Abstract
Tectal glioma (TG) is a rare low-grade tumor occurring predominantly in the pediatric population. There has been no detailed analysis of molecular alterations in TG. Risk factors associated with inferior outcome and long-term sequelae of TG have not been well-documented. We retrospectively studied TGs treated or referred for review at St. Jude Children’s Research Hospital (SJCRH) between 1986 and 2013. Longitudinal clinical data were summarized, imaging and pathology specimen centrally reviewed, and tumor material analyzed with targeted molecular testing and genome-wide DNA methylation profiling. Forty-five patients with TG were included. Twenty-six (57.8%) were male. Median age at diagnosis was 9.9 years (range, 0.01–20.5). Median follow-up was 7.6 years (range, 0.5–17.0). The most common presenting symptoms were related to increased intracranial pressure. Of the 22 patients treated at SJCRH, 19 (86%) required cerebrospinal fluid diversion and seven (32%) underwent tumor-directed surgery. Five patients (23%) received radiation therapy and four (18%) systemic therapy. Ten-year overall and progression-free survival were 83.9 ± 10.4% and 48.7 ± 14.2%, respectively. Long-term morbidities included chronic headaches, visual symptoms and neurocognitive impairment. Lesion ≥3cm2, contrast enhancement and cystic changes at presentation were risk factors for progression. Among those with tumor tissue available, 83% showed growth patterns similar to pilocytic astrocytoma and 17% aligned best with diffuse astrocytoma. BRAF duplication (a marker of KIAA1549-BRAF fusion) and BRAF V600E mutation were detected in 25% and 7.7%, respectively. No case had histone H3 K27M mutation. DNA methylation profile of TG was distinct from other brain tumors. In summary, TG is an indolent, chronic disease with unique clinical and molecular profiles and associated with long term morbidities. Large size, contrast enhancement and cystic changes are risk factors for progression.
Electronic supplementary material
The online version of this article (10.1186/s40478-018-0602-5) contains supplementary material, which is available to authorized users.
Keywords: Tectal glioma, Imaging findings, Prognostic factors, Histopathology, DNA methylation profiling, Long-term follow-up
Introduction
Tectal glioma (TG) is a rare tumor with a predilection for the pediatric population [18]. It involves critical locations in the brainstem including superior and inferior colliculi and the narrow passage of aqueduct of Sylvius. TG may be diagnosed by its typical appearance on imaging and, if biopsied, as a low-grade glioma (LGG) histologically. Given the usual indolent course and risk associated with resection in such an eloquent area, the general recommendation is close observation after CSF diversion for hydrocephalus. Many studies on patient outcome are based on neurosurgical series with possible bias [5, 8, 9, 16, 17, 20, 22, 25, 26, 28, 32, 38, 42, 43, 45, 48]. Data on progression predictors, long-term morbidities, and molecular features of this peculiar group of LGG are lacking. We report comprehensively the clinical, neurocognitive, imaging, histologic and molecular features of TG cases treated or reviewed at St. Jude Children’s Research Hospital (SJCRH) over three decades. We found that while clinically indolent, TG is associated with significant long-term morbidities. Although morphologically similar to pilocytic astrocytoma (PA) of other sites of the central nervous system, TG shows a distinct DNA methylation profile. We have identified large size, contrast enhancement and cystic changes as risk factors for progression.
Material and methods
Study population
Forty-five patients with TG treated (n = 22) or referred for case review (n = 23) at SJCRH between January 1986 and December 2017 were reviewed. Diagnosis was based on typical imaging findings (tumor intrinsic to or centered in the tectal plate) and supported by histopathology when available. Comprehensive clinical, imaging and histopathologic data were reviewed as available. Long-term morbidities, including those affecting neurocognitive function were summarized.
MRI and image analysis
MR images acquired at diagnosis and first progression, if applicable, were centrally reviewed by a board-certified neuroradiologist (JHH). Each tumor was measured in three orthogonal planes, assessed for T1 and T2 signal intensity and circumscription, and graded for the proportions of cystic and/or enhancing tumor components and enhancement avidity at each time-point. The relative apparent diffusion coefficient (rADC) was calculated relative to normal-appearing cerebellum [23]. Progressive disease (PD) was defined as an increase of ≥25% in the product of the two greatest perpendicular diameters compared to baseline [49].
Histopathologic and molecular studies
The histopathology of cases with available tissue (n = 30) was centrally reviewed by a board-certified neuropathologist (JC). For immunohistochemistry, we used antibodies against GFAP (Ventana, 760–4345, prediluted), Olig2 (Cell Marque, 387 M-15, diluted 1:50), neurofilament (Ventana, 760–2661, prediluted), and Ki67 (Dako, M7240, diluted 1:100). Histone H3 K27M mutant proteins were detected with a rabbit polyclonal antibody (EMD Millipore, ABE419, diluted 1:600). BRAF V600E mutant protein was detected with a mouse monoclonal antibody (Ventana, 790–4855, prediluted). Chromosome 7q34 duplication, a surrogate marker for KIAA1549-BRAF fusion, was detected by interphase fluorescence in situ hybridization (iFISH) with a probe developed in-house (information available upon request).
Genome-wide DNA methylation profiling and analysis
Genomic DNA (≥250 ng from each sample) was extracted from formalin-fixed paraffin-embedded (FFPE) tissue from nine TG samples with adequate tissue and analyzed using Illumina Infinium MethylationEPIC BeadChip arrays in accordance with the manufacturer’s instructions. Nineteen non-NF1 hypothalamic PAs (HTPAs, n = 9) and cerebellar PAs (CBPAs, n = 10) were also retrieved from the institutional tumor bank for comparison. Reference methylation profiles of 8 brain tumor entities (rosette-forming glioneuronal tumor, dysembryoplastic neuroepithelial tumor, ganglioglioma, subependymal giant cell astrocytoma, MYB-altered low-grade glioma, histone H3 K27M-mutant diffuse midline glioma, and IDH-mutant diffuse astrocytoma / oligodendroglioma) and normal tissue from the hypothalamus, pons, cerebellum and white matter were obtained from publicly available database for comparison [6]. Array data analysis was performed using R v.3.5.0 with several packages from Bioconductor [36]. Raw signal intensities were obtained from IDAT files by using minfi package v.1.26.0 and normalized by performing background correction and a dye-bias correction for both color channels with the functional normalization method [2, 13]. Poor quality (P > 0.01) and failed probes (n = 29,567) were removed from the downstream analysis. The following filtering criteria were applied: removal of probes targeting the X and Y chromosomes (n = 8971), removal of probes containing single-nucleotide polymorphism (n = 13,776), and removal of probes not mapping uniquely to the human reference genome (hg19) allowing for one mismatch (n = 3965). In total, 400,253 probes targeting CpG sites were kept. Beta-values of the 1000 most variable CpG sites were derived for further analysis. t-SNE analysis was performed using Rtsne package v.0.13 with theta = 0.0 [24, 44]. Agglomerative nesting hierarchical clustering analysis was performed using cluster package v.2.0.7-1 with Euclidean distances and a generalized average method [27].
