Abstract
Diffuse reflectance spectroscopy (DRS) has been used in murine studies to quantify tumor perfusion and therapeutic response. These studies frequently use inhaled isoflurane anesthesia, which depresses the respiration rate and results in the desaturation of arterial oxygen saturation, potentially affecting tissue physiological parameters. However, there have been no controlled studies quantifying the effect of isoflurane anesthesia on DRS-derived physiological parameters of murine tissue. The goal of this study was to perform DRS on Balb/c mouse (n = 10) tissue under various anesthesia conditions to quantify effects on tissue physiological parameters, including total hemoglobin concentration, tissue oxygen saturation, oxyhemoglobin and reduced scattering coefficient. Two independent variables were manipulated including metabolic gas type (pure oxygen vs. medical air) and isoflurane concentration (1.5 to 4.0%). The 1.5% isoflurane and 1 L/min oxygen condition most closely mimicked a no-anesthesia condition with oxyhemoglobin concentration within 89% ± 19% of control. The time-dependent effects of isoflurane anesthesia were tested, revealing that anesthetic induction with 4.0% isoflurane can affect DRS-derived physiological parameters up to 20 minutes post-induction. Finally, spectroscopy with and without isoflurane anesthesia was compared for colon tumor Balb/c-CT26 allografts (n = 5) as a representative model of subcutaneous murine tumor allografts. Overall, isoflurane anesthesia yielded experimentally-induced depressed oxyhemoglobin, and this depression was both concentration and time dependent. Investigators should understand the dynamic effects of isoflurane on tissue physiological parameters measured by DRS. These results may guide investigators in eliminating, limiting, or managing anesthesia-induced physiological changes in DRS studies in mouse models.
OCIS codes: (170.2680) Gastrointestinal; (170.3660) Light propagation in tissues; (170.3890) Medical optics instrumentation; (170.6510) Spectroscopy, tissue diagnostics; (170.7050) Turbid media
1. Introduction
Diffuse reflectance spectroscopy (DRS) is a non-invasive method which can be used to quantify volumetric total hemoglobin concentration (THC), tissue oxygen saturation (StO2), and tissue scattering at or within accessible tissue sites [1–10]. This technique has been adapted for studies of tumor perfusion and response to therapy, since THC and StO2 can be used to differentiate therapeutic responders from non-responders over the course of treatment [11–13]. DRS is widely used in murine studies in which subcutaneous or orthotopic tumor models are treated with anti-cancer agents or radiation therapy and tumor perfusion is monitored longitudinally over time [14–18]. For example, Turley et al. used a handheld DRS probe to show that Bevacizumab, an anti-VEGF monoclonal antibody, decreased oxyhemoglobin (THC * StO2) in melanoma tumor xenografts over a 7-day study [14]. Spliethoff et al. used DRS to show that cisplatin, a chemotherapy drug, caused an increase in tumor StO2 in an orthotopic model of mammary tumors over a 7-day study [15]. Finally, Hu et al. used DRS to show that oxygenation kinetics of pharynx squamous cell carcinoma xenografts changed prior to tumor volume changes in response to radiation therapy [16]. These studies indicate that DRS provides clinically relevant, quantitative, and functional information that can be used to monitor tumor response to various types of chemotherapy, radiation therapy, or immunotherapy.
Anesthesia is typically used in murine studies because it reduces the animals’ stress, enables easy manipulation of the mice, allows for injections of cancer cells and anti-cancer agents, and allows for accompanying surgical procedures. Anesthetic agents used in mouse studies can be delivered via inhalational (isoflurane or sevoflurane) or injected (pentobarbital or ketamine/xylazine) routes [19]. According to the American Veterinary Medical Association (AVMA), the Institute for Laboratory Animal Research (ILAR), and the Cornell University Institutional Animal Care and Use Committee (IACUC), the most common and recommended anesthesia technique for mice is inhaled isoflurane, a halogenated anesthetic gas supplemented with either 21% (i.e. room air equivalent) or 100% oxygen (O2) [19–21]. The minimum alveolar concentration (MAC), which is the anesthesia required to prevent movement in response to surgical stimuli in 50% of subjects, is 1.4% for mice under isoflurane anesthesia [19]. Therefore, the most common practice in DRS studies is placing mice in an induction chamber where anesthesia is quickly induced at 3.0-5.0% isoflurane, and then transferred to a nose cone where anesthesia is maintained at 1.5-3.0% isoflurane, with a constant gas flow rate of 1 L/min [14–17, 19, 22–25]. Isoflurane is a respiratory and myocardial depressant, which causes increased partial pressure of carbon dioxide and bicarbonate levels in arterial blood [26, 27]. Thus, even in the presence of O2 delivery via nose cone, isoflurane results in tissue O2 desaturation, which may be a confounding variable when studying tissue perfusion of subcutaneous murine models in response to therapy. Additionally, some therapies, such as chemotherapy or immunotherapy, depend on adequate tissue perfusion and O2 saturation to be effective [28]. DRS can quantify these perfusion metrics and help understand if limitations exist for emerging cancer therapies [29]. However, there have been no studies analyzing the effects of isoflurane anesthesia on DRS-derived physiological parameters of murine tissue.
The present study fills this knowledge gap by monitoring DRS-derived physiological parameters of murine tissue while mice were under various anesthesia conditions. Physiological parameters studied include THC, StO2, tissue oxyhemoglobin (HbO2), and reduced scattering coefficient (μs’). It should be noted that DRS quantifies average StO2 sampled by light, rather than arterial oxygen saturation (SaO2), venous oxygen saturation (SvO2), or peripheral oxygen saturation (SpO2) [30, 31]. StO2 linearly correlates with the average of SaO2 and SvO2; thus, StO2 values are significantly lower than SaO2 [32]. HbO2 is the product of THC and StO2, and describes the concentration of O2-bound hemoglobin in circulation [33, 34]. This study was divided into four aims: 1) examine the effects of isoflurane anesthesia on DRS-derived physiological parameters of normal immunocompetent mouse tissue, 2) determine optimal anesthetic conditions for performing DRS while adhering to AVMA and IACUC standards [19–21], 3) characterize the time-dependent response of physiological parameters while maintaining mice on 1.5% isoflurane after induction with either 1.5% or 4.0% isoflurane, and 4) validate findings in a subcutaneous murine allograft model of colon carcinoma. An allograft model of colon carcinoma was chosen because they are well-established models in literature but are understudied regarding DRS. For the first aim, physiological parameters were quantified after manipulating two variables including metabolic gas type (O2 vs. medical air) and isoflurane concentration (1.5% to 4.0%). For the second aim, optimal anesthetic conditions were determined based on least significant differences between control (no-anesthesia) and experimental groups. For the third aim, mice were anesthetically induced with either 4.0% isoflurane for one minute or 1.5% isoflurane for four minutes. Following induction, mice were transferred to a nose cone and maintained on 1.5% isoflurane for 15 minutes to determine how initial induction conditions affect physiological properties over time. Physiological parameters were monitored via DRS every minute. Finally, for the fourth aim, an allograft model of murine colon carcinoma was used to demonstrate expected changes in DRS-derived tumor physiological parameters during isoflurane anesthesia.
The central hypothesis was that DRS can accurately monitor physiological changes associated with isoflurane anesthesia. Specially, isoflurane anesthesia was expected to yield experimentally-induced low StO2 and HbO2, but insignificant changes in THC and μs’, for both normal and subcutaneous tumor sites. Optimal anesthesia conditions were expected to occur at the lowest tested isoflurane concentration (1.5%) with 100% O2. Furthermore, StO2 and HbO2 were expected to change over time in response to anesthesia. This work aims to guide investigators in eliminating, limiting, or managing anesthesia-induced physiological changes in DRS studies in mouse models.
