Abstract
Despite the availability of an efficient vaccine, Yellow fever (YF), a viral disease transmitted by mosquitoes, is still a threat. In Brazil, the yellow fever virus (YFV) has been restricted to a jungle cycle for more than 70 years. However, YFV has recently invaded populated cities in the Southeast such as Rio de Janeiro where the opportunistic mosquito Aedes albopictus is well established. Using in vivo passages of YFV in Ae. albopictus, we have selected viral strains presenting substitutions in NS1 gene. We did 10 passages of YFV-74018 on two distinct Ae. albopictus populations: (i) Manaus collected from a YFV-endemic area in Amazonia and (ii) PNMNI from a YFV-free area in the state of Rio de Janeiro. Full viral genomes were deep sequenced at each passage. We obtained two YFV strains presenting a non-synonymous substitution in the NS1 gene. Interestingly, they intervened at two different positions in NS1 gene according to the mosquito population: I2772T in Ae. albopictus Manaus and S3303N in Ae. albopictus PNMNI. Both substitutions reached fixation at the passage 10. Our data suggest that YFV has the potential for adaption to Ae. albopictus thereby posing a threat to most cities in South America where this mosquito is present.
Introduction
In early January 2018, a mass immunization campaign was implemented to prevent the arrival and re-urbanization of Yellow fever (YF) in the populated cities of Rio de Janeiro and São Paulo states in Southeastern Brazil, which were declared free of YF for more than 70 years until 20171 (http://portalms.saude.gov.br/noticias/agencia-saude/42655-febre-amarela-ministerio-da-saude-atualiza-casos-no-pais). According to Brazil’s Ministry of Health, between July 2017 and February 2018, 723 human cases were confirmed in the country, of which 237 resulted in death (http://portalms.saude.gov.br/noticias/agencia-saude/42655-febre-amarela-ministerio-da-saude-atualiza-casos-no-pais). A unique molecular signature was detected in the genome of YFV strains circulating in the current outbreak2,3.
Yellow fever virus (YFV), an arbovirus of the Flavivirus genus and the Flaviviridae family, causes a disease endemic to tropical regions of Africa and South America. It is a single-stranded, positive sense RNA virus with a genome of approximately 11 kb. Seven genotypes are described: 5 in Africa (2 in West Africa (WAI and WAII) and 3 in East/Central Africa (EA, ECA, and Angola)) and 2 in South America (SAI and SAII)4. YFV strains circulating in the Americas derived from the West African genotype and most isolates from Brazil mainly belong to the South American genotype I5. In spite of the availability of effective vaccines, YF remains an important public health problem in Africa and South America, with an annual incidence of around 200,000 cases and 30,000 deaths (http://www.who.int/emergencies/yellow-fever/en/); 90% of them occur in Africa and fatality rates often exceed 20% corresponding to severe forms characterized clinically by liver and kidney failure. In Africa, YFV circulates within three distinct cycles: (i) a jungle cycle where YFV is transmitted between non-human primates by canopy-dwelling mosquitoes such as Aedes africanus, (ii) an intermediate or savannah cycle involving several zoophilic mosquitoes, and (iii) an urban cycle where YFV is transmitted between humans by the domestic and human-biting mosquito Aedes aegypti. In the Americas, YFV only persists today in a jungle cycle between non-human primates and sylvatic mosquitoes. After its introduction following the slave trade, 300–400 years ago, YFV caused devastating outbreaks in American harbors and succeeded in establishing a sylvatic enzootic cycle within the Amazon, Araguaia, and Orinoco river basins6,7. The last documented Aedes aegypti-vectored epidemic occurred in 1928 and 1929 in the city of Rio de Janeiro, when 738 cases and 478 deaths were reported respectively6. Then, the Pan-American eradication program of Ae. aegypti led to an elimination of urban YF8. Brazil was certified free of Ae. aegypti in 19579. Today, the jungle YFV cycle is still very active in Brazil, and it generates outbreaks every 6–10 years in the Southern, Southeast and Central-West regions, and every 14 years in Amazonia10. Humans are infected by the bite of forest canopy-dwelling mosquitoes of the genera Haemagogus (primary vectors; H. janthinomys, H. leucocelaenus and H. albomaculatus) and Sabethes (secondary vectors; S. chloropteros)3,11,12. However, with the increase of trade and travels with YF-endemic regions, imported cases are repeatedly reported outside YF historical regions; in March 2016, 11 Chinese workers returning from Angola developed disease symptoms13 in cities where competent Aedes mosquitoes were present. Thus, Ae. aegypti and Aedes albopictus may facilitate urban resurgence of YF in Aedes-infested regions of America14, Europe15 and Africa16.