Neuropsychologic evaluation
Cognitive assessments performed at SJCRH were reviewed (n = 10) for evidence of long-term neurocognitive impairment. For patients with multiple assessments, data from the most recent assessment were used. The cognitive domains most consistently included for analysis were global intelligence, working memory, processing speed, and academics (i.e., word reading and math calculation). Global intelligence (estimated or full-scale IQ score) was assessed with age-appropriate Wechsler scale or the Differential Abilities Scale, Second Edition [11, 47]. Working memory and processing speed were assessed with age appropriate Wechsler scale. Academics were assessed with Woodcock-Johnson Tests of Achievement, Wide Range Achievement Test, or Wechsler Individual Achievement Test [19, 46, 50]. All age-standardized scores were converted to z-scores (mean = 0 and standard deviation = 1). Impairment was defined as a z-score ≥ -1.33 (ninth percentile).
Statistical analysis
Statistical analysis was performed with R v.3.5.0. The date of diagnosis was defined as the date of the MRI on which the tumor was first detected. Progressive disease (PD) was defined by radiologic progression, together with clinical deterioration and/or a need for intervention. Tumor size and rADC were compared between baseline and progression by paired t-test. Survival analysis was performed with the Kaplan-Meier method. Overall survival (OS) was determined as the duration between diagnosis and death from any cause or last follow-up, whichever was earlier. Progression-free survival (PFS) was determined as the duration between diagnosis and the first detection of PD, death from any cause, or last follow-up, whichever was earlier. Variables were analyzed for their impact on survival by the log-rank test or the Cox proportional hazards model.
Results
Demographic and presenting features
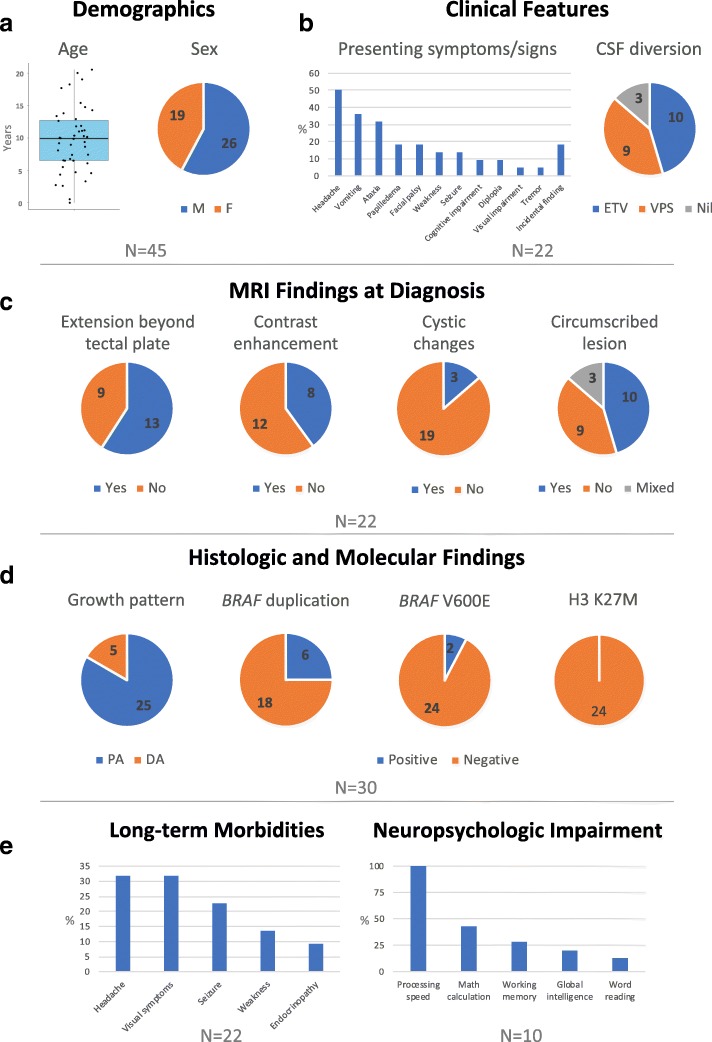
Forty-five patients with TG were included in this study (Fig. 1, Additional file 1: Figure S1). Twenty-six (58%) were males, and the median age of diagnosis was 9.9 years (range, 0.01–20.5). Among the 22 patients treated at SJCRH, two had neurofibromatosis type-1 (NF1) and four were diagnosed incidentally: one through antenatal ultrasound and three with failed vision screening (Additional file 2: Table S1). The other patients most commonly presented with headaches (n = 11) (Fig. 1). The median duration of symptoms before diagnosis was 0.46 year (range, 1 week-7.3 years). In the three patients for whom presentation preceded diagnosis by ≥6 years, a ventriculoperitoneal (VP) shunt was inserted for hydrocephalus because of a presumed aqueductal stenosis seen on CT; TG was diagnosed only after subsequent MRI (performed because of seizures in two patients and diplopia in one). One out of the 13 patients who underwent complete imaging with MRI brain and spine at diagnosis had evidence of metastasis.
Fig. 1.
a Demographics, b clinical features, c imaging characteristics, d histologic and molecular findings, and e long-term morbidities in patients with tectal glioma
CSF diversion and surgical and nonsurgical interventions
CSF diversion was required in 19/22 (86%) patients, being performed at presentation in all cases (Fig. 1, Table 1). The initial procedure was an endoscopic third ventriculostomy (ETV) in 10 patients and VP shunting in nine; an Ommaya reservoir was also inserted in eight patients who underwent ETV. Of those who underwent VP shunting, six (67%) required shunt revisions (range, 1–12 times) and one eventually required an ETV. Two patients had a subdural hematoma due to over-shunting, requiring evacuation. Of the patients who had ETV upfront, two (20%) experienced failure necessitating VP shunt placement. Tumor-directed surgery was performed in seven (32%) patients treated at SJCRH. Three had biopsies (two upfront, one at progression), three underwent gross-total resection (GTR) (one upfront, two at progression), and one underwent resection of a spinal metastasis at progression. Two of the patients who underwent GTR developed profound neurologic morbidities due to stroke. Five patients (23%) received focal radiotherapy at 54–55.8Gy: as upfront adjuvant therapy in two cases and at progression in three. One patient suffered from symptomatic radionecrosis requiring steroid and bevacizumab. Systemic therapy was used in four patients (18%) at progression, including one who received RT; a carboplatin-containing regimen was adopted in three out of these patients.
Table 1.
