Abstract
Background:
Costs attributable to criminal activity are a major component of the economic burden of substance use disorders, yet there is a paucity of empirical evidence on this topic. Our aim was to estimate the costs of crime associated with different forms and intensities of stimulant use.
Methods:
Retrospective cohort study, including individuals from three prospective cohorts in Vancouver, Canada, measured biannually (2011-2015), reporting stimulant use at baseline assessment. Monthly crime costs included policing, court, corrections, and criminal victimization (2016 CAD). We estimated monthly crime costs associated with mutually exclusive categories of crack, cocaine, methamphetamine, and polystimulant use, stratified by daily/non-daily use, relative to stimulant abstinence, as well as the independent effects of treatment (opioid agonist (OAT) and other addiction treatment). We used a two-part model, capturing the probability of criminal activity and costs of crime with generalized linear logistic and gamma regression models, respectively, controlling for age, gender, education, homelessness, mental health issues, employment, prior incarceration, alcohol and opioid use.
Results:
The study sample included 1,599 individuals (median age 39, 65.9% male) assessed over 5299 biannual interviews. Estimates of associated monthly crime costs ranged from $5449 [95%C.I.: $2180, $8719] for non-daily polystimulant use, to $8893 [$4196, $13,589] for daily polystimulant use. Cost differences between daily/non-daily use, injection/non-injection, and stimulant type were not statistically significant. Drug treatment was not associated with lower monthly crime costs in our sample.
Conclusions:
Substantial crime-related costs were associated with stimulant use, emphasizing the urgency for development and implementation of efficacious treatment regimens.
1.0. Introduction
Criminal activity is one of the largest components of the total societal costs attributable to illicit drug use in Canada and around the world. It is estimated that the direct costs (e.g. healthcare, law enforcement) of illicit drug use were as high as $3.57 billion (CAD) in Canada in 2002, with law enforcement costs comprising over 65% (Rehm et al., 2007). Direct costs have been estimated at $52.2 billion (USD) in the United States in 2007, with crime costs accounting for over 69% (National Drug Intelligence Center, 2011). Worldwide, stimulant use disorders are the second most common illicit drug use disorder after opioids, and the majority of the disease burden associated with stimulant use comes from cocaine (crack cocaine and cocaine hydrochloride) and amphetamines (specifically methamphetamine (MA)) (Degenhardt et al., 2014). Globally, MA use is more problematic than cocaine, due to dramatic physiological changes and sensitization in chronic users, as well as significantly higher prevalence beyond North and South America (Degenhardt et al., 2014; Degenhardt et al., 2013). In a literature review of studies estimating the economic benefits of addiction interventions, McCollister and French (2003) found that reductions in crime accounted for more than half of the total economic benefit in the majority of studies. More recent studies for treatment interventions found criminal activity to account for over 75% of accumulated lifetime direct costs for individuals with opioid use disorders (Nosyk et al., 2012), as well as a major component of total costs in other studies (Byford et al., 2013; Dijkgraaf et al., 2005; Zarkin et al., 2005).
High rates of drug use, particularly stimulants, among criminals have been observed in populations of arrestees and prison inmates (Karberg and James, 2005; ONDCP, 2014), however, the mechanism for the association between stimulant use and criminal activity is multifaceted (Goldstein, 1985). Pharmacological effects of stimulant use are well-known, and there is evidence that the risk of psychotic episodes and aggressive behavior increases in long-term users of methamphetamine (Harro, 2015), as well as similar neurocognitive problems in chronic cocaine users (Bolla et al., 1998). Furthermore, acute effects of drug use in reducing impulse control have been found to be more pronounced in stimulants than opiates (Badiani et al., 2011). Economic motivations for criminal activity stemming from stimulant use (such as acquisitive crime and other income generating activities) are perhaps the most direct mechanism for this relationship, given the high cost of illicit drugs (Bennett et al., 2008; Hepburn et al., 2016; Wilkins and Sweetsur, 2011).
Despite a large literature on the association between drug use and criminal behaviour, there are few studies examining the effects of stimulant use on criminal activity and associated costs. Flynn et al. (1999) estimated a range of $18,244 - $33,609 for yearly costs of crime of among untreated cocaine-dependent individuals, with significantly lower costs during and after treatment. Oser et al. (2011) found that stimulant use was associated with increased criminal activity amongst rural drug users, compared to no stimulant use. Vaughn et al. (2010) found that crack cocaine use was associated with higher odds of violence than powdered cocaine. However, the authors concluded that other heterogeneity in users was largely contributing to these differences. In a systematic review and meta-analysis, Bennett et al. (2008) found that the odds of offending was 1.9 times higher for amphetamine users and 6 times higher for crack users, compared to non-drug users.
To date, no effective pharmacological treatments have been identified for stimulant use disorders (Fischer et al., 2015). Contingency management and cognitive behavioural therapies (CM/CBT) have shown efficacy in trial-based settings, particularly short-run CM interventions, in which participants receive a prize or reward for maintaining abstinence (DeFulio et al., 2009; Jaffe et al., 2007; McKay et al., 2010; Rawson et al., 2006; Schumacher et al., 2007; Shoptaw et al., 2005). However, treatment modalities are far from standardized, and treatment utilization and outcomes are not systematically tracked in the province of British Columbia or elsewhere across Canada.
