Abstract
Background
Morphine and oxycodone are considered as wide-spreadly used opioids for moderate/severe cancer pain. However, debate exists about the evidence regarding their relative tolerability and underlying results.
Methods
A systematic search of online electronic databases, including PubMed, Embase, Cochrane library updated on October 2017 were conducted. The meta-analysis was performed including the studies that were designed as randomized controlled trials.
Results
In total, seven randomized clinical trials met our inclusion criteria. No statistical differences in analgesic effect between oxycodone and morphine were observed. Both the pooled analysis of API (MD =0.01, 95% CI -0.22 – 0.23; p = 0.96) and WPI (MD = − 0.05, 95% CI -0.21 – 0.30; p = 0.72) demonstrated clinical non-inferiority of the efficacy of morphine compared with oxycodone, respectively. Additionally, no significant difference in PRR response was observed in either oxycodone or morphine that were used in patients (MD =0.99, 95% CI -0.88 – 1.11; p = 0.87). With the pooled result of AEs indicating the comparable safety profiles between the 2 treatment groups, the meta-analysis on the nausea (OR = 1.20, 95% CI 0.90–1.59; p = 0.22), vomiting (OR = 1.33, 95% CI 0.75–2.38; p = 0.33), somnolence (OR = 1.35, 95% CI 0.95–1.93; p = 0.10), diarrhea (OR = 1.01, 95% CI 0.60–1,67; p = 0.98), and constipation (OR = 1.04, 95% CI 0.77–1.41; p = 0.79) was conducted, respectively.
Conclusions
In the current study, no remarkable difference was identified either in analgesic efficacy or in tolerability of oxycodone and morphine as the first-line therapy for patients with moderate to severe cancer pain. Thus, no sufficient clinical evidence on the superior effects of oxycodone to morphine was provided in this experimental hypothesis.
Keywords: Oxycodone, Morphine, Cancer pain, Meta-analysis
Background
The principle to treat cancer pain, the 3 step analgesic ladder, was developed by the World Health Organization (WHO) in 1986. This 3-step ladder treatment recommends the use of non-opioid analgesics for weak opioids and strong opioids for moderate–severe pain, indeed, these agents have guided the most effective treatment for cancer pain [1].
Overall there has been an increase of cancer patients attain satisfactory analgesia based on opioid therapy [2]. Opioids used to treat moderate-to-severe pain, if appropriately prescribed [3, 4]. Oral morphine has traditionally been widely used for treating patients with moderate or severe pain according to the WHO ladder Step-III [5, 6]. Reduced fluctuations in drug plasma concentrations are predicted to provide acceptable adverse effects and, potentially, better efficacy of taking short-acting opioids [7].
However, other strong opioids such as oxycodone can be used as alternatives [8, 9]. According to European Association for Palliative Care recommendations, oxycodone was alternative used in cancer patients to morphine in the 2001, and it frequently recommended in clinical use [10, 11]. Oxycodone (OX) has been showed a similar profile and has been found to provide statistically reduction in pain, primarily in the central nervous system [12].
More recent guidelines have recommended morphine and oxycodone as first-line opioids to treat cancer pain, while the evidence is limited [13, 14]. Several trails have compared the analgesic efficacy and adverse effects of different opioids conducted in cancer patients [15–17]. A comparable analgesic efficacy and safety profile was observed during the treatment, even though differences in design and assessment methods. No significant differences were found in two open-label RCTs comparing the first- line administration of morphine and oxycodone [17, 18].
Indeed, cancer patients with anxiety and depression experience an improvement in symp- toms of pain [21]. This would imply an inappropriate use of opioids for the “pain experience” and suffering [22]. Opioid abuse and addiction the most frequently reported in cancer pain patients receiving opioid analgesia [23–26]. In addition, the successful management of cancer pain is based on achieving adequate symptom relief with minimal adverse events (AEs) in a manner convenient for patients. Moreover, most RCTs comparing different opioids lack a good evidence base in the definition, measurement, and reporting of adverse events (AEs) [19].
On this basis, we launched this study aimed at assessing the effectiveness and safety of comparing morphine versus oxycodone in patients with cancer pain.
Methods and materials
Search strategy
Two investigators independently searched electronic databases: Pubmed, Embase, Cochrane library up to October 2017.The process was established to find all articles with the keywords: “oxycodone” “morphine” and “cancer pain”, and relevant Medical Subject Heading (MeSH) terms were utilized. The reference lists of all articles that dealt with the topic of interest were also hand-searched to check for additional relevant publications.
Medical Subject Heading (MeSH) terms including morphine, oxycodone, neoplasms,and pain.
Eligibility criteria
Studies were included in the meta-analysis should meet the following criteria: (1) the studies are designed as randomized controlled trials; (2) the primary outcome was to compare the patients with cancer-related pain who responded clinically to morphine and oxycodone as first-line treatment; (3) studies providing data of analgesic effect for both two groups, and Hazard Ratio (HR) with corresponding 95% CIs were provided; If we found duplicated or overlapped data in multiple reports, we just include the one with most complete information.
