Abstract
Background:
Supraclavicular brachial plexus provides complete and reliable anesthesia for upper limb surgeries. Adjuvants are added to local anesthetists to improve various block characteristics. There are limited studies comparing the efficacy of dexmedetomidine and fentanyl as an adjuvant to levobupivacaine.
Aims:
The aim of the study was to evaluate and compare the effect of dexmedetomidine versus fentanyl as an adjuvant with levobupivacaine in ultrasound-guided supraclavicular brachial plexus block.
Settings and Design:
This study design was a prospective, randomized, double-blind controlled study.
Subjects and Methods:
A total of 120 patients in the age group of 30–55 years with physical status American Society of Anesthesiologists Classes I and II undergoing elective upper limb surgeries under ultrasound-guided supraclavicular brachial plexus block were randomly divided into three groups of forty each after taking informed consent and approval from Hospital Ethics Committee: Group A received 25 ml of 0.5% levobupivacaine with 5 ml normal saline (NS). Group B received 25 ml of 0.5% levobupivacaine with 1 μg/kg dexmedetomidine diluted to the volume of 5 ml NS. Group C received 25 ml of 0.5% levobupivacaine with 1 μg/kg fentanyl diluted to the volume of 5 ml NS. Onset and duration of sensory and motor block and duration of analgesia were noted and any side effects were observed.
Statistical Analysis:
The distribution of variables tested with Shapiro–Wilk test. Group comparison of values was made by Kruskal–Wallis test followed by Mann–Whitney test.
Results:
There was fastest onset time as well as longer duration of sensory and motor block in dexmedetomidine group, intermediate in fentanyl group as compared to levobupivacaine group.
Conclusion:
This study concludes that addition of dexmedetomidine to levobupivacaine for supraclavicular brachial plexus block shortens the onset time and prolongs the duration of sensory and motor blockade as compared to the addition of fentanyl.
Keywords: Dexmedetomidine, fentanyl, levobupivacaine
INTRODUCTION
Supraclavicular brachial block is the popular and widely used nerve block technique for perioperative anesthesia and analgesia for surgery of upper extremity. The block is performed at the level of distal trunks and origin of the divisions, where the brachial plexus is confined to its smallest surface area, thus producing a rapid and reliable blockade of brachial plexus.
Local anesthetics are compounds that have the ability to interrupt the transmission of the action potential of excitable membranes by binding to specific receptors in the Na+ channels. Large volumes of local anesthetics required to produce desirable effects may result in systemic side effects.[1] Adjuvants have been added to increase analgesia and reduce total dose of local anesthetics used minimizing the risk for local anesthetic toxicity.
This study is to compare the efficacy of dexmedetomidine and fentanyl as an adjuvant to levobupivacaine in ultrasound-guided supraclavicular brachial plexus block.
SUBJECTS AND METHODS
This study was conducted after obtaining the Institutional Ethics Committee approval.
A total of 120 patients in the age group of 30–55 years with physical status American Society of Anesthesiologists (ASA) Classes I and II undergoing elective upper limb surgeries under ultrasound-guided supraclavicular brachial plexus block were randomly divided into three groups of 40 each: Group A received 25 ml of 0.5% levobupivacaine with 5 ml normal saline (NS), Group B received 25 ml of 0.5% levobupivacaine with 1 μg/kg dexmedetomidine diluted to the volume of 5 ml NS, and Group C received 25 ml of 0.5% levobupivacaine with 1 μg/kg fentanyl diluted to the volume of 5 ml NS.
Inclusion criteria were patients with (1) ASA Grade I and II, (2) age group of 30–55 years of either gender, and (3) undergoing elective upper limb surgeries below mid humerus level.
Exclusion criteria were patients with (1) any contraindication to regional anesthesia, (2) refusal for supraclavicular block and inability to give consent, (3) coagulation disorders, (4) local skin infection or disease and others, (5) ASA III and V, (6) body mass index >30 kg/m2, (7) history of anaphylaxis to local anesthetics and allergy to the study drugs, (8) history of any underlying renal or hepatic dysfunction, (9) history of pulmonary, cardiac, hematological, endocrinal, and neuromuscular disorders, (10) history of chronic drug or alcohol abuse or analgesics, (11) history of underlying psychological disorder, and (12) pregnant patients.
