Abstract
Dynamic psychological processes are most often assessed using self-report instruments. This places a constraint on how often and for how long data can be collected due to the burden placed on human participants. Smartphones are ubiquitous and highly personal devices, equipped with sensors that offer an opportunity to measure and understand psychological processes in real-world contexts over the long term. In this article, we present a novel smartphone approach to address the limitations of self-report in bipolar disorder where mood and activity are key constructs. We describe the development of MoodRhythm, a smartphone application that incorporates existing self-report elements from interpersonal and social rhythm therapy, a clinically validated treatment, and combines them with novel inputs from smartphone sensors. We reflect on lessons learned in transitioning from an existing self-report instrument to one that involves smartphone sensors and discuss the potential impact of these changes on the future of psychological assessment.
Keywords: bipolar disorder, mHealth, ecological momentary assessment, behavioral sensing, self-report, IPSRT, mental health
The rapid evolution and dissemination of mobile and sensing technologies have created unprecedented opportunities for the collection of personal data in an extremely granular, unobtrusive, and relatively affordable way. However, to transform this potential into practice requires the development of novel algorithms and methodologies that distill raw data into actionable knowledge. The rise of personal informatics—consumer-friendly tools that allow individuals to conveniently track a wide range of elements including mood, activity, and sleep (Li, Dey, & Forlizzi, 2010)—alongside the related “Quantified Self”1 movement, which focuses on individuals’ use of these tools to empower themselves, promises to enable people to take advantage of an ever-increasing amount of personal data. As early as 2006, the Institute of Medicine recognized that these technologies have the potential to transform mental health services by providing more continuous and precise information on patient-specific behavior, symptoms, and medication effects (Institute of Medicine, 2006).
Presently, researchers and clinical practitioners still rely almost entirely on what a person reports about their experience to understand psychological processes. For maximal understanding of a disease like bipolar disorder, it is helpful to assess manifestations of the disorder in everyday settings. One of the methods most commonly used to this end is ecological momentary assessment (EMA; Stone & Shiffman, 1994), a method that involves repeated sampling of individual experience in real time and in a person’s natural environment. The technique focuses on measurement “in the moment” (e.g., “how do you feel right now?”) as opposed to a retrospective assessment (e.g., “how have you felt over the past week?”). Such real-time assessment can not only reduce retrospective biases (e.g., mood congruent recall, availability heuristics, and confirmation bias) but its administration in natural settings can also help a clinician identify factors that may contribute to an individual’s symptoms as well evaluate whether patients are integrating skills from therapy into their everyday lives (Roche, Pincus, Rebar, Conroy, & Ram, 2014). The ability to continuously analyze connections among momentary experiences, behavioral patterns, and specific symptoms can also help in the fundamental conceptualization of mental disorders (Wichers, 2014). However, though EMA methods enable sensitive assessments of human behavior, they are still mostly driven by self-reported information. As a result, the depth and diversity of data they collect and the period over which they can be deployed are limited by human effort.
In this article, we describe the development and initial evaluation of a smartphone tool for use in the treatment of bipolar disorder that combines a clinically validated self-report instrument used in combination with an array of smartphone sensors to provide a continuous measure of clinically relevant behavior in bipolar disorder. We consider how self-reported instruments like this can be used in concert with smartphone sensing to facilitate continuous long-term measurement of clinically relevant factors.
Bipolar Disorder
The Dynamic Processes of Bipolar Disorder
Bipolar disorders, including classic manic-depressive illness (bipolar I disorder), bipolar II disorder, cyclothymia, and bipolar disorders not otherwise classified are common, lifelong, and life-threatening illnesses (Murray & Lopez, 1996) that are associated with poor functional and clinical outcomes (Judd et al., 2003), high suicide rates (Baldessarini & Tondo, 2003), and huge societal costs (Woods, 2000). Bipolar disorders affect approximately 5.7 million American adults—or about 2.6% of the U.S. population age 18 and older—in a given year (Kessler, Chiu, Demler, & Walters, 2005).
One of the most prominent features of bipolar disorder is its rhythmicity, including mood episodes that cycle on an approximately regular basis (Soreca, Frank, & Kupfer, 2009) and symptoms that reflect disturbances in the body’s circadian rhythms (Levenson & Frank, 2011). A number of theories and models have emerged over the past several decades that relate sleep and circadian rhythm disturbances to affective illnesses such as bipolar disorder (Ehlers, Frank, & Kupfer, 1988; Harvey, 2008). This interest in biological rhythms has given rise to a complementary interest in social rhythms—daily activities that serve to regulate biological rhythms—and in the examination of the role of lifestyle regularity in affective illnesses. A growing number of investigations link social rhythms, mood changes, and mood episodes in patients with affective illnesses (e.g., Haynes, McQuaid, Ancoli-Israel, & Martin, 2006; Malkoff-Schwartz et al., 1998). Substantial evidence now indicates that interventions targeting social rhythms, sleep–wake rhythms, and light–dark exposure may markedly improve affective illness outcomes (e.g., Frank et al., 2005; Miklowitz et al., 2007).
Social Rhythms and Interpersonal and Social Rhythm Therapy
The environmental cues that are central to setting the body’s circadian clock are called Zeitgebers (or “time givers”). Our own research has advanced what we term the Social Zeitgeber hypothesis (Ehlers et al., 1988), which suggests that certain life events may lead to episode onset through their effect on individuals’ social routines. These routines, in turn, almost certainly affect endogenous circadian rhythms leading to mood symptoms and, in vulnerable individuals, to mood episodes.
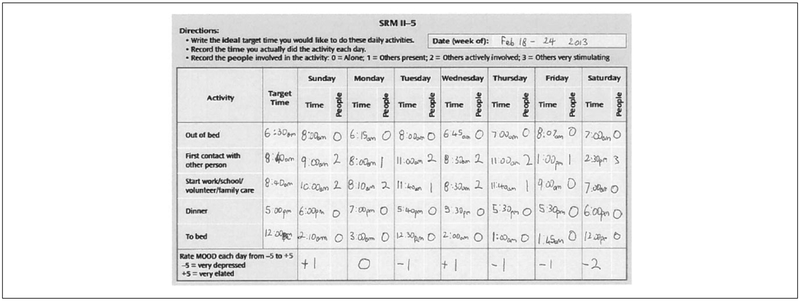
To test the Social Zeitgeber Hypothesis, we developed the Social Rhythm Metric (SRM; Figure 1), a paper-and-pencil self-report daily measure of social routines (Monk, Flaherty, Frank, Hoskinson, & Kupfer, 1990). The SRM, in turn, became a central element of interpersonal and social rhythm therapy (IPSRT; Frank, 2005), a psychosocial treatment for bipolar disorder that we developed approximately 20 years ago. We have demonstrated that IPSRT is associated with more rapid remission of bipolar depression (Miklowitz et al., 2007), longer symptom-free periods (Frank et al., 2005), and improved occupational functioning (Frank et al., 2008).