We excluded from the current meta-analysis: (1) non-randomized controlled studies; (2) data on the main outcomes were unavailable; (3) Studies including patients receiving either morphine or oxycodone combined with other drugs for cancer pain.
Quality assessment
Two investigators separately rated the quality of the retrieved studies. Study quality was assessed using Newcastle-Ottawa Quality Assessment Scale.
Data extraction
Two authors independently extracted the relevant data from each trial. Disagreement was revolved by consensus. From each of the eligible studies, the main categories based on the following: first author family name, publication year, study period, country, number of patients, study interventions, analgesic effect parameters (Pain Relief Rate, Average Pain Inventory and Worst Pain Inventory), and adverse reaction parameters (nausea, vomiting, somnolence, diarrhea, and constipation).
Statistical analysis
A sensitivity analysis was also performed to examine the impact on the overall results, depending on the heterogeneity across the included studies. Heterogeneity was examined by calculating I2 statistic [27]. Heterogeneity with an I2 of 25–50%, 50–75%, or > 75% were indicated low, moderate, or high heterogeneity, respectively [28]. When there was low heterogeneity among studies, data were analyzed using a fixed-effects model. Otherwise, the random effects model was used. p-value of 0.05 was considered statistically significant. The statistical analyses were per- formed using Review Manager version 5.3 software (Revman; The Cochrane collaboration Oxford, United Kingdom). The results of our meta-analysis were shown in forest plots. The Begg test and the Egger test were conducted to evaluate publication bias.
Results
Overview of literature search and study characteristics
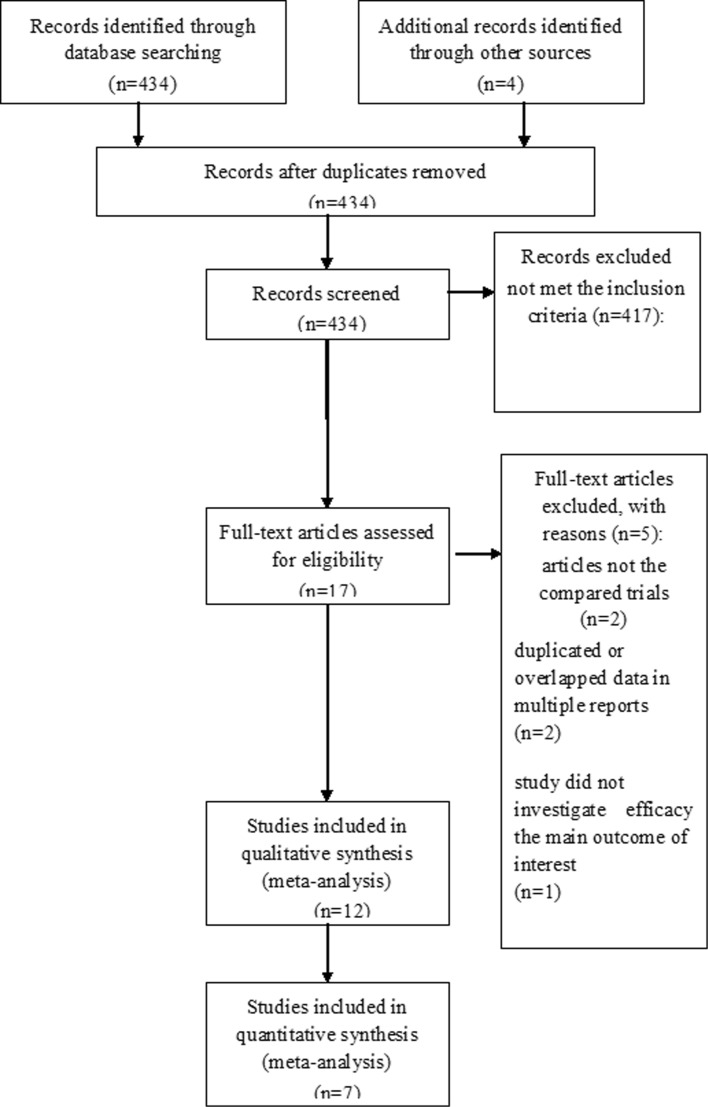
A total of 434 studies were retrieved initially for evaluation. Based on the criteria described in the methods, 12 publications were evaluated in more detail, but some did not provide enough detail of outcomes of two approaches. Therefore, a final total of 7 [17, 29–34] RCTs were included in this meta-analysis. The search process is described in Fig. 1.
Fig. 1.
PRISMA flow chart of selection process to identify studies eligible for pooling
All included studies in this study were based on moderate to high quality evidence. Table 1 describes the primary characteristics of the eligible studies in more detail.