Interventions and outcomes for patients treated at SJCRH
| No. | CSF diversion (no. of revision[s]) |
Ommaya | Surgery | Chemotherapy | RT | Indication for adjuvant | Long-term sequelae | Outcome | Duration of follow-up (y) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | VPS (1) | No | Bx upfront | Nil | 54 Gy | Upfront | Seizure; memory issues | Alive with SD | 12.67 |
| 2 | VPS (6) | No | Bx at progression, then repeated drainage of cyst; and GTR × 2 | POG9060 (ifosfamide) | 55.8 Gy | Multiple PD | Learning difficulties | Died of shunt failure | 6.78 |
| 3 | VPS (subdural) | No | Nil | Nil | Nil | N/A | HA + diplopia | Died of obstructive hydrocephalus | 7.72 |
| 4 | VPS (12) → ETV (1) | No | Nil | Carboplatin + tamoxifen | Nil | PD | HA, N, V, nystagmus, OA, VF defect, R CN VII deficit, hypopituitarism | Died of suicide | 10.72 |
| 5 | VPS (subdural) | No | Nil | Nil | Nil | N/A | Nil | Alive with SD | 16.98 |
| 6 | VPS | No | Nil | Nil | Nil | N/A | Spastic quadriplegic CP, epilepsy, severe mental retardation, | Alive with SD | 13.97 |
| 7 | VPS (2) | No | Bx upfront, then resection of spinal metastasis at progression | 1. Carboplatin + vincristine + temozolomide 2. Lomustine + procarbazine + vincristine |
Nil | PD (metastasis) | GHD, epilepsy off medications | Alive with SD | 11.24 |
| 8 | Nil | No | Nil | Nil | N/A | Migraine | Alive with SD | 11.28 | |
| 9 | ETV → VPS at progression | No | Bx upfront, resection at progression (complicated by hemorrhagic stroke) | Nil | 54 Gy | Upfront | L hemiparesis, bilateral CN IV and VI palsy | Alive with NED | 10.31 |
| 10 | ETV → VPS (1) | Yes | Bx at progression | 1. Carboplatin + vincristine + temozolomide 2. Vinblastine 3. Selumetinib |
Nil | PD (metastasis) | HA | Alive with SD on treatment | 9.37 |
| 11 | VPS (2) | No | Bx upfront inconclusive; 2 more Bxs at progression |
Nil | 54 Gy RT necrosis requiring steroid/bevacizumab |
PD | Pathological fracture due to steroid use | Alive with SD | 9.57 |
| 12 | Nil | No | Nil | Nil | 54 Gy | PD | Headache, L ptosis, xerostomia, ADHD | Alive with SD | 7.56 |
| 13 | VPS (2) | No | Nil | Nil | Nil | N/A | Seizure, bilateral exotropia, delay, learning difficulty, NF-1 related | Alive with SD | 9.81 |
| 14 | ETV | Yes | Nil | Nil | Nil | N/A | Nil | Alive with SD | 5.46 |
| 15 | ETV | Yes | Nil | Nil | Nil | N/A | Intermittent exotropia bilaterally | Alive with SD | 5.81 |
| 16 | Nil | No | Nil | Nil | Nil | N/A | Migraine | Alive with SD | 4.94 |
| 17 | ETV | Yes | Nil | Nil | Nil | N/A | Memory problem, NF-1 related | Alive with SD | 4.51 |
| 18 | ETV | Yes | Nil | Nil | Nil | N/A | HA? Migraine | Alive with SD | 3.64 |
| 19 | ETV | Yes | Nil | Nil | Nil | N/A | Abnormal EEG | Alive with SD | 1.49 |
| 20 | ETV | Yes | Nil | Nil | Nil | N/A | Nil | Alive with SD | 1.49 |
| 21 | ETV | Yes | Nil | Nil | Nil | N/A | Nil | Alive with SD | 1.24 |
| 22 | ETV | No | Bx upfront | Nil | Nil | N/A | Nil | Alive with SD | 0.51 |
ADHD attention-deficit hyperactivity disorder, Bx biopsy, CP cerebral palsy, CSF cerebrospinal fluid, CN cranial nerve, ETV endoscopic third ventriculostomy, GHD growth hormone deficiency, GTR gross total resection, HA headache, L left, N nausea, NF-1 neurofibromatosis type 1, OA optic atrophy, PD progressive disease, R right, RT radiotherapy, SD stable disease, V vomiting, VF visual field, VPS ventriculo-peritoneal shunt, y year(s)
Disease progression, patient outcome, and long-term morbidities
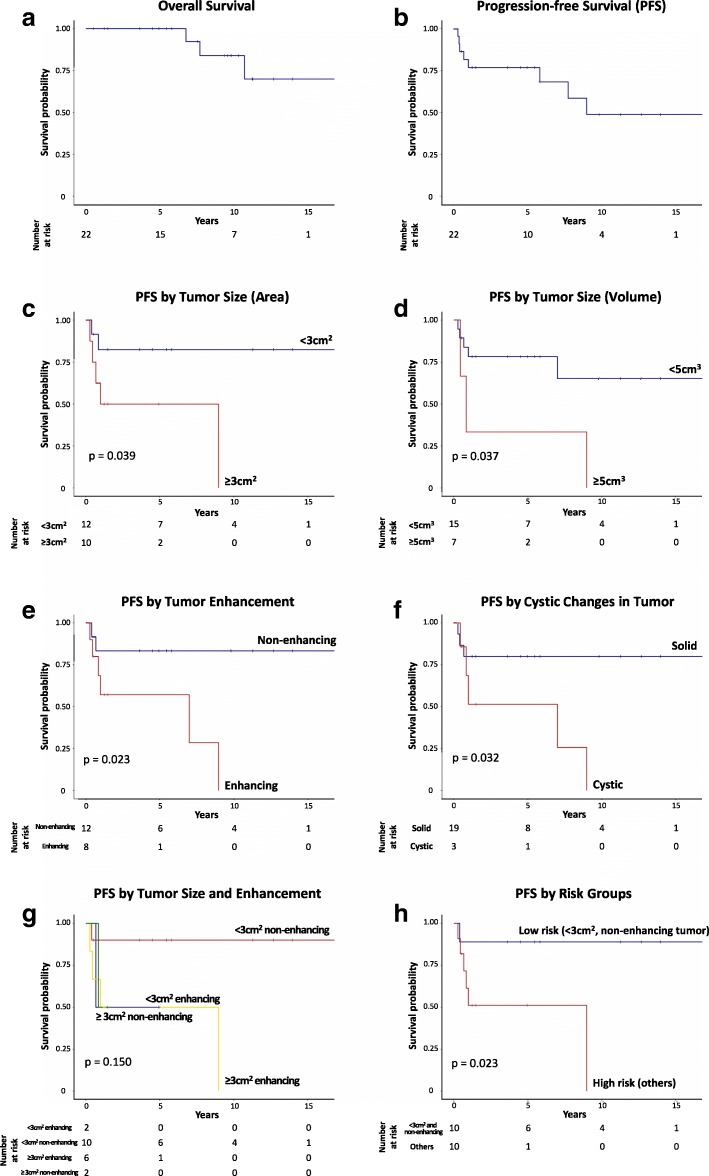
During the follow-up period (median, 7.64 years; range, 0.51–16.98), seven patients (32%) treated at SJCRH experienced progression, including two (9%) with metastasis (Table 1). Four patients had a single progression, whereas the remainder experienced two to four progressions. Of the two patients with metastasis, one had known metastatic deposit at the infundibular recess at diagnosis. The second patient did not undergo spinal MRI at diagnosis and was found to have infundibular and spinal metastasis 4 months after diagnosis. The median duration from diagnosis to first progression was 0.68 years (range, 0.28–8.98). Three patients (14%), including two with PD, died (of suicide, obstructive hydrocephalus and suspected shunt failure). This translates into a 5/10-year OS and PFS of 100%/83.9 ± 10.4%, and 76.8 ± 9.1%/48.7 ± 14.2% (Fig. 2). Patients with TG reported significant long-term morbidities, including persistent headaches and visual symptoms (Fig. 1). Cognitive assessments were completed and at a median age of 14.96 years (range, 4.5–24.92) and at a median 5.63 years (range, 0.44–9.55) after diagnosis. Impaired scores were most frequently identified in processing speed (7 out of 7 scores; 100%), working memory (2 out of 7; 28.6%) and academics (math, 3 out of 7, 42.9%). (Fig. 1, Additional file 3: Table S2).