2. Materials and methods
2.1 Murine models
The study was approved by the University of Arkansas Institutional Animal Care and Use Committee (IACUC #18060). Fifteen female Balb/c mice (strain: 000651, The Jackson Laboratory, ME, USA) aged nine weeks were purchased. Balb/c mice were housed in groups of three in five cages at 23°C ± 1°C and 50% ± 10% humidity on a 12:12 hour light-dark cycle. Food (8640, Teklad) and water was provided ad libitum. All 15 mice acclimated for seven days, including daily handling (2 minutes) for adaptation to future measurements, after arrival prior to the start of the study. After one week of acclimation, left flanks of the 10-week old Balb/c mice were shaved and Nair depilatory was applied for one minute to locally remove fur.
2.2 Cell line for allograft model of colon carcinoma
Five of the 15 Balb/c mice were randomly selected for tumor allotransplantation. CT26 (ATCC, CRL-2638), a colon carcinoma cell line derived from the Balb/c mouse strain, was maintained in Roswell Park Memorial Institute (RPMI)-1640 medium (ATCC, 30-2001) supplemented with 10% fetal bovine serum (ATCC, 30-2020), 1% antibiotic antimycotic solution (Sigma-Aldrich, A5955-100ML), and 0.2% amphotericin B/gentamicin (Thermo Fisher Scientific, R015010) at 37°C and 5% CO2. CT26 cells were brought to the third passage (P3). Then, 1x105 CT26 cells in sterile saline were injected subcutaneously into the left flank. Tumor allografts grew until they reached a volume of 100 mm3, measured via , which took 14.4 ± 2.2 days, upon which tumor underwent DRS measurements. Then, tumor allografts continued to grow until they reached 500 mm3, approximately 18.1 ± 1.2 days following implantation, upon which additional DRS measurements were taken to compare physiological parameters at different tumor sizes in response to isoflurane anesthesia. For controls, adjacent healthy flank tissue was measured.
2.3 Diffuse reflectance spectroscopy instrumentation
The custom, handheld DRS probe (FiberTech Optica, Kitchener, ON, Canada) was used in direct contact with tissue to perform all spectroscopy measurements. The brass probe tip is cylindrical with a diameter of 6.35 mm. The probe includes a 400 μm-core source fiber (FiberTech Optica, SUV400/440PI, 0.22 ± 0.02 NA) which delivers broadband light (450-900 nm) from a 20W tungsten-halogen lamp (Ocean Optics, HL-2000 HP) into tissue, and an adjacent 400-μm core detector fiber (FiberTech Optica, SUV400/440PI, 0.22 ± 0.02 NA) which transfers diffusely reflected light to a spectrometer (Ocean Optics, FLAME-S) with an optical resolution of 2.1 nm. The center-to-center source-detector separation (SDS) between these two optical fibers was 3.00 mm. All DRS measurements were performed in a dark environment.
The four physiological parameters were quantified by inputting raw DRS spectra into an experimental lookup-table (LUT)-based post-processing software with a priori values for oxygenated and deoxygenated hemoglobin extinction coefficients [8, 35, 36]. The software performed an iterative model fit, based on a standard damped least-squares nonlinear fitting method, on raw DRS data to quantify THC, StO2, HbO2, and μs’ [8]. Additionally, the chi-squared (Χ2) value indicated goodness-of-fit between the model fit and raw DRS data; for this study, if Χ2 values exceeded 1.0, data was rejected and re-acquired as this was likely due to user-induced movement artifacts during data collection (i.e. discarding data taken with small air gaps between probe and skin). Finally, the software is based on a fitting range (i.e. boundary conditions) for all four physiological parameters, as shown in Table 1. Lower and upper bounds were set to encompass a wide range of potential physiological parameters in murine skin and tumor tissue [37, 38]. The wavelength range used to fit the data was between 450 to 900 nm.
Table 1. Boundary conditions for quantifying in vivo physiological parameters.
| Physiological parameter | Lower Bound | Upper Bound |
|---|---|---|
| THC | 0 mg/mL | 150 mg/mL |
| StO2 | 0% | 100% |
| HbO2 | 0 mg/mL | 150 mg/mL |
| μs’ (750 nm) | 3 cm−1 | 12 cm−1 |
2.4 Controlling for confounding variables in mouse diffuse reflectance spectroscopy
Positioning of the mice during DRS measurements could potentially affect results by changing venous blood distribution. Therefore, for DRS measurements of mice under isoflurane anesthesia, mice were placed in the prone position. For DRS measurements of non-anesthetized mice, mice sat in the operator’s hand. Thus, the tumor and adjacent healthy skin were identically oriented during measurements in both anesthesia and non-anesthesia cases.
Next, the method of restraining non-anesthetized animals during measurements could affect results by increasing stress leading to altered hemodynamic and tissue blood volume levels [39, 40]. Mice were restrained by holding the base of the tail between index and middle fingers and allowing the mouse to rest in the palm, or, for the anesthesia conditions, in the prone position with a nose cone delivering isoflurane and metabolic gas. Stress was accounted for in two ways. First, all mice were handled daily for 2 minutes during the 7-day acclimation period to allow the mouse to adapt to DRS measurement procedures and provide reproducible results [40]. Additionally, mouse respiration rate was monitored during experiments. During DRS measurements of anesthetized animals, respiration rate was monitored visually by an operator not performing measurements. Safe respiration rate under anesthesia is 55-70 breaths per minute [41]. During DRS measurements of non-anesthetized animals, breath rate was not to exceed 150 breaths per minute (BPM) or a 10% increase from baseline prior to handling [41]. If BPM did not fall within these stress-related criteria, DRS measurements were not taken.
Finally, previous research has shown that absorption due to THC and StO2 decreases with both increasing probe-tissue pressure and time since the probe may physically compress blood out of the tissue site and impede the sampled tissue site from receiving replacement oxygenated blood [42]. Although probe-pressure effects were not directly measured in this study, probe-pressure effects have been shown to be nearly negligible (< 5% error) within a range of probe-skin pressures between 9 to 152 mN/mm2 (1.3 to 22.0 PSI) using a similar 6.35 mm-diameter DRS probe in short (< 2 s) contact durations. Normal probe-skin pressure tends to be less than 9 mN/mm2, and, for our setup, a contact time less than 1 s, justifying the non-use of an integrated pressure sensor [42].
2.5 Effect of isoflurane concentration on physiological tissue parameters
The aim of this experiment was to examine the effect of inhaled isoflurane anesthesia physiological parameters of murine tissue, measured by DRS, and determine optimal anesthetic conditions for DRS.
The normal, exposed left flank of Balb/c mice (n = 10) underwent DRS with varying anesthesia conditions. The control group received no anesthesia. Subsequent groups received isoflurane anesthesia (Henry Schein Animal Health, 1169567762) using a tabletop laboratory animal anesthesia system (VWR, 89012-492). Metabolic gas was varied between pure O2 (100% O2, Airgas, OX USP200) and medical air (21% O2, Airgas, AI USP200), with a constant flow rate of 1 L/min. Isoflurane concentration was varied between 1.5%, 2.0%, 3.0%, and 4.0%. Mice were induced and maintained on the same isoflurane concentration. Concentrations below 1.5% were not tested because such concentrations would be below the MAC value (1.4%) for isoflurane in mice [19]. Isoflurane concentrations above 4.0% were not tested since higher values are usually only used for isoflurane-induced euthanasia according to AVMA [20]. Furthermore, investigators generally do not exceed 4.0% isoflurane during anesthetic induction [14–17, 19, 22–25].
Mice were placed in a 2L induction chamber with an input connected to the isoflurane-gas mix and output connected to a disposable charcoal filter (VWR, 89012-608) housed in an externally ventilating chemical fume hood. Mice were anesthetically induced until they had no pedal reflex (firm toe pinch). Mice were then transferred to a second independent anesthesia circuit consisting of a 9 mm-diameter nose cone with an input connected to the isoflurane-gas mix and output connected to a disposable charcoal filter. To maintain body temperature, mice were placed on a water-based warming pad (Stryker, #TP12E) controlled by a warming pump (Stryker, #TP700) set to 42°C (107°F), as recommended by the Cornell University IACUC [21].