Table 1.
the primary characteristics of the eligible studies in more detail
| Study Year | Country | Study period | Age | N | Interventions | ||
|---|---|---|---|---|---|---|---|
| morphine | oxycodone; | morphine | oxycodone; | ||||
| Nashat Y 2003 | USA | NR | NR | NR | 20 | 22 | over-encapsulated oxymorphone ER (10, 20, or 40 mg) or over- encapsulated oxycodone CR (20, 40, or 80 mg). |
| Satoshi Inoue 2017 | Japan | 2014–2015 | 70.1 | 68.4 | 86 | 92 | hydromorphone extended-release tablets plus placebo oxycodone hydrochloride extended-release tablets 4 mg/day or placebo hydromorphone extended-release tablets plus oxycodone hydrochloride extended-release tablets 10 mg/day orally for 7 days (once-daily dosing for hydromorphone and twice-daily dosing for oxycodone) |
| O. Corli 2016 | Italy | 2011.5–2014.7 | 67.5 | 66.9 | 122 | 125 | morphine or oxycodone for 28 days.The initial dose of opioid was based on the recommendations of the European Association for Palliative Care/EAPC |
| Julia Riley 2015 | UK | 2006.5–2011.7 | 59.2 | 58.9 | 100 | 100 | the starting dose was determined by the treating physician on an individual patient basis and titrated accordingly until adequate pain control was achieved or intolerable side effects were re- ported by the patient. |
| Shiying Yu 2014 | China | NR | 53.5 | 52.7 | 125 | 123 | require between 40 and 184 mg of oral morphine or morphine equivalents every 24 h for chronic management of cancer pain |
| S. Mercadante 2010 | Italy | NR | NR | NR | 21 | 25 | receive 30 mg/d of sustained release oralmorphine or sustained release oral oxycodone(20 mg/d). |
| Ernesto Zecca 2016 | Italy | 2006.9.14–2007.12.21 | 61.8 | 62.1 | 95 | 92 | Opioid dosages were reported as oral morphine equivalent daily dose (MEDD) mg, converted using a 1.5:1 ratio between morphine and oxycodone. |
Clinical and methodological heterogeneity
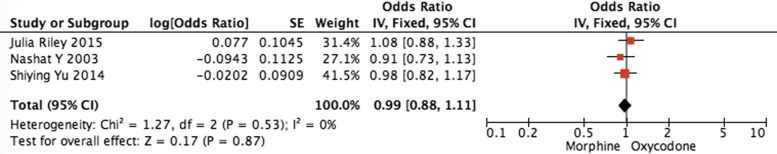
Pooled analysis of pain relief rate (PRR) comparing oxycodone with morphine on patients with cancer pain
The pooling analysis [29, 32, 33]revealed that there was no difference in composite PRR between oxycodone and morphine (MD =0.99, 95% CI -0.88 – 1.11; p = 0.87) (Fig. 2).
Fig. 2.
Pooled analysis of PRR comparing oxycodone with morphine on patients with cancer pain
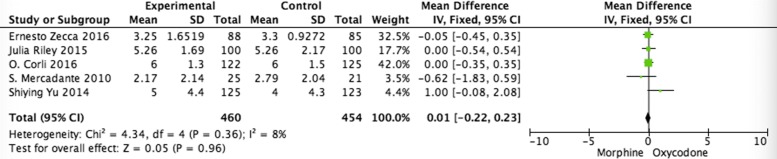
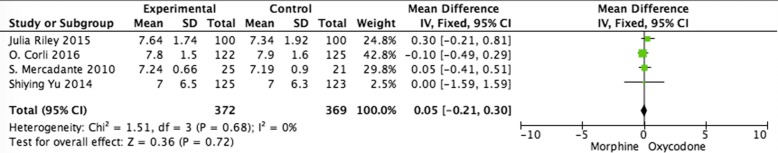
Pooled analysis of pain inventory (PI) comparing oxycodone with morphine on patients with cancer pain
A fixed- effects model was used to pool the PI data, since the heterogeneity across the four studies was very low. Both the pooled analysis of average pain inventory (API) (MD =0.01, 95% CI -0.22 – 0.23; p = 0.96) (Fig. 3) [17, 31–34] and worst pain inventory (WPI) (MD = − 0.05, 95% CI -0.21 – 0.30; p = 0.72) (Fig. 4) [17, 31–33] demonstrates clinical non-inferiority of the efficacy of morphine compared with oxycodone, respectively.
Fig. 3.
Pooled analysis of API comparing oxycodone with morphine on patients with cancer pain
Fig. 4.
