Abstract
To investigate the clinical characteristics and risk factors for miscarriage of intrauterine normal pregnancy of patients with a heterotopic pregnancy (HP) after treatment.
This was a retrospective study of medical records from CHA Bundang Medical Center. Sixty-four patients who were diagnosed with a HP between February 2006 and July 2017 were included in this study. All analyses were performed using SAS software, version 9.4 (SAS Institute, Inc., Cary, NC). P values < .05 were considered statistically significant.
Forty-eight patients had tubal ectopic pregnancies (EP), 10 patients had cornual EPs, 1 patient had a cesarean section scar EP, 4 patients had an ovarian EP, and 1 patient had bilateral tubal EP. Among the 64 patients, 14.1% (9/64) miscarried before 10 weeks of gestation after management. Mean gestational age (GA) at treatment was 5.97 ± 0.50 weeks and 6.80 ± 1.04 weeks for miscarriage and nonmiscarriage group, respectively (P = .008). Significant differences were observed between 2 groups in terms of ultrasonographic features at the time HP was diagnosed (P = .040) Logistic regression models indicated that gestational age at treatment showed significant differences between 2 groups (OR: 0.003, 95% CI: 0.001–0.604).
Immediate management after diagnosis could expect favorable prognosis of HP. GA at treatment was the only independent risk factor for miscarriage in patients with HP regardless of treatment methods.
Keywords: fetal heart beat, gestational age, heterotopic pregnancy, miscarriage, outcome
1. Introduction
Heterotopic pregnancy (HP) is defined as the simultaneous existence of intrauterine pregnancy (IUP) and extrauterine ectopic pregnancy (EP). The incidence of HP in patients with a natural pregnancy is about 1 in 10,000 to 1 in 50,000 pregnancies.[1] However, because assisted reproductive technologies (ARTs) are widely used, the incidence of HP is greater, ranging from 1 in 100 to 1 in 3600 pregnancies, with a prevalence of 0.5% to 1% among all pregnancies.[2]
The early diagnosis and treatment of HP are essential since rupture during EP causes life-threatening complications such as hypovolemic shock and maternal death. However, the diagnosis of HP in the early stage is difficult, since a visible IUP on transvaginal sonography (TVS) can easily lead clinicians to ignore the existence of a possible EP. Moreover, an EP might be too small to detect on TVS in the early stage, and β-human chorionic gonadotropin (hCG) measurements are not helpful to detect HP, although they are useful to distinguish an EP from a normal, early IUP.
The primary treatment goal of HP is successful removal of an EP while preserving a normal IUP. The treatment options of HP may be surgical, medical, or expectant. If the patient does not have a hemoperitoneum or symptoms such as abdominal pain, and findings that are seen on serial ultrasound do not worsen, expectant treatment may be performed. However, if the patient's condition is hemodynamically and symptomatically unstable, the EP must be removed through surgical treatment such as laparotomy or laparoscopy. In patients with an unruptured cornual or cesarean section scar EP, ultrasound-guided local injection of potassium chloride (KCL), methotrexate (MTX), or aspiration of the gestational sac (GS) can be considered. The early diagnosis and management of HP can reduce severe maternal morbidity and mortality, but whether the early treatment of EP has favorable effects on the outcomes of IUP has not been elaborated upon in detail. Several reports have evaluated the diagnosis, treatment, and outcomes of patients with an HP, but most of these studies are case reports.[1–3]
The purpose of this study was to evaluate the clinical characteristics of patients with HP, the risk factors of miscarriage of IUP after the treatment of HP.
2. Methods
This study was a retrospective study of 64 patients who were diagnosed with HP between February 2006 and July 2017 at Bundang CHA Medical Center, Korea. Ethical approval was obtained from the institutional review board of Bundang CHA Medical Center (CHAMC 2018-02-024).
Sixty-four patients who were diagnosed with HP were included in this study. Two patients became pregnant naturally and 62 patients became pregnant using an ART. The ARTs included controlled ovarian hyperstimulation and timed intercourse (COH-TI), intrauterine insemination (IUI), and in vitro fertilization (IVF). IUP was determined in patients in whom a yolk sac (YS) and/or fetal pole was detected in an intrauterine GS using TVS. We retrospectively analyzed the basic characteristics of the study group, including age, body mass index, parity, abortion history, EP history, gynecological surgery history, gestational age (GA) at the time HP was diagnosed, ultrasonography findings, clinical features, EP site, treatment method of HP, and pregnancy outcomes, including miscarriage immediately after treatment.
