Key Points
Almost 70% of this adult SCD cohort reports chronic daily pain.
Acute care utilization for adults has increased significantly when compared with those studied in the Cooperative Study of Sickle Cell Disease.
Abstract
The ESCAPED (Examining Sickle Cell Acute Pain in the Emergency vs Day Hospital) trial is an ongoing prospective study comparing outcomes of people with sickle cell disease (SCD) seeking care for acute pain management in either an emergency department or specialty infusion clinic. The objective of this paper is to describe the baseline characteristics and health care utilization of patients in the trial. This is a multicenter study across 4 US cities that enrolled all adults with SCD living within 60 miles (96.6 km) of a study site who were expected to have acute care utilization over the study period. Twenty-one percent of participants had no acute care visits in the first 12 months of follow-up. Using negative binomial regression, we describe subject characteristics that predict acute care utilization. Three hundred ninety-one subjects have completed 12 months of follow-up with a mean age of 34.5 years (standard deviation, 11.4), 60% are female. Fifty-four percent of subjects with hemoglobin SS disease and 46% with hemoglobin SC disease had 3 or more acute visits over the study period. The prevalence of chronic pain in this cohort was 68%. Predictors of higher rates of acute care utilization included being unemployed, having chronic pain, being on chronic transfusion therapy, having a history of stroke, and being on disability or on Medicaid. This is the first prospective cohort in the modern era, and it demonstrates much higher rates of acute care utilization than reported in the Cooperative Study of Sickle Cell Disease.
Visual Abstract

Introduction
Sickle cell disease (SCD) affects ∼100 000 individuals in the United States.1 Acute painful vaso-occlusive crises (VOCs) are the leading cause of emergency department (ED) utilization,2 affecting both patients with homozygous SS disease and with variant (compound heterozygous) SC or Sβ+ thalassemia. The extent of ED care, and subsequent hospitalizations, is high and is primarily borne by adults with the disease.3
As an alternative to ED care, a growing body of literature supports the role of the subspecialty infusion center (IC) in delivering individualized care to people with SCD.4,5 Benjamin et al first reported that the establishment of a dedicated SCD day hospital led to a 40% reduction in inpatient admissions relative to ED management.4 Since this seminal work, a number of papers have suggested that rapid assessment of VOC, close monitoring, and individualized care improve outcomes.6-9 However, there has not been a direct comparison between IC clinics and the ED as sites for pain management in SCD. The ESCAPED (Examining Sickle Cell Acute Pain in the Emergency vs Day Hospital) study is an ongoing multisite study comparing outcomes between patients seeking care in EDs and ICs. Here, we report the baseline characteristics and health care utilization of patients enrolled in the ESCAPED trial. This is the first prospective cohort describing acute care management for patients with SCD since the conclusion of the Cooperative Study of Sickle Cell Disease (CSSCD) in the 1980s.
Methods
The ESCAPED study is ongoing in 4 US cities (Baltimore, MD; Cleveland, OH; Milwaukee, WI; and Baton Rouge, LA). The primary outcomes for the main trial include time to first dose of opioid, time to reassessment of pain after the initial dose of pain medication, patient disposition after acute pain treatment (ie, hospitalized vs discharged home) and patient reported experience of care at each visit. The primary purpose of this substudy was to examine acute care utilization by the ESCAPED cohort, identify characteristics associated with the number of acute care visits, and compare it with the CSSCD cohort. Adults (18+ years) with any SCD genotype living within 60 miles (96.6 km) of a study site were screened for enrollment. Participants were enrolled during regular outpatient clinic visits. As the purpose of this study was to evaluate acute care utilization, we excluded individuals whose disease was well controlled on chronic transfusion therapy who had no acute visits in the 2 years before screening. This was done to avoid enrolling subjects who may not have any acute visits during the study period (fewer than 20 subjects from all sites were excluded on this basis). The study was institutional review board–approved at all 4 participating sites. After receiving informed consent, participants filled out a survey to collect demographic details, medical information, and self-reported presence or absence of chronic pain. Medical records were reviewed to confirm existing disease complications. By convention in SCD, kidney disease was defined as albuminuria >30 mg/g (or proteinuria) or an estimated glomerular filtration rate <90 mL/min body surface area–corrected.