Fig. 2.
a Overall survival and b progression-free survival of patients with longitudinal follow-up in our cohort. c-h Imaging predictors of progression-free survival
Imaging features and predictors of progression
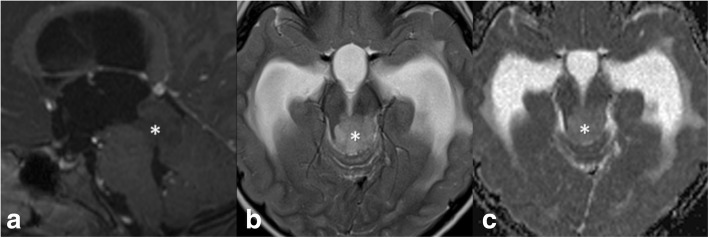
Imaging was available for review in 22 patients (19 patients treated at SJCRH and 3 seen for review). Images obtained at diagnosis revealed that nine patients (40.9%) had lesions confined to the tectal plate, whereas 13 (59.1%) had lesions extending to adjacent structures such as the tegmentum and thalami (Fig. 1, Additional file 4: Table S3). Mean tumor measurements at diagnosis were 4.3(±4.05) cm2. All lesions were isointense or hypointense on T1-weighted images and most were hyperintense on T2-weighted sequences (Fig. 3). Contrast enhancement was detected in 8/20 (40%) and cystic changes in 3/22 (14%), the presence of both were significantly correlated with lesions ≥3cm2 (P = 0.027 and 0.043 respectively). In those who had diffusion-weighted imaging (DWI, n = 18), the mean (±SD) relative apparent diffusion coefficient (rADC) was 1.69 (±0.47). Lesions with measured area greater than 3cm2 (P = 0.023), contrast enhancement (P = 0.039), and cystic changes (P = 0.037) at diagnosis predicted inferior PFS (Fig. 2). Other radiologic parameters, including tumor extent, tumor circumscription, and rADC values, as well as clinical parameters, namely sex, presenting symptoms, symptom duration before diagnosis and need for CSF diversion, were not significantly associated with PFS. In comparison of sequential MR images at diagnosis and progression (n = 8) (Additional file 5: Table S4), mean tumor measurements were 5.48 (±5.54) cm2 and 9.61 (±8.35) cm2, respectively, with mean increase of 88.19 (±51.49) %. All lesions enhanced at progression, with further increases in the extent and avidity of enhancement in those with pre-existing enhancement. One additional lesion (for a total of four out of eight) developed cystic change at progression, and intra-tumoral hemorrhage was evident in one patient. No significant alteration in rADC was observed at progression (P = 0.760).
Fig. 3.
Typical MRI features of tectal glioma. a Sagittal post-contrast T1-weighted image shows a typical non-enhancing, T1 hypointense lesion obstructing the cerebral aqueduct (*). b Axial T2-weighted image shows typical T2 hyperintensity of the lesion (*), and periventricular CSF accumulation indicative of hydrocephalus. c on ADC map, tectal gliomas (*) are typically high in signal (“facilitated” diffusion)
Histopathologic and molecular features
Thirty patients had tumor tissue available for pathology review. They included seven patients treated at SJCRH and 23 referred for case review (Figs 1 and 4, Additional file 6: Table S5). Sixteen patients had tumor samples from initial diagnosis available and 14 had samples obtained at progression. All specimens were classified as LGG and showed bland cytology. Twenty-five samples (83%) displayed histopathological features similar to PA (WHO grade I). These tumors had a non-infiltrative growth pattern with biphasic, alternating loose and more compact architecture, similar to PAs of other sites. The tumor cells had piloid morphology. Microcystic regions, Rosenthal fibers and eosinophilic granular bodies were frequent findings. Five (17%) had histopathological features aligned best with diffuse astrocytoma (DA) (WHO grade II). These tumors had a diffusely infiltrative growth pattern similar to DAs of other sites. Only 1/14 samples obtained at progression (7.1%) exhibited a DA growth pattern, suggesting that such finding does not equate an increased risk of progression. BRAF duplication consistent with the presence of KIAA1549-BRAF fusion was present in 6/24 samples (25%), whereas BRAF V600E mutation was detected in 2/26 samples (7.7%). All eight samples with BRAF alterations exhibited a PA-like growth pattern. In contrast, none of the 24 samples evaluated harbored the histone H3 K27M mutation. The prognostic value of BRAF alterations could not be meaningfully interpreted with the limited sample size.
Fig. 4.

