Abstract
Lateral neck radiography is often used as a screening tool in emergency departments for suspected acute epiglottitis. The qualitative radiographic signs have been mainly used. The aim of this study was to evaluate the accuracy of objective radiographic parameters to aid diagnosis of acute epiglottitis.
Patients who were diagnosed with acute epiglottitis from January 2006 to December 2016 were included in this case–control study. Control subjects with normal lateral neck radiograph findings were included at a 1:4 ratio during the same period. The clinical findings of the patients were assessed from electronic medical records and radiographs were interpreted by a board-certified radiologist and a board-certified emergency medicine physician. The widths of the 3rd cervical vertebral body, epiglottis base (EWB), epiglottis tip (EWT), aryepiglottic fold (AFW), and hypopharynx, as well as the dimensions of the retropharyngeal and retrotracheal soft tissues, were retrospectively measured. The sensitivity, specificity, and receiver operating characteristic (ROC) curves were analyzed for the measured parameters, and cutoff values were determined to predict acute epiglottitis. The predictive cutoff values of radiologic parameters were evaluated using 5-fold cross-validation.
A total 260 epiglottitis patients and 1166 controls were included in the study. In the ROC curve analysis, the EWB had an area under the ROC curve (AUROC) of 0.99 for a cutoff value of 5.02 mm (sensitivity, 96.2%; specificity, 98.2%). The EWT had an AUROC of 0.97 for a cutoff value of 4.84 mm (sensitivity, 91.2%; specificity, 97.3%). The AFW had an AUROC of 0.88 for a cutoff value of 6.59 mm (sensitivity, 86.5%; specificity, 78.8%). The 5-fold cross-validation achieved AUROCs of 0.97 for EWB, 0.94 for EWT, and 0.83 for AFW.
The objective radiographic parameters in lateral neck radiography may be useful in diagnosing acute epiglottitis. Further prospective studies may be warranted to evaluate the diagnostic performance in actual clinical practice.
Keywords: diagnosis, epiglottitis, radiography
1. Introduction
Epiglottitis is an inflammatory condition primarily of the epiglottis, vallecula, arytenoid cartilage, and aryepiglottic folds.[1–3] Acute epiglottitis is relatively rare but may progress rapidly to life-threatening airway obstruction.[4] Part of the clinical diagnosis of epiglottitis involves radiography and visualization. Direct visualization of the epiglottis using laryngoscopy remains the gold standard of diagnosis.[3] However, laryngoscopy examination requires special training and may not be readily available in emergency settings.[3] Lateral neck radiographs are low-cost and readily available and are often used as a screening tool in emergency departments for suspected acute epiglottitis.[3]
Many lateral neck radiographic studies have reported signs that were useful for diagnosing acute epiglottitis.[5–8] The findings have included the thumb sign, vallecula sign, thickened aryepiglottic fold, prevertebral soft-tissue swelling, and ballooning of the hypopharynx. However, these radiologic signs of epiglottitis are subjective. The reliability, sensitivity, and specificity of lateral neck radiography have recently been questioned. Only 79% of cases are diagnosed based on lateral neck radiographs.[9] In the case of mild or early epiglottitis, these characteristic signs may not be present. To improve sensitivity and specificity in the diagnosis of epiglottitis, several previous studies have proposed quantitative criteria such as epiglottic width instead of these subjective signs.[3,10–14] However, the generalization of the results of previous studies has been limited by small sample sizes. In addition, reported cutoff values have been in the range of 5.5 to 8 mm, which is relatively broad. Further research involving larger sample sizes may be needed to use these cutoff values in actual clinical settings. Hence, the purpose of this study was to evaluate the diagnostic performance of objective, measurable radiographic parameters and to suggest appropriate cutoff values for diagnosing acute epiglottitis in adults.
2. Methods
This retrospective study was conducted at a regional tertiary emergency center in South Korea, with an annual emergency department census of 45,000 patients. The study was approved by the Institutional Review Board of Samsung Changwon Hospital. Owing to the retrospective nature of the study, the need for informed consent was waived.