The goal of this study was to test a series of hypotheses about the association between stimulant use and crime costs. First, that stimulant use (stratified by type and use intensity) is positively associated with crime costs, relative to stimulant abstinence; second, that higher frequency of use is associated with higher crime costs within stimulant types; third, that different stimulant types and polystimulant use are associated with different levels of crime costs, holding intensity of use constant; and finally, that injection use is associated with higher crime costs than non-injection use within stimulant types.
2.0. Methods
2.1. Study Sample
Data for this analysis was derived from a series of ongoing open prospective cohort studies, conducted in Vancouver, involving people who use drugs, including the At-Risk Youth Study (ARYS), the AIDS Care Cohort to evaluate Exposure to Survival Services (ACCESS), and the Vancouver Injection Drug Users Study (VIDUS). The VIDUS study follows HIV-negative adults who inject drugs while the ACCESS study follows HIV-positive adults who inject drugs (Strathdee et al., 1997; Wood et al., 2009). ARYS is made up of street-involved youth aged 14-26 who report use of drugs other than, or in addition to, cannabis (Wood et al., 2006a; Wood et al., 2006b). Sampling and follow-up methodologies have been described in previous studies and surveys were structured identically to allow for combined longitudinal analysis (Strathdee et al., 1997; Tyndall et al., 2003; Wood et al., 2006a; Wood et al., 2006b). At baseline and semiannually thereafter, participants completed an interviewer-administered questionnaire and received $30 CAD at each visit. All studies were approved by the University of British Columbia/Providence Health Care Research Ethics Board.
Individuals included in this analysis entered the study between September 2005 and December 2013, and the data were collected from December 2011 to May 2015 to coincide with the inclusion of survey items comprehensively capturing criminal activity. During this period, individuals could have a maximum of seven biannual assessments. All individuals who had completed at least one follow-up interview during this period were eligible for inclusion. In addition, individuals were excluded if they had never reported stimulant use prior to the start of our sample period or at baseline. The reference group for our main analysis was past stimulant users who reported abstinence (no use of any stimulant drugs in the previous six months) at the time of assessment.
2.2. Crime Costs
Detailed survey questions included both the type and frequency of criminal acts committed in the past 30 days, categorized as violent offenses (such as assault, murder and weapons offenses), property crimes, drug dealing, sex work, legal status violation, disorderly conduct, and other offenses. Questions also included number of days incarcerated, on parole or under legal supervision in the past 30 days. Costs were assigned to each act by both the type of crime, as well as unit costs for the relevant expenditure categories. Monthly crime costs included all self-reported incidents of criminal activity, regardless of whether or not an individual was arrested for a particular act. Costs were calculated from a societal perspective, and included costs regardless of who incurred them or whether they corresponded directly to budgetary expenditures (Garrison et al., 2010). Total monthly crime costs were the combined costs of incident costs (police response), arrest processing and court costs for the criminal justice system, and criminal victimization (Krebs et al., 2014) (unit costs are presented in Supplementary material). Incident costs were derived from the overall operating budget of the Vancouver Police department, which captured the costs of police response to crime scenes, whether or not an arrest was made (Krebs et al., 2014). Arrest processing and court costs were assigned to acts where an individual reported being arrested, and incarceration costs to days an individual reported being incarcerated or on parole in the previous month. Victimization costs included medical expenses, cash losses and pain-and-suffering based on jury-compensation for victims (McCollister et al., 2010). Victimization costs were applied to violent offenses based on estimates for assaults, and property crimes as a weighted average based on cost estimates for break and enter and theft in McCollister et al. (2010), and the observed proportions of each type of crime in Vancouver, derived from the Vancouver Police Department and Statistics Canada (Krebs et al., 2014; McCollister et al., 2010). Incidents of sex work and drug dealing were only assigned costs if individuals reported being arrested, given that police are likely responding to only a fraction of total incidents (which we define as an individual reporting arrest), and were excluded from victimization costs, given the argument that these activities can be viewed as transactions with no direct costs of victimization (Dijkgraaf et al., 2005; Rajkumar and French, 1997; Zarkin et al., 2012). Monthly crime costs were adjusted to account for the proportion of days incarcerated in the past month.
2.3. Measures
Our primary independent variables were indicators of stimulant use in the past six months, grouped into one of eight mutually exclusive categories (Figure 1), including any use of powdered cocaine, daily or non-daily use of crack cocaine or methamphetamine, concurrent use of more than one stimulant drug (polystimulant), with daily use for polystimulant users specified as daily use of at least one stimulant, and a reference group of stimulant abstinent individuals. In addition to these categories, we also estimated the crime costs associated with individuals in treatment (either OAT or other non-OAT treatment modalities) in the previous six months.
Fig. 1.
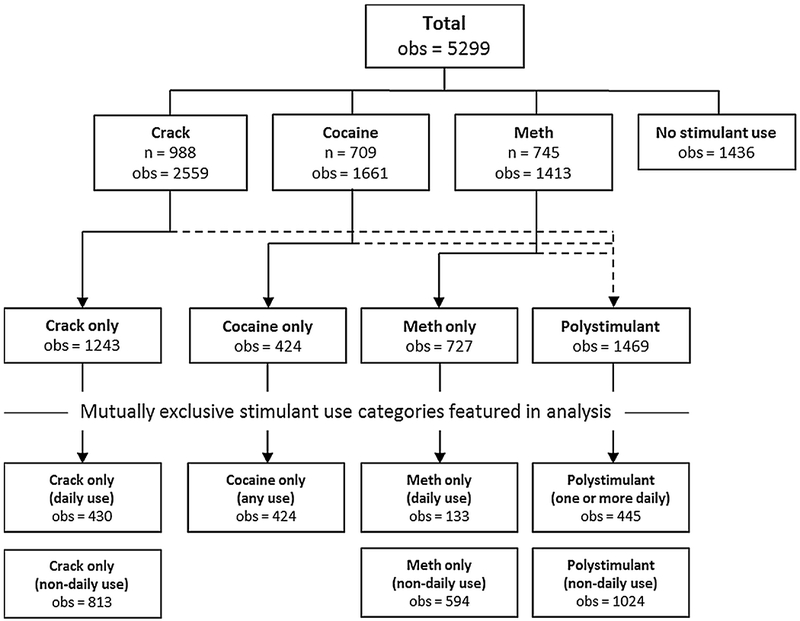
Observations within mutually exclusive stimulant use categories, and unique individuals reporting use of particular stimulant types at any assessment.
