Abstract
Background
Vitamin D deficiency is common in patients with chronic kidney disease (CKD), and is associated with endothelial dysfunction and cardiovascular disease. We performed a meta-analysis to assess the effect of vitamin D treatment on flow mediated vasodilation (FMD) in CKD patients.
Methods
PubMed/Medline, Web of Science, Embase and Cochrane trials and reviews were searched systematically for randomized controlled trials (RCT:s) using any vitamin D compound, at any stage of CKD, with FMD as outcome. Fixed and random effects models were performed using the standardized mean difference effect size post treatment for each trial. Heterogeneity was assessed by I2 statistics.
Results
4 trials were included, comprising 305 patients. One used both 1 and 2 μg for two intervention groups and was therefore split in two during the analysis. Patients in the included trials had a mean age of 44–65 years and were all in CKD 3 to 4. One study used cholecalciferol, the others all used paricalcitol as treatment. Study duration was 12–16 weeks. Intervention with vitamin D was associated with ameliorated FMD (STANDmean ES 0.78, 95% CI 0.55–1.01) in a fixed model. Heterogeneity was substantial (I2 = 84%). Secondary analysis with random model analysis also showed significant results.
Conclusions
Short term intervention with vitamin D is associated with improvements in endothelial function, as measured by FMD. This indicates positive effects of vitamin D on vascular disease in CKD. Limitations of this meta-analysis are the small number of studies performed, and the short duration of intervention.
Electronic supplementary material
The online version of this article (10.1186/s12882-018-1042-y) contains supplementary material, which is available to authorized users.
Keywords: Endothelial function, Flow mediated vasodilation, Cholecalciferol, Paricalcitol, Renal failure
Background
Chronic kidney disease (CKD) is a worldwide health issue, affecting 10–15% of the population with high costs both for patients and society [1, 2]. The main reasons for death is not, however, end stage renal disease, but more often cardiovascular events [2, 3]. The acknowledgement of kidney dysfunction as a strong risk factor for cardiovascular (CV) disease is highlighted in the European Society of Cardiology (ESC) [4] and the Kidney Disease Improving Global Outcome (KDIGO) guidelines [5]. Even so, treatment options to affect outcome are few, and evidence of these on cardiovascular hard end points are sparse.
Most CKD patients suffer a pronounced vascular disease, with endothelial dysfunction from early stages [6], and later on a marked vascular stiffening and arterial calcification [1, 3]. The reasons are multifactorial though with emphasis on chronic inflammation and disturbances in the hormonal mineral bone disorder (MBD) axis, with vitamin D deficiency, secondary hyperparathyreoidism (hPTH), high phosphate, and FGF-23 levels and downregulation of Klotho [1–3] [7].
Vitamin D has been shown to have anti-inflammatory and anti-oxidative properties ([8]). Vitamin D also down-regulates the expression of renin and has therefore gained interest as a possible treatment option in CKD [9, 10]. Meta-analyses from the last decade show that vitamin D affects residual albuminuria/proteinuria, on top of RAAS blockade [11–14] probably due to anti-inflammatory effects, such as downregulation of the TGF-beta pathway [13], downregulation of renin expressing genes [9, 10], and based on synergy with the AT1-receptor [15]. Glucose metabolism is another interesting area, where one meta-analysis shows positive effect on glucose control by treatment [16].
There has been some concern that active vitamin D compounds might cause a deterioration of renal function. Zhang et al. [17] performed a meta-analysis that showed higher creatinine levels with treatment, but no effect on eGFR when measured without creatinine, interpreted as no real effect on eGFR but probably higher creatinine due to an altered creatinine metabolism with active compounds [12]. These results are in line with other meta-analyses investigating the same area [12, 14].
Meta-analyses on cardiovascular risk and mortality show effect of treatment with vitamin D in CKD patients in observational studies [18, 19]. One meta-analysis [20] investigated the effect on cardiovascular endpoints in controlled trials, but could not show any benefit of treatment. These results may be questioned however, since none of the included studies had these endpoints as à priori primary or secondary endpoints, and the study durations varied from 3 weeks to 2 years.
There is a lack of interventional studies of vitamin D in CKD with sufficient power to answer questions on hard endpoints. In the absence of hard endpoints, surrogate markers of cardiovascular risk have been used in interventional trials, such as flow mediated vasodilation (FMD) since endothelial dysfunction precedes manifest vascular disease [21, 22]. In vitro data support the notion of a direct effect of vitamin D on endothelial function, with decreased oxidative stress and augmented levels of eNOS [23–25]. This makes endothelial function measured by FMD an interesting topic for a meta-analysis in the small, short duration studies performed in the area.
Methods
Study inclusion criteria.