Pooled analysis of WPI comparing oxycodone with morphine on patients with cancer pain
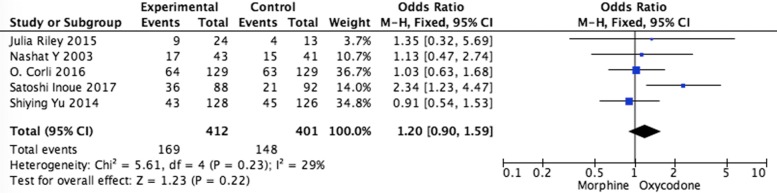
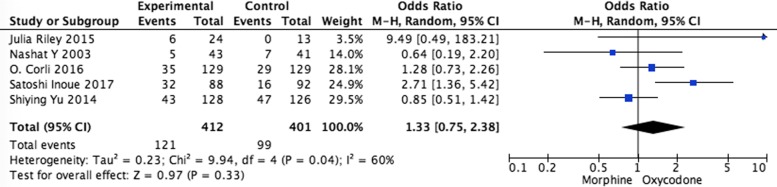
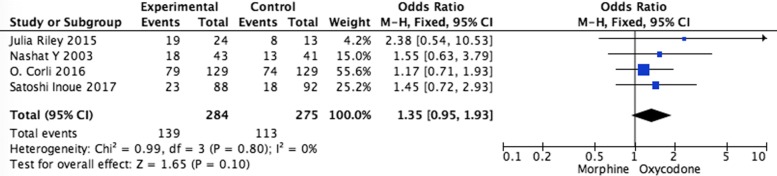
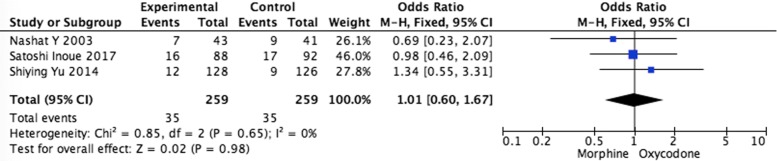
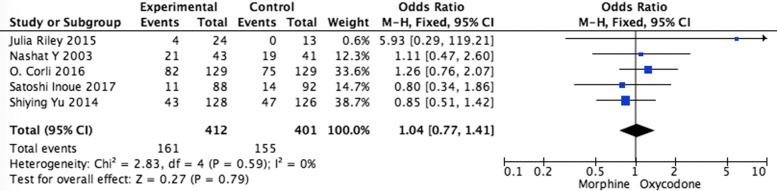
Pooled analysis of adverse reaction parameters comparing oxycodone with morphine on patients with cancer pain
Systematic evaluations of adverse effects (AEs) data analysis were shown in Figs. 5, 6, 7, 8 and 9. The most common treatment-related adverse events are nausea (OR = 1.20, 95% CI 0.90–1.59; p = 0.22), vomiting (OR = 1.33, 95% CI 0.75–2.38; p = 0.33), the somnolence (OR = 1.35, 95% CI 0.95–1.93; p = 0.10), diarrhea (OR = 1.01, 95% CI 0.60–1,67; p = 0.98), and constipation (OR = 1.04, 95% CI 0.77–1.41; p = 0.79) the difference had no statistical significance between oxycodone and morphine.
Fig. 5.
Pooled analysis of nausea comparing oxycodone with morphine on patients with cancer pain
Fig. 6.
Pooled analysis of vomiting comparing oxycodone with morphine on patients with cancer pain
Fig. 7.
Pooled analysis of somnolence comparing oxycodone with morphine on patients with cancer pain
Fig. 8.
Pooled analysis of diarrhea comparing oxycodone with morphine on patients with cancer pain
Fig. 9.
Pooled analysis of constipation comparing oxycodone with morphine on patients with cancer pain
Discussion
For patients with cancer pain, it is important to select the most appropriate manage- ment of moderate/severe cancer pain regardless of their disease stage to have a positive effect on the quality of life. Opioids are the mainstay of treatment for cancer pain at the second and third steps according to the 3-step analgesic ladder of the World Health Organization [1, 5, 35].
Morphine-like opioids are frequently used and can be interchangeable. The recently published EAPC recommendations [13] indicate that pain control did not differ significantly between morphine, oxycodone, and hydro-morphine, permitting a weak recommendation that any one of these drugs can be recognized as the treatment of choice for the treatment of moderate/severe pain in cancer patients.
The results of this meta-analysis demonstrate clinical non-inferiority of morphine compared with oxycodone in alleviating cancer pain, with respect to achieved a comparable clinical response whether morphine or oxycodone was used as first-line opioid in the treatment of cancer-related pain. The underlying opioid-related mechanisms for cancer patients including the inflammatory factors or apparent sprounting and then destruction of sensory, which are able to allow for assessment of pain in the early stage of disease [36].
Opioid metabolism was consistent with genetic differences and complex concomitant medications. The results of our analysis could be attributed to different factors.
First, at a molecular level, oxycodone has been identified as a different metabolic pathway compared with morphine. Intriguingly, some previous studies have demonstrated that morphine and oxycodone are addressed the underlying different opioid-related mechanisms: m- and k-opioid receptors, respectively [37, 38]. Oxycodone and its metabolites may have sufficient m-receptor activity [39], and an aggressive local disease, like cancer, may exclusively on peripheral k-opioid receptors. The k-opioid receptor agonists are specifically target analgesics in experimental models of visceral pain, acting peripherally [40, 41]. It has been shown that oxycodone was actually associated with benefit in the treatment of visceral pain than morphine [42, 43], it is perhaps that the prevalent peripheral activity of oxycodone as a putative k-agonist, and a relatively low affinity for m- receptors [44, 45].
Secondly, although morphine and oxycodone are widely used for cancer pain, previous report indicated that their effects on immune system are different. Chronic morphine treatment induces immunosuppression and abnormality of some immunological indexes including interleukin 2 production and natural killer (NK) cell activity. These findings emerged in an exploratory prospective study in animals and in vitro [46–48].
