Abstract
Background and Aims:
Preoperative anxiety is a major concern in patients undergoing any surgical procedure. Various drugs have been used to alleviate it. This study aims to compare the effects of oral melatonin versus oral alprazolam on preoperative anxiety, sedation, orientation, and cognitive function.
Materials and Methods:
A total of 90 adult patients were randomly allocated into three groups. Group M (n = 30) received oral melatonin 3 mg (2 tablets); Group A (n = 30) received oral alprazolam 0.25 mg (2 tablets), and Group P (n = 30) received placebo, multivitamin tablet (2 tablets) as premedication. The objectives of our study were to compare anxiety, sedation, orientation, and cognitive function using visual analog scale (VAS) anxiety score, Ramsay Sedation Score (RSS), orientation score, and Digit symbol substitution test (DSST) score before and after 120 min of giving premedication. For statistical analysis, paired t-test, Chi-square test, analysis of variance, and post hoc bonferroni test were used.
Results:
Mean VAS scores for anxiety (after 120 min) were significantly reduced in Group M (3.9 ± 1.53) and Group A (4.43 ± 1.67) when compared to Group P (4.73 ± 0.82) (P < 0.05). RSS was higher in Group A as compared to Group M and Group P (P < 0.05). No significant difference in orientation score was observed in all the three groups before and after premedication (P > 0.05). DSST score (cognitive function) was better in Group M when compared to both Group A and Group P (P < 0.05).
Conclusion:
Oral melatonin (6 mg) when used as a premedicant is an effective alternative to alprazolam regarding providing better anxiolysis, lesser sedation along with maintenance of cognitive, and psychomotor function.
Keywords: Alprazolam, cognitive function, melatonin, premedication, preoperative anxiety, sedation
INTRODUCTION
Preoperative anxiety is commonly experienced by the patients who are admitted to hospital for any surgery which can be described as an unpleasant state of tension or uneasiness that results from a patient's doubts or fears about the surgery and anesthesia.[1] It increases patient's catecholamine secretions which may lead to hypertension, tachycardia, and arrhythmias.[2] Benzodiazepines (midazolam and alprazolam) are most commonly used as a premedicant to alleviate perioperative anxiety and to produce amnesia and sedation; however, they may impair cognitive and psychomotor performance.[3]
Alprazolam (triazolobenzodiazepine) is a short-acting drug which has anxiolytic, sedative, hypnotic, anticonvulsant, and amnesic properties but may cause psychomotor impairment.[4] Melatonin (N-acetyl-5-methoxytryptamine) is an endogenous neurohormone secreted by the pineal gland. It has unique property of producing anxiolysis with no impairment of cognitive and psychomotor function that is highly desirable in routine perioperative care when given orally as a premedication. It has inhibitory action on central nervous system. It also has sedative, hypnotic, analgesic, anti-inflammatory, antioxidative, and chronobiotic effects; however, its analgesic effect remains controversial.[5,6,7,8]
The melatonin has been reported to be used as a premedicant in a dose range of 3–15 mg given orally or sublingually 50–90 min preoperatively. The peak effect of oral melatonin ranges from 60 to 150 min.[7,8] Various studies have been reported which compared midazolam with melatonin; however, a very few studies have compared alprazolam with melatonin. Hence, we hypothesized that melatonin (6 mg) when given orally as a premedication 120 min before the induction of anesthesia would provide adequate anxiolysis and arousable sedation with no effect on cognitive and psychomotor function along with stable hemodynamics and minimal side effects. In this study, we planned to compare the effects of oral melatonin and alprazolam as a premedication on various parameters including anxiety, sedation, orientation, and cognitive function.
MATERIALS AND METHODS
This prospective, randomized comparative study was conducted after clearance from local Institutional Ethical Committee in patients scheduled for various elective surgeries under general anesthesia. After valid written and informed consent, a total of 90 adult patients aged 18–60 years with the American Society of Anesthesiologists (ASA) physical status Classes 1 and 2, posted for various elective surgeries of >1 h duration under general anesthesia, were included in this study.
The study participants were randomly allocated into three groups of 30 patients each using computer-generated table of random numbers.