Figure 1.
The paper-based Social Rhythm Metric (SRM)–5 instrument.
Social Rhythm Metric
Since its initial development, the SRM—originally, a one-page, diary-like instrument that required patients to log when and with whom each of 17 event categories took place has evolved considerably based on IPSRT patient feedback. Not surprisingly, patients found the 17-item version too burdensome, leading to analyses showing that just 5 items (time of arising, time of first contact with another person, time of starting the day’s activity, time of dinner, and time of going to bed) of the original 17 items accounted for 79% of the variance in SRM scores (Monk, Frank, Potts, & Kupfer, 2002). Patients also suggested that we incorporate a daily mood rating alongside the times of these five social routines. Subsequent feedback from patients with bipolar II disorder (episodes of depression alternating with episodes of hypomania as opposed to full mania) led to the incorporation of a daily rating of energy. The current SRM paper tool thus comprises 7 items: 5 items relating to events and 2 to self-reported states.
This version of the SRM (“SRM-5”) has been tested and used as a therapeutic self-monitoring tool in evidence-based psychosocial interventions for affective illness, including IPSRT (Frank, 2005) and in a more limited version of the intervention that focuses exclusively on regularizing social routines (Corruble et al., 2014). We have shown that increased regularity of social routines, as measured by the SRM-5, is associated with symptomatic improvement (Swartz et al., 2011; Swartz, Frank, Frankel, Novick, & Houck, 2009) and significantly longer well intervals (Frank et al., 2005).
In the initial phase of IPSRT, the therapist introduces the SRM to patients. The patients are encouraged to record the times of the five daily social rhythm events along with mood and energy ratings for the day. The therapist reviews the SRM during each weekly session with the patient. In this phase, the therapeutic goal for the patient is to understand the dynamic relationship between routine instabilities and mood fluctuations. No specific effort is made to regulate daily rhythms.
In the subsequent phase of treatment, therapists and patients identify rhythms that are particularly unstable, based on the SRMs recorded in the initial phase. To stabilize daily rhythms, therapy involves identifying specific SRM goals. Such goals can have short-term (e.g., going to bed at 11:00 p.m. for a week), intermediate (e.g., maintaining regular sleep–wake up pattern for a month), and long-term (e.g., managing social relationships) objectives. These goals and objectives can be modified as therapy proceeds depending on patient needs. In addition, custom events (e.g., walking your dog) are often added to the tool to account for idiosyncratic activities that help stabilize patients’ daily routines.
Technology to Assess Mental Health
Prior Work Assessing Mental Health
As more people adopt today’s technology, treatment protocols in mental health involving technology are becoming increasingly acceptable, including for mental health. Indeed, the National Council for Behavioral Health (2014) is advocating for technology-based monitoring to be extended to mental health. Recent research has focused on the potential of smartphones for a wide range of uses including personalized tools for patients, patients’ individual symptom profiling and real-time assessments (Moskowitz, Russell, Sadikaj, & Sutton, 2009; Trull & Ebner-Priemer, 2013). A growing number of studies has begun using technology to deliver EMAs as part of psychological monitoring, for instance, to track interpersonal processes (Roche et al., 2014) or depression (Wichers et al., 2011).
Ambulatory assessment (AA) has been used in clinical psychology to track and infer mechanisms and dynamics of psychopathological symptoms, predict recurrence and onset of illness, assess and predict treatment effect, prevent relapse, and administer interventions (Trull & Ebner-Priemer, 2013). This approach comprises a wide range of methodologies focusing on assessing behavior and daily life experience in situ. AA can be broadly categorized into self-report, observational, and physiological/biological assessments. These methods can be continuous, event-based, interactive, time-based, randomly prompted, or a combination of these. Self-reporting, perhaps the most common form of AA, involves participants responding to queries about recent or current behavior or contexts. Again the frequency of these queries can be random, event- or time-based depending on the focus of the study. While such in situ assessment can be more reliable than retrospective reports, recall and bias issues can still affect self-reporting. Another potential major issue with self-reporting is reactivity—monitoring behavior might actually result in changing the behavior.
Instead of querying the participants, observational methods focus on the environmental cues like ambient sound, location, and activity that can provide insight into individual behavior and contexts. Physiological-based methods focus on monitoring processes that might be associated with psychopathology, personality, and problematic emotions and behavior. Examples of such assessment include electrodermal activity, cardiac activity and heart rate variability, cortisol, and actigraphy-based rest–active rhythms.
Prior Work Assessing Bipolar Disorder
Mobile sensor technology is a promising method to study aspects of bipolar disorder over a longer period of time and offers unique opportunities for intervention. A recent community-based survey with over 1,500 people with serious mental illnesses found that 72% of patients with bipolar disorder owned and used mobile phones regularly for calling, texting, and the Internet (Ben-Zeev, Davis, Kaiser, Krzsos, & Drake, 2013). In our recent survey, we found that 45% of individuals with bipolar disorder were already self-tracking mood, two thirds of the respondents reported using self-tracking data in discussions with a health care professional and 80% felt that technology had potential to help manage their illness, with a particular desire for more automated forms of digital symptom tracking (Murnane et al., 2016).
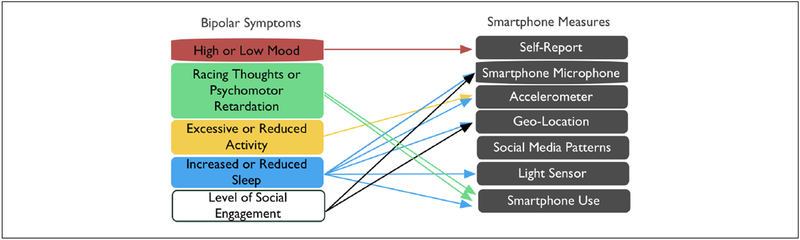
With the recent rise of smartphones with embedded sensors, the ability to track symptoms, provide feedback, and deliver interventions as part of clinical treatment has been expanded greatly. Smartphone sensing capabilities appear suited to the detection of key parameters of bipolar disorder: (a) sleep–wake/activity, (b) mental activity, and (c) the nature and frequency of social interaction. Indeed, examining the criteria for episodes of hypomania and depression, one finds that key indicators of episode onset (changes in activity, sleep, rate and intensity of speech, frequency and intensity of social contact) can all be passively collected using the suite of sensors and device use–logging capabilities available on all commodity smartphones (see Figure 2).