Baseline control variables included sex, education (completion of high school), and a history of incarceration. These were included to control for demographic and socioeconomic characteristics, as well as potential predisposition for criminality (Krebs et al., 2014). Time varying control variables included linear and quadratic age trends, homelessness, formal employment (full- or part-time), accessing mental health treatment, binge alcohol use, and opioid use, all in the previous six months. Indicators for homelessness and addiction treatment were included to control for their potential association with criminal activity, both directly and mediated through changes in drug use, specifically among opioid co-users (DeBeck et al., 2007; Schwartz et al., 2010). A variable for accessing mental health treatment was included to control for the potential association between mental health problems, drug use and criminal activity (Bolla et al., 1998; Harro, 2015). To test our hypothesis on the effects of injection drug use, we regressed crime costs on indicators for injection and concurrent injection/non-injection use in a subgroup of methamphetamine users. In this subgroup analysis, control variables were included for polystimulant use, and the reference group was non-injection MA users.
2.4. Statistical Analysis
Estimates for the association between stimulant use and monthly crime costs were derived using a two-part multiple regression model to account for the large number of observations with zero-valued monthly crime costs. The first part modeled the probability of having non-zero crime costs using a logit regression, while the second part estimated the level of non-zero costs using a Generalized Linear Model (GLM). For the GLM specification, we selected a log link function, and used modified Park tests to choose a gamma distribution for crime costs. We also estimated cluster-robust (Huber-White) standard errors to account for within-individual correlation of error terms resulting from repeated measures. We estimated marginal effects for both parts of the model, estimated at each individual’s respective covariate values. The resulting average marginal effects (AME) were interpreted as the population effect associated with stimulant use on monthly costs of crime, and were not conditional on individuals having positive crime costs. Data was prepared in SAS 9.4, and the analysis was conducted in Stata 14.1.
Given that cost data were derived from self-reported accounts of criminal activity, we chose a conservative approach consistent with Krebs et al. (2014) and excluded the top two percent of total crime cost observations from our final sample. This was done to limit the effect of extremely high cost and potentially uncertain responses on the representativeness of our results.
In sensitivity analysis, we examined two alternative scenarios to our baseline model, which considered costs from a societal perspective. First, we considered the perspective of a third-party payer, which only considered costs incurred by the criminal justice system (arrests, incidents and court costs) and not victimization costs. Second, we estimated our model using only costs of arrests and court proceedings, and not costs of incidents which were reported in survey assessments, but did not result in arrest. Finally, we estimated our model with the top outliers included, as well as a more restrictive upper bound in which we removed the top five percent of cost outliers for comparison.
3.0. Results
3.1. Study Sample Characteristics
A total of 1599 individuals (contributing 5299 observations, median of 3 [IQR: 2-4] per individual) met the primary inclusion criteria and 83.2% of individuals completed at least two assessments during the study period. Our sample was over 65.9% male, with 71.4% of individuals reporting prior incarceration at baseline. Summary statistics for our sample are presented in Table 1. Table 2 presents summary statistics for monthly crime costs by expenditure category, while Figure 1 depicts the number of observations by stimulant use category, and Figure 2 presents monthly crime costs by stimulant use category. Approximately half of all observations with crack cocaine and MA use (48.6% and 51.5% respectively) were individuals using only one type of stimulant drug, compared to 25.5% of powdered cocaine users. Additionally, individuals reported no criminal activity and had zero-valued monthly crime costs in 79.6% of all observations.
Table 1.
Descriptive statistics of individual baseline characteristics and time-varying covariates used in analysis.
| Baseline covariates (n = 1599) | Levels | n | (%) |
|---|---|---|---|
| Age (median [IQR]) | 39 [26,46] | – | – |
| Year of baseline assessment | <2007 | 786 | 49.2 |
| 2007–2009 | 504 | 31.5 | |
| >2009 | 309 | 19.3 | |
| Sex | Male | 1054 | 65.9 |
| Education | High School | 853 | 53.3 |
| Ever homeless | 1357 | 84.9 | |
| Ever in jail | 1141 | 71.4 | |
| Surveys completed | 1 | 269 | 16.8 |
| 2 | 289 | 18.1 | |
| 3 | 508 | 31.8 | |
| 4+ | 533 | 33.3 |
| Time-varying covariates (obs = 5299) | Levels | obs | (%) |
|---|---|---|---|
| Mental health treatment | 1843 | 34.8 | |
| Employed | 1389 | 26.2 | |
| Drug treatment | OAT | 1609 | 30.4 |
| Other (non-OAT) | 1838 | 34.7 | |
| Concurrent opioid use | 1943 | 36.7 | |
| Binge alcohol use | 1371 | 25.9 |
IQR – Interquartile range; OAT – Opioid agonist treatment.
