Abstract
Our understanding of the intracrine (or local) regulation of estrogen and other steroid synthesis and degradation expanded in the last decades, also thanks to recent technological advances in chromatography mass-spectrometry. Estrogen responsive tissues and organs are not passive receivers of the pool of steroids present in the blood but they can actively modify the intra-tissue steroid concentrations. This allows fine-tuning the exposure of responsive tissues and organs to estrogens and other steroids in order to best respond to the physiological needs of each specific organ. Deviations in such intracrine control can lead to unbalanced steroid hormone exposure and disturbances. Through a systematic bibliographic search on the expression of the intracrine enzymes in various tissues, this review gives an up-to-date view of the intracrine estrogen metabolisms, and to a lesser extent that of progestogens and androgens, in the lower female genital tract, including the physiological control of endometrial functions, receptivity, menopausal status and related pathological conditions. An overview of the intracrine regulation in extra gynecological tissues such as the lungs, gastrointestinal tract, brain, colon and bone is given. Current therapeutic approaches aimed at interfering with these metabolisms and future perspectives are discussed.
Keywords: intracrinology, endometrium, estrogens, lungs, gastrointestinal tract, central nervous system, bone
Introduction
The term “intracrinology,” coined in 1988 by prof Labrie, refers to the ability of peripheral tissues to use blood precursors and generate steroids (Labrie, 1991). Several studies have been published but several controversies still exist and relate to the following technical and biological aspects: (a) some intracrine enzymes in peripheral tissues have low expression (300–50,000-times lower than in endocrine glands Stoffel-Wagner, 2001; Murakami et al., 2006, close to the detection limit of standard methods like western blotting and immunohistochemistry -IHC); (b) the technology to robustly quantify steroids (liquid-/gas-chromatography tandem mass-spectrometry -LC-MS or GC-MS), became available during the last 5–10 years only (Rosner et al., 2013); (c) intracrine pathways are highly complex.
This review summarizes our knowledge of intracrinology in peripheral tissues like the endometrium, lungs, gastrointestinal tract (GIT), bone and central nervous system (CNS), with special attention to the metabolism of estrogens. Drug development and potential therapeutic approaches are discussed. In this review, the enzymes involved in steroid deactivation/clearance (Rižner, 2013, 2016; with the exclusion of steroid sulphotransferases) and those involved in the transport of conjugated steroids through the plasma membrane (Rižner et al., 2017) are not described. Studies on serum/tissue steroid levels are reported and discussed only if based on gold standard GC/LC-MS.
From ovarian estrogen synthesis to intracrinology
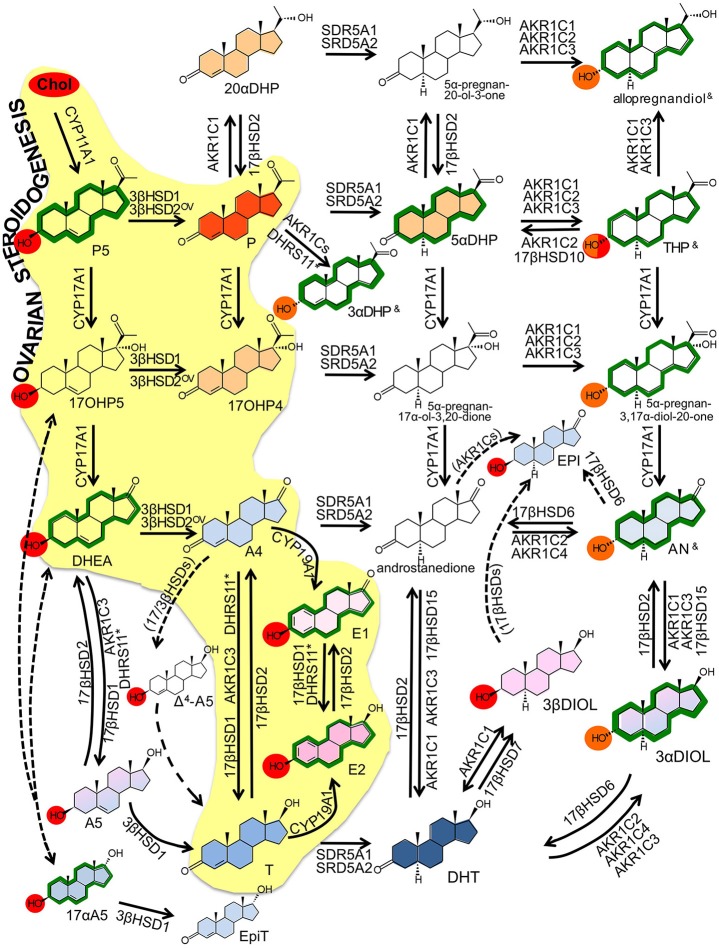
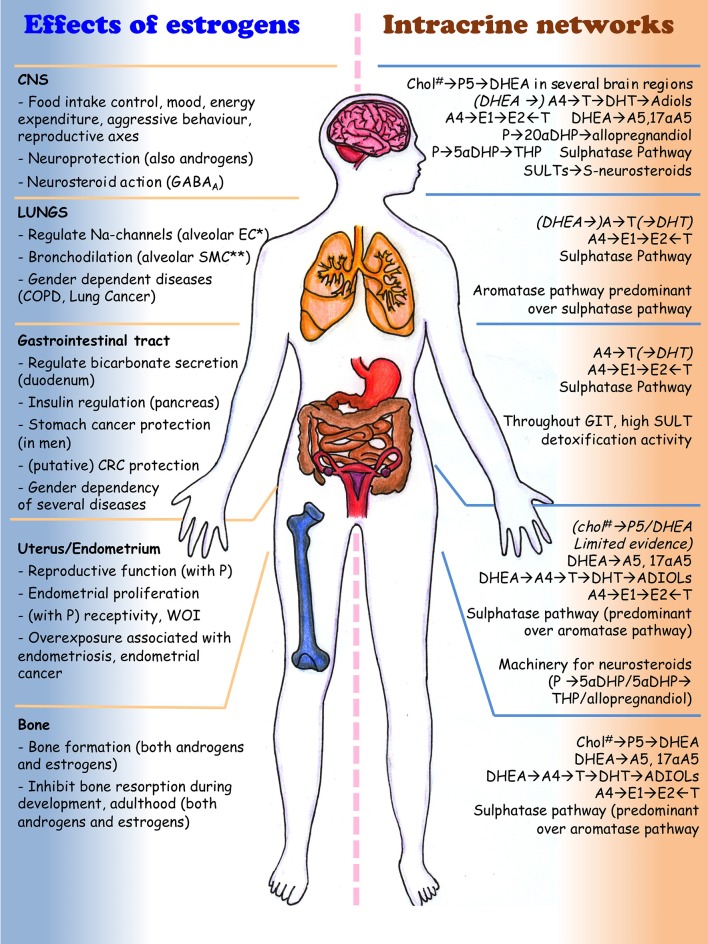
Local steroid metabolism is possible because those enzymes responsible for steroid synthesis in classical glands (ovaries, adrenals, testes) are expressed in peripheral tissues, where additional and alternative routes for metabolizing steroids are present and make intracrine networks intricate and flexible (Figures 1, 2, Tables 1, 2). In particular, several compounds generated through these pathways, although not being estrogens, can have estrogenic action, because able to bind and activate the estrogen receptors. The biologic activity of the various compounds is given in Table 1, and in Figure 2, by the color codes.
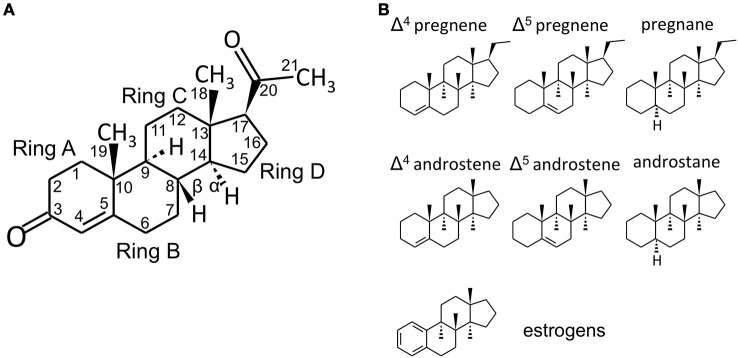
Figure 1.