Each subject was asked to remain in the cohort for 18 months. We continue to collect subjective and objective data from all visits for acute uncomplicated VOC, defined as an acute episode of pain with no other known cause that requires parenteral therapy for pain relief. Data collected at each visit consist of time to first dose of opioid, time to nurse reassessment after the first dose, and disposition. All subjects are contacted monthly, and, where available, statewide health information exchanges are reviewed to assure that all acute visits are captured.
We describe here the baseline characteristics of the entire cohort and their acute care visits over the first 12 months of enrollment. We used a series of negative binomial regression models to explore associations between subject characteristics and the number of acute visits for the subset of individuals in the cohort for at least 12 months.
Results
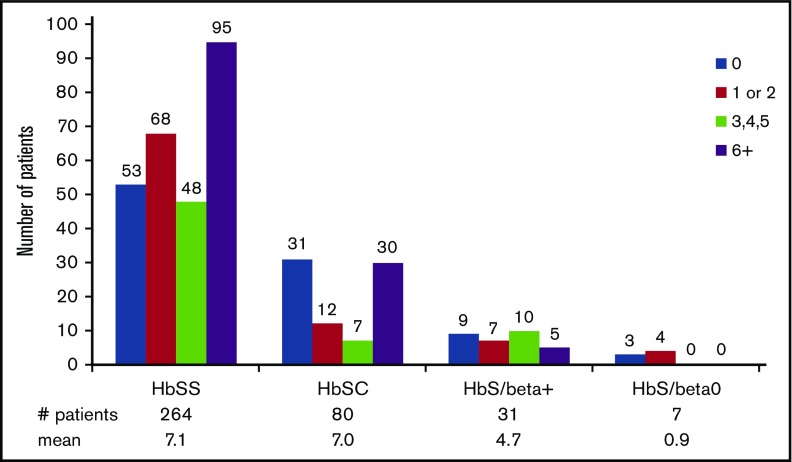
We have enrolled 483 participants in the ESCAPED trial; 391 have had at least 12 months of follow-up. The 391 subject’s characteristics are described in Table 1. The number of subjects lost to follow-up prior to 12 months of follow-up was 17, they are not included in this analysis. The mean age of the cohort is 34.5 years (SD, 11.4), and 60% of the cohort is female. The mean length of follow-up in these 391 subjects was 16.6 (SD, 1.8) months (range, 12-18 months). The mean number of acute visits per month for uncomplicated VOC by the cohort was 0.56 (SD, 0.83) with a median of 0.22 (interquartile range, 0.06-0.78). The median number of acute visits was 3.0 (interquartile range, 0.5-9.0). Fifty-four percent of patients with hemoglobin SS disease had 3 or more visits in the first 12 months of follow-up, with 36% having 6 or more visits. For those with hemoglobin SC disease, 47% had 3 or more acute visits, with 38% having >6 visits in the first 12 months of enrollment (Figure 1). Eighty-four subjects have had no acute visits after 12 months of follow-up.
Table 1.