Other studies have indicated relationship between morphine and the susceptibility to infections in animals [49, 50]. On the other hand, prospective study showed no relationship between oxycodone and the immunological indexes [48]. Moreover, compared to morphine itself, morphine’s metabolites (morphine-3- glucuronide and morphine-6-glucuronide) have similar effects on several immunological indexes [51, 52]. Based on the above pharmacological property background, morphine might be more effective than oxycodone. It is known that immunosuppression has effect on the development of infections, disease progression, and the choice of cancer therapy. Therefore, in the selection of opioids, immune system should be considered in cancer patients with pain.
Thirdly, the efficacy of different individual gene polymorphism on the pharmacodynamic effects of opioids in painful conditions is controversial [53–55]. The efficacy of various opioids in patients with cancer based on different receptors and their subtypes [55]. Genetic differences in the expression of different receptor subtypes could affect individual therapeutic efficacy [55–59].While, these results have not been replicated in different populations, because of differences in definition of phenotype and outcome measures used [60].
With regard to therapeutic safety, although opioids are the first-line drug for moderate to severe cancer pain [3, 4], opioid-related AEs (particularly at high doses) that led to discontinuation of study treatment can sometimes prevent adequate analgesia [20]. Heiskanen and Kalso [61] have shown similar results of adverse effects with the two drugs, reporting vomiting was more common (p < 0.01) with morphine, while constipation more frequent with oxycodone (p < 0.01). Mucci Lo Russo et al. [62] showed adverse effects with a statistically significant lower incidence regarding itching with oxycodone (p < 0.04) and two cases of hallucinations with morphine. While, other authors did not found significant differences in adverse effects [17, 18, 63].
Several questions remain to be answered. First, although some preclinical data are available in cancer pain models, the mechanism of action of morphine and oxycodone for moderate-to-severe pain remains to be debated. Second, different subgroups of patients might have differential responses to cancer pain treatment. Future research should aim to identify these subgroups, probably through the identification and validation of biomarkers, to refine the population of patients likely to obtain benefit from morphine and oxycodone.
Conclusion
In conclusion, morphine showed no inferiority or superiority when compared with oxycodone in terms of analgesic response or adverse effects. Currently, growing evidence has suggested that the pharmacokinetics and pharmacodynamics are different among opioids. As a result, different opioids are likely to differ in some respects. Additional studies, including comparison with controls and other opioids, will be necessary to confirm the results. Moreover, in the future, prospective, randomized, clinical trials are designed to evaluate the efficacy of different opioids in patients with cancer pain based on gene polymorphism.
Acknowledgments
Funding
No funding was received for this study.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AEs
Adverse events
- API
Average Pain Inventory
- CROM
Morphine
- CROO
Oxycodone
- HR
Hazard ratio
- MD
Mean difference
- OR
Odds ratio
- PRR
Pain Relief Rate
- WHO
World Health Organization
- WPI
Worst Pain Inventory
Authors’ contributions
Kai-Kai Guo made substantial contributions to conception and design of the study; Cheng-Qi Deng, Gui-Jun Lu and Guo-Li Zhao searched literature, extracted data from the collected literature and analyzed the data; Kai-Kai Guo wrote the manuscript; Gui-Jun Lu revised the manuscript; All authors approved the final version of the manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zech DF, Grond S, Lynch J, Hertel D, Lehmann KA. Validation of World Health Organization guidelines for cancer pain relief: a 10-year prospective study. Pain. 1995;63(1):65–76. doi: 10.1016/0304-3959(95)00017-M. [DOI] [PubMed] [Google Scholar]
- 2.Portenoy RK. Managing cancer pain poorly responsive to systemic opioid therapy. Oncology (Williston Park) 1999;13(5 Suppl 2):25–29. [PubMed] [Google Scholar]
- 3.American Society of Anesthesiologists A report by the American Society of Anesthesiologists Task Force on pain management, Cancer pain section. Anesthesiology. 1996;84:1243–1257. doi: 10.1097/00000542-199605000-00029. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) Expert Committee. Cancer pain relief and palliative care. Geneva: World Health Organization; 1990. Technical report series, No. 804. [PubMed]
- 5.World Health Organization. Cancer pain relief, second edition, with a guide to opioid availability. Geneva: World Health Organization; 1996.
- 6.Hanks GW, Conno F, Cherny N, et al. Morphine and alternative opioids in cancer pain: the EAPC recommendations. Br J Cancer. 2001;84(5):587–593. doi: 10.1054/bjoc.2001.1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferrell B, Wisdom C, Wenzl C, Brown J. Effects of controlled-released morphine on quality of life for cancer pain. Oncol Nurs Forum. 1989;16(4):521–526. [PubMed] [Google Scholar]
- 8.Cancer Pain Relief: With a Guide to Opioid Availability, 2nd ed. Geneva, Switzerland: World Health Organization; 1996.
