Abstract
Background:
There is growing evidence supporting the use of mobile health apps for the management of diabetes. Given the disproportionate impact of diabetes on Latinos, especially those with limited English proficiency (LEP) and low literacy, diabetes apps have the potential to address existing health disparities. Our study aimed to understand the current accessibility of diabetes apps for these populations.
Methods:
We searched the Android and iOS stores for the term “diabetes” to identify patient-facing diabetes apps. We reviewed the app store descriptions and user interfaces for Spanish availability. We assessed the readability of the descriptions in English and Spanish using the Lexile Analyzer and the Flesch-Kincaid Reading Grade Level.
Results:
Overall, in reviewing both app stores, 30% (28/92) of apps had descriptions available in Spanish, of which 41% (18/44) of Android apps were available in Spanish and 21% (10/48) iOS apps were available in Spanish. In addition, the readability of 94% (90/96) for the app store descriptions was above the recommended reading level for patient education material in English and Spanish. The overall kappa coefficient for app translation quality assessment was .72, reflecting moderate interrater agreement.
Conclusions:
Despite the evidence supporting the use of diabetes apps, they do not cater to the language needs of LEP Latino patients.
Keywords: health disparities, mobile health, health literacy, diabetes mellitus, digital divide, limited English proficiency
Diabetes disproportionately affects Latinos in the United States, with a prevalence and incidence of 17% and 12.8%, respectively, compared with 10% and 7.6% among non-Hispanic whites.1,2 The disparities in care experienced by Latinos have been linked to worse health outcomes.3 Latinos experience worse glycemic control and a higher rate of diabetes-related complications, including end stage renal disease, lower extremity amputations, and death.1,4 Diabetes-related mobile health apps may be effective tools to improve health outcomes and reduce disparities. However, disparities in care among Latinos may be in part due to limited English proficiency (LEP), limited literacy, and cultural barriers.5-8 Of Latinos, 32% speak English “less than very well.”9 To engage Latinos with chronic disease, diabetes apps must account for these limitations in English proficiency and health literacy.
Engaging patients in self-care is essential to addressing these barriers. Two reviews, one commissioned by the Institute of Medicine and the other by the Robert Wood Johnson Foundation, found that patients’ self-management of their chronic diseases and the promotion of patient engagement are associated with improved quality of life, functional autonomy, and decreased hospital use.10,11 Mobile health apps present a novel method of engaging patients in self-care and are particularly relevant for Latinos, who are among the most likely to own a smartphone and rely on it for Internet access.12-14 Of Latinos, 86% are interested in using health apps, 31% already use mobile health apps, and 34% are interested in using an app for diabetes management, according to an observational study.15
In 2015, there were more than 259 000 health apps and this number is growing.16 Of the 9% of apps that are disease specific, diabetes-related apps were the second most common.17 A growing body of literature suggests the potential of diabetes apps to impact health outcomes. A meta-analysis and systematic review of 22 and 13 trials, respectively, of mobile phone-based diabetes interventions demonstrated statistically significant improvements in glycemic control and self-management in diabetes care.18,19
Despite the interest in diabetes apps and evidence supporting their efficacy, little is known of their current state for Latino populations. A study looking at the top 20 diabetes apps found that 20% of iOS and 50% of Android apps were available in Spanish.20 They also found that app prices ranged from free to $10, with an average price of $5.03. However, this study sampled a small number of apps and did not focus on the readability or quality of Spanish translation, which are key factors that may influence the accessibility and uptake of apps by Latinos.
Addressing low health literacy is especially relevant for patient-focused tools.21 In the United States, the average person reads at an 8th grade reading level, while Medicare beneficiaries read at a 5th grade reading level.22,23 Furthermore, Overland et al found that among patients with diabetes randomized to read educational materials of different reading levels, 60% of the patients assigned to read 6th grade-level information understood it independently, whereas only 21% of patients who read the 9th grade-level information understood it.24 In fact, the Joint Commission recommends that patient educational materials should be at or below a 5th grade reading level.25
Given the prevalence of LEP Latinos, the importance of literacy to health, and the potential of mobile health apps, understanding whether diabetes apps are accessible to them is a critical question. In this study, we sought to determine how many diabetes apps are available in Spanish and to assess their readability based on both text complexity and quality of translation.