We conducted a case–control study of patients diagnosed with acute epiglottitis from January 2006 to December 2015. To enroll the case subjects, we recruited patients who were 18 years of age or older with an International Classification of Diseases 10th Revision (ICD-10) code of acute epiglottitis from the hospital database (ICD-10 diagnosis codes J05.10 and J05.11). Patients were excluded from the case subject group, if they met any of the following criteria: lack of a digitized lateral neck radiograph taken during the presenting episode, lack of diagnostic confirmation of acute epiglottitis by direct visualization or computed tomography of the neck region, and epiglottis parameters that cannot be measured using radiography. Among the patients who underwent lateral neck radiography between January 2006 and December 2015, those who were 18 years of age or older with normal radiologic readings were included as control subjects. Patients were excluded from the control group if they met any of the following criteria: past or current history of head and neck malignancy, past or current history of fracture or dislocation of the cervical spine, presence of symptoms suggesting acute epiglottitis (sore throat, fever, dysphagia, dyspnea, hoarseness, drooling), and epiglottis parameters that cannot be measured using radiography. According to the enrollment criteria, the initial recruitment rate for the case and control groups was approximately 1:4. After the initial recruitment, an emergency physician reviewed the demographic data, medical records, and radiographs of both groups and excluded the samples that were ineligible. The laryngoscopic findings of the case subjects were reviewed to identify and classify the location of major inflammation into 5 categories: inflammation of the epiglottis alone, inflammation of the aryepiglottic fold or arytenoid cartilage including the epiglottis, inflammation of the aryepiglottic fold alone, inflammation of the arytenoid cartilage alone, and inflammation of the aryepiglottic fold fused with the arytenoid cartilage.
All patients included in the study underwent routine lateral neck radiography at our institution. Radiographic views were obtained in the standing position with a 15° extension of the neck using a 70-kV and 14-mAs setting. A radiologist with 16 years of experience in radiographic interpretation and an emergency physician with 9 years of experience as a board-certified physician who were blinded to the demographic data and clinical information of the patients reviewed the radiographs on a picture-archiving and communication system (PACS; Marotech, Seoul, South Korea). The radiograph reading order was randomly assigned by a random order generator (http://www.random.org). The researchers retrospectively measured parameters including the 3rd cervical vertebral body width (C3W), epiglottic width at the base (EWB), epiglottic width at the tip (EWT), aryepiglottic fold width (AFW), hypopharynx width (HW), retropharyngeal soft tissue (RPS), and retrotracheal soft tissue (RTS) (Fig. 1). The definitions of the C3W, AFW, HW, RPS, and RTS were similar to those used in previous studies.[3,10–14] However, in our study, the epiglottic width used in previous research was redefined as the EWB, as the widest anteroposterior (AP) diameter of the epiglottis measured at the epiglottis base, which is perpendicular to a line that bisects the vallecula. The EWT was also added as a parameter to be measured in this study and was defined as the AP diameter of the epiglottis measured at a point 5 mm away from the tip of the epiglottis. The ratios of each parameter to the C3W were calculated to adjust for discrepancies caused by individual body size and radiographic magnification.[3,10] Two raters were informed of the definition of the radiographic parameters 2 weeks before the study measurements, and practiced with 30 samples randomly selected from the case and control patients. The precision of the measurements reached 0.01 mm. The measurements obtained by the 2 raters were averaged before analysis. The intra-class correlation coefficient (ICC) was analyzed to test the agreement of the measurements obtained by the 2 raters.
Figure 1.

Measurement of each parameter on lateral neck X-ray. Hypopharynx width (A, B): the width of the hypopharyngeal air column at the mid-height of the second cervical vertebral body. Epiglottic width at the tip (C, D): the anteroposterior (AP) diameter of the epiglottis at 5 mm from the tip. Epiglottic width at the base (E, F): the widest AP diameter of the epiglottis measured at or above a line drawn through the base of the epiglottis perpendicular to a line that bisects the vallecula. Retropharyngeal soft-tissue thickness (G, H): the prevertebral soft-tissue thickness at the mid-height of the 3rd cervical vertebral body. Third cervical vertebral body width (H, I): the AP diameter of the 3rd cervical vertebral body measured at the mid-height of the vertebral body. Aryepiglottic fold (J, K): the largest width of the aryepiglottic fold. Retrotracheal soft tissue thickness (L, M): the prevertebral soft-tissue thickness at the mid-height of the sixth cervical vertebral body.
