Abstract
Background:
The number of systematic reviews and meta-analyses published on the rotator cuff (RC) has increased markedly.
Purpose:
To quantify the number of systematic reviews and meta-analyses published on the RC and to provide a qualitative summary of the literature.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic search for all systematic reviews and meta-analyses pertaining to the RC published between January 2007 and September 2017 was performed with PubMed, MEDLINE, and the Cochrane Database of Systematic Reviews. Narrative reviews and non–English language articles were excluded.
Results:
A total of 1078 articles were found, of which 196 met the inclusion criteria. Included articles were summarized and divided into 15 topics: anatomy and function, histology and genetics, diagnosis, epidemiology, athletes, nonoperative versus operative treatment, surgical repair methods, concomitant conditions and surgical procedures, RC tears after total shoulder arthroplasty, biological augmentation, postoperative rehabilitation, outcomes and complications, patient-reported outcome measures, cost-effectiveness of RC repair, and quality of randomized controlled trials.
Conclusion:
A qualitative summary of the systematic reviews and meta-analyses published on the RC can provide surgeons with a single source of the most current literature.
Keywords: rotator cuff, repair, systematic review, meta-analysis
There has been an upsurge in the number of systematic reviews and meta-analyses pertaining to the rotator cuff (RC) over the past decade. These articles are published with the intent of providing busy surgeons with the most current information on a single condition by synthesizing all the available evidence with rigorous methods. However, with the steady increase in these types of studies, it can be difficult for providers to even stay up to date with this literature. A basic PubMed search for RC repair returned 430 articles in 2016 alone. To aid researchers and providers as they strive to remain current on this topic, we sought to quantify the number of systematic reviews and meta-analyses published on the RC in the past decade and provide a summary of this literature for easy reference.
Methods
A literature search was performed to identify all RC-related systematic reviews and meta-analyses published in English between January 2007 and September 2017. The search engines used were PubMed, Medline, and the Cochrane Database of Systematic Reviews. The search terms included RC, supraspinatus, infraspinatus, or subscapularis in combination with systematic review or meta-analysis. All systematic reviews and meta-analyses that examined research topics pertaining to the RC were included (eg, anatomy, epidemiology, diagnosis, treatment). Exclusion criteria were narrative reviews that did not report a systematic literature search, studies that did not separate RC tears from other RC pathology, and studies that pooled data pertaining to RC injuries with those of other orthopaedic injuries. Four authors (J.J., J.M., T.M., M.A.K.) independently reviewed the results of the literature search and compared their findings. Three authors (J.J., J.M., T.M.) reviewed each study in detail and summarized the study results. The articles were divided into 15 topics: anatomy and function, histology and genetics, diagnosis, epidemiology, athletes, nonoperative versus operative treatment, surgical repair methods, concomitant conditions and surgical procedures, RC tears after total shoulder arthroplasty, biological augmentation, postoperative rehabilitation, outcomes and complications, patient-reported outcome (PRO) measures, cost-effectiveness of RC repair, and quality of randomized controlled trials. A few articles were categorized under more than 1 topic because they examined multiple study aims (<5% of included papers).
Results
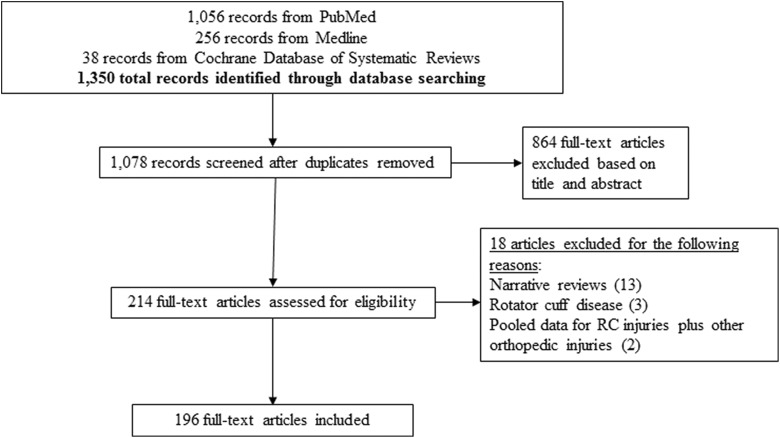
Figure 1 presents the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart. A total of 1078 articles were identified by the literature search, of which 196 met the inclusion criteria. The number of articles included for each RC topic are presented in Table 1.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart. RC, rotator cuff.
TABLE 1.
Number of Articles by Rotator Cuff Topica
| Topic of Systematic Review | Articles Found, n |
|---|---|
| Anatomy and function | 5 |
| Histology and genetics | 4 |
| Diagnosis | 19 |
| Epidemiology | 8 |
| Rotator cuff tears in athletes | 5 |
| Nonoperative vs operative treatment | 14 |
| Surgical repair methods | 43 |
| Concomitant conditions and surgical procedures | 9 |
| Rotator cuff tears after total shoulder arthroplasty | 2 |
| Biological augmentation | 29 |
| Postoperative rehabilitation | 21 |
| Outcomes assessment | 37 |
| Patient-reported outcome measures and their psychometric properties | 6 |
| Cost-effectiveness of rotator cuff repair | 1 |
| Quality of randomized controlled trials | 2 |
aTopics are not mutually exclusive.
Anatomy and Function
Sangwan et al195 systematically reviewed 20 studies that examined the function of RC muscles as dynamic stabilizers of the glenohumeral joint. Several studies indicated that RC muscles can inhibit joint translation, contribute to joint stiffness, have shorter moment arms for some movements, and activate prior to global muscles on electromyography with respect to certain shoulder movements. In a systematic review, Edouard et al46 indicated that the most reliable position for internal rotation (IR) and external rotation (ER) strength assessment was to be seated with 45º of shoulder abduction in the scapular plane. Berckmans et al16 systematically reviewed 14 studies that examined isokinetic RC strength assessment among healthy overhead athletes and concluded that greater IR force resulted in lower functional deceleration ratio (ER/IR) on the dominant side as compared with the nondominant side. In their systematic review of studies that examined electromyography activity of the shoulder muscles, Spall et al215 ascertained that RC tears were associated with longer duration of muscle activity in the upper trapezius during glenohumeral movements and greater fatigability of the anterior and middle deltoid during isometric hand gripping and overhead lifting. The activation ratio of only the latissimus dorsi was decreased for the RC tear group versus the control group (mean difference = –1.31; 95% CI, –2.36 to –0.25; P = .02), which suggests greater co-contraction of the latissimus dorsi during isometric abduction. Abe et al2 cited good reliability and validity for measuring muscle thickness on ultrasound (US) in the supraspinatus, biceps, and triceps when compared with cross-sectional area on magnetic resonance imaging (MRI) as well as manual measurement on cadavers. This suggests that muscle thickness may be predictive of muscle function.
Histology and Genetics
Dean et al38 systematically reviewed 101 studies that examined cellular and molecular changes in RC disease, as well as the pathogenesis of RC disease (Tables 2 and 3). To summarize, degenerative RC disease demonstrated histologic features consistent with inflammation and tendon healing. The progressive formation of collagen fibers, mainly types II and III, are associated with loss of the normal tendon structure and myxoid degeneration. Proinflammatory cytokines accelerate remodeling, amplify biomechanical adaptivity, and promote tenocyte apoptosis, which subsequently creates an imbalance between the catabolic and anabolic systems. In the catabolic state, there is a decrease in tissue inhibitors of metalloproteinases (TIMPs), resulting in higher levels of metalloproteinase, a matrix-remodeling protein. Furthermore, TIMPs may play a role in the degradation of proinflammatory cytokines, and their relative decrease may contribute to the local inflammatory state. As the total collagen content decreases, smaller and more disorganized fibrils form. The increase in tenascin-C and fibronectin is consistent with the wound-healing process.
TABLE 2.
Changes to the Extracellular Matrix Components and Enzymes in Rotator Cuff Diseasea
| Matrix Components | Matrix Enzymes |
|---|---|
| Type I collagen ↑116
Type II collagen ↑57,161 Type III collagen ↑10,87,100,116,180,182 ↑ (RCT vs non-RCT82) Type X collagen ↑161 Type I collagen α1 ↓8 ↑ (ftRCT vs ptRCT209) Type I collagen α2 ↓6,85 Type II collagen α1 ↑6,8,85 Type III collagen α1 ↑8,231 ↓6 Type VI collagen ↑7 α1 ↑8 Collagen crosslinking ↑10 Total collagen content ↓10,180,182 Calcium phosphate ↑180 Aggrecan ↑6,8,85,116 Biglycan ↑8 Decorin ↑8↓6,116 Clusterin ↑6,135 Elastin ↓6 Fibronectin ↑ (RCT vs non-RCT230) Osteopontin ↑225 Tenascin-C ↑57,80 Versican ↑8 GAG content ↑8,180 Chondroitin sulphate ↑7,57,180,181 Dermatan sulphate ↑7,180,181 Hyalauronan ↑181 Hyaluronic acid ↑181 α-Skeletal muscle actin and of myosin heavy polypeptide 1 ↑55 |
MMP-1 ↑19,63,89,103,105,156,234↓108
MMP-2 ↑156 ↑ (ftRCT vs ptRCT224) MMP-3 ↑87,156 ↓103,105,108,117 ↑ (ftRCT vs ptRCT247) MMP-9 ↑19,103,105,209,234 ↑ (ftRCT vs ptRCT224) MMP-13 ↑83,108,117,156,209 TIMP-1 ↓117 TIMP-2 ↓117 TIMP-3 ↓6,85 ADAM10 ↓6 Transglutaminase 2 ↓152 |
| Other Enzymes | |
| COX-1 ↑19,234
COX-2 ↑19,169,209,234 Cathepsin D ↑63 iNOS ↑209,222 eNOS ↑222 | |
| Transcription Factors | |
| SOX9 ↑6,8
FOXO1A ↑ (massive tears199) FOXO3A ↑ (in tears greater than one-third199) |
aIncludes changes to other enzymes and transcription factors. ↑, increased; ↓, decreased. Used with permission from Dean et al.38 ADAM, a disintegrin and metalloproteinases; COX, cyclooxygenase; FOX, forkhead box protein; ftRCT, full-thickness rotator cuff tear; GAG, glycosaminoglycan; MMP, matrix metalloproteinase; NOS, nitric oxide synthase; ptRCT, partial-thickness rotator cuff tear; RCT, rotator cuff tear; SOX9, sex-determining region Y-box 9 protein; TIMP, tissue inhibitor of metalloproteinase.
TABLE 3.
Changes to Cytokines, Growth Factors, Neuronal Factors, Apoptosis/Cell Cycle–Related Factors, and Other Factors in Rotator Cuff Diseasea
| Cytokines/Growth Factors | Apoptosis/Cell Cycle Related |
|---|---|
| IL-1α ↑19,234
IL-1ra ↑60–62 IL-1β ↑18,19,60–62,99,191,209,234 IL-2 ↓136,140 IL-6 ↑18,19,99,136,209,234 IL-11 ↑136,140 IL-15 ↑136 IL-18 ↑136 Stromal derived factor 1α ↑18,94 TNFα ↑19,99,191,209,234 VEGF ↑103,104,135,169,209 ↑ (associated with motion pain242) IGF-1 ↓6,85 TGF-β ↑161,191 bFGF ↑161,191 FGF 18 ↑140 BMP2 and BMP7 ↑161 Small inducible cytokines ↑19 Macrophage inhibitory factor ↑136 Heparin affinity regulatory peptide ↑8 Five-lipoxygenase activating protein ↑169 Hepatocyte growth factor ↓140 |
HIF-1α ↑15,103,135↓136,137,140
BNIP-3 ↑15 BCL-2 ↑135 Caspase 3 ↑136,137 Caspase 8 ↑136,137,140 Heat shock protein 27 ↑136,137,140 Heat shock protein 70 ↑136,137,140 Poly(ADP-ribose) polymerase ↑136,140 Type-2 angiotensin II receptor ↓136,140 cFLIP ↑137 cFLIP receptor ↑137 p-53 induced gene I, cell division cycle 25A, Max protein, meiotic recombination 11 homolog A ↑140 Peroxiredoxin 5 ↑237 P53 ↑121,140 P53 inhibitors ↓121 NF-KB ↓121 Receptor activator of NF-KB ↑121 |
| Neuronal Factors | Others |
| Substance P ↑89 (higher in nonperforated RCTs vs perforated62) β-endorphin ↑89 Anti-NGF30 ↑136,140 PGP9.5, GAP43 ↑241 Glutamate receptor 5, glutamate receptor metabotropic 6, glutamate receptor inotropic 3A, GABA receptor α1 ↑140 AMPA1, glutamate receptor interacting protein 1/2 ↓140 |
Ubiquitin proteasome pathway UBE2A and UBE3A ↑ (massive
tears vs small/controls199) Calpain (CAPN1) and CTSB (lysosomal enzyme) ↑ (massive tears vs small/controls199) vWF ↑169 T-cell receptor variable βchain ↑136 Ig chain, T-cell receptor α chain ↓136 GATA binding protein, PAF acetylhydrolase, Attractin, IgG-2b chain ↑136,140 Insulin induced gene 1, FGFr1, nuclear receptor coactivator 2, G protein coupled receptor 54, Ephrin A1, Thyrotroph embryonic factor, Odd Oz/ten-m homolog 2, POU domain, TNF 11, TGF-β binding protein 3, T-cell receptor β chain, cytochrome b-245, CD3 γ chain, polyprotein 1-microglobulin, Fc receptor IgE, solute carrier family 2, adenosine deaminsae, integrin-linked kinase ↑140 Dynein, nuclear receptor subfamily 2 group F member 1, Homeobox A1, FGF receptor 3, MHC class I-like sequence, T-cell receptor β chain, killer cell lectin-like receptor, strain T-cell receptor ↓140 T-cell receptor ↓136,140 |
a↑, increased; ↓, decreased. Used with permission from Dean et al.38 AMPA, alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid; ADP, adenosine diphosphate; BCL, B-cell lymphoma; BMP, bone morphogenetic protein; cFLIP, cellular FLICE (FADD-like IL-1beta-converting enzyme)-inhibitory protein; CTSB, cathepsin B; FGF, fibroblast growth factor; GABA, gamma-aminobutyric acid; GAP43, growth-associated protein 43; HIF, hypoxia-inducible factor; IGF, insulin-like growth factor; IL, interleukin; NF-KB, nuclear factor kappa light chain enhancer of activated B cells; NGF, nerve growth factor; PGP9.5, protein gene product 9.5; RCT, rotator cuff tear; TGF, transforming growth factor; TNF, tumor necrosis factor; UBE, ubiquitin conjugating enzyme; VEGF, vascular endothelial growth factor; vWF, Von Willebrand factor.
Hegedus et al69 cited that hypervascularity was associated with RC tears, although it tended to decrease with increasing tear size. The initial response to tendon injury or degeneration involved neovascularization and hyperemia, whereas hypovascularity contributed to degenerative lesions and aging. Nutrition and genetics could also play a role in vascular changes, but further research is needed. Two systematic reviews examined gene expression and protein composition in RC tendons.34,202 Dabija et al34 documented that RC tears were significantly associated with haplotypes in DEFB1, FGFR1, FGF3, ESRRB, and FGF10 and 2 single-nucleotide polymorphisms within SAP30BP and SASH1. Sejersen et al202 found that RC tears were associated with increased BNip3 in 1 study and increased expression of hypoxia inducible factor 1α, vascular endothelial growth factor, and metalloproteinases 1 and 9 in 4 studies. Moreover, the authors found that 2 studies cited no correlation between apoptotic and cytokine gene expression and tear size or histologic grade among patients with supraspinatus tears, while 1 study did not find a correlation between tear size and apoptotic markers.
Diagnosis
Predictors of RC Diagnosis
Raynor and Kuhn177 systematically reviewed 21 studies to determine which patient history factors were predictive of anatomic diagnoses among patients with atraumatic shoulder pain. Predictors of a diagnosis of an RC tear included history of hypercholesterolemia, family history of RC disease, excessive lifting, above-shoulder work, handheld vibration work, or age >60 years.