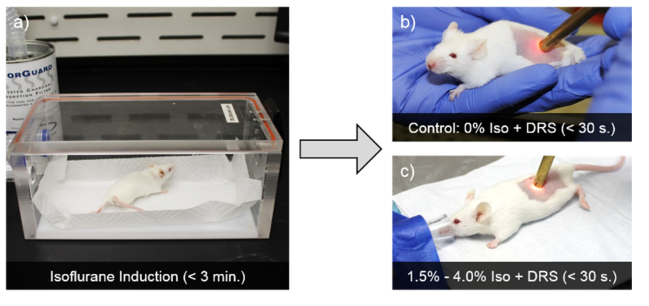
The DRS probe was placed in direct contact with the exposed skin of the left flank. DRS measurements were taken with an integration time of 75 ms, and the probe was in direct contact with skin for less than 1 s to mitigate probe-pressure effects. Ten DRS measurements were averaged over the course of 30 seconds per mouse, with the probe being completely removed from the skin between each data take. Total time under anesthesia was less than 5 minutes in all cases. Paired t-tests were used to compare groups since each mouse was subject to all groups. Figure 1 shows the experimental setup.
Fig. 1.
Balb/c mice in experimental groups underwent isoflurane induction for less than 3 minutes, depending on concentration (1.5%, 2.0%, 3.0%, or 4.0%), using either 1 L/min of 100% or 21% O2 (a). Then, mice underwent less than 30 seconds of 10 consecutive DRS measurements on healthy tissue of the exposed left flank in either control (b), or experimental (1.5%, 2.0%, 3.0%, or 4.0% isoflurane) groups (c). During maintenance, mice were maintained on a warming pad.
2.6 Temporal effects of isoflurane anesthesia on physiological tissue parameters
The aim of this experiment was to characterize the time-dependent physiological parameter response while maintaining the mouse on 1.5% isoflurane after isoflurane induction.
DRS measurements were taken on left flank of conscious mice (n = 10) every minute for five minutes with no isoflurane anesthesia as a baseline. Mice were restrained within the palm of the hand gently holding the tail, held no more than three inches above the work surface.
Then, mice were placed into the 2L induction chamber supplied with either 4.0% isoflurane for one minute or 1.5% isoflurane for four minutes with 1 L/min O2. No DRS measurements occurred during induction. Mice were then transferred to a nose cone and maintained on 1.5% isoflurane and 1 L/min O2 for 15 minutes, with DRS measurements taken every minute. A maximum of 15 minutes was chosen since it takes approximately 10-15 minutes for mice to fully respond to a change in isoflurane concentration [41]. Therefore, to control for intergroup and intragroup variation, DRS measurements must occur only after the mouse has presumably fully responded to such change. Throughout DRS measurements under anesthesia, mice were maintained on a water-based warming pad (Stryker, #TP12E) controlled by a warming pump (Stryker, #TP700) set to 42°C (107°F).
Following 15 minutes of isoflurane maintenance, mice were removed from anesthesia and DRS measurements were taken every minute for 5 minutes. DRS measurements were taken with an integration time of 75 ms. Figure 2 visualizes the experimental set-up.
Fig. 2.
Conscious Balb/c mice underwent DRS for 5 minutes. Then, mice were anesthetically induced for 1 or 4 minutes with 4.0% or 1.5% isoflurane (Iso), respectively, and 1 L/min O2. Following induction, mice were transferred to a nose cone and underwent DRS for 15 minutes at 1.5% isoflurane and 1 L/min O2. Finally, mice were removed from the nose cone and the left flank underwent DRS for 5 minutes.
For each mouse, physiological parameters (THC, StO2, HbO2, and μs’) were normalized to the highest value over the 25-minute data acquisition period. Then, normalized values of all mice were averaged as a function of time. Both normalized and non-normalized data are presented.
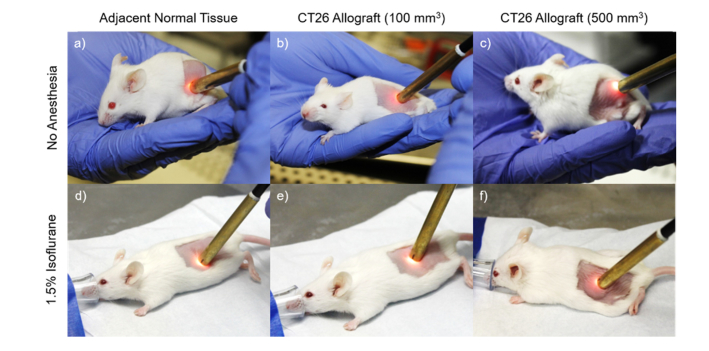
2.7 Physiological parameters of CT26 colon carcinoma allografts
A second cohort of Balb/c mice (n = 5) with CT26 murine colon carcinoma allografts underwent DRS as a representative model of subcutaneous tumor allografts. Measurements with (1.5% isoflurane and 1 L/min O2) and without anesthesia were performed on allografts at volumes of 100 mm3 and 500 mm3 and an immediately adjacent normal site. Mice were placed in the 2L induction chamber (1.5% isoflurane and 1 L/min O2) until loss of pedal reflex and transferred to the nose cone. Ten DRS measurements were averaged per site at an integration time of 75 ms per spectra to minimize motion artifacts. Figure 3 visualizes the experimental set-up.
Fig. 3.
DRS was performed on Balb/c mouse (10 weeks old) to quantify physiological parameters (THC, StO2, HbO2, and μs’) in subcutaneous CT26 tumor allografts at a volume of 100 mm3 (b, e), 500 mm3 (c, f), and adjacent normal tissue (a, d) both with (d, e, f) and without isoflurane anesthesia (a, b, c). Anesthesia was constant at 1.5% isoflurane and 1 L/min O2.
3. Results
3.1 Effect of isoflurane concentration on physiological tissue parameters
The left flank of Balb/c mice (n = 10) underwent DRS measurements while varying isoflurane concentration between 0.0% (control, no anesthesia) and 4.0%, and varying metabolic gas between 21% O2 and 100% O2.
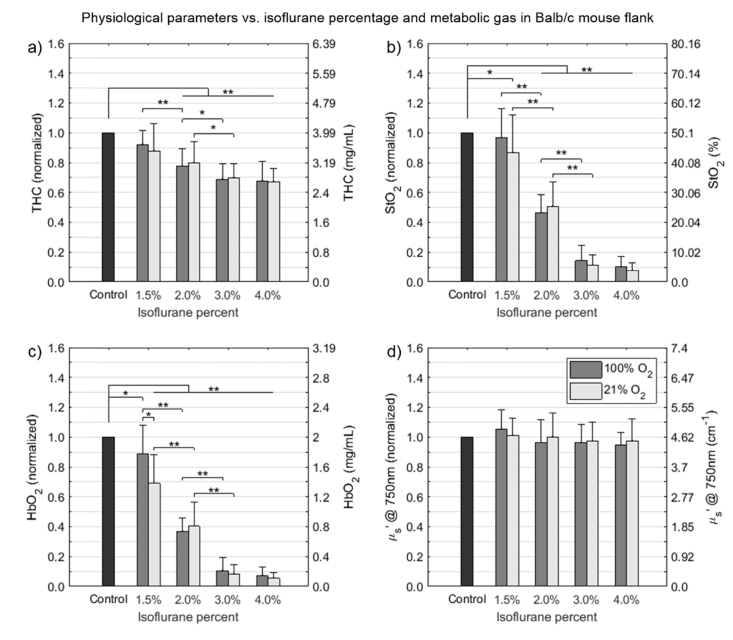
For THC (Fig. 4(a)), there were no significant differences between using O2 or air. However, there was a significant decrease in THC compared to control as isoflurane exceeds 2.0% (p < 0.01). At 4.0% isoflurane, THC dropped to 68% (p < 0.01) and 67% (p < 0.01) compared to the control in O2 and air, respectively.
Fig. 4.
