Abstract
Objectives
To examine cancer-related worry in adolescent and young adult (AYA) cancer survivors and its relationship with posttraumatic growth over time, as the relationship between these constructs has not been assessed longitudinally in this population.
Methods
153 AYA cancer survivors completed measures of cancer-related worry and posttraumatic growth three times across approximately one year. Descriptive statistics were calculated for cancer-related worry items, and mixed-effects modeling assessed the relationship between cancer-related worry and posttraumatic growth.
Results
Most participants reported at least moderate cancer-related worry in at least one area at each assessment (88.2-93.9% across time points). Worry about future health was the most prevalent concern (65.4%-83.7% across time points). Cancer-related worry was positively related to posttraumatic growth in the mixed-effects model. However, post hoc analyses indicated that cancer-related worry and posttraumatic growth were modestly related; there was no evidence that either construct predicted the other over time.
Conclusions
Cancer-related worry appears to be a common psychosocial outcome in AYA cancer survivors. However, cancer-related worry appears to be only modestly related to the development of posttraumatic growth, implying that these may be independent constructs despite theoretical literature suggesting that posttraumatic growth may stem from posttraumatic distress. Thus it is necessary to assess AYA survivors for cancer-related worry and posttraumatic growth, and develop interventions to target cancer-related worry and foster posttraumatic growth.
Keywords: adaptation, adolescent, anxiety, cancer, oncology, posttraumatic growth, survivors, young adult
Background
Approximately 70,000 adolescents and young adults (AYAs) are diagnosed with cancer in the United States each year,1 and a substantial number of these AYAs will become long-term survivors.2 AYA cancer intersects with a key period in psychosocial development3–5 and often disrupts important developmental tasks, such as education, career pursuits, social relationships, romantic relationships, and plans to start a family. The necessity to rely upon others for help during a time typically marked by increasing individuation and identity development has the potential to have long-lasting psychosocial implications. AYA cancer survivors report a range of psychosocial concerns that are unique to this age group, and they experience complex challenges relating to the transition to survivorship.6 Therefore, it is essential to examine psychosocial outcomes specific to this population in order to develop interventions to alleviate distress and foster positive psychological adaptation following treatment for cancer diagnosed during adolescence or young adulthood. For the purposes of this paper, AYAs were defined as 15- to 25-year-old off-treatment survivors of cancer diagnosed between the ages of 14 and 21.
Posttraumatic Growth
Posttraumatic growth is defined as experiencing positive psychological and psychosocial change as a result of a traumatic life experience.7 In the theoretical literature about posttraumatic growth, Tedeschi and Calhoun7 broadly identify trauma according to Janoff-Bulmann’s conceptualization that trauma is a set of circumstances that significantly challenge an individual’s adaptive resources, while also disrupting the individual’s understanding of the world and his or her place in the world.8 The theory of posttraumatic growth posits that good can come from suffering and can manifest in many ways, including an increased appreciation for life, developing more meaningful interpersonal relationships, a greater sense of personal strength, reorganization of priorities, and a richer existential/spiritual life. Posttraumatic growth appears to be a common phenomenon among AYA cancer survivors, particularly in the areas of relationships with family and peers, future life plans/goals, and health competence.9–11 AYAs may be particularly primed to experience posttraumatic growth because the self-exploration inherent in identity development during this phase12 could lend itself to effective integration of the cancer experience into one’s sense of self.
A review of posttraumatic growth and related constructs across a range of traumatic events, including serious medical conditions, found that individuals who experience posttraumatic growth after a traumatic event report lower distress levels over time.13 Therefore, it is important to examine the processes that contribute to the development of posttraumatic growth in cancer survivors, particularly individuals diagnosed during adolescence or young adulthood. Posttraumatic growth has been linked to a variety of factors, such as resilience, social support, and optimism.14–17 However, Tedeschi and Calhoun theorized that distress following trauma is the primary driver of posttraumatic growth because posttraumatic growth results from psychological processing that occurs during distressed rumination about a highly negative life event.7 They propose that posttraumatic growth develops as individuals attempt to manage their distress and adapt to new circumstances created by the traumatic event. In this theory, the term ‘posttraumatic distress’ is not limited to the symptoms of posttraumatic stress disorder, but rather, includes any form of distress that could occur following a traumatic event, such as depression, anxiety, and worry. Thus, in this paper, the term posttraumatic distress will be used to encompass the broad range of distress that could occur following a traumatic event, whereas the term posttraumatic stress symptoms will be used to describe symptoms specifically associated with posttraumatic stress disorder (PTSD).
Within pediatric and young adult oncology, studies examining the potential relationship between posttraumatic distress and posttraumatic growth have reported conflicting results. Two studies have indicated a positive relationship between posttraumatic stress symptoms and posttraumatic growth.9, 18 In contrast, one study found a modest negative relationship between posttraumatic growth and perceived stress,16 and another found a negative relationship between posttraumatic growth and depression.18 Additionally, two studies found no relationship between posttraumatic stress symptoms and posttraumatic growth, suggesting that perhaps these phenomena are largely independent constructs.19, 20 However, one study reported a curvilinear relationship between re-experiencing symptoms of PTSD and two facets of posttraumatic growth: new possibilities and personal strengths, such that individuals reporting moderate levels of re-experiencing reported higher levels of posttraumatic growth than individuals reporting high levels of re-experiencing.21 The findings suggesting the possibility of a curvilinear relationship between posttraumatic distress and posttraumatic growth are consistent with findings presented in the broader posttraumatic growth literature.22
The conflicting literature in this area contains several limitations. First, the vast majority of studies examine only posttraumatic stress symptoms, whereas the theoretical literature defines posttraumatic distress more broadly to include other forms of distress.7 Therefore, it is possible that posttraumatic stress symptoms are not the most thorough examination of posttraumatic distress and should be broadened. Second, most studies assessed only linear relationships between posttraumatic distress and posttraumatic growth when there is evidence that the relationship between these constructs may be quadratic, due to a curvilinear relationship.21, 22 Additional research is needed to explore these limitations.