Physical Examination Tests
Several systematic reviews and meta-analyses examined the diagnostic accuracy of physical examination tests for diagnosing RC tears; however, there is substantial heterogeneity among these studies, and none replicated the same findings.13,58,66,70,73,78 The most accurate tests for diagnosing an RC tear are a positive painful arc test (likelihood ratio = 3.7; 95% CI, 1.9-7.0),73 a positive ER lag test (likelihood ratio = 7.2; 95% CI, 1.7-31),73 and possibly the lateral Jobe test.70 Hughes et al78 concluded that suspicion of an RC tear might be (1) increased by positive palpation, combined Hawkins–painful arc–infraspinatus test, Napoleon test, lift-off test, belly-press test, or drop-arm test and (2) decreased for negative palpation, empty can test, or Hawkins-Kennedy test; however, the authors determined that most tests were inaccurate and could not be recommended for clinical use. Full-thickness tears were most accurately diagnosed by a positive lag test (likelihood ratio = 5.6; 95% CI, 2.6-12).73 Gismervik et al58 and Beaudreuil et al13 reported the Jobe and empty can tests to be most accurate for diagnosing supraspinatus tears. The Patte test, resisted ER with the elbow at the side flexed at 90º, and resisted lateral rotation from neutral position were shown to be most accurate for diagnosing infraspinatus tears.13,66 The IR lag sign, belly-off, and modified belly-press tests were shown to be accurate for diagnosing subscapularis tears.66,70 Pugh et al174 systematically reviewed 5 studies that investigated various physical examination tests (ie, Hawkins, drop-arm, empty can, Patte, and bear-hug tests), concluding that they were not accurate and that they produced variable findings.
Imaging
A meta-analysis of 44 studies found high sensitivity (SE) and specificity (SP) for MRI when diagnosing RC tears: partial thickness (SE = 80%, SP = 95%) and full thickness (SE = 91%, SP = 97%).213 Also, higher–field strength MRI (3 T vs 1 T and 1.5 T) provided the highest diagnostic accuracy. Two meta-analyses estimated the pooled SE and SP for US when diagnosing RC tears: partial thickness (SE = 72%-84%, SP = 89%-93%) and full thickness (SE = 95%-96%, SP = 93%-96%).158,212 Smith et al212 also indicated that the diagnostic accuracy of US was higher for lower transducer frequency (7.5 vs ≥10 MHz) and readings by musculoskeletal versus general radiologists. Baombe11 concluded that US was accurate for diagnosing full-thickness RC tears but less accurate for diagnosing partial-thickness tears.
In a meta-analysis of 14 studies, McGarvey et al134 discovered that (1) 3-T MRI and 3-T magnetic resonance arthrogram (MRA) showed excellent diagnostic accuracy for full-thickness supraspinatus tears, (2) 3-T 2-dimensional MRA was more sensitive (86.6% vs 80.5%, P = .01) but less specific (95.2% vs 100%, P < .001) than 3-T MRI for diagnosing partial-thickness tears, and (3) there was a trend toward 3-T MRA as the most accurate for diagnosing subscapularis tears. Two meta-analyses cited no differences in SE and SP for US, MRI, and MRA for diagnosing full-thickness RC tears.109,185 Alternatively, 2 meta-analyses determined that MRA was more sensitive and specific than US and MRI for diagnosing partial- and full-thickness tears.35,185 Kelly and Fessell91 ascertained higher SE and SP for diagnosing full- versus partial-thickness tears on US, MRI, and MRA but did not compare diagnostic accuracy among these imaging modalities.
Seitz and Michener201 systematically reviewed 5 case-control studies and indicated that acromiohumeral distance is less on US for patients with full-thickness RC tears versus healthy controls and those with subacromial impingement. Measuring the subacromial space with a linear measurement of the acromiohumeral distance for patients with an RC tear may be helpful in determining diagnosis and prognosis.
Indications for Surgery
On the basis of their systematic review, Oh et al151 concluded that (1) early surgical management may be warranted for traumatic acute tears and in the presence of weakness and substantial functional disability; (2) nonoperative management is often successful when symptom duration is <3 months but may be unsuccessful for symptoms that last >1 year; and (3) the influence of age and sex on operative prognosis is unclear, although workers’ compensation claims are associated with worse prognosis.
Epidemiology
According to a systematic review of 9 studies, patients with RC tears were 55 years old on average (range, 34-61 years), primarily male (77%), and most often injured by a fall onto an outstretched arm.126 Furthermore, the mean time to surgery was 9 weeks (range, 3-48 weeks); the most commonly torn tendon was the supraspinatus (84%); and most tears were <5 cm (58%). Eljabu et al48 discovered that asymptomatic RC tears increased in size, were associated with diminished muscle quality, and led to symptom development over the course of 3 years. In their review of the natural history of RC tears, Abdul-Wahab et al1 determined that atraumatic tears were associated with muscle weakness and minor discomfort that did not appear to increase with increasing tear size.
Risk factors of RC tears included the dominant arm (odds ratio [OR], 2.30; 95% CI, 1.01-5.25) and age ≥60 years (OR, 5.07; 95% CI, 2.45-10.51), according to a meta-analysis of 10 studies.198 As shown in Table 4, Teunis et al226 conducted a meta-analysis of 30 studies and determined that the prevalence of RC abnormalities increased from 9.7% at ≤20 years old to 62% at ≥80 years old (P < .001). Vincent et al233 also discovered more RC tears among older patients; however, this systematic review did not present prevalence rates, and the samples for the 2 clinical studies were primarily female and from a single country. Two systematic reviews of basic science and clinical studies ascertained that smoking is associated with increased prevalence of larger RC tears, degenerative changes, decreased tendon quality, reduced biomechanics, and increased stiffness.17,196 The association between smoking and RC tears was also shown to be time and dose dependent.17
TABLE 4.
Prevalence of Rotator Cuff Abnormalities Overall and Among Asymptomatic and Symptomatic Patients, in the General Population, and After Shoulder Dislocationa
| Age in Decades, y | ||||||||
|---|---|---|---|---|---|---|---|---|
| <20 | 20-29 | 30-39 | 40-49 | 50-59 | 60-69 | 70-79 | >80 | |
| Overallb | ||||||||
| Shoulders, n | 299 | 434 | 481 | 933 | 1531 | 1134 | 1032 | 268 |
| Prevalence cuff abnormality, % (n) | 9.7 (29) | 6.9 (30) | 13 (60) | 13 (117) | 19 (285) | 30 (338) | 41 (427) | 62 (166) |
| P value | <.001 | |||||||
| Odds ratio (95% CI) | Reference value | 0.69 (0.41-1.2) | 1.3 (0.83-2.1) | 1.3 (0.87-2.1) | 2.1 (1.4-3.2) | 4.0 (2.6-5.9) | 6.6 (4.4-9.8) | 15 (9.6-24) |
| P value | .18 | .24 | .19 | <.001 | <.001 | <.001 | <.001 | |
| Asymptomatic | ||||||||
| Shoulders, n | 0 | 75 | 70 | 470 | 807 | 495 | 468 | 59 |
| Prevalence cuff abnormality, % (n) | 6.7 (5) | 21 (15) | 4 (18) | 9.5 (77) | 16 (77) | 28 (130) | 56 (33) | |
| P value | <.001 | |||||||
| Odds ratio (95% CI) | — | Reference value | 3.8 (1.3-11) | 0.56 (0.20-1.5) | 1.5 (0.58-3.8) | 2.6 (1.0-6.6) | 5.4 (2.1-14) | 18 (6.3-50) |
| P value | .014 | .26 | .42 | .048 | <.001 | <.001 | ||
| General populationc | ||||||||
| Shoulders, n | 2 | 12 | 140 | 254 | 473 | 442 | 394 | 164 |
| Prevalence cuff abnormality, % (n) | 0 | 0 | 2.9 (4) | 7.9 (20) | 14 (67) | 31 (138) | 50 (196) | 65 (106) |
| P value | <.001 | |||||||
| Odds ratio (95% CI) | — | — | Reference value | 2.9 (0.97-8.7) | 5.6 (2.0-16) | 15 (5.6-43) | 34 (12-93) | 62 (22-177) |
| P value | .056 | .001 | <.001 | <.001 | <.001 | |||
| Symptomatic | ||||||||
| Shoulders, n | 264 | 193 | 212 | 123 | 163 | 120 | 109 | 8 |
| Prevalence cuff abnormality, % (n) | 9.9 (26) | 4 (8) | 14 (29) | 40 (50) | 61 (163) | 68 (81) | 63 (69) | 50 (4) |
| P value | <.001 | |||||||
| Odds ratio (95% CI) | Reference value | 0.40 (0.18-0.89) | 1.5 (0.83-2.55) | 6.2 (3.6-11) | 15 (8.7-24) | 19 (11-33) | 16 (9.0-28) | 9.2 (2.2-39) |
| P value | .20 | <.001 | <.001 | <.001 | <.001 | .003 | ||
| Dislocations | ||||||||
| Shoulders, n | 33 | 154 | 59 | 85 | 88 | 77 | 61 | 37 |
| Prevalence cuff abnormality, % (n) | 9 (3) | 11 (17) | 20 (12) | 34 (29) | 47 (41) | 55 (42) | 53 (32) | 62 (23) |
| P value | <.001 | |||||||
| Odds ratio (95% CI) | Reference value | 1.2 (0.34-4.5) | 2.6 (0.66-9.8) | 5.2 (1.5-18) | 8.7 (2.5-31) | 12 (3.4-43) | 11 (3.0-40) | 16 (4.2-64) |
| P value | .74 | .17 | .011 | .001 | <.001 | <.001 | <.001 | |
aItalic text indicates statistically significant difference. Used with permission from Teunis et al.226
bOverall sums asymptomatic, general population, symptomatic, and dislocations.
cGeneral population includes cadavers.
Athletes
Harris et al67 indicated that the rate of return to play (RTP) after RC repair was 55% to 73% among Major League Baseball pitchers and that about 25% of players never pitched in the league again. The rate of RTP was only 8% in 1 study; however, 66% of players had concurrent procedures, such as SLAP (superior labrum anterior and posterior) repair, which may have affected RTP. On the basis of pooled data from 12 articles, Plate et al172 discovered that the rate of RTP was 91% for contact sports, 40% for professional overhead athletes (although RC debridement was more common than RC repair for this group), and 83% for recreational overhead athletes. Berckmans et al16 determined that greater IR force resulted in a lower functional deceleration ratio (ER/IR) on the dominant side as compared with the nondominant extremity for healthy overhead athletes; however, the most effective exercise program for increasing RC strength could not be determined. Papalia et al165 systematically reviewed 22 studies of shoulder trauma among rugby players and cited 3 studies that ascertained the prevalence of RC tears in this population (2.1%-43%), and the most common mechanisms of injury included tackling and falling onto the arm. In a meta-analysis of 23 studies, Klouche et al95 reported that the overall rate of RTP for professional and recreational athletes was 84.7% (95% CI, 77.6%-89.8%) at 4 to 7 months after RC repair and that 65.9% (95% CI, 54.9%-75.4%) returned to an equivalent level of play. The rate of RTP for professional and competitive athletes was 49.9% (95% CI, 35.3%-64.6%).
Nonoperative vs Operative Treatment
Hawk et al68 systematically reviewed 8 studies of nonoperative management for RC tears and found that (1) physical therapy had a negative effect on pain and activities of daily living in comparison with RC surgery (2 studies), (2) extracorporeal shockwave therapy (1 study) or low-level laser therapy (1 study) was associated with greater improvement in pain and function than that of sham therapy, and (3) there was no difference in pain or function for subacromial corticosteroid injections versus diathermy (1 study). Bury et al23 determined that, as compared with general physical therapy for managing RC-related shoulder pain, scapula-focused approaches (including exercise therapy, stretches, and/or manual therapy) were associated with less disability at 6 weeks but not at 3 months after therapy. Abdul-Wahab et al1 discovered that 73% to 80% of patients with full-thickness atraumatic tears and 68% with traumatic RC tears could be treated with physical therapy, especially if there were no signs of impingement yet good active ER, integrity of the intramuscular tendon of the supraspinatus, and little to no atrophy of the supraspinatus. Ainsworth and Lewis4 systematically reviewed 10 studies that cited improved outcomes following rehabilitation for RC tears; however, none of these studies included a control group. Kamioka et al88 identified 1 study reporting that aquatic therapy plus land-based rehabilitation after RC repair resulted in greater improvement in passive flexion range of motion (ROM) measured at 3 and 6 weeks after surgery as compared with land-based rehabilitation alone. One systematic review that examined the effectiveness of manual and exercise therapy concluded that (1) exercise was superior to manual therapy but not to surgery, (2) there were no differences in pain or function for exercise and/or manual therapy versus glucocorticoid injection or subacromial decompression, and (3) exercise was associated with greater improvement in function over advice to maintain normal activities.159 On the basis of a systematic review of 5 studies, Braun et al21 was unable to identify a prognostic model to predict outcomes among patients who underwent physical therapy for RC disorders (subacromial impingement and/or RC tear).
Ryosa et al187 conducted a meta-analysis of data from 3 randomized controlled trials and documented greater improvement in pain following RC repair versus conservative management (mean difference = –0.93; 95% CI, –1.65 to –0.21; P = .01), although the observed difference in pain score was below the level of the minimal clinically important difference and there was considerable variation in conservative management among studies. Two systematic reviews cited support for operative versus nonoperative treatment of RC tears; 1 of these reviews also indicated improved function with rehabilitation versus no rehabilitation.79,200 According to a systematic review of 11 studies, injection of hyaluronic acid for RC tear was associated with improved pain and function as compared with corticosteroid injection, physical therapy, or saline.157 Only minor complications were found for hyaluronic acid, including vagal reaction and persistent pain at the injection site. Two overlapping systematic reviews cited 1 study that documented no difference in outcomes following hyaluronic acid versus corticosteroid injection.43,79 Abdul-Wahab et al1 determined that only 40% of patients who had corticosteroid or hyaluronate injection for RC tears were satisfied at 24 weeks. Given the findings of their systematic review, Robb et al183 concluded that nonsteroidal anti-inflammatory drugs and subacromial corticosteroid injections can be used with caution in addition to supervised exercise. Huisstede et al79 discovered 2 studies that did not observe a difference in pain or function for suprascapular nerve block with dexamethasone versus placebo for treating RC tears in the short term. Curtis33 systematically reviewed clinical, animal, and in vitro studies that examined the effect of nutrients on treating tendon injuries, concluding that there is limited evidence for consuming vitamin D, a multifaceted supplement (Tenosan), or cyanidin (a phytochemical in fruits and vegetables) to improve tendon healing.
Surgical Repair Methods
Double- vs Single-Row Repairs
Wall et al236 performed a systematic review of 15 cadaveric and animal studies that compared biomechanical properties for double-row (DR) versus single-row (SR) repairs. Nine studies favored DR repair with regard to tensile strength, construct failure, and gap formation, and 5 studies demonstrated that DR repairs increased native footprint coverage. Their review concluded that (1) DR repair restores more of the anatomic RC footprint and (2) SR repair is not biomechanically superior to DR repair.
Several overlapping systematic reviews reported up to 6 studies that documented improvement in PROs for DR and SR repairs, but there were no statistically significant differences between groups.‡ Five overlapping meta-analyses also cited no statistically significant differences in PROs between DR and SR repairs.31,39,138,171,205 Chen et al31 determined that for tears >3 cm, DR repairs had better PROs than did SR repairs. Three meta-analyses found that in comparison with SR repairs, DR repairs had better PROs and/or increased ROM overall and especially for tears measuring >3 cm.240,246,249
Several overlapping systematic reviews identified 2 studies that documented better healing rates for DR versus SR repair.147,167,173,197 DeHaan et al39 identified 4 studies that examined structural healing and indicated a borderline significant trend toward a higher retear rate for SR versus DR repairs (43.1% vs 27.2%, P = .06). Millett et al138 discovered an increased risk of retears for SR versus DR repairs (relative risk [RR], 1.76; 95% CI, 1.25-2.48), and this association was strongest for partial-thickness tears (RR, 1.99; 95% CI, 1.40-3.82). Several meta-analyses revealed that DR repairs have better structural healing versus SR repairs for tears measuring >3 cm.31,240,246 Zhang et al249 performed a meta-analysis of 8 studies and determined that the retear rate was less for DR versus SR repairs for partial-thickness tears; however, the rate of retear did not differ between repair methods for full-thickness tears. Two overlapping meta-analyses cited lower retear rates for DR and suture-bridge repairs versus SR repairs for tears measuring >1 cm.45, 71 Additionally, Duquin et al45 discovered that retear rates did not differ between SR repair methods (transosseous vs SR suture anchor) or between arthroscopic and nonarthroscopic repairs (open + mini-open [MO]) for any tear size with SR or DR repair. Hein et al71 indicated that retear rates did not differ between DR and suture-bridge repairs for any tear size.