Group M (n = 30) received oral melatonin 3 mg (2 tablets) 120 min before induction of anesthesia
Group A (n = 30) received oral alprazolam 0.25 mg (2 tablets) 120 min before induction of anesthesia
Group P (n = 30) received oral low-dose multivitamin tablets (2 tablets) 120 min before induction of anesthesia.
Patients with ASA physical status classes 3 and above, age >60 years, patients having allergy to any of the study drugs, pregnant women, patients with any mental illness, patients on steroids and antipsychotics, patients unable to read or write basic alphabets, patients with uncontrolled hypertension and diabetes were excluded from the study.
All patients underwent thorough preanesthetic check-up along with routine investigations before the surgery and explained about the anesthetic technique and perioperative course. All the patients were kept nil per oral for a minimum duration of 8 h before surgery. On the day of surgery, a written and informed consent was taken from all the patients after explaining about the nature of the study, various scales that were used in the study and were counseled regarding general anesthesia procedure which was used in the study. The visual analog scale (VAS) anxiety score, Ramsay Sedation Score (RSS), orientation score, the objective tests for cognitive performance such as Digit symbol substitution test (DSST) were explained to them and patients were asked to do it in a sample test.
The anxiety score was assessed using VAS anxiety score[9] which is equivalent to VAS score as used for pain on a 10 cm linear scale, one end “0” = no anxiety and other end “10” = worst imaginable anxiety was marked and patient was asked to put his/her finger in between the two according to the level of anxiety. Sedation was assessed with RSS:
1 – Patient is anxious and agitated or restless, or both
2 – Patient is cooperative, oriented, and tranquil
3 – Patient responds to commands only
4 – Patient exhibits brisk response to light glabellar tap or loud auditory stimulus
5 – Patient exhibits a sluggish response to light glabellar tap or loud auditory stimulus
6 – Patient exhibits no response.
Orientation was assessed with a three-point scale;
0 – None
1 – Orientation in either time or place
2 – Orientation in both.
The DSST [Figure 1] is a test to assess the psychomotor performance of a patient who was provided a pencil and paper with a sheet which has a key grid of numbers and matching symbols and a test section having numbers and empty boxes. This sheet of paper has a key with numbers 1–9 on its top and a different symbol was assigned to each number. There were five rows of 25 randomly distributed numbers without their corresponding symbol as empty boxes. After duration of 90s, the number of empty boxes filled up by the patient from left to right was counted, and a score was given for the number of correct symbols inserted. The decreased DSST scores were in favor of cognitive dysfunction.[10,11] The primary outcome measure was anxiety score while the secondary outcome measures were sedation score, orientation and cognitive and psychomotor functions.
Figure 1.
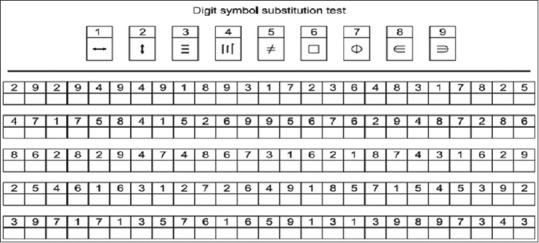
Digit symbol substitution test for assessment of cognitive function
The patients were shifted to the preoperative area in the operation theater 2 h before surgery. The various hemodynamic parameters including heart rate (HR), noninvasive blood pressure (NIBP), and oxygenation (SpO2) were recorded thereafter. The patient's level of anxiety and sedation along with orientation and cognitive functions (DSST) were assessed before giving the study medications. The study medications (tablets) were given to the patient 120 min before induction of general anesthesia according to the group allocation in a closed, opaque identical-sealed envelope by the resident anesthesiologist. The patients were asked to take the study medication orally with a sip of water only. The patients were evaluated again using the above-mentioned parameters and tests. The side effects, if any occurred during this period, were also noted.