Physiological parameters of THC (a), StO2 (b), HbO2 (c), and μs’ (d) of the normal left flank of Balb/c mice (n = 10) was compared for isoflurane concentration (1.5% to 4.0%) and either 100% O2 (dark gray) or 21% O2 (light gray). THC (a) and StO2 (b) were only affected by isoflurane concentration. HbO2 (c) was affected by both isoflurane concentration and metabolic gas. Finally, μs’ (d) was unaffected by increases in isoflurane concentration and metabolic gas. Even at low isoflurane concentrations (1.5%), physiological parameters were affected. Based on these results, O2 is the preferred metabolic gas over air, and 1.5% isoflurane is most appropriate when applicable. Control indicates measurements from non-anesthetized mice. Values are means ± SD. Significance is indicated by *(p<0.05) and ** (p<0.01).
For StO2 (Fig. 4(b)), there were no significant differences between using O2 or air, although average values for StO2 tended to be higher when using O2. Unlike THC, StO2 decreases rapidly, even at the minimum 1.5% isoflurane. For example, at 1.5% isoflurane with air, StO2 decreased to 87% (p = 0.028) compared to the control. StO2 continued to decrease within both O2 and air groups (p < 0.01) up to 3.0% isoflurane. Then, between 3.0% and 4.0% isoflurane, StO2 stabilized to ~8-15% compared to the control.
For HbO2 (Fig. 4(c)), despite there being no significant differences between using O2 or air for THC and StO2, there was a significant difference in HbO2 between using O2 and air at 1.5% isoflurane (p = 0.04), suggesting that O2 is the preferred metabolic gas compared to air with regards to DRS-derived physiological parameters. Most notably, there were significant differences between using 1.5% isoflurane and the control for both O2 (88%, p = 0.043) and air (69%, p < 0.01) groups. This finding suggests that even at the lowest isoflurane concentration (1.5%) above the MAC value (1.4%) for mice, DRS-derived HbO2 values were affected.
For μs’ (Fig. 4(d)), there were no significant differences between using O2 or air. Additionally, μs’ was unaffected by changes in isoflurane concentration. These findings suggest that all anesthesia conditions affect at least one of the tested physiological parameters. However, 1.5% isoflurane and 1 L/min O2 most closely mimicked ideal no-anesthesia conditions.
3.2 Temporal effects of isoflurane anesthesia on physiological tissue parameters
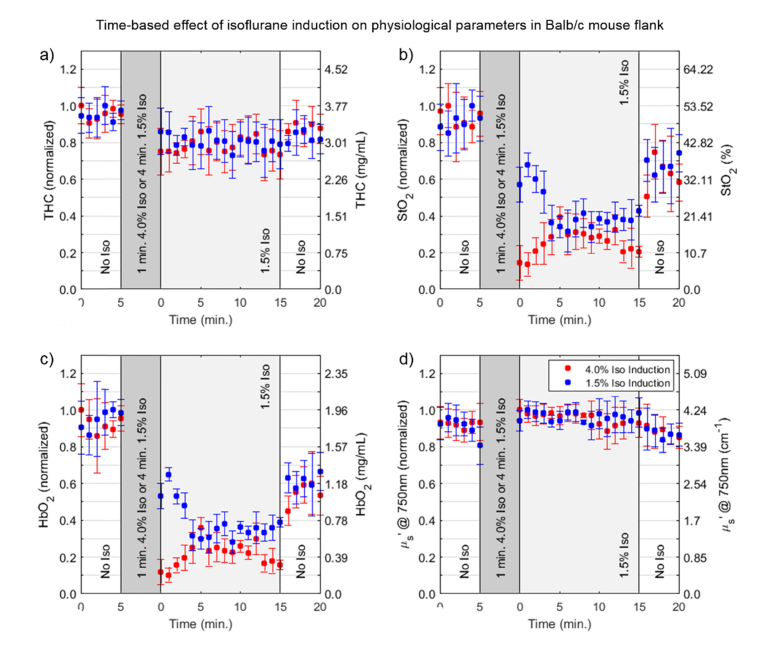
DRS measurements were taken on Balb/c mice (n = 10) every minute for five minutes with no isoflurane anesthesia as a baseline. During these five minutes, all physiological parameters remained stable. After one or four minutes with 4.0% or 1.5% isoflurane, respectively, and 1 L/min O2, mice were transferred to a nose cone with 1.5% isoflurane and 1 L/min O2.
For both 4.0% and 1.5% isoflurane induction condition, THC (Fig. 5(a)) decreased from approximately 3.7 mg/mL to 2.8-3.2 mg/mL and remained relatively stable throughout the 15-minute duration. During the 5-minute recovery period, THC showed a slight rise to approximately 3.4 mg/mL. For StO2, on the other hand (Fig. 5(b)), the induction period resulted in a decrease from approximately 50% to 31% and 7% for the 1.5% and 4.0% isoflurane induction conditions, respectively. For the 4.0% isoflurane condition, StO2 increased over time during the maintenance period, but not dramatically, having reached a final value of just 11% at the end of 15 minutes. On the other hand, for the 1.5% isoflurane condition, StO2 continued to decrease to 51% for 6 months, then rose back to 22% at the end of 15 minutes, indicating that, as expected, physiological changes occur more slowly in mice anesthetized with 1.5% isoflurane. Similarly, HbO2 (Fig. 5(c)), as anticipated, demonstrated similar trends to StO2.
Fig. 5.
Temporal effects of 1.5% and 4.0% isoflurane anesthesia induction on physiological parameters of THC (a), StO2 (b), HbO2 (c), and μs’ (d) of the normal left flank of Balb/c mice (n = 10). The μs’ (d) was unaffected by induction, maintenance, and recovery periods. Other physiological parameters all showed an initial decrease after induction, with a slight increase by the end of the 15-minute maintenance period, but not back to baseline values. Based on these results, it is clear than any isoflurane induction concentration influences DRS-derived physiological parameters. Values are means ± SD.
Finally, μs’ (Fig. 4(d)) was unaffected by isoflurane anesthesia. Following maintenance with 1.5% isoflurane and 1 L/min O2, mice were removed from isoflurane for a “recovery” period and DRS data was collected for an additional five minutes. Mice generally regained consciousness within one minute and full movement within two minutes, after which mice were gently restrained in the palm of the hand with the tail held secure between index and middle finger no more than three inches above the work surface. THC, StO2, and HbO2 increased within the five minutes; however, none reached 100% of the baseline values within the five-minute recovery period. On the other hand, μs’ remained constant during the 5 minutes of recovery.
From these experiments, physiological parameters were affected by anesthetic induction with both 1.5% and 4.0% isoflurane. It cannot be assumed, once 1.5% isoflurane maintenance begins, that physiological parameters are representative. THC, StO2, and HbO2 did not recover to the baseline values by the end of 15 minutes, nor did these physiological parameters fully recover after the five-minute recovery period.
3.3 Physiological parameters of CT26 colon carcinoma allografts
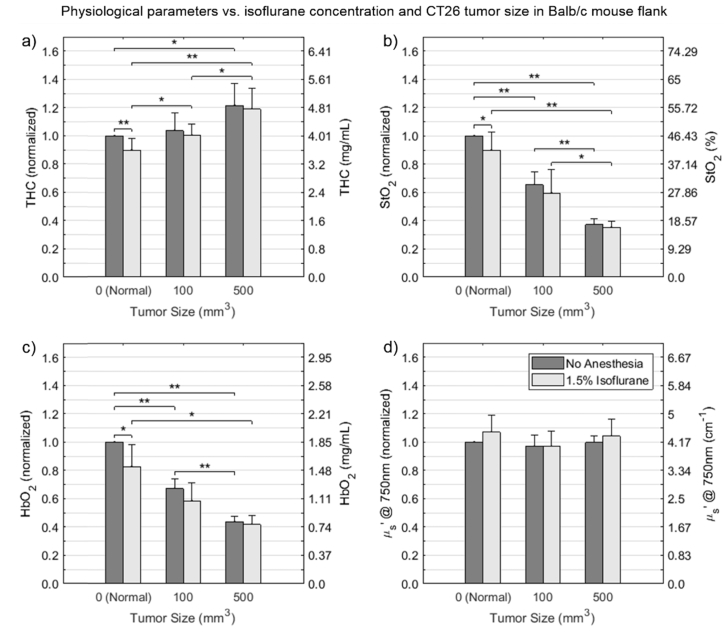
Colon carcinoma murine CT26 allografts in Balb/c mice at volumes of 100 mm3 and 500 mm3 were compared with adjacent normal tissue with (1.5% isoflurane and 1 L/min O2) and without isoflurane anesthesia to quantify physiological parameters (Fig. 6). All mice were induced with 1.5% isoflurane for four minutes to avoid the effects of 4.0% isoflurane seen in Fig. 4.