- 9.Riley J, Ross JR, Rutter D, et al. No pain relief from morphine? Individual variation in sensitivity to morphine and the need to switch to an alternative opioid in cancer patients. Support Care Cancer. 2006;14(1):56–64. doi: 10.1007/s00520-005-0843-2. [DOI] [PubMed] [Google Scholar]
- 10.Caraceni AT, Brunelli C, Rocco P, Minghetti P. Trends in opioid analgesics sales to community pharmacies and hospitals in Italy (2000-2010) Minerva Anestesiol. 2013;79(8):906–914. [PubMed] [Google Scholar]
- 11.International Narcotics Control Board. Technical reports 2014. Available at: http://www.incb.org/incb/en/ narcotic-drugs/Technical_Reports/narcotic_drugs_reports. html. Accessed 25 April 2016, 2015.
- 12.Reid CM, Martin RM, Sterne JA, Davies AN, Hanks GW. Oxycodone for cancer-related pain: meta-analysis of randomized controlled trials. Arch Intern Med. 2006;166(8):837–843. doi: 10.1001/archinte.166.8.837. [DOI] [PubMed] [Google Scholar]
- 13.Caraceni A, Hanks G, Kaasa S, et al. Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol. 2012;13(2):e58–e68. doi: 10.1016/S1470-2045(12)70040-2. [DOI] [PubMed] [Google Scholar]
- 14.Ahmedzai SH, Nauck F, Bar-Sela G, Bosse B, Leyendecker P, Hopp M. A randomized, double-blind, active-controlled, double-dummy, parallel-group study to determine the safety and efficacy of oxycodone/naloxone prolonged-release tablets in patients with moderate/severe, chronic cancer pain. Palliat Med. 2012;26(1):50–60. doi: 10.1177/0269216311418869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kress HG, Koch ED, Kosturski H, et al. Tapentadol prolonged release for managing moderate to severe, chronic malignant tumor-related pain. Pain Physician. 2014;17(4):329–343. [PubMed] [Google Scholar]
- 16.Mercadante S, Porzio G, Ferrera P, et al. Sustained-release oral morphine versus transdermal fentanyl and oral methadone in cancer pain management. Eur J Pain. 2008;12(8):1040–1046. doi: 10.1016/j.ejpain.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 17.Mercadante S, Tirelli W, David F, et al. Morphine versus oxycodone in pancreatic cancer pain: a randomized controlled study. Clin J Pain. 2010;26(9):794–797. doi: 10.1097/AJP.0b013e3181ecd895. [DOI] [PubMed] [Google Scholar]
- 18.Silvestri B, Bandieri E, Del P S, et al. Oxycodone controlled-release as first-choice therapy for moderate-to-severe cancer pain in Italian patients: results of an open-label, multicentre, observational study.[J]. Clin Drug Investig. 2008;28(7):399. [DOI] [PubMed]
- 19.Wiffen PJ, Derry S, Moore RA. Impact of morphine, fentanyl, oxycodone or codeine on patient consciousness, appetite and thirst when used to treat cancer pain. Cochrane Database Syst Rev. 2014;5:CD011056. doi: 10.1002/14651858.CD011056.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gammaitoni AR, Fine P, Alvarez N, McPherson ML, Bergmark S. Clinical application of opioid equianalgesic data. Clin J Pain. 2003;19(5):286–297. doi: 10.1097/00002508-200309000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Delgado M, Parsons HA, Li Z, Palmer JL, Bruera E. Symptom distress in advanced cancer patients with anxiety and depression in the palliative care setting. Support Care Cancer. 2009;17:573–579. doi: 10.1007/s00520-008-0529-7. [DOI] [PubMed] [Google Scholar]
- 22.Strasser F, Walker P, Bruera E. Palliative pain management: when both pain and suffering hurt. J Palliat Care. 2005;21(2):69–79. [PubMed] [Google Scholar]
- 23.Starr TD, Rogak LJ, Passik SD. Substance abuse in cancer pain. Curr Pain Headache Rep. 2010;14(4):268–275. doi: 10.1007/s11916-010-0118-6. [DOI] [PubMed] [Google Scholar]
- 24.Colson J, Koyyalagunta D, Falco FJ, Manchikanti L. A systematic review of observational studies on the effectiveness of opioid therapy for cancer pain. Pain Physician. 2011;14(2):E85–102. [PubMed] [Google Scholar]
- 25.Lee M, Silverman SM, Hansen H, Patel VB, Manchikanti L. A comprehensive review of opioid-induced hyperalgesia. Pain Physician. 2011;14(2):145–161. [PubMed] [Google Scholar]
- 26.Sehgal N, Smith HS, Manchikanti L. Peripherally acting opioids and clinical implications for pain control. Pain Physician. 2011;14(3):249–258. [PubMed] [Google Scholar]
- 27.Higgins J, et al. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 28.Higgins J, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gabrail NY, Dvergsten C, Ahdieh H. Establishing the dosage equivalency of oxymorphone extended release and oxycodone controlled release in patients with cancer pain: a randomized controlled study. Curr Med Res Opin. 2004;20(6):911–918. doi: 10.1185/030079904125003854. [DOI] [PubMed] [Google Scholar]