This meta-analysis was made in accordance with the PRISMA guidelines and checklist. We included randomized controlled trials using a placebo or no treatment group as control. The population was restricted to CKD patients, in any stage of the disease, with or without diabetes mellitus. Intervention was considered treatment or supplementation with any vitamin D compound. Outcome was limited to FMD. Exclusion criteria were combined vitamin D and calcium treatment, or comparison to other vitamin D compounds (active versus precursor) or to calcimimetics, without a non-treatment control group.
Data sources and searches
Together with two librarians specialized in data base searches, we performed a systematic search of available literature. To avoid too many negative results the search was set between year 2000 and 2018-03-22, since the cardiovascular protective effects of vitamin D were not investigated before that time. PubMed/Medline, Embase and Web of Science (WoS) as well as Cochrane reviews and Cochrane trials were searched in a systematic way. We used the MeSH-term for vitamin D as well as kidney disease and then all terms listed beneath, words from entry terms, and words found in relevant abstracts. Words used were checked against abstracts to make sure they were relevant. Search results were restricted to controlled trials and to the English language. Conference abstracts were included in the search. A full report of the search strategy, including information on software and special features, is available in the supplemental material.
Data extraction and methodological study quality
Data was extracted by two blinded investigators, in accordance with a standardized extraction form, including terms as study length, number of participants, vitamin D compound and dosage, age, CKD stage, and other treatments (Table 1). There were too few studies to account statistically for interrater reliability, but the extraction forms were well matched and differences resolved by discussion between the authors. Methodological study quality was assessed by the Jadad Score [26], which give 1–5 points for blinding, randomization and the account of all screened and included patients. There were no remaining questions after data extraction. Therefore no further contact with authors was needed.
Table 1.
Characteristics of included studies
| Author | Zoccali (− 14) | Lundwall 2 μg (− 15) | Lundwall 1 μg (− 15) | Theti (− 15) | Kumar (− 17) |
|---|---|---|---|---|---|
| Country | Italy | Sweden | Sweden | USA | India |
| Duration | 12 w | 12 w | 12 w | 12 w | 16 w |
| Sample size (nr) | 89, analysis on 88 | 24, ITT | 24, ITT | 60, 55 completed, analysis on 46 | 120, analysis on 117 |
| CKD stage | 3–4 | 3–4 | 3–4 | 3–4 | 3–4 |
| Treatment | paricalcitol | paricalcitol | paricalcitol | paricalcitol | Cholecalciferol |
| Dose | 2 μg daily | 2 μg daily | 1 μg daily | 1 μg daily | 300.000 IU at baseline and after 8 week |
| Baseline 25 (OH) D(nmol/l) | 35.5 | 65.1 | 66.7 | 1.25-OHD: 34.5 (pg/ml) | 33.2 |
| Age (mean) | 62.5 | 65.0 | 68.6 | 62.5 (median) | 44.2 |
| ACEi/ARB (%) | N/A | 80.6 | 80.6 | 69.1 | 67.5 |
| Jadad score | 4 | 4 | 4 | 3 | 5 |
| Underlying condition/DM | N/A | Non-diabetic patients | Non-diabetic patients | Diabetic nephropathy | Non-diabetic patients |
| Outcome | FMD | FMD,PWV,echo,iontophoresis,microcirculation | FMD,PWV,echo,iontophoresis,microcirculation | FMD | FMD,PWV |
ITT intention to treat, ACEi angiotensin converting enzyme inhibitor, ARB angiotensin receptor blocker, FMD flow mediated vasodilation, PWV pulse wave velocity, Echo echocardiography
Data synthesis and analysis
We used standardized mean difference effect size (STANDmean ES) [27, 28] between treated patients and placebo/no treatment patients post treatment to assess the effect of vitamin D on FMD. We used the weighted standard deviation (SD) [28], when SD was presented in the article. In one case SD had to be estimated from range as (max-min)/4. In one article neither the exact value post treatment nor SD measures were presented in the article or the supplemental material and we then used the t-value, estimated from the p-value post treatment as recommended [28, 29]. The effect size for each study was calculated according to Hedges g [27, 28]. Standard error (SE) and 95% confidence interval (CI) were computed for all studies. A positive effect size indicated a result in favour of the treatment group.
Overall STANDmean ES for all included studies was assessed with a fixed effects model. Studies were weighted with the inverse variance weights technique giving more weight to studies with larger populations to allow higher impact to studies that yield a more precise estimate [27]. SE and 95% CI were calculated for the overall ES.
We also performed a random effects model, according to the DerSimonian and Laird estimate [27].
We computed correlations of effect sizes and study populations and funnel plots to investigate publication bias [27, 28].