Mascarenhas et al130 and Spiegl et al217 systematically reviewed meta-analyses that compared DR and SR repairs, and both concluded that PROs were improved for DR versus SR repairs for tears measuring >3 cm and that structural healing was greater for DR versus SR repairs for tears of any size and tears >3 cm. Mascarenhas et al130 used the Jadad et al84 decision algorithm to identify the highest-quality meta-analyses, which were those by Chen et al,31 Zhang et al,249 and Millett et al.138
Brown et al22 performed a meta-analysis of 13 studies to evaluate the effect of suture configuration, repair method, and tear size on structural healing after RC repair. Retear rates did not differ by suture configuration (simple, mattress, and modified Mason-Allen sutures) or tear size for SR repairs, and the retear rates did not differ between DR suture anchor and suture-bridge repairs for any tear size, which were all performed with mattress sutures.
Transosseous-Equivalent Repairs
Mall et al127 systematically reviewed 5 biomechanical studies, of which 4 indicated better biomechanical properties when the medial-row anchors were tied before the lateral-row anchors. One study demonstrated no significant differences in contact pressure, mean failure load, and gap formation for a standard suture-bridge repair with knots tied at the medial row versus knotless repairs.
Transosseous Repairs
Coghlan et al32 identified 1 study that documented no statistically significant differences in PROs and retear rates for transosseous repair with Ethibond via the modified Mason-Allen suture technique versus transosseous repair with polydioxanone cord via the modified Kessler technique.
Arthroscopic vs MO Repairs
Nho et al146 performed a systematic review of 17 studies, of which only 4 directly compared arthroscopic with MO repairs and none ascertained a statistically significant difference in PROs between the groups. The complication rate was 3% for arthroscopic repair and 6.6% for MO repairs. Lindley and Jones114 performed a systematic review of 10 studies and found only 1 that indicated lower pain at 6 months after arthroscopic versus MO repair (P = .03); in addition, tears >3 cm had a higher retear rate when repaired arthroscopically (P = .04). Huang et al77 performed a meta-analysis of 18 studies and determined that the Constant score was better for MO versus all-arthroscopic repair (standardized mean difference = 0.87; 95% CI, 0.11-1.62; P = .03). Three meta-analyses did not find any statistically significant differences in PROs, ROM, or retear rates for arthroscopic versus MO repair.86,142,203 Gurnani et al65 conducted a meta-analysis of 16 studies and cited improvement in PROs after arthroscopic or MO RC repair, but they did not perform any statistical comparisons between these 2 repair methods.
Repair of Articular-Sided Partial-Thickness RC Tears
Bollier and Shea20 systematically reviewed 14 studies that assessed PROs after debridement with or without acromioplasty, completion and repair, or transtendon repair of a symptomatic partial articular-sided RC tear, of which only 1 retrospective nonrandomized study compared these procedures and indicated improved long-term results and decreased reoperation rates in the tear completion + MO repair group. Two overlapping meta-analyses compared tear conversion and repair versus transtendon repair for partial articular-sided RC tears. Sun et al221 performed a meta-analysis of 5 studies and did not find a statistically significant difference in American Shoulder and Elbow Surgeons (ASES) scores; however, the retear rate was higher for tear conversion and repair versus transtendon repair (11.3% vs 4.3%, P < .05). Ono et al155 conducted a meta-analysis of 3 studies and cited no statistically significant differences in Constant, ASES, and visual analog scale (VAS) scores as well as ROM and retear rates for tear conversion and repair versus transtendon repair.
Repair of Isolated Subscapularis Tears
Mall et al125 systematically reviewed 3 arthroscopic-repair and 6 open-repair level 4 noncomparative studies of patients with isolated subscapularis tears. They reported that (1) Constant scores and pain improved after arthroscopic or open repairs, (2) biceps tenodesis was the most commonly performed concomitant procedure, and (3) postoperative healing was good (90%-95%).
Surgical Management of Partial-Thickness RC Tears
Strauss et al220 discovered that 29% to 93% of patients had excellent outcomes after repair of a partial-thickness tear in 16 studies. Furthermore, debridement of partial-thickness tears <50% of the tendon’s thickness with or without acromioplasty resulted in good outcomes, although 7% to 35% of partial-thickness tears progressed to full-thickness tears. Katthagen et al90 reported (1) good outcomes following arthroscopic repair of partial-thickness tears >50% thickness and (2) no difference in outcomes for in situ repair versus repair of the tendon after completion to full-thickness tear. However, Pedowitz et al168 determined that repair of partial-thickness tears >50% thickness failed and concluded that there was weak evidence for the 50% rule for arthroscopic surgery. Papalia et al162 systematically reviewed 23 studies and generally reported improvement in ROM and PROs following repair of partial-thickness tears; however, treatment options and PRO measures varied greatly among studies, which limited comparisons.
Surgical Management of Massive and Irreparable RC Tears
Henry et al72 pooled data from 18 studies of arthroscopic repair of chronic massive RC tears and determined that the rate of retear was 79% and that there was an improvement in postoperative VAS (5.9 to 1.7), active ROM (125º to 169º), and the Constant score (49 to 74). Two overlapping systematic reviews examined postoperative PROs for latissimus dorsi tendon transfer (LDT-T) among patients with irreparable tears.118,145 Namdari et al145 reviewed 10 noncomparative studies and cited improvement in clinical scores, pain, ROM, and strength following LDT-T. Longo et al118 reported 19 studies that demonstrated restoration of active ER after LDT-T; they also discovered 3 studies that showed increased active ER and anterior elevation for LDT-T plus teres major transfer versus LDT-T alone. Tendon transfers for irreparable tears can be technically challenging and associated with neurovascular risks; thus, techniques involving a graft or synthetic patch have been developed to aid in bridging the gap and to allow the tendon to reconnect to the anatomic footprint. Lewington et al112 found increased structural integrity on MRI for biceps tendon autograft (58% vs 26%, P = .04) and fascia lata autograft (79% vs 58%, P < .05) when compared with partial primary repairs for irreparable tears. High structural healing rates for allografts (74%-90%), xenografts (73%-100%), and synthetic materials (60%-90%) for bridging reconstruction were also found.
Concomitant Conditions and Surgical Procedures
Two overlapping meta-analyses compared outcomes of full-thickness RC repairs with concomitant acromioplasty versus without acromioplasty.50,214 Song et al214 indicated that ASES scores were higher for RC repairs with acromioplasty versus without acromioplasty; however, no other statistically significant differences in pain, ROM, or retear rates were cited in either meta-analysis.50 Redondo-Alonso et al178 determined that 22% to 78.5% of patients in 5 studies had chronic pathology of the supraspinatus and the long head of the biceps tendon. Leroux et al110 conducted a meta-analysis of 12 studies and discovered that biceps tenodesis was associated with higher postoperative Constant scores (92.8 vs 90.6, P < .01) and fewer biceps deformities (15.5% vs 3.9%, P < .01) than tenotomy when performed concurrently with RC repair. In a meta-analysis of 903 patients undergoing RC repair, Shang et al204 also indicated that tenotomy was associated with worse Constant scores (standard mean difference = –0.23, P = .03) and increased odds of Popeye deformities (OR, 2.78; P < .0001) than tenodesis. Among patients with SLAP tears and concomitant RC tears, Erickson et al49 cited no difference in PROs after tenotomy for patients aged ≥40 versus <40 years. Gombera and Sekiya59 discovered that persistent pain and dysfunction after shoulder dislocation were often associated with an RC tear. Surgical repair of acute RC repairs after shoulder dislocation was typically associated with better PROs than nonoperative management. Two systematic reviews cited no statistically significant differences in PROs following RC repair with subacromial decompression versus without.26,32
RC Tears After Total Shoulder Arthroplasty
Levy et al111 performed a meta-analysis of 1259 patients from 15 studies that examined the incidence of RC tears after total shoulder arthroplasty, and they reported that 11% of patients had superior cuff tears, 3% had subscapularis tears, and 1% underwent reoperation for RC tear after total shoulder arthroplasty. Horner et al74 systematically reviewed 11 studies that examined indications for shoulder arthroscopy after total shoulder arthroplasty, and they determined that 19% of patients underwent arthroscopy for evaluation of the RC and/or associated impingement and 4% for RC tear.
Biological Augmentation
Platelet-Rich Plasma
Given the low intrinsic healing potential of tendon tissue and its degenerative nature, augmentation for tissue regeneration is an expanding area of research. Platelet-rich plasma (PRP) is a common augmentation strategy for both conservative and operative management of RC tears.53 PRP is rich in soluble growth factors that may be involved in tissue regeneration and vascularization.54 PRP can also stimulate angiogenesis and increase cell migration, differentiation/proliferation, and extracellular matrix production.244 Five overlapping systematic reviews evaluated the effectiveness of PRP for conservative management of RC tears or in combination with arthroscopic RC repair.5,53,123,139,164 Miranda et al139 reported 10 laboratory studies that indicated positive or partially positive results in favor of PRP; however, 70.6% of 7 clinical studies and 75% of 8 meta-analyses did not find a statistically significant difference in clinical outcomes for PRP use versus control. Filardo et al53 found that 5 of 8 studies reported improved function and pain with PRP use for chronic RC tears managed conservatively, but only 5 of 18 studies cited improved PROs and lower retear rates with the use of PRP at the time of arthroscopic RC repair. Maffulli et al123 systematically reviewed 3 evidence level 1 or 2 studies and determined that the only PRO that differed between the PRP group and controls was postoperative pain score. Andia and Maffulli5 discovered 1 study that documented lower retear rates with PRP use for small and medium RC tears and 1 study that cited increased retears for PRP use for massive tears, suggesting that tear size is influential. Papalia et al164 found that 1 of 7 studies indicated decreased retears and better Rowe scores with the use of PRP versus control and that 1 other study indicated increased retears when PRP was used.
Five of 11 overlapping meta-analyses reported no statistically significant differences in PROs and/or retear rates for PRP use versus control among patients undergoing arthroscopic RC repair.§ Two meta-analyses cited no overall differences in retear rates and postoperative PROs for PRP use versus control.193,248 However, Saltzman et al193 performed subgroup analyses and demonstrated that PRP use was associated with lower retear rates for (1) DR repairs of small- or medium-sized versus large or massive tears, (2) PRP application at the tendon-bone interface, (3) application of a solid PRP matrix versus liquid, and (4) DR versus SR repairs. Zhang et al248 also determined that PRP use was associated with a lower retear rate for small- and medium-sized tears versus large- and massive-sized tears. Yang et al244 performed a meta-analysis of 8 studies and discovered that PRP use was associated with better Constant, Simple Shoulder Test, and VAS scores, although there were no statistically significant differences in ASES and UCLA (University of California, Los Angeles) scores and overall retear rates for PRP use versus control. Also, stratifying by tear size and length of follow-up had no statistically significant effect on the association between PRP use and PROs. In a meta-analysis of 5 studies, Cai et al24 indicated that PRP use was associated with a lower retear rate overall (RR, 0.05; 95% CI, 0.31-0.83) and a lower retear rate for mild to moderate versus severe to massive tears (RR, 0.35; 95% CI, 0.14-0.90). Similarly, Vavken et al232 discovered that PRP use was associated with a lower retear rate for tears <3 cm versus >3 cm (RR, 0.60; 95% CI, 0.37-0.97); however, PRP use was not found to be cost-effective.
Stem Cells
Mesenchymal stem cells (MSCs) are capable of differentiating into multiple cell lines, and they provide a twofold mechanism of repair: MSCs (1) are capable of differentiating into new tenocytes and directly forming new tendon tissue and (2) can modulate the local immune response to stimulate surrounding cells for growth factor and cytokine production.25,37,64,148,170 Ahmad et al3 reviewed 27 preclinical and 5 clinical studies that demonstrated that MSCs were able to survive and differentiate into tenocytes when placed in tendon environments, increase collagen fiber density, enhance tissue architecture, and restore a nearly normal tendon-bone interface. Only 1 randomized controlled trial was cited, which noted that skin-derived tendon cells produced better clinical results than autologous plasma. Obaid and Connell150 determined that MSCs can autopopulate allografts in vitro and indicated promising results for using MSCs with tendon repairs in animal models; however, more in vivo human trials are needed. Pas et al166 systematically reviewed 2 nonrandomized studies that evaluated bone marrow–derived stem cells as an additive for RC repair, and both studies demonstrated fewer retears; however, 1 study did not have a control group, and neither study assessed PROs in a blinded fashion. A systematic review of 10 animal studies and 7 human studies cited (1) improved healing rates and load to failure with the use of MSCs in the animal studies, (2) several potential sources for harvesting MSCs for treating RC pathology (RC tendon, subacromial bursa, long head of the biceps tendon, and the proximal humerus), and (3) 1 case series that reported good repair integrity at 1 year after RC repair with MSCs but did not include a control group.14 Imam et al81 identified 1 laboratory-based study that discovered a superior number of progenitor cells from the iliac crest versus the tibia and calcaneus and 4 clinical studies that indicated improved outcomes and good structural integrity (approximately ≥90%) for RC repairs augmented with bone marrow aspirate concentrate, although 2 of these studies did not include a control group.
Scaffolds
Scaffolds for augmentation of RC repairs, including xenografts, allografts, and synthetic matrices, can facilitate cellular growth and collagen deposition. Thangarajah et al227 systematically reviewed 11 clinical studies and 6 animal studies that evaluated scaffold use for augmentation of RC repairs. Two studies cited improved clinical outcomes for augmentation with an acellular dermal matrix and a nonabsorbable polypropylene patch versus control; 1 study determined that augmentation with porcine small intestinal mucosa was associated with less muscle strength versus control; the remaining 8 clinical studies either found no statistically significant differences between the augmentation and control groups or did not include a control group. The animal studies showed native cell infiltration; 3 separate studies demonstrated a higher load to failure for augmentation with porcine intestinal submucosa, an acellular dermal matrix, and an electrospun fibrous membrane versus control; and 1 study indicated better tensile strength for MSCs versus augmentation with polyglycolic acid. Longo et al119 concluded that the benefits of extracellular matrix grafts include the capability to decrease in vivo mechanical forces on the tendon repair during healing and prevent gap formation while the host cells infiltrate and heal; furthermore, biologic scaffolds have type I collagen and higher affinity for host cells as compared with synthetic scaffolds but higher risk of immunogenicity. Papalia et al164 cited good clinical results for autograft augmentation in 3 uncontrolled studies, worse clinical results and more complications for porcine xenografts in 4 of 5 studies, good clinical results for allografts in 5 of 9 studies (2 controlled, 3 uncontrolled), and good clinical results for synthetic devices in 6 of 7 uncontrolled studies. Ono et al153 determined that repairs for large to massive tears with grafts had increased healing (OR, 2.48; 95% CI, 1.58-3.90) and better PROs (P ≤ .02) versus repairs without grafts; however, statistical significance was reached only when 1 or 2 studies were excluded for practical or statistical reasons. Bridging grafts were associated with lower VAS pain scores (1 vs 3, P = .01) versus graft augmentation for large to massive tears, although healing rates did not differ for bridging versus augmentation (77.9% vs 64%, P = .21).154 In a systematic review of 10 studies, Ferguson et al51 reported that allograft augmentation was associated with more intact repairs as compared with primary repair controls in 4 studies and that polypropylene patches were associated with improved structural (83% vs 59% and 49%, P < .01) and functional outcomes as compared with controls and xenograft augmentation, respectively.
Gene Therapy
Rotini et al184 found that gene therapy with adenovirus in vitro demonstrated capabilities of transferring genes to fibroblasts; however, genes that can be transcribed for tendon healing have yet to be identified.
Postoperative Rehabilitation
Types of Postoperative Rehabilitation Programs
The American Society of Shoulder and Elbow Therapists conducted a systematic review of 117 studies to develop a consensus statement regarding rehabilitation after arthroscopic RC repair.228 The society recommended a 2-week period of immobilization, followed by performance of protected passive ROM during weeks 2 to 6, re-establishment of active ROM after 6 weeks, progression to strengthening at week 12, and finally the return to sport or work when appropriate.