In late 2016, a severe YFV epidemic was declared in southeastern Brazil, in a region highly infested by Ae. aegypti and Ae. albopictus2,17. Ae. albopictus was first detected in southeastern Brazil in 198618. This opportunistic species is able to colonize distinct habitats acting as a possible link between the jungle cycle and the urban cycle19,20. Despite being susceptible to infection with YFV in laboratory conditions, infected Ae. albopictus have never been found in natural settings17,19. However, it is coincidently more densely distributed in the Southeast region where the YFV is actively transmitted21 (http://portalarquivos.saude.gov.br/images/pdf/2017/junho/02/COES-FEBRE-AMARELA–INFORME-43–Atualiza----o-em-31maio2017.pdf), enhancing significantly the chances of contacts between this mosquito and the virus. We hypothesize that YFV can be experimentally selected for a potential transmission by Ae. albopictus. We passaged an YFV isolate (SAI lineage 1D, isolated in 2001) on two distinct populations of Ae. albopictus, collected from a YFV-endemic area (Manaus) and a YFV-free area (Rio de Janeiro). Heads of 30 mosquitoes (containing disseminated virus from the midgut) were pooled at late days post-infection and inoculated for amplification on Ae. albopictus C6/36 cells. Then newly produced virions were harvested and used for the next mosquito oral infection. After five rounds of cycling on Ae. albopictus, virus was detected in mosquito saliva ready to be transmitted by bite. After five additional passages using virus collected from saliva, resulting viral strains were examined to identify genetic changes in the viral genome.
Results
YFV is excreted in mosquito saliva after 4 passages in Ae. albopictus
After a first blood meal at a titer of 106.5 FFU/mL, 30 mosquitoes were examined at 21 days post-infection (dpi) and no viral particles were detected in any mosquito saliva. Then mosquito heads which most likely contain virus that has disseminated from the midgut into the hemocele, were ground and amplified once on C6/36 cells. Passages 1 to 4 were performed as described previously (Fig. 1A); except P2, viral titers obtained after incubation of mosquito head homogenates on C6/36 cells were around 107 FFU/mL. The virus became detectable in mosquito saliva from P5 (Fig. 1B). Then, next passages (P6-S to P10-S) were performed using virus produced from saliva pooled from 30 mosquitoes. Viral titers in saliva remained high, fluctuating from 108–8.3 FFU/mL (P6) to 108.1-8.2 FFU/mL (P10) (Fig. 1B).
Figure 1.
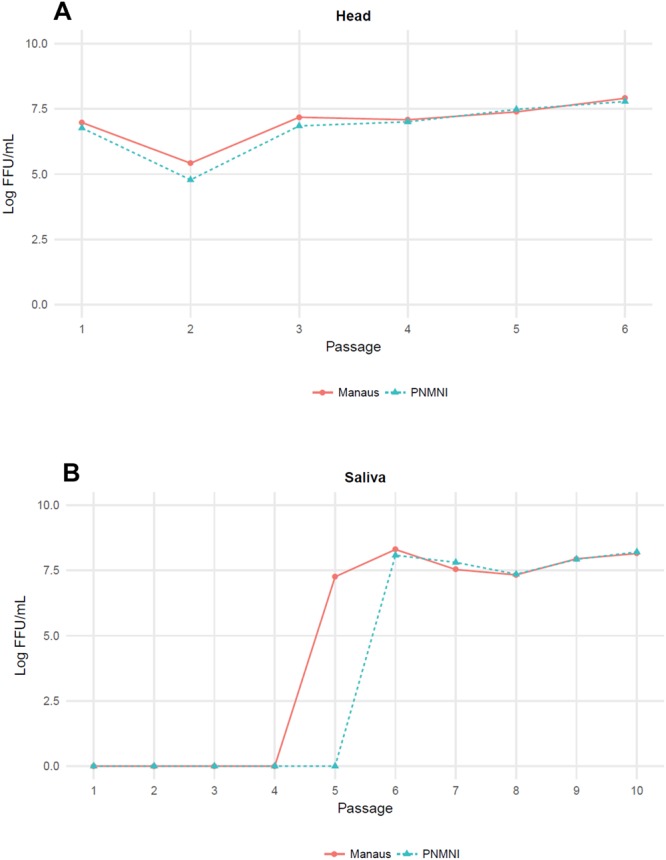
Viral titers obtained at each passage of YFV on Ae. albopictus mosquitoes (A) using virus collected from head and (B) from saliva. Mosquitoes were orally infected with YFV-74018. After 21 days, mosquitoes were processed as follows: (i) heads were collected and ground, and (ii) mosquito saliva were pooled. Head and saliva homogenates were incubated on Ae. albopictus C6/36 cells for 8 days. Collected supernatants were used to initiate the next passage. 30 mosquitoes were used at each passage.
Experimental selection of YFV transmitted by Ae. albopictus
To test whether YFV can become adapted for a potential transmission by Ae. albopictus, YFV-74018 was submitted to 10 passages in two populations of Ae. albopictus collected from two distinct regions: (i) Manaus in a YFV-endemic area and (ii) PNMNI in a YFV-free area of Rio de Janeiro (Fig. 2). Additionally, the virus was passaged 10 times in duplicate in Ae. albopictus C6/36 cells as a cell culture control. Full viral genomes were examined by deep sequencing at each passage (1–10) and for passages 0 (parental strain), and 10 for the C6/36 cells control.