Table 2.
Descriptive statistics for monthly crime cost components among observations with positive crime costs (2016 CAD).
| Incidents | Court | Corrections | Victimization | Total | |
|---|---|---|---|---|---|
| % Zero (of all obs) | 94.75 | 97.60 | 82.47 | 96.41 | 79.58 |
| Mean | $16,977 | $407 | $1677 | $2561 | $21,622 |
| SD | $56,211 | $1363 | $1358 | $9922 | $63,399 |
| Median | $0 | $0 | $1426 | $0 | $1426 |
| IQR | [$0, $4602] | [$0, $0] | [$1426, $1426] | [$0, $0] | [$1426, $6469] |
| 99th Percentile | $285,325 | $6389 | $7393 | $58,075 | $321,153 |
SD – Standard deviation; IQR – Interquartile range.
Descriptive statistics calculated for data used in baseline model specification, which excludes the top two percent of monthly crime cost outliers.
Fig. 2.
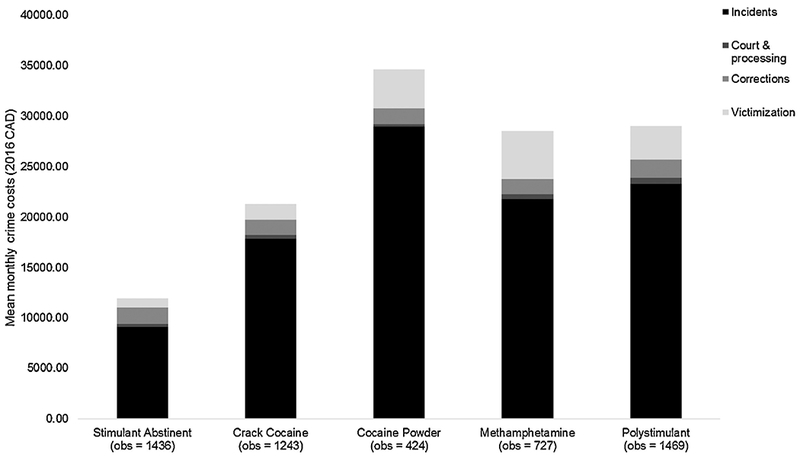
Average monthly crime costs among observations with positive crime costs, by mutually exclusive stimulant use group and expenditure category (2016 CAD).
3.2. Results of Two-Part Regression Models
In the baseline specification of our two-part model regression analysis, we found a positive and significant association between crime costs and MA, polystimulant and cocaine use, relative to abstinence (p < 0.05). AME estimates for associated monthly crime costs were $5449 [95% C.I. $2180, $8719] for non-daily polystimulant use, $5723 [$2013, $9434] for nondaily MA use, $5845 [$663, $11,028] for daily MA use, $5864 [$1220, $10,508] for powdered cocaine use, and $8893 [$4196, $13,589] for daily polystimulant use (Table 3). In addition to our comparison between stimulant use and stimulant abstinence, we also tested differences in crime costs between stimulant use categories, holding intensity of use constant (e.g. daily MA vs. daily crack cocaine, or non-daily MA vs. non-daily crack cocaine). We could not reject the null hypothesis of no difference in associated crime costs across stimulant use categories for either daily or non-daily use intensities. Although estimates for crime costs associated with daily use were higher within each stimulant use category, these differences were not significant. Finally, estimates for independent associations between OAT and non-OAT treatments, and monthly crime costs were not significant (Table 3).
Table 3.
Monthly crime costs associated with mutually exclusive categories of stimulant use, relative to stimulant abstinence, and daily vs. non-daily use intensity, derived from two-part multiple regression results (2016 CAD).
| Stimulant use vs. No use (1) |
Daily vs. Non-daily (2) |
||||
|---|---|---|---|---|---|
| Daily (n = 430) | $4441* | [−$153, $9034] | $976 | [−$4282, $6235] | |
| Crack Cocaine | Non-daily (n = 813) | $3464 | [−$830, $7758] | Reference | |
| No use (n = 1436) | Reference | ||||
| Daily (n = 133) | $5845** | [$663, $11,028] | $122 | [−$4968, $5212] | |
| Methamphetamine | Non-daily (n = 594) | $5723*** | [$2013, $9434] | Reference | |
| No use (n = 1436) | Reference | ||||
| Daily (n = 445) | $8893*** | [$4196, $13,589] | $3444* | [−$515, $7402] | |
| Polystimulant | Non-daily (n = 1024) | $5449*** | [$2180, $8719] | Reference | |
| No use (n = 1436) | Reference | ||||
| Powdered Cocaine | Any use (n = 424) | $5864** | [$1220, $10,508] | ||
| No use (n = 1436) | Reference | ||||
| Treatment (OAT) | Yes (n = 1609) | −$3722 | [−$8213, $769] | ||
| No (n = 3690) | Reference | ||||
| Other treatment (non-OAT) | Yes (n = 1838) | $1336 | [−$2672, $5343] | ||
| No (n = 3461) | Reference | ||||
Observations: 5299.
Control variables include: age, gender, education, history of incarceration, mental health issues, employment, homelessness, opioid use, and alcohol use.
Average marginal effect estimates presented with 95% confidence intervals in brackets.
p < 0.1
p < 0.05
p < 0.01
In addition to our baseline model, we also estimated monthly crime costs associated with injection vs. non-injection use in a subgroup of MA users. Neither estimate for injection or concurrent injection/non-injection MA use was significantly associated with higher crime costs relative to non-injection MA use (Table 4).