- 30.Inoue S, Saito Y, Tsuneto S, Aruga E, Ide A, Kakurai Y. A randomized, double-blind study of hydromorphone hydrochloride extended-release tablets versus oxycodone hydrochloride extended-release tablets for cancer pain: efficacy and safety in Japanese cancer patients (EXHEAL: a phase III study of EXtended-release HydromorphonE for cAncer pain reLief) J Pain Res. 2017;10:1953–1962. doi: 10.2147/JPR.S136937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Corli O, Floriani I, Roberto A, et al. Are strong opioids equally effective and safe in the treatment of chronic cancer pain? A multicenter randomized phase IV 'real life' trial on the variability of response to opioids. Ann Oncol. 2016;27(6):1107–1115. doi: 10.1093/annonc/mdw097. [DOI] [PubMed] [Google Scholar]
- 32.Riley J, Branford R, Droney J, et al. Morphine or oxycodone for cancer-related pain? A randomized, open-label, controlled trial. J Pain Symptom Manag. 2015;49(2):161–172. doi: 10.1016/j.jpainsymman.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 33.Yu S, Shen W, Yu L, Hou Y, Han J, Richards HM. Safety and efficacy of once-daily hydromorphone extended-release versus twice-daily oxycodone hydrochloride controlled-release in chinese patients with cancer pain: a phase 3, randomized, double-blind, multicenter study. J Pain. 2014;15(8):835–844. doi: 10.1016/j.jpain.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 34.Zecca E, Brunelli C, Bracchi P, et al. Comparison of the tolerability profile of controlled-release oral morphine and oxycodone for Cancer pain treatment. An open-label randomized controlled trial. J Pain Symptom Manag. 2016;52(6):783–794. doi: 10.1016/j.jpainsymman.2016.05.030. [DOI] [PubMed] [Google Scholar]
- 35.Meuser T, Pietruck C, Radbruch L, Stute P, Lehmann KA, Grond S. Symptoms during cancer pain treatment following WHO-guidelines: a longitudinal follow-up study of symptom prevalence, severity and etiology. Pain. 2001;93(3):247–257. doi: 10.1016/S0304-3959(01)00324-4. [DOI] [PubMed] [Google Scholar]
- 36.Lindsay TH, Jonas BM, Sevcik MA, et al. Pancreatic cancer pain and its correlation with changes in tumor vasculature, macrophage infiltration, neuronal innervation, body weight and disease progression. Pain. 2005;119(1–3):233–246. doi: 10.1016/j.pain.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 37.Nielsen CK, Ross FB, Smith MT. Incomplete, asymmetric, and route-dependent cross-tolerance between oxycodone and morphine in the dark Agouti rat. J Pharmacol Exp Ther. 2000;295(1):91–99. [PubMed] [Google Scholar]
- 38.Nielsen CK, Ross FB, Lotfipour S, Saini KS, Edwards SR, Smith MT. Oxycodone and morphine have distinctly different pharmacological profiles: radioligand binding and behavioural studies in two rat models of neuropathic pain. Pain. 2007;132(3):289–300. doi: 10.1016/j.pain.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 39.Lemberg K, Kontinen V, Siskonen A, et al. Anti-nociception by spinal and systemic oxycodone: why does the route make a difference? Anesthesiology. 2006;105:801–812. doi: 10.1097/00000542-200610000-00027. [DOI] [PubMed] [Google Scholar]
- 40.Riviere PJ. Peripheral kappa-opioid agonists for visceral pain. Br J Pharmacol. 2004;141(8):1331–1334. doi: 10.1038/sj.bjp.0705763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vanderah TW, Schteingart CD, Trojnar J, et al. FE200041 (D-Phe-D-Phe-D-Nle-D-Arg-NH2): a peripheral efficacious k-opioid agonist with unprecedented selectivity. J Pharmacol Exp Ther. 2004;310:326–333. doi: 10.1124/jpet.104.065391. [DOI] [PubMed] [Google Scholar]
- 42.Staahl C, Dimcevski G, Andersen SD, et al. Differential effect of opioids in patients with chronic pancreatitis: an experimental pain study. Scand J Gastroenterol. 2007;42(3):383–390. doi: 10.1080/00365520601014414. [DOI] [PubMed] [Google Scholar]
- 43.Staahl C, Christrup LL, Andersen SD, Arendt-Nielsen L, Drewes AM. A comparative study of oxycodone and morphine in a multi-modal, tissue-differentiated experimental pain model. Pain. 2006;123(1–2):28–36. doi: 10.1016/j.pain.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 44.Peckham EM, Traynor JR. Comparison of the antinociceptive response to morphine and morphine-like compounds in male and female Sprague-Dawley rats. J Pharmacol Exp Ther. 2006;316(3):1195–1201. doi: 10.1124/jpet.105.094276. [DOI] [PubMed] [Google Scholar]