Figure 2.
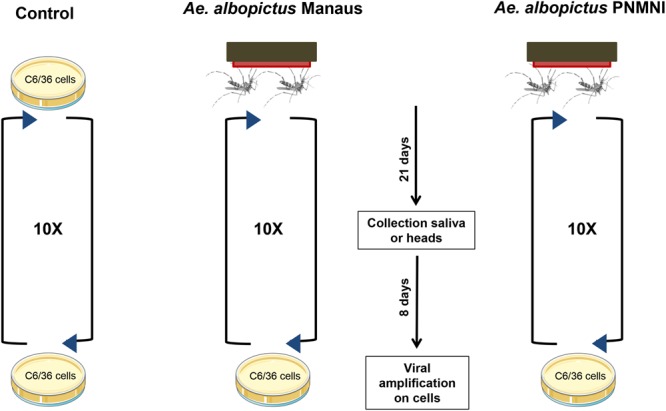
Experimental design to enhance YFV transmission by Ae. albopictus. The YFV-74018 was passaged 10 times on two populations of Ae. albopictus: (i) Manaus collected in a YFV-endemic area in Amazonia, and (ii) PNMNI collected from Rio de Janeiro, a YFV-free area. Each passage includes: the oral infection of mosquitoes with YFV, collection of mosquito saliva at day 21 post-infection, viral amplification on Ae. albopictus derived C6/36 cell culture, and initiation of the next passage using the viral suspension obtained. Control isolates were serially passaged 10 times on C6/36 cells.
The YFV-74018 yielded a mean sequencing depth of 424X covering 97.3% of the reference genome at >100X. All passages had a mean coverage between 352X and 494X, paving between 85.6 and 98.6% of the reference genome at >100X. When YFV-74018 was serially passaged on the C6/36 cells control, no major changes in single nucleotide variants (SNV) frequencies were detected. Contrariwise, consensus level variants were detected when YFV-74018 was passaged in Ae. albopictus mosquitoes, Manaus (Fig. 3A) and PNMNI (Fig. 3B). In Manaus mosquitoes, a total of 23 consensus level variants were detected from P1 to P10-S: 22 from P1 to P6 when using mosquito head homogenates as source for the next passage (head-derived) and 16 variants from P6-S to P10-S when pools of mosquito saliva were used for passages (saliva-derived) (Fig. 3A). Sixteen among 23 were located in non-structural genes (NS1, NS2A, NS3, NS4B and NS5). A group of 10 consensus level variants (positions 1376, 2044, 3832, 4810, 4816, 5445, 5509, 5602, 5605, and 7597) were present in all passages (head- or saliva-derived). A group of 6 consensus level variants were specific to head-derived passages (positions 259, 709, 2998, 6023, 6113, and 10011) and one to saliva-derived passages (position 2772). Interestingly, this last consensus level variant (position 2772) was first detected at P8-S and become fixed at P10-S; it is located in the NS1 gene (Fig. 3A).
Figure 3.
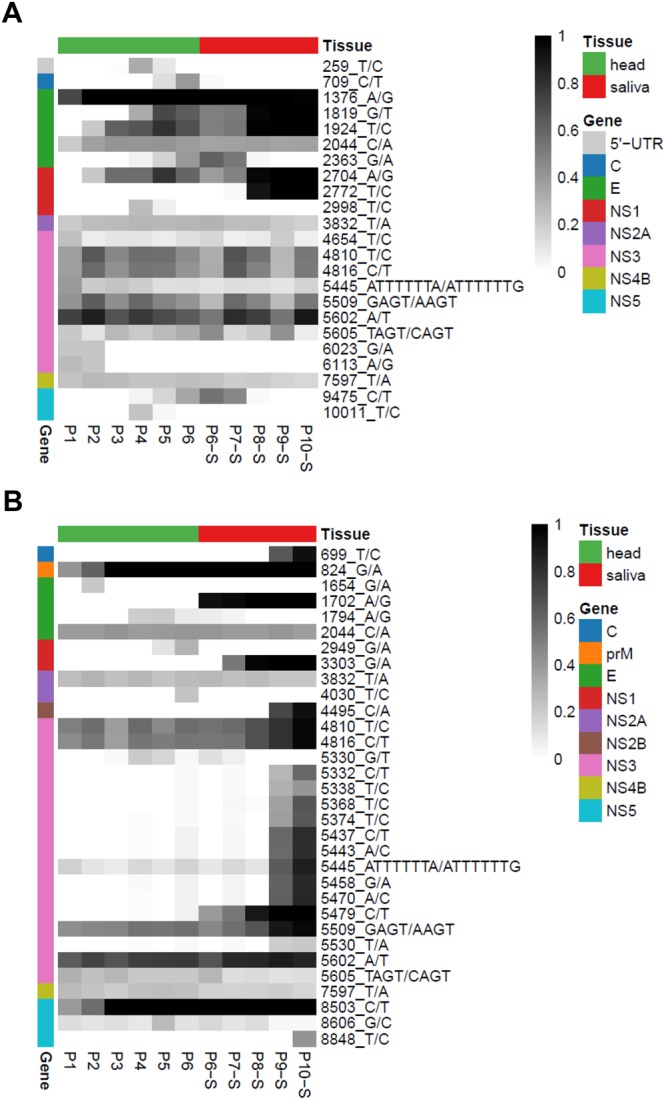
Heatmap indicating variant frequency differences between the reference genome YFV-74018 and isolates selected after passages on Ae. albopictus Manaus (A) and PNMNI (B). All 10 passages were deep sequenced: P1 to P5 were performed using homogenates of mosquito heads, and P6-S to P10-S with mosquito saliva. The intensity of black corresponds to the variant frequency. Only variants for which the frequency is above 20% are shown.