A miscarriage after treatment was defined as an abortion before a GA of 10 weeks, excluding those with a vanishing intrauterine twin pregnancy after treatment. HP was diagnosed via transvaginal or abdominal ultrasonography. Patients had routine elective ultrasonography within 5 to 6 weeks of gestation. Those with symptoms such as abdominal pain or vaginal bleeding underwent emergent ultrasonography. Ultrasonography was performed to evaluate the status of the intrauterine fetus, including single or twin pregnancy fetuses, presence of a YS or fetal heart activity, EP site, and presence of a hemoperitoneum. Treatment was performed within 24 hours if HP was suspected. The operation time was calculated as the time from when a skin incision was made to the time when the skin was closed, and the anesthesia time was calculated as the time from when the patient first underwent an anesthetic procedure to when the patient awoke from anesthesia.
For the statistical analyses, the Chi-square test or Fisher exact test was used for categorical variables and the 2-sample t test or Wilcoxon rank sum test was used for continuous variables. Logistic regression with the penalized maximum likelihood estimation method was used to estimate odds ratios with 95% confidence intervals for risk factors of miscarriage after the treatment of HP. All analyses were performed using SAS software, version 9.4 (SAS Institute, Inc., Cary, NC). All P values <.05 were considered statistically significant.
3. Results
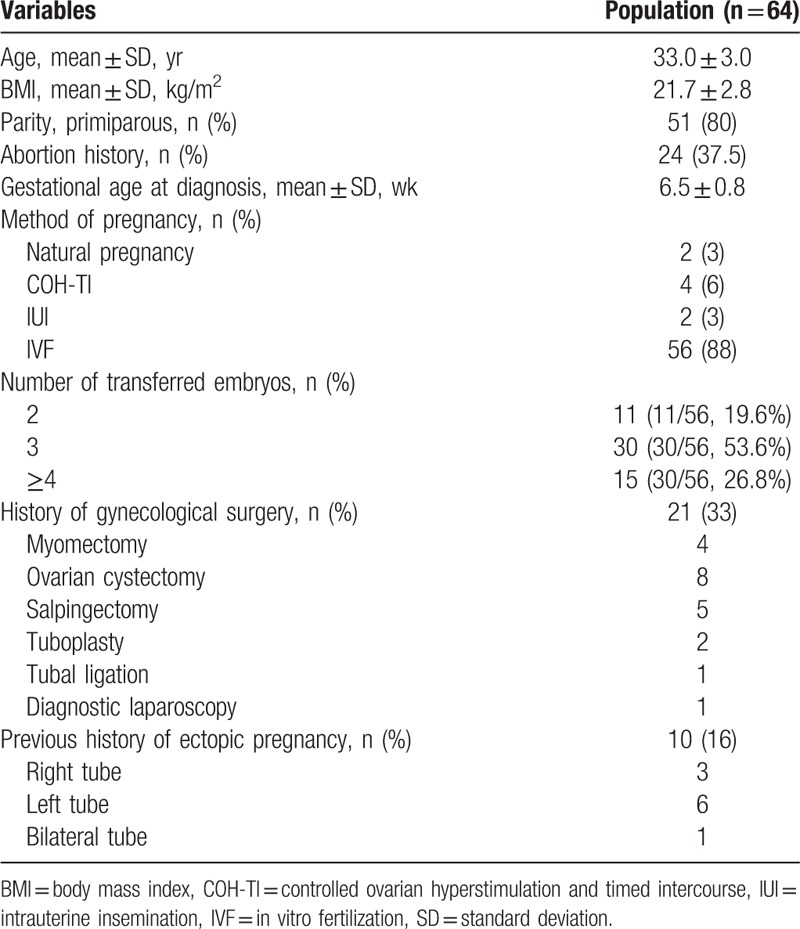
The basic characteristics of patients were investigated. Twenty-one (33%) patients had a history of gynecological surgery and 8 (12.5%) patients had undergone tubal surgery. Ten (16%) patients had a history of EP among study population (Table 1).
Table 1.
Basic characteristics of patients.