Steroid structure. (A) structure of the C21 steroid progesterone (P, used as an example), with carbon numbering and steroid ring numbering. In the storied graphics in Figures 1B and 2, the H groups and the relative bonds will be omitted (with the exclusion of the H in 5α-reduced steroids - androstanes and pregnanes). Methyl groups will be indicated by the bonds only without the CH3 group. (B) structures of C21 pregnene (Δ4 and Δ5, i.e., double bond between C4 and C5 or between C5 and C6, respectively), pregnane (5α-reduced steroid), C19 androstene (Δ4, Δ5) and androstane and C18 (A-ring)-aromatic estrogens. Chemical structures were designed with the aid of Sketcher V2.4 (Ihlenfeldt et al., 2009), available online at PubChem (www.ncbi.nlm.nih.gov; pubchem.ncbi.nlm.nih.gov) (Kim et al., 2016).
Figure 2.
Intracrine networks. Major intracrine networks metabolizing steroids. In this figure, each reaction reports the catalyzing enzymes whose role in that specific reaction is established based on robust evidences (in vitro, ex vivo, in vivo). Additional enzymes whose involvement in the same reactions is less robustly demonstrated or based only on in silico or cell-free assay are reported in Table 2. The role of 17βHSD3 is disregarded in this figure because restricted to tissues that are not assessed in the present review (testes, prostate, Table 2).
Color codes:
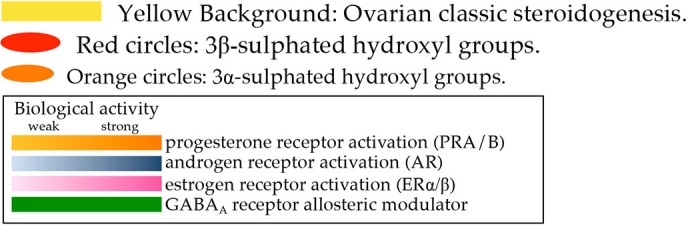
OV ovarian specific referring to 3β-HSD2 (see text); — dotted arrows indicate reactions that are not fully demonstrated to occur or for which the responsible enzyme is not identified yet; (enzyme name) enzymes indicated by brackets are supposed to catalyze the indicated reaction based on the theoretical assumptions, no experimental proof is yet available; & these compounds (THP, 3αDHP and allopregnandiol) exist as various hydroxyl α/β isomers (3, 5, 17) with no activity, classic action or neuroactivity (see Table 2); * the role of DHRS11 in steroid metabolism is reported only recently by one publication (Endo et al., 2016).
Table 1.
Major steroidal compounds.
| 1. Abbreviation (used here) | Blood concentration ** (nM) | Biologic activity*** | Entries* | |
|---|---|---|---|---|
| 2. Common name | ||||
| 3. Chemical name | ||||
| 1. none | PREGNANES | n.d. | CAS:516-59-6 | |
| 2. none | HMDB:60408 | |||
| 3.5α-pregnan-20-ol-3-one1 | CB:0504265 | |||
| ChEBI:81469 | ||||
| 1. none | 3a. M S: 28–4910 | 3a. GABAA+ | ||
| 2. allopregnandiol (4 isomers) | 3a. F: 0.2–0.710; S: 13–2010 | |||
| 3 a. 5α-pregnane-3α,20α-diol ∧ | a.CAS:566-58-5 | |||
| b. 5α-pregnane-3β,20β-diol | b.CAS:516-53-0 | |||
| c. 5α-pregnane-3β,20β-diol | c.CAS:516-53-0 | |||
| d. 5α-pregnane-3β,20α-diol | d.CAS:516-53-0 | |||
| 1.5αDHP | F: 0.2–1.1(5, 10) | PR+ GABAA+ | CAS:566-65-4 | |
| 2. allopregnanedione | HMDB:0003759 | |||
| 3.5α-pregnane-3,20-dione | ChEBI:28952 | |||
| 1. none | n.d. | CAS:570-59-2 | ||
| 2. none | CB:4441841 | |||
| 3.5α-pregnan-17α-ol-3,20-dione | ||||
| 1. none | n.d. | CAS:6890-65-9 | ||
| 2. none | CB:7269033 | |||
| 3.5α-pregnan-3,17α-diol-20-one 2∧ | ||||
| 1. THP (isomer 1/4) | All: 0.2–106 | GABAA+ | CAS:516-54-1 | |
| 2. allopregnanolone3 | M: 0.1–0.210; S: 3.6–1010 | HMDB:0001449 | ||
| 3.3α-hydoxy-5α-pregnan-20-one | F: 0.1–0.210; S: 4.0–6.710 | PC:262961 | ||
| 1. THP (isomer 2/4) | M S: 8.6–1810 | GABAA+ | CAS:128-20-1 | |
| 2. pregnanolone3 | F: 0.06–0.110; S: 5.5–1010 | HMDB:0062782 | ||
| 3.3α-hydroxy-5β-pregnan-20-one | CHEBI:1712 | |||
| PC:31402 | ||||
| 1. THP (isomer 3/4) | M S: 7.8–1010 | GABAA− | CAS:516-55-2 | |
| 2. isopregnanolone3 | F: 0.08–0.210; S: 3.7–7.110 | (THP-S) | HMDB:0001455 | |
| 3.3β-hydoxy-5α-pregnan-20-one | PC:92787 | |||
| 1. THP (isomer 4/4) | All: 0.3–36 | CAS:128-21-2 | ||
| 2. epipregnanolone3 | M S: 0.4–0.610 | GABAA− | HMDB:0001471 | |
| 3.3β-hydoxy-5β-pregnan-20-one | F: 0.02–0.0410; S: 1.5–2.510 | (THP-S) | PC:228491 | |
| 1.3αDHP | PREGNENES | n.d. | GABAA+ | CAS:25680-68-6 |
| 2.3α-dihydroprogesterone | PC:121951 | |||
| 3.4-pregnen-3α-ol-20-one | ||||
| 1.3βDHP4 | n.d. | PC:121951 | ||
| 2.3β-dihydroprogesterone | ||||
| 3.4-pregnen-3β-ol-20-one | ||||
| 1. P | M: 0–0.46 | PR+ | HMDB:01830 | |
| 2. progesterone | Fpre: 0–806 | |||
| 3.4-pregnene-3,20-dione | Fpost: 0–0.46 | |||
| 1.17OHP | M: 0.61–7.06 | PR+ | CAS:68-96-2 | |
| 2.17α-hydroxyprogesterone | F: 0.21–2.36 | HMDB:0000374 | ||
| 3.17-hydroxypregn-4-en-3,20-dione | CHEBI:17252 | |||
| PC:6238 | ||||
| 1.20αDHP | PREGNENES | Fpre: 0.8–11.76 | PR+ | CAS:145-14-2 |
| 2.20α-dihydroprogesterone | HMDB:0003069 | |||
| 3.20α-hydroxypreg-4-en-3-one | PC:8956 | |||
| 1.17OHP5 | M: 1.0–12 6 | CAS:387-79-1 | ||
| 2.17-hydroxypregnenolone | F: 0–6.06 | HMDB:0000363 | ||
| 3.5-Pregnen-3β,17α-diol-20-one | CHEBI:28750 | |||
| PC:3032570 | ||||
| 1. P5 | M: 1–156; S: 200–1,0006 | GABAA− (P5-S) | CAS:145-13-1 | |
| 2. pregnenolone | Fpre: 1.0–156; S: 100–1,0006 | HMDB:0000253 | ||
| 3. pregn-5-en-3β-ol-20-one | Fpost: 1.0–156; S: 10–5006 | CHEBI:16581 | ||