After arrival of the patient in operation theater, peripheral intravenous (iv) line (18 G) was secured and Ringer lactate infusion was started. A multipara monitor was attached thereafter to record baseline HR, NIBP, and SpO2. All patients were given glycopyrrolate 0.004 mg/kg iv and tramadol 2 mg/kg iv as a premedication, and preoxygenation was done with 100% O2 for 3 min. General anesthesia was induced with etomidate 0.2 mg/kg iv slowly till loss of response to verbal commands and eyelash reflex then succinylcholine 2 mg/kg iv was administered followed by bag and mask ventilation for 60 s. The patient was intubated thereafter with appropriate-sized cuffed endotracheal tube and maintained with atracurium 0.5 mg/kg loading dose and 0.01 mg/kg maintenance dose along with sevoflurane (2%) and nitrous oxide (N2O):Oxygen (O2) in 40:60 mixture. Paracetamol 15 mg/kg iv in 100 ml normal saline was administered slowly 15 min before completion of surgery. At the end of surgical procedure, reversal was done with neostigmine 0.05 mg/kg and glycopyrrolate 0.008 mg/kg iv, and patient was extubated thereafter after complete recovery from general anesthesia.
Statistical analysis
Statistical analysis was done using SPSS version 20 (IBM SPSS Statistics Inc., Chicago, Illinois, USA). Based on the previous studies, a sample size was calculated to be 30 patients to be randomly allocated in each group keeping a power of 0.8, α error of 0.05 and allowing for study error and attrition.[12,13,14,15] Descriptive statistics included computation of percentages, means, and standard deviations. The paired t-test (for quantitative data to compare before and after observations), analysis of variance (ANOVA) (for quantitative data within three groups) with post hoc Bonferroni test (to make more intragroups comparison) and repeated measures ANOVA (for quantitative data within three groups at different time interval) were used for comparison of all clinical indicators. Chi-square test was used for the comparison of qualitative data. P ≤ 0.05 was considered statistically significant.
RESULTS
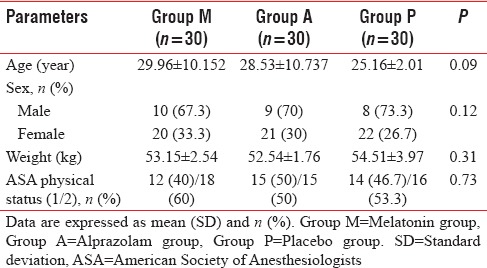
The three groups were comparable with respect to demographic profile including mean age, sex, weight, and ASA physical status, P > 0.05 [Table 1].
Table 1.
Demographic profile in three groups
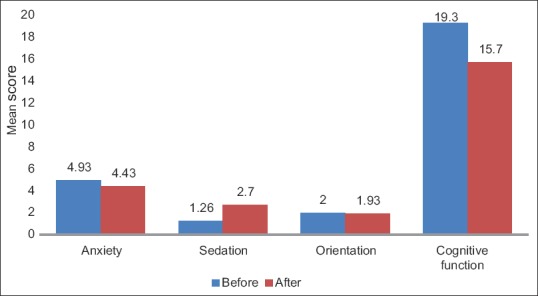
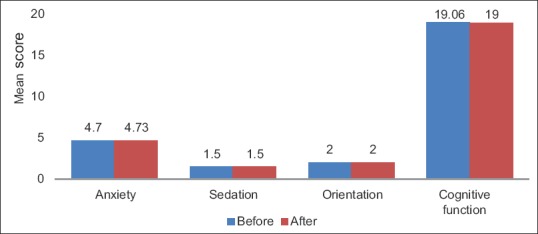
In Group M, VAS anxiety score was 0–3 in none of the patients, 4–6 in 27 (90%) patients and 7–10 in 3 (10%) patients, just before oral melatonin intake whereas it was 0–3 in 12 (40%) patients, 4–6 in 16 (53.3%) patients and 7–10 in 2 (6.7%) patients, and 120 min after melatonin intake. Mean VAS score was significantly reduced (4.9 ± 1.02–3.9 ± 1.52, before and after 120 min of melatonin intake, respectively) (P = 0.005), [Table 2 and Figure 2]. Similarly, in Group A, VAS anxiety score was 0–3 in none of the patients, 4–6 in 26 (86.7%) patients, and 7–10 in 4 (13.3%) patients, just before intake of oral alprazolam whereas it was 0–3 in 8 (26.7%) patients, 4–6 in 18 (60%) patients, and 7–10 in 4 (13.3%) patients, 120 min after intake. Mean VAS score was 4.93 ± 1.41 before intake of alprazolam which was reduced to 4.43 ± 1.67, 120 min after intake, which was statistically significant (P = 0.01), [Table 2 and Figure 3]. In Group P, VAS anxiety score was found to be statistically insignificant after 120 min of giving multivitamin tablet (P = 0.8), [Table 2 and Figure 4].