Fig. 6.
Comparison of the physiological parameters, THC, StO2, HbO2, and μs’ of subcutaneous CT26 tumor allografts and adjacent normal tissue both with (light gray) and without (dark gray) isoflurane anesthesia. Similar to previous findings, THC, StO2, and HbO2 were reduced when comparing the no-anesthesia and 1.5% isoflurane conditions in adjacent normal tissue. Results demonstrate that isoflurane anesthesia causes experimentally-reduced HbO2 values, and that StO2 and HbO2 decreased with increasing allograft tumor volumes, whereas THC increased and μs’ remained constant. Values are means ± SD. Significance is indicated by *(p<0.05) and ** (p<0.01).
For adjacent tissue locations (no tumor), there was significant reduction in physiological parameters for the anesthesia condition compared to the no anesthesia condition for THC (p < 0.01), StO2 (p = 0.04), and HbO2 (p = 0.02). However, overall trends within the anesthesia and no anesthesia groups were similar, with insignificant reductions in physiological parameters when using 1.5% isoflurane and 1 L/min O2. Additionally, as tumor size increased, StO2 and HbO2 decreased while THC increased and μs’ remained constant. Further comparisons across and within groups were visually expressed in Fig. 6.
4. Discussion
Isoflurane anesthesia is a known respiratory and myocardial depressant, causing increased serum carbon dioxide and bicarbonate levels, and decreased arterial pressure. Despite this, isoflurane is commonly applied as an anesthetic agent in studies investigating volumetric perfusion of murine tissue, which is the aim of many DRS-based studies. To better understand the effects of isoflurane anesthesia on DRS-derived physiological parameters, the present study monitored murine THC, StO2, HbO2, and μs’ using DRS under various anesthesia conditions. Understanding the effects of isoflurane anesthesia on these tissue physiological parameters will help guide investigators in DRS experimental design.
In this study, increasing isoflurane concentration significantly decreased THC, StO2, and HbO2 while having no effect on µs’ (Figs. 4-6). Of all four DRS-derived physiological parameters, StO2 was most influenced by changes in isoflurane concentration. Furthermore, using 100% O2, rather than 21% O2, resulted in closer approximation to no-anesthesia controls (Fig. 4), a trend echoed by Gerling et al. who showed that supplying 100% O2 led to increased StO2 [43]. Because of this, 100% O2 was used throughout the remainder of the study.
In Fig. 4(b), StO2 did not decrease (50% to 48%, p = 0.32) when comparing the no-anesthesia control to the 1.5% isoflurane condition. However, StO2 drastically decreased from 48% to 6% when increasing isoflurane from 1.5% to 4.0% in normal tissue. StO2 values of ~6% have been observed in similar spectroscopy studies of mice tissue during anesthesia [15]. StO2 linearly correlates with the average of SaO2 and SvO2; thus, StO2 values are significantly lower than SaO2 [32], which can be measured via pulse oximetry [44]. Decreased StO2 is primarily caused by isoflurane-induced decreased mean arterial blood pressure (MAP) [45]. Szczesny et al. measured MAP of mice under increasing isoflurane concentrations, and showed that MAP decreased from 80 mmHg to below 40 mmHg as isoflurane concentration was increased from 1.0% to 4.0% [46]. Constantinides et al. echoed this trend, showing that MAP decreased from 85 mmHg to 73 mmHg when increasing isoflurane concentration from 1.0% to 2.0% with 100% O2. Additionally, this research showed that MAP decreased from 92 mmHg to 84 mmHg when decreasing O2 from 100% to 21% with 1.5% isoflurane [47].
To our knowledge, no other studies report StO2 (as low as 6% in Fig. 4(b)) at high (4.0%) concentrations of isoflurane, since many studies state they DRS acquisition during isoflurane maintenance of 1.5%. However, this statement paints an incomplete picture. This report is important because the most common anesthetic practice in DRS studies is placing mice in an induction chamber where anesthesia is induced at ~4.0% isoflurane [19]. This isoflurane concentration can have long-lasting effects on blood physiology, even when mice are transferred to a nose cone where isoflurane is maintained at 1.5% (Fig. 5). Therefore, we show that isoflurane induction, not just maintenance, highly affects DRS-derived StO2 (Fig. 5). We recommend 1.5% isoflurane with 100% O2 for both induction and maintenance, despite increased time to loss of pedal reflex.
Of note are conflicting results from a study by Farzam et al. In this study, mice were anesthetized and maintained on 3.5% and 2.0% isoflurane, respectively, and StO2 values were ~75% in orthotopic renal cell carcinoma tumors [48], a stark increase from our StO2 of 22% at 2.0% isoflurane (Fig. 4(b)). However, this study analyzed an orthotopic, rather than subcutaneous, tumor model of a different cell line. In a more comparable study, Rajaram et al. reported StO2 values near 30% under similar isoflurane conditions (1.5%) and wavelength ranges (350 to 850 nm) of murine skin at a comparable SDS (2.5 mm) [49]. The wavelength range used to fit data and SDS are paramount when comparing between studies.
Unlike hemodynamic physiological parameters, the µs’ was unaffected by changes in isoflurane concentration and O2 levels. Tissue scattering is primarily caused by local density of lipid membranes from cellular tissues, mitochondria, lysosomes, and collagenous tissue like the skin [50], which was the primary tissue type interrogated in this experiment. These scattering structures are unaffected by isoflurane conditions, resulting in stable µs’.
Based on these results, isoflurane anesthesia should be carefully considered when performing DRS studies to quantify THC, StO2, and HbO2; however, some invasive and minimally invasive studies cannot eliminate the anesthesia use. For example, Spliethoff et al. used a 21G optical needle probe to perform deep intratumoral DRS measurements to overcome sampling depth limitations with mice under anesthesia [15]. Westerkamp et al. performed postmortem DRS on liver tissue following hepatectomy [51]. Finally, Palmer et al. performed DRS on 4T1 mammary tumor allografts while concurrently measuring the partial pressure of O2 using an OxyLite sensor, which required anesthesia [18]. Thus, it is not always applicable to perform live DRS with no anesthesia; 100% O2 with minimal isoflurane (1.5%) is recommended in these cases. Using a minimum of 1.5% isoflurane for induction over a four-minute period also drastically decreased StO2 and HbO2, although changes were slower to occur compared to 4.0% isoflurane induction (Fig. 5). If anesthesia is needed when measuring in vivo physiological parameters via DRS, it may be more representative to slowly induce anesthesia with 1.5% isoflurane rather than rapidly inducing anesthesia with 4.0% isoflurane and lowering concentration for anesthesia maintenance.
Finally, THC, StO2, HbO2, and μs’ of Balb/c-CT26 colon tumor were measured via DRS. Figure 6a indicates that increased tumor volume correlates to increased THC. Across Figs. 4-6, we report THC of 2.8 to 4.0 mg/mL in normal tissue and 4.0 to 4.8 mg/mL in subcutaneous CT26 tumor allografts under 1.5% isoflurane anesthesia, comparable to a study by Spliethoff et al [15] in similar conditions. Increased tumor THC is due to increased tumor microvasculature coupled with increased ratio of deoxyhemoglobin to oxyhemoglobin. This trend of increased tumor THC is well known [52, 53]. Figure 6b shows that StO2 of tumors with volumes of 500 mm3 was ~14%, both with and without 1.5% isoflurane. This low StO2 value is similar to a study by Spliethoff et al., which reported slightly lower StO2 values of 2-6% in larger mammary xenograft tumors (up to 800 mm3) using 1.5% isoflurane anesthesia [15]. Rich et al. reported similar StO2 values of 5-15% in head and neck cancer xenograft tumors, measured using photoacoustic imaging [54]. Finally, Rajaram et al. reported DRS-derived StO2 around 20% for mammary xenografts at 1.5% isoflurane anesthesia [49]. The Rajaram study also reported a ~1.5x decrease in StO2 of 100 mm3 mammary tumor xenografts compared to normal tissue, whereas this present study reports a ~1.6x decrease (Fig. 6(b)) in StO2 of 100 mm3 colon tumor allografts compared to normal tissue. The comparable StO2 values in these studies lend support to our results. HbO2 in Fig. 6(c) demonstrates similar trends as StO2. In Fig. 6(d), µs’ was unaffected by tumor size and isoflurane, similar to Figs. 4 and 5.