Table 4.
Monthly crime costs associated with mutually exclusive categories of injection and concurrent injection/non-injection use, relative to non-injection-only use, derived from two-part multiple regression results in methamphetamine user subgroup (2016 CAD).
| Injection vs. Non-injection (1) |
|||
|---|---|---|---|
| Methamphetamine | Injection (n = 602) | $6327* | [−$835, $13490] |
| Both (n = 406) | $1349 | [−$3849, $6547] | |
| Non-injection (n = 405) | Reference | ||
Observations: 1413.
Control variables include: age, gender, education, history of incarceration, mental health issues, employment, homelessness, polystimulant use, opioid use, and alcohol use. Average marginal effects presented with 95% confidence intervals in brackets.
p < 0.1.
3.3. Sensitivity Analysis
In sensitivity analysis of alternative payer perspectives, results were similar in direction and statistical significance, with slightly smaller magnitude when including only third-party payer costs. For estimates including arrests and court costs only, the magnitude of estimates was lower than either societal or third-party payer perspectives, and only daily methamphetamine, daily and non-daily polystimulant use categories were significantly higher than abstinence. Results of testing differences between daily and non-daily use as well as across drug types were robust. Lastly, when the top two percent of monthly crime cost observations were included in the sample, most associations were no longer significantly different from abstinence, with the exception of the daily polystimulant use, and results were robust, though smaller in magnitude, when the top five percent of monthly crime costs were excluded (results available in Supplementary material).
4.0. Discussion
4.1. Findings
We found a positive and significant association between stimulant use and monthly crime costs for powdered cocaine, MA and polystimulant use, relative to stimulant abstinence. We did not find significant differences between levels of use intensity within stimulant types, across stimulant types, or between routes of administration of methamphetamine.
Estimates for both OAT and other substance use treatment (non-OAT) did not allow us to conclude that either had independently beneficial effects amongst users in our analytic sample (i.e. a significant negative association with monthly crime costs). Since neither treatment was specifically targeted toward stimulant use, we were not necessarily expecting to observe a significant association with lower crime costs among those in our analytic sample, however, we wanted to consider the potential for positive spillover effects and increased pro-social behaviour resulting from any type of addiction treatment. This was informed by results from Krebs et al. (2014) and Krebs et al. (2016), which found that OAT was more effective in reducing crime costs among opioid users who were co-using stimulants. Although estimates for OAT in our study were not independently associated with lower crime costs, opioid users comprised only a subset of our analytic sample, as the inclusion criteria was not related to opioid use or OAT history. Additionally, our reference group for OAT was individuals not receiving OAT, regardless of concurrent stimulant or opioid use and cannot be directly compared to estimates reported elsewhere for OAT treatment among opioid users.
Our finding of positive and significant associations between monthly crime costs and drug use for the majority of stimulant use categories was consistent with other studies (Bennett et al., 2008; Oser et al., 2011), and similar in magnitude to crime cost estimates of drug users in-relapse or out-of-treatment, compared to in-treatment or abstinent (Flynn et al., 1999; Krebs et al., 2014; Krebs et al., 2016). Our finding that monthly crime costs associated with powdered cocaine use were not significantly different than crack cocaine was consistent with Vaughn et al. (2010), who found no differences in violent behavior after controlling for contextual variables and co-morbid disorders. Furthermore, our result that powdered cocaine, but not crack cocaine use, was significantly associated with higher monthly crime costs relative to stimulant abstinence, was contrary to results in Stewart et al. (2014) suggesting that crack cocaine was associated with higher amounts criminal activity. Due to differences in measurement for both drug use and criminal activity, however, these results are not directly comparable with our estimates. Additionally, this result may be due, in part, to a high proportion of injection users of powdered cocaine in our study, relative to the general population (Novak and Kral, 2011), which has shown to be associated with other high-risk behaviours (Lloyd-Smith et al., 2009; Tyndall et al., 2003).
The result that daily use was not associated with higher crime costs than non-daily use was somewhat surprising, however, this may have been affected by less precise estimates given the rarity of criminal activity and smaller group sizes, once users were stratified by daily and non-daily use. In addition, our measure for stimulant use intensity was may not have been sensitive enough to detect these differences. As such, the association between stimulant use intensity and crime costs remains an open question for future research. The literature on substance use and crime, as well as the neurological effects of binge stimulant use suggests that intensity of use may be an important moderator of the effects of drug use. In addition to nearly 80% of observations having zero-valued crime costs, over 60% of stimulant using individuals in our analytic sample reported no criminal activity throughout the duration of their follow-up. This illustrates what is typically the case; that criminal activity is a relatively rare event, and crime costs are characterized by a small number of events and individuals having a substantial influence on the total costs.
4.2. Limitations
There are several potential limitations to our analysis. First, that our data was collected via self-report surveys. Survey data has demonstrated to be a reliable measure for arrests when recall windows are appropriately short, with no consistent bias toward over or under reporting (Johnson et al., 2005). Since our survey instruments only asked respondents to report criminal activity from the past 30 days, it is unlikely that the length of recall time was a significant problem. In the case of drug use in particular, other studies have found that potential bias may go in the direction of underreporting, given the possibility of respondent mistrust of interviewers when reporting illegal activity (Johnson and Golub, 2007). Given that our analytic sample was from a longitudinal cohort in which over 80% of individuals were measured over multiple cycles, trust between respondents and interviewers was likely stronger than in cross-sectional surveys where respondents were only interviewed once.