Methods
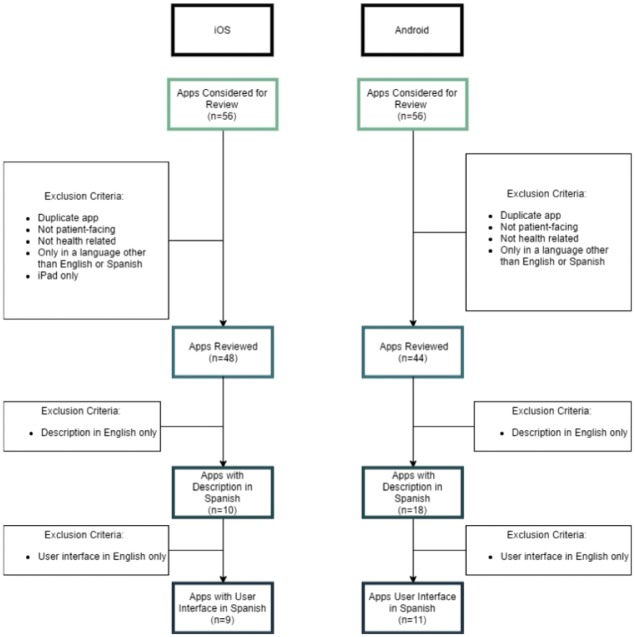
We performed a search for the term “diabetes” in both the United States Google Play and the iOS App Store. To capture apps available in English and Spanish, we changed the language settings in the app stores and the testing devices to Spanish. The search was performed on May 31, 2016. The app reviews occurred from June to July 2016. We considered the top 56 apps presented by the search algorithm for each app store. We purposefully sampled 56 apps because they reflected apps most likely to be in active use. Apps were excluded if they were: not health related, near duplicates, available on the iPad only, not patient-facing, aimed at providers (such as reference apps), or available only in a language other than Spanish or English (Figure 1).
Figure 1.
Evaluation of diabetes mobile apps.
We downloaded each app onto an iPad running iOS 9.3.5 or a Nexus 5 running Android 6.0.1. Though we used the iPad as our testing device, we only considered iPhone apps (which can run on iPads) since we wanted to assess only apps accessible on smartphones. We reviewed information from the app store or app website to record the following app characteristics: platform, developer, cost, downloads (only available for Android), user rating, and number of user ratings.
To determine language availability, we designated an app as available in Spanish based on the language of the app description when the language setting of the device and app store was set to Spanish. For the iOS App Store, we reviewed whether Spanish was listed under the available languages. If the description was available in Spanish or Spanish was listed as an available language, we downloaded the app to confirm the language of the app interface or if the app itself had a language setting that included Spanish, resulting in a change of the interface language.
We measured the readability of the app store description in both English and Spanish. We used the app descriptions as proxy for the app text, since the app text itself was not formatted appropriately for the readability metrics (i.e., use of incomplete sentences and phrases). Only complete sentences of the app store descriptions were used to fit the readability scales requirements. For English readability, we used the online Lexile Analyzer and the Flesch-Kincaid Reading Grade Level.26 For Spanish, we used the online Lexile Analyzer.27
For apps with Spanish descriptions available, two native Spanish speakers evaluated the translation quality using a Likert-type scale. The scale used 3 tiers:
Low quality: many grammatical errors and incorrect translations leading to difficulty in comprehension
Moderate quality: some grammatical errors, but still comprehensible
High quality: no grammatical errors and comprehensible
Results
General Characteristics
We identified and reviewed 44 Android apps and 48 iOS apps meeting the inclusion and exclusion criteria. Most of the selected apps in both Android and iOS stores were free. The largest plurality of Android app downloads was between 10 000 and 50 000. The median number of user ratings for iOS apps was 719 and the median for Android apps was 179 user ratings. The apps in both stores were generally well-rated with mean user ratings of 4.2 and 4.1 out of 5 for Android and iOS apps, respectively (Table 1).
Table 1.