Among the 64 patients in this study, 19 patients had a normal twin pregnancy. Among those with a twin IUP, a patient had a miscarriage and 3 patients had a vanishing twin after treatment that resulted in a single-born live birth. The location of the EP was determined with TVS with confirmation via laparoscopy in most of the cases. Forty-eight patients had tubal pregnancies (Fig. 1), 10 patients had cornual pregnancies (Fig. 2A), a patient had a cesarean section scar pregnancy (Fig. 2B), 4 patients had ovarian pregnancies (Fig. 3A) and all patients underwent laparoscopic operation (Fig. 3B).
Figure 1.
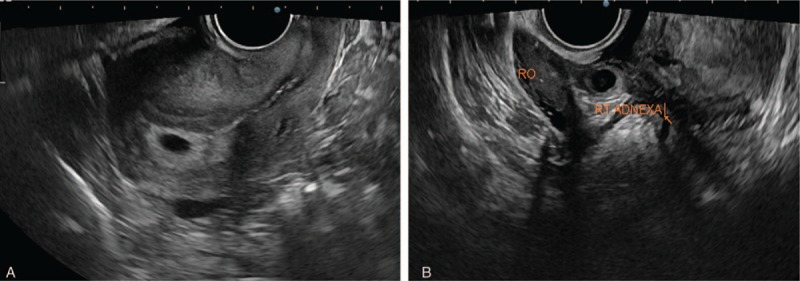
(A) Sonographic feature of normal intrauterine pregnancy of heterotopic pregnancy and (B) right tubal pregnancy in same patient.
Figure 2.
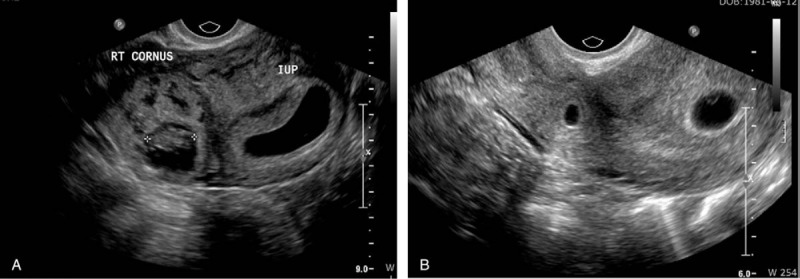
(A) Sonographic feature of heterotopic pregnancy with right cornual ectopic pregnancy. (B) Sonographic feature of heterotopic pregnancy with cesarean section scar ectopic pregnancy.
Figure 3.
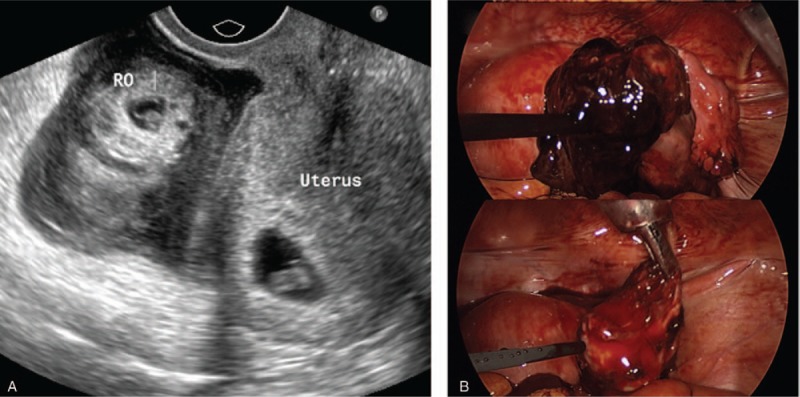
(A) Sonographic feature of heterotopic pregnancy with right ovarian ectopic pregnancy. (B) Laparoscopic finding of heterotopic pregnancy with ruptured right ovarian ectopic pregnancy.
At the time of diagnosis, 1 patient had only a GS; 10 patients had a GS, YS, and absence of fetal heart activity; and 53 patients had fetal heart activity of the IUP that was seen on ultrasonography (Table 2).
Table 2.
Clinical features at the time of diagnosis.