Table 2.
Intragroup comparison of mean study parameters among all three groups
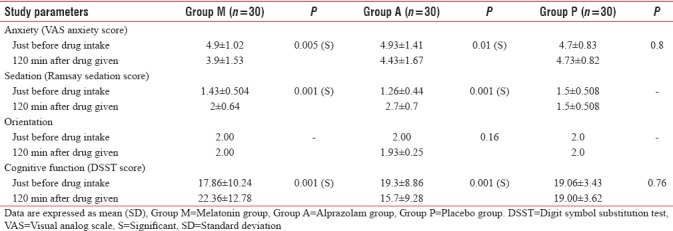
Figure 2.
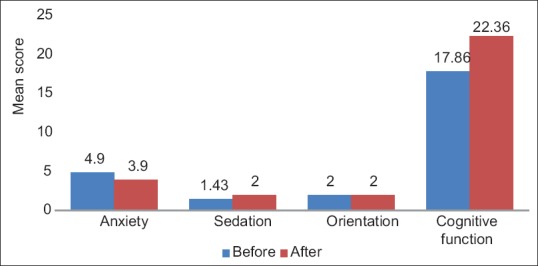
Comparison of mean study parameters among Group M. Group M=Melatonin group
Figure 3.
Comparison of mean study parameters among Group A. Group A=Alprazolam group
Figure 4.
Comparison of mean study parameters among Group P. Group P =Placebo group
On intergroup comparison, VAS anxiety score (after 120 min of premedication) was significantly reduced in Group M and Group A when compared to Group P (P < 0.05). However, VAS score was also statistically significant between Group M and Group A (P < 0.05), [Table 3].
Table 3.
Intergroup comparison of various study parameters (120 min after premedication) in three groups
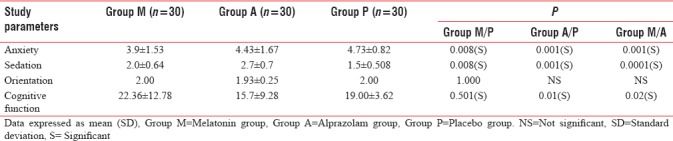
In Group M, RSS was 1 in 17 (56.7%) patients, 2 in 13 (43.3%), and 3 in none of the patients, just before intake of oral melatonin whereas it was 1 in 6 (20%) patients, 2 in 18 (60%) patients, and 3 in 6 (20%) patients, 120 min after melatonin intake. Mean sedation score was 1.43 ± 0.504 just before intake of melatonin, which was increased to 2.0 ± 0.64, 120 min after intake, which was statistically significant (P = 0.001), [Figure 2]. In Group A, RSS was 1 in 22 (73.3%) patients, 2 in 8 (26.7%) patients, and 3 and 4 in none of the patients before intake of alprazolam but none of the patients had score 1, 13 (43.3%) patients had score 2 while 13 (43.3%) patients had score 3, and 4 (13.3%) patients had score 4, 120 min after intake. Mean sedation score was 1.26 ± 0.44 just before alprazolam intake which increased to 2.7 ± 0.7, 120 min after intake, which was statistically significant (P = 0.001), [Table 2 and Figure 3]. In Group P, no significant difference in sedation was found on intragroup comparison (P > 0.05), [Figure 4].
A significant difference was noted in RSS on the intergroup comparison (after 120 min of premedication) in all the three groups (P < 0.05). The sedation scores were significantly more in alprazolam group when compared to both melatonin and placebo groups [Table 3].
In Group M, orientation score was 2 in 30 (100%) patients just before intake of melatonin which remained same after 120 min while in Group A, orientation score was 2 in 30 (100%) patients before intake of alprazolam which was reduced to 1 in 2 (6.7%) patients and remained 2 in 28 (93.3%) patients, 120 min after intake. Mean orientation score was 2 just before alprazolam intake which was decreased to 1.93 ± 0.25, 120 min after intake, (P = 0.16), [Figure 3]. In Group P, orientation score was 2 in 30 (100%) patients just before intake of the multivitamin tablet which remained same after 120 min [Table 2 and Figure 4]. No significant difference was noted in orientation scores in between the three groups (P > 0.05).