Additionally, in tumors, there were insignificant decreases in THC, StO2, and HbO2 when using 1.5% isoflurane compared to a no-anesthesia control, suggesting it may be appropriate to monitor percent changes in physiological parameters over time. In longitudinal treatment studies, accompanying non-endpoint procedures such as chemotherapy, radiation therapy, immunotherapy, or other treatment or observation procedures requiring anesthesia should ideally be performed after DRS measurements have concluded.
One limitation of this study is the focus on non-invasive DRS of readily accessible murine tissue, such as skin and subcutaneous tumor allografts, which only requires contact between the probe and skin directly overlying the tumor. Additionally, DRS was the only technique used to quantify THC, StO2, HbO2, and μs’ and cannot provide insights into tumor vascular heterogeneity [8, 55–57]. Other optical techniques exist to quantify these parameters including diffuse optical imaging (DOI) [55], hyperspectral imaging [58], and near infrared spectroscopy (NIRS), which extends the wavelength range of DRS into the near infrared to quantify additional endogenous chromophores such as fat and water [15, 59–61]. For example, DOI combined with magnetic resonance imaging can differentiate tumors with low and high vascular heterogeneity, and hyperspectral imaging can quantify vascular O2 supply and blood flow in rodent models. These spectral and imaging techniques would benefit from an in-depth analysis at how anesthetic drugs affect results. Next, DRS-derived physiological parameters were only quantified in response to isoflurane anesthesia. Despite being the most common type of anesthetic used in DRS-based mouse studies, other anesthesia drugs exist including sevoflurane, Pentobarbital, and ketamine/xylazine [19]. Finally, further tests with additional cell lines for murine subcutaneous allografts or xenografts will generalize results. An allograft model of colon carcinoma (Balb/c-CT26) was chosen because they are well-established models in literature but are understudied regarding DRS. Results compare well with other allograft/xenograft tumors in terms of physiological parameters (THC, StO2, HbO2, and μs’).
The findings presented here suggest that DRS is a valid tool to dynamically monitor changes in physiological parameters. These findings indicate that DRS has the potential to help investigators understand if limitations exist for certain cancer therapies that directly depend on tumor O2 consumption and help guide investigators in managing anesthesia-induced physiological changes in DRS studies of murine subcutaneous tumor allografts. Future studies analyzing DRS-derived physiological parameters in response to these drugs will increase the generalization of our findings.
Conclusion
Diffuse reflectance spectroscopy can be effectively used to monitor dynamic fluctuations in tissue physiological parameters, such as total hemoglobin concentration, tissue oxygen saturation, oxyhemoglobin, and tissue scattering, and is an attractive tool for monitoring tumor response to therapy. Additionally, diffuse reflectance spectroscopy has the potential to help investigators understand if limitations exist for certain cancer therapies, such as chemotherapy or PDT, that directly depend on oxygen consumption and well-perfused tumors. Investigators using this tool should understand the dynamic effects of isoflurane concentration on resulting physiologic values. We show that isoflurane induction, not just maintenance, highly affect hemodynamic parameters. Alternative methods to diffuse reflectance spectroscopy, such as pulse oximetry, should be considered when monitoring arterial, rather than tissue, oxygen saturation, during anesthesia.
Acknowledgements
We thank the entire team of the Translational Biophotonics and Imaging Laboratory for continued constructive support for this study and Dr. Narasimhan Rajaram for guidance in the spectroscopy setup and data post-processing.
Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the acknowledged funding agencies.
Funding
National Institutes of Health (1R15CA202662-01); National Science Foundation Graduate Research Fellowship Program (G.G., DGE-1450079); the Arkansas Biosciences Institute; the University of Arkansas Doctoral Academy Fellowship.
Disclosures
The authors declare that there are no conflicts of interest related to this article.
References and links
- 1.Rajaram N., Aramil T. J., Lee K., Reichenberg J. S., Nguyen T. H., Tunnell J. W., “Design and validation of a clinical instrument for spectral diagnosis of cutaneous malignancy,” Appl. Opt. 49(2), 142–152 (2010). 10.1364/AO.49.000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glennie D. L., Hayward J. E., Farrell T. J., “Modeling changes in the hemoglobin concentration of skin with total diffuse reflectance spectroscopy,” J. Biomed. Opt. 20(3), 035002 (2015). 10.1117/1.JBO.20.3.035002 [DOI] [PubMed] [Google Scholar]
- 3.Yu B., Shah A., Nagarajan V. K., Ferris D. G., “Diffuse reflectance spectroscopy of epithelial tissue with a smart fiber-optic probe,” Biomed. Opt. Express 5(3), 675–689 (2014). 10.1364/BOE.5.000675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glennie D. L., Hayward J. E., McKee D. E., Farrell T. J., “Inexpensive diffuse reflectance spectroscopy system for measuring changes in tissue optical properties,” J. Biomed. Opt. 19(10), 105005 (2014). 10.1117/1.JBO.19.10.105005 [DOI] [PubMed] [Google Scholar]
- 5.Chin L. C. L., Cook E. K., Yohan D., Kim A., Niu C., Wilson B. C., Liu S. K., “Early biomarker for radiation-induced wounds: day one post-irradiation assessment using hemoglobin concentration measured from diffuse optical reflectance spectroscopy,” Biomed. Opt. Express 8(3), 1682–1688 (2017). 10.1364/BOE.8.001682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fong C. J., Garzon M. C., Hoi J. W., Kim H. K., Lauren C. T., Morel K., Geller L., Antonov N., Weitz N., Wu J., Hielscher A. H., “Assessment of infantile hemangiomas using a handheld wireless diffuse optical spectroscopic device,” Pediatr. Dermatol. 34(4), 386–391 (2017). 10.1111/pde.13150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Greening G. J., James H. M., Muldoon T. J., Optical Phantoms: Diffuse and Sub-diffuse Imaging and Spectroscopy Validation (SPIE Spotlights, 2015). [Google Scholar]
- 8.Greening G. J., James H. M., Dierks M. K., Vongkittiargorn N., Osterholm S. M., Rajaram N., Muldoon T. J., “Towards monitoring dysplastic progression in the oral cavity using a hybrid fiber-bundle imaging and spectroscopy probe,” Sci. Rep. 6(1), 26734 (2016). 10.1038/srep26734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hennessy R., Goth W., Sharma M., Markey M. K., Tunnell J. W., “Effect of probe geometry and optical properties on the sampling depth for diffuse reflectance spectroscopy,” J. Biomed. Opt. 19(10), 107002 (2014). 10.1117/1.JBO.19.10.107002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karsten A. E., Singh A., Karsten P. A., Braun M. W., “Diffuse reflectance spectroscopy as a tool to measure the absorption coefficient in skin: South African skin phototypes,” Photochem. Photobiol. 89(1), 227–233 (2013). 10.1111/j.1751-1097.2012.01220.x [DOI] [PubMed] [Google Scholar]
- 11.Yu Y. H., Zhu X., Mo Q., G., andCui Y., “Prediction of neoadjuvant chemotherapy response using diffuse optical spectroscopy in breast cancer,” Clin. Transl. Oncol. 20, 524–533(2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thong P., Lee K., Toh H. J., Dong J., Tee C. S., Low K. P., Chang P. H., Bhuvaneswari R., Tan N. C., Soo K. C., “Early assessment of tumor response to photodynamic therapy using combined diffuse optical and diffuse correlation spectroscopy to predict treatment outcome,” Oncotarget 8(12), 19902–19913 (2017). 10.18632/oncotarget.15720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schaafsma B. E., van de Giessen M., Charehbili A., Smit V. T., Kroep J. R., Lelieveldt B. P., Liefers G. J., Chan A., Löwik C. W., Dijkstra J., van de Velde C. J., Wasser M. N., Vahrmeijer A. L., “Optical mammography using diffuse optical spectroscopy for monitoring tumor response to neoadjuvant chemotherapy in women with locally advanced breast cancer,” Clin. Cancer Res. 21(3), 577–584 (2015). 10.1158/1078-0432.CCR-14-0736 [DOI] [PubMed] [Google Scholar]