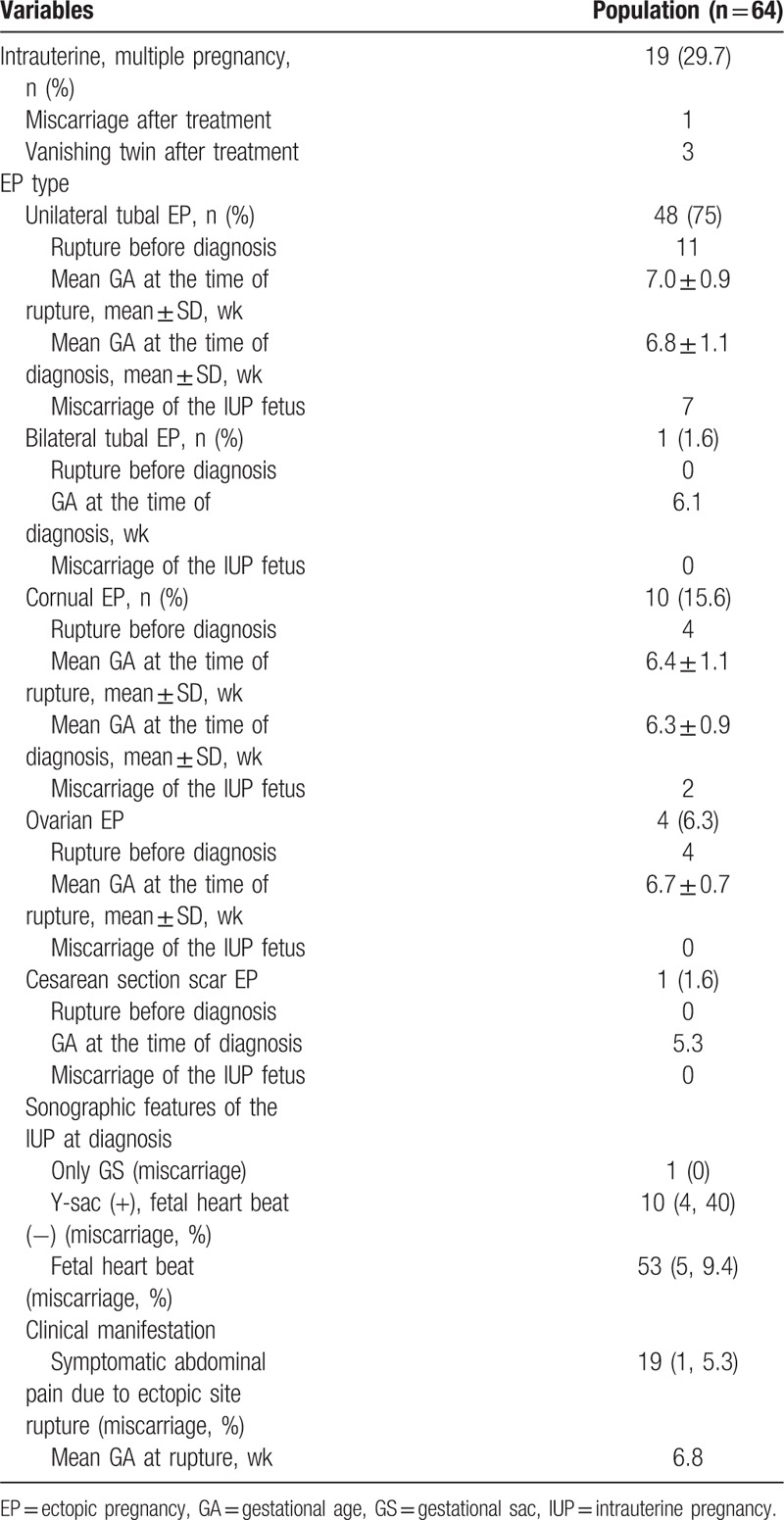
We investigated the management of HP (Table 3). Among those with a tubal HP, 47 patients underwent laparoscopic salpingectomy, 1 patient underwent exploratory salpingectomy, and 1 patient underwent ultrasound-guided GS aspiration. In addition, among 10 patients with a cornual HP, 5 patients underwent laparoscopic cornual resection, 4 patients received an ultrasound-guided KCL injection, and 1 patient received an ultrasound-guided MTX injection after spontaneously miscarrying her IUP fetus. One patient with a cesarean section scar HP miscarried an EP fetus soon after treatment.
Table 3.
Treatment of ectopic pregnancy.