In PNMNI mosquitoes, a total of 32 consensus level variants were detected from P0 to P10-S: 26 from P1 to P6 and 29 variants from P6-S to P10-S (Fig. 3B). Twenty-six among 32 were located in non-structural genes (NS1, NS2A, NS2B, NS3, NS4B and NS5). A group of 11 consensus level variants (positions 824, 2044, 3832, 4810, 4816, 5509, 5602, 5605, 7597, 8503, and 8606) were present in all passages (head- or saliva-derived). Three consensus level variants were specific to head-derived passages (positions 1654, 2949, and 4030) and 6 to saliva-derived passages (positions 699, 1702, 3303, 4495, 5530, and 8848). Two consensus level variants (positions 1702 and 3303) were first detected in saliva-derived passages and became fixed at P10-S; the position 1702 was located in E gene and 3303 in NS1 gene (Fig. 3B).
Emergence of YFV variants in mosquito saliva
When focusing on the viral populations present in mosquito saliva from P6-S (as in previous passages, no virus was found in saliva), we detected three consensus level variants: A1702G, T2772C, and G3303A, reaching the 100% fixation at P10-S.
In Ae. albopictus Manaus, one variant with T2772C in NS1 gene detected from P8-S corresponded to a non-synonymous substitution from isoleucine to threonine. It started to be detected at P7-S (2.5%) and increased rapidly to reach fixation in three passages at P10-S (Fig. 4). In Ae. albopictus PNMNI, two variants were detected: A1702G from P6-S and G3303A from P7-S (Fig. 5). The A1702G change in E gene led to synonymous substitution (lysine), reached 80% of frequency from P6-S and became fixed at P10-S (frequency = 100%) (Fig. 5A). The G3303A change in NS1 gene induced a non-synonymous substitution from serine to asparagine and reached 100% from P8-S (Fig. 5B). These results indicate that YFV-74018 can accumulate mutations that facilitate virus transmission after passages on Ae. albopictus. However, passaging on Manaus or PNMNI did not select the same substitution.
Figure 4.

Frequency of the T2772C variant detected after the passage P7-S in Ae. albopictus Manaus. This substitution corresponds to a non-synonymous change from isoleucine to threonine in NS1 gene.
Figure 5.

Frequencies of the K1702K and S3303N variants detected after the passages P6-S and P7-S respectively in Ae. albopictus PNMNI. Only the substitution S3303N corresponds to a non-synonymous change from serine to asparagine in NS1 gene.
Discussion
Here we describe YFV strains selected after 10 passages on Ae. albopictus mosquitoes to mimic repeated interactions of the virus with an invasive mosquito previously described as a poor YFV vector. Against all expectations, YFV has been detected in field-collected Ae. albopictus in Southeastern Brazil in 2017 (http://www.iec.gov.br/portal/descoberta/). YFV variants selected after 10 passages differed according to the mosquito population: Manaus mosquitoes selected one variant T2772C inducing a non-synonymous change in NS1 while PNMNI selected two variants, A1702G leading to a synonymous substitution in E gene and G3303A to a non-synonymous substitution in NS1 gene.
Ae. albopictus has not been found infected with YFV in South America until recently17. Alarmingly, YFV was detected in field-collected Ae. albopictus in Southeastern Brazil in 2017 (http://www.iec.gov.br/portal/descoberta/). This mosquito originally from Southeast Asia22, was firstly found in Brazil in the state of Rio de Janeiro in 198618 and in Manaus, state of Amazonas, in 200223. It colonizes a wide range of habitats from peri-urban sites to forested environments and thus comes into close contacts with the YFV jungle cycle where the virus persists despite the mass Pan-American program of YF control during the first half of the 20th century24. Ae. albopictus from Manaus are likely genetically different from Ae. albopictus from Rio de Janeiro owing to differences on date and sources of introduction25 suggesting that both Ae. albopictus populations behave as different filters for selecting viral variants26.