Dickinson et al41 reported greater improvement in postoperative PROs for supervised versus unsupervised therapy in 1 of 5 studies and cryotherapy versus no cryotherapy in 2 of 5 studies. In a systematic review by Du Plessis et al,44 continuous passive motion was associated with greater ROM in 2 studies, less pain in 1 study, and increased strength in 1 study as compared with physical therapy. Baumgarten et al12 conducted a systematic review of 4 studies to determine an optimal rehabilitation program after RC repair. Overall, outcome scores were improved for all types of therapies but did not significantly differ for (1) continuous passive motion versus physical therapy or manual passive motion and (2) supervised versus unsupervised physical therapy. Two other systematic reviews also cited no statistically significant differences in PROs for continuous passive motion versus manual therapy.79,245 Thomson et al229 systematically reviewed 11 studies and discovered improved postoperative PROs overall but did not find any single rehabilitation program to be superior to another. Marik and Roll128 indicated (1) strong evidence to support postoperative rehabilitation involving progressive tendon forces plus standard rehabilitation and (2) inconclusive evidence regarding other types of postoperative rehabilitation (ie, continuous passive motion, supervised vs unsupervised therapy, and land-based vs aquatic-based therapy).
Early vs Delayed Postoperative Rehabilitation
Edwards et al47 systematically reviewed 22 studies that examined electromyography activity during rehabilitation exercises in normal shoulders to determine which exercises met a cut point of ≤15% maximal voluntary isometric contraction and were not likely to result in excessive loading in the early postoperative rehabilitation period. They identified 19 active-assisted exercises that met the aforementioned criteria and would be appropriate for loading the supraspinatus or infraspinatus.
Several overlapping meta-analyses and systematic reviews compared outcomes for early versus delayed postoperative rehabilitation.28,29,115,128,131,245 The definitions of early and delayed rehabilitation varied greatly across these studies, with early ROM beginning immediately after surgery to 6 weeks postoperatively and with delayed ROM beginning 3, 4, or 6 weeks postoperatively. Four meta-analyses and 1 systematic review documented no statistically significant differences in functional outcomes, ROM, and retear rates for early versus delayed rehabilitation.28,29,115,131,245 A few meta-analyses found some evidence for better ER30,56,207 and forward elevation56,179 for early ROM but better function30,56 and healing30 for delayed ROM. When making comparisons with delayed passive ROM (3-6 weeks after surgery), Kluczynski et al98 discovered (1) fewer retears for early passive ROM (within 1 week of surgery) for tears ≤3 cm repaired by transosseous or SR methods and (2) increased retears for early passive ROM for tears >5 cm repaired by DR or any other method. When making comparisons with delayed active ROM (≥6 weeks), Kluczynski et al97 found increased retears in small (≤3 cm) and large (>3 or 5 cm) tears for early active ROM (<6 weeks). Three systematic reviews of overlapping meta-analyses determined that early ROM is associated with better ROM, but there is no difference in functional outcomes, pain, or healing rates between early and delayed ROM.75,131,194 However, there is some evidence that larger tears may be associated with more retears for early versus delayed ROM.75,194 The meta-analyses with the highest-quality rankings were those by Chan et al28 and Riboh and Garrigues.75,179
Outcomes and Complications
Surgical Repair
Two systematic reviews reported significant improvement in ROM and PROs after RC repair.126,251 Zuke et al251 found that within 6 months of surgery, all indicated complications, the majority of postoperative improvement in strength and ROM, and the majority of retears had occurred. Spennacchio et al216 systematically reviewed 10 articles that examined long-term (≥5 years) outcomes of arthroscopic RC repair and discovered that all of the studies demonstrated improvement in PROs and satisfactory results. In a meta-analysis of 6 studies, Shen et al206 determined that DR repairs had decreased risk of retears overall (RR, 1.71; 95% CI, 1.18-2.49) and partial-thickness retears (RR, 2.16; 95% CI, 1.26-3.71) versus SR repairs; however, there were no statistically significant differences in PROs between DR and SR repairs. Two meta-analyses and 1 systematic review reported that retears were associated with worse PROs and/or reduced strength after SR, DR, or all-arthroscopic RC repairs versus intact RCs.186,211,243 DiSilvestro et al42 indicated that patients returned to driving at a mean of 2 months after RC repair.
Standard assessment and reporting of complications, especially shoulder stiffness, after arthroscopic RC repair are lacking, as demonstrated in a systematic review by Audige et al.9 Sixteen definitions of the terms “frozen shoulder,” “shoulder stiffness,” and “stiff painful shoulder” were identified; diagnostic criteria for stiffness varied greatly among studies; and 12 definitions of restricted ROM were cited. Randelli et al176 found that 73% of 56 studies reported complications after RC repair, with retears (11%-94%) and stiffness (2%-11%) being the most common. Less commonly, anesthetic, neurovascular, thromboembolic, and septic complications were indicated. Two overlapping systematic reviews identified risk factors for postoperative stiffness, including workers’ compensation status, age <50 years, calcific tendinitis or adhesive capsulitis, concomitant labral repair, tear size, subscapularis tears, biceps tears, preoperative ROM, diabetes, open repairs, single-tendon repairs, and partial articular supraspinatus tendon avulsion repair.40,163
Revision Surgery
Ladermann et al101,102 performed 2 overlapping systematic reviews of 10 evidence level 3 or 4 studies that examined outcomes following revision arthroscopic RC repair. Improvement in ROM and function after revision repair was found, and predictors of worse outcomes included female sex, tear recurrence after revision repair, preoperative active forward flexion <135º, and preoperative VAS pain score >5.102 Furthermore, the authors concluded that most recurrent tears could be treated conservatively but revision surgery may be warranted for younger patients, a tear involving 3 tendons, and tears involving the subscapularis.101
Surgical Repair With Stiffness
Sabzevari et al188 reported that preoperative stiffness is associated with decreased preoperative ROM among patients undergoing RC repair; however, postoperative outcomes did not differ between those with and without preoperative stiffness. Papalia et al163 also cited strong evidence for arthroscopic capsular release among patients with shoulder stiffness secondary to RC repair.
Surgical Repair With Augmentation
Steinhaus et al219 systematically reviewed 24 studies that examined outcomes after patch use with RC repair and discovered similar improvement in ROM, strength, and PROs for all augmentation and interposition techniques—except xenografts, which demonstrated less improvement in outcome scores versus the other techniques. Retear rates were 44% for xenografts, 23% for allografts, and 15% for synthetic grafts.
Repair of Subscapularis Tears
In a systematic review of 8 studies, Saltzman et al192 indicated improvement in PROs, ROM, and strength after arthroscopic repair of isolated subscapularis tears, and the retear rate ranged from 4.8% to 11.8%. Shin et al208 systematically reviewed 8 studies that examined outcomes following pectoralis major tendon transfer for irreparable subscapularis tendon ruptures. They reported a low incidence of postoperative nerve palsy (1%) and overall improvement in Constant and pain scores; however, Constant scores were significantly greater after subcoracoid transfer versus supracoracoid transfer of the pectoralis major tendon (P < .001).
Predictors of Postoperative Outcomes
Several overlapping systematic reviews and meta-analyses examined predictors of retears and worse outcomes after RC repair.∥ Predictors of retears included older age,52,106,133,144,190 smoking,196 increased tear size,52,106,133,144,175,190 additional biceps or acromioclavicular procedures,52,106 preoperative fatty infiltration,52,93,133,175 multiple tendon involvement,52,175 diabetes,175 DR repairs,175 increased retraction of the tendon,52 and decreased bone mineral density.52 Predictors of worse outcomes included older age,52 female sex,52 smoking,17,196 diabetes,52 lower baseline scores,190 workers’ compensation status,92,106,175,190 decreased preoperative muscle strength,52,175 increased tear size,52 preoperative fatty infiltration,93 <3 months between injury and surgery,143 decreased sports activity,52 preoperative shoulder stiffness,52 and obesity.52,96 Two reviews also determined that patients with a workers’ compensation claim took longer to return to work and were less satisfied after RC repair.36,92 Weinheimer et al239 indicated that low surgeon volume (<12 surgical procedures per year) predicted increased length of stay, increased operating time, and an increase in reoperation rate. Raman et al175 evaluated the strength of each predictive factor and discovered preoperative fatty infiltration to be the strongest predictor of retears (Figure 2).
Figure 2.
Flowchart of predictors. Pre-op, preoperative; WCB, Workers’ Compensation Board. Used with permission from Raman et al.175
Silva et al210 systematically reviewed 14 studies of patients aged ≥65 years who underwent arthroscopic, MO, or open surgical repair of a symptomatic RC tear, and all studies demonstrated significant improvement between pre- and postoperative outcomes, with an overall postoperative patient satisfaction rate >90% and a healing rate of 78%. Downie and Miller43 reported improved outcomes after surgery among patients >60 years old. MacKechnie et al122 systematically reviewed 7 studies of open or arthroscopic repair of full-thickness RC tears of patients <55 years old and found that 81% of patients had traumatic tears; all studies that evaluated postoperative strength and pain showed improvement; and 82% of patients had satisfactory results. Lazarides et al107 systematically reviewed 12 studies of patients <40 years old and determined that RC etiology was of traumatic origin in 8 studies and due to chronic overuse among elite throwers in 4 studies; 11 of these studies indicated good outcomes, although many elite throwers had difficulty returning to play (25%-97%).
Marx et al129 systematically reviewed 86 articles from 6 major orthopaedic journals to determine how many reported indications for RC surgery (eg, duration of symptoms), which can subsequently influence patient outcomes. Of the retrieved articles, 44% did not report the duration of symptoms; <50% did not report a history of trauma or limitations of activities of daily living; and 48% failed to describe attempts at nonoperative management before surgery.
PRO Measures
Standardization of measures for assessing outcomes after operative and nonoperative treatment for RC tears is lacking, which makes it difficult to compare studies and may account for inconsistent findings across studies. Makhni et al124 systematically reviewed 156 studies from 6 orthopaedic journals with a high impact factor and found that 63% reported ROM, 38% indicated quantitative strength measurements, 65% evaluated tendon integrity via imaging, and 16% to 61% included at least 1 of the 5 most common functional scores: Constant (61%), ASES (59%), UCLA (35%), Simple Shoulder Test (28%), and adjusted Constant (16%). Page et al160 systematically reviewed the outcome domains and instruments used in 171 randomized controlled trials that examined the effectiveness of physical therapy interventions for shoulder pain, including 101 studies of patients with pain associated with RC disease. The outcome domains that were assessed included shoulder pain (87%), function (72%), ROM (67%), adverse events (27%), global assessment of treatment success (24%), strength (18%), health-related quality of life (18%), work disability (4%), and referral for surgery (2%). VAS was the most commonly reported measure of shoulder pain, and the Constant score and the Shoulder Pain and Disability Index were the most commonly used measures of shoulder function. Saccomanno et al189 systematically reviewed 120 studies to determine the reliability of MRI for assessing repaired RCs. Structural integrity was the most commonly used criterion, and the dichotomized Sugaya classification had the highest reliability (kappa = 0.80-0.91).
Many PROs are available for assessing pain and function associated with RC tears; however, it is important to select high-quality PROs that demonstrate good psychometric properties (valid, reliable, and responsive). As shown in Table 5, Huang et al76 systematically reviewed 73 studies to examine the psychometric properties of 16 PROs used among patients with RC tears. The Western Ontario Rotator Cuff Index (WORC) had the best overall quality, followed by the Disabilities of the Arm, Shoulder and Hand (DASH) score, Shoulder Pain and Disability Index, and Simple Shoulder Test; however, the most commonly cited PROs (ASES and Constant scores) demonstrated the lowest quality. In a systematic review of 120 articles that reported on 11 PROs, St-Pierre et al218 indicated that (1) only the ASES and Upper Limb Functional Index had a measurement error <10% of the global score and (2) the minimum detectable change and minimal clinically important difference ranged from 6.4% to 20.8% and 8% to 20%, respectively. Longo et al120 examined the psychometric properties of the WORC and the Rotator Cuff Quality of Life Measure (RC-QOL) in 16 studies and determined that the methodological quality was adequate on some properties (construct validity, reliability, responsiveness, internal consistency, and translation) but needed improvement on others. Makhni et al124 created metrics to evaluate 16 PROs with respect to comprehensiveness (the total number of pain, functional, and quality-of-life/satisfaction metrics included in each study) and efficiency (the comprehensiveness score divided by the number of survey components). The most comprehensive PROs were the RC-QOL and Penn Shoulder Score, and the most efficient was the UCLA, DASH, and Constant score.
TABLE 5.
Quality of Measurement Properties per Questionnaire: Summarya
| Internal Consistency | Reliability | Measurement Error | Content Validity | Structural Validity | Hypothesis Testing | Criterion Validity | Responsiveness | |
|---|---|---|---|---|---|---|---|---|
| ASES | – | ++ | – | ? | ? | – – | ? | ? |
| Constant | ? | ++ | ? | NA | NA | – – | ? | + |
| DASH | ? | ++ | – – | NA | ++ | + | NA | ++ |
| KSS | ? | NA | NA | ? | NA | ? | ? | ? |
| L’Insalata | ? | ? | NA | ? | NA | ? | ? | ? |
| OSS | ? | – | NA | ? | NA | + | NA | ? |
| Penn | ? | + | ? | ? | NA | ? | NA | ? |
| RC-QOL | ? | ? | NA | ? | NA | – | NA | ? |
| SAL | NA | + | NA | NA | NA | ? | NA | NA |
| SDQ | ? | ? | NA | NA | NA | – | NA | ? |
| SPADI | +++ | ++ | – – | NA | +++ | –/+ | ? | + |
| SST | +++ | ++ | – | ? | NA | +/+ | ? | + |
| SSV | NA | NA | NA | NA | NA | – | NA | NA |
| UCLA | ? | + | ? | NA | NA | + | ? | ? |
| WOOS | NA | + | NA | NA | NA | ? | NA | ? |
| WORC | ++ | ++ | ? | +++ | NA | ++ | NA | + |
aA plus sign (+) indicates positive evidence; a question mark (?), indeterminate evidence; and a negative sign (–), negative evidence. Used with permission from Huang et al.76 ASES, American Shoulder and Elbow Surgeons shoulder outcome score; Constant, Constant-Murley score; DASH, Disabilities of the Arm, Shoulder and Hand score; KSS, Korean Shoulder Scoring System; L’Insalata, L’Insalata Shoulder Rating Questionnaire; NA, no information available; OSS, Oxford Shoulder Score; Penn, Penn Shoulder Score; RC-QOL, Quality-of-Life Outcome Measure for Rotator Cuff Disease; SAL, Shoulder Activity Level; SDQ, Shoulder Disability Questionnaire; SPADI, Shoulder Pain and Disability Index; SST, Simple Shoulder Test score; SSV, Subjective Shoulder Value; UCLA, University of California, Los Angeles shoulder score; WOOS, Western Ontario Osteoarthritis Shoulder index; WORC, Western Ontario Rotator Cuff Index.
Cost-effectiveness of RC Repair
In 2015, Nwachukwu et al149 systematically reviewed 3 studies and reported that (1) the lifetime age-weighted mean societal savings was US$13,771 per RC repair, (2) the mean lifetime gain in quality-adjusted life years for RC repair was 0.81 based on the Health Utility Index, and (3) SR repairs were more cost-effective than DR repairs.
Quality of Randomized Controlled Trials
Tadjerbashi et al223 evaluated the quality of 50 randomized controlled trials involving shoulder arthroscopy, of which 22 involved the RC. The Jadad quality score was 3 of 5 (highest quality) for all shoulder studies, although the authors did not stratify by type of shoulder arthroscopy. McCormick et al132 also reported a mean Jadad score of 3 for their systematic review of 54 randomized controlled trials involving RC disorders, although 63% of these studies were nonoperative. Furthermore, they determined that these studies were often lacking in the following CONSORT criteria (used for standard reporting of clinical trials): trial design descriptions (66%), descriptions of randomization type (65%), and power analysis (46%).
Conclusion
This systematic review offers a comprehensive summary of all systematic reviews and meta-analyses published on various topics related to the RC. There is a substantial body of literature pertaining to the RC; however, for some topics, evidence is lacking or flawed, or the results are conflicting. There is substantial evidence indicating that the most accurate physical examinations for diagnosing RC tears are a positive painful arc and positive ER lag test and that the most accurate diagnostic imaging tools are US, MRI, and MRA. However, further research is needed to determine which of these imaging modalities is the most accurate for diagnosis. There is considerable evidence showing that rehabilitation is better than no rehabilitation for nonoperative management of RC tears, although RC repair was shown to be superior to rehabilitation alone. Moreover, there is no evidence to support the use of injections for nonoperative management of RC tears. With respect to operative management, the consensus is that DR repairs result in better outcomes and fewer retears than SR repairs, especially for tears >3 cm. The most commonly reported complications after RC repair are retears and stiffness, although standard reporting and consistent definitions of postoperative complications are lacking. Predictors of retears and poor postoperative outcomes were examined in many studies and include older age, female sex, smoking, increased tear size, preoperative fatty infiltration, preoperative shoulder stiffness, diabetes, workers’ compensation claim, decreased preoperative muscle strength, and concomitant procedures.
