to 100% of athletes returned at a mean 2 to 30 weeks after a wide variety of surgical treatments for varying anatomic entities.3,12,14,15,17,20,24–27
TABLE 4.
Comparative Techniquesa
| Study | Total (male/female), n | Age Range, y | Repair Technique | RTP Rate, % | Mean Time to RTP, wk |
|---|---|---|---|---|---|
| Current study | 85 (73 /12) | 15-65 | Common aponeurosis repair | 96 | 17.8 |
| Previous literature (weighted average) | 583 (579/4) | 17-50 | 92 | 9.9 | |
| Meyers et al17 (2000) | 157 (157/0) | NR | Pelvic floor repair | 96 | NR |
| Muschaweck and Berger20 (2010) | 129 (128/1) | 21-29 | Minimal repair | 83 | 2.0 |
| Brannigan et al3 (2000) | 85 (85/0) | 18-50 | Modified Shouldice repair | 96 | NR |
| Polglase et al24 (1991) | 64 (62/2) | NR | Bassini repair with Tanner slide or transversalis fascia plication | 93 | NR |
| Malycha and Lovell15 (1992) | 50 (NR) | NR | Posterior inguinal wall reinforcement | 93 | NR |
| Steele et al25 (2004) | 47 (47/0) | 19-41 | Modified Bassini repair | 79 | NR |
| Joesting12 (2002) | 45 (NR) | NR | Modified Lichtenstein repair | 90 | NR |
| Van Der Donckt et al26 (2003) | 41 (41/0) | 17-34 | Bassini repair and adductor longus tenotomy | 100 | 30.0 |
| Kumar et al14 (2002) | 35 (34/1) | 23-45 | Repair of external oblique and Prolene darn or Lichtenstein mesh repair of posterior inguinal canal | 93 | 14.0 |
| Ziprin et al27 (1999) | 25 (25/0) | 22-37 | Repair of external oblique and inguinal canal | 100 | 11.6 |
aNR, not reported; RTP, return to play.
Nonetheless, our results raise several questions, and there does appear to be an association with poorer outcomes after RA-AL aponeurotic plate repair. Our indications are based on very specific clinical and imaging findings, yielding a reliable return to high-level athletics. However, there appear to be factors associated with a delayed return, a partial return, or an inability to return. A small subset of patients had significant dysfunction even with normal daily activities.
Prior surgical treatment of an inguinal hernia correlated with decreased return to play and significantly poorer outcomes. Within this subset of patients, there was significant overlap with the patient group that underwent multiple operative procedures. There were patients who had undergone more than 1 inguinal hernia repair, and none improved their pain or function. The inability to return to high-level competition raises the question of failed inguinal hernia repair in the setting of RA-AL aponeurotic plate injuries. However, of the patients with prior inguinal hernia repair, 1 was a Division I track athlete, 1 was a collegiate soccer player, and 1 was a collegiate cheerleader. The track athlete rated himself at 95% of normal and only had some soreness at top speeds. The soccer player returned to 85% of normal sports function and was able to play more than 80 minutes, with only limited soreness after practices or games. Prior hernia surgery is not necessarily a marker of poor outcomes, but patients with prior inguinal hernia surgery for the same complaint need to be carefully evaluated and appropriately counseled. Patients who have undergone more total procedures to the groin or hip region also need to be cautioned that a longer return to sport or worse overall functional scores are not uncommon in this patient group.
In contrast, patients who underwent a single surgical procedure did extremely well. All were able to return to sport, with the lowest sports function rating of 80% of normal. Overall, the sports function scores averaged 96%. There were no complications. The mean time to return to play was 3.9 months. None of the patients reported abnormal function, and only 1 rated his or her hip function as “nearly normal” instead of “normal.” The HOS scores were also the highest of all groups. As with most other surgical procedures of this nature, the initial procedure typically yields the best outcomes, and poorer outcomes tend to follow with subsequent operative procedures. This appeared to hold true with the current cohort as well, and the difference was dramatic. Some difference is expected simply because of postoperative scarring causing pain, but the functional differences and speed of return to play suggest that the dysfunction caused by higher numbers of prior surgeries and/or other coexisting abnormalities (FAI, entrapment neuropathies, osteitis pubis, psychosocial factors, etc) offsets the benefits of RA-AL aponeurotic plate repair alone. A statistically significant difference was found in functional percentages, HOS scores, and rates of return to play. This is a strong conclusion, and while the numbers associated with prior inguinal hernia repair were relatively low, a thorough evaluation is critical, and careful consideration is paramount.