| PC:8955 | ||||
| 1. none | ANDROSTANES | HMDB:0000899 | ||
| 2. androstanedione | M: 0.37 | CHEBI:22542 | ||
| 3.5α-androstane-3,17-dione | ||||
| 1. AN | All: 0.5–0.97 | AR+ weak | HMDB:0000031 | |
| 2. androsterone | M: 0.4–4.06,10; S: 617–1,08010 | GABAA+ | ||
| 3.3α-hydroxy-5α-androstan-17-one | F: 0.3–0.610; S: 359–1,07010 | |||
| 1.5βAN | M: 0.09–0.210; S: 32–7010 | GABAA+ | CAS:53-42-9 | |
| 2. etiocholanolone | F: 0.1–0.4 10; S: 34–8810 | HMDB:00490 | ||
| 3.3α-hydroxy-5β-androstan-17-one | CHEBI:28195 | |||
| PC:5880 | ||||
| 1.3αDIOL | M: 0.4–0.59,10; S: 35–12110 | ERβ+ weak | HMDB:0000495 | |
| 2. androstanediol | F: 0.03–0.06 10; S: 2.4–4.810 | GABAA+ | ||
| 3.5α-androstane-3α,17β-diol | ||||
| 1.3βDIOL | All: 0.157 | |||
| 2.3β-androstanediol | M S: 34–10310 | ERβ+ | HMDB:0000493 | |
| 3.5α-androstane-3β,17β-diol | F S: 8.7–1810 | |||
| 1. EPI | M: 0.3–0.79,10; S: 211–53210 | AR+ weak | CAS:481-29-8 | |
| 2. epiandrosterone | F: 0.3–0.710; S: 172–35010 | HMDB:0000365 | ||
| 3.3β-hydroxy-17-oxo-5α-androstane | CHEBI:541975 | |||
| PC:441302 | ||||
| 1. DHT | M: 0/85–3.5 (50–100)6 | AR+ | HMDB:0002961 | |
| 2. dihydrotestosterone | Fpre: 0.08–1.36 | CHEBI:16330 | ||
| 3.17β-hydroxy-5α-androstan-3-one | Fpost: 0.03–1.656 | PC:10635 | ||
| ANDROSTENES | CAS:481-30-1 | |||
| 1. EpiT8 | M: 1.3–2.97 | AR+ weak9 | HMDB:0000628 | |
| 2. epitestosterone | CHEBI:42534 | |||
| 3.17α-hydroxy-4-androsten-3-one | CB:10204 | |||
| CAS 521-17-5 | ||||
| 1. A5 | M: 2.6–3.79,10; S: 243–49410 | AR+ weak | HMDB:0003818 | |
| 2. androstenediol | F: 0.8–1.110,11; S: 85–30210 | CHEBI:2710 | ||
| 3. androst-5-ene-3β,17β-diol | PC:10634 | |||
| 1.17αA5 | n.d. | AR+ weak | CAS:521-17-5 | |
| 2.17α- androstenediol | GAB AA− | HMDB:0003818 | ||
| 3. androst-5-ene-3β,17α-diol | CHEBI:2710 | |||
| PC:10634 | ||||
| 1. Δ4-A5 | n.d. | CAS:1156-92-9 | ||
| 2.4-androstenediol | HMDB:0005849 | |||
| 3. androst-4-ene-3β,17β-diol | PC:12476620 | |||
| 1. DHEA | M: 10–256; S: 2K-10K6 | GABAA− | HMDB:0000077 | |
| 2. dehydroepiandrosterone | Fpre: 3.0–306; S: 1K-8K6 | (DHEA and DHEA-S) | ||
| 3. (3β)-3-hydroxyandrost-5-en-17-one | Fpost: 2.0–206; S: 1K-6K6 | |||
| 1. Abbreviation (used here) | Blood concentration ** (nM) | Biologic activity*** | Entries* | |
| 2. Common name | ||||
| 3. Chemical name | ||||
| 1. A4 | ANDROSTENES | All: 3.1–5.97 | AR+ | CAS:63-05-8 |
| 2. androstenedione | HMDB:0000053 | |||
| 3.4-Androstene-3,17-dione | CHEBI:16422 | |||
| 1. T | M: 5–256 | CAS:55-22-0 | ||
| 2. testosterone | Fpre: 0.2–2.06 | AR+ | HMDB:0000234 | |
| 3.17β-hydroxyandrost-4-ene-3-one | Fpost: 0.2–1.06 | CHEBI:17347 | ||
| 1. E2 | ESTROGENS | M: 0.02–0.046 | CAS:50-28-2 | |
| 2.17β-estradiol | Fpre: 0.005–1.06 | ER+ | HMDB:0000151 | |
| 3. (17β)-estra-1,3,5(10)-triene-3,17-diol | Fpost: 0.005–0.086 | CHEBI:16469 | ||
| 1. E1 | M: 0.033–0.16; S: 2.0–4.06 | CAS:53-16-7 | ||
| 2. estrone | Fpre: 0.015–0.5; S: 2.0–5.06 | ER+ | HMDB:0000145 | |
| 3.3-hydroxy-1,3,5(10)-estratrien-17-one | Fpost: 0.01–0.12; S: 5–20(X10−3) 6 | CHEBI:17263 | ||
List of the steroids discussed in the present review with the major features. Nomenclature of these compounds is variable and aliases are given as Supplemental Materials.
CAS: Chemical Abstracts Service, a division of the American Chemical Society (www.cas.org. Accessed on date: February 2018); HMDB: Human Metabolome Data Base (www.hmdb.ca. Accessed on date: February 2018) (Wishart et al., 2013); CB: Chemical Book (www.chemicalbook.com. Accessed on date: February 2018); ChEBI (www.ebi.ac.uk/chebi. Accessed on date: February 2018) (Morgat et al., 2015); PC: PubChem (www.ncbi.nlm.nih.gov; pubchem.ncbi.nlm.nih.gov. Accessed on date: February 2018) (Kim et al., 2016).
M: male subjects; F: female subjects; Fpre: female premenopausal subjects; Fpost: female postmenopausal subjects; -S: sulphated compounds.
PR, ER, AR: compound activates the indicated steroid receptor; GABAA allosteric positive (+) or negative (–) modulator.
This isomer is shown in Figure 2.
n.d.: not determined.
20β-/5β-isomers exist (CB8678436, Chemical Book - www.chemicalbook.com. Accessed on date: February 2018); 2Isomer 5α-pregnan-3β,17α-diol-20-one exists (CB:0291774, Chemical Book - www.chemicalbook.com. Accessed on date: February 2018); 3In general, 5α-reduced and 3α-hydroxysteroids are positive allosteric modulator of GABAA, whereas 3α- and 3β-sulphated hydroxysteroids and 5β-reduced steroids are negative allosteric modulator of GABAA. The 3β-hydroxy isomers of THP are inactive (Belelli and Lambert, 2005; Gibbs et al., 2006; 4This compound is GABAA receptor inactive; 5Pearson Murphy et al., 2001; 6Mueller et al., 2015), 7Data extracted from the Human Metabolome Data Base-HMDB (www.hmdb.ca. Accessed on date: February 2018) (Wishart et al., 2013); 8This compound is strong inhibitor of SRD5As. 9Kancheva et al. (2007) and 10Bicikova et al. (2013).
Table 2.
Major enzymes involved in steroidogenesis.