A high number of consensus level variants were detected from P1 to P10-S: 32 in PNMNI and 23 in Manaus. Genetic characteristics of viruses passaged on mosquitoes can be described using mean of nonsynonymous to synonymous nucleotide substitutions (dN/dS) per site, codon usage bias and frequencies of CG. dN/dS (0.45–0.67; Supplementary Table 1) were 10–15 times higher than values obtained from field-isolated YFV strains (0.04327; <0.25). It suggests that our experimental design by forcing adaptation of YFV to Ae. albopictus produced a high purifying selection pressure generating a vast majority of synonymous mutations. In addition, only slight variations of codon usage bias were detected with values close to 53 suggesting a random codon usage for each amino acid (Supplementary Table 2). Moreover, the number of CG dinucleotides between passage 1 and passage 10 was slightly different for Ae. albopictus PNMNI and comparable for Ae. albopictus Manaus suggesting a low rate of evolution without likely any phenotypic effects (Supplementary Table 3).
Interestingly, beside variants present all along the 10 passages, 7 were detected only in mosquito saliva from passage 6: one in Ae. albopictus Manaus and 6 in Ae. albopictus PNMNI. Among them, three reached fixation at passage 10: I2772T in Ae. albopictus Manaus and two others in Ae. albopictus PNMNI (K1702K and S3303N). The synonymous 1702 substitution in E gene would not cause any significant change. On the other hand, the two other substitutions I2772T and S3303N are located in the NS1 gene. Genetic characteristics of viruses passaged on Ae. albopictus can be described using codon usage bias and frequencies of CG. NS1 is a highly conserved non-structural protein which has been described under different forms including a secreted hexamer protein. NS1 has been incriminated in eliciting the immune response28, activating the TLRs and inhibiting the complement system29,30. Disease severity and increased viremia are likely correlated to a high concentration of NS131. Mutations in the NS1 gene may modify its ability to trigger immune responses and avoid being the target of antivirals. The detection of these substitutions in experimental conditions with an increase of virus titers in Ae. albopictus saliva should alert us about the potential of YFV to emerge from a sylvatic cycle to reach peri-urban areas where this mosquito is well established. Collectively, this may facilitate the establishment of urban YF cycles in countries where Ae. albopictus is present.
Methods
Ethics Statements
The Institut Pasteur animal facility has received accreditation from the French Ministry of Agriculture to perform experiments on live animals in compliance with the French and European regulations on care and protection of laboratory animals. This study was approved by the Institutional Animal Care and Use Committee (IACUC) at the Institut Pasteur. Mosquito collections in Brazil were approved by local environmental authorities (PNMNI license 001/14–15; SISBIO-MMA licenses 37362-2 and 012/2016). No specific permits were required for performing mosquito collections in Brazil. This study did not involve endangered or protected species.
Viruses
Mosquitoes were orally infected with one YFV isolate belonging to the SAI genotype, isolated from a human fatal case in 2001; it corresponds to the lineage 1D FIOCRUZ 74018/MG/01 (YFV-74018)32. The isolate has been passaged four times on Ae. albopictus C6/36 cells and viral stocks were stored at −80 °C until use for mosquito challenges.
Mosquitoes
Two populations of Ae. albopictus were originated from a YFV-endemic area in the Amazon (Manaus) and a YFV-free area in the state of Rio de Janeiro (Parque Nacional Municipal de Nova Iguaçu-PNMNI)17. Generation F1 for Manaus and PNMNI respectively were challenged with YFV-74018. Eggs were immerged in dechlorinated tap water and larvae were fed with yeast tablets renewed every 2–3 days. Pupae were collected manually and grouped in bowls placed in cages. Adults were fed ad libitum with a 10% sucrose solution in standardized conditions (27 ± 1 °C; 80 ± 10% RH; 16 h:8 h light:dark cycle).
Experimental selection by serial passages on Ae. albopictus
For the first passage, mosquitoes were orally challenged with YFV-74018 provided in a blood-meal (washed rabbit erythrocytes) at a final titer of 106.5 FFU/mL as previously described17. Engorged mosquitoes were incubated at 28 °C for 21 days and then processed for saliva collection33. Saliva or head homogenates of 30 mosquitoes were pooled and the volume of the pool was adjusted to 600 µL with L15 prior to filtration through a Millipore H membrane (0.22 µm). An aliquot of 300 µL of each sample was used to inoculate a sub-confluent flask (25 cm2) of C6/36 Ae. albopictus cells. After 1 hour, the inoculum was discarded and cells were rinsed once with medium. L15 medium (5 mL) complemented with 2% FBS were added and cells were incubated for 8 days at 28 °C. Cell culture supernatants were then collected and provided to mosquitoes to run the next passage. Passages 1 to 5 were performed using homogenates of mosquito heads as saliva was not infectious or at a very scanty viral titer, and passages 6 to 10 with mosquito saliva which became infectious from P5. C6/36 supernatants collected at each passage were used undiluted for the next mosquito blood-meal without titration. Control isolates corresponded to serially passaged viruses on C6/36 cells to identify mutations resulting from genetic drift or adaptation to insect cell line.