Patient characteristics
| Characteristics (n = 391) | Value |
|---|---|
| Sex, % | |
| Female | 59.8 |
| Male | 40.2 |
| Sickle cell anemia (SCA) | |
| SCA, % | 69.3 |
| SC variant, % | 28.6 |
| Mean age (SD) | 34.5 (11.4) |
| Graduated high school, % | |
| Y | 80.8 |
| N | 15.9 |
| Employed, % | |
| Y | 40.9 |
| N | 57.8 |
| Insured by Medicaid, % | |
| Y | 53.7 |
| N | 42.5 |
| Married or with significant other, % | |
| Y | 23.3 |
| N | 76.5 |
| Residence, live alone, % | |
| Y | 28.9 |
| N | 71.1 |
| Low annual income, <$20 000, % | |
| Y | 47.1 |
| N | 47.5 |
| Disability, % | |
| Y | 59.8 |
| N | 39.4 |
| Have PCP, % | |
| Y | 67.8 |
| N | 32.2 |
| Kidney disease, % | |
| Y | 14.3 |
| N | 82.6 |
| Leg ulcer, % | |
| Y | 4.9 |
| N | 93.4 |
| Stroke, % | |
| Y | 13.0 |
| N | 84.9 |
| Retinopathy, % | |
| Y | 19.2 |
| N | 78.0 |
| Avascular necrosis, % | |
| Y | 33.0 |
| N | 65.2 |
| Priapism, male only, % | |
| Y | 30.6 |
| N | 69.4 |
| Chronic pain, % | |
| Y | 67.5 |
| N | 32.5 |
| Opioid use, % | |
| Long acting only | 3.1 |
| Short acting only | 56.3 |
| Both | 36.8 |
| None | 3.3 |
| On chronic transfusions, % | |
| Y | 11.8 |
| N | 88.2 |
| On hydroxyurea (SCA only), % | |
| Y | 63.8 |
| N | 35.8 |
N, no; PCP, primary care provider; SD, standard deviation; Y, yes.
Figure 1.
Number of acute care visits in the first 12 months of follow-up in the ESCAPED trial by genotype.
The prevalence of self-reported chronic pain in this cohort was 68%. More than 90% of the cohort reported using opioids, with 56% reporting the use of short-acting opioids only, and 36.8% reporting the use of both short- and long-acting opioids. In univariate analysis (Table 2), participants who were employed had fewer acute visits than unemployed patients (mean 4.2 vs 8.2; incidence rate ratio (IRR), 0.51 [95% CI, 0.38-0.68]). Individuals with chronic pain (mean 8.1 vs 3.9; IRR, 2.08 [95% CI, 1.53-2.83]), on chronic transfusion therapy (mean 10.4 vs 6.2; IRR, 1.68 [95% CI, 1.08-2.61]), with a history of stroke (mean 9.8 vs 6.3; IRR, 1.56 [95% CI, 1.02-2.38]), on disability (mean 8.1 vs 4.5; IRR, 1.79 [95% CI, 1.34-2.40]), or those on Medicaid (mean 7.3 vs 5.6; IRR, 1.30 [95% CI, 0.97-1.76]) had more acute visits than those without these characteristics. The use of long-acting opioids was associated with more acute care visits (IRR, 3.19 [95% CI, 1.45-7.73]), and those on no opioids had significantly fewer acute care visits (IRR, 0.31 [95% CI, 0.14-0.73]) compared with those on short acting opioids only. No association was found between avascular necrosis (AVN) and utilization; however, those with AVN were 2.56 times more likely to report chronic pain (95% CI, 1.55-4.21) than those without AVN. There was a trend toward decreased utilization for those on hydroxyurea, but it was not statistically significant (IRR, 0.87 [95% CI, 0.62-1.32]).
Table 2.