| Chromosome | Protein (aa)** | ||
|---|---|---|---|
| 1. Abbr. | Gene size* | Dalton | 1. Name 2. Family |
| 2. Gene ID | mRNA size* | Localization (L)*** | 3. Catalysis 4. Substrates**** |
| 3. Gene name(s) | Exons (no) | 5. Distribution 6. Cofactor | |
| 1. StAR | Chr: 8p11.23 | 1. steroidogenic acute regulatory protein | |
| 2. 6770 | gene: 8.6 | aa: 285 | 2. cytochrome P450 |
| 3. STAR, STARD1 | mRNA: 1.6 | Dalton: 31,914 | 3. facilitate transport of cholesterol to mitochondria |
| Exons: 8 | L: mitochon | 4. cholesterol | |
| 5. restricted (adrenal, testis, ovary, placenta) | |||
| 1. CYP11A1 | 1. cytochrome P450 side-chain cleavage enzyme | ||
| 2. 1583 | Chr: 15q24.1 | 2. cytochrome P450, type I | |
|
3. CYP11A1; CYP11A; CYPXIA1; P450SCC |
Gene: 30.0 | aa: 521 | 3. cleavage of cholesterol side-chain |
| mRNA: 2.0 | Dalton: 60,102 | 4. cholesterol→P5 | |
| Exons: 9 | L: mitochon | 5. restricted (adrenal, testis, ovary, placenta) | |
| 6. NADP/NADPH | |||
| 1. CYP17A1 | Chr: 10q24.32 | 1. steroid 17α-hydroxylase/17,20-lyase | |
| 2. 1586 | Gene: 6.6 | aa: 508 | 2. cytochrome P450, type II |
| 3. CYP17A1; CPT7; CYP17; S17AH; P450C17 | mRNA: 1.9 | Dalton: 57,371 | 3. 17α-hydroxylase and 17,20-lyase activities |
| Exons: 8 | L: EndRet | 4. P5→DHEA; P→A4$; 5αDHP→androstanedione; THP→ 5α-pregnan-3,17α-diol-20-one | |
| 5. restricted (adrenal, testis, ovary, placenta) | |||
| 6. NADP/NADPH | |||
| 1. CYP19A1 | Chr: 15q21.1 | 1. cytochrome P450 aromatase | |
| 2. 1588 | Gene: 130.6 | aa: 503 | 2. cytochrome P450, type II |
| 3. CYP19A1; ARO; ARO1; CPV1; CYAR; CYP19; CYPXIX; P-450AROM | mRNA: 1.5–4.5 | Dalton: 57,883 | 3. oxidative demethylation of C19 to C18 (aromatisation) |
| Exons: 10 | L: EndRet | 4. A → E1; T → E2 | |
| 5. restricted (adrenal, testis, ovary, placenta) | |||
| 6. NADP/NADPH | |||
| 1. 3βHSD1 | Chr: 1p11–12 | 1. 3β-hydroxysteroid dehydrogenase/Δ5 → 4 isomerase type I | |
| 2. 3283 | Gene: 8.1 | aa: 373 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD3B1; HSD3B; HSDB3; SDB3A; (more∧∧) | mRNA: 1.7 | Dalton: 42,252 | 3. oxidative conversion of Δ5 3β-hydroxyl to Δ4 keto-steroids |
| Exons: 4 | L: membrane | 4. P5→P; 17OHP5→17OHP4; DHEA→A4; A5→T; 17αA5→EpiT | |
| 5. selectively distributed (placenta, periphery) | |||
| 6. NADP/NADPH or NAD/NADH | |||
| 1. 3βHSD2 | Chr: 1p11–13 | 1. 3β-hydroxysteroid dehydrogenase/Δ5→4 isomerase type II | |
| 2. 3284 | Gene: 8.1 | aa: 372 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD3B2; HSDB; HSD3B; SDR11E2 | mRNA: 1.7 | Dalton: 42,052 | 3. oxidative conversion of Δ5-3β-hydroxyl to Δ4-ketosteroids |
| Exons: 4 | L: mitochon | 4. P5→P; 17OHP5→17OHP4; DHEA→A4 | |
| 5. restricted (adrenal, testis, ovary) | |||
| 6. NADP/NADPH or NAD/NADH | |||
| 1. 17βHSD1 | Chr: 17q11–21 | 1. 17β-hydroxysteroid dehydrogenase type 1 | |
| 2. 3,292 | Gene: 6.0 | aa: 328 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B1 | mRNA: 1–2.4 | Dalton: 34,950 | 3. reduction of 17-keto to 17β-hydroxyl (estrogens) |
| E2DH; HSD17; EDHB17; EDH17B2; SDR28C1; (more∧∧) | Exons: 6 | L: cytoplasm | 4. (established) E1→E2; (A4→T in rodents) (postulated) DHEA→A51; P→20αDHP2; |
| DHT→3βDIOL11; DHT→ androstanedione11 | |||
| 5. selectively distributed (ovary, placenta (low in endometrium, breast)14,15 | |||
| 6. NADP/NADPH | |||
| 1. 17βHSD2 | Chr: 16q24.1–2 | 1. 17β-hydroxysteroid dehydrogenase type 2 | |
| 2. 3294 | Gene: 63 | aa: 387 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B2 HSD17; SDR9C2; EDH17B2 | mRNA: 1.5 | Dalton: 42,785 | 3. oxidation of 17β-hydroxyl to 17-keto (estrogens & androgens) |
| Exons: 5 | L: EndRet |
4. (established) E2→E1; T→A4; DHT→androstanedione1,10; 20αDHP→P16; 5α-pregnan-20-ol -3-one→5αDHP16; A5→DHEA1; 3αDIOL→AN5 (postulated) 3αDIOL→AN(1, 10); DHT→androstanedione1; A5→DHEA1; allopregnandiol→ THP16 |
|
|
5. selectively distributed (liver, intestine, endometrium, placenta, pancreas, prostate, colon, kidney. Negative in heart, brain, skeletal muscle, spleen, thymus, ovary, or testis)(14, 17) |
|||
| 6. NAD/NADH | |||
| 1. 17βHSD3&& | Chr: 9q22 | 1. 17β-hydroxysteroid dehydrogenase type 3 | |
| 2. 3293 | Gene: 67 | aa: 310 | 2. short chain dehydrogenase/reductase superfamily |
|
3. HSD17B3 EDH17B3; |
mRNA: 1.2 | Dalton: 34,516 | 3. reduction of 17-keto to 17β-hydroxyl (androgens) |
| Exons: 11 | L: EndRet |
4. (established) A4→T (postulated) AN→3αDIOL(1, 3, 10); androstanedione→DHT(1, 9, 10) |
|
| 5. restricted (testis; low in brain, blood, skin, adipose tissue)14 | |||
| 6. NADP/NADPH | |||
| 1. 17βHSD4 | Chr: 5q23.1 | aa: 736 | 1. 17β-hydroxysteroid dehydrogenase type 4 |
| 2. 3295 | Gene: 184 | Dalton: 79,686 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B4 | mRNA: 2.9 | L: Peroxisome mitochon | 3. fatty acid β-oxidation (steroids in pigs) |
| DBP; MFE-2; MPF-2; PRLTS1; SDR8C1 | Exons: 28 |
4. (established) very long chain branched fatty acids, bile acids (postulated) A5→DHEA1; E2→E114 |
|
| 5. ubiquitous (liver, heart, prostate, testis, lung, skeletal muscle, kidney, pancreas, thymus, ovary, intestine, placenta, brain, spleen, colon, lymphocytes)14 | |||
| 6. NAD/NADH | |||
| 1. 17βHSD6 | Chr: 12q13 | aa: 317 | 1. 17β-hydroxysteroid dehydrogenase type 6 |
| 2. 8630 | Gene: 24.5 | Dalton: 35,966 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B6 | mRNA: 1.6 |
L: EndRet microsomes |
3. 3α-3β-epimerase; 17β-hydroxyl oxidation (5α-reduced steroids); retinoids |
| HSE; RODH; SDR9C6 | Exons: 8 |
4. (established) 3αDIOL→DHT10; AN→androstanedione5; AN→EPI (postulated) 3αDIOL→AN5; E2→E15 |
|
| 5. selectively distributed (liver, testis, lung, spleen, brain, ovary, kidney, adrenal, prostate)14 | |||
| 6. NAD/NADP | |||
| 1. 17βHSD7 | Chr: 1q23 | 1. 17β-hydroxysteroid dehydrogenase type 7 | |
| 2. 51478 | Gene: 22.1 | aa: 341 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B7 | mRNA: 1.5 | Dalton: 38,206 | 3. 3-ketosteroid reductase of sterols |
| PRAP; SDR37C1 | |||
| Exons: 9 | L: EndRet | 4. (established) Sterols/cholesterol biosynthesis; DHT→3βDIOL1 | |