To assess heterogeneity we calculated I2 statistics where < 50% was considered as minimal heterogeneity, 50–75% as moderate and > 75% as substantial heterogeneity [30, 31].
Results
Study selection
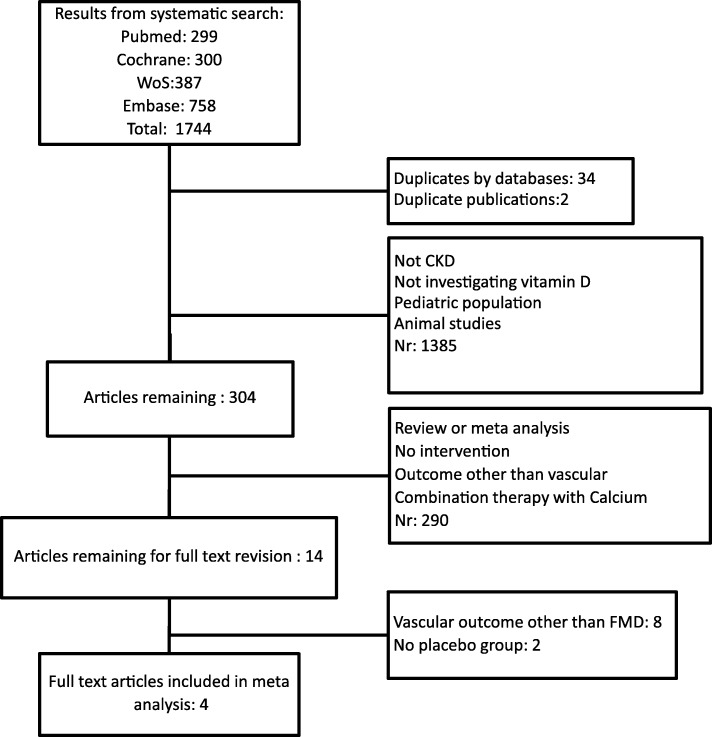
The screening and selection of articles was performed by two blinded investigators (author 1 and 4), and disagreements were resolved by discussion with the other authors. There were no remaining disagreements after the selection process. A total of 1744 articles were found searching the databases. After a first screening of title and abstract 304 articles remained. Of these, 14 were selected for full review. Four studies met the full inclusion criteria (Fig. 1). After discussion with all authors, one study was divided into two treatment groups, with 1 and 2 μg of paricalcitol, using the same placebo group as control. The 1 and 2 μg groups were regarded separately, thus resulting in 5 studies used in the meta-analysis. We did not find any conference abstract without a published article that was of relevance for our research question.
Fig. 1.
Flow diagram of the selection process
Study characteristics
Study characteristics are presented in Table 1. Study size varied from 24 to 120 participants, and study duration from 12 to 16 weeks. Four studies examined the effects of treatment with paricalcitol in doses of 1 or 2 μg, and one study used cholecalciferol administered in two oral doses of 300,000 IU at baseline and after 8 weeks. Mean age was 59.9 years (mean) ranging from mean/median values of 44–65 years. All patients were in CKD stage 3–4.
Quality assessment and risk of bias
The Cochrane Handbook 5–1 and the Jadad score were used to assess quality and risk of bias. Sequence generation, allocation sequence concealment, and risk of incomplete outcome data were assessed by the Jadad score. The 5 included studies had Jadad scores of 3–5, indicating median to high quality and an overall low risk of biased data. Selective outcome reporting was assessed during the screening and selection process, since we only used one outcome in the final analysis. None of the found studies reported FMD in the methodological section, but not in the results section. This together with our specified outcome indicate a low risk of selective outcome reporting.
Publication bias was assessed by rank correlation and by visual inspection of a funnel plot, and these results did not indicate publication bias. We also searched ClinicalTrials.gov without finding any unpublished material of interest for our inclusion criteria.