Univariate associations of acute care utilization
| Characteristics | Incident rate ratio (95% CI) | Mean number of acute care utilizations (SD) | |||
|---|---|---|---|---|---|
| Sex (F vs M) | 1.04 (0.77, 1.39) | F | M | ||
| 6.8 (10.5) | 6.6 (9.3) | ||||
| SCA (SCA vs SC variant) | 1.07 (0.78, 1.48) | SCA | SC variant | ||
| 6.9 (10.4) | 6.5 (9.5) | ||||
| Age | 0.98 (0.97, 0.997)** | NA | |||
| Graduated high school (Y vs N) | 0.81 (0.54, 1.21) | Y | N | ||
| 6.4 (10.1) | 7.9 (9.9) | ||||
| Employed (Y vs N) | 0.51 (0.38, 0.68)**** | Y | N | ||
| 4.2 (7.0) | 8.2 (11.2) | ||||
| Insured by Medicaid (Y vs N) | 1.30 (0.97, 1.76)* | Y | N | ||
| 7.3 (10.2) | 5.6 (9.4) | ||||
| Married or with significant other (Y vs N) | 0.90 (0.64, 1.27) | Y | N | ||
| 6.2 (9.6) | 6.9 (10.2) | ||||
| Residence, live alone (Y vs N) | 0.93 (0.68, 1.28) | Y | N | ||
| 6.4 (10.0) | 6.8 (10.1) | ||||
| Low annual income, <$20 000 (Y vs N) | 1.13 (0.84, 1.53) | Y | N | ||
| 7.2 (10.6) | 6.4 (9.8) | ||||
| Disability (Y vs N) | 1.79 (1.34, 2.40)**** | Y | N | ||
| 8.1 (11.0) | 4.5 (8.0) | ||||
| Have PCP (Y vs N) | 1.20 (0.88, 1.64) | Y | N | ||
| 7.1 (10.9) | 5.9 (8.0) | ||||
| Kidney disease (Y vs N) | 1.38 (0.92, 2.09) | Y | N | ||
| 8.9 (13.4) | 6.5 (9.5) | ||||
| Leg ulcer (Y vs N) | 1.39 (0.71, 2.72) | Y | N | ||
| 9.3 (18.7) | 6.6 (9.5) | ||||
| Stroke (Y vs N) | 1.56 (1.02, 2.38)** | Y | N | ||
| 9.8 (12.5) | 6.3 (9.6) | ||||
| Retinopathy (Y vs N) | 1.37 (0.95, 1.98)* | Y | N | ||
| 8.7 (12.2) | 6.4 (9.6) | ||||
| AVN (Y vs N) | 1.17 (0.86, 1.60) | Y | N | ||
| 7.5 (10.5) | 6.4 (9.9) | ||||
| Priapism, male only (Y vs N) | 1.0 (0.61, 1.63) | Y | N | ||
| 6.5 (8.5) | 6.6 (9.7) | ||||
| Chronic pain (Y vs N) | 2.08 (1.53, 2.83)**** | Y | N | ||
| 8.1 (11.1) | 3.9 (6.6) | ||||
| Opioid use (long acting vs short acting) | 3.19 (1.56, 7.73)*** | Short acting | Long acting | Both | None |
| (both vs short acting) | 2.15 (1.61, 2.88)**** | 4.6 (7.5) | 14.6 (17.4) | 9.8 (11.8) | 1.4 (4.1) |
| (none vs short acting) | 0.31 (0.14, 0.73)*** | ||||
| On chronic transfusions (Y vs N) | 1.68 (1.08, 2.61)** | Y | N | ||
| 10.4 (13.3) | 6.2 (9.4) | ||||
| On hydroxyurea (Y vs N) (SCA only) | 0.87 (0.62, 1.23) | Y | N | ||
| 6.6 (8.9) | 7.5 (12.7) | ||||
CI, confidence interval; F, female; M, male; NA, not applicable.
.05 < P < .1; **P < .05; ***P < .01; ****P < .001.
Discussion
The ESCAPED trial is the first modern, multicenter, prospective cohort to describe acute care utilization for adults with SCD. Brousseau et al3 described acute care utilization in a retrospective cohort. They found that patients had a mean of 2.59 encounters per year, with 18- to 30-year-olds having the highest utilization rates, with 4.80 encounters per year. Our study demonstrates higher rates of acute care utilization in this cohort, when compared with that study, and higher than results from a prospective trial in an earlier era. The CSSCD described acute care utilization by adults and children in the 1980s. In that study, Platt et al described pain rates in 3578 individuals; 39% of patients with homozygous SS disease had no annual visits for VOC.2 In the ESCAPED study, only 22% of adults with homozygous SS disease had no annual visits for VOC. Strikingly, only 8% of subjects 20 years or older in the CSSCD had 3 or more acute care visits in a year, whereas in the ESCAPED cohort, 54% of patients with homozygous SS disease had 3 or more annual visits. Similar differences in utilization exist for those with variant SC disease, in which fewer than 5% of the CSSCD cohort had >3 visits per year compared with 46% in the ESCAPED cohort. While SC is seen as a less severe form of the disease, our trial demonstrates that this population suffers from frequent painful events requiring acute care utilization.