Figure 2.
Bipolar symptoms and potential smartphone measures.
Studies employing technology-based self-tracking show good receptivity and adherence by individuals with bipolar disorder (Bauer et al., 2004; Bopp et al., 2010; Schärer et al., 2002). Recent research has provided promising evidence that sensors can detect aspects of behavior relevant to bipolar disorder. In the MONARCA project, Frost, Doryab, Faurholt-Jepsen, Kessing, and Bardram (2013) developed a smartphone app to provide better disease insights by collecting data relevant to the behavioral trends of bipolar disorder. Based on data collected over 6 months, they found that patient mood correlated with physical activity, levels of stress, sleep, and phone use. Another study used phone call duration, speech analysis, and movement data from smart-phones to identify manic and depressive states (Grünerbl et al., 2014). From 12 weeks of data with 10 patients, their system recognized bipolar states and the transitions between those states (assessed using the Hamilton Rating Scale for Depression and Young Mania Rating Scale) with 76% accuracy. Vanello et al. described a speech analysis algorithm that takes into account voiced segmentation and pitch information to characterize states of patients of bipolar disorder (Lu et al., 2012; Vanello, 2012).
While there is a long history of using custom forms of behavioral sensing, such as the Actiwatch which detects physical activity and sleep behavior, in efforts to understand and treat bipolar disorders, patient adherence and acceptance of these technologies can limit the effectiveness of their application (Prociow, Wac, & Crowe, 2012). Individuals with bipolar disorder are particularly sensitive to issues of stigma and often refuse to use any device that might identify them as being “different.” Most important, the promise of passive sensing has not yet had an impact on clinical practice: The data collected via sensors have been limited almost exclusively to research, as opposed to clinical, settings.
Although recent work has shown success in using smart-phones to measure variables relevant to bipolar disorder, there has been no work, to the best of our knowledge, that has sought to use sensor data to replicate or “fill holes” in the data collected by self-report instruments used in existing, clinically validated interventions like IPSRT. Smartphone-based sensing of social rhythms could support patients who find self-tracking challenging to maintain, thereby increasing the quantity of clinically relevant information. There is also the potential for automatic sensing to measure the event or behavior of interest as it occurs and hence to provide a higher degree of ecological validity than current self-report methods. Perhaps a crucial difference with the SRM, which measures social rhythms to infer well-being, compared with other self-report diaries like, for example, Thought Diaries that are used in cognitive behavioral therapy, is that self-report of the SRM is not a prerequisite for valid data. If self-report could be replaced it would be, whereas in CBT, self-report is integral to the intervention (and is expected to have a therapeutic effect).
Design and Evaluation of MoodRhythm
In this section, we describe the design and evaluation of MoodRhythm, a cross-platform mobile app, built using an Open mHealth Architecture (Estrin & Sim, 2010). We describe the central design elements of the patient-facing app, how this design emerged from an iterative Participatory Design process (Muller & Kuhn, 1993) involving individuals with bipolar disorder and, finally, the results of a clinical pilot.
Challenges With the Paper-Based SRM
Although the SRM has been proven effective for tracking social routines, its paper-and-pencil format has multiple disadvantages, both as a clinical tool and a research instrument. Even well intentioned patients often forget to complete their SRM forms or do so inaccurately, particularly if adherence is challenged by episodes of mania or depression. These shortcomings echo well-identified limitations of paper diaries (Stone, Shiffman, Schwartz, Broderick, & Hufford, 2003) such as inconsistent completion, unreliable data as a result of retrospective recall (Coughlin, 1990). Clinician’s assessment of their patients’ social rhythms that is crucial to making treatment decision is hindered by the limitations of the paper-based tracking and patient retrospective recall.
Concerns have been raised among researchers about the degree to which illness severity, presence of psychosis, and absence of insight may interfere with the validity of self-reported measures (Altman, Hedeker, Janicak, Peterson, & Davis, 1994). That is, while observer-rated assessment of symptoms is considered reliable (Altman et al., 1994), the dependability of self-reported mood—especially during mania—remains more questionable, with studies showing mixed results when it comes to the reliable completion of self-rating assessments (Altman, 1998; Goodwin & Jamison, 2007; Rucci, Calugi, Miniati, & Fagiolini, 2013).
Although prior studies that used the paper-based SRM form have demonstrated that the social rhythm score do covary with mood, this is based on a generalized model as extracted from several research studies. In other words, the instrument is limited by the relevance to each patient of the five social rhythm events that the instrument is set up to track. An improved approach would be to identify individual social rhythm events that are key for each person.
Participatory Design of MoodRhythm
We realized that capturing the dynamic process of bipolar disorder might be greatly facilitated by the development of a smartphone application that not only permitted the completion of the self-report parts of the SRM on a device that was constantly (or nearly constantly) in the patient’s possession but could also enable automatic detection of a range of bipolar disorder-relevant parameters over the long term without the patient needing to provide explicit input. An electronic version of the SRM could both help address the issue of self-report bias and also relieve some of the burden for patients of self-tracking by harnessing latent passive sensing capabilities in order to automatically collect relevant social rhythm information. Such promising benefits have the potential to significantly enhance self-awareness and overall treatment quality.
In order to ensure the new system, MoodRhythm, met the needs of individuals with bipolar disorder, we sought to engage them integrally in the development of the application through Participatory Design. This is a user-centered development “approach towards computer systems design in which the people destined to use the system play a crucial role in designing it” (Schuler & Namioka, 1993, p. XI). Participatory Design developed in Scandinavia as a method for involving workers extensively in the development of their work environment and practices (Ehn, 1993; Kyng & Greenbaum, 1991). It has since been used more broadly as a method to integrate the participant’s perspective and knowledge of the design space. The end user is involved at all phases of the design process, having an equal hand in directing development directions. Involving end users early on and working closely with them can help avoid unpromising design paths, develop a more comprehensive understanding of the target domain and ultimately increase the likelihood that the resultant technology meets the needs of the end users.
Nowhere is such an approach more fitting than serious mental illness since patients’ lived experience is markedly different to system developers and clinicians. In particular, bipolar disorder has been associated with: deficits in performance IQ, disturbances in attention and concentration, short-term memory impairment, limitations in executive function (Robinson et al., 2006), as well as above-average creativity (Nowakowska, Strong, Santosa, Wang, & Ketter, 2005).