To assess the accuracy of clinicians using only subjective signs when diagnosing acute epiglottitis, 100 plain films from the case and control subjects were randomly selected and reviewed by 21 emergency medicine physicians. The physicians were blinded to the results of the patients’ diagnoses and determined only whether epiglottitis was suspected on each lateral neck radiograph. Each case was reviewed using the PACS, and the radiographs used did not contain any identifying information.
2.1. Statistical analysis
Continuous variables are presented as mean and standard deviation and were compared using the Student t test. Categorical variables are presented as proportions and were compared using the Chi-squared test. The sensitivity, specificity, and receiver operating characteristic (ROC) curve were analyzed for the measured parameters and the ratio of each parameter to the C3W. We performed 5-fold cross-validation for internal validation of radiologic parameters demonstrating good or excellent performance with ROC curve analysis. After all patients were randomly partitioned into five sets, the cutoff value of each radiologic parameter for diagnosing acute epiglottitis was cross-validated. A P-value of less than .05 was considered statistically significant. Data were analyzed mainly using the Statistical Package for the Social Sciences version 24.0 (SPSS Inc, Chicago, IL, USA). MedCalc version 12.2 (MedCalc Inc, Mariakerke, Belgium) was used to produce an interactive dot diagram of the ROC curve. The comparison of areas under the ROC curve (AUROCs) was performed by the method of Hanley & McNeil where the p values are adjusted by Bonferroni correction.[15] STATA (Stata Corporation, College Station, TX, USA) was used for cross-validation.
3. Results
A total of 301 patients with a discharge diagnosis of acute epiglottitis were recruited, 41 of whom were excluded for the following reasons: 28 patients had no digitized radiographs available because only a direct laryngoscopic visualization was used to confirm the diagnosis; in 13 patients, epiglottis parameters could not be measured because the epiglottis was attached to the tongue on the radiograph. A total of 1265 potential control subjects were included, 99 of whom were excluded for the following reasons: 61 patients had at least 1 symptom suggesting epiglottitis; in 26 patients, the epiglottis parameters could not be measured because the epiglottis was attached to the tongue on the radiograph; 2 patients had a history of head and neck malignancy; 7 patients had a history of fracture of the cervical spine; 3 patients had swelling around the vallecula caused by fish bone foreign bodies identified using laryngoscopy. Finally, lateral neck radiographs of 260 case subjects and 1166 control subjects were analyzed.
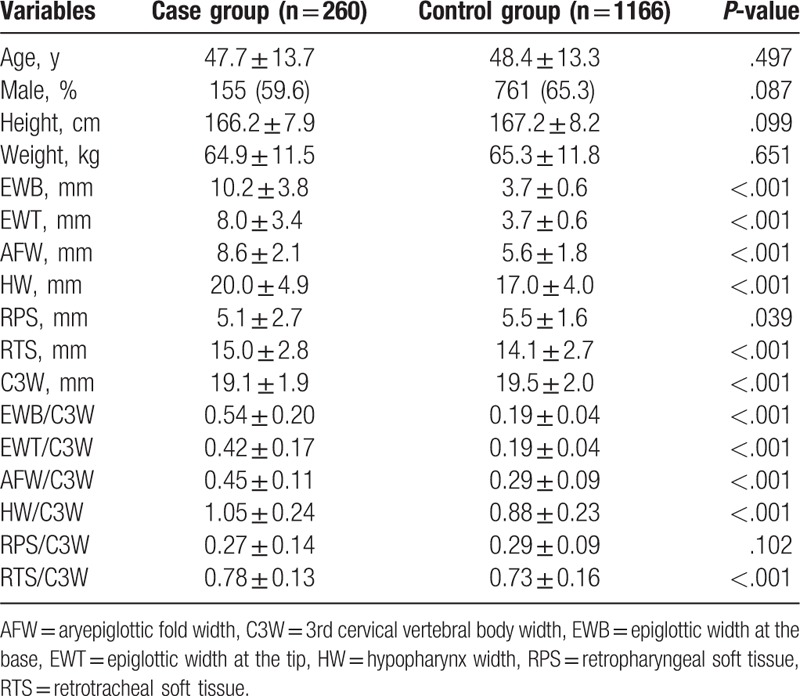
The ICCs for the EWB, EWT, AFW, HW, RPS, RTS, and C3W were 0.98, 0.97, 0.89, 0.91, 0.93, 0.94, and 0.95, respectively (P < .001). No significant differences in age, sex, weight, or height were observed between the 2 groups (Table 1). Measurements of most radiologic parameters in the case group were significantly larger than those in the control group, except RPS and RPS/C3W (Table 1).