Cancer-Related Worry
Worry is a form of distress that has been defined as a cognitive process in which people feel anxious due to concerns regarding uncertainty about the future and the possibility of negative events.23 In qualitative studies, AYA survivors have described concerns about fertility, the possibility of recurrence, late effects of treatment, finances, employment options, and the transition to more independent life after treatment completion.24–26 In one study, investigators assessed cancer-related worry in a Canadian sample of AYA survivors of pediatric cancer as part of a scale development project.27, 28 This study found that more than half of survivors were worried about their risk of late effects of their cancer treatment, while slightly less than half the sample worried about fertility, risk of recurrence, or risk of developing a new cancer. Almost half of the participants reported that cancer was always at the back of their minds, and a small portion of survivors reported worrying about cancer every day. Females reported more worry than males, and survivors who had received more intensive treatment worried more than those who received less intensive treatment. Additionally, about one third of the sample reported worrying about the risk of developing a new cancer or about fertility when they were not at high risk for those effects. Another quantitative study indicated that substantial numbers of AYAs with, or in remission from, cancer have worries about death and dying.29
Although such worries are common among cancer survivors of all ages, they may be particularly acute for individuals who experience them in emerging adulthood, a time when people typically work toward financial stability, consider starting families, and become more independent through career and educational pursuits. The worries described by AYA cancer survivors reflect Tedeschi and Calhoun’s proposed process of re-evaluating one’s view of oneself and one’s place in the world.7 AYA survivors’ worries indicate the process of learning to live in a world where perhaps they cannot have their own biological children through natural means, if at all; a world where they may feel like perpetual patients due to late effects of treatment and the possibility of recurrence; a world where their financial and career trajectories are thrown off track. As such, these worries should be considered as potential drivers of the development of posttraumatic growth.
Despite its prevalence in the qualitative literature, quantitative information about cancer-related worry is limited. Most studies addressing AYAs’ cancer-related worries describe their relationship to other outcomes without including descriptive information about cancer-related worry,30, 31 and these studies typically include current AYAs who were diagnosed at any age, rather than those diagnosed specifically during adolescence or young adulthood. 27, 28, 30–32 Thus, it is important to report descriptive information about the prevalence of cancer-related worries in survivors of cancer diagnosed in adolescence or young adulthood, as this is a unique period of psychosocial development.3–5
Aims and Hypotheses
The aims of this study were to use quantitative methods to describe AYAs’ cancer-related worries and to longitudinally examine the relationship cancer-related worry may have with posttraumatic growth. With regard to the first aim, it was predicted that the majority of survivors would report at least moderate cancer-related worry in at least one domain (e.g., fertility concerns, fear of recurrence, worry when attending cancer-related follow-up visits), with few survivors indicating worry across all measured domains. This prediction was based on the prominence of cancer-related worry as an emergent theme in the qualitative literature (e.g., 24–26, 33, 34) and prior research with AYA survivors of pediatric cancer.28 For the second aim, it was predicted that individuals reporting moderate levels of cancer-related worry would experience more posttraumatic growth over time than either those reporting low cancer-related worry or those reporting high levels of cancer-related worry, thus resulting in a quadratic relationship between cancer-related worry and posttraumatic growth. This hypothesis was based on the literature suggesting a quadratic relationship between posttraumatic distress and posttraumatic growth.21, 22
Methods
Procedure
This project is part of a larger study at a large urban medical center investigating identity development in AYA survivors of cancer diagnosed during adolescence or young adulthood. Following approval by the Institutional Review Board at Memorial Sloan Kettering Cancer Center (Protocol #09-001), potential participants were identified through the hospital’s medical records database. Participants’ eligibility included: 1) current age 15-25; 2) first cancer diagnosis at age 14-21; 3) at least six months post-treatment; 4) able to provide consent if aged 18 or older, or able to provide assent in combination with parental consent if under the age of 18; 5) English-speaking. Survivors with cognitive impairment, as identified by their primary physicians, were excluded if the impairment was severe enough to preclude them from being able to provide informed consent/assent or complete the study assessments.
Eligible survivors received a letter from the principal investigator outlining the purpose of the study and inviting their participation. The letter was accompanied by an informed consent document, sample questionnaire, and a postage-paid envelope to return all completed documents. A research assistant contacted survivors (or their parents, in the case of minors) by phone if they had not responded to the letter within two weeks and obtained informed consent from interested survivors above the age of 18, and assent and parental consent for survivors younger than 18. Assessments took place by phone or through a paper survey sent either by mail or secure email by a trained research assistant. Participants were assessed at three time points, which were scheduled approximately six to eight months apart. This time period was chosen because it was considered appropriate for assessment of subtle changes over time. All measures utilized for this study were administered at all time points.
Participants
A total of 453 AYAs were screened for eligibility, and 382 were determined to be eligible. The study team was able to contact 221 survivors. Sixty-eight survivors declined to participate. For survivors who provided a refusal reason, reasons included: too busy (n = 15), not interested (n=22), not comfortable (n=16), and privacy concerns (n=1). The final sample consists of 153 survivors. Participants had an average age of 21.8 years (SD=2.6 years; Range=16.2-25.9 years) at study enrollment. 58.2% were male (n=89), and 86.9% were non-Hispanic White (n=133). See Table 1 for demographic and medical characteristics of the sample.
Table 1.