While we accounted for observable heterogeneity by including a number of a priori-specified control variables in our regression analysis, there was still potential for unmeasured confounding. A common method to address this problem in panel data is fixed effects estimation, which uses each individual as his or her own control to eliminate time-invariant heterogeneity, whether observed or unobserved. Although this specification is not currently available for two-part model estimation packages, we were able to re-estimate Part I of our model using a fixed-effects logit specification for the probability of an individual having any crime costs in the previous six months. While this reduced the size of our analytical sample, as we could only estimate within-individual effects among the subset of those who exhibited variation in criminal activity over time, fixed-effects logit estimates for stimulant use were consistent in direction with Part I of our baseline model, though most estimates were smaller in magnitude and only daily MA use remained significantly higher than stimulant abstinence (Supplementary material).
Finally, caution must be exercised when generalizing these results. Injection drug use was a criterion for selection into the VIDUS and ACCESS studies, while 49.7% of individuals from the ARYS cohort included in our sample had used injection drugs. Our analytic sample was located in a unique urban Canadian setting, characterized by socioeconomic marginalization and easy access to illicit drug markets (DeBeck et al., 2007; Richardson et al., 2015; Ti et al., 2014). As a result, there are a number of contextual effects that may be quite different when dealing with a broader cross-section of stimulant users, including structural factors such as higher levels of policing activity and higher probabilities of police interaction and arrests among this cohort than might be the case in other settings.
4.3. Implications
As there are no evidence-based pharmacologic approaches for treating stimulant use disorders, and other promising forms of psychosocial therapy have yet to show persistent effects across settings or over longer time horizons, the implications of this study in estimating the benefits of treatment are largely hypothetical. The treatment variables included in our analysis represented an exploratory assessment of the potential for positive effects for stimulant users from non-stimulant-specific treatments, however, we would expect an effective, evidence-based treatment regimen for stimulant use disorders to have considerably larger effects. For example, if an effective treatment regimen was identified and capable of generating an 80% reduction in crime costs, similar to what has been recently estimated for OAT and opioid users (Krebs et al., 2014; Krebs et al., 2016), as well as individuals in long-term residential treatment for cocaine use disorders (Flynn et al., 1999), there are potential average monthly cost savings of $4691 per cocaine user, $4676 per daily MA user, and $7114 per daily polystimulant user treated. This is in addition to many other potential health benefits and cost savings, such as reduced health care costs, that could be generated by an effective treatment program (Baser et al., 2011; French and Martin, 1996). Even with all tangible costs such as policing, healthcare and victimization included, these estimates can still be considered a lower bound for the overall societal costs of criminal activity (Basu et al., 2008).
4.4. Conclusion
Most types of stimulant use were associated with increased monthly crime costs. If new, effective treatment modalities for stimulant use disorders can generate similar reductions in crime costs to what has been estimated for OAT, there are potentially large economic benefits, in addition to public health benefits, to reap from such treatments.
Supplementary Material
Acknowledgements
The authors thank the study participants for their contribution to the research, as well as current and past researchers and staff. Drs. Kora DeBeck, Kanna Hayashi, M-J Milloy and Lindsey Richardson are supported by Canadian Institutes of Health Research New Investigator Awards. Dr. Kora DeBeck is supported by a Michael Smith Foundation for Health Research/St. Paul’s Hospital Foundation–Providence Health Care Career Scholar Award and Drs. M-J Milloy, Bohdan Nosyk and Lindsey Richardson are supported by Michael Smith Foundation for Health Research Scholar Awards. This research was undertaken, in part, thanks to the funding from the Canada Research Chairs program through a Tier 1 Canada Research Chair in Inner City Medicine which supports Dr. Evan Wood. Dr. Bohdan Nosyk holds a St. Paul’s Hospital CANFAR Chair in HIV/AIDS Research.
Role of funding source
The VIDUS cohort study was supported by the US National Institutes of Health(U01DA038886), the ACCESS cohort study was supported by the US National Institutes of Health (R01DA021525), the ARYS cohort study was supported by the US National Institutes of Health (U01DA038886) and the Canadian Institutes of Health Research(MOP-286532). This study was supported by the Canadian Institutes of Health Research (MOP-133538).
Footnotes
Conflicts of interest
None to declare.