Table 1.
Demography and radiographic parameters of the case and control groups.
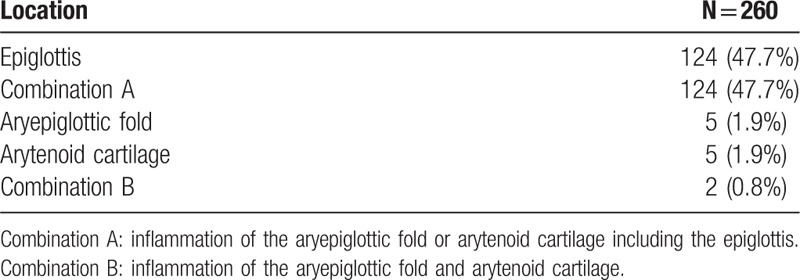
The locations of major inflammation among the supraglottic structures are summarized in Table 2. The 2 most common locations were the epiglottis alone and the aryepiglottic fold or arytenoid cartilage including the epiglottis, followed by the aryepiglottic fold or arytenoid cartilage alone, and the aryepiglottic fold and arytenoid cartilage.
Table 2.
Locations of major inflammation among the supraglottic structures.
The discriminative power of the diagnosis of epiglottitis for the overall study population, according to each parameter and the ratio of each parameter to the C3W, is shown in Figure 2 and Table 3. The EWB had an area under the ROC curve (AUROC) of 0.99 for a cutoff value of 5.02 mm (sensitivity, 96.2%; specificity, 98.2%). Interestingly, very little overlap of the distribution of EWB for the case and control subjects was observed in the interactive dot diagram in the ROC curve analysis (Fig. 3). The EWT had an AUROC of 0.97 for a cutoff value of 4.84 mm (sensitivity, 91.2%; specificity, 97.3%). The AFW had an AUROC of 0.88 for a cutoff value of 6.59 mm (sensitivity, 86.5%; specificity, 78.8%). The HW had an AUROC of 0.66 for a cutoff value of 21.56 mm (sensitivity, 40.8%; specificity, 88.1%). The RPS had an AUROC of 0.66 for a cutoff value of 4.79 mm (sensitivity, 63.5%; specificity, 67.2%). The RTS had an AUROC of 0.58 for a cutoff value of 13.06 mm (sensitivity, 75.8%; specificity, 40.4%). A comparison of AUROC values showed that, when compared with the EWT and AFW, the EWB had significantly greater discriminatory power (P = .001 and P < .001, respectively).
Figure 2.