Viral titration by focus forming assay
Samples were titrated by focus fluorescent assay on Ae. albopictus C6/36 cells34. Samples were serially diluted and inoculated onto C6/36 cells in 96-well plates. After an incubation of 5 days at 28 °C, cells were stained using hyper-immune ascetic fluid specific to each virus as the primary antibody and conjugated goat anti-mouse as the secondary antibody. Titers were expressed as FFU/mL.
Virus deep sequencing
Total RNA was extracted from cell culture supernatant using the Nucleospin RNA II kit (Macherey-Nagel, Hœrdt, France) according to the manufacturer’s instructions. Six overlapping amplicons were produced using the reverse transcriptase Platinum® Taq High Fidelity polymerase enzyme (Thermo Fisher Scientific, Massachusetts, USA) and specific primers (Supplementary Table 4). PCR products were pooled in equimolar proportions. After Qubit quantification using Qubit® dsDNA HS Assay Kit and Qubit 2.0 fluorometer (ThermoFisher Scientific), amplicons were fragmented (sonication) into fragments of 200 bp long. Libraries were built adding barcode, for sample identification, and primers to fragmented DNA using AB Library Builder System (ThermoFisher Scientific). To pool equimolarly the barcoded samples, a quantification step by the 2100 Bioanalyzer instrument (Agilent Technologies, California, USA) was performed. An emulsion PCR of the pools and loading on a 520 chip were realised using the automated Ion Chef instrument (ThermoFisher Scientific). Sequencing was performed using the S5 Ion torrent technology (ThermoFisher Scientific) following manufacturer’s instructions. Consensus sequence was obtained after mapping the reads on reference (inoculum strain) using CLC genomics workbench software (Qiagen, Hilden, Germany). A de novo contig was also produced to ensure that the consensus sequence was not affected by the reference sequence.
Bioinformatic analysis
Quality control of the data
The quality control of the sequencing data has been performed using FastQC (v 0.11.5) (https://www.bioinformatics.babraham.ac.uk/projects/fastqc/) and MultiQC (v 0.7)35. Reads were trimmed using Trimmomatic (v 0.36)36 with the parameters “Leading:2 Trailing:3 Slidingwindow:4:15 Minlen:36”. In order to filter any reads which could come from the mosquito host, sequences were mapped using BWA mem (v 0.7.7)37 against Ae. albopictus derived C6/36 cells (assembly GCA001876365.2). The SAM file produced was converted, sorted and indexed using Samtools (v 1.3)38 and the unmapped reads were extracted using SamToFastq from Picard Tools (v 2.8.1) (http://broadinstitute.github.io/picard/).
Variant calling
These unmapped reads were then mapped using BWA mem (v 0.7.7)37 and default parameters against the reference genome YFV-7401832. The duplicated reads were marked with MarkDuplicates from Picard Tools (v 2.8.1) (http://broadinstitute.github.io/picard/). Finally, the variant calling was done with freebayes (v 1.1.0)39 using the option -pooled-continuous. A filter has been applied with vcffilter from vcflib (v 1.0.0)39 to select only SNP variants with a quality score above 20. The results analysis has finally been done under R (v 3.3.1) (https://www.R-project.org) with the packages VariantAnnotation (v 1.20.3)40, pheatmap (v 1.0.8) (https://CRAN.R-project.org/package=pheatmap) and ggplot2 (v2.2.1) (https://www.springer.com/us/book/9780387981413).
Electronic supplementary material
Acknowledgements
We thank Laurence Mousson and Pei-Shi Yen for technical help. We warmly thank Peter Sahlins for correcting the manuscript. This study was funded by the Institut Pasteur, the French Government’s Investissement d’Avenir program, Laboratoire d’Excellence “Integrative Biology of Emerging Infectious Diseases” (grant n°ANR-10-LABX-62-IBEID), the PTR (grant n°528), the CAPES-COFECUB (grant 799-14), and the FAPERJ- Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (grant E-26/102.351/2013-CNE).
Author Contributions
F.A. performed the experiments. A.P. did the bioinformatic analysis. G.P. did the virus deep sequencing. D.C.L. was involved in collecting mosquito samples. M.V. participated in preparing viral samples. X.D.L., R.L.O. and A.-B.F. participated in conceiving and designing the experiments, analyzing/interpreting the data and the writing of the article. All authors reviewed the paper.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Adrien Pain and Géraldine Piorkowski contributed equally.
Contributor Information
Xavier de Lamballerie, Email: xavier.de-lamballerie@univ-amu.fr.
Ricardo Lourenço-de-Oliveira, Email: lourenco@ioc.fiocruz.br.
Anna-Bella Failloux, Email: anna-bella.failloux@pasteur.fr.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-32198-4.