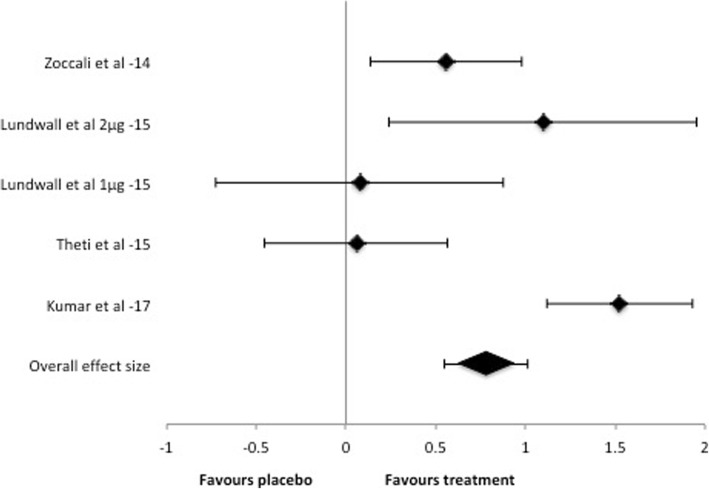
FMD outcome
Five studies with a total number of 305 patients were evaluated. There was no difference between the intervention group and the placebo group in measures of FMD at baseline in any study. Fixed effects model analysis of these studies indicated an overall effect of vitamin D treatment on FMD measures (STANDmean ES 0.78, 95% CI 0.55–1.01) (Fig. 2). Random effects model also showed a positive effect of treatment (STANDmean ES 0.67 95% CI 0.06–1.29). The heterogeneity across the included studies according to I2 statistics was substantial for the fixed model (I2 = 84%), but minimal for the random model (I2 = 0%). The number of studies was too few to perform a meta-regression to investigate the heterogeneity in the fixed model.
Fig. 2.
Forest plot of standardized effect size post intervention. A positive value indicates ameliorated FMD response in treated patients
Discussion
This meta-analysis of existing publications on intervention with vitamin D on measures of FMD shows significant effect on endothelial function, an important factor in vascular disease. Two studies using FMD as outcome were not included due to the lack of a control group. Chitalia et al. [23] showed positive effects using Cholecalciferol 300,000 IU, given as two doses at the beginning and at 8 weeks, in a 16 week duration trial. Kendrick et al. [32] compared cholecalciferol 2000 IU with calcitriol 0.5 μg daily for 6 months and did not detect any change in FMD.
There is a lack of interventional vitamin D studies with enough power to investigate hard endpoints. Instead, surrogate markers of cardiovascular risk have been used, such as pulse wave velocity and pulse wave-form analysis (PWV/PWA) and flow mediated vasodilatation (FMD) [21, 22, 33, 34]. Whereas PWV/PWA are complex measures of both beta-2 induced vasodilation [34], arterial stiffening and calcification [3], FMD is primarily a measure of the capacity of the endothelial cells to produce Nitic Oxide (NO) [35]. Since FMD is a measure of function and not structure, it is an earlier sign of vascular disease, and likely easier to affect by shorter duration of treatment. Even so, PWV and FMD are interrelated [36] and both are predictors of cardiovascular risk [6, 22, 33, 34, 37].
There seem to be a discrepancy between the results for PWV/PWA and FMD after treatment with vitamin D compounds to CKD patients. The reasons are probably many, but one important factor might be, that PWV/PWA is also a measure of arterial remodelling. Although probably due to inflammation in the first place [7], when established the structural changes in the vasculature are likely harder to affect and reverse. CKD patients have an accelerated remodelling with fibrosis and calcification [1, 3], and concerns have been raised [7] that we may intervene too late in the process in our attempts to ameliorate CKD associated vascular disease.
For these reasons we chose to use FMD as the only outcome. It is a more direct measure of NO availability, with clear antioxidant, anti-inflammatory and eNOS upregulating pathways for vitamin D actions [23–25].
We found 14 studies measuring the effect of vitamin D on different aspects of vascular function in CKD. Of these, 10 studied the effect on PWV and or PWAix with 26–120 participants, duration of 8 to 44 weeks, with CKD stage 3–5 and various vitamin D compounds and doses. Three studies reported positive effects on PWV [38–40], the rest did not detect any change after treatment. Two articles [41, 42] assessed iontophoresis by acetylcholine showing ameliorated microvascular function with treatment, though interpreted with caution due to the small number of patients and short duration. One study investigated reactive hyperaemia index, with no significant change in treated patients [43].
We chose a fixed model statistical analysis as our primary model. The reason was the few and small studies performed, which makes the results hard to generalize and thus indicated the use of a fixed model [27]. Even so, the random model performed as a secondary analysis also showed significant results of vitamin D intervention on FMD, which may allow generalization of our results.
There was, not surprisingly, a substantial heterogeneity in the fixed model. There were too few studies to perform a meta-regression of significant cofactors, but when the studies were inspected for clinical heterogeneity there were some important differences. The largest study [38] had the strongest effect size and the youngest population, originating from India, while the other populations were from western countries. In this study cholecalciferol was used as treatment in comparison with paricalcitol 1 to 2 μg in the other studies. This study also had the longest duration (16 weeks), and the highest Jadad score (5p). There was also a difference in baseline 25OH-vitamin D with significantly lower levels in the two studies with the strongest effect sizes [38, 44]. Theti et al. [45], who failed to show significant results, included only patients with diabetic nephropathy, in contrast to Kumar et al. [38] and Lundwall et al. [42] who excluded diabetics.