Demographic and Medical Characteristics (n = 153)
| N (%) or Variable Mean (SD; range) | |
|---|---|
| Age at Baseline (years) | 21.8 (2.6; 16 - 25) |
| Age at Diagnosis (years) | 16.8 (1.9; 14 – 20) |
| Time Since Diagnosis (months) | 54.4 (24.8; 10 – 120) |
| Time Since Treatment Completion (months) | 44.1 (24.2; 6 – 100) |
| Gender | |
| Male | 89 (58.2) |
| Female | 64 (41.8) |
| Race/Ethnicity | |
| White | 140 (91.5) |
| Black/African American | 6 (3.9) |
| American Indian/Alaska Native | 2 (1.3) |
| Asian/Pacific Islander | 2 (1.3) |
| Other | 3 (2.0) |
| Current Grade in School if a Student | |
| 10th Grade | 1 (.9) |
| 11th Grade | 3 (2.8) |
| 12th Grade | 9 (8.5) |
| 2 yr College | 7 (6.6) |
| 4 yr College | 70 (66.0) |
| Graduate School | 10 (9.4) |
| Other | 6 (5.7) |
| Highest Grade Completed if not a Student | |
| 12th Grade | 4 (8.5) |
| Some of a 2 yr college | 1 (2.1) |
| Graduated from a 2 yr college | 3 (6.4) |
| Some of a 4 yr college | 6 (12.8) |
| Graduated from a 4 yr college | 28 (59.6) |
| Completed Graduate School | 2 (4.3) |
| Completed training other than college | 1 (2.1) |
| Other | 2 (4.3) |
| Employment Status | |
| Employed (Full Time) | 44 (28.8) |
| Employed (Part Time) | 49 (32.0) |
| On Leave/Disability | 2 (1.3) |
| Unemployed but looking | 23 (15.0) |
| Unemployed not looking | 34 (22.2) |
| Other | 1 (0.7) |
| Diagnosis | |
| Carcinoma | 1 (0.7) |
| Germ Cell | 23 (15.0) |
| Leukemia | 9 (5.9) |
| Lymphoma | 52 (34.0) |
| Sarcoma | 38 (24.8) |
| Other | 30 (19.6) |
| Treatment | |
| Chemotherapy | 118 (77.1) |
| Radiation Therapy | 65 (42.5) |
| Surgery | 121 (79.1) |
| Multimodal | 112 (73.2) |
Analysis of available demographic information for non-participants showed that the sample did not differ from participants with regard to diagnosis, gender, or time since treatment completion. However, there were significant differences with regard to age. At the time of baseline or refusal, participants were significantly older than non-participants, who had a mean age of 20.5 (SD=3.0), (t (219)=3.28, p=.001). Participants were also older than non-participants (M=16.2, SD=1.8) at time of diagnosis, (t (212)=2.24, p=.03). Given the cited reasons for refusal and the significant age difference between participants and non-participants, it appears that younger AYA survivors may have been less interested in participating in research and had more time constraints prohibiting participation than older AYA survivors.
Measures
Demographic variables
Sociodemographic information was collected by participant self-report and through review of medical records. Disease and treatment information were obtained from survivors’ medical records.
Posttraumatic growth
Posttraumatic growth was assessed using the Posttraumatic Growth Inventory (PTGI),35 a 21-item scale assessing positive outcomes reported by people who have experienced traumatic events. Areas assessed by the PTGI include: relating to others, new possibilities, personal strength, spiritual change, and appreciation of life. Items are rated on a six-point Likert scale ranging from 0=I did not experience this to 5=I experienced this change to a very great degree. The total score is the sum of all items, and the subscale scores are the sum of all items included in the subscale. The phrase, “as a result of my cancer diagnosis and/or treatment” was added to instructions to tailor the scale to the cancer experience. The PTGI has demonstrated good convergent and construct validity, as well as good reliability (overall α=.90, factors ranged from .67-.85). In this sample, all subscales showed significant moderate-high correlations with one another (r=.41-.72) and the total score showed good reliability (α=.94 at baseline); therefore, the total score was used in all analyses.
Cancer-Related Worry
As no scale measuring cancer-related worry had been published at the time this data was collected, the research team developed a preliminary cancer-related worry scale. The research team developed seven individual items assessing cancer-related worries pertinent to AYAs (see Appendix A). As recommended by Streiner, Norman, and Cairney, 36 these questions were developed from an earlier qualitative phase of this study in which 26 semi-structured individual interviews (90 minutes in length) and four focus groups (n=17) were conducted by a combination of a trained research assistant, a qualitative methods specialist, and the principal investigator. Interviews and focus groups utilized interview guides containing topics and probes developed based on themes derived from the literature and clinical practice (JSF). Interviews were audio-recorded, transcribed, and imported into ATLAS.ti as part of the larger study, and analyses were guided by grounded theory and thematic content with an inductive data-driven approach. Interviews were independently coded by four trained coders. For more detailed information on the qualitative part of the study, see Barnett, Shuk, Conway, Ford 37 and Benedict, Shuk, Ford 38 The resulting items fell into five domains: worry about recurrence, general worry about future health, worry about fertility, sense of vulnerability, and experiencing distress due to reminders of the cancer experience. When appropriate, items were reverse scored so higher scores would indicate greater distress. Items 3 and 4 were reverse scores of the same general idea (worry about future health) and responses were highly correlated (r=.59; p<.001 at baseline); therefore, they were combined into one item by calculating the mean of the two items after score reversal. Items were then summed to create a total cancer-related worry score (possible range 5-26). The cancer-related worry scale had acceptable reliability at Times 1 (α=.70) and 2 (α=.74), and approached acceptable reliability at Time 3 (α=.62).