Multiple studies examined the effectiveness of various types of biological augmentation for RC treatment, including PRP, stem cells, and scaffolds. Laboratory studies tended to report favorable findings for PRP use, although the results of clinical studies are inconsistent. There is some evidence suggesting that PRP is beneficial for conservative management of RC tears, but there is less evidence for the use of PRP at the time of RC repair. Also, increased retears were found for massive tears following PRP use, which suggests that tear size may be influential. A few studies demonstrated fewer retears and good outcomes following the use of stem cells, although most of these studies did not include a control group. Several studies also demonstrated good outcomes for repairs with various types of grafts, including autografts, allografts, and bridging grafts; however, more research is needed to determine which of these specific grafts is superior to the others.
A large body of literature examined postoperative rehabilitation strategies. There is little to no evidence to support the use of continuous passive motion, supervised (vs unsupervised) therapy, and cryotherapy. There is conflicting evidence with regard to early versus delayed postoperative rehabilitation, which may in part be due to variation in the timing of rehabilitation among studies. However, there is some evidence suggesting that early rehabilitation may be beneficial for smaller tears but harmful for larger tears.
Standardization of outcome measurement is lacking in the literature. Only 63% of studies included measures of ROM; 65% evaluated tendon integrity; and 38% measured strength. Despite being ranked as having low quality, the most commonly used outcome measures include the Constant (61%), ASES (59%), and UCLA (35%) scores. The WORC, DASH, Shoulder Pain and Disability Index, and Simple Shoulder Test were reported to have the highest quality. The quality of operative and nonoperative randomized controlled trials involving RC disorders was found to be moderate (Jadad score, 3 of 5), suggesting that higher-quality trials are needed. Also, only 50% to 60% of randomized controlled trials adhered to the CONSORT criteria for standard reporting of randomized controlled trials. In conclusion, this summary of systematic reviews and meta-analyses on the RC provides surgeons with a single source of the most current literature.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the Ralph C. Wilson Jr Foundation. L.J.B. is a paid speaker/presenter for Arthrex, has received royalties from Zimmer Biomet, and has received hospitality payments from Prodigy Surgical Distribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Abdul-Wahab TA, Betancourt JP, Hassan F, et al. Initial treatment of complete rotator cuff tear and transition to surgical treatment: systematic review of the evidence. Muscles Ligaments Tendons J. 2016;6(1):35–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Abe T, Loenneke JP, Thiebaud RS, Loftin M. Morphological and functional relationships with ultrasound measured muscle thickness of the upper extremity and trunk. Ultrasound. 2014;22(4):229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ahmad Z, Wardale J, Brooks R, Henson F, Noorani A, Rushton N. Exploring the application of stem cells in tendon repair and regeneration. Arthroscopy. 2012;28(7):1018–1029. [DOI] [PubMed] [Google Scholar]
- 4. Ainsworth R, Lewis JS. Exercise therapy for the conservative management of full thickness tears of the rotator cuff: a systematic review. Br J Sports Med. 2007;41(4):200–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Andia I, Maffulli N. Muscle and tendon injuries: the role of biological interventions to promote and assist healing and recovery. Arthroscopy. 2015;31(5):999–1015. [DOI] [PubMed] [Google Scholar]
- 6. Archambault JM, Jelinsky SA, Lake SP, Hill AA, Glaser DL, Soslowsky LJ. Rat supraspinatus tendon expresses cartilage markers with overuse. J Orthop Res. 2007;25(5):617–624. [DOI] [PubMed] [Google Scholar]
- 7. Archer RS, Bayley JI, Archer CW, Ali SY. Cell and matrix changes associated with pathological calcification of the human rotator cuff tendons. J Anat. 1993;182(pt 1):1–11. [PMC free article] [PubMed] [Google Scholar]
- 8. Attia M, Scott A, Duchesnay A, et al. Alterations of overused supraspinatus tendon: a possible role of glycosaminoglycans and HARP/pleiotrophin in early tendon pathology. J Orthop Res. 2012;30(1):61–71. [DOI] [PubMed] [Google Scholar]
- 9. Audige L, Blum R, Muller AM, Flury M, Durchholz H. Complications following arthroscopic rotator cuff tear repair: a systematic review of terms and definitions with focus on shoulder stiffness. Orthop J Sports Med. 2015;3(6):2325967115587861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bank RA, TeKoppele JM, Oostingh G, Hazleman BL, Riley GP. Lysylhydroxylation and non-reducible crosslinking of human supraspinatus tendon collagen: changes with age and in chronic rotator cuff tendinitis. Ann Rheum Dis. 1999;58(1):35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Baombe JP. BET 2: is ultrasound a reliable way of detecting rotator cuff injuries of the shoulder? Emerg Med J. 2014;31(7):605–607. [DOI] [PubMed] [Google Scholar]
- 12. Baumgarten KM, Vidal AF, Wright RW. Rotator cuff repair rehabilitation: a level I and II systematic review. Sports Health. 2009;1(2):125–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Beaudreuil J, Nizard R, Thomas T, et al. Contribution of clinical tests to the diagnosis of rotator cuff disease: a systematic literature review. Joint Bone Spine. 2009;76(1):15–19. [DOI] [PubMed] [Google Scholar]
- 14. Beitzel K, Solovyova O, Cote MP, et al. The future role of mesenchymal stem cells in the management of shoulder disorders. Arthroscopy. 2013;29(10):1702–1711. [DOI] [PubMed] [Google Scholar]
- 15. Benson RT, McDonnell SM, Knowles HJ, Rees JL, Carr AJ, Hulley PA. Tendinopathy and tears of the rotator cuff are associated with hypoxia and apoptosis. J Bone Joint Surg Br. 2010;92(3):448–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Berckmans K, Maenhout AG, Matthijs L, Pieters L, Castelein B, Cools AM. The isokinetic rotator cuff strength ratios in overhead athletes: assessment and exercise effect. Phys Ther Sport. 2017;27:65–75. [DOI] [PubMed] [Google Scholar]
- 17. Bishop JY, Santiago-Torres JE, Rimmke N, Flanigan DC. Smoking predisposes to rotator cuff pathology and shoulder dysfunction: a systematic review. Arthroscopy. 2015;31(8):1598–1605. [DOI] [PubMed] [Google Scholar]
- 18. Blaine TA, Cote MA, Proto A, Mulcahey M, Lee FY, Bigliani LU. Interleukin-1beta stimulates stromal-derived factor-1alpha expression in human subacromial bursa. J Orthop Res. 2011;29(11):1695–1699. [DOI] [PubMed] [Google Scholar]
- 19. Blaine TA, Kim YS, Voloshin I, et al. The molecular pathophysiology of subacromial bursitis in rotator cuff disease. J Shoulder Elbow Surg. 2005;14(1)(suppl S):84S–89S. [DOI] [PubMed] [Google Scholar]
- 20. Bollier M, Shea K. Systematic review: what surgical technique provides the best outcome for symptomatic partial articular-sided rotator cuff tears? Iowa Orthop J. 2012;32:164–172. [PMC free article] [PubMed] [Google Scholar]
- 21. Braun C, Hanchard NC, Batterham AM, Handoll HH, Betthauser A. Prognostic models in adults undergoing physical therapy for rotator cuff disorders: systematic review. Phys Ther. 2016;96(7):961–971. [DOI] [PubMed] [Google Scholar]
- 22. Brown MJ, Pula DA, Kluczynski MA, Mashtare T, Bisson LJ. Does suture technique affect re-rupture in arthroscopic rotator cuff repair? A meta-analysis. Arthroscopy. 2015;31(8):1576–1582. [DOI] [PubMed] [Google Scholar]
- 23. Bury J, West M, Chamorro-Moriana G, Littlewood C. Effectiveness of scapula-focused approaches in patients with rotator cuff related shoulder pain: a systematic review and meta-analysis. Man Ther. 2016;25:35–42. [DOI] [PubMed] [Google Scholar]
- 24. Cai YZ, Zhang C, Lin XJ. Efficacy of platelet-rich plasma in arthroscopic repair of full-thickness rotator cuff tears: a meta-analysis. J Shoulder Elbow Surg. 2015;24(12):1852–1859. [DOI] [PubMed] [Google Scholar]
- 25. Caplan AI, Dennis JE. Mesenchymal stem cells as trophic mediators. J Cell Biochem. 2006;98(5):1076–1084. [DOI] [PubMed] [Google Scholar]
- 26. Chahal J, Mall N, MacDonald PB, et al. The role of subacromial decompression in patients undergoing arthroscopic repair of full-thickness tears of the rotator cuff: a systematic review and meta-analysis. Arthroscopy. 2012;28(5):720–727. [DOI] [PubMed] [Google Scholar]
- 27. Chahal J, Van Thiel GS, Mall N, et al. The role of platelet-rich plasma in arthroscopic rotator cuff repair: a systematic review with quantitative synthesis. Arthroscopy. 2012;28(11):1718–1727. [DOI] [PubMed] [Google Scholar]
- 28. Chan K, MacDermid JC, Hoppe DJ, et al. Delayed versus early motion after arthroscopic rotator cuff repair: a meta-analysis. J Shoulder Elbow Surg. 2014;23(11):1631–1639. [DOI] [PubMed] [Google Scholar]
- 29. Chang KV, Hung CY, Han DS, Chen WS, Wang TG, Chien KL. Early versus delayed passive range of motion exercise for arthroscopic rotator cuff repair: a meta-analysis of randomized controlled trials. Am J Sports Med. 2015;43(5):1265–1273. [DOI] [PubMed] [Google Scholar]
- 30. Chen L, Peng K, Zhang D, Peng J, Xing F, Xiang Z. Rehabilitation protocol after arthroscopic rotator cuff repair: early versus delayed motion. Int J Clin Exp Med. 2015;8(6):8329–8338. [PMC free article] [PubMed] [Google Scholar]
- 31. Chen M, Xu W, Dong Q, Huang Q, Xie Z, Mao Y. Outcomes of single-row versus double-row arthroscopic rotator cuff repair: a systematic review and meta-analysis of current evidence. Arthroscopy. 2013;29(8):1437–1449. [DOI] [PubMed] [Google Scholar]
- 32. Coghlan JA, Buchbinder R, Green S, Johnston RV, Bell SN. Surgery for rotator cuff disease. Cochrane Database Syst Rev. 2008;1:CD005619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Curtis L. Nutritional research may be useful in treating tendon injuries. Nutrition. 2016;32(6):617–619. [DOI] [PubMed] [Google Scholar]
- 34. Dabija DI, Gao C, Edwards TL, Kuhn JE, Jain NB. Genetic and familial predisposition to rotator cuff disease: a systematic review. J Shoulder Elbow Surg. 2017;26(6):1103–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol. 2009;192(6):1701–1707. [DOI] [PubMed] [Google Scholar]
- 36. de Moraes VY, Godin K, Dos Santos JB, Faloppa F, Bhandari M, Belloti JC. Influence of compensation status on time off work after carpal tunnel release and rotator cuff surgery: a meta-analysis. Patient Saf Surg. 2013;7(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. de Vos RJ, Windt J, Weir A. Strong evidence against platelet-rich plasma injections for chronic lateral epicondylar tendinopathy: a systematic review. Br J Sports Med. 2014;48(12):952–956. [DOI] [PubMed] [Google Scholar]
- 38. Dean BJ, Franklin SL, Carr AJ. A systematic review of the histological and molecular changes in rotator cuff disease. Bone Joint Res. 2012;1(7):158–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. DeHaan AM, Axelrad TW, Kaye E, Silvestri L, Puskas B, Foster TE. Does double-row rotator cuff repair improve functional outcome of patients compared with single-row technique? A systematic review. Am J Sports Med. 2012;40(5):1176–1185. [DOI] [PubMed] [Google Scholar]
- 40. Denard PJ, Ladermann A, Burkhart SS. Prevention and management of stiffness after arthroscopic rotator cuff repair: systematic review and implications for rotator cuff healing. Arthroscopy. 2011;27(6):842–848. [DOI] [PubMed] [Google Scholar]
- 41. Dickinson RN, Kuhn JE, Bergner JL, Rizzone KH. A systematic review of cost-effective treatment of postoperative rotator cuff repairs. J Shoulder Elbow Surg. 2017;26(5):915–922. [DOI] [PubMed] [Google Scholar]
- 42. DiSilvestro KJ, Santoro AJ, Tjoumakaris FP, Levicoff EA, Freedman KB. When can I drive after orthopaedic surgery? A systematic review. Clin Orthop Relat Res. 2016;474(12):2557–2570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Downie BK, Miller BS. Treatment of rotator cuff tears in older individuals: a systematic review. J Shoulder Elbow Surg. 2012;21(9):1255–1261. [DOI] [PubMed] [Google Scholar]
- 44. Du Plessis M, Eksteen E, Jenneker A, et al. The effectiveness of continuous passive motion on range of motion, pain and muscle strength following rotator cuff repair: a systematic review. Clin Rehabil. 2011;25(4):291–302. [DOI] [PubMed] [Google Scholar]
- 45. Duquin TR, Buyea C, Bisson LJ. Which method of rotator cuff repair leads to the highest rate of structural healing? A systematic review. Am J Sports Med. 2010;38(4):835–841. [DOI] [PubMed] [Google Scholar]
- 46. Edouard P, Samozino P, Julia M, et al. Reliability of isokinetic assessment of shoulder-rotator strength: a systematic review of the effect of position. J Sport Rehabil. 2011;20(3):367–383. [DOI] [PubMed] [Google Scholar]
- 47. Edwards PK, Ebert JR, Littlewood C, Ackland T, Wang A. A systematic review of EMG studies in normal shoulders to inform postoperative rehabilitation following rotator cuff repair. J Orthop Sports Phys Ther. 2017;47(12):931–944. [DOI] [PubMed] [Google Scholar]
- 48. Eljabu W, Klinger HM, von Knoch M. The natural history of rotator cuff tears: a systematic review. Arch Orthop Trauma Surg. 2015;135(8):1055–1061. [DOI] [PubMed] [Google Scholar]
- 49. Erickson J, Lavery K, Monica J, Gatt C, Dhawan A. Surgical treatment of symptomatic superior labrum anterior-posterior tears in patients older than 40 years: a systematic review. Am J Sports Med. 2015;43(5):1274–1282. [DOI] [PubMed] [Google Scholar]
- 50. Familiari F, Gonzalez-Zapata A, Ianno B, Galasso O, Gasparini G, McFarland EG. Is acromioplasty necessary in the setting of full-thickness rotator cuff tears? A systematic review. J Orthop Traumatol. 2015;16(3):167–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ferguson DP, Lewington MR, Smith TD, Wong IH. Graft utilization in the augmentation of large-to-massive rotator cuff repairs: a systematic review. Am J Sports Med. 2016;44(11):2984–2992. [DOI] [PubMed] [Google Scholar]
- 52. Fermont AJ, Wolterbeek N, Wessel RN, Baeyens JP, de Bie RA. Prognostic factors for successful recovery after arthroscopic rotator cuff repair: a systematic literature review. J Orthop Sports Phys Ther. 2014;44(3):153–163. [DOI] [PubMed] [Google Scholar]
- 53. Filardo G, Di Matteo B, Kon E, Merli G, Marcacci M. Platelet-rich plasma in tendon-related disorders: results and indications. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):1984–1999. [DOI] [PubMed] [Google Scholar]
- 54. Fu CJ, Sun JB, Bi ZG, Wang XM, Yang CL. Evaluation of platelet-rich plasma and fibrin matrix to assist in healing and repair of rotator cuff injuries: a systematic review and meta-analysis. Clin Rehabil. 2017;31(2):158–172. [DOI] [PubMed] [Google Scholar]