All the patients were visited a day before surgery and explained in detail the anesthetic procedure. All the patients were kept nil orally at least 6 h before surgery. Tablet alprazolam 0.25 mg and tablet ranitidine 150 mg were given orally at 6 am in the morning of surgery with a sip of water.
For the supraclavicular plexus block, the patients were placed in the supine position with their heads turned in the direction opposite the neutral position, along the body. Subsequently, the probe linear type (12 MHZ) of the ultrasound equipment wrapped within a sterile rubber glove was placed on supraclavicular fossa to locate the subclavian artery and brachial plexus cluster. After local anesthetic infiltration, a 50 mm 22 G insulated short beveled stimulation needle (Stimuplex A, B. Braun Melsungen AG, Germany) was inserted toward the brachial plexus cluster from lateral to medial in the long axis of the ultrasound beam after locating the subclavian artery and brachial plexus cluster. Once the needle tip reached the brachial plexus cluster on the ultrasound image, 30 ml of drug was injected as appropriate for the group of study.
Completion of injection was considered as time 0. Sensory and motor blockade evaluation was done every 1 min, till the onset of the successful sensory and motor block, and then hourly till the complete regression of the block.
The sensory block was evaluated in the distribution of four nerves – musculocutaneous, median, radial, and ulnar with the pinprick method using a 3-point scale:[2] 0 = normal sensation; 1 = loss of sensation of pinprick (analgesia); and 2 = loss of sensation of touch (anesthesia).
Onset time to sensory block was defined as the time from completion of injection (time 0) to the time sensory block began to be detected (Score 1) in the distribution of any one of the major nerves.
The time to complete sensory block was taken from time 0 to the achievement of a Score 2 in the distribution of all the major nerves.
Total duration of sensory block was the duration from the end of local anesthetic administration to complete resolution of anesthesia from distribution of all four nerves, i.e., Score 0.
Total duration of analgesia was taken from the time of complete sensory block to the first request of rescue analgesia postoperatively.
Motor block was evaluated for four nerves (elbow flexion, thumb opposition, thumb abduction, and thumb adduction).
Motor blockade was graded on 3-point scale:[2] 0 = no block (normal motor functions with full flexion and extension of the elbow, wrist, and fingers); 1 = decreased motor strength with the ability to move fingers only; and 2 = complete motor blockade with the inability to move fingers.
Onset of motor block was taken as the time from the time of completion of injection of study drug to detection of a motor block of Score ≥1.
The time from completion of drug injection to the attainment of a Score of 2 was taken as the time to complete motor block.
Total duration of motor block was defined as time interval between the end of local anesthetic administration and the recovery of complete motor function of the hand and fingers, i.e., Score 0.
Quality of block was assessed on a 3-point scale by anesthesiologist who was blinded to study drugs as:[3] 0 = complete failure; 1 = inadequate block; and 2 = successful block.
Plexus block was considered successful when all four nerve territories were completely blocked for both sensory and motor block.
If any patient will have incomplete block, such patients were managed with supplemental analgesia with intravenous ketamine (1.5 mg/kg) and propofol (2 mg/kg), and block was considered as inadequate block.
The block was judged to have failed, if anesthesia is found inadequate in any of the major nerve distribution after 30 min of injecting of drug into the sheath and such patients were then excluded from the study and were taken under general anesthesia. Only successful block cases were taken in the study.
The heart rate, respiratory rate, oxygen saturation, and blood pressure (systolic, diastolic, and mean arterial) were noted, hence every 5 min till 30 min and then every 30 min till the end of the surgery. Hypotension was defined to be a fall in mean arterial pressure of >20% of baseline values and treated with a bolus of 100 ml fluid and if uncorrected, injection mephentermine 3 mg bolus, intravenously. Bradycardia was defined as pulse rate of ≤50/min and was treated with an intravenous bolus of injection atropine 0.6 mg.