Analysis Plan
Means and standard deviations were calculated for all cancer-related worry items. The percentage of participants indicating at least moderate distress on each item was also calculated. Moderate distress was indicated by a score of 4 out of 5. Finally, the number of worries endorsed was calculated for each participant.
Mixed-effects modeling was used to assess the relationship between cancer-related worry and posttraumatic growth across the three time points.39 This longitudinal analysis is robust in its approach toward missing data, as it accounts for intra-individual outcome correlations resulting from repeated assessments, and it allows the number of repeated assessments to vary across individuals. Schwartz’s Bayesian Criterion (BIC) was examined for posttraumatic growth to assess the nature of change of posttraumatic growth over time. Given the wide range of variables that have been associated with the current variables of interest in the existing literature, all demographic, disease, and treatment-related variables that were significantly correlated with either cancer-related worry or posttraumatic growth at any time point were regressed on posttraumatic growth, and a backward elimination process was used in which the variable with the highest p-value was eliminated at each step until only variables with p-values less than or equal to .05 were remained. Remaining variables were entered as covariates in the final model predicting posttraumatic growth from cancer-related worry and cancer-related worry × time. Potential covariates assessed included gender, chemotherapy, radiation therapy, surgery, current age, age at diagnosis, and time since diagnosis. The intercept was entered as a random effect, and all predictor variables were entered as fixed effects.
Results
Missing Data
All 153 survivors completed the baseline questionnaire, 121 survivors completed questionnaires at Time 2 and 119 survivors completed questionnaires at Time 3. Participants who completed all three assessments did not differ significantly from those who completed 1-2 assessments with regard to gender, ethnicity, diagnosis, current age, age at diagnosis, time since diagnosis, time since completing treatment, treatment type, baseline cancer-related worry score, or baseline posttraumatic growth score.
Aim 1: Description of Cancer-Related Worries
Mean cancer-related worry scores across the three time points were 14.59 (SD=4.38), 14.47 (SD=4.27), and 14.56 (SD=3.94), respectively. Descriptive statistics for items included in the total cancer-related worry score are presented in Table 2. Worry about future health was the most prevalent concern across all time points, with means ranging from 4.03 to 4.16 and a modal score of 4 (moderate disagreement with not worrying about future health) on a scale of 1-5 at all time points. The majority of participants (65.4%-83.7% across all time points) reported at least moderate worry about their future health and how their cancer treatment may affect their health as they get older. The prevalence of other worries ranged from 27.5% to 47.4% across the three time points. The majority of participants endorsed moderate cancer-related worry in 1-3 domains at each time point. The number of participants not endorsing at least moderate cancer-related worry in any domain ranged from 6.1% to 11.8% across the three time points, and the number of participants endorsing at least moderate cancer-related worry in all five domains ranged from 5.0% to 12.6%.
Table 2.
Descriptive Information for Cancer-Related Worry Items
| Items Included in Total Cancer-Related Worry Score | Mean (SD) Mode T1 |
% ≥ Moderate Distress T1 |
Mean (SD) Mode T2 |
% ≥ Moderate Distress T2 |
Mean (SD) Mode T3 |
% ≥ Moderate Distress T3 |
|---|---|---|---|---|---|---|
| 1. I come across things in my everyday life that remind me of certain aspects of my cancer experience and make me anxious and/or upset. † | 2.72 (1.28) 4 |
32.7% | 2.65 (1.27) 2 |
31.1% | 2.57 (1.17) 2 |
27.5% |
| 2. Having had cancer has made me feel that I am vulnerable and that bad things can happen to me at any time. † | 2.80 (1.34) 2 |
35.1% | 2.76 (1.30) 2 |
32.7% | 3.02 (1.31) 4 |
47.4% |
| 3. I worry about how receiving cancer treatment may affect my health as I get older. † | 3.60 (1.25) 4 |
65.4% | 3.77 (1.17) 4 |
72.3% | 3.78 (1.15) 4 |
74.2% |
| 4. I don’t worry about my future health. | 4.14 (1.07) 5 |
77.7% | 4.03 (1.04) 4 |
79.8% | 4.16 (.98) 5 |
83.7% |
| 5. I worry about the effect that cancer has had on my fertility and my ability to have children. † | 2.90 (1.43) 3 |
34.0% | 2.95 (1.21) 3 |
33.6% | 2.97 (1.28) 3 |
35.4% |
| 6. How often do you feel anxious or worried about getting cancer again (responses 1-6)? † | 2.28 (1.46) 3 |
45.4% | 2.21 (1.34) 2 |
41.9% | 2.15 (1.34) 2 |
38.6% |
Note: Moderate distress indicated by a score of 4 (Moderately Agree/Moderately Disagree/Often/Monthly)
Reverse scored so higher scores indicate higher distress
Aim 2: The Relationship Between Cancer-Related Worry and Posttraumatic Growth
Mean posttraumatic growth scores across the three time points were 68.25 (SD=20.19), 66.50 (SD=17.92), and 66.16 (SD=18.85), respectively. Based on a comparison of BIC for linear (BIC=3065.52) and quadratic (BIC=3070.07) models, it was determined that a linear model best described the change in posttraumatic growth over time and the quadratic time term was not included in the final model. Estimates of fixed effects are presented in Table 3. Cancer-related worry had a significant, positive effect on change in posttraumatic growth (p=.01), and time had a significant, negative effect (p=.02). The cancer-related worry × time effect was not significant (p=.25), indicating that change in cancer-related worry over time did not predict posttraumatic growth. Age at diagnosis showed a significant, negative effect (p<.001), and a history of chemotherapy treatment had a significant positive effect (p=.01). The effects of gender and surgical treatment did not remain significant after adding cancer-related worry to the model.
Table 3.