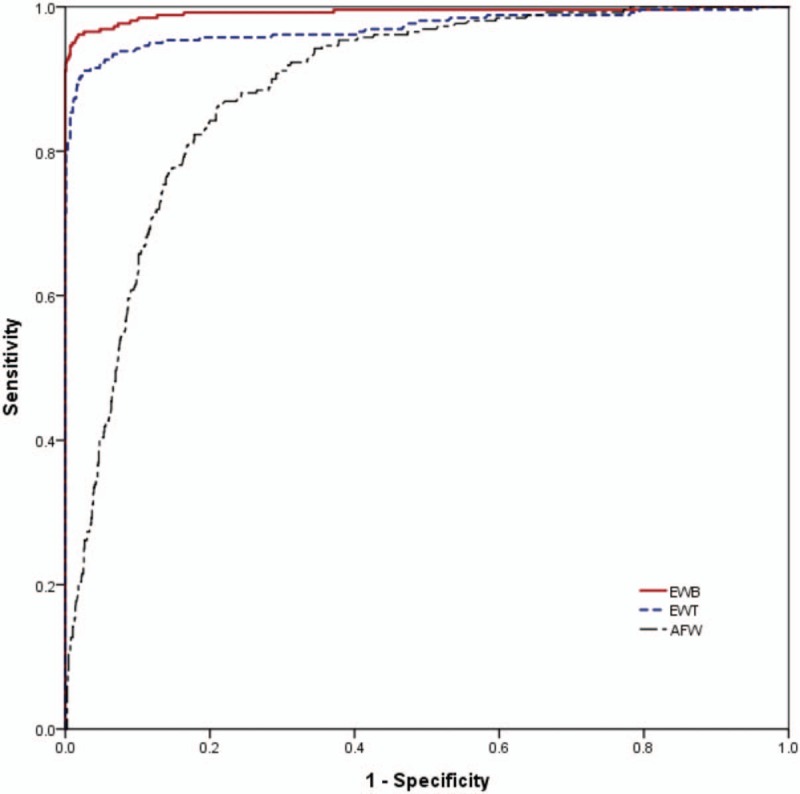
Receiver operating characteristic curves for various radiographic parameters. AFW = aryepiglottic fold width, EWB = epiglottic width at the base, EWT = epiglottic width at the tip.
Table 3.
Diagnostic characteristics of the radiographic parameters and the ratios with reference to the 3rd cervical vertebral body width.
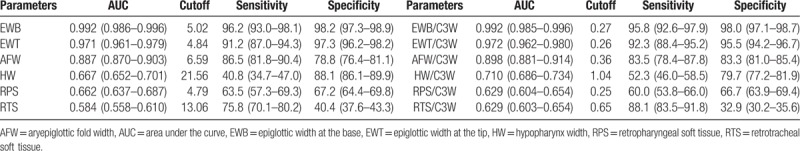
Figure 3.
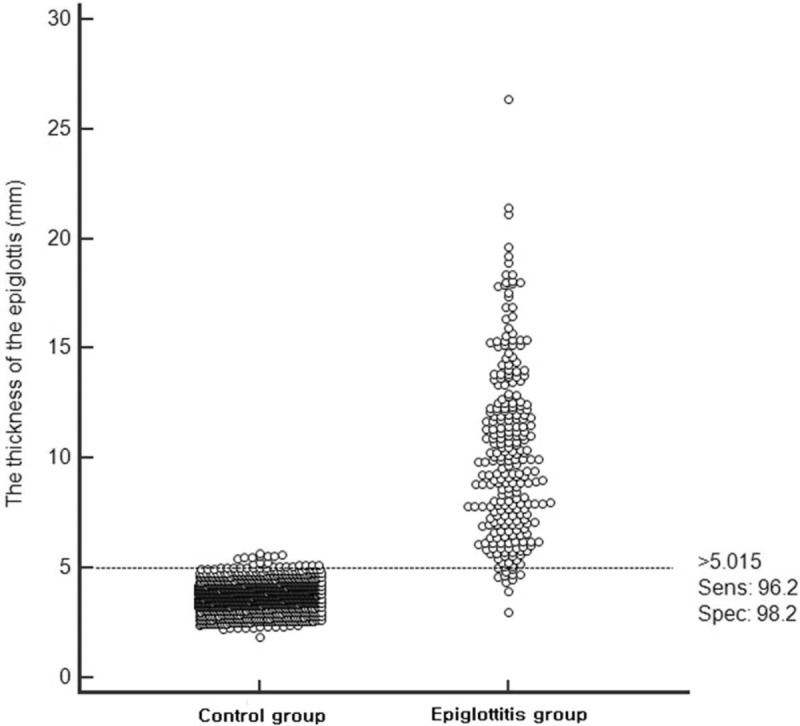
Interactive dot diagram of the receiver operating characteristic curve for correlation between the epiglottis width at the base and the diagnosis of epiglottitis. The horizontal dashed line indicates the cutoff point with the smallest overlap of the 2 groups. The cutoff point of the thickness of the epiglottis base was 5.015 mm. The corresponding test characteristics of sensitivity and specificity were 96.2% and 98.2%, respectively.