Even though the number of studies were too few for subgroup analyses, it is interesting to discuss the fact that the two studies that did not show positive effect of treatment with paricalcitol both used 1 μg [42, 45], in comparison with the others using 2 μg. One of them, Theti et al., [45] was also the only one investigating the effects on diabetic nephropathy. Highly interesting is also the fact that the study with the strongest effect size [38], used inactive treatment with cholecalciferol, to patients substantially younger than in the other studies, but in the same CKD stage (3–4).
Of note, there seem to be a tendency to less negative effects on calcium and phosphate metabolism with treatments using precursors of vitamin D [11–14, 46]. This might be favourable in treating vascular disease, and is also supported by a study of Zoccali et al. [47]. They saw, in a sub-study of the PENNY trial [44], that the effect of paricalcitol on FMD was most pronounced in patients with no change in phosphate during the study, and abolished in patients with the highest rise in phosphate levels, indicating the importance of different aspects of CKD mineral and bone disorders. These results might imply the use of phosphate binders in combination with active vitamin D.
Conclusion
Even though our results are hard to generalize due to the small number of studies and patients included, we show favourable effects in both the fixed and the random model, suggesting benefits of vitamin D intervention on endothelial function. Our results also indicate that the highest impact is seen in younger patients, probably due to an earlier stage of disease, where vascular remodelling has not yet been established. It might also be more favourable with the precursor than with active treatment, especially since there seemed to be a need of high doses of active compounds for effects. This is possibly due to less increased calcium and phosphate levels with inactive treatment. There is still a great need for larger and longer studies on this topic, to a proper selection of CKD patients at earlier stages of their vascular disease, and with sufficient power to assess hard endpoints.
Additional files
(SearchCochrane): Data search Cochrane; Data search strategy for Cochrane reviews and Cochrane trials. (DOCX 18 kb)
(Search Pubmed): Data search PubMed/Medline; Data search strategy for PubMed/Medline (DOCX 24 kb)
(Web of Science, Embase): Data search Web of Science and Embase; Data search strategy for Web of Science and Embase. (DOCX 128 kb)
(search software): Additional search information; Includes details about search software used, and special features used in the different searches. (DOCX 66 kb)
(MAdataBMCN): Individual study data; Includes an excel file with the data used to perform the statistical part of the meta-analysis. (XLSX 50 kb)
Acknowledgements
We would like to thank librarians Love Strandberg and Maria Lund at Danderyd Hospital library for excellent expert guidance in searching the databases. We would also like to thank Gunilla Bohlin, professor, for expert knowledge and guidance in meta-analysis techniques.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its Additional files 1, 2, 3, 4 and 5.
Abbreviations
- ACE-i
angiotensin converting enzyme inhibitor
- ARB
Angiotensin receptor blocker
- CI
confidence interval
- CKD
chronic kidney disease
- CV
Cardiovascular
- ESC
European Society of Cardiology
- Echo
Echocardiography
- FMD
flow mediated vasodilation
- hPTH
hyperparathyreoidism
- ITT
intention to treat
- KDIGO
Kidney Disease Improving Global Outcome
- MBD
Mineral bone disorder
- NO
Nitic Oxide
- PWA
Pulse wave-form analysis
- PWV
Pulse wave velocity
- RCTs
Randomized controlled trials
- SD
standard deviation
- SE
Standard error
- STANDmean ES
standardized mean difference effect size
- WoS
Web of Science
Author’s contribution
KL worked out the study design and together with the librarians performed the database search, and the screening and selection of articles. She also did the statistical work and wrote the manuscript and gave approval of final version to be published. JS guided in the planning of study design, performed the screening and selection of articles, and revised the manuscript and gave approval of final version to be published. SJ guided in the planning of study design, participated in the discussions during the selection process, and revised the manuscript and gave approval of final version to be published. GJ guided in the planning of study design, participated in the discussions during the selection process, and revised the manuscript and gave approval of final version to be published. All authors ensure that the ICMJE guidelines are fulfilled. All authors read and approved the final manusript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
JS and SJ have earlier (2009-10) received institutional grants from Abbvie for investigator initiated studies of vitamin D.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kristina Lundwall, Phone: +46 731 589999, Email: kristina.lundwall@sll.se.
Stefan H. Jacobson, Email: stefan.jacobson@sll.se
Gun Jörneskog, Email: gun.jorneskog@sll.se.
Jonas Spaak, Email: jonas.spaak@ki.se.