References
- 1.Possas C, Martins RM, Oliveira RL, Homma A. Urgent call for action: avoiding spread and re-urbanisation of yellow fever in Brazil. Mem Inst Oswaldo Cruz. 2018;113:1–2. doi: 10.1590/0074-02760170361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bonaldo MC, et al. Genome analysis of yellow fever virus of the ongoing outbreak in Brazil reveals polymorphisms. Mem Inst Oswaldo Cruz. 2017;112:447–451. doi: 10.1590/0074-02760170134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gómez Mariela Martínez, Abreu Filipe Vieira Santos de, Santos Alexandre Araujo Cunha dos, Mello Iasmim Silva de, Santos Marta Pereira, Ribeiro Ieda Pereira, Ferreira-de-Brito Anielly, Miranda Rafaella Moraes de, Castro Marcia Gonçalves de, Ribeiro Mario Sergio, Laterrière Junior Roberto da Costa, Aguiar Shirlei Ferreira, Meira Guilherme Louzada Silva, Antunes Deborah, Torres Pedro Henrique Monteiro, Mir Daiana, Vicente Ana Carolina Paulo, Guimarães Ana Carolina Ramos, Caffarena Ernesto Raul, Bello Gonzalo, Lourenço-de-Oliveira Ricardo, Bonaldo Myrna Cristina. Genomic and structural features of the yellow fever virus from the 2016–2017 Brazilian outbreak. Journal of General Virology. 2018;99(4):536–548. doi: 10.1099/jgv.0.001033. [DOI] [PubMed] [Google Scholar]
- 4.Barrett AD, Higgs S. Yellow fever: a disease that has yet to be conquered. Annu Rev Entomol. 2007;52:209–229. doi: 10.1146/annurev.ento.52.110405.091454. [DOI] [PubMed] [Google Scholar]
- 5.Bryant JE, Holmes EC, Barrett AD. Out of Africa: a molecular perspective on the introduction of yellow fever virus into the Americas. PLoS Pathog. 2007;3:e75. doi: 10.1371/journal.ppat.0030075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soper, F. L. Ventures in World Health. PAHO Scientific Publication355. (1977).
- 7.Quiroga, R. & Vidal, R. Presentacion por paises. 14–15 (1998).
- 8.Staples JE, Monath TP. Yellow fever: 100 years of discovery. JAMA. 2008;300:960–962. doi: 10.1001/jama.300.8.960. [DOI] [PubMed] [Google Scholar]
- 9.Soper FL. The elimination of urban yellow fever in the Americas through the eradication of Aedes aegypti. American journal of public health and the nation’s health. 1963;53:7–16. doi: 10.2105/AJPH.53.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monath TP, Vasconcelos PF. Yellow fever. Journal of clinical virology: the official publication of the Pan American Society for Clinical Virology. 2015;64:160–173. doi: 10.1016/j.jcv.2014.08.030. [DOI] [PubMed] [Google Scholar]
- 11.Vasconcelos PF, et al. Genetic divergence and dispersal of yellow fever virus, Brazil. Emerg Infect Dis. 2004;10:1578–1584. doi: 10.3201/eid1009.040197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cardoso Jda C, et al. Yellow fever virus in Haemagogus leucocelaenus and Aedes serratus mosquitoes, southern Brazil, 2008. Emerg Infect Dis. 2010;16:1918–1924. doi: 10.3201/eid1612.100608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilder-Smith, A. & Leong, W. Y. Importation of yellow fever into China: assessing travel patterns. J Travel Med24, 10.1093/jtm/tax008 (2017). [DOI] [PubMed]
- 14.Massad Eduardo, Amaku Marcos, Coutinho Francisco Antonio Bezerra, Struchiner Claudio José, Lopez Luis Fernandez, Coelho Giovanini, Wilder-Smith Annelies, Burattini Marcelo Nascimento. The risk of urban yellow fever resurgence in Aedes-infested American cities. Epidemiology and Infection. 2018;146(10):1219–1225. doi: 10.1017/S0950268818001334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amraoui, F., Vazeille, M. & Failloux, A. B. French Aedes albopictus are able to transmit yellow fever virus. Euro surveillance: bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin21, 10.2807/1560-7917.ES.2016.21.39.30361 (2016). [DOI] [PMC free article] [PubMed]
- 16.Jupp PG, Kemp A. Laboratory vector competence experiments with yellow fever virus and five South African mosquito species including Aedes aegypti. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2002;96:493–498. doi: 10.1016/S0035-9203(02)90417-7. [DOI] [PubMed] [Google Scholar]
- 17.Couto-Lima D, et al. Potential risk of re-emergence of urban transmission of Yellow Fever virus in Brazil facilitated by competent Aedes populations. Sci Rep. 2017;7:4848. doi: 10.1038/s41598-017-05186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Consoli RAGB, O. R. Principais mosquitos de importância sanitária no Brasil. Rio de Janeiro. Editora FIOCRUZ, p. 228. (1994).