Characteristics of 28 Spanish Available Diabetes Apps, 2016.
| iOS | Android | |
|---|---|---|
| Spanish availabilitya | ||
| Description in Spanish | 10 (21%) | 18 (41%) |
| App interface in Spanish | 9 (19%) | 11 (25%) |
| Store ratingsb | ||
| No rating | 0 (0) | 0 (0) |
| 0-1 | 0 (0) | 0 (0) |
| >1-2 | 0 (0) | 0 (0) |
| >2-3 | 0 (0) | 1 (4%) |
| >3-4 | 5 (18%) | 3 (11%) |
| >4-5 | 5 (18%) | 14 (50%) |
| Median number of ratings (range) | 534 (49-13 514) | 244.5 (7-10 117) |
| Number of downloads (Android only)c | ||
| 100-500 | 1 (6%) | |
| 500-1000 | 0 (0) | |
| 1000-5000 | 1 (6%) | |
| 5000-10 000 | 3 (17%) | |
| 10 000-50 000 | 5 (28%) | |
| 50 000-100 000 | 4 (22%) | |
| 100 000-500 000 | 3 (17%) | |
| 500 000-1 000 000 | 1 (6%) | |
| 1 000 000-5 000 000 | 0 (0) | |
| Costd | ||
| Free | 9 (90%) | 17 (94%) |
| $1.99 | 1 (10%) | |
| $3.13 | 1 (6%) | |
Percentage based on total number of apps reviewed for each platform.
Percentage based on total number of apps available in Spanish.
Percentage based on total number of apps available in Spanish on Android.
Percentage based on total number of apps available in Spanish on each platform.
For apps available in Spanish on the Android store, most were free except for one app, which cost $3.13. Similarly, on the iOS store, most Spanish apps were free, except for one app which cost $1.99. User ratings were both 4.2. Most Android apps were downloaded 10 000 to 50 000 times. The median number of ratings on the Android store was 245 and 534 on the iOS store.
Language Availability and Readability
Overall, across both app stores, 30% (28/92) of apps had descriptions available in Spanish. Based on app descriptions, 41% (18/44) of Android apps were available in Spanish and 21% (10/48) iOS apps were available in Spanish. Once downloaded, 25% (11/44) of Android apps and 19% (9/48) of iOS apps had actual interfaces in Spanish (Table 1).
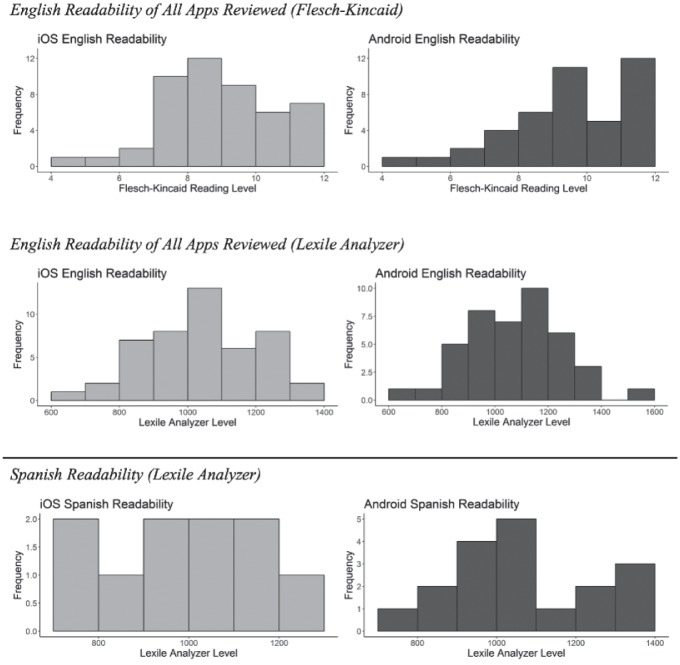
In English, the description in both stores had a 9th grade reading level based the Flesch-Kincaid Reading Level. Similarly, the Lexile measure was equivalent to an English readability grade between 7th-10th grade for the Android store and 6th-9th grade on the iOS store. In Spanish, the average Lexile measure was 970L on the iOS store. On the Android store, the average Spanish Lexile measure was 1070L (Figure 2).
Figure 2.
English and Spanish readability of diabetes apps.
For Android apps, rater 1 found 56% (10/18) had high quality translation, 28% (5/18) had moderate quality translation and 17% (3/18) had low quality translation. Rater 2 found 77% (14/18) had high quality translation and the rest of the apps were of moderate quality. Among iOS apps, rater 1 found all translations to be of high quality, whereas rater 2 found all but one translation to be of high quality. The kappa coefficient for app translation quality assessment was 0.72, reflecting moderate interrater agreement.