To develop MoodRhythm, we drew on the expertise of members of an academic research team (primarily information and computer scientists at a research university in the Northeastern United States), a team of professional psychological researchers, clinicians with expertise in conducting (and training others in the use of) IPSRT and most important, individuals with bipolar disorder. We provided all stakeholders long-term opportunities (over the course of 1 year) to serve as codesigners.
During the design process, participants used the mobile app in their daily lives and shared their feedback, design insights, and suggestions for enhancements to the app at least once a week. Iterations of the prototype app were wire-lessly sent to participants’ smartphones in response to this feedback. This process allowed participants to provide feedback on an ongoing basis during the design process and helped to identify and address concerns that patients and clinicians might have about these technologies and ensure the resulting system was effective in the messiness of everyday life. For a more complete report of the value of this process and the responses of users to the design of the mobile app, see Matthews et al. (2015).
Overview of MoodRhythm
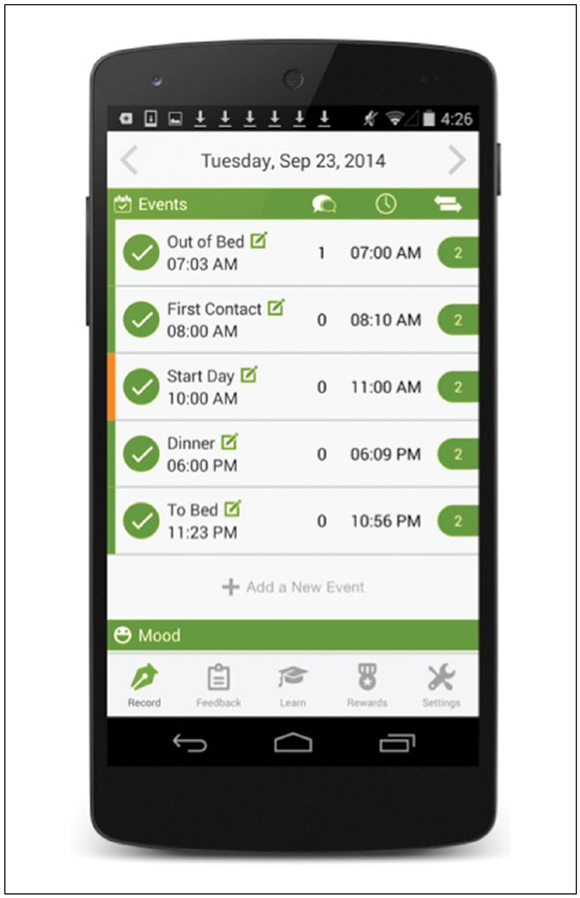
MoodRhythm helps patients track the five basic activities used in the prototypical paper version of the SRM (e.g., getting out of bed, starting your day, having dinner, etc.), but also enables them to add custom events that help anchor their social rhythm (see Figure 3). Patients can set daily routine targets and track how closely they meet these target times. Notes can be used to record additional information such as the amount of medication taken or factors that may have affected a patient’s routine or mood.
Figure 3.
MoodRhythm’s self-report screen.
The diary is designed to provide an at-a-glance summary of the patient’s successes in meeting their rhythm goals for both the current and preceding days. If the patient completes an activity within their customizable time window (the default is 45 minutes, the time period used to score hitting an event’s target in the traditional paper form), then the bar to the left turns green. When the window is about to elapse and an event is not yet recorded, the bar appears yellow (a “warning” that a potential rhythm disruption is occurring). If a patient misses the target, then the bar turns red.
Feedback from patients and therapists indicated that most bipolar disease patients completed their paper-based SRM entries in batches at the end of the day. Our goal was to support momentary use of the app to increase patient awareness of their daily targets and to limit the impact of memory impairments, poor concentration, and variations across stages of the illness. To achieve this, we implemented several paths to streamline the recording process including using notifications and making it possible for patients to quickly record SRM events directly from the notification panel on their smartphone.
On the diary screen in the app, users can quickly record an event by clicking the green radio button (Figure 3), which automatically enters the current time. If more detail is needed, clicking anywhere on the right-hand side of the screen brings up a more detailed form. Since fine-figured dexterity can be an issue for some patients due to medication side effects, we made the button (including the hit area) and other user interface elements as large as possible.
In the clinic, therapists typically use the patient’s SRM in two stages. Initially, it is used to map the patient’s current routine, without setting targets. Stage 2 requires using this collected data to set targets that the therapist and patient both agree are realistic. To mirror this clinical use of the paper diary, MoodRhythm supports both open-ended tracking and target-based tracking. The system places no limits on the number of events a user can create and monitor.
Extending the SRM Instrument
MoodRhythm takes advantage of a variety of smartphone sensors to passively detect social rhythms, levels of social interaction, and other aspects of daily life that are critical to wellness among individuals with bipolar disorder, with the ultimate aim to infer many of the activities included in the prototypical paper-based SRM instrument. The app continuously collects data from the phone’s light sensor, accelerometers, and microphone, as well as information about phone use events such as screen unlocks and battery charging state.
Our work in this area draws on several years’ of peer-reviewed algorithm design and empirical research in these areas, with sleep and social inference accuracies approaching 85% to 90% with minimal intervention on the user’s part (Lane et al., 2011). Our algorithm to measure levels of social interaction computes the frequency and duration of face-to-face conversations that a phone’s owner has over the course of the day based on an analysis of audio data continuously collected using the smartphone’s built-in microphone. The embedded microphone is activated every 2 minutes to capture ambient sound. If human speech is detected, the microphone remains active. To preserve privacy, audio recordings are not recorded, but instead processed data in real time on the smartphone to only extract and store features (e.g., spectral content and regularity, loudness) that are useful for detecting the presence of human voice but insufficient to reconstruct speech content (Wyatt, Choudhury, Bilmes, & Kitts, 2011). Using these privacy-sensitive audio features and probabilistic inference techniques, it is possible to reliably estimate the number of conversations an individual engages in, the duration of the conversations, and how much time a given individual speaks within a conversation along with speaking rate and variations in pitch (Wyatt et al., 2011).