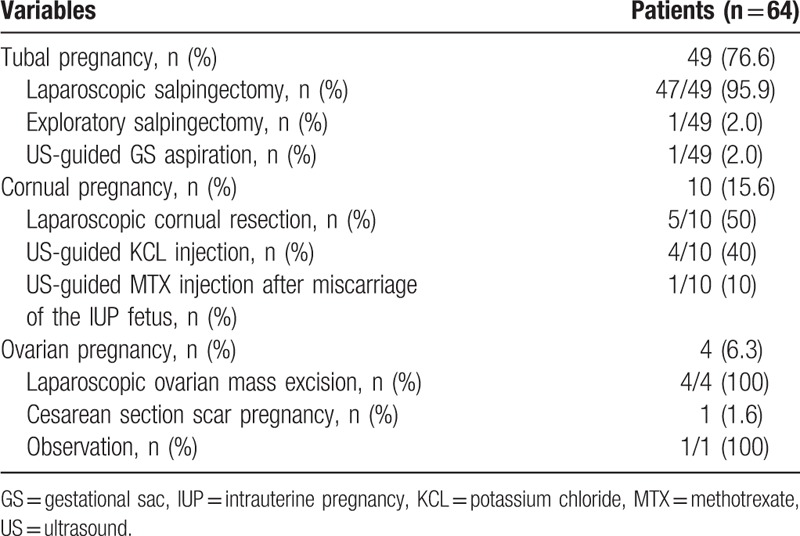
Four patients with an ovarian HP underwent laparoscopic excision of an ovarian mass.
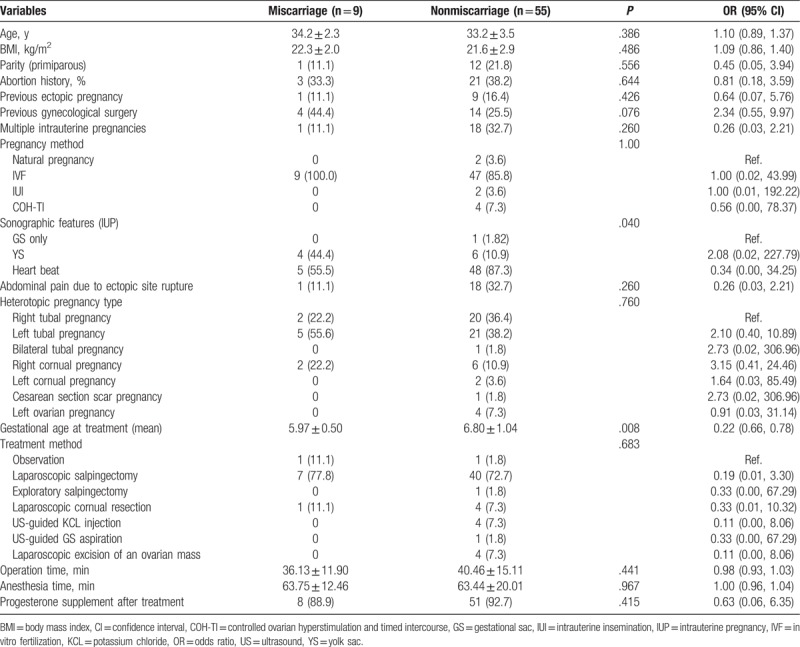
Among the 64 patients, 9 miscarried before 10 weeks’ gestation, within 3 weeks of surgery (Table 4). Twenty-nine pregnant women had a live birth at our institution, and 23 patients delivered babies at full term. None of the HP babies who were born at our hospital had major anomalies. The risk factors of miscarriage after the treatment of HP were compared between the miscarriage (n = 9) and nonmiscarriage group (n = 55) (Table 5). There were no significant differences in terms of history of EP, method of pregnancy, type of HP, method of management, operation time, and anesthesia time. However, significant differences were observed between the 2 groups in terms of ultrasonographic features at the time HP was diagnosed (P = .039) and GA at treatment (P = .008). However, when we performed logistic regression, GA at treatment was the only independent risk factor for miscarriage in patients with HP regardless of treatment methods (OR: 0.003, 95% CI: 0.001–0.604).
Table 4.
Neonatal outcomes of heterotopic pregnancy.