Discussion
In our study, we found that the majority of diabetes apps on the Android and iOS stores were not available in Spanish and were written at a complex reading level. Compared to previous studies looking at app availability in Spanish, our study found a lower availability than reported. Schroeder et al reviewed 20 diabetes apps and reported an overall Spanish availability of 35% (7/20), 50% (5/10) on the Android store and 20% (2/10) on the iOS store. Our broader review of diabetes apps found that 41% (18/44) of Android apps and 21% (10/48) of iOS apps appeared to be available in Spanish based on the app store description. However, only 25% (11/44) of Android apps and 19% (9/48) of iOS actually had user interfaces in Spanish. Given this discrepancy, app developers should translate content beyond app descriptions and ensure translated interfaces. Ultimately, our results reveal a discrepancy between the gaps in care for LEP Latino diabetes patients and the current linguistic accessibility of diabetes apps. Previous studies have identified the development of language and health literacy as important factors for personalizing technology-based interventions.28 Moreover, linguistic appropriateness and cultural tailoring have been identified as factors contributing to the quality and safety of health information technology among LEP patients.5 These guidelines have yet to make a significant impact on the development of diabetes apps.
To our knowledge, this is the first paper looking at the readability of app store descriptions as a metric of technology access for low literacy patients. Based on Joint Commission guidelines, the recommended English reading level for health content is 5th grade or below (Lexile measure: 830L-1010L).23 However, our study found the readability of 94% (90/96) app store description to be above the 5th grade a reading level in English, and complex in Spanish as well. Nationally, 35% or 77 million US adults are considered to have low health literacy, with even higher rates among the elderly and minorities, including Latinos.21 For patients with diabetes, low health literacy is common.29 Furthermore, given the importance of health literacy, the development of new technology tools must account for these differences to be accessible and engage patients. Previous studies looking at online content have shown that all English content and 86% of Spanish online health information required high school level or greater reading ability.30 This persists in the mobile arena based on the findings of our study. This may propagate a new digital divide, which no longer relates to access to technology, but rather relates to a lack of content for LEP and low literacy populations.
We specifically chose Spanish as our primary language since it is the second most common language in the United States after English. Translation is only the first step for tailoring technology interventions for Spanish-speaking patients. Observing Spanish-speaking patients using these apps would provide insight into their ability to gain purported the benefits. Though readability scales provide information on text complexity, they do not provide information on cultural appropriateness and cannot supplant the direct testing of patient comprehension. However, they provide guidance for content development. The use of app descriptions as proxies and translation assessment with a nonvalidated Likert-type scale are additional limitations.
Conclusions
Given the prevalence of LEP Latino diabetes patients and their poor health outcomes, our study reveals an unmet opportunity for health apps to engage them in their care.
Acknowledgments
The authors would like to thank Dr Juan Henao for his support in reviewing app descriptions.
Footnotes
Abbreviation: LEP, limited English proficiency.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr. Jorge A. Rodriguez received support from a career development award from the Office of Diversity, Inclusion and Career Advancement at Beth Israel Deaconess Medical Center.
ORCID iD: Jorge A. Rodriguez  http://orcid.org/0000-0003-4990-3713.
http://orcid.org/0000-0003-4990-3713.
References
- 1. Schneiderman N, Llabre M, Cowie CC, et al. Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care. 2014;37(8):2233-2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. American Diabetes Association. Statistics about diabetes. 2017. Available at: http://www.diabetes.org/diabetes-basics/statistics/. Accessed March 21, 2017.
- 3. Agency for Healthcare Research and Quality. 2013 National Healthcare Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality; January 2013. [Google Scholar]
- 4. US Department of Health & Human Services Office of Minority Health. Diabetes and Hispanic Americans. 2016. Available at: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlID=63. Accessed March 21, 2017.