| 5. widely distributed (ovary, uterus, placenta, liver, breast, testis, neuronal tissue, adrenal gland, small intestine, prostate, adipose tissue lung, and thymus)(14, 18) | |||
| 6. NADP/NADPH | |||
| 1. 17βHSD8 | Chr: 6p21.3 | 1. 17β-hydroxysteroid dehydrogenase type 8 | |
| 2. 7923 | Gene: 2.2 | aa: 261 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B8 | mRNA: 1.0 | Dalton: 26,974 | 3. fatty acid elongation; steroid 17βHSD action (rodents). |
| KE6; FABG; HKE6; FABGL; RING2; H2-KE6; (more∧∧) | Exons: 9 | L: mitochon | 4. (established) fatty acids (postulated) E2→E1 |
| 5. widely distributed (prostate, placenta, kidney, brain, cerebellum, heart, lung, small intestine, ovary, testis, adrenal, stomach, liver, adrenals)14−19 | |||
| 6. NAD/NADP | |||
| 1. 17βHSD9 | Chr: 12q23 | 1. 17β-hydroxysteroid dehydrogenase type 9 | |
| 2. 5959 | Gene: 4.4 | aa: 318 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B9 | mRNA: 1.4 | Dalton: 34,979 | 3. retinoid metabolism (steroid metabolism in rodents) |
| RDH5; (more∧∧) | Exons: 4 | L: EndRet | 4. (established) retinoids (postulated) AN→3αDIOL1; androstanedione→DHT1 |
| 1. 17βHSD10 | Chr: Xp11.2 | 1. 17β-hydroxysteroid dehydrogenase type 10 | |
| 2. 3028 | Gene: 3.1 | aa: 261 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B10 | mRNA: 0.9 | Dalton: 26,923 | 3. fatty acids & steroid oxidation; tRNA maturation |
| ABAD; CAMR; ERAB; HCD2; MHBD; HADH2; MRPP2; MRX17; MRX31; (more∧∧) | Exons: 6 | L: mitochon |
4. (established) Isoleucine, fatty acid, bile acid metabolism, THP→5αDHP(20, 34) (postulated) 3αDIOL→AN1,9; DHT→androstanedione1,9; T→A41 |
| 5. nearly ubiquitous (liver, small intestine, colon, kidney, heart, brain, placenta, lung, ovary, testis, spleen, thymus, prostate, leukocyte)14 | |||
| 6. NAD/NADH | |||
| 1. 17βHSD11 | Chr: 4q22.1 | 1. 17β-hydroxysteroid dehydrogenase type 11 | |
| 2. 51170 | Gene: 54.9 | aa: 300 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B11 | mRNA: 1.9 | Dalton: 32,936 | 3. Short-chain alcohol dehydrogenases |
| DHRS8; PAN1B; RETSDR2; SDR16C2; (more∧∧) | Exons: 7 | L: EndRet | 4. (established) lipids, sec. alcohols/ketones (postulated) 3αDIOL→AN1,9 |
| 5. nearly ubiquitous (liver, intestine, kidney, adrenal gland, heart, lung, testis, ovary, placenta, sebaceous gland and pancreas)14,21 | |||
| 6. NAD/NADH | |||
| 1. 17βHSD12 | Chr: 11p11.2 | 1. 17β-hydroxysteroid dehydrogenase type 12 | |
| 2. 51144 | Gene: 170.1 | aa: 312 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B12 | mRNA: 2.6 | Dalton: 34,324 | 3. fatty acid elongation, steroid 17βHSD reductive action (rodents) |
| KAR; SDR12C1 | Exons: 11 | L: EndRet | 4. (established) branched/long chain fatty acids (postulated) E1→E2 |
| 5. ubiquitous (heart, skeletal muscle, liver, kidney, adrenal gland, testis, placenta, brain, pancreas, GIT, trachea, lung, thyroid, prostate, aorta, bladder, spleen, skin, ovary, breast, uterus, vagina)(14, 22) | |||
| 6. NADP/NADPH | |||
| 1. 17βHSD13 | Chr: 4q22.1 | 1. 17β-hydroxysteroid dehydrogenase type 13 | |
| 2. 345275 | Gene: 19.1 | aa: 300 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B13 | mRNA: 2.3 | Dalton: 33,655 | 3. and 4. unknown |
| SCDR9; NIIL497; (more∧∧) | Exons: 6 | L: extracell/EndRet |
5. restricted (liver; low in bone marrow, lung, ovary, testis, kidney, skeletal muscle brain, bladder)14 |
| 1. 17βHSD14 | Chr: 19q13.33 | 1. 17β-hydroxysteroid dehydrogenase type 14 | |
| 2. 51171 | Gene: 23.7 | aa: 270 | 2. short chain dehydrogenase/reductase superfamily |
| 3. HSD17B14 | mRNA: 1.3 | Dalton: 28,317 | 3. fatty acid & prostaglandin metabolism; 17βHSD activity |
| DHRS10; SDR47C1; retSDR3 | Exons: 8 | L: cytoplasm |
4. (established) fatty acids (postulated) 3αDIOL→AN1,9; E2→E14; T→A44; A5→DHEA5 |
| 5. widely distributed (brain, liver, placenta, breast)14 | |||
| 6. NAD/NADH | |||
| 1. 17βHSD15 | Chr: 14q24.1 | 1. retinol dehydrogenase 11 | |
| 2. 51109 | Gene: 19.0 | aa: 318 | 2. short chain dehydrogenase/reductase superfamily |
| 3. RDH11; PSDR1; ARSDR1; (more∧∧) | mRNA: 1.8 | Dalton: 35,386 | 3. dehydrogenase activity of retinoid and steroids |
| Exons: 9 | L: cytoplasm | 4. (established) retinoids (post.) AN→3αDIOL1,9; androstanedione→DHT1,9 | |
|
5. widely distributed 6. NADP/NADPH |
|||
| 1. DHRS1123 | Chr: 17q12 | 1. dehydrogenase/reductase 11 | |
| 2. 79154 | Gene: 9.0 | aa: 260 | 2. short chain dehydrogenase/reductase superfamily |
| 3. DHRS11 | mRNA: 1.6 | Dalton: 28,308 | 3. steroid 17HSD & 3βHSD activities; bile acids metabolism |
| ARPG836; SDR24C1; spDHRS11 | Exons: 7 | L: extracell |
4. E1→E2; A4→T; DHEA→A5; androstanedione→DHT; AN→3αDIOL; P→3αDHP23 5. nearly ubiquitous (testis, small intestine, colon, kidney)23 6. NADP/NADPH |
| 1. AKR1C1 | Chr: 10p14–15 | 1. aldo-ketoreductase family 1 member C1 | |
| 2. 1645 | Gene: 20.0 | aa: 323 | 2. aldo-ketoreductase family |
| 3. AKR1C1 | mRNA: 12 | Dalton: 36,788 | 3. 20αHSD (strong) and 17βHSD (weak) activities; moderate 3-keto reduction to 3β-hydroxyl (> 3α) |
| C9, DDH, DDH1, DD1, H-37, HBAB, MBAB HAKRC; DD1/DD2; 2-ALPHA-HSD; 20-ALPHA-HSD | Exons: 9 | L: cytoplasm |
4. (established) P→20αDHP6; 5αDHP→5α-pregnan-20-ol-3-one6; THP→allopregnandiol6; DHT→3βDIOL7; androstanedione→DHT7; 5α-pregnan-20-ol-3-one→allopregnandiol16; 5αDHP→THP16 (post.) DHT→3αDIOL7; A4→T7; E1→E27; 3αDIOL→AN7; 20αDHP→ P7; DHT→3βDIOL24; 5α-pregnan-17α-ol-3,20-dione→5α-pregnan-3,17α-diol-20-one16 |
| 5. ubiquitous | |||
| 6. NADP/NADPH or NAD/NADH | |||
| 1. AKR1C2 | Chr: 10p14–15 | 1. aldo-ketoreductase family 1 member C2 | |
| 2. 1646 | Gene: 30.6 | aa: 323 | 2. aldo-ketoreductase family |
|
3. AKR1C2 DD; DD2; TDD; BABP; DD-2; DDH2; HBAB; HAKRD; MCDR2; SRXY8; DD/BABP; AKR1C-pseudo |
mRNA: 1.3 Exons: 9 |
Dalton: 36,735 L: cytoplasm |
3. 20αHSD (weak) and 17βHSD activities; 3-keto reduction to 3α- hydroxyl; bile-acid binding protein activity |
|
4. (established) DHT→3αDIOL7,12; 5αDHP→THP7; androstanedione→AN25; 5α-pregnan-20-ol-3-one→ allopregnandiol16; 5αDHP→THP16; 5α-pregnan-17α-ol-3,20-dione→5α-pregnan-3,17α-diol-20-one16 (postulated) A4→ T7; E1→E27; P→20αDHP7; 3αDIOL→ DHT7; T→A47 |
|||
| 5. ubiquitous | |||
| 6. NADP/NADPH or NAD/NADH | |||