Mixed Effects Model Predicting Posttraumatic Growth from Total Cancer-Related Worry Score
| Variable | Estimate | SE | t | p Value |
|---|---|---|---|---|
| Cancer-Related Worry | .61 | .25 | 2.49 | .01 |
| Time† | −.96 | .41 | −2.34 | .02 |
| Male Gender | −5.13 | 2.67 | −1.92 | .06 |
| Age at Diagnosis‡ | −2.99 | .68 | −4.41 | <.001 |
| Chemotherapy | 8.42 | 3.16 | 2.67 | .01 |
| Surgery | .40 | .23 | 1.72 | .09 |
| Cancer-Related Worry × Time | .03 | .03 | 1.16 | .25 |
in months;
centered to create a meaningful intercept
Post Hoc Analyses
To further understand the relationship between cancer-related worry and posttraumatic growth across the three time points, cross-lagged correlations were calculated, partialling out the effect of demographic, disease, and treatment variables that were included in the primary analyses (see Figure 1). Contrary to expectations, initial posttraumatic growth appeared to predict cancer-related worry over time, as Time 2 posttraumatic growth was modestly, but significantly, positively correlated with Time 3 cancer-related worry (r=.20, p=.05). However, Fisher z-transformations indicated that there was not a significant difference in the magnitude of the correlations for posttraumatic growth predicting cancer-related worry and the correlations for cancer-related worry predicting posttraumatic growth.
Figure 1.
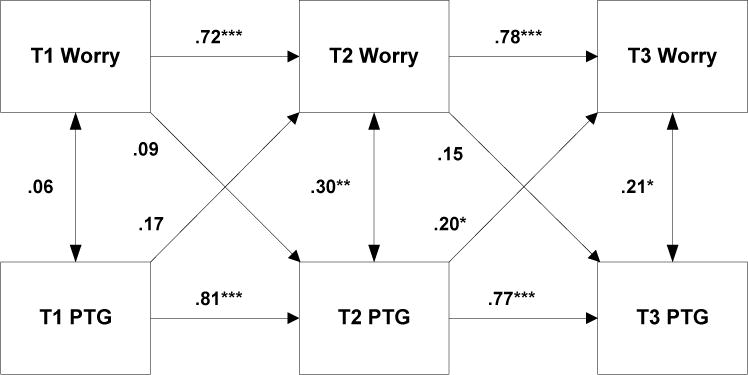
Cross-Lagged Partial Correlations Between cancer-related worry and posttraumatic growth (PTG)
*p ≤ .05; **p ≤ .01; ***p ≤ .001
Note: The following variables were partialled out: gender, age at diagnosis, chemotherapy treatment, surgery
Additionally, bivariate correlations were conducted to more fully understand the effects of covariates on cancer-related worry. Cancer-related worry was modestly, but significantly, negatively related to time since diagnosis and time since completing treatment at all time points (r’s=−.20 to −.30; p’s=.002 to .021) with the exception of the relationship between worry and time since diagnosis at Time 3 (p>.05). There was little indication of a relationship between age at diagnosis and cancer-related worry, with a modest significant correlation emerging only at Time 1 (r=.20, p=.02). Cancer-related worry was also not associated with age at baseline. Similarly, posttraumatic growth was not significantly related to time since diagnosis or time since treatment completion.
Conclusions
Although cancer-related worry is commonly discussed in the qualitative literature,24, 26, 33 it has rarely been examined quantitatively in the AYA population. Similarly, posttraumatic growth is a documented phenomenon among various groups of trauma survivors, including AYA cancer survivors, 9–11 yet little is understood about its theorized relationship with posttraumatic distress in this population. 7 This study is one of the first to quantitatively describe cancer-related worry in this population and the first to examine the relationship between cancer-related worry and posttraumatic growth. This is also the first study to examine the relationship between posttraumatic growth and posttraumatic distress longitudinally in this population.
As hypothesized, cancer-related worry was prevalent in this sample and few participants endorsed cancer-related worry in all domains. These results tentatively confirm qualitative evidence that cancer-related worry is a common psychosocial outcome for AYAs following treatment completion,24–26 and that most survivors do not experience all cancer-related worries.40 However, each of the worries assessed was endorsed by sizeable portions of the sample, suggesting that AYAs experience a range of cancer-related worries, with concerns about future health emerging as a prominent concern. These results are relatively consistent with the worries reported by AYA survivors of pediatric cancer.28
In the mixed-effects model, cancer-related worry was a significant predictor of posttraumatic growth across the three time points, as hypothesized. However, contrary to existing evidence that the relationship between posttraumatic distress and posttraumatic growth may be quadratic,22 a linear model was the best fit for the relationship between cancer-related worry and posttraumatic growth in this sample. Therefore, the results of the mixed-effects model initially appeared to support Tedeschi and Calhoun’s theory that posttraumatic growth stems from cognitive processing that takes place during distressed rumination with higher levels of distress predicting higher levels of posttraumatic growth.7 It is notable that in this sample, age at diagnosis was the strongest predictor of posttraumatic growth, with survivors diagnosed at younger ages reporting higher levels of posttraumatic growth. One possible explanation for this finding is that it could be related to the developmental task of identity development, such that older AYAs are more likely than younger AYAs to be in the phase of identity achievement (i.e., commitment to a set of goals, values, and life choices following a period of self-exploration).12, 41 It may be easier to experience and recognize positive changes as a result of cancer before one has fully committed to goals, values, and life choices that are likely to be disrupted by the cancer experience.