References
- 1.Leonard O, Spaak J, Goldsmith D. Regression of vascular calcification in chronic kidney disease - feasible or fantasy? A review of the clinical evidence. Br J Clin Pharmacol. 2013;76(4):560–72. doi: 10.1111/bcp.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ronco C, Di Lullo L. Cardiorenal syndrome. Heart Fail Clin. 2014;10(2):251–80. doi: 10.1016/j.hfc.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Schlieper G, Schurgers L, Brandenburg V, Reutelingsperger C, Floege J. Vascular calcification in chronic kidney disease: an update. Nephrol Dial Transplant. 2016;31(1):31–39. doi: 10.1093/ndt/gfv111. [DOI] [PubMed] [Google Scholar]
- 4.Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corr U, Cosyns B, Deaton C, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2016;37(29):2315–81. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoya G. Clinical guidelines National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classificaiton, and stratification. Ann Intern Med. 2003;139:137–47. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- 6.Stam F, van Guldener C, Becker A, Dekker JM, Heine RJ, Bouter LM, Stehouwer CD. Endothelial dysfunction contributes to renal function-associated cardiovascular mortality in a population with mild renal insufficiency: the Hoorn study. J Am Soc Nephrol. 2006;17(2):537–45. doi: 10.1681/ASN.2005080834. [DOI] [PubMed] [Google Scholar]
- 7.Zoccali C, London G. Con: vascular calcification is a surrogate marker, but not the cause of ongoing vascular disease, and it is not a treatment target in chronic kidney disease. Nephrol Dial Transplant. 2015;30(3):352–57. doi: 10.1093/ndt/gfv021. [DOI] [PubMed] [Google Scholar]
- 8.Vojinovic J. Vitamin D receptor agonists' anti-inflammatory properties. Ann N Y Acad Sci. 2014;1317(1):47–56. [DOI] [PubMed]
- 9.Li Y, Kong J, Wei M, Chen Z, Liu S, Cao L. 1,25 dihydroxyvitamin D3 is a negative regulator of renin angiotensin system. J Clin Investig. 2002;110(2):229–38. doi: 10.1172/JCI0215219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yuan W, Pan W, Kong J, Zheng W, Szeto FL, Wong KE, Cohen R, Klopot A, Zhang Z, Li YC. 1,25-Dihydroxyvitamin D 3 suppresses renin gene transcription by blocking the activity of the cyclic AMP response element in the renin gene promoter. J Biol Chem. 2007;282(41):29821–30. doi: 10.1074/jbc.M705495200. [DOI] [PubMed] [Google Scholar]
- 11.Cheng J, Zhang W, Zhang X, Li X, Chen J. Efficacy and safety of paricalcitol therapy for chronic kidney disease: a meta-analysis. Clin J Am Soc Nephrol. 2012;7(3):391–400. doi: 10.2215/CJN.03000311. [DOI] [PubMed] [Google Scholar]
- 12.De Borst MH, Hajhosseiny R, Tamez H, Wenger J, Thadhani R, Goldsmith DJA. Active vitamin D treatment for reduction of residual proteinuria: a systematic review. J Am Soc Nephrol. 2013;24(11):1863–71. doi: 10.1681/ASN.2013030203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han T, Rong G, Quan D, Shu Y, Liang Z, She N, Liu M, Yang B, Cheng G, Lv Y, et al. Meta-analysis: the efficacy and safety of paricalcitol for the treatment of secondary hyperparathyroidism and proteinuria in chronic kidney disease. Biomed Res Int. 2013:320560. [DOI] [PMC free article] [PubMed]
- 14.Xu L, Wan X, Huang Z, Zeng F, Wei G, Fang D, Deng W, Li Y. Impact of vitamin D on chronic kidney diseases in non-Dialysis patients: a meta-analysis of randomized controlled trials. PLoS One. 2013;8(4):e61387. doi: 10.1371/journal.pone.0061387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Deb DK, Kong J, Ning G, Wang Y, Li G, Chen Y, Zhang Z, Strugnell S, Sabbagh Y, et al. Long-term therapeutic effect of vitamin D analog doxercalciferol on diabetic nephropathy: strong synergism with AT1 receptor antagonist. AJP: Renal Physiology. 2009;297(3):F791–801. doi: 10.1152/ajprenal.00247.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sarathy H, Pramanik V, Kahn J, Abramowitz MK, Meier K, Kishore P, Melamed ML. The effects of short-term vitamin D supplementation on glucose metabolism in dialysis patients: a systematic review and meta-analysis. Int Urol Nephrol. 2015;47(3):537–49. doi: 10.1007/s11255-015-0909-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang Q, Li M, Zhang T, Chen J. Effect of vitamin D receptor activators on glomerular filtration rate: a meta-analysis and systematic review. PLoS One. 2016;11(1):e0147347. doi: 10.1371/journal.pone.0147347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duranton F, Rodriguez-Ortiz ME, Duny Y, Rodriguez M, Daurès J-P, Argilés A. Vitamin D treatment and mortality in chronic kidney disease: a systematic review and meta-analysis. Am J Nephrol. 2013;37(3):239–48. doi: 10.1159/000346846. [DOI] [PubMed] [Google Scholar]