- 14.Turley R. S., Fontanella A. N., Padussis J. C., Toshimitsu H., Tokuhisa Y., Cho E. H., Hanna G., Beasley G. M., Augustine C. K., Dewhirst M. W., Tyler D. S., “Bevacizumab-induced alterations in vascular permeability and drug delivery: a novel approach to augment regional chemotherapy for in-transit melanoma,” Clin. Cancer Res. 18(12), 3328–3339 (2012). 10.1158/1078-0432.CCR-11-3000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spliethoff J. W., Evers D. J., Jaspers J. E., Hendriks B. H., Rottenberg S., Ruers T. J. M., “Monitoring of tumor response to Cisplatin using optical spectroscopy,” Transl. Oncol. 7(2), 230–239 (2014). 10.1016/j.tranon.2014.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu F., Vishwanath K., Salama J. K., Erkanli A., Peterson B., Oleson J. R., Lee W. T., Brizel D. M., Ramanujam N., Dewhirst M. W., “Oxygen and perfusion kinetics in response to fractionated radiation therapy in FaDu head and neck cancer xenografts are related to treatment outcome,” Int. J. Radiat. Oncol. Biol. Phys. 96(2), 462–469 (2016). 10.1016/j.ijrobp.2016.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vishwanath K., Klein D., Chang K., Schroeder T., Dewhirst M. W., Ramanujam N., “Quantitative optical spectroscopy can identify long-term local tumor control in irradiated murine head and neck xenografts,” J. Biomed. Opt. 14(5), 054051 (2009). 10.1117/1.3251013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palmer G. M., Viola R. J., Schroeder T., Yarmolenko P. S., Dewhirst M. W., Ramanujam N., “Quantitative diffuse reflectance and fluorescence spectroscopy: tool to monitor tumor physiology in vivo,” J. Biomed. Opt. 14(2), 024010 (2009). 10.1117/1.3103586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gargiulo S., Greco A., Gramanzini M., Esposito S., Affuso A., Brunetti A., Vesce G., “Mice anesthesia, analgesia, and care, Part I: anesthetic considerations in preclinical research,” ILAR J. 53, 55(2012). [DOI] [PubMed] [Google Scholar]
- 20. Leary S., Underwood W., Anthony R., Cartner S., Corey D., Grandin T., Greenacre C., Gwaltney-Brant S., McCrackin M. A., Meyer R., Miller D., Shearer J., Yanong R., Golab G. C., Patterson-Kane E., “AVMA Guidelines for the Euthanasia of Animals: 2013 Edition,” A. V. M. Association , ed. (American Veterinary Medical Association, Schaumburg, IL 60173, 2013). [Google Scholar]
- 21. Bliss S., “Rodent Anesthesia (Animal Care and Use Procedure 101.02)” (Cornell University Institutional Animal Care and Use Committee, 2017), retrieved 2017, https://ras.research.cornell.edu/care/documents/ACUPs/ACUP101.pdf. [Google Scholar]
- 22.Leung H. M., Gmitro A. F., “Fluorescence and reflectance spectral imaging system for a murine mammary window chamber model,” Biomed. Opt. Express 6(8), 2887–2894 (2015). 10.1364/BOE.6.002887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang H. W., Putt M. E., Emanuele M. J., Shin D. B., Glatstein E., Yodh A. G., Busch T. M., “Treatment-induced changes in tumor oxygenation predict photodynamic therapy outcome,” Cancer Res. 64(20), 7553–7561 (2004). 10.1158/0008-5472.CAN-03-3632 [DOI] [PubMed] [Google Scholar]
- 24.Vishwanath K., Yuan H., Barry W. T., Dewhirst M. W., Ramanujam N., “Using optical spectroscopy to longitudinally monitor physiological changes within solid tumors,” Neoplasia 11(9), 889–900 (2009). 10.1593/neo.09580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yu G., Durduran T., Zhou C., Wang H. W., Putt M. E., Saunders H. M., Sehgal C. M., Glatstein E., Yodh A. G., Busch T. M., “Noninvasive monitoring of murine tumor blood flow during and after photodynamic therapy provides early assessment of therapeutic efficacy,” Clin. Cancer Res. 11(9), 3543–3552 (2005). 10.1158/1078-0432.CCR-04-2582 [DOI] [PubMed] [Google Scholar]
- 26.Cesarovic N., Nicholls F., Rettich A., Kronen P., Hässig M., Jirkof P., Arras M., “Isoflurane and sevoflurane provide equally effective anaesthesia in laboratory mice,” Lab. Anim. 44(4), 329–336 (2010). 10.1258/la.2010.009085 [DOI] [PubMed] [Google Scholar]
- 27.Thal S. C., Plesnila N., “Non-invasive intraoperative monitoring of blood pressure and arterial pCO2 during surgical anesthesia in mice,” J. Neurosci. Methods 159(2), 261–267 (2007). 10.1016/j.jneumeth.2006.07.016 [DOI] [PubMed] [Google Scholar]
- 28.Ueda S., Roblyer D., Cerussi A., Durkin A., Leproux A., Santoro Y., Xu S., O’Sullivan T. D., Hsiang D., Mehta R., Butler J., Tromberg B. J., “Baseline tumor oxygen saturation correlates with a pathologic complete response in breast cancer patients undergoing neoadjuvant chemotherapy,” Cancer Res. 72(17), 4318–4328 (2012). 10.1158/0008-5472.CAN-12-0056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang Y., Goel S., Duda D. G., Fukumura D., Jain R. K., “Vascular normalization as an emerging strategy to enhance cancer immunotherapy,” Cancer Res. 73(10), 2943–2948 (2013). 10.1158/0008-5472.CAN-12-4354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teng Y., Ding H., Huang L., Li Y., Shan Q., Ye D., Ding H., Chien J., Hwang B., “Non-invasive measurement and validation of tissue oxygen saturation covered with overlying tissues,” ScienceDirect 18, 1083–1088 (2008). [Google Scholar]
- 31.Sircan-Kucuksayan A., Uyuklu M., Canpolat M., “Diffuse reflectance spectroscopy for the measurement of tissue oxygen saturation,” Physiol. Meas. 36(12), 2461–2469 (2015). 10.1088/0967-3334/36/12/2461 [DOI] [PubMed] [Google Scholar]
- 32.Hueber D. M., Franceschini M. A., Ma H. Y., Zhang Q., Ballesteros J. R., Fantini S., Wallace D., Ntziachristos V., Chance B., “Non-invasive and quantitative near-infrared haemoglobin spectrometry in the piglet brain during hypoxic stress, using a frequency-domain multidistance instrument,” Phys. Med. Biol. 46(1), 41–62 (2001). 10.1088/0031-9155/46/1/304 [DOI] [PubMed] [Google Scholar]
- 33.Chung S. H., Cerussi A. E., Merritt S. I., Ruth J., Tromberg B. J., “Non-invasive tissue temperature measurements based on quantitative diffuse optical spectroscopy (DOS) of water,” Phys. Med. Biol. 55(13), 3753–3765 (2010). 10.1088/0031-9155/55/13/012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee J., Cerussi A. E., Saltzman D., Waddington T., Tromberg B. J., Brenner M., “Hemoglobin measurement patterns during noninvasive diffuse optical spectroscopy monitoring of hypovolemic shock and fluid replacement,” J. Biomed. Opt. 12(2), 024001 (2007). 10.1117/1.2715189 [DOI] [PubMed] [Google Scholar]
- 35. Prahl S., “Optical Absorption of Hemoglobin” (Oregon Medical Laser Center, 2015), retrieved http://omlc.org/spectra/hemoglobin/. [Google Scholar]
- 36.Greening G. J., James H. M., Powless A. J., Hutcheson J. A., Dierks M. K., Rajaram N., Muldoon T. J., “Fiber-bundle microendoscopy with sub-diffuse reflectance spectroscopy and intensity mapping for multimodal optical biopsy of stratified epithelium,” Biomed. Opt. Express 6(12), 4934–4950 (2015). 10.1364/BOE.6.004934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sabino C. P., Deana A. M., Yoshimura T. M., da Silva D. F. T., França C. M., Hamblin M. R., Ribeiro M. S., “The optical properties of mouse skin in the visible and near infrared spectral regions,” J. Photochem. Photobiol. B 160, 72–78 (2016). 10.1016/j.jphotobiol.2016.03.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Prahl S. A., “Optical Absorption of Hemoglobin” (1999), retrieved January 1, 2016, http://omlc.org/spectra/hemoglobin/.