There are a number of possible reasons for the increase in utilization seen in the modern era. First, in an era of improved outcomes for children with homozygous SS disease (because of infectious prophylaxis, transfusions to prevent stroke, and hydroxyurea), the adult population with SCD is changing and expanding. That is, the data from the ESCAPED trial are a reflection of the survival into adulthood of people living with severe disease. However, the impact of improved pediatric care is unlikely to explain difference in utilization in variant SC disease, in which survival has not changed.
Second, the national approach to pain changed during the era of “pain as the fifth vital sign” initiative. Introduced in 1996 by the American Pain Society, this emphasized the importance of assessing and treating pain appropriately. Providers have become more aggressive and skilled at managing pain in this era. Patients may be better informed about the importance of seeking care and have more confidence that they will receive adequate pain relief. This more aggressive approach to pain management has led to increased access to opioids. One could link increased utilization by patients as being a result of drug seeking behavior. However, although it exists, opioid use disorder in this patient population has been noted to be uncommon in prior studies.10,11 In this era of an opioid epidemic, there are no modern data on opioid use disorder in those with SCD, and further study is required. More study is also needed to better understand whether increased access to opioids at home has increased the risk of developing a chronic pain syndrome that leads to higher utilization, or if access to opioids at home is being used effectively to treat chronic pain.
Thirty-nine percent of the ESCAPED cohort used long-acting opioids, and 56% used short-acting opioids. These findings are similar to those of the PiSCES (Pain in Sickle Cell Epidemiology Study)12 project, a study examining daily pain in people with SCD, with similar rates of long-acting opioid use but a slightly higher number using short-acting opioids in the current study. In PiSCES, 29% of patients reported pain in >95% of diary days13; in the current study, 68% of patients reported chronic daily pain. These differences likely reflect a different measure of chronic daily pain, and further study is needed, using a standardized approach to measuring chronic daily pain.
Although there was a trend toward decreased acute care utilization for those on hydroxyurea, it was not statistically significant. As the primary outcome of the ESCAPED trial is an examination of the quality of acute care, data on hydroxyurea adherence were no collected. Numerous studies note that adherence to hydroxyurea is often poor and that improved adherence is associated with improved outcomes including decreased acute care utilization.14-16 The efficacy of hydroxyurea is well established, and the lack of association of hydroxyurea with acute care utilization likely reflects poor adherence to therapy.
There are a number of limitations to this study. Subjects were identified to have chronic pain by self-report with a question asking if they had chronic daily pain. There is no evidence-based definition of chronic pain for individuals with SCD, but Dampier et al17 have recently suggested diagnostic criteria that can be used in future studies. Another limitation is that we examined associations and not causality; although we saw an association between employment and decreased acute care utilization, it is unclear whether being employed suggests less severe disease and ability to work or reflects people who are more skilled at disease management and reducing acute care utilization.
The finding that a history of chronic pain was associated with a greater number of acute visits is not surprising. What is remarkable is the very high prevalence of chronic pain in this cohort, which we expect is representative of the adult sickle population in the United States. We fear that current approaches to both acute and chronic pain are suboptimal and look forward to the testing of new approaches to pain management in this population of patients.
Acknowledgment
This work was supported by the Patient-Centered Outcomes Research Institute (PCORI; IHS-1403-11888).
Authorship
Contribution: S.L., C.H., J.S., R.V., D.R., M.P., A.K., C.G., L.B., M.W., and M.S. designed the research; S.L., J.L., J.R.S., J.F., and R.S. performed the research; R.S., J.B., B.G., S.F., and A.P. collected data; H.W., C.Y.H., R.V., J.S., S.L., J.L., J.F., and J.R.S. analyzed and interpreted data; and S.L., J.S., and H.W. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Sophie Lanzkron, Johns Hopkins School of Medicine, 1830 E. Monument St, Suite 7300, Baltimore, MD 21205; e-mail: slanzkr@jhmi.edu.