The ratios of EWB, EWT, and AFW to the C3W (EWB/C3W, EWT/C3W, and AFW/C3W) were also accurate in diagnosing acute epiglottitis. The AUROC values of EWB/C3W and EWT/C3W were above 0.90, and that of AFW/C3W was also close to 0.90. However, no statistically significant differences were observed among the AUROC values when comparing individual parameters with ratios of each parameter to the C3W, except for AFW (EWB vs EWB/C3W, EWT vs EWT/C3W, and AFW vs AFW/C3W, P = .56, P = .75, and P = .01, respectively).
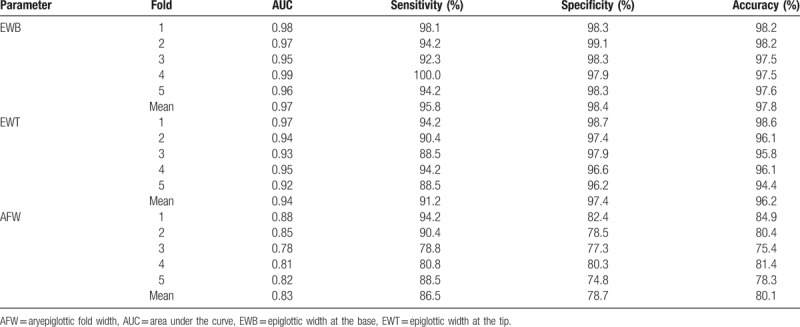
The results of cross-validation of the radiologic parameters are shown in Table 4. Only a small reduction was observed in each accuracy measurement in all of the cross-validated parameters. Five-fold cross-validation using predictive cutoff values achieved AUROCs of 0.97 for EWB (sensitivity, 95.8%; specificity, 98.4%), 0.94 for EWT (sensitivity, 91.2%; specificity, 97.4%), and 0.83 for AFW (sensitivity, 86.5%; specificity, 78.7%).
Table 4.
Prediction performance of the radiographic parameters using 5-fold cross-validation.
The emergency physicians attained a median accuracy of 67% (range, 50–90%) in diagnosing acute epiglottitis solely on the basis of plain films, without the assistance of the objective parameters.
4. Discussion
In this study, we assessed the performance of several objective radiographic parameters in the diagnosis of epiglottitis. Among these objective parameters, the diagnostic accuracy of EWB, EWT, AFW, EWB/C3W, EWT/C3W, and AFW/C3W was excellent. Conversely, the accuracy of diagnosing epiglottitis using lateral neck radiographs with subjective signs alone was low.
Several previous studies have used objective parameters in the diagnosis of acute epiglottitis.[3,10–13] Most studies have found the epiglottic width (EW), the ratio of the EW to the 3rd or 4th cervical vertebral body width, and AFW to be objective parameters for aiding in the diagnosis of acute epiglottitis.[3] However, the results of these studies may be limited to actual clinical applications because of their small sample sizes; in most of the studies, the number of samples in the disease group was <100. Our study, with 260 cases, is the largest to date and confirms previously published findings.
Previous studies have reported a cutoff value of EW for diagnosis in acute epiglottitis ranging from 5.5 to 8 mm, which is somewhat broad.[3] The cutoff of EWB in this study was approximately 5 mm, lower than the lowest reported cutoff value of 5.5 mm. Even at cutoff values lower than those reported, the diagnostic accuracy of the EWB values proposed in our study was as high as that in previous studies. Interestingly, very little overlap was observed in the distribution of EWB values between the case and control patients in the present study. In the case group, the number of patients with an EWB value of <5.69 mm, which was the cutoff value for diagnosing epiglottitis with 100% specificity, was only 23 (8.8%). In this study, the diagnostic performance of the measurable objective parameter was excellent. We also investigated the diagnosis of epiglottitis using only subjective signs, with no objective parameters, and obtained an accuracy of 67%. Ng et al reported that the frequencies of the thumb and vallecula signs on lateral neck radiographs were 77% and 1.4%, respectively.[16] Lee et al also reported a similar frequency for the thumb sign (65.9%), but that of the vallecular sign was documented at 53.9%.[14] Based on false-negative results of qualitative signs in neck radiography, they indicated that the diagnostic strategy for acute epiglottitis using neck radiography needs to be modified.[14] Given the relatively low accuracy of using only subjective signs and the high sensitivity and specificity achieved using the objective parameters in this study for lateral neck radiographs, the latter seem to play a screening role in the diagnosis of acute epiglottitis before a confirmatory test such as neck computed tomography or laryngoscopy.