Despite initial results appearing to support Tedeschi and Calhoun’s theory of posttraumatic growth,7 post hoc cross-lagged correlation coefficients indicated only a modest relationship between cancer-related worry and posttraumatic growth over time, and there was no significant difference between the effect of cancer-related worry on posttraumatic growth and the effect of posttraumatic growth on worry. Thus, it appears that cancer-related worry and posttraumatic growth may be independent constructs in this population, a hypothesis that has also been proposed in reference to the relationship between posttraumatic stress symptoms and posttraumatic growth.19, 20
In this context, it is possible that a different theory of managing stressful life events may better capture the experience of AYA cancer survivors. For example, the Social-Cognitive Transition Model of Adjustment42 draws upon social-cognitive theories (e.g., 7) and coping theory43 to explain positive and negative adaptations to cancer that occur within the context of a person’s pre-developed beliefs and current environment. This theory identifies several domains that are commonly challenged by a cancer diagnosis, each of which could result in a positive transition (e.g., posttraumatic growth) or a negative transition (e.g., distress). Identified domains include life trajectory, self-control, self-worth, attachments, and spiritual/existential life. Challenges to different domains could result in different outcomes (i.e., positive transitions versus negative transitions) depending upon the person’s pre-determined beliefs about a particular domain and the environment’s response to the effect of cancer on that particular domain. This theory allows for the co-occurrence of distress and posttraumatic growth without tying these concepts to one another in a causal fashion. Thus, the Social-Cognitive Transition Model of Adjustment may better account for the findings of the current study.
Alternatively, it is possible that results were affected by the timing of assessments. Perhaps a relationship between cancer-related worry and posttraumatic growth would have emerged had assessments begun shortly after diagnosis or treatment completion, allowing for examination of how these constructs unfolded over time from an earlier baseline.
Study Limitations
This study was limited by a relatively small sample and high rates of missing data, which are common challenges of working with this population, particularly with regard to longitudinal assessments. It is possible that a larger sample would have allowed for the emergence of additional patterns that were not significant in this study, such as significant effects for time since diagnosis or time since treatment. Similarly, it should be noted that without normative data for this population, it is unclear if this sample’s cancer-related worry and posttraumatic growth distributions are representative of the general population of AYA cancer survivors. For instance, this sample was predominantly White, so it is unclear if these results are generalizable to AYA survivors of other racial or ethnic backgrounds.
Additionally, this study did not assess some factors that could affect cancer-related worry and posttraumatic growth, such as receipt of a survivorship care plan, the intensity of treatment, or experiencing a previous trauma. Finally, although the cancer-related worry scale demonstrated adequate reliability, it was a preliminary effort at measuring this construct and, thus, was not subjected to the rigorous psychometric evaluation necessary for formal scale development. However, it is notable that this preliminary scale was extremely similar to a recently published scale that was subjected to more rigorous psychometric evaluation,27 thus providing support for the face validity of the current items.
Clinical Implications
Cancer-related worry has been found to be related to anxiety and depression in cancer survivors,44 and, thus, could be an important target for interventions given its prevalence among AYA survivors. As recommended in the Standards for Psychosocial Care of Children with Cancer and Their Families,45 ongoing assessment is necessary to screen for the development of distress, such as cancer-related worry, and appropriate interventions should be provided to address these concerns as they arise. Additionally, posttraumatic growth has been linked to lower levels of distress over time and interventions to promote posttraumatic growth may be useful in fostering positive adaptation following treatment. Appropriate interventions might include cognitive behavioral therapy to target cancer-related worry, tasks to promote the development of posttraumatic growth (e.g., specifically asking survivors to reflect upon positive changes that may have occurred as a result of their cancer diagnoses), or helping AYA survivors develop and maintain a support network to help them manage cancer-related difficulties should they arise.
Future Directions
Additional research should be conducted to validate, and perhaps expand upon, a previously developed cancer-related worry scale, such as the one developed by Klassen and colleagues,27, 28 with a sample of AYA survivors diagnosed during adolescence or young adulthood. Additionally, given the screening recommendations proposed in the Standards for Psychosocial Care of Children with Cancer and Their Families,45 and the documented relationship between cancer-related worry and adverse psychosocial outcomes among cancer survivors,44 it is important to incorporate assessment of cancer-related worry into routine psychosocial screening for AYA survivors. Similarly, future research should examine the role of other variables that have been linked to posttraumatic growth in other populations of cancer patients and survivors, such as resilience, social support, and optimism.14–17
Further, given that few survivors endorsed cancer-related worry in all domains, future research should aim to determine if there are particular groups of AYA survivors for whom different cancer-related worry domains are particularly relevant and if there are specific cancer-related worries that are tied to relevant psychosocial outcomes, such as depression, or anxiety. Finally, it is necessary to gain a broader perspective on how these results fit into the overall cancer experience, from treatment through long-term survivorship, and assess how factors such as treatment intensity, receipt of a cancer survivor healthcare plan, and involvement in long-term follow-up care programs may affect cancer-related worry and posttraumatic growth after ending active treatment.
Acknowledgments
This work was supported by the American Cancer Society (grant number MRSG-07-165-01-CPPB to JSF), and the National Cancer Institute at the National Institutes of Health (grant 5T32CA00946-32 supporting GAM, PI: JSO; grant P30 CA008748 PI: CT).
Appendix A
Cancer-Related Worry Items
| Item | Response Options |
|---|---|
| 1. I come across things in my everyday life that remind me of certain aspects of my cancer experience and make me anxious and/or upset. † | 1 = Strongly Agree 2 = Moderately Agree 3 = Neither Agree nor Disagree 4 = Moderately Disagree 5 = Strongly Disagree |
| 2. Having had cancer has made me feel that I am vulnerable and that bad things can happen to me at any time. † | |
| 3. I worry about how receiving cancer treatment may affect my health as I get older. † | |
| 4. I don’t worry about my future health. | |
|
| |
| 5. I worry about the effect that cancer has had on my fertility and my ability to have children. † | 1 = Frequently 2 = Often 3 = Sometimes 4 = Rarely 5 = Never |
|
| |
| 6. How often do you feel anxious or worried about getting cancer again? Check all that apply.† | 1 = Daily 2 = Weekly 3 = Monthly 4 = About once every six months 5 = About once a year 6 = Never |
Reverse scored when calculating total cancer-related worry scale
Footnotes
Conflict of Interest Statement
None of the authors have any conflicts of interest to report.