In Group M, DSST score was 17.86 ± 10.24 just before melatonin intake which was increased to 22.36 ± 12.78, 120 min after intake, which was statistically significant (P = 0.001), [Figure 2]. While in Group A, DSST score was 19.3 ± 8.86 just before alprazolam intake which was significantly reduced to 15.7 ± 9.28, 120 min after intake (P = 0.001), [Figure 3]. In Group P, DSST score was found to be statistically insignificant both before and after giving premedication as placebo (P = 0.76), [Table 2 and Figure 4]. The cognitive function (DSST score) was significantly improved in Group M when compared to Group A. A significant difference was also found in DSST scores between Group A and Group P as this score was significantly reduced in alprazolam group (P < 0.05), [Table 3]. However, no significant difference was noted between melatonin and placebo groups.
DISCUSSION
Benzodiazepines are usually the most common drugs used as a premedication to alleviate preoperative anxiety. They enhance the effect of neurotransmitter gamma amino butyric acid (GABA) on GABAA receptor to produce anxiolysis, sedation, amnesia, and anticonvulsant effects. Benzodiazepines may impair cognitive and psychomotor performance. Alprazolam at doses of 0.5 mg and higher has been reported to impair immediate and delayed recall and recognition.[3,4,16]
Melatonin in a dose of 1–5 mg has been reported to increase 10–100 times more plasma levels than the endogenous night time levels. Melatonin (3–6 mg) when given orally has also been reported to produce significant anxiolysis and sedation at 60–120 min after premedication with a calm, tranquil patient along with stable hemodynamics and minimal side effects which favors to choose a dose of 6 mg in our study.[2,5,6,7,12] The reported literature of the effect of melatonin on the orientation score with respect to time and place is variable but it remained preserved in perioperative period of our study. Various studies have reported that melatonin lacks anterograde amnesia which is a desirable feature of this drug to be used as premedication.[7]
Significant reduction in anxiety score was found in Group M and Group A as compared to Group P and reduction was more effective in patients having VAS anxiety score between 4 and 6 before premedication. However, the reduction in the level of anxiety was greater in Group M as compared to Group A. Our study showed that reduction in anxiety was greater in melatonin group when compared to alprazolam group which was supported by study done by Pokharel et al.[13] who reported that VAS anxiety scores were significantly reduced from their baseline scores at various time intervals in all the groups except in placebo group; however, they compared the combination of melatonin and alprazolam and melatonin (3 mg) or alprazolam (0.5 mg) alone.(P < 0.001) Ionescu et al.[17] reported that oral melatonin (3 mg) when used as a premedication in laparoscopic cholecystectomies produced significant anxiolysis at this dose. This was also supported by Mowafi and Ismail,[18] who reported that melatonin provides anxiolysis, enhances analgesia, and promotes better operating conditions during cataract surgery under topical anesthesia as melatonin significantly reduced the anxiety scores (median, interquartile range) from 5 (3.5–6) to 3 (2–3) after premedication and to 3 (2–3.5) during surgery (P = 0.04 and P = 0.005 compared with the placebo group, respectively). Naguib and Samarkandi[14] compared melatonin and midazolam for premedication in adult patients and showed that 0.05 mg/kg melatonin was associated with preoperative anxiolysis and sedation without impairment of cognitive and psychomotor skills or affecting the quality of recovery which favors the use of melatonin (6 mg) in our study as it provided significant anxiolysis and adequate sedation along with preserved cognitive and psychomotor function which is desirable for these patients. However, in contrast to our study, Patel and Kurdi[15] compared the effects of oral melatonin and midazolam on preoperative anxiety, sedation, cognitive, and psychomotor functions and found both drugs comparable regarding reducing anxiety; however, they had used melatonin in a dose of 0.4 mg/kg which is higher than our dose. De Witte et al.[4] reported that alprazolam may be an effective alternative to midazolam to reduce the anxiety with no amnesia; however, it may be associated with greater impairment of psychomotor function in the early postoperative period which needs to be avoided. Although our results showed significant reduction in VAS anxiety scores in melatonin group when compared to alprazolam group, some other studies also compared oral melatonin with midazolam and found comparable anxiety scores in two groups which is in contrast to our study.[12,14,17,19]