References
- Badiani A, Belin D, Epstein D, Calu D, Shaham Y, 2011. Opiate versus psychostimulant addiction: the differences do matter. Nat Rev Neurosci 12, 685–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baser O, Chalk M, Fiellin DA, Gastfriend DR, 2011. Cost and utilization outcomes of opioid-dependence treatments. Am J Manag Care 17, S235–248. [PubMed] [Google Scholar]
- Basu A, Paltiel AD, Pollack HA, 2008. Social costs of robbery and the cost-effectiveness of substance abuse treatment. Health Econ 17, 927–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett T, Holloway K, Farrington D, 2008. The statistical association between drug misuse and crime: A meta-analysis. Aggression and Violent Behavior 13, 107–118. [Google Scholar]
- Bolla KI, Cadet JL, London ED, 1998. The neuropsychiatry of chronic cocaine abuse. J Neuropsychiatry Clin Neurosci 10, 280–289. [DOI] [PubMed] [Google Scholar]
- Byford S, Barrett B, Metrebian N, Groshkova T, Cary M, Charles V, Lintzeris N, Strang J, 2013. Cost-effectiveness of injectable opioid treatment v. oral methadone for chronic heroin addiction. The British Journal of Psychiatry 203, 341–349. [DOI] [PubMed] [Google Scholar]
- DeBeck K, Shannon K, Wood E, Li K, Montaner J, Kerr T, 2007. Income generating activities of people who inject drugs. Drug and Alcohol Dependence 91, 50–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeFulio A, Donlin WD, Wong CJ, Silverman K, 2009. Employment-based abstinence reinforcement as a maintenance intervention for the treatment of cocaine dependence: a randomized controlled trial. Addiction 104, 1530–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Baxter AJ, Lee YY, Hall W, Sara GE, Johns N, Flaxman A, Whiteford HA, Vos T, 2014. The global epidemiology and burden of psychostimulant dependence: findings from the Global Burden of Disease Study 2010. Drug Alcohol Depend 137, 36–47. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Whiteford HA, Ferrari AJ, Baxter AJ, Charlson FJ, Hall WD, Freedman G, Burstein R, Johns N, Engell RE, Flaxman A, Murray CJ, Vos T, 2013. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010. Lancet 382, 1564–1574. [DOI] [PubMed] [Google Scholar]
- Dijkgraaf MG, van der Zanden BP, de Borgie CA, Blanken P, van Ree JM, van den Brink W, 2005. Cost utility analysis of co-prescribed heroin compared with methadone maintenance treatment in heroin addicts in two randomised trials. Bmj 330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer B, Kuganesan S, Gallassi A, Malcher-Lopes R, van den Brink W, Wood E, 2015. Addressing the stimulant treatment gap: A call to investigate the therapeutic benefits potential of cannabinoids for crack-cocaine use. Int J Drug Policy 26, 1177–1182. [DOI] [PubMed] [Google Scholar]
- Flynn PM, Kristiansen PL, Porto JV, Hubbard RL, 1999. Costs and benefits of treatment for cocaine addiction in DATOS. Drug Alcohol Depend 57, 167–174. [DOI] [PubMed] [Google Scholar]
- French MT, Martin RF, 1996. The costs of drug abuse consequences: a summary of research findings. J Subst Abuse Treat 13, 453–466. [DOI] [PubMed] [Google Scholar]
- Garrison LP Jr., Mansley EC, Abbott TA 3rd, Bresnahan BW, Hay JW, Smeeding J, 2010. Good research practices for measuring drug costs in cost-effectiveness analyses: a societal perspective: the ISPOR Drug Cost Task Force report--Part II. Value Health 13, 8–13. [DOI] [PubMed] [Google Scholar]
- Goldstein PJ, 1985. The drugs/violence nexus: A tripartite conceptual framework. Journal of drug issues 15, 493–506. [Google Scholar]
- Harro J, 2015. Neuropsychiatric Adverse Effects of Amphetamine and Methamphetamine. Int Rev Neurobiol 120, 179–204. [DOI] [PubMed] [Google Scholar]
- Hepburn K, Barker B, Nguyen P, Dong H, Wood E, Kerr T, DeBeck K, 2016. Initiation of drug dealing among a prospective cohort of street-involved youth. Am J Drug Alcohol Abuse 42, 507–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffe A, Shoptaw S, Stein J, Reback CJ, Rotheram-Fuller E, 2007. Depression ratings, reported sexual risk behaviors, and methamphetamine use: latent growth curve models of positive change among gay and bisexual men in an outpatient treatment program. Exp Clin Psychopharmacol 15, 301–307. [DOI] [PubMed] [Google Scholar]
- Johnson BD, Golub A, 2007. The potential for accurately measuring behavioral and economic dimensions of consumption, prices, and markets for illegal drugs. Drug Alcohol Depend 90, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BD, Taylor A, Golub A, 2005. Research Note: How Accurate are Arrestees’ Self-Reports of Their Criminal Justice Histories? Justice Research and Policy 7, 81–101. [Google Scholar]
- Karberg JC, James DJ, 2005. Substance dependence, abuse, and treatment of jail inmates, 2002 US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; Washington, DC. [Google Scholar]
- Krebs E, Kerr T, Montaner J, Wood E, Nosyk B, 2014. Dynamics in the costs of criminality among opioid dependent individuals. Drug Alcohol Depend 144, 193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs E, Urada D, Evans E, Huang D, Hser YI, Nosyk B, 2016. The costs of crime during and after publicly-funded treatment for opioid use disorders: a population-level study for the state of California. Addiction 15, 13729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Smith E, Wood E, Li K, Montaner JSG, Kerr T, 2009. Incidence and determinants of initiation into cocaine injection and correlates of frequent cocaine injectors. Drug and Alcohol Dependence 99, 176–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCollister KE, French MT, 2003. The relative contribution of outcome domains in the total economic benefit of addiction interventions: a review of first findings. Addiction 98, 1647–1659. [DOI] [PubMed] [Google Scholar]
- McCollister KE, French MT, Fang H, 2010. The cost of crime to society: new crime-specific estimates for policy and program evaluation. Drug Alcohol Depend 108, 98–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Coviello D, Morrison R, Cary MS, Skalina L, Plebani J, 2010. Randomized trial of continuing care enhancements for cocaine-dependent patients following initial engagement. J Consult Clin Psychol 78, 111–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Drug Intelligence Center, 2011. The Economic Impact of Illicit Drug Use on American Society.