Degree of sedation was monitored at all intervals as that of vital parameter monitoring during the surgery using the Ramsay Sedation Scale;[3] 1: awakened and alert; 2: sedated, but responding to verbal stimulus; 3: sedated, but responding to mild physical stimulus, 4: sedated, but responding to moderate or strong physical stimulus; and 5: not arousable.
On arrival in the postanesthesia care unit, pain scoring was assessed using 4-point verbal numeric rating pain scale (VNRS)[4] on movement of operated arm: 0 = no pain; 1–3 = mild pain; 4–7 = moderate pain; and 7–10 = severe pain.
VNRS on movement was assessed hourly following surgery till the request of first analgesic.
Any patient showing VNRS >3 was given 1 g paracetamol infusion intravenously. A Total number of rescue injections given during first 24 hours of postoperative period, was recorded.
Surgeon satisfaction was graded as[4] 0 – excellent: perfect analgesia and muscle relaxation; 1 – good: good analgesia with acceptable muscle relaxation; 2 – moderate: satisfactory analgesia but poor muscle relaxation; and 3 – unsuccessful: inadequate analgesia and muscle relaxation.
Patient satisfaction score was measured with a 5-point numerical scale:[4] 1 = very satisfied; 2 = satisfied; 3 = undecided; 4 = dissatisfied; and 5 = very dissatisfied. Postoperative vitals assessed every hour till the regression of block. Any side effects such as nausea, vomiting, and sedation were noted. Postoperative sedation score was assessed hourly till the regression of block.
RESULTS
Demographic data including patients' age, gender, height, weight, and ASA grade distribution were comparable in both the groups.
The three groups were comparable with respect to hemodynamics both intraoperatively and postoperatively, the difference being statistically insignificant.
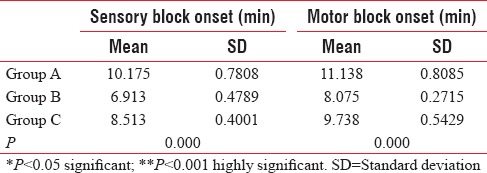
This table shows the onset of sensory and motor block which was highly significant statistically in these three groups showing the fastest onset of sensory[5] and motor block in Group B as compared to Group A and C (P < 0.001) [Table 1].
Table 1.
The onset of sensory and motor block which was highly significant statistically in these three groups showing fastest onset of sensory and motor block in Group B as compared to Group A and C (P<0.001)
The duration of sensory and motor block was highly significant statistically in these three groups being shortest in Group A, longest in Group B, and intermediate in Group C (P < 0.001) [Figure 1].
Figure 1.
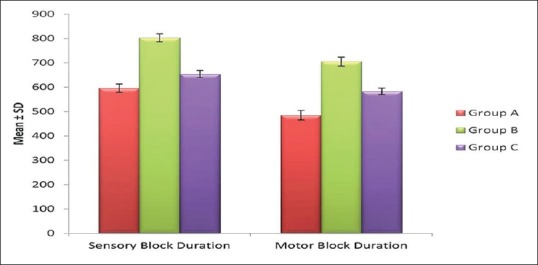
This graph shows the duration of sensory and motor block among three groups being shortest in Group A, longest in Group B, and intermediate in Group C
Total duration of analgesia was longest in Group B followed by Group C and shortest in Group A; thus, it is highly significant statistically (P = 0.000) [Figure 2].
Figure 2.
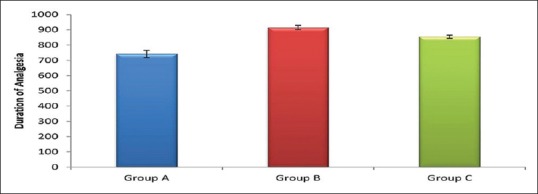
This graph shows the total duration of analgesia which was longest in Group B followed by Group C and shortest in Group A
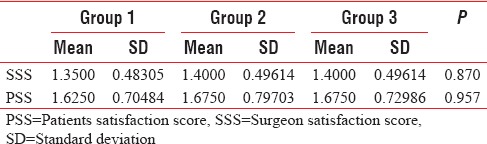
This table shows that the patients' satisfaction score and surgeon satisfaction score are statistically insignificant in all the three groups [Table 2].
Table 2.