Physical activity is captured via the smartphone’s accelerometers, which detect movement. Based on the amount and intensity of movement detected by the phone, the system identifies and stores a high-level representation of the patient’s physical activity state (e.g., active vs. sedentary). To detect a person’s location, the app uses the Android location service, which combines Global Position System, Wi-Fi, and cellular data to provide location estimations. MoodRhythm also collects communication patterns including SMS and call logs. The sensor data are stored on the smartphone and securely transmitted to our remote study server periodically. The impact of the app on battery life is reasonable, permitting 16 hours of continuous sensing after a full recharge.
Effectiveness and Acceptance of MoodRhythm
In a small clinical pilot over four weeks with seven individuals with bipolar disorder, we found evidence that automated sensing can be used to accurately infer the patients’ SRM score (Abdullah et al., 2016). During the study, participants completed SRM entries using an Android version of the smartphone app. Using location, distance travelled, conversation frequency, and nonstationary duration as inputs, our generalized model achieves root mean square error of 1.40, a reasonable performance given the range of SRM score (0–7). Personalized models further improved performance, with a mean root mean square error of 0.92 across users. Classifiers using the sensor streams were able to predict stable (SRM score ≥ 3.5) and unstable (SRM score < 3.5) states with high accuracy (precision: 0.85 and recall: 0.86). This study provided initial evidence that automatic smartphone sensing is a feasible approach for inferring social rhythmicity and may be used over a long period of time to provide continuous measurement.
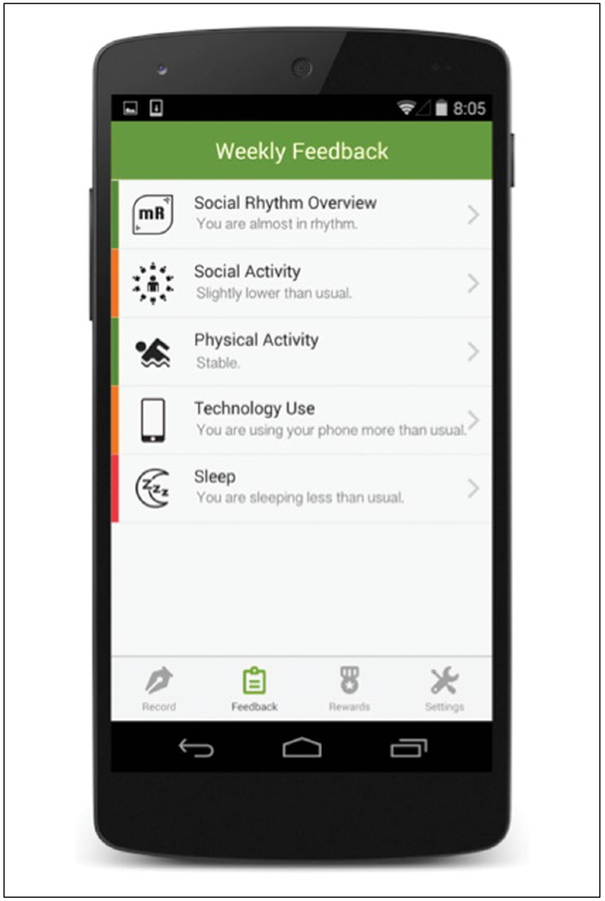
Perhaps most crucially, we also found that participants are very happy to use MoodRhythm and do not encounter challenges using the software. This is reflected in our poststudy usability survey—average System Usability Scale rating (Brooke, 1996) across participants was 85.94 (SD = 10.43), which is higher than 90th percentile when compared against prior scores of other systems. A principal factor in the acceptance of the technology related to the convenience of using the smartphone to record activities. Another key aspect was reducing the time to receive feedback (see Figures 3 and 4) for patients, who typically only reflect on the paper forms when they see their psychiatrist: Getting the visual feedback when my day worked within the targeted times gave me more confidence that I could meet my doctor’s expectations.
Figure 4.
MoodRhythm’s feedback screen.
Discussion
From Paper to Smartphone to Sensor
The combination of self-report and automatically sensed data collection opens up research possibilities to explore characteristics of bipolar disorders that we were not able to reliably examine with previous versions of the SRM instrument. For example, the appropriate timescale of the dynamic process of bipolar disorder is an empirical question that, to our knowledge has not been formally addressed in research and probably differs from disorder subtype-to-subtype and even person-to-person. In our own work, we have seen that the timescale for bipolar I disorder is likely quite different from that of bipolar II disorder—our patients with bipolar I disorder never question our request that they provide a single rating of their mood at the end of each day, whereas the patients we have worked with who have a bipolar II diagnosis frequently find it nearly impossible to attach a single-mood rating to a given day because they report experiencing so much mood variability of the course of a day. Thus, the question of how often to record mood (and/or energy) appears to be a function of the bipolar subtype in question. As implied, “once daily” measurement seems to be sufficient for individuals with bipolar I disorder, while more frequent monitoring—perhaps as often as every couple of waking hours—may be required to get an accurate picture of mood variability for individuals with some bipolar sub-types. From a clinical perspective, making it easy to collect the data and providing feedback opens up the possibility for patients and therapists to take a longitudinal view of patient’s social rhythms and mood.
Many other approaches that employ self-report diaries, hinge on patient reflection to facilitate change. This is not the case with the SRM. The measurement of social rhythms is a particularly suitable candidate for automatic detection because it does not require patients to actively reflect on an internal state. The Social Zeitgeber hypothesis identifies social rhythm disruption as a causal factor that can lead to a manic or depressive episode. If smartphone sensing of social rhythms proves similarly effective in larger scale studies, then it may become unnecessary for patients to actively engage in EMA self-report over a long period of time as part of therapy (or at least infrequently).
However, while smartphone sensing offers the potential to unobtrusively measure a person’s social rhythms, it is important to consider the impact, positive or negative, that replacing self-reported EMA might have on participants at various stages of managing their illness and learning about IPSRT.
When a participant is asked to take an action that is out of the ordinary, there is the possibility that this action will result in a change. This applies to EMAs that involve self-report. The simple act of paying more attention to one’s mood for a week as part of an EMA protocol might result in a greater awareness of variations in how one is feeling and, as a consequence, change the patient’s behavior or affect.
Self-tracking of social rhythms in IPSRT may give patients whose disorder makes them feel very out of control and who have been told there is nothing they can do to control their moods except take their medication, some sense of control. It also serves a central function of IPSRT, namely stabilizing social routines through the use of target times for each event.