In our study, we identified that the EWB/C3W ratio as well as the EWB, as in previous studies, is an accurate parameter in the diagnosis of acute epiglottitis. However, the increase in accuracy when applying the ratio was not as great when applied to the EW alone. The EW alone may be sufficient to diagnose acute epiglottitis.
In this study, we measured the EW at 2 sites, whereas all previous studies have measured the EW only at the base level. Our study revealed that measuring the EW at the base level has a slightly higher discriminative power than measuring it at the level adjacent to the tip. A possible explanation for this finding is that, histologically, the base of the epiglottis is thicker than the tip.[17] Additionally, in laryngoscopic examinations of epiglottitis patients, the tip of the epiglottis is rarely locally inflamed; in most cases, inflammation progresses across multiple anatomic structures of the supraglottis. We speculate that the discriminative power of the EWB is probably the highest because most of the structural parts of the supraglottis are connected to the base of the epiglottis.
Swelling in acute epiglottitis may also occur at the aryepiglottic fold. Wong et al and Lee et al reported that the AFW demonstrates strong performance in the diagnosis of epiglottitis.[3,14] The discriminative power of the AFW in this study was as accurate as that of the EWB. In the case of focal inflammation of the aryepiglottic fold or arytenoid cartilage rather than the epiglottis in the supraglottic structure, the thickness of the EWB may be close to normal. In such patients, the AFW parameter may be helpful in screening epiglottitis. In our study, 11 out of 23 patients with EWB values <5.69 mm had inflammation localized to the aryepiglottic fold or arytenoid cartilage rather than the epiglottis. However, caution may be required in measurement and interpretation because the ICC is lower than that of the EW.[3]
This study had several limitations. First, this was a retrospective study conducted in a single center. Second, selection bias may have occurred because X-ray and confirmative investigation were not performed for all patients with suspected epiglottitis. A prospective study may be necessary to solve this problem. Third, although we used the same protocol for all lateral neck radiographs, the soft-tissue structures may have varied in size depending on the respiration and radiographic technique. Fourth, our study was limited to examining a South Korean population. Data were also unavailable comparison of EW in other demographic groups. Therefore, the results cannot be generalized. Fifth, analysis was based on cohort data generated during the study period without matching of control patients to case patients for constitutional confounders. The factors required for matching were not known precisely and the correlation between EWB and age, weight, and height was extremely weak in the control group of this study (correlation coefficients: 0.04, 0.06, and 0.05, respectively). In addition, the difference in EWB between male and female patients was only 0.1 mm (3.77 mm vs 3.66 mm, respectively, P = .003). We believe that matching for these factors will produce little change in the outcome.
5. Conclusion
Measurement of objective parameters including the EW on lateral neck radiographs for acute epiglottitis diagnosis is highly accurate and may be useful for screening diagnosis. Additional studies may be needed to determine the applicability to actual clinical practice.
Acknowledgment
The authors thank Mi Hyeon Jin for providing statistical advice for this study.
Author contributions
Conceptualization: Kyung Hee Kim, Yong Hwan Kim.
Data curation: Kyung Hee Kim, Jun Ho Lee, Dong Woo Lee, Seung Yong Cha.
Formal analysis: Jun Ho Lee, Yun Gyu Song.
Investigation: Dong Woo Lee, Seung Yong Cha, Yun Gyu Song.
Methodology: Seong Youn Hwang.
Supervision: Yong Hwan Kim.
Validation: Yong Hwan Kim.
Writing – original draft: Jun Ho Lee.
Writing – review & editing: Yong Hwan Kim, Seong Youn Hwang.