The difference in outcomes between men and women is complex because of confounding factors. RA-AL aponeurotic plate injuries are less common in women, and women have more potential sources for the cause of pelvic or groin pain.17 Nevertheless, this is the largest series to date describing women undergoing RA-AL aponeurotic plate repair. Half of the women had undergone more than 1 surgical procedure: 3 with prior hernia repair and 2 with prior hip arthroscopic surgery for FAI. A statistically significant difference between sexes was found in hip function, sports function, and the HOS score but not in time to return to play. There was, however, a statistically significant difference in the number of operative procedures in women, which may represent at least part of the cause of the worse outcomes. Despite these differences, 5 of 11 women returned to 100% athletic function, of whom 1 had undergone 3 prior inguinal hernia repairs and 1 had undergone hip arthroscopy. Childbearing and other gynecological conditions could have some effect here, but those data are not available.
One published series that examined inguinal canal abnormalities reported 15 athletes who underwent plication of the transversalis fascia and suturing of the conjoint tendon to the inguinal ligament.8 While 13 patients successfully returned to sport, 2 required eventual adductor release and were subsequently able to return to play.
Meyers et al18 published a series of 8500 patients evaluated for groin pain, which included over 5000 surgical procedures. They identified multiple different abnormalities, which were addressed with 26 different procedures. Roughly 70% of these patients suffered from adductor and rectus injuries and were treated with rectus repair and adductor tenotomy. Overall, 95% were able to return to full athletic competition within 3 months.
Athletic pubalgia is also seen at high rates in athletes with FAI. Hammoud et al9 retrospectively evaluated 38 professional athletes who had undergone arthroscopic treatment of FAI and who also had symptoms of athletic pubalgia; 32% had previously undergone surgery for athletic pubalgia, and 1 patient underwent both FAI and athletic pubalgia surgery performed in the same setting. In this subgroup with FAI and athletic pubalgia, none returned to competition with AP repair alone. Symptoms related to athletic pubalgia resolved after FAI treatment alone in 39% of patients. All patients who underwent athletic pubalgia and FAI surgery returned to professional sport, with 36 of 38 patients returning to previous levels of play. In the current study, 4 patients had undergone prior hip arthroscopic surgery for FAI, and 1 underwent subsequent hip arthroscopic surgery. One was unable to return to athletics, reported a functional score of 40%, and suffered from dyspareunia. Another suffered from dyspareunia and reported her athletic function as 20%. She is currently being evaluated for nerve entrapment. The other 3 patients are doing excellently. We do not have data collected on patients presenting with both athletic pubalgia and FAI symptoms for comparison with the data from Hammoud et al.9
The weaknesses of our study include the retrospective nature and lack of control group. Future prospective studies with preoperative scores and preinjury sport-specific statistical data could better define improvement after surgery and any residual functional deficit after repair. Biomechanical testing of adductor strength could determine the weakness, if any, caused by adductor tenotomy. Functional scores were subjective, and return-to-play data were based on patient recall, so these must be cautiously weighed. Preoperative data on duration of symptoms were also not available. Analysis of specific patient groups was limited because of the small sizes of these patient subsets. The causality of specifics such as prior hernia surgery, female sex, and total number of surgical procedures is difficult because of the significant crossover within these groups. Limited data on level of play before and after surgery was also a significant limitation of our study. Furthermore, follow-up imaging would substantiate reconstitution of the RA-AL aponeurotic plate.
Conclusion
This study showed that our technique for RA-AL aponeurotic plate repair is safe and effective in patients diagnosed with RA-AL aponeurotic plate injuries. The complication rate was low, and functional outcome scores were overall excellent. Patients who had undergone prior surgery, especially female patients, had a longer return to sport and had significantly lower functional scores. Conversely, patients who underwent a single surgical procedure did exceptionally better. Patients were able to return to prior levels of sport at a high rate, and only a small proportion experienced any functional deficits. Athletic pubalgia with an RA-AL aponeurotic plate injury can safely and effectively be treated with an adductor-to–rectus abdominis turn-up flap.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from St Vincent’s Health System.