- 39.Sikora M., Konopelski P., Pham K., Wyczalkowska-Tomasik A., Ufnal M., “Repeated restraint stress produces acute and chronic changes in hemodynamic parameters in rats,” Stress 19(6), 621–629 (2016). 10.1080/10253890.2016.1244667 [DOI] [PubMed] [Google Scholar]
- 40.Zhao X., Ho D., Gao S., Hong C., Vatner D. E., Vatner S. F., “Arterial pressure monitoring in mice,” Curr. Protoc. Mouse Biol. 1, 105–122 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ewald A. J., Werb Z., Egeblad M., “Monitoring of vital signs for long-term survival of mice under anesthesia,” Cold Spring Harb. Protoc. 2011(2), t5563 (2011). 10.1101/pdb.prot5563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lim L., Nichols B., Rajaram N., Tunnell J. W., “Probe pressure effects on human skin diffuse reflectance and fluorescence spectroscopy measurements,” J. Biomed. Opt. 16(1), 011012 (2011). 10.1117/1.3525288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gerling M., Zhao Y., Nania S., Norberg K. J., Verbeke C. S., Englert B., Kuiper R. V., Bergström A., Hassan M., Neesse A., Löhr J. M., Heuchel R. L., “Real-time assessment of tissue hypoxia in vivo with combined photoacoustics and high-frequency ultrasound,” Theranostics 4(6), 604–613 (2014). 10.7150/thno.7996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Al-Samir S., Goossens D., Cartron J. P., Nielsen S., Scherbarth F., Steinlechner S., Gros G., Endeward V., “Maximal oxygen consumption is reduced in aquaporin-1 knockout mice,” Front. Physiol. 7, 347 (2016). 10.3389/fphys.2016.00347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oshita S., Uchimoto R., Oka H., Saka Y., Takeshita H., Funatsu N., “Correlation between arterial blood pressure and oxygenation in tetralogy of Fallot,” J. Cardiothorac. Anesth. 3(5), 597–600 (1989). 10.1016/0888-6296(89)90159-2 [DOI] [PubMed] [Google Scholar]
- 46.Szczesny G., Veihelmann A., Massberg S., Nolte D., Messmer K., “Long-term anaesthesia using inhalatory isoflurane in different strains of mice-the haemodynamic effects,” Lab. Anim. 38(1), 64–69 (2004). 10.1258/00236770460734416 [DOI] [PubMed] [Google Scholar]
- 47.Constantinides C., Mean R., Janssen B. J., “Effects of isoflurane anesthesia on the cardiovascular function of the C57BL/6 mouse,” ILAR J. 52, 21 (2012). [PMC free article] [PubMed] [Google Scholar]
- 48.Farzam P., Johansson J., Mireles M., Jiménez-Valerio G., Martínez-Lozano M., Choe R., Casanovas O., Durduran T., “Pre-clinical longitudinal monitoring of hemodynamic response to anti-vascular chemotherapy by hybrid diffuse optics,” Biomed. Opt. Express 8(5), 2563–2582 (2017). 10.1364/BOE.8.002563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rajaram N., Reesor A. F., Mulvey C. S., Frees A. E., Ramanujam N., “Non-invasive, simultaneous quantification of vascular oxygenation and glucose uptake in tissue,” PLoS One 10(1), e0117132 (2015). 10.1371/journal.pone.0117132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jacques S. L., “Optical properties of biological tissues: a review,” Phys. Med. Biol. 58(11), R37–R61 (2013). 10.1088/0031-9155/58/11/R37 [DOI] [PubMed] [Google Scholar]
- 51.Westerkamp A. C., Pully V. V., Karimian G., Bomfati F., Veldhuis Z. J., Wiersema-Buist J., Hendriks B. H., Lisman T., Porte R. J., “Diffuse reflectance spectroscopy accurately quantifies various degrees of liver steatosis in murine models of fatty liver disease,” J. Transl. Med. 13(1), 309 (2015). 10.1186/s12967-015-0671-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brown J. Q., Wilke L. G., Geradts J., Kennedy S. A., Palmer G. M., Ramanujam N., “Quantitative optical spectroscopy: A robust tool for direct measurement of breast cancer vascular oxygenation and total hemoglobin content in vivo,” Cancer Res. 69(7), 2919–2926 (2009). 10.1158/0008-5472.CAN-08-3370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang H. W., Jiang J. K., Lin C. H., Lin J. K., Huang G. J., Yu J. S., “Diffuse reflectance spectroscopy detects increased hemoglobin concentration and decreased oxygenation during colon carcinogenesis from normal to malignant tumors,” Opt. Express 17(4), 2805–2817 (2009). 10.1364/OE.17.002805 [DOI] [PubMed] [Google Scholar]
- 54.Rich L. J., Seshadri M., “Photoacoustic monitoring of tumor and normal tissue response to radiation,” Sci. Rep. 6(1), 21237 (2016). 10.1038/srep21237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kwong T. C., Hsing M., Lin Y., Thayer D., Unlu M. B., Su M. Y., Gulsen G., “Differentiation of tumor vasculature heterogeneity levels in small animals based on total hemoglobin concentration using magnetic resonance-guided diffuse optical tomography in vivo,” Appl. Opt. 55(21), 5479–5487 (2016). 10.1364/AO.55.005479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Valdés P. A., Roberts D. W., Lu F. K., Golby A., “Optical technologies for intraoperative neurosurgical guidance,” Neurosurg. Focus 40(3), E8 (2016). 10.3171/2015.12.FOCUS15550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mourant J. R., Marina O. C., Hebert T. M., Kaur G., Smith H. O., “Hemoglobin parameters from diffuse reflectance data,” J. Biomed. Opt. 19, 37004 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hendargo H. C., Zhao Y., Allenby T., Palmer G. M., “Snap-shot multispectral imaging of vascular dynamics in a mouse window-chamber model,” Opt. Lett. 40(14), 3292–3295 (2015). 10.1364/OL.40.003292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kawaguchi F., Kawaguchi A. T., Murayama C., Kamijo A., Haida M., “Liposome-encapsulated hemoglobin improves tumor oxygenation as detected by near-infrared spectroscopy in colon carcinoma in mice,” Artif. Organs 41(4), 327–335 (2017). 10.1111/aor.12825 [DOI] [PubMed] [Google Scholar]
- 60.Chen H., Lin Z., Mo L., Wu T., Tan C., “Near-infrared spectroscopy as a diagnostic tool for distinguishing between normal and malignant colorectal tissues,” BioMed Res. Int. 2015, 472197 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kondepati V. R., Heise H. M., Backhaus J., “Recent applications of near-infrared spectroscopy in cancer diagnosis and therapy,” Anal. Bioanal. Chem. 390(1), 125–139 (2008). 10.1007/s00216-007-1651-y [DOI] [PubMed] [Google Scholar]