- 19.Zheng Z, Shi H, Jia J, Li D, Lin S. Vitamin D supplementation and mortality risk in chronic kidney disease: a meta-analysis of 20 observational studies. BMC Nephrol. 2013;14:199. doi: 10.1186/1471-2369-14-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mann MC, Hobbs AJ, Hemmelgarn BR, Roberts DJ, Ahmed SB, Rabi DM. Effect of oral vitamin D analogs on mortality and cardiovascular outcomes among adults with chronic kidney disease: a meta-analysis. Clin Kidney J. 2015;8(1):41–48. doi: 10.1093/ckj/sfu122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muiesan ML, Salvetti M, Paini A, Monteduro C, Galbassini G, Poisa P, Porteri E, Agabiti-Rosei C, Paderno V, Belotti E, et al. Prognostic role of flow-mediated dilatation of the brachial artery in hypertensive patients. J Hypertens. 2008;26(8):1612–18. doi: 10.1097/HJH.0b013e328304b083. [DOI] [PubMed] [Google Scholar]
- 22.Yeboah J, Folsom AR, Burke GL, Johnson C, Polak JF, Post W, Lima J, Crouse JR, Herrington DM. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the multi-ethnic study of atherosclerosis. Circulation. 2009;120(6):502–09. doi: 10.1161/CIRCULATIONAHA.109.864801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chitalia N, Ismail T, Tooth L, Boa F, Hampson G, Goldsmith D, Kaski JC, Banerjee D. Impact of vitamin D supplementation on arterial vasomotion, stiffness and endothelial biomarkers in chronic kidney disease patients. PLoS One. 2014;9(3):e91363. doi: 10.1371/journal.pone.0091363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jia X, Xu J, Gu Y, Gu X, Li W, Wang Y. Vitamin D suppresses oxidative stress-induced microparticle release by human umbilical vein endothelial cells. Biol Reprod. 2017;96:199–210. doi: 10.1093/biolre/bio142604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu J, Jia X, Gu Y. Vitamin D reduces oxidative stress – induced Procaspase-3/ROCK1 activation and MP release by placental trophoblasts. J Clin Endocrinol Metab. 2017;102(6):2100–2110. doi: 10.1210/jc.2016-3753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 27.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 28.Hesser H, Andersson G. Introduktion till metaanalyser och systematiska översikter: Studentlitteratur; 2015.
- 29.Card NE. Applied meta-analysis for social science research: Guilford Press; 2012.
- 30.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Higgins JPT, Green S. Cochrane Handbook for systematic reviews of intervention version 5.1.0: The Cochrane Collaboration; 2011.
- 32.Kendrick J, Andrews E, You Z, Moreau K, Nowak KL, Farmer-Bailey H, Seals DR, Chonchol M. Cholecalciferol, calcitriol, and vascular function in CKD: a randomized, double-blind trial. Clinical J Am Soc Nephrology. 2017;12(9):1438–46. doi: 10.2215/CJN.01870217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chowienczyk PJ, Kelly RP, MacCallum H, Millasseau SC, Andersson TLG, Gosling RG, Ritter JM, Änggård EE. Photoplethysmographic assessment of pulse wave reflection. J Am Coll Cardiol. 1999;34(7):2007–2014. doi: 10.1016/S0735-1097(99)00441-6. [DOI] [PubMed] [Google Scholar]
- 34.Wilkinson IB, Hall IR, MacCallum H, Mackenzie IS, McEniery CM, van der Arend BJ. Shu Y-e, MacKay LS, Webb DJ, Cockcroft JR. Pulse-wave analysis: clinical evaluation of a noninvasive, widely applicable method for assessing endothelial function. Arterioscler Thromb Vasc Biol. 2002;22(1):147–52. doi: 10.1161/hq0102.101770. [DOI] [PubMed] [Google Scholar]
- 35.Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, ma C, Deanfield J, Drexler H, Gerhard-Herman M, Herrington D, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the international brachial artery reactivity task force. J Am Coll Cardiol. 2002;39(2):257–265. doi: 10.1016/S0735-1097(01)01746-6. [DOI] [PubMed] [Google Scholar]
- 36.Soltész P, Dér H, Kerekes G, Szodoray P, Szücs G, Dankó K, Shoenfeld Y, Szegedi G, Szekanecz Z. A comparative study of arterial stiffness, flow-mediated vasodilation of the brachial artery, and the thickness of the carotid artery intima-media in patients with systemic autoimmune diseases. Clin Rheumatol. 2009;28(6):655–662. doi: 10.1007/s10067-009-1118-y. [DOI] [PubMed] [Google Scholar]