Histologic features of tectal glioma. a Most tectal gliomas demonstrate typical morphologic features of pilocytic astrocytoma, including alternating loose and more compact architecture, bland cytology, Rosenthal fibers, and sclerotic vessels, as well as glomeruloid microvascular proliferation. b, c The tumor cells are diffusely and strongly positive for GFAP and Olig2. d Occasional entrapped axons are highlighted by neurofilament (NFP) staining. e Ki67 labeling is minimal. f BRAF V600E mutant protein is detected by immunohistochemical staining in a few cases. g Occasionally, tectal glioma may have a more diffuse growth pattern, similar to that of a diffuse astrocytoma, with numerous entrapped axons (highlighted by NFP staining, h)
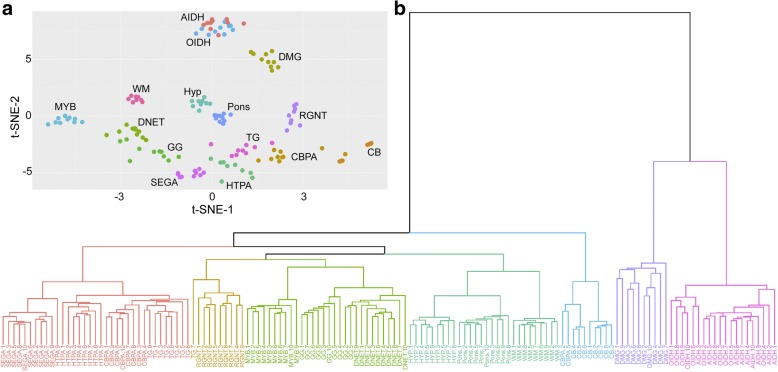
Genome-wide DNA methylation profiling
Analysis of genomic DNA methylation profiles by t-SNE plot and unsupervised cluster analysis demonstrated that TG harbors methylation patterns distinct from PAs of nearby sites (cerebellum, CBPA, and hypothalamus, HTPA) and also other brain tumors including rosette-forming glioneuronal tumor (RGNT), dysembryoplastic neuroepithelial tumor (DNET), ganglioglioma (GG), subependymal giant cell astrocytoma (SEGA), MYB-altered LGG, histone H3 K27M-mutant diffuse midline glioma (DMG), and IDH-mutant diffuse astrocytoma (AIDH) / oligodendroglioma (OIDH), and normal tissue from the hypothalamus (Hyp), pons, cerebellum (CB) and white matter (WM) (Fig. 5).
Fig. 5.
Genome-wide DNA methylation profiling support tectal glioma as a molecularly distinct entity. a t-SNE plot and b dendrogram of unsupervised cluster analysis comparing DNA methylation profile of tectal glioma with those of 10 other brain tumor entities including PAs of nearby sites (cerebellum, CBPA, and hypothalamus, HTPA), rosette-forming glioneuronal tumor (RGNT), dysembryoplastic neuroepithelial tumor (DNET), ganglioglioma (GG), subependymal giant cell astrocytoma (SEGA), MYB-altered LGG, histone H3 K27M-mutant diffuse midline glioma (DMG) and IDH-mutant diffuse astrocytoma (AIDH) / oligodendroglioma (OIDH), and normal tissue from hypothalamus (Hyp), pons, cerebellum (CB) and white matter (WM) demonstrate that tectal glioma forms a distinct cluster
Discussion
We have reported imaging findings, histopathology, molecular analysis and outcomes of children with TG compiled over a period of three decades. The presentation of TG is often typified by symptoms of raised intracranial pressure and delayed diagnosis, with most reports describing a lead time of 3–6 months [1, 4, 5, 8, 15, 16, 37, 39, 41, 43, 45]. Misdiagnosis of TG as aqueductal stenosis based on CT, as in three of our patients, was common and was associated with even longer symptom durations before TG diagnosis [5]. The more widespread application of MRI for neuroimaging has resulted in incidental diagnoses of TG [1, 14, 17, 22, 26, 32–34, 41, 42, 48]. TG was an incidental finding in up to 27% of patients in various series and in an even higher percentage when MRI was part of a structured surveillance, as in children with NF1 [14, 33]. Whether TG diagnosis in this context is truly beneficial for patient outcomes remains uncertain [40].
Initial treatment of pediatric TG presented with obstructive hydrocephalus involves CSF diversion. VPS use has been associated with frequent failures, the need for revision, issues with MR compatibility, and over-shunting [4, 8, 15, 16, 28, 41]. Consequently, ETV has replaced shunt insertion as the preferred method of CSF diversion [9, 20, 26, 48]. Ommaya reservoirs can be safely inserted during ETV, allowing emergent CSF withdrawal in the event of ETV failure [10]. Concomitant tumor resection is best avoided because of its inherent risks [25]. Lapras and colleagues reported their experience in resecting 12 tectal plate lesions upfront, with GTR being achieved in nine patients and partial resection in three [25]. However, this accomplishment was at the expense of a vegetative state and death in one patient and surgical complications requiring early re-operation in four others, as well as other complications including visual-field defects, Parinaud syndrome, and mutism in further patients. Other studies reserved tumor biopsy/resection for disease progression [22, 43]. Similar to our cohort, around one-third of patients in the literature eventually required tumor-directed surgery, and visual deficits, gaze palsies, and intracranial hemorrhages remained significant complications. In view of the significant surgical morbidities, biopsy or resection of TG should only be reserved for tumors with an atypical radiographic appearance, and for debulking as well as to guide targeted treatment (such as BRAF and MEK inhibitors) at progression [5, 39, 42].
Adjuvant therapy with chemotherapy and/or focal radiation is often employed in patients with PD [4, 5, 14, 17, 21, 25, 30, 32, 34, 38, 41–43, 45]. In our study, significant predictors of progression included tumor size greater than 3cm2, contrast enhancement and cystic changes at diagnosis, confirming the suggestions of previous reports [22, 34, 43]. To evaluate the role of adjuvant therapy and treatment outcome, we extensive reviewed clinical reports on pediatric TG (< 21 years at diagnosis, 5 or more patients) and combined with data from our cohort (Additional file 7: Table S6) [1, 4, 5, 7–9, 14–17, 20–22, 25, 26, 28, 30, 32–34, 37–39, 41–43, 45, 48]. Among 26 studies reporting details of adjuvant therapy, 56/463 patients (12.1%) received focal radiation with doses of 50.2–56.8Gy, whereas 26/463 (5.6%) received systemic therapy [1, 4, 5, 8, 9, 14–17, 21, 25, 26, 28, 30, 32–34, 37–39, 41–43, 45, 48]. Patient outcomes were reported in 28 studies, with 495/508 patients (97.4%) surviving for average durations ranging from 2 to 10 years at follow-up [1, 4, 5, 8, 9, 14–17, 20–22, 25, 26, 28, 30, 32–34, 37–39, 41–43, 45, 48]. In the studies describing PD (n = 24), 121 of 453 patients (26.7%) displayed clinical and/or radiographic PD, with the average duration from diagnosis to progression ranging from 3 months to 7.8 years [1, 4, 5, 8, 9, 14–17, 20–22, 28, 30, 32–34, 38, 39, 41–43, 48]. Of the 13 patients who died, eight died of PD (one had high-grade glioma [HGG]), one died of metastatic neuroblastoma, one died of VPS infection, and three deaths were from our series discussed earlier. These data suggest that the vast majority of children with TG, despite the risk of progression in a quarter, are long-term survivors with salvage adjuvant treatment. Such findings are striking in the context of most TG not being surgically removed and the extent of resection being one of the most important prognostic factors in other LGGs [35].