- 45.Kalso E. How different is oxycodone from morphine? Pain. 2007;132:227–228. doi: 10.1016/j.pain.2007.09.027. [DOI] [PubMed] [Google Scholar]
- 46.Flores LR, Wahl SM, Bayer BM. Mechanisms of morphine-induced immunosuppression: effect of acute morphine administration on lymphocyte trafficking. J Pharmacol Exp Ther. 1995;272(3):1246–1251. [PubMed] [Google Scholar]
- 47.Welters ID, Menzebach A, Goumon Y, et al. Morphine suppresses complement receptor expression, phagocytosis, and respiratory burst in neutrophils by a nitric oxide and mu(3) opiate receptor-dependent mechanism. J Neuroimmunol. 2000;111(1–2):139–145. doi: 10.1016/S0165-5728(00)00401-X. [DOI] [PubMed] [Google Scholar]
- 48.Sacerdote P, Manfredi B, Mantegazza P, Panerai AE. Antinociceptive and immunosuppressive effects of opiate drugs: a structure-related activity study. Br J Pharmacol. 1997;121(4):834–840. doi: 10.1038/sj.bjp.0701138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chao CC, Sharp BM, Pomeroy C, Filice GA, Peterson PK. Lethality of morphine in mice infected with toxoplasma gondii. J Pharmacol Exp Ther. 1990;252(2):605–609. [PubMed] [Google Scholar]
- 50.Risdahl JM, Peterson PK, Chao CC, Pijoan C, Molitor TW. Effects of morphine dependence on the pathogenesis of swine herpesvirus infection. J Infect Dis. 1993;167(6):1281–1287. doi: 10.1093/infdis/167.6.1281. [DOI] [PubMed] [Google Scholar]
- 51.Thomas PT, Bhargava HN, House RV. Immunomodulatory effects of in vitro exposure to morphine and its metabolites. Pharmacology. 1995;50(1):51–62. doi: 10.1159/000139266. [DOI] [PubMed] [Google Scholar]
- 52.Carrigan KA, Lysle DT. Morphine-6b-glucuronide induces potent immunomodulation. Int Immunopharmacol. 2001;1(5):821–831. doi: 10.1016/S1567-5769(01)00020-0. [DOI] [PubMed] [Google Scholar]
- 53.Reyes-Gibby CC, Shete S, Rakvag T, et al. Exploring joint effects of genes and the clinical efficacy of morphine for cancer pain: OPRM1 and COMT gene. Pain. 2007;130(1–2):25–30. doi: 10.1016/j.pain.2006.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ross JR, Riley J, Taegetmeyer AB, et al. Genetic variation and response to morphine in cancer patients: catechol-O-methyltransferase and multidrug resistance-1 gene polymorphisms are associated with central side effects. Cancer. 2008;112(6):1390–1403. doi: 10.1002/cncr.23292. [DOI] [PubMed] [Google Scholar]
- 55.Stamer UM, Bayerer B, Stuber F. Genetics and variability in opioid response. Eur J Pain. 2005;9(2):101–104. doi: 10.1016/j.ejpain.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 56.Sinatra RS, Hyde NH, Harrison DM. Oxymorphone revisited. Semin Anesth. 1988;7(3):209–215. [Google Scholar]
- 57.Galvan A, Skorpen F, Klepstad P, et al. Multiple loci modulate opioid therapy response for cancer pain. Clin Cancer Res. 2011;17(13):4581–4587. doi: 10.1158/1078-0432.CCR-10-3028. [DOI] [PubMed] [Google Scholar]
- 58.Droney JM, Gretton SK, Sato H, et al. Analgesia and central side-effects: two separate dimensions of morphine response. Br J Clin Pharmacol. 2013;75(5):1340–1350. doi: 10.1111/bcp.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Branford R, Droney J, Ross JR. Opioid genetics: the key to personalized pain control? Clin Genet. 2012;82(4):301–310. doi: 10.1111/j.1399-0004.2012.01923.x. [DOI] [PubMed] [Google Scholar]
- 60.Droney J, Riley J, Ross JR. Evolving knowledge of opioid genetics in cancer pain. Clin Oncol (R Coll Radiol) 2011;23(6):418–428. doi: 10.1016/j.clon.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 61.Heiskanen T, Kalso E. Controlled-release oxycodone and morphine in cancer related pain. Pain. 1997;73(1):37–45. doi: 10.1016/S0304-3959(97)00072-9. [DOI] [PubMed] [Google Scholar]
- 62.Mucci-LoRusso P, Berman BS, Silberstein PT, et al. Controlled-release oxycodone compared with controlled-release morphine in the treatment of cancer pain: a randomized, double-blind, parallel-group study. Eur J Pain. 1998;2(3):239–249. doi: 10.1016/S1090-3801(98)90020-9. [DOI] [PubMed] [Google Scholar]
- 63.Bruera E, Belzile M, Pituskin E, et al. Randomized, double-blind, cross-over trial comparing safety and efficacy of oral controlled-release oxycodone with controlled-release morphine in patients with cancer pain. J Clin Oncol. 1998;16(10):3222–3229. doi: 10.1200/JCO.1998.16.10.3222. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.