- Nosyk B, Guh DP, Bansback NJ, Oviedo-Joekes E, Brissette S, Marsh DC, Meikleham E, Schechter MT, Anis AH, 2012. Cost-effectiveness of diacetylmorphine versus methadone for chronic opioid dependence refractory to treatment. Cmaj 184, 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak SP, Kral AH, 2011. Comparing Injection and Non-Injection Routes of Administration for Heroin, Methamphetamine, and Cocaine Uses in the United States. Journal of addictive diseases 30, 248–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ONDCP, 2014. ADAM II 2013 Annual Report. Washington, D.C. [Google Scholar]
- Oser C, Leukefeld C, Staton-Tindall M, Duvall J, Garrity T, Stoops W, Falck R, Wang J, Carlson R, Sexton R, Wright P, Booth B, 2011. Criminality Among Rural Stimulant Users in the United States. Crime Delinq 57, 600–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar AS, French MT, 1997. Drug abuse, crime costs, and the economic benefits of treatment. Journal of Quantitative Criminology 13, 291–323. [Google Scholar]
- Rawson RA, McCann MJ, Flammino F, Shoptaw S, Miotto K, Reiber C, Ling W, 2006. A comparison of contingency management and cognitive-behavioral approaches for stimulant-dependent individuals. Addiction 101, 267–274. [DOI] [PubMed] [Google Scholar]
- Rehm J, Gnam W, Popova S, Baliunas D, Brochu S, Fischer B, Patra J, Sarnocinska-Hart A, Taylor B, 2007. The costs of alcohol, illegal drugs, and tobacco in Canada, 2002. J Stud Alcohol Drugs 68, 886–895. [DOI] [PubMed] [Google Scholar]
- Richardson LA, Long C, DeBeck K, Nguyen P, Milloy MJS, Wood E, Kerr TH, 2015. Socio-economic marginalization in the structural production of vulnerability to violence among people who use illicit drugs. Journal of epidemiology and community health 69, 686–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher JE, Milby JB, Wallace D, Meehan DC, Kertesz S, Vuchinich R, Dunning J, Usdan S, 2007. Meta-analysis of day treatment and contingency-management dismantling research: Birmingham Homeless Cocaine Studies (1990-2006). J Consult Clin Psychol 75, 823–828. [DOI] [PubMed] [Google Scholar]
- Schwartz B, Wetzler S, Swanson A, Sung SC, 2010. Subtyping of substance use disorders in a high-risk welfare-to-work sample: a latent class analysis. J Subst Abuse Treat 38, 366–374. [DOI] [PubMed] [Google Scholar]
- Shoptaw S, Reback CJ, Peck JA, Yang X, Rotheram-Fuller E, Larkins S, Veniegas RC, Freese TE, Hucks-Ortiz C, 2005. Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug Alcohol Depend 78, 125–134. [DOI] [PubMed] [Google Scholar]
- Stewart MJ, Fulton HG, Barrett SP, 2014. Powder and crack cocaine use among opioid users: is all cocaine the same? J Addict Med 8, 264–270. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Patrick DM, Currie SL, Cornelisse PG, Rekart ML, Montaner JS, Schechter MT, O’Shaughnessy MV, 1997. Needle exchange is not enough: lessons from the Vancouver injecting drug use study. Aids 11, F59–65. [DOI] [PubMed] [Google Scholar]
- Ti L, Richardson L, DeBeck K, Nguyen P, Montaner J, Wood E, Kerr T, 2014. The impact of engagement in street-based income generation activities on stimulant drug use cessation among people who inject drugs. Drug Alcohol Depend 141, 58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyndall MW, Currie S, Spittal P, Li K, Wood E, O’Shaughnessy MV, Schechter MT, 2003. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. Aids 17, 887–893. [DOI] [PubMed] [Google Scholar]
- Vaughn MG, Fu Q, Perron BE, Bohnert AS, Howard MO, 2010. Is crack cocaine use associated with greater violence than powdered cocaine use? Results from a national sample. Am J Drug Alcohol Abuse 36, 181–186. [DOI] [PubMed] [Google Scholar]
- Wall R, Rehm J, Fischer B, Brands B, Gliksman L, Stewart J, Medved W, Blake J, 2000. Social costs of untreated opioid dependence. J Urban Health 77, 688–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkins C, Sweetsur P, 2011. The association between spending on methamphetamine/amphetamine and cannabis for personal use and earnings from acquisitive crime among police detainees in New Zealand. Addiction 106, 789–797. [DOI] [PubMed] [Google Scholar]
- Wood E, Kerr T, Marshall BD, Li K, Zhang R, Hogg RS, Harrigan PR, Montaner JS, 2009. Longitudinal community plasma HIV-1 RNA concentrations and incidence of HIV-1 among injecting drug users: prospective cohort study. Bmj 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood E, Stoltz JA, Li K, Montaner JS, Kerr T, 2006a. Changes in Canadian heroin supply coinciding with the Australian heroin shortage. Addiction 101,689–695. [DOI] [PubMed] [Google Scholar]
- Wood E, Stoltz JA, Montaner JS, Kerr T, 2006b. Evaluating methamphetamine use and risks of injection initiation among street youth: the ARYS study. Harm Reduct J 3, 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarkin GA, Cowell AJ, Hicks KA, Mills MJ, Belenko S, Dunlap LJ, Houser KA, Keyes V, 2012. Benefits and Costs of Substance Abuse Treatment Programs for State Prison Inmates: Results from a Lifetime Simulation Model. Health Econ 21, 633–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarkin GA, Dunlap LJ, Hicks KA, Mamo D, 2005. Benefits and costs of methadone treatment: results from a lifetime simulation model. Health Econ 14, 1133–1150. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