| 1. AKR1C3 | Chr: 10p14–15 | 1. aldo-ketoreductase family 1 member C3 | |
| 2. 8644 | Gene: 13 | aa: 323 | 2. aldo-ketoreductase family |
|
3. HSD17B5 AKR1C3 DD3; DDX; PGFS; HAKRB; HAKRe; HA1753; HSD17B5; hluPGFS |
mRNA: 1.2 Exons: 9 |
Dalton: 36,853 L: cytoplasm |
3. 20αHSD (weak) and 17βHSD activities (androgens); 3-keto reduction to 3α-/β-hydroxyl (weak); 11-ketoprostaglandin reductase3 |
| 4. (established) A4→T7; DHT→3αDIOL7; 3αDIOL→AN7; 5αDHP→ THP7; 5α-pregnan-20-ol-3-one→ allopregnandiol16; 5αDHP→THP16; DHEA→A57; 5α-pregnan-17α-ol-3,20-dione→5α-pregnan-3,17α-diol-20-one16; androstanedione→DHT24 (postulated) E1→E27;T→A47; 20αDHP→ P7 | |||
| 5. nearly ubiquitous (prostate, mammary gland, liver, kidney, lung, heart, uterus, testis, brain, skeletal muscle, adipose tissue, pancreas, hearth, skeletal muscle, thymus, ovary, small intestine and colon)14,26 | |||
| 6. NADP/NADPH or NAD/NADH | |||
| 1. AKR1C4 | Chr: 10p15.1 | 1. aldo-ketoreductase family 1 member C4 | |
| 2. 1109 | Gene: 25.2 | aa: 323 | 2. aldo-ketoreductase family |
| 3. AKR1C4 | mRNA: 1.2 | Dalton: 37,067 | 3. 20αHSD (weak) and 17βHSD activities; 3-keto reduction to 3α-hydroxyl (>3β). |
| C11; CDR; DD4; CHDR; DD-4; HAKRA; | Exons: 9 | L: cytoplasm |
4. (established) DHT→3αDIOL7,10; androstanedione→AN7,8; other$$$ (postulated) A4→ T7; E1,→E27; P→20αDHP7; 3αDIOL→DHT7 |
| 5. restricted (liver) 6. NADP/NADPH or NAD/NADH | |||
|
1. SRD5A1 2. 6715 3. SRD5A1 S5AR 1 |
Chr: 5p15.31 Gene: 41.0 mRNA: 2.3 Exons: 5(7) |
aa: 259 Dalton: 29,459 L: EndRet |
1. steroid 5α-reductase 1 2. steroid 5α reductase family 3. androgen and pregnene metabolism 4. T→DHT; A4→androstanedione; 17OHP4→5α-pregnan-17α-ol-3,20-dione; P→5αDHP; 20αDHP→5α-pregnan-20-ol-3-one 5. ubiquitous |
| 1. SRD5A2 | Chr: 2p23.1 | 1. steroid 5α-reductase 2 | |
| 2. 6716 | Gene: 178.3 | aa: 254 | 2. steroid 5α reductase family |
| 3. SRD5A2 | mRNA: 2.5 | Dalton: 28,393 | 3. androgen and pregnene metabolism |
| Exons: 5 | L: microsomes | 4. T→DHT; A4→androstanedione | |
| 5. restricted (prostate and androgen sensitive tissues) | |||
| 1. SRD5A3 | Chr: 4q12 | 1. steroid 5α-reductase 3 | |
| 2. 79644 | Gene: …. | aa: 318 | 2. steroid 5α reductase AND polyprenol reductase subfamily |
| 3. SRD5A3 | mRNA: 4.1 | Da: 36,521 | 3. androgen and pregnene metabolism |
| CDG1P; CDG1Q; KRIZI; SRD5A2L; SRD5A2L1 | Exons: 6 | L: EndRet | 4. T→DHT; A4→androstanedione; 17OHP4→5α-pregnan-17α-ol-3,20-dione; P→5αDHP; 20αDHP→5α-pregnan-20-ol-3-one |
| 5. ubiquitous | |||
| 1. STS | Chr: Xp22.31 | 1. steroid sulphatase | |
| 2. 412 | Gene: 208.3 | aa: 583 | 2. sulphatase |
| 3. STS | mRNA: 6.4 | Dalton: 65,492 | 3. hydrolyses several 3β-hydroxysteroid sulfates |
| ES; ASC; XLI; ARSC; SSDD; ARSC1 | Exons: 16 | L: microsomes EndRet | 4. sulpho conjugated cholesterol, E1, E2, DHEA, P5, 17OHP5S, A5, EPI |
| 5. ubiquitous (lung, aorta, thyroid, uterus, liver and testis)27−30 | |||
| 1. SULT1E1 | Chr: 4q13.3 | 1. estrogen sulphotransferase | |
| 2. 6783 | Gene: 50.0 | aa: 35126 | 2. sulphotransferase 1 |
| 3. SULT1E1 | mRNA: 1.8 | Dalton: 35,126 | 3. sulpho-conjugation of steroids |
| EST; STE; EST-1; ST1E1; (more∧∧) | Exons: 9 | L: cytoplasm | 4. E1, DHEA (low affinity for E2) |
|
5. moderately distributed (liver, adrenal, small intestine; low in brain, lung, testis, leukocytes, placenta, salivary gland, stomach, thymus, trachea, uterus, kidney)(30, 31) |
|||
| 1. SULT2A1 | Chr: 19q13.3 | 1. dehydroepiandrosterone sulphotransferase | |
| 2. 6822 | Gene: 15.9 | aa: 285 | 2. sulphotransferase 1 |
| 3. SULT2A1 | mRNA: 2.0 | Dalton: 33,780 | 3. sulpho-conjugation of steroids, bile acids |
| HST; ST2; STD; hSTa; DHEAS; ST2A1; | Exons: 6 | L: cytoplasm | 4. DHEA, P5, AN, 17OHP532, A532, AN33, EPI, bile acids |
|
5. restricted (liver, adrenal, small intestine (low in colon, hearth, prostate, stomach, testis, thyroid)30 |
|||
| 1. SULT2B1 | Chr: 19q13.33 | 1. alcohol sulphotransferase | |
| 2. 6820 | Gene: 48.5 | aa: 365 | 2. sulphotransferase 1 |
| 3. SULT2B1 | mRNA: 1.3 | Dalton: 41,308 | 3. sulpho-conjugation of steroids |
| HSST2; ARCI14 | Exons: 7 | L: cytoplasm | 4. cholesterol, DHEA |
| 5. moderately distributed (placenta, prostate, lung (low in kidney, salivary gland, small intestine, trachea)30 | |||
| 1. SULT1A1 | Chr: 16p11.2 | 1. phenol sulphotransferase 1 | |
| 2. 6817 | Gene: 18.4 | aa: 295 | 2. sulphotransferase 1 |
| 3. SULT1A1 | mRNA: 1.3 | Dalton: 34,165 | 3. sulpho-conjugation of steroids |
| PST; STP; STP1; P-PST; ST1A1; ST1A3; TSPST1; HAST1/HAST2 | Exons: 13 | L: cytoplasm | 4. E2 |
| 5. nearly ubiquitous (adrenal, bone marrow, brain, colon, hearth, kidney, liver, lung, pancreas, leukocytes, placenta, prostate, salivary gland, skeletal muscle, small intestine, spinal cord, spleen, stomach, testis, thymus, thyroid, trachea, uterus)30 |
List of all enzymes discussed in the present review with the major features. Gene and gene product nomenclature is complex and variable and alias are given as Supplemental Materials. Gene structure (chromosome location, gene length), transcript features (length, exons) and protein characteristics (amino-acid length, molecular weigh and cell localization) were obtained from GeneCards (www.genecards.org. Accessed on date: February 2018) (Stelzer et al., 2016).
Length in kilo nucleotides.
number of amino-acids.
Abbreviations: EndRet: endoplasmic reticulum; extracell: extracellular; mitochon: mitochondria.
For some enzymes, substrate specificity based on robust evidences are indicated as ‘established’, whereas other reactions whose catalyzes is supported by less robust experimental evidences (mostly using recombinant proteins in vitro/cell-free assays) are indicated as “postulated.”
This reaction of CYP17A1 does not occur in vivo in humans (Miller and Auchus, 2011).
AKR1C4 has an important detoxifying function in the liver and converts chlordecone into chlordecone alcohol.
17βHSD3 is testis specific and the reactions catalyzed by this enzyme are not reported in Figure 2.
For this gene, additional gene names exist, for details see NCBI database (https://www.ncbi.nlm.nih.gov/).