The Promise of Continuous Ecologically Valid Measurement
The smartphone facilitates the continuous measurement of what before was practically impossible through self-reported means. The major benefit of incorporating smart-phones into these kinds of treatments lies in the capacity of smartphone’s to measure in near continuous fashion clinically relevant factors in ecologically valid settings. Prior research has demonstrated this potential in various domains (e.g., Rabbi, Aung, Zhang, & Choudhury, 2015). In our pilot sensing study, we used self-reported data from a smartphone-based SRM to validate sensor data. It is worth considering whether in the future the SRM instrument should be left to the side entirely, and instead, only use self-reported and third-party measures of mood state to validate the sensing approach.
While in situ smartphone-based assessment can have a significant impact on therapeutic practices, current instantiations of these technologies have a number of limitations. In particular, potential ambiguity related to the proximity of the phone to the participant can result in incorrect classifications (e.g., data streams indicating that a participant has been sedentary for a long time compared with streams produced by a participant who forgot to carry his phone). Such noise in data can also result from variations in use. Unlike smartwatches that can be expected to be worn on a person’s wrist, smartphones can be carried and used in many different ways. In the future, we can expect wearable devices and smartphones to converge into a consistent and on-body form factor, which may serve to diminish this uncertainty. For now, the smartphone is a more established personal device than the novel wearable devices that are emerging in the marketplace, and it is more likely to remain charged and used by its owner. Furthermore, the smartphone does not only offer the possibility of measuring real-world behavior but offers a strong signal of smartphone-mediated behavior (e.g., SMS use, phone calls, alarm use, etc.). In other contexts, researchers are increasingly finding that such soft-sensed data—data harvested from a person’s use and interactions with their smartphone—provide helpful data on behavior and state (e.g., Abdullah, Matthews, Murnane, Gay, & Choudhury, 2014).
EMA to EMI
Smartphones open up the possibility of harvesting a broad array of data pertinent to social rhythms without active user engagement. Machine learning algorithms can then use this information to tune measurements and interventions for each patient based on their routines, activities, behaviors, and preferences. Compared with a generalized strategy, such individualized approaches would be particularly useful since each patient’s symptoms can manifest in idiosyncratic ways (e.g., a manic phase might result in different shopping behavior for one patient and increased social interaction for another). Gold-standard research and intervention approaches could employ novel research designs (e.g., N = 1) that harness smartphone sensors to unobtrusively monitor individual dynamic processes and set individual thresholds and markers for stability and instability. Adopting this approach could then increase the benefits for individuals to participate promising that they will learn something specific to them.
The automatic identification of behavioral rhythms may also be used in similar treatments or as a standalone intervention to assess individual well-being on a continual basis, offering novel opportunities for clinical intervention in serious mental illness.
It has only recently become possible as a result of technological inventions to present feedback on data collected via EMA to participants. In the existing clinical process, it is not possible to provide in situ feedback that can help patients continue recovery or sustain behavior to prevent future mood episodes. Using smartphones to deliver momentary interventions, thus, has the potential to become a core component of delivering therapy when it is needed and where it is needed. Such ecological momentary interventions (EMI) could be triggered by either an automated system or a therapist, based on collected data.
Moreover, it may also be possible for smartphone applications to mirror the therapeutic process. In IPSRT, for example, the therapist uses the SRM and information provided by the patient to create an achievable daily schedule with the goal of stabilizing mood. EMA could be used as a rough approximation of this therapeutic process to drive EMI. For example, based on social rhythms detected by sensor data and self-reported mood, the smartphone could incrementally suggest adjusted schedule times and monitor individual progress toward these goals. A similar approach was taken in recent work to encourage physical activity (Rabbi et al., 2015); users’ existing patterns of behavior and their current location, as detected via the smartphone sensors, were used to suggest new walking routes.
In this way, sensing data could support a continuous monitoring system that prompts real-time in situ interventions. Self-management often starts with psychoeducation. It is a core component of IPSRT. Therapists particularly focus on educating patients about the disorder including information about symptoms, medications, and the possible role of social and circadian disruptions (Frank, Swartz, & Kupfer, 2000). Even after recovery, psychoeducation can play a crucial role in sustaining healthy behavior. But, current psychoeducation in clinical practice often has same generic content for all participants. Being able to monitor behavioral trends and instantaneously detect disruptions can open up ways to provide personalized psychoeducation content for specific context. For example, unstable sleep–wake cycles of a participant could result in a reminder of how a similar pattern affected the participant before and the importance of maintaining rhythmicity. Examples of real-time EMI could include the following: suggesting contextualized therapeutic activities and even adjusting the way the smartphone app interacts with the user and presents feedback, as suggested in our prior work (Matthews et al., 2015).
Conclusion
There is tremendous potential to make significant advances in ecologically valid measurement and intervention through the synthesis of advances in the fields of bipolar disorder treatment, behavioral sensing, and mobile health design. Our initial effort in this space, MoodRhythm, helped overcome many of the limitations of the paper-based SRM and directly tackled the challenges patients face by providing a convenient self-report app that also has the potential for long-term monitoring across phases of the illness via the use of smartphone sensors. This combination of self-report and passive sensing has wide application for lifelong diseases like bipolar disorder where it can be extremely challenging to maintain regular self-tracking, but where self-reported information, particularly at the outset of treatment, can be a highly valuable activity leading to critical insights for the patient and their clinician. Smartphone technology also opens up a new possibility of context-specific and ecologically valid interventions. Yet there are important considerations that will determine the effectiveness of these new technologies such as how to process and present this significant amount of data to clinicians and patients, and crucially how to understand the factors related to the acceptance by all end users of these new technologies.
Acknowledgments
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: M.M., E.F., and T.C. co-founded and have equity interest in HealthRhythms. G.G. serves on the advisory board for HealthRhythms.