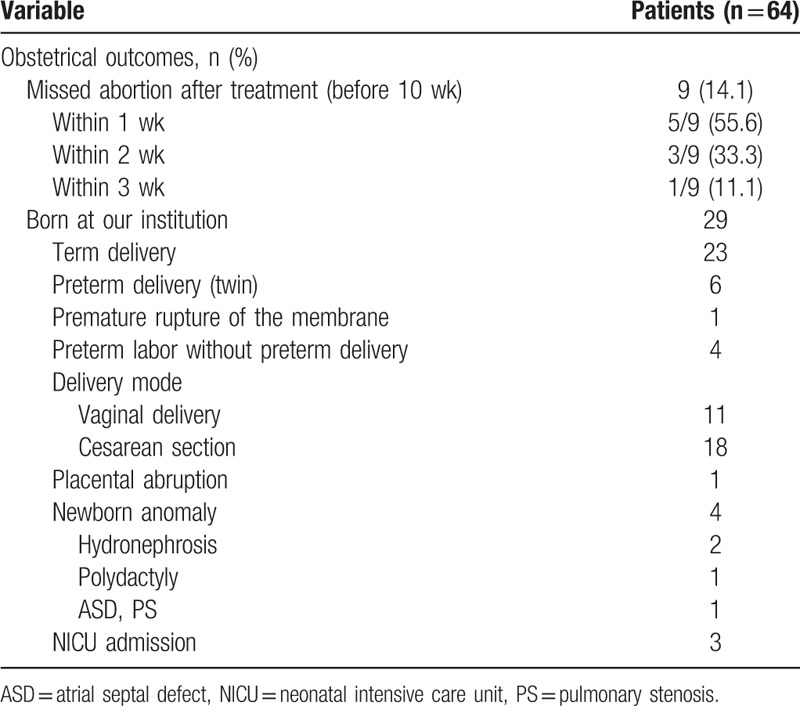
Table 5.
Risk factors of miscarriage after the treatment of patients with heterotopic pregnancy.
4. Discussion
EP is defined as an abnormally implanted pregnancy outside the intrauterine cavity, and occurs in 1% to 2% of all pregnancies. The most frequent EP site is the ampulla portion of the fallopian tube.[4] HP is the simultaneous existence of a normal IUP and EP and is a rare condition in patients with a naturally conceived pregnancy. However, with the widespread use of ART, especially in those with an embryo transfer, the incidence of HP is increasing. The EP site in those with an HP may be the fallopian tube, cornual area of the uterus, cesarean section scar, cervix, ovary, and other peritoneal spaces. Because most studies reported data on small sample sizes or case reports, the most common ectopic site of HP has not been well established, but tubal EP in those with an HP is considered the most frequent site, similar to those with EP alone.[5,6]
In our study, 62 patients conceived with ART, including 56 who conceived via IVF. In patients with a natural pregnancy, it was difficult to suspect HP until symptoms such as abdominal pain, vaginal bleeding, and rectal tenesmus occur. In addition, measurement of serum hCG is not useful for detecting HP, and ultrasonography in the early gestational stage is not helpful for diagnosing HP. However, in patients with an ART-conceived pregnancy, the diagnosis can be made and treatment can be performed earlier because there is an increased risk of HP.
Based on the results of our study, it might be difficult to suspect the presence of ovarian EP if symptoms are not present. Moreover, ovarian EP is rare, and it is not easy to distinguish ovarian pregnancy from a corpus luteum via ultrasonography, owing to echogenic similarities between them. If ovarian EP is diagnosed late, an IUP may progress to advanced gestation without loss of pregnancy, because advanced-gestation fetuses with fetal heart activity have a lower possibility of being aborted.
The risk factors for miscarriage in our study were different from those in other reports. Previous studies indicated that earlier symptoms before diagnosis, such as abdominal pain or vaginal bleeding, and later treatment of HP were independent predictors of early pregnancy loss.[3,5] A recent study found that abdominal pain before HP was diagnosed was an independent risk factor for miscarriage in those with an HP.[7] However, we found that the symptoms of abdominal pain and hemoperitoneum due to rupture of the EP site did not affect the prognosis of patients with an IUP. Additionally, our study showed that the GA at treatment was earlier in the miscarriage group than it was in the nonmiscarriage group. There were more patients with a normal pregnancy with fetal heart activity in the nonmiscarriage group than in the miscarriage group. This is possibly because a fetus with a later GA could endure more difficulties, such as operative and anesthetic circumferences, and fetuses with an advanced GA might enter the stable stage.