- 55. Fuchs B, Zumstein M, Regenfelder F, et al. Upregulation of alpha-skeletal muscle actin and myosin heavy polypeptide gene products in degenerating rotator cuff muscles. J Orthop Res. 2008;26(7):1007–1011. [DOI] [PubMed] [Google Scholar]
- 56. Gallagher BP, Bishop ME, Tjoumakaris FP, Freedman KB. Early versus delayed rehabilitation following arthroscopic rotator cuff repair: a systematic review. Phys Sportsmed. 2015;43(2):178–187. [DOI] [PubMed] [Google Scholar]
- 57. Gigante A, Marinelli M, Chillemi C, Greco F. Fibrous cartilage in the rotator cuff: a pathogenetic mechanism of tendon tear? J Shoulder Elbow Surg. 2004;13(3):328–332. [DOI] [PubMed] [Google Scholar]
- 58. Gismervik SO, Drogset JO, Granviken F, Ro M, Leivseth G. Physical examination tests of the shoulder: a systematic review and meta-analysis of diagnostic test performance. BMC Musculoskelet Disord. 2017;18(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Gombera MM, Sekiya JK. Rotator cuff tear and glenohumeral instability: a systematic review. Clin Orthop Relat Res. 2014;472(8):2448–2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Gotoh M, Hamada K, Yamakawa H, et al. Interleukin-1-induced glenohumeral synovitis and shoulder pain in rotator cuff diseases. J Orthop Res. 2002;20(6):1365–1371. [DOI] [PubMed] [Google Scholar]
- 61. Gotoh M, Hamada K, Yamakawa H, et al. Perforation of rotator cuff increases interleukin 1beta production in the synovium of glenohumeral joint in rotator cuff diseases. J Rheumatol. 2000;27(12):2886–2892. [PubMed] [Google Scholar]
- 62. Gotoh M, Hamada K, Yamakawa H, Inoue A, Fukuda H. Increased substance P in subacromial bursa and shoulder pain in rotator cuff diseases. J Orthop Res. 1998;16(5):618–621. [DOI] [PubMed] [Google Scholar]
- 63. Gotoh M, Hamada K, Yamakawa H, Tomonaga A, Inoue A, Fukuda H. Significance of granulation tissue in torn supraspinatus insertions: an immunohistochemical study with antibodies against interleukin-1 beta, cathepsin D, and matrix metalloprotease-1. J Orthop Res. 1997;15(1):33–39. [DOI] [PubMed] [Google Scholar]
- 64. Guevara-Alvarez A, Schmitt A, Russell RP, Imhoff AB, Buchmann S. Growth factor delivery vehicles for tendon injuries: mesenchymal stem cells and platelet rich plasma. Muscles Ligaments Tendons J. 2014;4(3):378–385. [PMC free article] [PubMed] [Google Scholar]
- 65. Gurnani N, van Deurzen DFP, van den Bekerom MPJ. Shoulder-specific outcomes 1 year after nontraumatic full-thickness rotator cuff repair: a systematic literature review and meta-analysis. Shoulder Elbow. 2017;9(4):247–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Hanchard NC, Lenza M, Handoll HH, Takwoingi Y. Physical tests for shoulder impingements and local lesions of bursa, tendon or labrum that may accompany impingement. Cochrane Database Syst Rev. 2013;(4):CD007427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Harris JD, Frank JM, Jordan MA, et al. Return to sport following shoulder surgery in the elite pitcher: a systematic review. Sports Health. 2013;5(4):367–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Hawk C, Minkalis AL, Khorsan R, et al. Systematic review of nondrug, nonsurgical treatment of shoulder conditions. J Manipulative Physiol Ther. 2017;40(5):293–319. [DOI] [PubMed] [Google Scholar]
- 69. Hegedus EJ, Cook C, Brennan M, Wyland D, Garrison JC, Driesner D. Vascularity and tendon pathology in the rotator cuff: a review of literature and implications for rehabilitation and surgery. Br J Sports Med. 2010;44(12):838–847. [DOI] [PubMed] [Google Scholar]
- 70. Hegedus EJ, Goode A, Campbell S, et al. Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. Br J Sports Med. 2008;42(2):80–92. [DOI] [PubMed] [Google Scholar]
- 71. Hein J, Reilly JM, Chae J, Maerz T, Anderson K. Retear rates after arthroscopic single-row, double-row, and suture bridge rotator cuff repair at a minimum of 1 year of imaging follow-up: a systematic review. Arthroscopy. 2015;31(11):2274–2281. [DOI] [PubMed] [Google Scholar]
- 72. Henry P, Wasserstein D, Park S, et al. Arthroscopic repair for chronic massive rotator cuff tears: a systematic review. Arthroscopy. 2015;31(12):2472–2480. [DOI] [PubMed] [Google Scholar]
- 73. Hermans J, Luime JJ, Meuffels DE, Reijman M, Simel DL, Bierma-Zeinstra SM. Does this patient with shoulder pain have rotator cuff disease? The Rational Clinical Examination systematic review. JAMA. 2013;310(8):837–847. [DOI] [PubMed] [Google Scholar]
- 74. Horner NS, de Sa D, Heaven S, et al. Indications and outcomes of shoulder arthroscopy after shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25(3):510–518. [DOI] [PubMed] [Google Scholar]
- 75. Houck DA, Kraeutler MJ, Schuette HB, McCarty EC, Bravman JT. Early versus delayed motion after rotator cuff repair. Am J Sports Med. 2017;45(12):2911–2915. [DOI] [PubMed] [Google Scholar]
- 76. Huang H, Grant JA, Miller BS, Mirza FM, Gagnier JJ. A systematic review of the psychometric properties of patient-reported outcome instruments for use in patients with rotator cuff disease. Am J Sports Med. 2015;43(10):2572–2582. [DOI] [PubMed] [Google Scholar]
- 77. Huang R, Wang S, Wang Y, Qin X, Sun Y. Systematic review of all-arthroscopic versus mini-open repair of rotator cuff tears: a meta-analysis. Sci Rep. 2016;6:22857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Hughes PC, Taylor NF, Green RA. Most clinical tests cannot accurately diagnose rotator cuff pathology: a systematic review. Aust J Physiother. 2008;54(3):159–170. [DOI] [PubMed] [Google Scholar]
- 79. Huisstede BM, Koes BW, Gebremariam L, Keijsers E, Verhaar JA. Current evidence for effectiveness of interventions to treat rotator cuff tears. Man Ther. 2011;16(3):217–230. [DOI] [PubMed] [Google Scholar]
- 80. Hyvonen P, Melkko J, Lehto VP, Jalovaara P. Involvement of the subacromial bursa in impingement syndrome of the shoulder as judged by expression of tenascin-C and histopathology. J Bone Joint Surg Br. 2003;85(2):299–305. [DOI] [PubMed] [Google Scholar]
- 81. Imam MA, Holton J, Horriat S, et al. A systematic review of the concept and clinical applications of bone marrow aspirate concentrate in tendon pathology. SICOT J. 2017;3:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ishii H, Brunet JA, Welsh RP, Uhthoff HK. “Bursal reactions” in rotator cuff tearing, the impingement syndrome, and calcifying tendinitis. J Shoulder Elbow Surg. 1997;6(2):131–136. [DOI] [PubMed] [Google Scholar]
- 83. Jacob J, Eisemon E, Sheibani-Rad S, Patel A, Jacob T, Choueka J. Matrix metalloproteinase levels as a marker for rotator cuff tears. Orthopedics. 2012;35(4):e474–e478. [DOI] [PubMed] [Google Scholar]
- 84. Jadad AR, Cook DJ, Browman GP. A guide to interpreting discordant systematic reviews. CMAJ. 1997;156(10):1411–1416. [PMC free article] [PubMed] [Google Scholar]
- 85. Jelinsky SA, Lake SP, Archambault JM, Soslowsky LJ. Gene expression in rat supraspinatus tendon recovers from overuse with rest. Clin Orthop Relat Res. 2008;466(7):1612–1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Ji X, Bi C, Wang F, Wang Q. Arthroscopic versus mini-open rotator cuff repair: an up-to-date meta-analysis of randomized controlled trials. Arthroscopy. 2015;31(1):118–124. [DOI] [PubMed] [Google Scholar]
- 87. Joseph M, Maresh CM, McCarthy MB, et al. Histological and molecular analysis of the biceps tendon long head post-tenotomy. J Orthop Res. 2009;27(10):1379–1385. [DOI] [PubMed] [Google Scholar]
- 88. Kamioka H, Tsutani K, Mutoh Y, et al. A systematic review of nonrandomized controlled trials on the curative effects of aquatic exercise. Int J Gen Med. 2011;4:239–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Karahan S, Kincaid SA, Baird AN, Kammermann JR. Distribution of beta-endorphin and substance P in the shoulder joint of the dog before and after a low impact exercise programme. Anat Histol Embryol. 2002;31(2):72–77. [DOI] [PubMed] [Google Scholar]
- 90. Katthagen JC, Bucci G, Moatshe G, Tahal DS, Millett PJ. Improved outcomes with arthroscopic repair of partial-thickness rotator cuff tears: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):113–124. [DOI] [PubMed] [Google Scholar]
- 91. Kelly AM, Fessell D. Ultrasound compared with magnetic resonance imaging for the diagnosis of rotator cuff tears: a critically appraised topic. Semin Roentgenol. 2009;44(3):196–200. [DOI] [PubMed] [Google Scholar]
- 92. Kemp KA, Sheps DM, Luciak-Corea C, Styles-Tripp F, Buckingham J, Beaupre LA. Systematic review of rotator cuff tears in workers’ compensation patients. Occup Med (Lond). 2011;61(8):556–562. [DOI] [PubMed] [Google Scholar]
- 93. Khair MM, Lehman J, Tsouris N, Gulotta LV. A systematic review of preoperative fatty infiltration and rotator cuff outcomes. HSS J. 2016;12(2):170–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Kim YS, Bigliani LU, Fujisawa M, et al. Stromal cell-derived factor 1 (SDF-1, CXCL12) is increased in subacromial bursitis and downregulated by steroid and nonsteroidal anti-inflammatory agents. J Orthop Res. 2006;24(8):1756–1764. [DOI] [PubMed] [Google Scholar]
- 95. Klouche S, Lefevre N, Herman S, Gerometta A, Bohu Y. Return to sport after rotator cuff tear repair: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1877–1887. [DOI] [PubMed] [Google Scholar]
- 96. Kluczynski MA, Bisson LJ, Marzo JM. Does body mass index affect outcomes of ambulatory knee and shoulder surgery? Arthroscopy. 2014;30(7):856–865. [DOI] [PubMed] [Google Scholar]
- 97. Kluczynski MA, Isenburg MM, Marzo JM, Bisson LJ. Does early versus delayed active range of motion affect rotator cuff healing after surgical repair? A systematic review and meta-analysis. Am J Sports Med. 2016;44(3):785–791. [DOI] [PubMed] [Google Scholar]
- 98. Kluczynski MA, Nayyar S, Marzo JM, Bisson LJ. Early versus delayed passive range of motion after rotator cuff repair: a systematic review and meta-analysis. Am J Sports Med. 2015;43(8):2057–2063. [DOI] [PubMed] [Google Scholar]
- 99. Ko JY, Wang FS, Huang HY, Wang CJ, Tseng SL, Hsu C. Increased IL-1beta expression and myofibroblast recruitment in subacromial bursa is associated with rotator cuff lesions with shoulder stiffness. J Orthop Res. 2008;26(8):1090–1097. [DOI] [PubMed] [Google Scholar]
- 100. Kumagai J, Sarkar K, Uhthoff HK. The collagen types in the attachment zone of rotator cuff tendons in the elderly: an immunohistochemical study. J Rheumatol. 1994;21(11):2096–2100. [PubMed] [Google Scholar]
- 101. Ladermann A, Denard PJ, Burkhart SS. Management of failed rotator cuff repair: a systematic review. J ISAKOS. 2016;1(1):32–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Ladermann A, Denard PJ, Burkhart SS. Revision arthroscopic rotator cuff repair: systematic review and authors’ preferred surgical technique. Arthroscopy. 2012;28(8):1160–1169. [DOI] [PubMed] [Google Scholar]
- 103. Lakemeier S, Reichelt JJ, Patzer T, Fuchs-Winkelmann S, Paletta JR, Schofer MD. The association between retraction of the torn rotator cuff and increasing expression of hypoxia inducible factor 1alpha and vascular endothelial growth factor expression: an immunohistological study. BMC Musculoskelet Disord. 2010;11:230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Lakemeier S, Reichelt JJ, Timmesfeld N, Fuchs-Winkelmann S, Paletta JR, Schofer MD. The relevance of long head biceps degeneration in the presence of rotator cuff tears. BMC Musculoskelet Disord. 2010;11:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Lakemeier S, Schwuchow SA, Peterlein CD, et al. Expression of matrix metalloproteinases 1, 3, and 9 in degenerated long head biceps tendon in the presence of rotator cuff tears: an immunohistological study. BMC Musculoskelet Disord. 2010;11:271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Lambers Heerspink FO, Dorrestijn O, van Raay JJ, Diercks RL. Specific patient-related prognostic factors for rotator cuff repair: a systematic review. J Shoulder Elbow Surg. 2014;23(7):1073–1080. [DOI] [PubMed] [Google Scholar]
- 107. Lazarides AL, Alentorn-Geli E, Choi JH, et al. Rotator cuff tears in young patients: a different disease than rotator cuff tears in elderly patients. J Shoulder Elbow Surg. 2015;24(11):1834–1843. [DOI] [PubMed] [Google Scholar]
- 108. Lehmann LJ, Schollmeyer A, Stoeve J, Scharf HP. Biochemical analysis of the synovial fluid of the shoulder joint in patients with and without rotator cuff tears [in German]. Z Orthop Unfall. 2010;148(1):90–94. [DOI] [PubMed] [Google Scholar]
- 109. Lenza M, Buchbinder R, Takwoingi Y, Johnston RV, Hanchard NC, Faloppa F. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev. 2013;(9):CD009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Leroux T, Chahal J, Wasserstein D, Verma NN, Romeo AA. A systematic review and meta-analysis comparing clinical outcomes after concurrent rotator cuff repair and long head biceps tenodesis or tenotomy. Sports Health. 2015;7(4):303–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Levy DM, Abrams GD, Harris JD, Bach BR, Jr, Nicholson GP, Romeo AA. Rotator cuff tears after total shoulder arthroplasty in primary osteoarthritis: a systematic review. Int J Shoulder Surg. 2016;10(2):78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Lewington MR, Ferguson DP, Smith TD, Burks R, Coady C, Wong IH. Graft utilization in the bridging reconstruction of irreparable rotator cuff tears: a systematic review. Am J Sports Med. 2017;45(13):3149–3157. [DOI] [PubMed] [Google Scholar]
- 113. Li X, Xu CP, Hou YL, Song JQ, Cui Z, Yu B. Are platelet concentrates an ideal biomaterial for arthroscopic rotator cuff repair? A meta-analysis of randomized controlled trials. Arthroscopy. 2014;30(11):1483–1490. [DOI] [PubMed] [Google Scholar]
- 114. Lindley K, Jones GL. Outcomes of arthroscopic versus open rotator cuff repair: a systematic review of the literature. Am J Orthop (Belle Mead NJ). 2010;39(12):592–600. [PubMed] [Google Scholar]
- 115. Littlewood C, Bateman M, Clark D, et al. Rehabilitation following rotator cuff repair: a systematic review. Shoulder Elbow. 2015;7(2):115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Lo IK, Boorman R, Marchuk L, Hollinshead R, Hart DA, Frank CB. Matrix molecule mRNA levels in the bursa and rotator cuff of patients with full-thickness rotator cuff tears. Arthroscopy. 2005;21(6):645–651. [DOI] [PubMed] [Google Scholar]
- 117. Lo IK, Marchuk LL, Hollinshead R, Hart DA, Frank CB. Matrix metalloproteinase and tissue inhibitor of matrix metalloproteinase mRNA levels are specifically altered in torn rotator cuff tendons. Am J Sports Med. 2004;32(5):1223–1229. [DOI] [PubMed] [Google Scholar]
- 118. Longo UG, Franceschetti E, Petrillo S, Maffulli N, Denaro V. Latissimus dorsi tendon transfer for massive irreparable rotator cuff tears: a systematic review. Sports Med Arthrosc. 2011;19(4):428–437. [DOI] [PubMed] [Google Scholar]
- 119. Longo UG, Lamberti A, Maffulli N, Denaro V. Tendon augmentation grafts: a systematic review. Br Med Bull. 2010;94:165–188. [DOI] [PubMed] [Google Scholar]