Luu-The and Labrie (2010), Labrie and Labrie (2013), and Labrie (2015); 2 Smuc and Rizner (2009), 3 Miller et al. (2012b), 4 Sivik (2012); 5 GeneCards (www.genecards.org. Accessed on date: February, 2018) Stelzer et al. (2016), 6 Smuc and Rizner (2009), 7 Penning et al. (2004), Steckelbroeck et al. (2010); 8 Jin et al. (2011), 9Manenda et al. (2016), 10Balk and Knudsen (2008), 11Gangloff et al. (2003), 12Bélanger et al. (2002), 13Perez Carrion et al. (1994), 14Möller et al. (1999), Moeller and Adamski (2009), 15Cornel et al. (2017), 16Sinreih et al. (2017b), 17Casey et al. (1994), 18Törn et al. (2003), 19Ohno et al. (2008), 20Yang et al. (2016), 21Chai et al. (2003), 22Sakurai et al. (2006), 23Endo et al. (2016). 24Rižner and Penning (2014), 25Manenda et al. (2016), 26Lin et al. (1997), 27Miki et al. (2002), 28Foster et al. (2008a), 29Purohit and Foster (2012), 30Mueller et al. (2015), 31Marchais-Oberwinkler et al. (2011), Mueller et al. (2015), 32Rege et al. (2016), 33Strott (2002), and 34Yang et al. (2016).
Ovarian steroidogenesis
Transformation of cholesterol to 17β-estradiol (E2) involves first the production of dehydroepiandrosterone (DHEA) in theca cells through the action of steroidogenic acute regulatory protein (StAR) that facilitates the transport of cholesterol into mitochondria, followed by CYP11A1 (rate-limiting) and CYP17A1 (Figure 2); the ovarian pathway is indicated by the yellow background; reviewed by (Miller and Auchus, 2011; Andersen and Ezcurra, 2014). CYP11A1 is a type I CYP localized in mitochondria that uses nicotine-adenine-dinucleotide-phosphate (NADPH) and ferredoxin (Fdx)/ferredoxin reductase (FdR) to cleave the cholesterol side chain and produce pregnenolone (P5). Type II CYP17A1, localized in the endoplasmic reticulum (EndRet), has both 17α-hydroxylase and 17,20-lyase activities. It uses NADPH and P450 oxidoreductase (POR) to first hydroxylate P5 to 17α-hydroxypregnenolone (17OHP5) (17α-hydroxylase action), followed by 17,20-lyase action to release DHEA. Gonad specific type 2 3β-hydroxysteroid dehydrogenase (3βHSD2) has 3β-dehydrogenase and Δ5 to Δ4 isomerase activities and converts DHEA to androstenedione (A4). Next, CYP19A1 catalyzes the oxidative demethylation of C19 androgens to C18 estrogens, with A-ring aromatisation; hence A4 is converted to estrone (E1). The final conversion of E1 (with low affinity for the estrogen-receptors -ERs) to E2 (high affinity for ERs and high estrogenic potency) is catalyzed by 17βHSD1 that reduces 17-keto to 17β-hydroxyl steroids. In the ovary, the 17-keto group of A4 can be reduced to 17β-hydroxyl by AKR1C3/17βHSD5 yielding testosterone (T) that is converted to E2 by CYP19A1. Upon ovulation, high 3βHSD2 levels in the corpus luteum lead to high progesterone (P) generation from P5.
Intracrine steroidogenesis
The expression of StAR, CYP11A1 and CYP17A1 is demonstrated in a limited number of peripheral tissues (see later and Tables 6–8). However, pregnenes, pregnanes, androstenes and androstanes generated from these initial steps (but also abundantly available as circulating precursors) can be further metabolized locally thus generating a plethora of compounds with various biological activities (estrogenic, androgenic, progestogenic and neuroactive; Tables 1, 2 and Figure 2). The Δ5 to Δ4 isomerization of androstenes (DHEA, androstenediol -A5- and 17αA5) and pregnenes (P5, 17OHP5) is catalyzed by 3βHSD1, which is the peripheral counterpart of ovarian 3βHSD2. Also 3βHSD2, whose expression was initially considered to be restricted to endocrine tissues, is detected peripherally in recent reports (Stoffel-Wagner, 2001; Tsai et al., 2001; Attar et al., 2009; Huhtinen et al., 2014; Osinski et al., 2018). Due to the high concentration of DHEA (both in blood and tissues), its conversion to A4 by 3βHSDs is relevant to the formation of downstream androgens and of estrogens. Additionally, 3βHSDs convert A5 and the isomer 17αA5 to T and epitestosterone (EpiT). Although minor, in the context of women's health, these pathways are relevant. A5, together with 3α and 3βDIOL (generated by AKR1Cs from DHT and AN, see below) activate both ERs and have estrogenic action (especially 3βDIOL, a potent ERβ binder). A5 possesses immune stimulatory activity whereas its 17α isomer (17αA5) has androgenic, antitumor and neuroactivity. Additionally, EpiT is a weak AR binder and a strong endogenous inhibitor of SRD5As (Loria and Graf, 2012). The endogenous occurrence of 17αA5 is demonstrated in humans (Laatikainen et al., 1971) but its route of synthesis is unclear (Shimizu, 1979). A 17αHSD able to convert A4 to EpiT and DHEA to 17αA5 is characterized in mice (Bellemare et al., 2005) but no human homologous is described yet. Similarly to the ovaries, androgen to estrogen conversion is catalyzed by CYP19A1.
A particularly important reaction is controlled by oxidative and reductive 17βHSDs, which interconvert 17-keto and 17β-hydroxysteroids. Since 17β-hydroxysteroids (T and E2) have higher affinity for the receptors than the keto-steroids (A4 and E1), this balance determines the final androgenic/estrogenic activity. Fourteen 17βHSDs exist, whose specificity is determined by tissue distribution, intracellular localization and biochemistry (Table 2); reviewed thoroughly in (Mindnich et al., 2004; Moeller and Adamski, 2006, 2009; Prehn et al., 2009; Miller and Auchus, 2011). Unpublished data also refer to a 15th 17βHSD (see Table 2; reported in Luu-The et al., 2008) with a putative role in androgen metabolism. With the exclusion of 17βHSD5 (AKR1C3, see below), all other 17βHSDs belong to the short-chain dehydrogenase (SRD) family.
Although all 17βHSDs have been postulated to use steroids as substrates based on cell-free or in vitro assays, recent investigations based on substrate specificity (Laplante et al., 2009) and knock-out (KO) models (Table 4) better clarified their roles. Type 1 17βHSD is the estrogenic enzyme and coverts E1 to E2 both in the ovary and in peripheral tissue. Type 2 17βHSD oxidizes 17-hydroxyl groups (E2 and T) to the 17-keto forms (E1 and A4), and possesses also a 20α-hydroxyl oxidative action, through which this enzyme generates P from 20αDHP. Type 6 17βHSD uses 5α-reduced androgens and has 17-hydroxyl oxidative activity (converting androsterone -AN- to androstanedione) and 3-hydroxyl oxidative activity (converting 3αDIOL to the most potent androgen dihydrotestosterone -DHT). Additional catalytic actions for 17βHSD6 (epimerase or 17-hydroxydehydrogenase) are demonstrated in vitro (Table 2). Type 14 17βHSD is postulated to have 17β-hydroxyl oxidative action on various steroids, type 7 is involved in cholesterol metabolism as indicated by KO mice (Table 4), whereas there is apparently little/no in vivo role of types 8, 9, 10, 11 and 12 17βHSDs on steroid metabolism (Table 2 and indicated by KO mice, Table 4). Recently, a novel SRD, DHRS11, was shown to possess in vitro 17-keto to 17β-hydroxyl reductive action (able to use E1, Δ5 or Δ4 androstenes, androstanes), plus reductive 3βHSD activity toward Δ4 pregnenes and other compounds (5β-steroids, bile acids; Table 2 and Figure 2; Endo et al., 2016).
Table 4.