The patients satisfaction score and surgeon satisfaction score is statistically insignificant in all the three groups
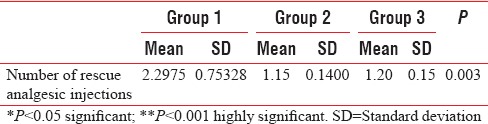
The use of rescue analgesia is maximum in Group A as compared to Group B and C which was statistically significant (P < 0.05) [Table 3].
Table 3.
The use of rescue analgesia is maximum in Group A as compared to Group B and C which was statistically significant (P<0.05)
There were no significant side effects in any group except for Grade 2 sedation seen in Group B, the difference being statistically significant (P = 0.000) [Figure 3].
Figure 3.
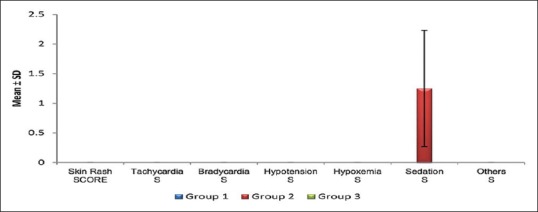
This graph shows the side effects in any of these three groups which shows that there were no significant side effects in any group except for Grade 2 sedation seen in Group B
DISCUSSION
Brachial plexus block is one of the peripheral nerve blockades used for upper limb surgeries. It has many advantages over general anesthesia such as effective analgesia with good motor blockade, awake patients, extended postoperatively analgesia, early mobilization, no airway manipulation, and avoiding polypharmacy. Recent interest in ultrasound-guided supraclavicular blocks may be due to (1) easy image acquisition relating to superficial location of brachial plexus at this level; (2) identifying pleura thus minimizing the risk of pneumothorax; (3) shortening the block performance time; (4) reducing the number of needle pricks. (5) shortening of block onset time. (6) reducing accidental vascular puncture. (7) allowing dose reduction of local anesthetic, and (8) enhanced block quality.[6,7] Levobupivacaine, the isolated S(-) isomer of bupivacaine is the latest local anesthetic and has been shown to be less cardiotoxic than bupivacaine. It has same efficacy for the time to reach sensory block and total duration of sensory block as that of bupivacaine,[8] but it has better toxicity profile than bupivacaine.[9] A variety of adjuvants have been studied for brachial plexus blockade including opioid and nonopioid agents, but studies showing effects of adding dexmedetomidine and fentanyl to levobupivacaine in brachial plexus block is limited, so this study is being chosen. The dose selection in this study was based on the historic evidence of optimally used drugs which are safe to use. In this study, we used 25 ml of 0.5% of levobupivacaine with 5 ml NS which was supplemented with either 1 μg/kg dexmedetomidine or 1 μg/kg of fentanyl. In our study, mean onset time of sensory and motor block was fastest in dexmedetomidine group as compared to fentanyl group and it is slowest in levobupivacaine group.
Duration of onset of sensory and motor block is longest in dexmedetomidine group, intermediate in fentanyl group, and shortest in levobupivacaine group. These results are in concordance with a study by Mathur et al.,[10] Esmaoglu et al.,[11] and Kaygusuz et al.,[12] but none of these studies compared dexmedetomidine with fentanyl as an adjuvant to levobupivacaine. Even some studies are in contrary to our study like the study conducted by Das et al.,[13] who showed no difference in onset time with the use of dexmedetomidine with ropivacaine. This difference could be due to the use of ropivacaine in their study as compared to levobupivacaine in our study. Duration of analgesia is longest in dexmedetomidine group as compared to fentanyl group, thus showing that dexmedetomidine has better pain control than fentanyl. Both drugs did not produce any potential side effects except for sedation in dexmedetomidine group which did not require any treatment thus can be termed as safe drugs.