The unique clinical behavior of TG might be explained by its anatomical location and the differences in tumor biology among LGGs from various body sites. In our study, we for the first time interrogated the molecular distinctiveness of TG by performing targeted studies (of BRAF alterations and histone mutations) and genome-wide DNA methylation profiling. The frequency of KIAA1549-BRAF fusion (by the presence of BRAF locus duplication on iFISH) in TG (25%) appeared to be lower than that in PAs from the cerebellum (92%) and supratentorium (59%), whereas the frequency of BRAF V600E mutation (7.7%) appeared to be intermediate between the two (0% and 10% respectively) [3, 52]. Despite the extra-tectal extension of a proportion of tumors, the lack of histone H3 K27M mutations in all 24 samples supported the biological distinctiveness of TG from other midline diffuse gliomas of the brainstem, which are often characterized by such histone mutations and a more aggressive clinical course. DNA methylation profiling has established a role in defining clinically relevant subgroups in CNS tumors such as medulloblastoma, ependymoma and HGG [12, 31, 51]. Our comparison of the methylation profiles of TG and cerebellar/hypothalamic PAs revealed molecular heterogeneity among these morphologically similar lesions, further supporting the biological uniqueness of TG.
Pediatric TG should be considered a chronic disease, in which care for long-term morbidities is of paramount importance. Caregivers should be informed of the common long term morbidities in patients with TG including chronic headache, persistent visual symptoms and neurocognitive impairments [1, 4, 14, 16, 20, 22, 25, 28, 29, 39, 43, 48]. Neuropsychologic assessments in our cohort suggested areas of deficit in working memory, processing speed and academics, specifically math, thus adding to prior reports of problems in visual attention deficits, behavior problems, and academic achievement, calling for neuropsychologic evaluation as standard of care in patients with TG [1, 14]. Despite the retrospective nature of our analysis and limitation on available material and follow-up information on some of the cases, we comprehensively addressed the clinical, imaging, histologic and molecular distinctiveness of TG. Our findings provide evidence supporting TG as a distinct diagnostic entity.
Conclusion
Tectal glioma is a clinically indolent disease and biologically distinct from other LGGs. Symptoms are frequently due to obstructive hydrocephalus and diagnosis can be made based on typical MRI features. CSF diversion by ETV is sufficient for most patients. Disease progression may be predicted by size, contrast enhancement and cystic change on initial MRI. Long-term follow-up for morbidities including neuropsychologic impairments is necessary for patients with this chronic illness.
Additional files
Figure S1. Number of patients who underwent clinical, radiologic and pathologic review in our cohort. (TIF 881 kb)
Table S1. Demographics and presenting symptoms in patients treated at SJCRH. (DOCX 23 kb)
Table S2. Characteristics of patients who underwent neuropsychologic testing in our cohort. (DOCX 22 kb)
Table S3. Centrally reviewed diagnostic imaging features in our study cohort. (DOCX 27 kb)
Table S4. Evolution of imaging features at disease progression. (DOCX 24 kb)
Table S5. Histopathologic features and molecular findings. (DOCX 24 kb)
Table S6. Summary of literature on pediatric tectal glioma. (DOCX 47 kb)
Acknowledgements
The authors would like to thank Emily Walker in the Hartwell Center of St. Jude Children’s Research Hospital for her technical support on genomic DNA methylation profiling, Raven Holcomb and Alice Slusher in the Department of Pathology for their assistant in performing immunohistochemistry and tissue processing, Susana Raimondi and James Dalton in the Department of Pathology for their assistance in performing fluorescence in situ hybridization, Matthew Lear at St. Jude Biorepository for his assistance in providing study material, Dianne Scott and Stacey Davis in the Department of Pathology for administrative support, and Keith A. Laycock, PhD, ELS for scientific editing of the manuscript.
Funding
JC receives research support from the American Lebanese Syrian Associated Charities (ALSAC) through the Department of Pathology of St. Jude Children’s Research Hospital.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding authors upon reasonable request.
Authors’ contributions
APYL, JHH, LMJ, MG, SA, SW, PK, AG, JC and IQ analyzed and interpreted the results. JHH performed central review of the imaging findings. JC performed central pathology review. LMJ and MG reviewed and analyzed the neuropsychological assessment data. APYL, YG, JC and IQ collected the patient cohort. SW performed statistical analysis. XL and JC performed molecular analysis. APYL, JHH, LMJ, MG, XL, JC and IQ wrote the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This study has been approved by Institutional Review Board (XPD15–104, XPD18–006).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jason Chiang, Phone: (901) 595-1035, Email: jason.chiang@stjude.org.
Ibrahim Qaddoumi, Phone: (901) 595-2365, Email: ibrahim.qaddoumi@stjude.org.
References
- 1.Aarsen FK, Arts WF, Van Veelen-Vincent ML, Lequin MH, Catsman-Berrevoets CE. Long-term outcome in children with low grade tectal tumours and obstructive hydrocephalus. Eur J Paediatr Neurol. 2014;18:469–474. doi: 10.1016/j.ejpn.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Aryee MJ, Jaffe AE, Corrada-Bravo H, Ladd-Acosta C, Feinberg AP, Hansen KD, Irizarry RA. Minfi: a flexible and comprehensive bioconductor package for the analysis of Infinium DNA methylation microarrays. Bioinformatics. 2014;30:1363–1369. doi: 10.1093/bioinformatics/btu049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bergthold G, Bandopadhayay P, Hoshida Y, Ramkissoon S, Ramkissoon L, Rich B, Maire CL, Paolella BR, Schumacher SE, Tabak B. Expression profiles of 151 pediatric low-grade gliomas reveal molecular differences associated with location and histological subtype. Neuro-Oncology. 2015;17:1486–1496. doi: 10.1093/neuonc/nov045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bowers DC, Georgiades C, Aronson LJ, Carson BS, Weingart JD, Wharam MD, Melhem ER, Burger PC, Cohen KJ. Tectal gliomas: natural history of an indolent lesion in pediatric patients. Pediatr Neurosurg. 2000;32:24–29. doi: 10.1159/000028893. [DOI] [PubMed] [Google Scholar]