References
- 1. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia. Ann Plast Surg. 2005;55(4):393–396. [DOI] [PubMed] [Google Scholar]
- 2. Akermark C, Johansson C. Tenotomy of the adductor longus tendon in the treatment of chronic groin pain in athletes. Am J Sports Med. 1992;20(6):640–643. [DOI] [PubMed] [Google Scholar]
- 3. Brannigan AE, Kerin MJ, McEntee GP. Gilmore’s groin repair in athletes. J Orthop Sports Phys Ther. 2000;30(6):329–332. [DOI] [PubMed] [Google Scholar]
- 4. Brunt LM. Surgical treatment of sports hernia: open mesh approach In: Diduch DR, Brunt LM, eds. Sports Hernia and Athletic Pubalgia. New York, NY: Springer US; 2014:133–142. [Google Scholar]
- 5. Economopoulos KJ, Milewski MD, Hanks JB, Hart JM, Diduch DR. Radiographic evidence of femoroacetabular impingement in athletes with athletic pubalgia. Sports Health. 2014;6(2):171–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Estwanik JJ, Sloane B, Rosenberg MA. Groin strain and other possible causes of groin pain. Phys Sportsmed. 1990;18(2):54–65. [DOI] [PubMed] [Google Scholar]
- 7. Farber AJ, Wilckens JH. Sports hernia: diagnosis and therapeutic approach. J Am Acad Orthop Surg. 2007;15(8):507–514. [DOI] [PubMed] [Google Scholar]
- 8. Hackney RG. The sports hernia: a cause of chronic groin pain. Br J Sports Med. 1993;27(1):58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hammoud S, Bedi A, Magennis E, Meyers WC, Kelly BT. High incidence of athletic pubalgia symptoms in professional athletes with symptomatic femoroacetabular impingement. Arthroscopy. 2012;28(10):1388–1395. [DOI] [PubMed] [Google Scholar]
- 10. Jack RA, Evans DC, Echo A, et al. Performance and return to sport after sports hernia surgery in NFL players. Orthop J Sports Med. 2017;5(4):2325967117699590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jakoi A, O’Neill C, Damsgaard C, Fehring K, Tom J. Sports hernia in National Hockey League players. Am J Sports Med. 2013;41(1):107–110. [DOI] [PubMed] [Google Scholar]
- 12. Joesting DR. Diagnosis and treatment of sportsman’s hernia. Curr Sports Med Rep. 2002;1(2):121–124. [DOI] [PubMed] [Google Scholar]
- 13. Kluin J. Endoscopic evaluation and treatment of groin pain in the athlete. Am J Sports Med. 2004;32(4):944–949. [DOI] [PubMed] [Google Scholar]
- 14. Kumar A, Doran J, Batt ME, Nguyen-Van-Tam JS, Beckingham IJ. Results of inguinal canal repair in athletes with sports hernia. J R Coll Surg Edinb. 2002;47:561–565. [PubMed] [Google Scholar]
- 15. Malycha P, Lovell G. Inguinal surgery in athletes with chronic groin pain: the “sportsman’s” hernia. Aust N Z J Surg. 1992;62(2):123–125. [DOI] [PubMed] [Google Scholar]
- 16. Martin RL, Philippon MJ. Evidence of reliability and responsiveness for the Hip Outcome Score. Arthroscopy. 2008;24(6):676–682. [DOI] [PubMed] [Google Scholar]
- 17. Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes: PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28(1):2–8. [DOI] [PubMed] [Google Scholar]
- 18. Meyers WC, McKechnie A, Philippon MJ, Horner MA, Zoga AC, Devon ON. Experience with “sports hernia” spanning two decades. Ann Surg. 2008;248(4):656–665. [DOI] [PubMed] [Google Scholar]
- 19. Murphy G, Foran P, Murphy D, Tobin O, Moynagh M, Eustace S. “Superior cleft sign” as a marker of rectus abdominus/adductor longus tear in patients with suspected sportsman’s hernia. Skeletal Radiol. 2013;42(6):819–825. [DOI] [PubMed] [Google Scholar]
- 20. Muschaweck U, Berger L. Minimal repair technique of sportsmen’s groin: an innovative open-suture repair to treat chronic inguinal pain. Hernia. 2010;14(1):27–33. [DOI] [PubMed] [Google Scholar]
- 21. Omar IM, Zoga AC, Kavanagh EC, et al. Athletic pubalgia and “sports hernia”: optimal MR imaging technique and findings. Radiographics. 2008;28(5):1415–1438. [DOI] [PubMed] [Google Scholar]
- 22. Orchard J, Read JW, Verrall GM, Slavotinek JP. Pathophysiology of chronic groin pain in the athlete. Int Sports Med J. 2000;1(1):1–16. [Google Scholar]
- 23. Paajanen H, Montgomery A. Surgical treatment of sports hernia: laparoscopic approach In: Diduch DR, Brunt LM, eds. Sports Hernia and Athletic Pubalgia. New York, NY: Springer US; 2014:143–152. [Google Scholar]
- 24. Polglase AL, Frydman GM, Farmer KC. Inguinal surgery for debilitating chronic groin pain in athletes. Med J Aust. 1991;155(10):674–677. [PubMed] [Google Scholar]
- 25. Steele P, Annear P, Grove JR. Surgery for posterior inguinal wall deficiency in athletes. J Sci Med Sport. 2004;7(4):415–421. [DOI] [PubMed] [Google Scholar]
- 26. Van Der Donckt K, Steenbrugge F, Van Den Abbeele K, Verdonk R, Verhelst M. Bassini’s hernial repair and adductor longus tenotomy in the treatment of chronic groin pain in athletes. Acta Orthop Belg. 2003;69(1):35–41. [PubMed] [Google Scholar]
- 27. Ziprin P, Williams P, Foster ME. External oblique aponeurosis nerve entrapment as a cause of groin pain in the athlete. Br J Surg. 1999;86(4):566–568. [DOI] [PubMed] [Google Scholar]