- 120. Longo UG, Saris D, Poolman RW, Berton A, Denaro V. Instruments to assess patients with rotator cuff pathology: a systematic review of measurement properties. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):1961–1970. [DOI] [PubMed] [Google Scholar]
- 121. Lundgreen K, Lian OB, Engebretsen L, Scott A. Tenocyte apoptosis in the torn rotator cuff: a primary or secondary pathological event? Br J Sports Med. 2011;45(13):1035–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. MacKechnie MA, Chahal J, Wasserstein D, Theodoropoulos JS, Henry P, Dwyer T. Repair of full-thickness rotator cuff tears in patients aged younger than 55 years. Arthroscopy. 2014;30(10):1366–1371. [DOI] [PubMed] [Google Scholar]
- 123. Maffulli N, Longo UG, Loppini M, Berton A, Spiezia F, Denaro V. Tissue engineering for rotator cuff repair: an evidence-based systematic review. Stem Cells Int. 2012;2012:418086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Makhni EC, Steinhaus ME, Morrow ZS, et al. Outcomes assessment in rotator cuff pathology: what are we measuring? J Shoulder Elbow Surg. 2015;24(12):2008–2015. [DOI] [PubMed] [Google Scholar]
- 125. Mall NA, Chahal J, Heard WM, et al. Outcomes of arthroscopic and open surgical repair of isolated subscapularis tendon tears. Arthroscopy. 2012;28(9):1306–1314. [DOI] [PubMed] [Google Scholar]
- 126. Mall NA, Lee AS, Chahal J, et al. An evidenced-based examination of the epidemiology and outcomes of traumatic rotator cuff tears. Arthroscopy. 2013;29(2):366–376. [DOI] [PubMed] [Google Scholar]
- 127. Mall NA, Lee AS, Chahal J, et al. Transosseous-equivalent rotator cuff repair: a systematic review on the biomechanical importance of tying the medial row. Arthroscopy. 2013;29(2):377–386. [DOI] [PubMed] [Google Scholar]
- 128. Marik TL, Roll SC. Effectiveness of occupational therapy interventions for musculoskeletal shoulder conditions: a systematic review. Am J Occup Ther. 2017;71(1):7101180020p1-7101180020p11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Marx RG, Koulouvaris P, Chu SK, Levy BA. Indications for surgery in clinical outcome studies of rotator cuff repair. Clin Orthop Relat Res. 2009;467(2):450–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Mascarenhas R, Chalmers PN, Sayegh ET, et al. Is double-row rotator cuff repair clinically superior to single-row rotator cuff repair: a systematic review of overlapping meta-analyses. Arthroscopy. 2014;30(9):1156–1165. [DOI] [PubMed] [Google Scholar]
- 131. Mazuquin BF, Wright AC, Russell S, Monga P, Selfe J, Richards J. Effectiveness of early compared with conservative rehabilitation for patients having rotator cuff repair surgery: an overview of systematic reviews. Br J Sports Med. 2018;52(2):111–121. [DOI] [PubMed] [Google Scholar]
- 132. McCormick F, Cvetanovich GL, Kim JM, et al. An assessment of the quality of rotator cuff randomized controlled trials: utilizing the Jadad score and CONSORT criteria. J Shoulder Elbow Surg. 2013;22(9):1180–1185. [DOI] [PubMed] [Google Scholar]
- 133. McElvany MD, McGoldrick E, Gee AO, Neradilek MB, Matsen FA., 3rd Rotator cuff repair: published evidence on factors associated with repair integrity and clinical outcome. Am J Sports Med. 2015;43(2):491–500. [DOI] [PubMed] [Google Scholar]
- 134. McGarvey C, Harb Z, Smith C, Houghton R, Corbett S, Ajuied A. Diagnosis of rotator cuff tears using 3-Tesla MRI versus 3-Tesla MRA: a systematic review and meta-analysis. Skeletal Radiol. 2016;45(2):251–261. [DOI] [PubMed] [Google Scholar]
- 135. Millar NL, Reilly JH, Kerr SC, et al. Hypoxia: a critical regulator of early human tendinopathy. Ann Rheum Dis. 2012;71(2):302–310. [DOI] [PubMed] [Google Scholar]
- 136. Millar NL, Wei AQ, Molloy TJ, Bonar F, Murrell GA. Cytokines and apoptosis in supraspinatus tendinopathy. J Bone Joint Surg Br. 2009;91(3):417–424. [DOI] [PubMed] [Google Scholar]
- 137. Millar NL, Wei AQ, Molloy TJ, Bonar F, Murrell GA. Heat shock protein and apoptosis in supraspinatus tendinopathy. Clin Orthop Relat Res. 2008;466(7):1569–1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Millett PJ, Warth RJ, Dornan GJ, Lee JT, Spiegl UJ. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg. 2014;23(4):586–597. [DOI] [PubMed] [Google Scholar]
- 139. Miranda I, Sanchez-Alepuz E, Lucas FJ, Carratala V, Gonzalez-Jofre CA. Use of platelet-rich plasma in the treatment of rotator cuff pathology: what has been scientifically proven? Rev Esp Cir Ortop Traumatol. 2017;61(4):249–258. [DOI] [PubMed] [Google Scholar]
- 140. Molloy TJ, Kemp MW, Wang Y, Murrell GA. Microarray analysis of the tendinopathic rat supraspinatus tendon: glutamate signaling and its potential role in tendon degeneration. J Appl Physiol (1985). 2006;101(6):1702–1709. [DOI] [PubMed] [Google Scholar]
- 141. Moraes VY, Lenza M, Tamaoki MJ, Faloppa F, Belloti JC. Platelet-rich therapies for musculoskeletal soft tissue injuries. Cochrane Database Syst Rev. 2014;(4):CD010071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Morse K, Davis AD, Afra R, Kaye EK, Schepsis A, Voloshin I. Arthroscopic versus mini-open rotator cuff repair: a comprehensive review and meta-analysis. Am J Sports Med. 2008;36(9):1824–1828. [DOI] [PubMed] [Google Scholar]
- 143. Mukovozov I, Byun S, Farrokhyar F, Wong I. Time to surgery in acute rotator cuff tear: a systematic review. Bone Joint Res. 2013;2(7):122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Muller AM, Flury M, Alsayed HN, Audige L. Influence of patient and diagnostic parameters on reported retear rates after arthroscopic rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2089–2099. [DOI] [PubMed] [Google Scholar]
- 145. Namdari S, Voleti P, Baldwin K, Glaser D, Huffman GR. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J Bone Joint Surg Am. 2012;94(10):891–898. [DOI] [PubMed] [Google Scholar]
- 146. Nho SJ, Shindle MK, Sherman SL, Freedman KB, Lyman S, MacGillivray JD. Systematic review of arthroscopic rotator cuff repair and mini-open rotator cuff repair. J Bone Joint Surg Am. 2007;89(suppl 3):127–136. [DOI] [PubMed] [Google Scholar]
- 147. Nho SJ, Slabaugh MA, Seroyer ST, et al. Does the literature support double-row suture anchor fixation for arthroscopic rotator cuff repair? A systematic review comparing double-row and single-row suture anchor configuration. Arthroscopy. 2009;25(11):1319–1328. [DOI] [PubMed] [Google Scholar]
- 148. Nixon AJ, Watts AE, Schnabel LV. Cell- and gene-based approaches to tendon regeneration. J Shoulder Elbow Surg. 2012;21(2):278–294. [DOI] [PubMed] [Google Scholar]
- 149. Nwachukwu BU, Schairer WW, Bernstein JL, Dodwell ER, Marx RG, Allen AA. Cost-effectiveness analyses in orthopaedic sports medicine: a systematic review. Am J Sports Med. 2015;43(6):1530–1537. [DOI] [PubMed] [Google Scholar]
- 150. Obaid H, Connell D. Cell therapy in tendon disorders: what is the current evidence? Am J Sports Med. 2010;38(10):2123–2132. [DOI] [PubMed] [Google Scholar]
- 151. Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Indications for rotator cuff repair: a systematic review. Clin Orthop Relat Res. 2007;455:52–63. [DOI] [PubMed] [Google Scholar]
- 152. Oliva F, Zocchi L, Codispoti A, et al. Transglutaminases expression in human supraspinatus tendon ruptures and in mouse tendons. Biochem Biophys Res Commun. 2009;379(4):887–891. [DOI] [PubMed] [Google Scholar]
- 153. Ono Y, Davalos Herrera DA, Woodmass JM, Boorman RS, Thornton GM, Lo IK. Can grafts provide superior tendon healing and clinical outcomes after rotator cuff repairs? A meta-analysis. Orthop J Sports Med. 2016;4(12):23259 67116674191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Ono Y, Davalos Herrera DA, Woodmass JM, Boorman RS, Thornton GM, Lo IK. Graft augmentation versus bridging for large to massive rotator cuff tears: a systematic review. Arthroscopy. 2017;33(3):673–680. [DOI] [PubMed] [Google Scholar]
- 155. Ono Y, Woodmass JM, Bois AJ, Boorman RS, Thornton GM, Lo IK. Arthroscopic repair of articular surface partial-thickness rotator cuff tears: transtendon technique versus repair after completion of the tear—a meta-analysis. Adv Orthop. 2016;2016:7468054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Osawa T, Shinozaki T, Takagishi K. Multivariate analysis of biochemical markers in synovial fluid from the shoulder joint for diagnosis of rotator cuff tears. Rheumatol Int. 2005;25(6):436–441. [DOI] [PubMed] [Google Scholar]
- 157. Osti L, Buda M, Buono AD, Osti R, Massari L. Clinical evidence in the treatment of rotator cuff tears with hyaluronic acid. Muscles Ligaments Tendons J. 2015;5(4):270–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Ottenheijm RP, Jansen MJ, Staal JB, et al. Accuracy of diagnostic ultrasound in patients with suspected subacromial disorders: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2010;91(10):1616–1625. [DOI] [PubMed] [Google Scholar]
- 159. Page MJ, Green S, McBain B, et al. Manual therapy and exercise for rotator cuff disease. Cochrane Database Syst Rev. 2016;(6):CD012224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Page MJ, McKenzie JE, Green SE, et al. Core domain and outcome measurement sets for shoulder pain trials are needed: systematic review of physical therapy trials. J Clin Epidemiol. 2015;68(11):1270–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Panni AS, Milano G, Lucania L, Fabbriciani C, Logroscino CA. Histological analysis of the coracoacromial arch: correlation between age-related changes and rotator cuff tears. Arthroscopy. 1996;12(5):531–540. [DOI] [PubMed] [Google Scholar]
- 162. Papalia R, Franceschi F, Del Buono A, Maffulli N, Denaro V. Results of surgical management of symptomatic shoulders with partial thickness tears of the rotator cuff. Br Med Bull. 2011;99:141–154. [DOI] [PubMed] [Google Scholar]
- 163. Papalia R, Franceschi F, Vasta S, Gallo A, Maffulli N, Denaro V. Shoulder stiffness and rotator cuff repair. Br Med Bull. 2012;104:163–174. [DOI] [PubMed] [Google Scholar]
- 164. Papalia R, Franceschi F, Zampogna B, D’Adamio S, Maffulli N, Denaro V. Augmentation techniques for rotator cuff repair. Br Med Bull. 2013;105:107–138. [DOI] [PubMed] [Google Scholar]
- 165. Papalia R, Tecame A, Torre G, Narbona P, Maffulli N, Denaro V. Rugby and shoulder trauma: a systematic review. Transl Med UniSa. 2015;12:5–13. [PMC free article] [PubMed] [Google Scholar]
- 166. Pas HI, Moen MH, Haisma HJ, Winters M. No evidence for the use of stem cell therapy for tendon disorders: a systematic review. Br J Sports Med. 2017;51(13):996–1002. [DOI] [PubMed] [Google Scholar]
- 167. Pauly S, Gerhardt C, Chen J, Scheibel M. Single versus double-row repair of the rotator cuff: does double-row repair with improved anatomical and biomechanical characteristics lead to better clinical outcome? Knee Surg Sports Traumatol Arthrosc. 2010;18(12):1718–1729. [DOI] [PubMed] [Google Scholar]
- 168. Pedowitz RA, Higashigawa K, Nguyen V. The “50% rule” in arthroscopic and orthopaedic surgery. Arthroscopy. 2011;27(11):1584–1587. [DOI] [PubMed] [Google Scholar]
- 169. Perry SM, McIlhenny SE, Hoffman MC, Soslowsky LJ. Inflammatory and angiogenic mRNA levels are altered in a supraspinatus tendon overuse animal model. J Shoulder Elbow Surg. 2005;14(1)(suppl S):79S–83S. [DOI] [PubMed] [Google Scholar]
- 170. Pers YM, Ruiz M, Noel D, Jorgensen C. Mesenchymal stem cells for the management of inflammation in osteoarthritis: state of the art and perspectives. Osteoarthritis Cartilage. 2015;23(11):2027–2035. [DOI] [PubMed] [Google Scholar]
- 171. Perser K, Godfrey D, Bisson L. Meta-analysis of clinical and radiographic outcomes after arthroscopic single-row versus double-row rotator cuff repair. Sports Health. 2011;3(3):268–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Plate JF, Haubruck P, Walters J, et al. Rotator cuff injuries in professional and recreational athletes. J Surg Orthop Adv. 2013;22(2):134–142. [DOI] [PubMed] [Google Scholar]
- 173. Prasathaporn N, Kuptniratsaikul S, Kongrukgreatiyos K. Single-row repair versus double-row repair of full-thickness rotator cuff tears. Arthroscopy. 2011;27(7):978–985. [DOI] [PubMed] [Google Scholar]
- 174. Pugh S, Callaghan M, Ferguson C. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 1: which is the best clinical test for diagnosing a full thickness rotator cuff tear? Emerg Med J. 2009;26(12):881. [DOI] [PubMed] [Google Scholar]
- 175. Raman J, Walton D, MacDermid JC, Athwal GS. Predictors of outcomes after rotator cuff repair—a meta-analysis. J Hand Ther. 2017;30(3):276–292. [DOI] [PubMed] [Google Scholar]
- 176. Randelli P, Spennacchio P, Ragone V, Arrigoni P, Casella A, Cabitza P. Complications associated with arthroscopic rotator cuff repair: a literature review. Musculoskelet Surg. 2012;96(1):9–16. [DOI] [PubMed] [Google Scholar]
- 177. Raynor MB, Kuhn JE. Utility of features of the patient’s history in the diagnosis of atraumatic shoulder pain: a systematic review. J Shoulder Elbow Surg. 2016;25(4):688–694. [DOI] [PubMed] [Google Scholar]
- 178. Redondo-Alonso L, Chamorro-Moriana G, Jimenez-Rejano JJ, Lopez-Tarrida P, Ridao-Fernandez C. Relationship between chronic pathologies of the supraspinatus tendon and the long head of the biceps tendon: systematic review. BMC Musculoskelet Disord. 2014;15:377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Riboh JC, Garrigues GE. Early passive motion versus immobilization after arthroscopic rotator cuff repair. Arthroscopy. 2014;30(8):997–1005. [DOI] [PubMed] [Google Scholar]
- 180. Riley GP, Harrall RL, Constant CR, Cawston TE, Hazleman BL. Prevalence and possible pathological significance of calcium phosphate salt accumulation in tendon matrix degeneration. Ann Rheum Dis. 1996;55(2):109–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Riley GP, Harrall RL, Constant CR, Chard MD, Cawston TE, Hazleman BL. Glycosaminoglycans of human rotator cuff tendons: changes with age and in chronic rotator cuff tendinitis. Ann Rheum Dis. 1994;53(6):367–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Riley GP, Harrall RL, Constant CR, Chard MD, Cawston TE, Hazleman BL. Tendon degeneration and chronic shoulder pain: changes in the collagen composition of the human rotator cuff tendons in rotator cuff tendinitis. Ann Rheum Dis. 1994;53(6):359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Robb G, Arroll B, Reid D, Goodyear-Smith F. Summary of an evidence-based guideline on soft tissue shoulder injuries and related disorders—part 2: management. J Prim Health Care. 2009;1(1):42–49. [PubMed] [Google Scholar]
- 184. Rotini R, Fini M, Giavaresi G, et al. New perspectives in rotator cuff tendon regeneration: review of tissue engineered therapies. Chir Organi Mov. 2008;91(2):87–92. [DOI] [PubMed] [Google Scholar]
- 185. Roy JS, Braen C, Leblond J, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med. 2015;49(20):1316–1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Russell RD, Knight JR, Mulligan E, Khazzam MS. Structural integrity after rotator cuff repair does not correlate with patient function and pain: a meta-analysis. J Bone Joint Surg Am. 2014;96(4):265–271. [DOI] [PubMed] [Google Scholar]