References
- 1.Howlander N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2013. Bethesda, MD: National Cancer Institute; 2016. [Google Scholar]
- 2.Bleyer A. Latest estimates of survival rates of the 24 most common cancers in adolescent and young adult Americans. Journal of Adolescent and Young Adult Oncology. 2011;1:37–42. doi: 10.1089/jayao.2010.0005. [DOI] [PubMed] [Google Scholar]
- 3.Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–480. [PubMed] [Google Scholar]
- 4.Erikson EH. Identity and the Life Cycle. New York, NY: International Universities Press; 1959. [Google Scholar]
- 5.Steinberg L, Morris AS. Adolescent development. Annu Rev Psychol. 2001;52:83–110. doi: 10.1146/annurev.psych.52.1.83. [DOI] [PubMed] [Google Scholar]
- 6.Barnett M, McDonnell G, DeRosa A, et al. Psychosocial outcomes and interventions among cancer survivors diagnosed during adolescence and young adulthood (AYA): A systematic review. J Cancer Surviv. 2016 doi: 10.1007/s11764-016-0527-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tedeschi RG, Calhoun LG. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychol Inq. 2004;15:1–18. [Google Scholar]
- 8.Janoff-Bulman R. Shattered Assumptions. New York, NY: Free Press; 1992. [Google Scholar]
- 9.Barakat LP, Alderfer MA, Kazak AE. Posttraumatic growth in adolescent survivors of cancer and their mothers and fathers. J Pediatr Psychol. 2006;31:413–419. doi: 10.1093/jpepsy/jsj058. [DOI] [PubMed] [Google Scholar]
- 10.Bellizzi KM, Smith A, Schmidt S, et al. Positive and negative psychosocial impact of being diagnosed with cancer as an adolescent or young adult. Cancer. 2012;118:5155–5162. doi: 10.1002/cncr.27512. [DOI] [PubMed] [Google Scholar]
- 11.Park CL, Chmielewski J, Blank TO. Post-traumatic growth: finding positive meaning in cancer survivorship moderates the impact of intrusive thoughts on adjustment in younger adults. Psychooncology. 2010;19:1139–1147. doi: 10.1002/pon.1680. [DOI] [PubMed] [Google Scholar]
- 12.Marcia JE. Development and validation of ego identity status. J Pers Soc Psychol. 1966;3:551–558. doi: 10.1037/h0023281. [DOI] [PubMed] [Google Scholar]
- 13.Linley PA, Joseph S. Positive change following trauma and adversity: A review. J Trauma Stress. 2004;17:11–21. doi: 10.1023/B:JOTS.0000014671.27856.7e. [DOI] [PubMed] [Google Scholar]
- 14.Büyükaşik-Colak C, Gündoğdu-Aktürk E, Bozo O. Mediating role of coping in the dispositional optimism-posttraumatic growth relation in breast cancer patients. The Journal of Psychology. 2012;146:471–483. doi: 10.1080/00223980.2012.654520. [DOI] [PubMed] [Google Scholar]
- 15.Dong X, Li G, Liu C, et al. The mediating role of resilience in the relationship betwen social support and posttraumatic growth among colorectal cancer survivors with permanent intestinal ostomies: A structural equation model analysis. Eur J Oncol Nurs. 2017;29:47–52. doi: 10.1016/j.ejon.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 16.Love C, Sabiston CM. Exploring the links between physical activity and posttraumatic growth in young adult cancer survivors. Psychooncology. 2011;20:278–286. doi: 10.1002/pon.1733. [DOI] [PubMed] [Google Scholar]
- 17.Park JH, Jung YS, Jung Y. Factors influencing posttraumatic growth in survivors of breast cancer. Journal of Korean Academic Nursing. 2016;46:454–462. doi: 10.4040/jkan.2016.46.3.454. [DOI] [PubMed] [Google Scholar]
- 18.Arpawong TE, Oland A, Milam JE, Ruccione K, Meeske KA. Post-traumatic growth among an ethnically diverse sample of adolescent and young adult cancer survivors. Psychooncology. 2013;22:2235–2244. doi: 10.1002/pon.3286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klosky JL, Krull KR, Kawashima T, et al. Relations between posttraumatic stress and posttraumatic growth in long-term survivors of childhood cancer: A report from the childhood cancer survivor study. Health Psychol. 2014;33:878–882. doi: 10.1037/hea0000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tillery R, Howard Sharp KM, Okado Y, Long A, Phipps S. Profiles of resilience and growth in youth with cancer and healthy comparisons. J Pediatr Psychol. 2016;41:290–297. doi: 10.1093/jpepsy/jsv091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zebrack B, Kwak M, Salsman J, et al. The relationship between posttraumatic stress and posttraumatic growth among adolescent and young adult (AYA) cancer patients. Psychooncology. 2015;24:162–168. doi: 10.1002/pon.3585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shakespeare-Finch J, Lurie-Beck J. A meta-analytic clarification of the relationship between posttraumatic growth and symptoms of posttraumatic distress disorder. J Anxiety Disord. 2014;28:223–229. doi: 10.1016/j.janxdis.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 23.MacLeod AK, Williams JMG, Bekerian DA. Worry is reasonable: The role of explanations in pessimism about future personal events. J Abnorm Psychol. 1991;100:478–486. doi: 10.1037//0021-843x.100.4.478. [DOI] [PubMed] [Google Scholar]