Our results showed that both melatonin and alprazolam caused significant sedation in patients as compared to placebo. Among Group M and Group A, melatonin caused less sedation than alprazolam. Our results are supported by the studies done by Naguib and Samarkandi[14] in which increased levels of sedation was found in the melatonin and midazolam groups compared with placebo that was evident at 60 and 90 min after premedication. Our study results were also supported by Pokharel et al.,[13] who found significantly increased sedation scores in all the groups. The intergroup comparison in our study showed that alprazolam produces highest degree of sedation as compared to melatonin and placebo. Melatonin produced adequate arousable sedation which was very much desirable as against the deep sedation produced by alprazolam so the patients who received melatonin required less precise monitoring than patients who received alprazolam.[19]
In our study, alprazolam caused change in orientation score in patients when compared to melatonin and placebo groups; however, there was no significant difference in orientation scores in all the three groups before and after giving study medications which are in concordance with the studies done by Patel and Kurdi and Pokharel et al.[13,15,19]
Cognitive function is also one of the essential tools for the assessment of neurological and behavioral functions. Higher mental functions were assessed by DSST.[10,11] There was decline in cognitive function in Group A as compared to Group P whereas the cognitive function was enhanced or maintained in Group M when compared to Group A and P. Melatonin was more effective in the maintenance of cognitive function as compared to alprazolam. Our findings were also supported by Patel and Kurdi[15] who studied the effects of oral melatonin and oral midazolam on cognitive and psychomotor functions and found the increased DSST scores in melatonin group used for assessing the cognitive function of the patients. This favors the use of melatonin as an effective alternative to alprazolam as it preserved the cognitive and psychomotor skills of the patient.[20,21]
As far as limitations of our study are concerned, the sample size was small as the inference drawn from this study population could not be extrapolated for patients with associated comorbid conditions and for obese patients. We did not measure the dose-response curves of plasma drug concentration for both of the study drugs because we had assumed a certain effect of each drug at its particular dose on the basis of available literature which might have resulted in variable results. Further studies needs to be conducted with different doses of melatonin and a larger sample size to find out an optimal and safe dose of oral melatonin as well as to prove its efficacy over benzodiazepines to be used as a premedicant.
CONCLUSION
We conclude that melatonin is an effective alternative to alprazolam as oral melatonin (6 mg) when used as a premedication is found to be a better anxiolytic when compared to alprazolam with lesser sedation and preserved cognitive and psychomotor functions which are the desirable features of a drug to be used as a premedicant.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kim WS, Byeon GJ, Song BJ, Lee HJ. Availability of preoperative anxiety scale as a predictive factor for hemodynamic changes during induction of anesthesia. Korean J Anesthesiol. 2010;58:328–33. doi: 10.4097/kjae.2010.58.4.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta P, Jethava D, Choudhary R, Jethava DD. Role of melatonin in attenuation of haemodynamic responses to laryngoscopy and intubation. Indian J Anaesth. 2016;60:712–8. doi: 10.4103/0019-5049.191667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wittenborn JR. Effects of benzodiazepines on psychomotor performance. Br J Clin Pharmacol. 1979;7(Suppl 1):61S–7S. doi: 10.1111/j.1365-2125.1979.tb04667.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Witte JL, Alegret C, Sessler DI, Cammu G. Preoperative alprazolam reduces anxiety in ambulatory surgery patients: A comparison with oral midazolam. Anesth Analg. 2002;95:1601–6. doi: 10.1097/00000539-200212000-00024. [DOI] [PubMed] [Google Scholar]