Footnotes
Abbreviations: AFW = aryepiglottic fold width, AP = anteroposterior, AUROC = area under the receiver operating characteristic curve, C3W = 3rd cervical vertebral body width, EW = epiglottic width, EWB = epiglottic width at the base, EWT = epiglottic width at the tip, HW = hypopharynx width, ICC = intra-class correlation coefficient, ROC = receiver operating characteristic, RPS = retropharyngeal soft tissue, RTS = retrotracheal soft tissue.
The authors have no conflicts of interest to disclose.
References
- [1].Woo JK, van Hasselt CA. Acute epiglottitis: a misnomer. Otolaryngol Head Neck Surg 1994;111:538–9. [DOI] [PubMed] [Google Scholar]
- [2].Nizam R, Lerakis S, Sherman CB, et al. Acute epiglottitis in a nonagenarian. J Am Geriatr Soc 1996;44:613. [DOI] [PubMed] [Google Scholar]
- [3].Wong YK, Pan NY, Chu CY, et al. Diagnosing epiglottitis with radiographs: can we be more objective? Hong Kong J Emerg Med 2016;23:168–75. [Google Scholar]
- [4].Shapiro J, Eavey RD, Baker AS. Adult supraglottitis: a prospective analysis. JAMA 1988;259:563–7. [PubMed] [Google Scholar]
- [5].Hodge KM, Ganzel TM. Diagnostic and therapeutic efficiency in croup and epiglottitis. Laryngoscope 1987;97:621–5. [DOI] [PubMed] [Google Scholar]
- [6].Swischuk LE. Emergency Radiology of the Acutely Ill or Injured Child. 2nd edBaltimore: Williams and Wilkins; 1986. [Google Scholar]
- [7].Podgore JK, Bass JW. The “thumb sign” and “little finger sign” in acute epiglottitis. J Pediatr 1976;88:154–5. [DOI] [PubMed] [Google Scholar]
- [8].Schabel SI, Katzberg RW, Burgener FA. Acute inflammation of epiglottitis and supraglottic structures in adults. Radiology 1977;122:601–4. [DOI] [PubMed] [Google Scholar]
- [9].Mayo-Smith MF, Hirsch PJ, Wodzinski SF, et al. Acute epiglottitis in adults: an eight year experience in Rhode Island. N Engl J Med 1986;314:1133–9. [DOI] [PubMed] [Google Scholar]
- [10].Rothrock SG, Pignatiello GA, Howard RM. Radiologic diagnosis of epiglottitis: objective criteria for all ages. Ann Emerg Med 1990;19:978–82. [DOI] [PubMed] [Google Scholar]
- [11].Schumaker HM, Doris PE, Birnbaum G. Radiographic parameters in adult epiglottitis. Ann Emerg Med 1984;13:588–90. [DOI] [PubMed] [Google Scholar]
- [12].Nemzek WR, Katzberg RW, Vanslyke MA, et al. A Reappraisal of the radiologic findings of acute inflammation of the epiglottis and supraglottic structures in adults. Am J Neuroradiol 1995;16:495–502. [PMC free article] [PubMed] [Google Scholar]
- [13].Yong MG, Choo MJ, Yum CS, et al. Radiologic laryngeal parameters in acute supraglottitis in Korean adults. Yonsei Med J 2001;42:367–70. [DOI] [PubMed] [Google Scholar]
- [14].Lee SH, Yun SJ, Kim DH, et al. Do we need a change in ED diagnostic strategy for adult acute epiglottitis? Am J Emerg Med 2017;35:1519–24. [DOI] [PubMed] [Google Scholar]
- [15].Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 1983;148:839–43. [DOI] [PubMed] [Google Scholar]
- [16].Ng HL, Sin LM, Li MF, et al. Acute epiglottitis in adults: a retrospective review of 106 patients in Hong Kong. Emerg Med J 2008;25:253–5. [DOI] [PubMed] [Google Scholar]
- [17].Kano M, Shimizu Y, Okayama K, et al. A morphometric study of age-related changes in adult human epiglottis using quantitative digital analysis of cartilage calcification. Cells Tissues Organs 2005;180:126–37. [DOI] [PubMed] [Google Scholar]