- 5.Boydston WR, Sanford RA, Muhlbauer MS, Kun LE, Kirk E, Dohan JFC, Schweitzer JB. Gliomas of the Tectum and periaqueductal region of the mesencephalon. Pediatr Neurosurg. 1991;17:234–238. doi: 10.1159/000120603. [DOI] [PubMed] [Google Scholar]
- 6.Capper D, Jones DTW, Sill M, Hovestadt V, Schrimpf D, Sturm D, Koelsche C, Sahm F, Chavez L, al RDE. DNA methylation-based classification of central nervous system tumours. Nature. 2018;555:469–474. doi: 10.1038/nature26000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dabscheck G, Prabhu SP, Manley PE, Goumnerova L, Ullrich NJ. Risk of seizures in children with tectal gliomas. Epilepsia. 2015;56:e139–e142. doi: 10.1111/epi.13080. [DOI] [PubMed] [Google Scholar]
- 8.Dağlıoğlu E, Çataltepe O, Akalan N. Tectal gliomas in children: the implications for natural history and management strategy. Pediatr Neurosurg. 2003;38:223–231. doi: 10.1159/000069823. [DOI] [PubMed] [Google Scholar]
- 9.Diaz RJ, Girgis FM, Hamiltonn MG. Endoscopic third ventriculostomy for hydrocephalus due to tectal glioma. Can J Neurol Sci. 2014;41:476–481. doi: 10.1017/S0317167100018515. [DOI] [PubMed] [Google Scholar]
- 10.Drake J, Chumas P, Kestle J, Pierre-Kahn A, Vinchon M, Brown J, Pollack IF, Arai H. Late rapid deterioration after endoscopic third ventriculostomy: additional cases and review of the literature. J Neurosurg Pediatr. 2006;105:118–126. doi: 10.3171/ped.2006.105.2.118. [DOI] [PubMed] [Google Scholar]
- 11.Elliott CD. Differential ability scales. 2. San Antonio, TX: Harcourt Assessment, City; 2007. [Google Scholar]
- 12.Ellison DW, Kocak M, Dalton J, Megahed H, Lusher ME, Ryan SL, Zhao W, Nicholson SL, Taylor RE, Bailey S, et al. Definition of disease-risk stratification groups in childhood medulloblastoma using combined clinical, pathologic, and molecular variables. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2011;29:1400–1407. doi: 10.1200/jco.2010.30.2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fortin JP, Labbe A, Lemire M, Zanke BW, Hudson TJ, Fertig EJ, Greenwood CM, Hansen KD. Functional normalization of 450k methylation array data improves replication in large cancer studies. Genome Biol. 2014;15:503. doi: 10.1186/s13059-014-0503-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gass D, Dewire M, Chow L, Rose SR, Lawson S, Stevenson C, Pai AL, Jones B, Sutton M, Lane A. Pediatric tectal plate gliomas: a review of clinical outcomes, endocrinopathies, and neuropsychological sequelae. J Neuro-Oncol. 2015;122:169–177. doi: 10.1007/s11060-014-1700-2. [DOI] [PubMed] [Google Scholar]
- 15.Gomez-Gosalvez F, Menor F, Morant A, Clemente F, Escriva P, Carbonell J, Mulas F. Tectal tumours in paediatrics. A review of eight patients Revista de neurologia. 2000;33:605–611. [PubMed] [Google Scholar]
- 16.Grant GA, Avellino AM, Loeser JD, Ellenbogen RG, Berger MS, Roberts TS. Management of intrinsic gliomas of the tectal plate in children. Pediatr Neurosurg. 1999;31:170–176. doi: 10.1159/000028857. [DOI] [PubMed] [Google Scholar]
- 17.Griessenauer CJ, Rizk E, Miller JH, Hendrix P, Tubbs RS, Dias MS, Riemenschneider K, Chern JJ. Pediatric tectal plate gliomas: clinical and radiological progression, MR imaging characteristics, and management of hydrocephalus. J Neurosurg Pediatr. 2014;13:13–20. doi: 10.3171/2013.9.PEDS13347. [DOI] [PubMed] [Google Scholar]
- 18.Guillamo J-S, Doz F, Delattre J-Y. Brain stem gliomas. Curr Opin Neurol. 2001;14:711–715. doi: 10.1097/00019052-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Jastak S, Wilkinson G. Wide Range Achievement Test - Revised. Wilmington, DE: Jastak Associates, City; 1984. [Google Scholar]
- 20.Javadpour M, Mallucci C. The role of neuroendoscopy in the management of tectal gliomas. Childs Nerv Syst. 2004;20:852–857. doi: 10.1007/s00381-004-0942-2. [DOI] [PubMed] [Google Scholar]
- 21.Kaufmann A, Gerber NU, Kandels D, Azizi AA, Schmidt R, Warmuth-Metz M, Pietsch T, Kortmann R-D, Gnekow AK, Grotzer MA (2018) Management of Primary Tectal Plate low-Grade Glioma in pediatric patients: results of the multicenter treatment study SIOP-LGG 2004. Neuropediatrics [DOI] [PubMed]
- 22.Kershenovich A, Silman Z, de Rungs D, Koral K, Gargan L, Weprin B. Tectal lesions in children: a long-term follow-up volumetric tumor growth analysis in surgical and nonsurgical cases. Pediatr Neurosurg. 2016;51:69–78. doi: 10.1159/000442795. [DOI] [PubMed] [Google Scholar]
- 23.Koral K, Alford R, Choudhury N, Mossa-Basha M, Gargan L, Gimi B, Gao A, Zhang S, Bowers DC, Koral KM. Applicability of apparent diffusion coefficient ratios in preoperative diagnosis of common pediatric cerebellar tumors across two institutions. Neuroradiology. 2014;56:781–788. doi: 10.1007/s00234-014-1398-z. [DOI] [PubMed] [Google Scholar]
- 24.Krijthe J (2015) Rtsne: T-Distributed Stochastic Neighbor Embedding using a Barnes-Hut Implementation, https://github.com/jkrijthe/Rtsne
- 25.Lapras C, Bognar L, Turjman F, Villanyi E, Mottolese C, Fischer C, Jouvet A, Guyotat J. Tectal plate gliomas. Part I: microsurgery of the tectal plate gliomas. Acta Neurochir. 1994;126:76–83. doi: 10.1007/BF01476414. [DOI] [PubMed] [Google Scholar]
- 26.Li KW, Roonprapunt C, Lawson HC, Abbott IR, Wisoff J, Epstein F, Jallo GI. Endoscopic third ventriculostomy for hydrocephalus associated with tectal gliomas. Neurosurg Focus. 2005;18:1–4. doi: 10.3171/foc.2005.18.6.3. [DOI] [PubMed] [Google Scholar]
- 27.Maechler M, Rousseeuw P, Struyf A, Hubert M, Hornik K (2018) Cluster: cluster analysis basics and extensions. R package version 2.0.7-1.:
- 28.May PL, Blaser SI, Hoffman HJ, Humphreys RP, Harwood-Nash DC. Benign intrinsic tectal “tumors” in children. J Neurosurg. 1991;74:867–871. doi: 10.3171/jns.1991.74.6.0867. [DOI] [PubMed] [Google Scholar]