- 24.D’Agostino NM, Edelstein K. Psychosocial challenges and resource needs of young adult cancer survivors: implications for program development. J Psychosoc Oncol. 2013;31:585–600. doi: 10.1080/07347332.2013.835018. [DOI] [PubMed] [Google Scholar]
- 25.Gorman JR, Usita PM, Madlensky L, Pierce JP. Young breast cancer survivors: their perspectives on treatment decisions and fertility concerns. Cancer Nurs. 2011;34:32–40. doi: 10.1097/NCC.0b013e3181e4528d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keim-Malpass J, Baernholdt M, Erickson JM, Ropka ME, Schroen AT, Steeves RH. Blogging through cancer: young women’s persistent problems shared online. Cancer Nurs. 2013;36:163–172. doi: 10.1097/NCC.0b013e31824eb879. [DOI] [PubMed] [Google Scholar]
- 27.Klassen AF, Rosenberg-Yunger ZRS, D’Agostino NM, et al. The development of scales to measure childhood cancer survivors’ readiness for transition to long-term follow-up care as adults. Health Expect. 2014;18:1941–1955. doi: 10.1111/hex.12241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang R, Syed IA, Nathan PC, Barr RD, Rosenberg-Yunger ZRS, Klassen AF. Exploring cancer worry in adolescent and young adult survivors of childhood cancers. Journal of Adolescent and Young Adult Oncology. 2015;4:192–199. doi: 10.1089/jayao.2015.0029. [DOI] [PubMed] [Google Scholar]
- 29.Hølge-Hazelton B, Timm HU, Graugaard C, Boisen KA, Sperling CD. “Perhaps I will die young.” Fears and worries regarding disease and death among Danish adolescents and young adults with cancer. A mixed method study. Support Care Cancer. 2016 doi: 10.1007/s00520-016-3322-z. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 30.Cox CL, McLaughlin RA, Steen BD, Hudson MM. Predicting and modifying substance use in childhood cancer survivors: Application of a conceptual model. Oncol Nurs Forum. 2006;33:51–60. doi: 10.1188/06.ONF.51-60. [DOI] [PubMed] [Google Scholar]
- 31.Cox CL, Montgomery M, Rai SN, McLaughlin R, Steen BD, Hudson MM. Supporting breast self-examination in female childhood cancer survivors: A secondary analysis of a behavioral intervention. Oncol Nurs Forum. 2008;35:423–430. doi: 10.1188/08.ONF.423-430. [DOI] [PubMed] [Google Scholar]
- 32.Weigers ME, Chester MA, Zebrack BJ, Goldman S. Self-reported worries among long-term survivors of childhood cancer and their peers. J Psychosoc Oncol. 1999;16:1–23. [Google Scholar]
- 33.Carpentier MY, Fortenberry JD, Ott MA, Brames MJ, Einhorn LH. Perceptions of masculinity and self-image in adolescent and young adult testicular cancer survivors: Implications for romantic and sexual relationships. Psychooncology. 2011;20:738–745. doi: 10.1002/pon.1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thompson AL, Long KA, Marsland AL. Impact of childhood cancer on emerging adult survivors’ romantic relationships: a qualitative account. J Sex Med. 2013;10(Suppl 1):65–73. doi: 10.1111/j.1743-6109.2012.02950.x. [DOI] [PubMed] [Google Scholar]
- 35.Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J Trauma Stress. 1996;9:455–471. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- 36.Streiner DL, Norman GR, Cairney J. Health measurement scales: A practical guideto their development and use. 5. Oxford, United Kingdom: Oxford University Press; 2015. [Google Scholar]
- 37.Barnett M, Shuk EM, Conway FP, Ford JS. Cancer-related disclosure among adolescent and young adult cancer survivors: A qualitative study. Journal of Adolescent & Young Adult Oncology. 2014;3:123–129. doi: 10.1089/jayao.2013.0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Benedict C, Shuk E, Ford JS. Fertility Issues in Adolescent and Young Adult Cancer Survivors. Journal of Adolescent and Young Adult Oncology. 2016;5:48–57. doi: 10.1089/jayao.2015.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Raudenbush SW, Bryk AS. Hierarchical linear models. Newbury Park, CA: Sage; 2002. [Google Scholar]
- 40.Stefanek ME, Shaw A, Degeorge D, Tsottles N. Illness-related worry among cancer patients: Prevalence, severity, and content. Cancer Invest. 1989;7:365–371. doi: 10.3109/07357908909039865. [DOI] [PubMed] [Google Scholar]
- 41.Meilman PW. Cross-sectional age changes in ego identity status during adolescence. Dev Psychol. 1979;15:230–231. [Google Scholar]
- 42.Brennan J. Adjustment to cancer- Coping or personal transition? Psychooncology. 2001;10:1–18. doi: 10.1002/1099-1611(200101/02)10:1<1::aid-pon484>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 43.Lazarus RS, Folkman S. Stress appraisal and coping. New York, NY: Springer; 1984. [Google Scholar]
- 44.Deimling GT, Bowman KF, Sterns S, Wagner LJ, Kahana B. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology. 2006;15:306–320. doi: 10.1002/pon.955. [DOI] [PubMed] [Google Scholar]
- 45.Lown AE, Philips F, Schwartz LA, Rosenberg AR, Jones B. Psychosocial follow-up in survivorship as a standard of care in pediatric oncology. Pediatric Blood Cancer. 2015;62:S514–584. doi: 10.1002/pbc.25783. [DOI] [PMC free article] [PubMed] [Google Scholar]