- 37.Flammer AJ, Anderson T, Celermajer DS, Ma C, Deanfield J, Ganz P, Hamburg NM, Lüscher TF, Shechter M, Taddei S, et al. The assessment of endothelial function: from research into clinical practice. Circulation. 2012;126(6):753–767. doi: 10.1161/CIRCULATIONAHA.112.093245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kumar V, Yadav AK, Lal A, Kumar V, Singhal M, Billot L, Gupta KL, Banerjee D, Jha V. A randomized trial of vitamin D supplementation on vascular function in CKD. J Am Soc Nephrol. 2017;10:3100–08. doi: 10.1681/ASN.2017010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kumar V, Yadav AK, Singhal M, Kumar V, Lal A, Banerjee D, Gupta KL, Jha V. Vascular function and cholecalciferol supplementation in CKD: a self-controlled case series. J Steroid Biochem Mol Biol. 2018;180:19–22. doi: 10.1016/j.jsbmb.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 40.Levin A, Tang M, Perry T, Zalunardo N, Beaulieu M, Dubland JA, Zerr K. Randomized controlled trial for the effect of vitamin D supplementation on vascular stiffness in CKD. Clin J Am Soc Nephrol. 2017;12:1–17. doi: 10.2215/CJN.10791016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dreyer G, Tucker AT, Harwood SM, Pearse RM, Raftery MJ, Yaqoob MM. Ergocalciferol and microcirculatory function in chronic kidney disease and concomitant vitamin D deficiency: an exploratory, double blind, randomised controlled trial. PLoS One. 2014;9(7):e99461. doi: 10.1371/journal.pone.0099461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lundwall K, Jörneskog G, Jacobson SH, Spaak J. Paricalcitol, microvascular and endothelial function in non-diabetic chronic kidney disease: a randomized trial. Am J Nephrol. 2015;42(4):265–273. doi: 10.1159/000441364. [DOI] [PubMed] [Google Scholar]
- 43.Pihlstrøm HK, Gatti F, Hammarström C, Eide IA, Kasprzycka M, Wang J, Haraldsen G, Svensson MHS, Midtvedt K, Mjøen G, et al. Early introduction of oral paricalcitol in renal transplant recipients. An open-label randomized study. Transpl Int. 2017;30(8):827–840. doi: 10.1111/tri.12973. [DOI] [PubMed] [Google Scholar]
- 44.Zoccali C, Curatola G, Panuccio V, Tripepi R, Pizzini P, Versace M, Bolignano D, Cutrupi S, Politi R, Tripepi G, et al. Paricalcitol and endothelial function in chronic kidney disease trial. Hypertension. 2014;64(5):1005–1011. doi: 10.1161/HYPERTENSIONAHA.114.03748. [DOI] [PubMed] [Google Scholar]
- 45.Thethi TK, Bajwa MA, Ghanim H, Jo C, Weir M, Gold AB, Umpierrez G, Desouza C, Dandona P, Fang-hollingsworth Y, et al. Effect of paricalcitol on endothelial function and inflammation in type 2 diabetes and chronic kidney disease. J Diabetes Complicat. 2015;29:433–37. doi: 10.1016/j.jdiacomp.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kandula P, Dobre M, Schold JD, Schreiber MJ, Jr, Mehrotra R, Navaneethan SD. Vitamin D supplementation in chronic kidney disease: a systematic review and meta-analysis of observational studies and randomized controlled trials. Clin J Am Soc Nephrol. 2011;6(1):50–62. doi: 10.2215/CJN.03940510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zoccali C, Torino C, Curatola G, Panuccio V, Tripepi R, Pizzini P, Versace M, Bolignano D, Cutrupi S, Ghiadoni L, et al. Serum phosphate modifies the vascular response to vitamin D receptor activation in chronic kidney disease (CKD) patients. Nutr Metab Cardiovasc Dis. 2016;26(7):581–89. doi: 10.1016/j.numecd.2016.03.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SearchCochrane): Data search Cochrane; Data search strategy for Cochrane reviews and Cochrane trials. (DOCX 18 kb)
(Search Pubmed): Data search PubMed/Medline; Data search strategy for PubMed/Medline (DOCX 24 kb)
(Web of Science, Embase): Data search Web of Science and Embase; Data search strategy for Web of Science and Embase. (DOCX 128 kb)
(search software): Additional search information; Includes details about search software used, and special features used in the different searches. (DOCX 66 kb)
(MAdataBMCN): Individual study data; Includes an excel file with the data used to perform the statistical part of the meta-analysis. (XLSX 50 kb)
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its Additional files 1, 2, 3, 4 and 5.