- 19.Lourenco-de-Oliveira R, Vazeille M, de Filippis AM, Failloux AB. Aedes aegypti in Brazil: genetically differentiated populations with high susceptibility to dengue and yellow fever viruses. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2004;98:43–54. doi: 10.1016/S0035-9203(03)00006-3. [DOI] [PubMed] [Google Scholar]
- 20.Maciel-de-Freitas R, Neto RB, Goncalves JM, Codeco CT, Lourenco-de-Oliveira R. Movement of dengue vectors between the human modified environment and an urban forest in Rio de Janeiro. J Med Entomol. 2006;43:1112–1120. doi: 10.1093/jmedent/43.6.1112. [DOI] [PubMed] [Google Scholar]
- 21.Carvalho RG, Lourenco-de-Oliveira R, Braga IA. Updating the geographical distribution and frequency of Aedes albopictus in Brazil with remarks regarding its range in the Americas. Mem Inst Oswaldo Cruz. 2014;109:787–796. doi: 10.1590/0074-0276140304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith CE. The history of dengue in tropical Asia and its probable relationship to the mosquito Aedes aegypti. The Journal of Tropical Medicine and Hygiene. 1956;59:243–251. [PubMed] [Google Scholar]
- 23.Fe NF, das G Vale Barbosa M, Alecrim WD, Guerra MV. [Registration of the occurrence of Aedes albopictus in an urban zone in Manaus, Amazonas, Brazil] Rev Saude Publica. 2003;37:674–675. doi: 10.1590/S0034-89102003000500020. [DOI] [PubMed] [Google Scholar]
- 24.Bres PL. A century of progress in combating yellow fever. Bulletin of the World Health Organization. 1986;64:775–786. [PMC free article] [PubMed] [Google Scholar]
- 25.Maia RT, Scarpassa VM, Maciel-Litaiff LH, Tadei WP. Reduced levels of genetic variation in Aedes albopictus (Diptera: Culicidae) from Manaus, Amazonas State, Brazil, based on analysis of the mitochondrial DNA ND5 gene. Genetics and molecular research: GMR. 2009;8:998–1007. doi: 10.4238/vol8-3gmr624. [DOI] [PubMed] [Google Scholar]
- 26.Vazeille M, et al. Importance of mosquito “quasispecies” in selecting an epidemic arthropod-borne virus. Sci Rep. 2016;6:29564. doi: 10.1038/srep29564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sall AA, et al. Yellow fever virus exhibits slower evolutionary dynamics than dengue virus. J Virol. 2010;84:765–772. doi: 10.1128/JVI.01738-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rastogi M, Sharma N, Singh SK. Flavivirus NS1: a multifaceted enigmatic viral protein. Virol J. 2016;13:131. doi: 10.1186/s12985-016-0590-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen J, Ng MM, Chu JJ. Activation of TLR2 and TLR6 by Dengue NS1 Protein and Its Implications in the Immunopathogenesis of Dengue Virus Infection. PLoS Pathog. 2015;11:e1005053. doi: 10.1371/journal.ppat.1005053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chung KM, et al. West Nile virus nonstructural protein NS1 inhibits complement activation by binding the regulatory protein factor H. Proc Natl Acad Sci USA. 2006;103:19111–19116. doi: 10.1073/pnas.0605668103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Young PR, Hilditch PA, Bletchly C, Halloran W. An antigen capture enzyme-linked immunosorbent assay reveals high levels of the dengue virus protein NS1 in the sera of infected patients. J Clin Microbiol. 2000;38:1053–1057. doi: 10.1128/jcm.38.3.1053-1057.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Filippis AM, et al. Outbreak of jaundice and hemorrhagic fever in the Southeast of Brazil in 2001: detection and molecular characterization of yellow fever virus. J Med Virol. 2002;68:620–627. doi: 10.1002/jmv.10226. [DOI] [PubMed] [Google Scholar]
- 33.Dubrulle M, Mousson L, Moutailler S, Vazeille M, Failloux AB. Chikungunya virus and Aedes mosquitoes: saliva is infectious as soon as two days after oral infection. PLoS One. 2009;4:e5895. doi: 10.1371/journal.pone.0005895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Payne AF, Binduga-Gajewska I, Kauffman EB, Kramer LD. Quantitation of flaviviruses by fluorescent focus assay. J Virol Methods. 2006;134:183–189. doi: 10.1016/j.jviromet.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 35.Ewels P, Magnusson M, Lundin S, Kaller M. MultiQC: summarize analysis results for multiple tools and samples in a single report. Bioinformatics. 2016;32:3047–3048. doi: 10.1093/bioinformatics/btw354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bolger AM, Lohse M, Usadel B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30:2114–2120. doi: 10.1093/bioinformatics/btu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li, H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. arXiv 1303.3997v1 [q-bio.GN] (2013).
- 38.Li H, et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics. 2009;25:2078–2079. doi: 10.1093/bioinformatics/btp352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garrison, E. & Gabor, M. Haplotype-based variant detection from short-read sequencing. arXiv:1207.3907 [q-bio.GN] (2012).
- 40.Obenchain V, et al. VariantAnnotation: a Bioconductor package for exploration and annotation of genetic variants. Bioinformatics. 2014;30:2076–2078. doi: 10.1093/bioinformatics/btu168. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