- 29.Mohme M, Fritzsche FS, Mende KC, Matschke J, Löbel U, Kammler G, Westphal M, Emami P, Martens T. Tectal gliomas: assessment of malignant progression, clinical management, and quality of life in a supposedly benign neoplasm. Neurosurg Focus. 2018;44:E15. doi: 10.3171/2018.3.FOCUS1850. [DOI] [PubMed] [Google Scholar]
- 30.Mottolese C, Szathmari A, Beuriat PA, Frappaz D, Jouvet A, Hermier M. Tectal plate tumours. Our experience with a paediatric surgical series Neurochirurgie. 2015;61:193–200. doi: 10.1016/j.neuchi.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 31.Pajtler KW, Witt H, Sill M, Jones DT, Hovestadt V, Kratochwil F, Wani K, Tatevossian R, Punchihewa C, Johann P. Molecular classification of ependymal tumors across all CNS compartments, histopathological grades, and age groups. Cancer Cell. 2015;27:728–743. doi: 10.1016/j.ccell.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pollack IF, Pang D, Albright AL. The long-term outcome in children with late-onset aqueductal stenosis resulting from benign intrinsic tectal tumors. J Neurosurg. 1994;80:681–688. doi: 10.3171/jns.1994.80.4.0681. [DOI] [PubMed] [Google Scholar]
- 33.Pollack IF, Shultz B, Mulvihill JJ. The management of brainstem gliomas in patients with neurofibromatosis 1. Neurology. 1996;46:1652–1660. doi: 10.1212/WNL.46.6.1652. [DOI] [PubMed] [Google Scholar]
- 34.Poussaint TY, Kowal JR, Barnes PD, Zurakowski D, Anthony DC, Goumnerova L, Tarbell NJ. Tectal tumors of childhood: clinical and imaging follow-up. Am J Neuroradiol. 1998;19:977–983. [PMC free article] [PubMed] [Google Scholar]
- 35.Qaddoumi I, Sultan I, Gajjar A. Outcome and prognostic features in pediatric gliomas : a review of 6212 cases from the surveillance, epidemiology and end results (SEER) database. Cancer. 2009;115:5761–5770. doi: 10.1002/cncr.24663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.R Core Team (2018) R: A language and environment for statistical computing https://www.R-project.org/
- 37.Ramelli GP, Cortesi C, Boscherini D, Faggin R, Bianchetti MG. Age-dependent presentation of tectal plate tumors: preliminary observations. J Child Neurol. 2011;26:377–380. doi: 10.1177/0883073810382141. [DOI] [PubMed] [Google Scholar]
- 38.Ramina R, Coelho Neto M, Fernandes YB, Borges G, Honorato DC, Arruda WO. Intrinsic tectal low grade astrocytomas: is surgical removal an alternative treatment? Long-term outcome of eight cases. Arq Neuropsiquiatr. 2005;63:40–45. doi: 10.1590/S0004-282X2005000100008. [DOI] [PubMed] [Google Scholar]
- 39.Robertson PL, Muraszko KM, Brunberg JA, Axtell RA, Dauser RC, Turrisi AT. Pediatric midbrain tumors: a benign subgroup of brainstem gliomas. Pediatr Neurosurg. 1995;22:65–73. doi: 10.1159/000120879. [DOI] [PubMed] [Google Scholar]
- 40.Roth J, Keating RF, Myseros JS, Yaun AL, Magge SN, Constantini S. Pediatric incidental brain tumors: a growing treatment dilemma. J Neurosurg Pediatr. 2012;10:168–174. doi: 10.3171/2012.6.PEDS11451. [DOI] [PubMed] [Google Scholar]
- 41.Squires LA, Allen JC, Abbott R, Epstein FJ. Focal tectal tumors management and prognosis. Neurology. 1994;44:953–953. doi: 10.1212/WNL.44.5.953. [DOI] [PubMed] [Google Scholar]
- 42.Stark AM, Fritsch MJ, Claviez A, Dörner L, Mehdorn HM. Management of tectal glioma in childhood. Pediatr Neurol. 2005;33:33–38. doi: 10.1016/j.pediatrneurol.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 43.Ternier J, Wray A, Puget S, Bodaert N, Zerah M, Sainte-Rose C. Tectal plate lesions in children. J Neurosurg Pediatr. 2006;104:369–376. doi: 10.3171/ped.2006.104.6.369. [DOI] [PubMed] [Google Scholar]
- 44.van der Maaten LJP, Hinton GE (2008) Visualizing High-Dimensional Data Using t-SNE. Journal of Machine Learning ResearchNov (9): 2579–2605
- 45.Vandertop WP, Hoffman HJ, Drake JM, Humphreys RP, Rutka JT, Amstrong DC, Becker LE. Focal midbrain tumors in children. Neurosurgery. 1992;31:186-194. doi: 10.1097/00006123-199208000-00003. [DOI] [PubMed] [Google Scholar]
- 46.Wechsler D. Wechsler individual achievement test. 3. San Antonio, TX: Psychological Corporation, City; 2009. [Google Scholar]
- 47.Wechsler D. Wechsler intelligence scale for children. 5. Bloomington, MN: Pearson, City; 2014. [Google Scholar]
- 48.Wellons Iii JC, Tubbs RS, Banks JT, Grabb B, Blount JP, Oakes WJ, Grabb PA. Long-term control of hydrocephalus via endoscopic third ventriculostomy in children with tectal plate gliomas. Neurosurgery. 2002;51:63–68. doi: 10.1097/00006123-200207000-00010. [DOI] [PubMed] [Google Scholar]
- 49.Wen PY, Chang SM, Van den Bent MJ, Vogelbaum MA, Macdonald DR, Lee EQ. Response assessment in Neuro-oncology clinical trials. J Clin Oncol. 2017;35:2439–2449. doi: 10.1200/JCO.2017.72.7511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Woodcock RW, KS MG, Mather N. Woodcock-Johnson III tests of achievement. Itasca, IL: Riverside Publishing, City; 2001. [Google Scholar]
- 51.Wu G, Diaz AK, Paugh BS, Rankin SL, Ju B, Li Y, Zhu X, Qu C, Chen X, Zhang J, et al. The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nat Genet. 2014;46:444–450. doi: 10.1038/ng.2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang J, Wu G, Miller CP, Tatevossian RG, Dalton JD, Tang B, Orisme W, Punchihewa C, Parker M, al QI. Whole-genome sequencing identifies genetic alterations in pediatric low-grade gliomas. Nat Genet. 2013;45:602–612. doi: 10.1038/ng.2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Number of patients who underwent clinical, radiologic and pathologic review in our cohort. (TIF 881 kb)
Table S1. Demographics and presenting symptoms in patients treated at SJCRH. (DOCX 23 kb)
Table S2. Characteristics of patients who underwent neuropsychologic testing in our cohort. (DOCX 22 kb)
Table S3. Centrally reviewed diagnostic imaging features in our study cohort. (DOCX 27 kb)
Table S4. Evolution of imaging features at disease progression. (DOCX 24 kb)
Table S5. Histopathologic features and molecular findings. (DOCX 24 kb)
Table S6. Summary of literature on pediatric tectal glioma. (DOCX 47 kb)
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding authors upon reasonable request.