In our study, the EP locations did not appear to be a risk factor of miscarriage of an IUP fetus after HP was managed. A cesarean section scar HP and bilateral tubal HP without symptoms were determined via routinely performed TVS at 5.3 and 6.1 weeks of gestation, respectively. A cesarean section scar HP is relatively easy to diagnose with TVS; therefore, early diagnosis might be possible. However, 1 patient with a cesarean section scar EP spontaneously miscarried without treatment, and her IUP progressed to advanced gestation, without losing the fetus.
If the patient is hemodynamically stable and does not have abdominal pain, expectant management might be considered. We managed these patients with just one session of treatment, without further injection of medicine or surgery in any patient. Several studies reported that HP with a local injection of MTX or KCL or combined use of MTX and KCL at the EP site led to the delivery of healthy babies,[8–10] although most reports were small-sized case reports. However, the use of MTX should be avoided due to MTX-related teratogenicity. Case reports of MTX exposure after the misdiagnosis of EP have proven that MTX embryopathy can appear due to early exposure to MTX.[11]
In our study, the surgical treatments of HP were mostly laparoscopic. Compared with open laparotomy, in laparoscopy, general anesthesia and high intraabdominal carbon dioxide pressure from the pneumoperitoneum can be harmful during early pregnancy. High intraabdominal pressure can cause uterine contraction and result in fetal loss. Therefore, short operation and anesthesia times and low intraabdominal pressure during surgery have been highlighted. However, laparoscopy can provide better visualization and exposure, early return of bowel function, less postoperative pain, and early ambulation. Therefore, laparoscopic surgery takes precedence over open laparotomy in pregnant women who require surgery. Several previous studies proved that laparoscopic surgery is now as safe as open surgery during pregnancy, with no deleterious effects on either the mother or child.[7,12]
The incidences of ovarian EP and bilateral EP are very low. The incidence of ovarian EP in those with natural conception ranges from 1 in 2100 to 1 in 7000 pregnancies and accounts for 3% of all EPs.[13] Spontaneous, bilateral, tubal EP has an estimated incidence of 1 in 725 to 1 in 1580 EPs or 1 of 200,000 pregnancies.[14,15] Since pregnancy via ART increases the risk of HP, a thorough ultrasonographic examination should be performed in patients who become pregnant via ART, paying attention to the number of embryos that are transferred during IVF-conceived pregnancy. After pregnancy is confirmed using the hCG level, patients should be warned about the possibility of HP even if routinely scheduled TVS appears to be normal. A short-term ultrasonographic examination is required in patients where HP was overlooked before the EP ruptures.
Previous studies showed miscarriage rates of 6% to 33% and live birth rates of 53% to 93% after the treatment of an HP.[5] The miscarriage rate in our study was similar to that in previous reports. Furthermore, early, spontaneous abortion occurs in 10% to 25% of all pregnancies.[16] The treatment of HP in early pregnancy can be considered safe because there were no significant differences in the miscarriage rates of HP and normal pregnancies between our study and previous studies.
The limitation of this study is that it is a retrospective study with a small sample size. A randomized clinical trial on a larger scale is ideal and necessary to validate the findings of this study. In general, however, the incidence of HP is very low. Therefore, it is difficult to perform a randomized clinical trial with a large sample size.
In conclusion, the early diagnosis and treatment of HP are crucial to prevent maternal life-threatening conditions. GA at treatment was the only independent risk factor for miscarriage in patients with HP regardless of treatment methods. When patients are diagnosed with an HP, most of pregnant women have extreme anxiety. Therefore, our findings would be useful when counseling patients before treatment.
Author contributions
Data curation: Eun Duc Na, Hee Young Cho.
Methodology: Eun Duc Na, Inkyung Jung, Hyeon Chul Kim.
Writing—original draft: Eun Duc Na, Hee Young Cho.
Formal analysis: Inkyung Jung, Seok Jae Heo.
Validation: Inkyung Jung, Hee Young Cho.
Conceptualization: Dong Hee Choi, Hwang Kwon, Hyeon Chul Kim, Suk Ho Kang, Hee Young Cho.
Investigation: Dong Hee Choi, Hwang Kwon, Hyeon Chul Kim, Suk Ho Kang, Hee Young Cho.
Software: Seok Jae Heo.
Project administration: Suk Ho Kang.
Supervision: Suk Ho Kang, Hee Young Cho.