References
- Abdullah S, Matthews M, Frank E, Doherty G, Gay G, & Choudhury T (2016). Automatic detection of social rhythms in bipolar disorder. Journal of the American Medical Informatics Association. Advance online publication. doi: 10.1093/jamia/ocv200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdullah S, Matthews M, Murnane EL, Gay G, & Choudhury T (2014, September). Towards circadian computing: Early to bed and early to rise makes some of us unhealthy and sleep deprived Paper presented at the Proceedings of the 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Seattle, WA. [Google Scholar]
- Altman E (1998). Rating scales for mania: Is self-rating reliable? Journal of Affective Disorders, 50, 283–286. [DOI] [PubMed] [Google Scholar]
- Altman EG, Hedeker DR, Janicak PG, Peterson JL, & Davis JM (1994). The Clinician-Administered Rating Scale for Mania (CARS-M): Development, reliability, and validity. Biological Psychiatry, 36, 124–134. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, & Tondo L (2003). Suicide risk and treatments for patients with bipolar disorder. Journal of the American Medical Association, 290, 1517–1519. [DOI] [PubMed] [Google Scholar]
- Bauer M, Grof P, Gyulai L, Rasgon N, Glenn T, & Whybrow PC (2004). Using technology to improve longitudinal studies: Self-reporting with ChronoRecord in bipolar disorder. Bipolar Disorders, 6, 67–74. [DOI] [PubMed] [Google Scholar]
- Ben-Zeev D, Davis KE, Kaiser S, Krzsos I, & Drake RE (2013). Mobile technologies among people with serious mental illness: Opportunities for future services. Administration and Policy in Mental Health and Mental Health Services Research, 40, 340–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bopp JM, Miklowitz DJ, Goodwin GM, Stevens W, Rendell JM, & Geddes JR (2010). The longitudinal course of bipolar disorder as revealed through weekly text messaging: A feasibility study. Bipolar Disorders, 12, 327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooke J (1996). SUS: A “quick and dirty” usability scale In Jordan PW, Thomas B, Weerdmeester BE & McClelland IL (Eds.), Usability evaluation in industry (pp. 189–194). Milton Park, England: Taylor & Francis. [Google Scholar]
- Corruble E, Frank E, Gressier F, Courtet P, Bayle F, Llorca P-M, … Gorwood P (2014). Morningness–eveningness and treatment response in major depressive disorder. Chronobiology International, 31, 283–289. [DOI] [PubMed] [Google Scholar]
- Coughlin SS (1990). Recall bias in epidemiologic studies. Journal of Clinical Epidemiology, 43, 87–91. [DOI] [PubMed] [Google Scholar]
- Ehlers CL, Frank E, & Kupfer DJ (1988). Social zeitgebers and biological rhythms: A unified approach to understanding the etiology of depression. Archives of General Psychiatry, 45, 948–952. [DOI] [PubMed] [Google Scholar]
- Ehn P (1993). Scandinavian design: On participation and skill In Schuler D (Ed.), Participatory design: Principles and practices (pp. 41–77). Hillsdale, NJ: Lawrence Erlbaum. [Google Scholar]
- Estrin D, & Sim I (2010). Open mHealth architecture: An engine for health care innovation. Science, 330, 759–760. [DOI] [PubMed] [Google Scholar]
- Frank E (2005). Treating bipolar disorder: A clinician’s guide to interpersonal and social rhythm therapy. New York, NY: Guilford Press. [Google Scholar]
- Frank E, Kupfer DJ, Thase ME, Mallinger AG, Swartz HA, Fagiolini AM, … Thompson W (2005). Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Archives of General Psychiatry, 62, 996–1004. [DOI] [PubMed] [Google Scholar]
- Frank E, Soreca I, Swartz HA, Fagiolini AM, Mallinger AG, Thase ME, … Kupfer DJ (2008). The role of interpersonal and social rhythm therapy in improving occupational functioning in patients with bipolar I disorder. American Journal of Psychiatry, 165, 1559–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank E, Swartz HA, & Kupfer DJ (2000). Interpersonal and social rhythm therapy: Managing the chaos of bipolar disorder. Biological Psychiatry, 48, 593–604. [DOI] [PubMed] [Google Scholar]
- Frost M, Doryab A, Faurholt-Jepsen M, Kessing LV, & Bardram JE (2013, September). Supporting disease insight through data analysis: Refinements of the monarca self-assessment system Paper presented at the Proceedings of the 2013 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Zurich, Switzerland. [Google Scholar]
- Goodwin FK, & Jamison KR (2007). Manic-depressive illness: Bipolar disorders and recurrent depression (Vol. 1). Oxford, England: Oxford University Press. [Google Scholar]
- Grünerbl A, Muaremi A, Osmani V, Bahle G, Öhler S, Tröster G, … Lukowicz P (2014). Smartphone-based recognition of states and state changes in bipolar disorder patients. IEEE Journal of Biomedical and Health Informatics, 19, 140–148. [DOI] [PubMed] [Google Scholar]
- Harvey A (2008). Sleep and circadian rhythms in bipolar disorder: Seeking synchrony, harmony, and regulation. American Journal of Psychiatry, 165, 820–829. [DOI] [PubMed] [Google Scholar]
- Haynes PL, McQuaid J, Ancoli-Israel S, & Martin JL (2006). Disrupting life events and the sleep-wake cycle in depression. Psychological Medicine, 36, 1363–1373. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2006). Improving the quality of health care for mental and substance-use conditions (Quality Chasm Series). Washington, DC: National Academies. [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, Coryell W, Endicott J, Maser JD, … Keller MB (2003). A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Archives of General Psychiatry, 60, 261–269. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyng M, & Greenbaum J (1991). Cooperative design: Bringing together the practices of users and designers In Nissen H-E, Klein HK & Hirschheim R (Eds.), Information systems research: Contemporary approaches & emergent traditions (pp. 405–416). Amsterdam, Netherlands: North-Holland. [Google Scholar]
- Lane ND, Mohammod M, Lin M, Yang X, Lu H, Ali S, … Campbell A (2011, May). Bewell: A smart-phone application to monitor, model and promote wellbeing Paper presented at the 5th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth2011), Dublin, Ireland. [Google Scholar]
- Levenson J, & Frank E (2011). Sleep and circadian rhythm abnormalities in the pathophysiology of bipolar disorder In Manji HK & Zarate CA Jr. (Eds.), Behavioral neurobiology of bipolar disorder and its treatment (pp. 247–262). Berlin, Germany: Springer. [DOI] [PubMed] [Google Scholar]
- Li I, Dey A, & Forlizzi J (2010, April). A stage-based model of personal informatics systems Paper presented at the Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Atlanta, GA. [Google Scholar]
- Lu H, Frauendorfer D, Rabbi M, Mast MS, Chittaranjan GT, Campbell AT, … Choudhury T (2012, September). StressSense: Detecting stress in unconstrained acoustic environments using smartphones Paper presented at the Proceedings of the 2012 ACM Conference on Ubiquitous Computing, Pittsburgh, PA. [Google Scholar]