CONCLUSION
In our study, we found that dexmedetomidine when added to levobupivacaine for supraclavicular brachial plexus block shortens the onset times of sensory and motor block and prolongs the duration of sensory and motor blockade and duration of analgesia as compared to the addition of fentanyl to levobupivacaine. The added advantage of hemodynamic stability and minimal side effects makes it a potential adjuvant for nerve blocks.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Vermeylen K, Engelen S, Sermeus I, Soetens F, Van de Velde M. Supraclavicular brachial plexus blocks: Review and current practice. Acta Anaesth Belg. 2011;62:15–21. [PubMed] [Google Scholar]
- 2.Jadon A, Dixit S, Kedia SK, Chakraborty S, Agrawal A, Sinha N. Interscalene brachial plexus block for shoulder arthroscopic surgery: Prospective randomised controlled study of effects of 0.5% ropivacaine and 0.5% ropivacaine with dexamethasone. Indian J Anaesth. 2015;59:171–6. doi: 10.4103/0019-5049.153039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reddy VS, Shaik NA, Donthu B, Reddy Sannala VK, Jangam V. Intravenous dexmedetomidine versus clonidine for prolongation of bupivacaine spinal anesthesia and analgesia: A randomized double-blind study. J Anaesthesiol Clin Pharmacol. 2013;29:342–7. doi: 10.4103/0970-9185.117101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holdgate A, Asha S, Craig J, Thompson J. Comparison of a verbal numeric rating scale with the visual analogue scale for the measurement of acute pain. Emerg Med (Fremantle) 2003;15:441–6. doi: 10.1046/j.1442-2026.2003.00499.x. [DOI] [PubMed] [Google Scholar]
- 5.Yadav AK, Agrawal M, Ahmad S, Kejarwal AK, Singh K. A comparison of fentanyl and dexmedetomidine as an adjuvant to levobupivacaine in supraclavicular brachial plexus block for upper limb surgery : a prospective randomized single-blind controlled study. IJCMR. 2016;3:785–9. [Google Scholar]
- 6.Kapral S, Krafft P, Eibenberger K, Fitzgerald R, Gosch M, Weinstabl C, et al. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994;78:507–13. doi: 10.1213/00000539-199403000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Ootaki C, Hayashi H, Amano M. Ultrasound-guided infraclavicular brachial plexus block: An alternative technique to anatomical landmark-guided approaches. Reg Anesth Pain Med. 2000;25:600–4. doi: 10.1053/rapm.2000.18184. [DOI] [PubMed] [Google Scholar]
- 8.Leone S, Di Cianni S, Casati A, Fanelli G. Pharmacology, toxicology, and clinical use of new long acting local anesthetics, ropivacaine and levobupivacaine. Acta Biomed. 2008;79:92–105. [PubMed] [Google Scholar]
- 9.Kanazi GE, Aouad MT, Jabbour-Khoury SI, Al Jazzar MD, Alameddine MM, Al-Yaman R, et al. Effect of low-dose dexmedetomidine or clonidine on the characteristics of bupivacaine spinal block. Acta Anaesthesiol Scand. 2006;50:222–7. doi: 10.1111/j.1399-6576.2006.00919.x. [DOI] [PubMed] [Google Scholar]
- 10.Mathur R, Yogesh M, Kalla P, Sanjay A randomized double blind prospective study to compare the characteristics of levobupivacaine with clonidine or dexmedetomidine as an adjuvant in supraclavicular brachial plexus block. Int J Sci Res. 2017;5:549–51. [Google Scholar]
- 11.Esmaoglu A, Yegenoglu F, Akin A, Turk CY. Dexmedetomidine added to levobupivacaine prolongs axillary brachial plexus block. Anesth Analg. 2010;111:1548–51. doi: 10.1213/ANE.0b013e3181fa3095. [DOI] [PubMed] [Google Scholar]
- 12.Kaygusuz K, Kol IO, Duger C, Gursoy S, Ozturk H, Kayacan U, et al. Effects of adding dexmedetomidine to levobupivacaine in axillary brachial plexus block. Curr Ther Res Clin Exp. 2012;73:103–11. doi: 10.1016/j.curtheres.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Das A, Majumdar S, Halder S, Chattopadhyay S, Pal S, Kundu R, et al. Effect of dexmedetomidine as adjuvant in ropivacaine-induced supraclavicular brachial plexus block: A prospective, double-blinded and randomized controlled study. Saudi J Anaesth. 2014;8:S72–7. doi: 10.4103/1658-354X.144082. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]