Visualization: Hee Young Cho.
Hee Young Cho: 0000-0001-7064-5056.
Footnotes
Abbreviations: ART = assisted reproductive technology, COH-TI = controlled ovarian hyperstimulation and timed intercourse, EP = ectopic pregnancy, GA = gestational age, GS = gestational sac, hCG = human chorionic gonadotropin, HP = heterotopic pregnancy, IUI = intrauterine insemination, IUP = intrauterine pregnancy, IVF = in vitro fertilization, KCL = potassium chloride, MTX = methotrexate, TVS = transvaginal ultrasonography, YS = yolk sac.
The authors have no conflicts of interest to disclose.
References
- [1].Basile F, Di Cesare C, Quagliozzi L, et al. Spontaneous heterotopic pregnancy, simultaneous ovarian, and intrauterine: a case report. Case Rep Obstet Gynecol 2012;2012:509694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Talbot K, Simpson R, Price N, et al. Heterotopic pregnancy. J Obstet Gynaecol 2011;31:7–12. [DOI] [PubMed] [Google Scholar]
- [3].Sijanovic S, Vidosavljevic D, Sijanovic I. Methotrexate in local treatment of cervical heterotopic pregnancy with successful perinatal outcome: case report. J Obstet Gynaecol Res 2011;37:1241–5. [DOI] [PubMed] [Google Scholar]
- [4].Mascarenhas MN, Flaxman SR, Boerma T, et al. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med 2012;9:e1001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Lyu J, Ye H, Wang W, et al. Diagnosis and management of heterotopic pregnancy following embryo transfer: clinical analysis of 55 cases from a single institution. Arch Gynecol Obstet 2017;296:85–92. [DOI] [PubMed] [Google Scholar]
- [6].Li JB, Kong LZ, Yang JB, et al. Management of heterotopic pregnancy: experience from 1 tertiary medical center. Medicine 2016;95:e2570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Cookingham LM, Goossen RP, Sparks AET, et al. Successful treatment algorithm for evaluation of early pregnancy after in vitro fertilization. Fertil Steril 2015;104:932.e1–7.e1. [DOI] [PubMed] [Google Scholar]
- [8].Vitner D, Lowenstein L, Deutsch M, et al. Dilation and curettage: successful treatment for a heterotopic intrauterine and a twin cervical pregnancy. Isr Med Assoc J 2011;13:115–6. [PubMed] [Google Scholar]
- [9].Yu Y, Xu W, Xie Z, et al. Management and outcome of 25 heterotopic pregnancies in Zhejiang, China. Eur J Obstet Gynecol Reprod Biol 2014;180:157–61. [DOI] [PubMed] [Google Scholar]
- [10].Hyoun SC, Obican SG, Scialli AR. Teratogen update: methotrexate. Birth Defects Res A Clin Mol Teratol 2012;94:187–207. [DOI] [PubMed] [Google Scholar]
- [11].Wilasrusmee C, Sukrat B, McEvoy M, et al. Systematic review and meta-analysis of safety of laparoscopic versus open appendicectomy for suspected appendicitis in pregnancy. Br J Surg 2012;99:1470–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Andrews J, Farrell S, Andrews J. Spontaneous bilateral tubal pregnancies: a case report. J Obstet Gynaecol Can 2008;30:51–4. [DOI] [PubMed] [Google Scholar]
- [13].Forster S, Reimer T, Rimbach S, et al. [CAMIC recommendations for surgical laparoscopy in non-obstetric indications during pregnancy]. Zentralbl Chir 2016;141:538–44. [DOI] [PubMed] [Google Scholar]
- [14].Park SH, Park MI, Choi JS, et al. Laparoscopic appendectomy performed during pregnancy by gynecological laparoscopists. Eur J Obstet Gynecol Reprod Biol 2010;148:44–8. [DOI] [PubMed] [Google Scholar]
- [15].Comstock C, Huston K, Lee W. The ultrasonographic appearance of ovarian ectopic pregnancies. Obstet Gynecol 2005;105:42–5. [DOI] [PubMed] [Google Scholar]
- [16].Wang X, Chen C, Wang L, et al. Conception, early pregnancy loss, and time to clinical pregnancy: a population-based prospective study. Fertil Steril 2003;79:577–84. [DOI] [PubMed] [Google Scholar]