- 5.Naguib M, Gottumukkala V, Goldstein PA. Melatonin and anesthesia: A clinical perspective. J Pineal Res. 2007;42:12–21. doi: 10.1111/j.1600-079X.2006.00384.x. [DOI] [PubMed] [Google Scholar]
- 6.Maitra S, Baidya DK, Khanna P. Melatonin in perioperative medicine: Current perspective. Saudi J Anaesth. 2013;7:315–21. doi: 10.4103/1658-354X.115316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yousaf F, Seet E, Venkatraghavan L, Abrishami A, Chung F. Efficacy and safety of melatonin as an anxiolytic and analgesic in the perioperative period: A qualitative systematic review of randomized trials. Anesthesiology. 2010;113:968–76. doi: 10.1097/ALN.0b013e3181e7d626. [DOI] [PubMed] [Google Scholar]
- 8.Dawson D, Encel N. Melatonin and sleep in humans. J Pineal Res. 1993;15:1–2. doi: 10.1111/j.1600-079x.1993.tb00503.x. [DOI] [PubMed] [Google Scholar]
- 9.Aitken RC. Measurement of feelings using visual analogue scales. Proc R Soc Med. 1969;62:989–93. doi: 10.1177/003591576906201005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim C, Hong S, Kim B, Cheon J, Lee Y, Koh H, et al. Comparison of various tests designed to assess the recovery of cognitive and psychomotor function after ambulatory anesthesia. Korean J Anesthesiol. 2008;55:291–7. [Google Scholar]
- 11.Rosano C, Newman AB, Katz R, Hirsch CH, Kuller LH. Association between lower digit symbol substitution test score and slower gait and greater risk of mortality and of developing incident disability in well-functioning older adults. J Am Geriatr Soc. 2008;56:1618–25. doi: 10.1111/j.1532-5415.2008.01856.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Naguib M, Samarkandi AH. Premedication with melatonin: A double-blind, placebo-controlled comparison with midazolam. Br J Anaesth. 1999;82:875–80. doi: 10.1093/bja/82.6.875. [DOI] [PubMed] [Google Scholar]
- 13.Pokharel K, Tripathi M, Gupta PK, Bhattarai B, Khatiwada S, Subedi A, et al. Premedication with oral alprazolam and melatonin combination: A comparison with either alone – A randomized controlled factorial trial. Biomed Res Int 2014. 2014 doi: 10.1155/2014/356964. 356964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naguib M, Samarkandi AH. The comparative dose-response effects of melatonin and midazolam for premedication of adult patients: A double-blinded, placebo-controlled study. Anesth Analg. 2000;91:473–9. doi: 10.1097/00000539-200008000-00046. [DOI] [PubMed] [Google Scholar]
- 15.Patel T, Kurdi MS. A comparative study between oral melatonin and oral midazolam on preoperative anxiety, cognitive, and psychomotor functions. J Anaesthesiol Clin Pharmacol. 2015;31:37–43. doi: 10.4103/0970-9185.150534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verster JC, Volkerts ER. Clinical pharmacology, clinical efficacy, and behavioral toxicity of alprazolam: A review of the literature. CNS Drug Rev. 2004;10:45–76. doi: 10.1111/j.1527-3458.2004.tb00003.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ionescu D, Bodescu C, Ilie A, Miclutia I, Iancu A, Ion D, et al. Melatonin as premedication for laparoscopic cholecystectomy: A double blind placebo controlled study. South Afr J Anaesth Analg. 2008;14:8–11. [Google Scholar]
- 18.Mowafi HA, Ismail SA. Melatonin improves tourniquet tolerance and enhances postoperative analgesia in patients receiving intravenous regional anesthesia. Anesth Analg. 2008;107:1422–6. doi: 10.1213/ane.0b013e318181f689. [DOI] [PubMed] [Google Scholar]
- 19.Acil M, Basgul E, Celiker V, Karagöz AH, Demir B, Aypar U, et al. Perioperative effects of melatonin and midazolam premedication on sedation, orientation, anxiety scores and psychomotor performance. Eur J Anaesthesiol. 2004;21:553–7. doi: 10.1017/s0265021504007094. [DOI] [PubMed] [Google Scholar]
- 20.Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. 4th ed. New York: Oxford University Press; 2004. [Google Scholar]
- 21.Han ES, Lee Y, Kim J. Association of cognitive impairment and frailty in community dwelling older adults. Int Psychogeriatr. 2013;23:1–9. doi: 10.1017/S1041610213001841. [DOI] [PubMed] [Google Scholar]