- Malkoff-Schwartz S, Frank E, Anderson B, Sherrill JT, Siegel L, Patterson D, & Kupfer DJ (1998). Stressful life events and social rhythm disruption in the onset of manic and depressive bipolar episodes: A preliminary investigation. Archives of General Psychiatry, 55, 702–707. [DOI] [PubMed] [Google Scholar]
- Matthews M, Voida S, Abdullah S, Doherty G, Choudhury T, Im S, & Gay G (2015, August). In situ design for mental illness: Considering the pathology of bipolar disorder in mhealth design Paper presented at the MobileHCI ‘15: 17th International Conference on Human-Computer Interaction with Mobile Devices and Services Proceedings, Copenhagen, Denmark. [Google Scholar]
- Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Kogan JN, Sachs GS, … Ostacher MJ (2007). Intensive psychosocial intervention enhances functioning in patients with bipolar depression: Results from a 9-month randomized controlled trial. American Journal of Psychiatry, 164, 1340–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk TH, Flaherty JF, Frank E, Hoskinson K, & Kupfer DJ (1990). The social rhythm metric: An instrument to quantify the daily rhythms of life. Journal of Nervous and Mental Disease, 178, 120–126. [DOI] [PubMed] [Google Scholar]
- Monk TH, Frank E, Potts JM, & Kupfer DJ (2002). A simple way to measure daily lifestyle regularity. Journal of Sleep Research, 11, 183–190. [DOI] [PubMed] [Google Scholar]
- Moskowitz DS, Russell JJ, Sadikaj G, & Sutton R (2009). Measuring people intensively. Canadian Psychology/ Psychologie Canadienne, 50, 131–140. [Google Scholar]
- Muller MJ, & Kuhn S (1993, June). Participatory design. Communications of the ACM, 36, 24–28. [Google Scholar]
- Murnane E, Cosley D, Chang P, Guha S, Frank E, Gay G, & Matthews M (2016). Self-monitoring practices, attitudes, and needs of individuals with bipolar disorder: Implications for the design of technologies to manage mental health. Journal of the American Medical Informatics Association, 23, 477–484. doi: 10.1093/jamia/ocv165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJL, & Lopez AD (1996). The global burden of disease (Vol. 1). Cambridge, MA: Harvard University Press. [Google Scholar]
- National Council For Behavioral Health. (2014). Behavioral health IT: The foundation for coordinated care. Retrieved from http://www.thenationalcouncil.org/topics/behavioral-health-information-technology
- Nowakowska C, Strong CM, Santosa CM, Wang PW, & Ketter TA (2005). Temperamental commonalities and differences in euthymic mood disorder patients, creative controls, and healthy controls. Journal of Affective Disorders, 85, 207–215. [DOI] [PubMed] [Google Scholar]
- Prociow P, Wac K, & Crowe J (2012). Mobile psychiatry: Towards improving the care for bipolar disorder. International Journal of Mental Health Systems, 6(1), 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabbi M, Aung MH, Zhang M, & Choudhury T (2015, September). MyBehavior: Automatic personalized health feedback from user behaviors and preferences using smart-phones Paper presented at the Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Osaka, Japan. [Google Scholar]
- Robinson LJ, Thompson JM, Gallagher P, Goswami U, Young AH, Ferrier IN, & Moore PB (2006). A meta-analysis of cognitive deficits in euthymic patients with bipolar disorder. Journal of Affective Disorders, 93, 105–115. [DOI] [PubMed] [Google Scholar]
- Roche MJ, Pincus AL, Rebar AL, Conroy DE, & Ram N (2014). Enriching psychological assessment using a person-specific analysis of interpersonal processes in daily life. Assessment, 21, 515–528. [DOI] [PubMed] [Google Scholar]
- Rucci P, Calugi S, Miniati M, & Fagiolini A (2013). A review of self-report and interview-based instruments to assess mania and hypomania symptoms. Journal of Psychopathology, 19, 143–159. [Google Scholar]
- Schärer LO, Hartweg V, Valerius G, Graf M, Hoern M, Biedermann C, … Forsthoff A (2002). Life charts on a palmtop computer: First results of a feasibility study with an electronic diary for bipolar patients. Bipolar Disorders, 4(Suppl. 1), 107–108. [DOI] [PubMed] [Google Scholar]
- Schuler D, & Namioka A (Eds.). (1993). Participatory design: Principles and practices. Boca Raton, FL: CRC Press. [Google Scholar]
- Soreca I, Frank E, & Kupfer DJ (2009). The phenomenology of bipolar disorder: What drives the high rate of medical burden and determines long-term prognosis? Depression and Anxiety, 26, 73–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone AA, & Shiffman S (1994). Ecological momentary assessment (EMA) in behavorial medicine. Annals of Behavioral Medicine, 16, 199–202. [Google Scholar]
- Stone AA, Shiffman S, Schwartz JE, Broderick JE, & Hufford MR (2003). Patient compliance with paper and electronic diaries. Controlled Clinical Trials, 24, 182–199. [DOI] [PubMed] [Google Scholar]
- Swartz HA, Frank E, Frankel DR, Novick D, & Houck P (2009). Psychotherapy as monotherapy for the treatment of bipolar II depression: A proof of concept study. Bipolar Disorders, 11, 89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz HA, Frank E, O’Toole K, Newman N, Kiderman H, Carlson S, … Wells KF (2011). Implementing interpersonal and social rhythm therapy for mood disorders across a continuum of care. Psychiatric Services, 62, 1377–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, & Ebner-Priemer U (2013). Ambulatory assessment. Annual Review of Clinical Psychology, 9, 151–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanello N, Guidi A, Gentili C, Werner S, Bertschy G, Valenza G, … Scilingo EP (2012, Aug-Sep). Speech analysis for mood state characterization in bipolar patients Paper presented at the Engineering in Medicine and Biology Society (EMBC), 2012 Annual International Conference of the IEEE, San Diego, CA. [DOI] [PubMed] [Google Scholar]
- Wichers M (2014). The dynamic nature of depression: A new micro-level perspective of mental disorder that meets current challenges. Psychological Medicine, 44, 1349–1360. [DOI] [PubMed] [Google Scholar]
- Wichers M, Simons CJP, Kramer IMA, Hartmann JA, Lothmann C, Myin-Germeys I, … van Os J (2011). Momentary assessment technology as a tool to help patients with depression help themselves. Acta Psychiatrica Scandinavica, 124, 262–272. [DOI] [PubMed] [Google Scholar]
- Woods SW (2000). The economic burden of bipolar disease. Journal of Clinical Psychiatry, 61(Suppl. 13), 38–41. [PubMed] [Google Scholar]
- Wyatt D, Choudhury T, Bilmes J, & Kitts JA (2011). Inferring colocation and conversation networks from privacy-sensitive audio with implications for computational social science. ACM Transactions on Intelligent Systems and Technology (TIST), 2(1), 1–7. [Google Scholar]