References
- 1.Hassell KL. Population estimates of sickle cell disease in the U.S. Am J Prev Med. 2010;38(4, suppl):S512-S521. [DOI] [PubMed] [Google Scholar]
- 2.Platt OS, Thorington BD, Brambilla DJ, et al. Pain in sickle cell disease. Rates and risk factors. N Engl J Med. 1991;325(1):11-16. [DOI] [PubMed] [Google Scholar]
- 3.Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. Acute care utilization and rehospitalizations for sickle cell disease. JAMA. 2010;303(13):1288-1294. [DOI] [PubMed] [Google Scholar]
- 4.Benjamin LJ, Swinson GI, Nagel RL. Sickle cell anemia day hospital: an approach for the management of uncomplicated painful crises. Blood. 2000;95(4):1130-1136. [PubMed] [Google Scholar]
- 5.Lanzkron S, Carroll CP, Hill P, David M, Paul N, Haywood C Jr. Impact of a dedicated infusion clinic for acute management of adults with sickle cell pain crisis. Am J Hematol. 2015;90(5):376-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Imbach P. Day hospital versus inpatient management: an economic initiative of a pediatric center, examplified on uncomplicated vaso-occlusive crises of children with sickle cell disease. Pediatr Blood Cancer. 2008;51(3):317. [DOI] [PubMed] [Google Scholar]
- 7.Raphael JL, Kamdar A, Beavers MB, Mahoney DH, Mueller BU. Treatment of uncomplicated vaso-occlusive crises in children with sickle cell disease in a day hospital. Pediatr Blood Cancer. 2008;51(1):82-85. [DOI] [PubMed] [Google Scholar]
- 8.Adewoye AH, Nolan V, McMahon L, Ma Q, Steinberg MH. Effectiveness of a dedicated day hospital for management of acute sickle cell pain. Haematologica. 2007;92(6):854-855. [DOI] [PubMed] [Google Scholar]
- 9.Wright J, Bareford D, Wright C, et al. Day case management of sickle pain: 3 years experience in a UK sickle cell unit. Br J Haematol. 2004;126(6):878-880. [DOI] [PubMed] [Google Scholar]
- 10.Britto MT, Garrett JM, Dugliss MA, et al. Risky behavior in teens with cystic fibrosis or sickle cell disease: a multicenter study. Pediatrics. 1998;101(2):250-256. [DOI] [PubMed] [Google Scholar]
- 11.Solomon LR. Treatment and prevention of pain due to vaso-occlusive crises in adults with sickle cell disease: an educational void. Blood. 2008;111(3):997-1003. [DOI] [PubMed] [Google Scholar]
- 12.Smith WR, McClish DK, Dahman BA, et al. Daily home opioid use in adults with sickle cell disease: the PiSCES project. J Opioid Manag. 2015;11(3):243-253. [DOI] [PubMed] [Google Scholar]
- 13.Smith WR, Penberthy LT, Bovbjerg VE, et al. Daily assessment of pain in adults with sickle cell disease. Ann Intern Med. 2008;148(2):94-101. [DOI] [PubMed] [Google Scholar]
- 14.Badawy SM, Thompson AA, Lai JS, Penedo FJ, Rychlik K, Liem RI. Adherence to hydroxyurea, health-related quality of life domains, and patients’ perceptions of sickle cell disease and hydroxyurea: a cross-sectional study in adolescents and young adults. Health Qual Life Outcomes. 2017;15:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou J, Han J, Nutescu EA, Gordeuk VR, Saraf SL, Calip GS. Hydroxycarbamide adherence and cumulative dose associated with hospital readmission in sickle cell disease: a 6-year population-based cohort study. Br J Haematol. 2018;182(2):259-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lanzkron S, Haywood C Jr, Fagan PJ, Rand CS. Examining the effectiveness of hydroxyurea in people with sickle cell disease. J Health Care Poor Underserved. 2010;21(1):277-286. [DOI] [PubMed] [Google Scholar]
- 17.Dampier C, Palermo TM, Darbari DS, Hassell K, Smith W, Zempsky W. AAPT diagnostic criteria for chronic sickle cell disease pain. J Pain. 2017;18(5):490-498. [DOI] [PubMed] [Google Scholar]