- 187. Ryosa A, Laimi K, Aarimaa V, Lehtimaki K, Kukkonen J, Saltychev M. Surgery or conservative treatment for rotator cuff tear: a meta-analysis. Disabil Rehabil. 2017;39(14):1357–1363. [DOI] [PubMed] [Google Scholar]
- 188. Sabzevari S, Kachooei AR, Giugale J, Lin A. One-stage surgical treatment for concomitant rotator cuff tears with shoulder stiffness has comparable results with isolated rotator cuff tears: a systematic review. J Shoulder Elbow Surg. 2017;26(8):e252–e258. [DOI] [PubMed] [Google Scholar]
- 189. Saccomanno MF, Cazzato G, Fodale M, Sircana G, Milano G. Magnetic resonance imaging criteria for the assessment of the rotator cuff after repair: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):423–442. [DOI] [PubMed] [Google Scholar]
- 190. Saccomanno MF, Sircana G, Cazzato G, Donati F, Randelli P, Milano G. Prognostic factors influencing the outcome of rotator cuff repair: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3809–3819. [DOI] [PubMed] [Google Scholar]
- 191. Sakai H, Fujita K, Sakai Y, Mizuno K. Immunolocalization of cytokines and growth factors in subacromial bursa of rotator cuff tear patients. Kobe J Med Sci. 2001;47(1):25–34. [PubMed] [Google Scholar]
- 192. Saltzman BM, Collins MJ, Leroux T, et al. Arthroscopic repair of isolated subscapularis tears: a systematic review of technique-specific outcomes. Arthroscopy. 2017;33(4):849–860. [DOI] [PubMed] [Google Scholar]
- 193. Saltzman BM, Jain A, Campbell KA, et al. Does the use of platelet-rich plasma at the time of surgery improve clinical outcomes in arthroscopic rotator cuff repair when compared with control cohorts? A systematic review of meta-analyses. Arthroscopy. 2016;32(5):906–918. [DOI] [PubMed] [Google Scholar]
- 194. Saltzman BM, Zuke WA, Go B, et al. Does early motion lead to a higher failure rate or better outcomes after arthroscopic rotator cuff repair? A systematic review of overlapping meta-analyses. J Shoulder Elbow Surg. 2017;26(9):1681–1691. [DOI] [PubMed] [Google Scholar]
- 195. Sangwan S, Green RA, Taylor NF. Stabilizing characteristics of rotator cuff muscles: a systematic review. Disabil Rehabil. 2015;37(12):1033–1043. [DOI] [PubMed] [Google Scholar]
- 196. Santiago-Torres J, Flanigan DC, Butler RB, Bishop JY. The effect of smoking on rotator cuff and glenoid labrum surgery: a systematic review. Am J Sports Med. 2015;43(3):745–751. [DOI] [PubMed] [Google Scholar]
- 197. Saridakis P, Jones G. Outcomes of single-row and double-row arthroscopic rotator cuff repair: a systematic review. J Bone Joint Surg Am. 2010;92(3):732–742. [DOI] [PubMed] [Google Scholar]
- 198. Sayampanathan AA, Andrew TH. Systematic review on risk factors of rotator cuff tears. J Orthop Surg (Hong Kong). 2017;25(1):2309499016684318. [DOI] [PubMed] [Google Scholar]
- 199. Schmutz S, Fuchs T, Regenfelder F, Steinmann P, Zumstein M, Fuchs B. Expression of atrophy mRNA relates to tendon tear size in supraspinatus muscle. Clin Orthop Relat Res. 2009;467(2):457–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Seida JC, LeBlanc C, Schouten JR, et al. Systematic review: nonoperative and operative treatments for rotator cuff tears. Ann Intern Med. 2010;153(4):246–255. [DOI] [PubMed] [Google Scholar]
- 201. Seitz AL, Michener LA. Ultrasonographic measures of subacromial space in patients with rotator cuff disease: a systematic review. J Clin Ultrasound. 2011;39(3):146–154. [DOI] [PubMed] [Google Scholar]
- 202. Sejersen MH, Frost P, Hansen TB, Deutch SR, Svendsen SW. Proteomics perspectives in rotator cuff research: a systematic review of gene expression and protein composition in human tendinopathy. PLoS One. 2015;10(4):e0119974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Shan L, Fu D, Chen K, Cai Z, Li G. All-arthroscopic versus mini-open repair of small to large sized rotator cuff tears: a meta-analysis of clinical outcomes. PLoS One. 2014;9(4):e94421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Shang X, Chen J, Chen S. A meta-analysis comparing tenotomy and tenodesis for treating rotator cuff tears combined with long head of the biceps tendon lesions. PLoS One. 2017;12(10):e0185788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Sheibani-Rad S, Giveans MR, Arnoczky SP, Bedi A. Arthroscopic single-row versus double-row rotator cuff repair: a meta-analysis of the randomized clinical trials. Arthroscopy. 2013;29(2):343–348. [DOI] [PubMed] [Google Scholar]
- 206. Shen C, Tang ZH, Hu JZ, Zou GY, Xiao RC. Incidence of retear with double-row versus single-row rotator cuff repair. Orthopedics. 2014;37(11):e1006–e1013. [DOI] [PubMed] [Google Scholar]
- 207. Shen C, Tang ZH, Hu JZ, Zou GY, Xiao RC, Yan DX. Does immobilization after arthroscopic rotator cuff repair increase tendon healing? A systematic review and meta-analysis. Arch Orthop Trauma Surg. 2014;134(9):1279–1285. [DOI] [PubMed] [Google Scholar]
- 208. Shin JJ, Saccomanno MF, Cole BJ, Romeo AA, Nicholson GP, Verma NN. Pectoralis major transfer for treatment of irreparable subscapularis tear: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):1951–1960. [DOI] [PubMed] [Google Scholar]
- 209. Shindle MK, Chen CC, Robertson C, et al. Full-thickness supraspinatus tears are associated with more synovial inflammation and tissue degeneration than partial-thickness tears. J Shoulder Elbow Surg. 2011;20(6):917–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. Silva BM, Cartucho A, Sarmento M, Moura N. Surgical treatment of rotator cuff tears after 65 years of age: a systematic review. Acta Med Port. 2017;30(4):320–329. [DOI] [PubMed] [Google Scholar]
- 211. Slabaugh MA, Nho SJ, Grumet RC, et al. Does the literature confirm superior clinical results in radiographically healed rotator cuffs after rotator cuff repair? Arthroscopy. 2010;26(3):393–403. [DOI] [PubMed] [Google Scholar]
- 212. Smith TO, Back T, Toms AP, Hing CB. Diagnostic accuracy of ultrasound for rotator cuff tears in adults: a systematic review and meta-analysis. Clin Radiol. 2011;66(11):1036–1048. [DOI] [PubMed] [Google Scholar]
- 213. Smith TO, Daniell H, Geere JA, Toms AP, Hing CB. The diagnostic accuracy of MRI for the detection of partial- and full-thickness rotator cuff tears in adults. Magn Reson Imaging. 2012;30(3):336–346. [DOI] [PubMed] [Google Scholar]
- 214. Song L, Miao L, Zhang P, Wang WL. Does concomitant acromioplasty facilitate arthroscopic repair of full-thickness rotator cuff tears? A meta-analysis with trial sequential analysis of randomized controlled trials. Springerplus. 2016;5(1):685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Spall P, Ribeiro DC, Sole G. Electromyographic activity of shoulder girdle muscles in patients with symptomatic and asymptomatic rotator cuff tears: a systematic review and meta-analysis. PM R. 2016;8(9):894–906. [DOI] [PubMed] [Google Scholar]
- 216. Spennacchio P, Banfi G, Cucchi D, D’Ambrosi R, Cabitza P, Randelli P. Long-term outcome after arthroscopic rotator cuff treatment. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):523–529. [DOI] [PubMed] [Google Scholar]
- 217. Spiegl UJ, Euler SA, Millett PJ, Hepp P. Summary of meta-analyses dealing with single-row versus double-row repair techniques for rotator cuff tears. Open Orthop J. 2016;10:330–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218. St-Pierre C, Desmeules F, Dionne CE, Fremont P, MacDermid JC, Roy JS. Psychometric properties of self-reported questionnaires for the evaluation of symptoms and functional limitations in individuals with rotator cuff disorders: a systematic review. Disabil Rehabil. 2016;38(2):103–122. [DOI] [PubMed] [Google Scholar]
- 219. Steinhaus ME, Makhni EC, Cole BJ, Romeo AA, Verma NN. Outcomes after patch use in rotator cuff repair. Arthroscopy. 2016;32(8):1676–1690. [DOI] [PubMed] [Google Scholar]
- 220. Strauss EJ, Salata MJ, Kercher J, et al. Multimedia article: the arthroscopic management of partial-thickness rotator cuff tears—a systematic review of the literature. Arthroscopy. 2011;27(4):568–580. [DOI] [PubMed] [Google Scholar]
- 221. Sun L, Zhang Q, Ge H, Sun Y, Cheng B. Which is the best repair of articular-sided rotator cuff tears: a meta-analysis. J Orthop Surg Res. 2015;10:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Szomor ZL, Appleyard RC, Murrell GA. Overexpression of nitric oxide synthases in tendon overuse. J Orthop Res. 2006;24(1):80–86. [DOI] [PubMed] [Google Scholar]
- 223. Tadjerbashi K, Rosales RS, Atroshi I. Intervention randomized controlled trials involving wrist and shoulder arthroscopy: a systematic review. BMC Musculoskelet Disord. 2014;15:252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Tajana MS, Murena L, Valli F, Passi A, Grassi FA. Correlations between biochemical markers in the synovial fluid and severity of rotator cuff disease. Chir Organi Mov. 2009;93(suppl 1):S41–S48. [DOI] [PubMed] [Google Scholar]
- 225. Takeuchi E, Sugamoto K, Nakase T, et al. Localization and expression of osteopontin in the rotator cuff tendons in patients with calcifying tendinitis. Virchows Arch. 2001;438(6):612–617. [DOI] [PubMed] [Google Scholar]
- 226. Teunis T, Lubberts B, Reilly BT, Ring D. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg. 2014;23(12):1913–1921. [DOI] [PubMed] [Google Scholar]
- 227. Thangarajah T, Pendegrass CJ, Shahbazi S, Lambert S, Alexander S, Blunn GW. Augmentation of rotator cuff repair with soft tissue scaffolds. Orthop J Sports Med. 2015;3(6):23259 67115587495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Thigpen CA, Shaffer MA, Gaunt BW, Leggin BG, Williams GR, Wilcox RB., 3rd The American Society of Shoulder and Elbow Therapists’ consensus statement on rehabilitation following arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25(4):521–535. [DOI] [PubMed] [Google Scholar]
- 229. Thomson S, Jukes C, Lewis J. Rehabilitation following surgical repair of the rotator cuff: a systematic review. Physiotherapy. 2016;102(1):20–28. [DOI] [PubMed] [Google Scholar]
- 230. Tillander B, Franzen L, Fibronectin Norlin R, MMP-1 and histologic changes in rotator cuff disease. J Orthop Res. 2002;20(6):1358–1364. [DOI] [PubMed] [Google Scholar]
- 231. Tomonaga A, Hamada K, Gotoh M, Yamakawa H, Kobayashi K, Fukuda H. Expression of procollagen alpha 1 type III mRNA in rotator cuff tears. Tokai J Exp Clin Med. 2000;25(3):125–134. [PubMed] [Google Scholar]
- 232. Vavken P, Sadoghi P, Palmer M, et al. Platelet-rich plasma reduces retear rates after arthroscopic repair of small- and medium-sized rotator cuff tears but is not cost-effective. Am J Sports Med. 2015;43(12):3071–3076. [DOI] [PubMed] [Google Scholar]
- 233. Vincent K, Leboeuf-Yde C, Gagey O. Are degenerative rotator cuff disorders a cause of shoulder pain? Comparison of prevalence of degenerative rotator cuff disease to prevalence of nontraumatic shoulder pain through three systematic and critical reviews. J Shoulder Elbow Surg. 2017;26(5):766–773. [DOI] [PubMed] [Google Scholar]
- 234. Voloshin I, Gelinas J, Maloney MD, O’Keefe RJ, Bigliani LU, Blaine TA. Proinflammatory cytokines and metalloproteases are expressed in the subacromial bursa in patients with rotator cuff disease. Arthroscopy. 2005;21(9):1076. [DOI] [PubMed] [Google Scholar]
- 235. Wall LB, Keener JD, Brophy RH. Clinical outcomes of double-row versus single-row rotator cuff repairs. Arthroscopy. 2009;25(11):1312–1318. [DOI] [PubMed] [Google Scholar]
- 236. Wall LB, Keener JD, Brophy RH. Double-row vs single-row rotator cuff repair: a review of the biomechanical evidence. J Shoulder Elbow Surg. 2009;18(6):933–941. [DOI] [PubMed] [Google Scholar]
- 237. Wang MX, Wei A, Yuan J, et al. Antioxidant enzyme peroxiredoxin 5 is upregulated in degenerative human tendon. Biochem Biophys Res Commun. 2001;284(3):667–673. [DOI] [PubMed] [Google Scholar]
- 238. Warth RJ, Dornan GJ, James EW, Horan MP, Millett PJ. Clinical and structural outcomes after arthroscopic repair of full-thickness rotator cuff tears with and without platelet-rich product supplementation: a meta-analysis and meta-regression. Arthroscopy. 2015;31(2):306–320. [DOI] [PubMed] [Google Scholar]
- 239. Weinheimer KT, Smuin DM, Dhawan A. Patient outcomes as a function of shoulder surgeon volume: a systematic review. Arthroscopy. 2017;33(7):1273–1281. [DOI] [PubMed] [Google Scholar]
- 240. Xu C, Zhao J, Li D. Meta-analysis comparing single-row and double-row repair techniques in the arthroscopic treatment of rotator cuff tears. J Shoulder Elbow Surg. 2014;23(2):182–188. [DOI] [PubMed] [Google Scholar]
- 241. Xu Y, Bonar F, Murrell GA. Neoinnervation in rotator cuff tendinopathy. Sports Med Arthrosc Rev. 2011;19(4):354–359. [DOI] [PubMed] [Google Scholar]
- 242. Yanagisawa K, Hamada K, Gotoh M, et al. Vascular endothelial growth factor (VEGF) expression in the subacromial bursa is increased in patients with impingement syndrome. J Orthop Res. 2001;19(3):448–455. [DOI] [PubMed] [Google Scholar]
- 243. Yang J, Jr, Robbins M, Reilly J, Maerz T, Anderson K. The clinical effect of a rotator cuff retear. Am J Sports Med. 2017;45(3):733–741. [DOI] [PubMed] [Google Scholar]
- 244. Yang J, Sun Y, Xu P, Cheng B. Can patients get better clinical outcomes by using PRP in rotator cuff repair: a meta-analysis of randomized controlled trials. J Sports Med Phys Fitness. 2016;56(11):1359–1367. [PubMed] [Google Scholar]
- 245. Yi A, Villacis D, Yalamanchili R, Hatch GF., 3rd A comparison of rehabilitation methods after arthroscopic rotator cuff repair: a systematic review. Sports Health. 2015;7(4):326–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Ying ZM, Lin T, Yan SG. Arthroscopic single-row versus double-row technique for repairing rotator cuff tears: a systematic review and meta-analysis. Orthop Surg. 2014;6(4):300–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247. Yoshihara Y, Hamada K, Nakajima T, Fujikawa K, Fukuda H. Biochemical markers in the synovial fluid of glenohumeral joints from patients with rotator cuff tear. J Orthop Res. 2001;19(4):573–579. [DOI] [PubMed] [Google Scholar]
- 248. Zhang Q, Ge H, Zhou J, Cheng B. Are platelet-rich products necessary during the arthroscopic repair of full-thickness rotator cuff tears: a meta-analysis. PLoS One. 2013;8(7):e69731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249. Zhang Q, Ge H, Zhou J, Yuan C, Chen K, Cheng B. Single-row or double-row fixation technique for full-thickness rotator cuff tears: a meta-analysis. PLoS One. 2013;8(7):e68515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250. Zhao JG, Zhao L, Jiang YX, Wang ZL, Wang J, Zhang P. Platelet-rich plasma in arthroscopic rotator cuff repair: a meta-analysis of randomized controlled trials. Arthroscopy. 2015;31(1):125–135. [DOI] [PubMed] [Google Scholar]
- 251. Zuke WA, Leroux TS, Gregory BP, et al. Establishing maximal medical improvement after arthroscopic rotator cuff repair. Am J Sports Med. 2018;46(4):1000–1007. [DOI] [PubMed] [Google Scholar]