- 5. López L, Green AR, Tan-McGrory A, King R, Betancourt JR. Bridging the digital divide in health care: the role of health information technology in addressing racial and ethnic disparities. Jt Comm J Qual Patient Saf. 2011;37(10):437-445. [DOI] [PubMed] [Google Scholar]
- 6. Jacobs EA, Agger-Gupta N, Chen AH, Piotrowski A, Hardt EJ. Language Barriers in Health Care Settings: An Annotated Bibliography of the Research Literature. Woodland Hills, CA: California Endowment; 2003. Available at: www.calendow.org. [Google Scholar]
- 7. Fernandez A, Schillinger D, Warton EM, et al. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: The Diabetes Study of Northern California (DISTANCE). J Gen Intern Med. 2011;26(2):170-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475-482. [DOI] [PubMed] [Google Scholar]
- 9. US Census Bureau. Language Spoken at Home by Ability to Speak English for the Population 5 Years and over (Hispanic or Latino). Universe: Hispanic or Latino population 5 years and over more information 2011-2015. American Community Survey 5-Year Estimates; Available at: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_5YR_B16006&prodType=table. Accessed July 28, 2017. [Google Scholar]
- 10. Bodenheimer T, Berry-Millett R. Care management of patients with complex health care needs. Synth Proj Res Synth Rep. 2009;(19):pii:52372. [PubMed] [Google Scholar]
- 11. James J. Health Policy Brief: Patient Engagement. Health Affairs. 2013: 1-5. doi: 10.1377/hpb2013.4. [DOI] [Google Scholar]
- 12. Singh K, Drouin K, Newmark LP, et al. Many mobile health apps target high-need, high-cost populations, but gaps remain. Health Aff (Millwood). 2016;35(12):2310-2318. [DOI] [PubMed] [Google Scholar]
- 13. Singh K, Drouin K, Newmark LP, et al. Patient-facing mobile apps to treat high-need, high-cost populations: a scoping review. JMIR Mhealth Uhealth. 2016;4(4):e136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Brown BYA, López G, Lopez MH. Digital Divide Narrows for Latinos as More Spanish Speakers and Immigrants Go Online. Washington, DC: Pew Research Center; 2016. [Google Scholar]
- 15. Ramirez V, Johnson E, Gonzalez C, et al. Assessing the use of mobile health technology by patients: an observational study in primary care clinics. JMIR Mhealth Uhealth. 2016;4(2):e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. mHealth App Developer Economics 2015: The Current Status and Trends of the mHealth App Market. 2015. Available at: https://research2guidance.com/product/mhealth-developer-economics-2015/
- 17. Patient Adoption of mHealth. Available at: http://www.imshealth.com/en/thought-leadership/quintilesims-institute/reports/patient-adoption-of-mhealth. Accessed March 21, 2017.
- 18. Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med. 2011;28(4):455-463. [DOI] [PubMed] [Google Scholar]
- 19. Bonoto BC, de Araújo VE, Godói IP, et al. efficacy of mobile apps to support the care of patients with diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth. 2017;5(3):e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Williams JP, Schroeder D. Popular glucose tracking apps and use of mHealth by Latinos with diabetes: review. JMIR Mhealth Uhealth. 2015;3(3):e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Office of Disease Prevention and Health Promotion. America’s Health Literacy: Why We Need Accessible Health Information. An Issue Brief From the US Department of Health and Human Services; 2008. Available at: https://health.gov/communication/literacy/issuebrief/. Accessed March 21, 2017. [Google Scholar]
- 22. Doak CC, Doak LG, Root JH. Assessing suitability of materials. In: Doak CC, Doak LG, Root JH, eds. Teaching Patients with Low Literacy Skills. 2nd ed. Philadelphia, PA: J.B. Lippincott; 1996:41-60. [Google Scholar]
- 23. Stossel LM, Segar N, Gliatto P, Fallar R, Karani R. Readability of patient education materials available at the point of care. J Gen Intern Med. 2012;27(9):1165-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Overland JE, Hoskins PL, McGill MJ, Yue DK. Low literacy: a problem in diabetes education. Diabet Med. 1993;10(9):847-850. [DOI] [PubMed] [Google Scholar]
- 25. The Joint Commission: A Roadmap for Hospitals Advancing Effective Communication, Cultural Competence, and Patient-and Family-Centered Care Quality Safety Equity Project Staff Project Advisors. Oakbrook Terrace, IL: 2010. [cited 2017 Apr 11]; (1-102). Available from: http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727pdf. [Google Scholar]
- 26. Lexile® Analyzer. The Lexile® Framework for Reading. Available at: https://lexile.com/analyzer/. Accessed April 10, 2017.
- 27. Find a Book. MetaMetrics Inc. Available at: https://fab.lexile.com/. Accessed July 10, 2017.
- 28. Lopez L, Tan-Mcgrory A, Horner G, Betancourt JR. Eliminating disparities among Latinos with type 2 diabetes: effective eHealth strategies. J Diabetes Complications. 2016;30(3):554-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cavanaugh K, Huizinga MM, Wallston KA, et al. Association of numeracy and diabetes control. Ann Intern Med. 2008;148(10):737-746. [DOI] [PubMed] [Google Scholar]
- 30. Berland GK, Elliott MN, Morales LS, et al. Health information on the internet: accessibility, quality, and readability in English and Spanish. JAMA. 200l;285(20):2612-2621. [DOI] [PMC free article] [PubMed] [Google Scholar]