Mouse models (knockouts - KO or transgenic-TG, i.e., ubiquitous expression of the gene, unless specified) for intracrine enzymes.
| Gene∧ | Modification MGI ID$ | Phenotype |
|---|---|---|
| SatAR | Null/KO1 MGI: 2388706 |
Endocrine (steroids) & reproductive endocrinology
- abnormal endocrine organs (adrenal, ovaries, prostate, testis). - decreased steroids and increased adrenocorticotropin level. - adrenocortical insufficiency. - loss of negative feedback regulation at hypothalamic-pituitary levels. |
|
Additional Growth retardation neo/post natal lethality (incomplete penetrance). Reproductive system: abnormal uterus; incomplete spermatogenesis; abnormal genitalia. |
||
| CYP11A1 | Null/KO2 MGI:5464022 |
Endocrine (steroids) and reproductive endocrinology - abnormal adrenal gland morphology. - increased circulating adrenocorticotropin level. - lack of steroid production. - decreased corticosterone and aldosterone levels. |
| Null/KO3 MGI: 2183813 |
Additional Neonatal lethality (rescued by steroid supplementation); abnormal mitochondrion morphology; abnormal lipid level. Reproductive system: abnormal genitalia, prostate, testis morphology and spermatogenesis; Nervous system: abnormal adrenaline and noradrenaline level; abnormal food intake, hypoactivity; postnatal growth retardation. |
|
| CYP17A1 | Null/KO4 MGI:3722780 |
Endocrine (steroids) & reproductive endocrinology - increased circulating cholesterol level. - decreased T level. - early reproductive senescence. |
| Null/KO5 MGI:3047328 Null/KO MGI:5605834 |
Additional Homozygous embryonic lethality (Ed7, between implantation and somite formation). Reproductive system: abnormal sperm flagellum morphology/asthenozoospermia; reduced male fertility. Bone: abnormal bone structure, mineral content and density. Metabolism: increased total body fat; decreased lean body mass; increased circulating creatinine level; increased fasted circulating glucose level. Nervous system: abnormal sexual interaction. |
|
| CYP19A1 | Null/KO6 MGI:2179439 |
Endocrine (steroids) and reproductive endocrinology - increased circulating cholesterol, T, DHT, FSH, LH and prolactin. - decreased circulating E2 level. - abnormal endometrium (thin, decreased uterus weight). - abnormal ovary (absence of follicles and corpus luteum, anovulation). |
| Null/KO7
MGI:2154536 Null/KO8 MGI:2389548 |
Additional Reproductive system: ovary hemorrhage and cysts; increased seminal vesicle weight and abnormal seminiferous tubule epithelium and oligozoospermia; female infertility and reduced male fertility. Metabolism: increased fat; obesity and susceptibility to weight gain. Bone: decreased bone mineral density and bone mass; increased bone resorption, osteoclast cell number; abnormal compact and trabecular bone morphology. Metabolism: increased circulating glucose and triglyceride levels; impaired glucose tolerance; insulin resistance; hepatic steatosis; abnormal liver physiology. Nervous system: abnormal short term spatial reference memory; abnormal emotion/affect behavior; abnormal barbering behavior; increased grooming behavior; abnormal locomotor activation, bradykinesia; abnormal mating frequency. |
|
| 17βHSD1 | Null/KO9 MGI:5576042 and 3799948 |
Endocrine (steroids) & reproductive endocrinology - abnormal corpus luteum morphology and decreased number. - increased ovarian E1:E2 and A4:T ratios. - increased LH level. - reduced P level. |
|
Additional Increased circulating alkaline phosphatase level, pigmentation, abnormal retinal pigmentation, abnormal lens morphology, abnormal retina morphology, abnormal retinal pigmentation. Reproductive system: increased ovary weight; reduced female fertility. Metabolism: decreased circulating glucose level. Nervous system: abnormal behavior, response to light, sleep behavior, decreased exploration in new environment; abnormal motor coordination/balance. |
||
| 17bHSD1 | TG10 |
Reproductive endocrinology - female have increased T levels. - increased E1  E2 conversion. E2 conversion.- masculinization in females. - develop benign/malignant breast, ovarian and endometrial conditions. |
| 17βHSD2 | Null/KO11 MGI:3773836 |
No clear reproductive endocrinology phenotype Additional Heterozygous mice: growth retardation at birth ant postnatal; premature death; renal degeneration. Reproductive system: 70% embryonic lethality (Ed11.5) due to placental defects (homozygous); small and abnormal placenta morphology; Nervous system: brain phenotype with enlarged ventricles; abnormal cortex morphology; impaired balance, coordination, abnormal sleep pattern, megacephaly. |
| TG12 |
Reproductive endocrinology - low T level. |
|
|
Additional Growth retardation; delayed eye opening; impaired retinoic signaling. Reproductive system: disrupted spermatogenesis. Bone: decreased bone formation (pre-pubertal age); decreased IGF-I and osteocalcin levels. |
||
| 17βHSD4 | Null/KO13 |
No clear reproductive endocrinology phenotype Additional Neonatal and postnatal lethality; postnatal growth retardation; abnormal mitochondrion morphology; abnormal bile salt level; hepatic steatosis. Reproductive system: abnormal testis and spermatid morphology; seminiferous tubule degeneration; small testis; abnormal gametogenesis; reduced male fertility. Nervous system: microgliosis; Purkinje cell degeneration; astrocytosis; axon degeneration; abnormal suckling behavior; increased anxiety-related response, tremors, ataxia, impaired coordination, hypoactivity, lethargy; abnormal gait. GIT: abnormal intestinal absorption. Metabolism: decreased body weight; abnormal lipid homeostasis and decreased fatty acid level. |
| 17βHSD7 | Null/KO14 MGI:3811923 |
Endocrine (steroids) Cholesterol biosynthesis. |
| Null/KO15 MGI:4456868 |
Additional Decreased embryo size; embryo lethality due to heart malformations (Ed10.5); abnormal blood vessel and capillary morphology. Nervous system: brain malformations; forebrain hypoplasia; increased neural tube apoptosis. |
|
| 17βHSD9 | Null/KO16
MGI: 2446073 Null/KO17 MGI:2388375 |
No clear reproductive endocrinology phenotype Additional Visual defects; abnormal eye electrophysiology, delayed dark adaptation. |
| 17βHSD10 | Null/KO18 |
No clear reproductive endocrinology phenotype Additional Mitochondria dysfunction; reduced plasma glucose and increase insulin levels. Nervous system: neuronal damage. |
| TG (brain specific)19 |
No clear reproductive endocrinology phenotype Additional Nervous system: Protect against ischemia, Parkinson, Alzheimer disease model |
|
| 17βHSD11 | Null/KO20
MGI:5581418 |
No clear reproductive endocrinology phenotype Additional Increased total circulating protein level. Nervous system: hyperactivity. |
| 17βHSD12 | Null/KO21 |
No clear reproductive endocrinology phenotype Additional Embryo lethality Ed 9.5; impaired organogenesis; reduced arachidonic acid synthesis. Reproductive system: ovarian dysfunction, fertility problems, smaller litters, significantly fewer numbers of ductal branches than wild type female mammary glands; ovulation problems. Nervous system: high embryo expression in neuronal structures. |
| 17βHSD13 | Null/KO22
MGI:5007180 |
No clear phenotype associated. |
| 17βHSD14 | Null/KO23 MGI:5007181 |
No clear reproductive endocrinology phenotype Additional Increased IgG2a level. Reproductive system: oligozoospermia, testis degeneration, male infertility. Nervous system: increased response to stress-induced hyperthermia. |
| 17βHSD15 | Null/KO24
MGI:3526658 & 3586379 |
No clear reproductive endocrinology phenotype Additional Abnormal eye electrophysiology, delayed dark adaptation |
| AKR1C3/ 17βHSD5* | Null/KO25 MGI:3527218 |
Reproductive endocrinology - long gestation, parturition failure. - increased levels of P. - prolonged estrous and diestrous. |
| Null/KO26 MGI:3774264 |
Additional Small litter size, the number of pups, especially live pups, was markedly decreased hematopoietic system phenotype. Nervous system: Some behavioral phonotype, |
|
| SRD5A1 | Null/KO27 MGI:1857454 |
Reproductive endocrinology - parturition defects, rescued by 3α-DIOL supplementation. |
|
Additional Decreased litter size; small prostate. |
||
| SRD5A2 | Null/KO28 MGI:2178039 |
Reproductive endocrinology
- T accumulation in reproductive tissues. - impaired androgen-dependent gene expression. - parturition defects, rescued by 3α-DIOL supplementation. |
|
Additional Decreased litter size; small prostate. |
||
| SRD5A3 | Null/KO29 MGI:5520177 |
Mouse not thoroughly characterized Embryonic lethality, abnormal heart morphology, abnormal neural tube closure |
| SULT1E1 | Null/KO30 MGI:3529586 |
Reproductive endocrinology - elevated circulating estrogen levels. |
|
Additional Disturbed platelet physiology. Reproductive system: leyding cell hyperplasia and abnormal morphology; abnormal testis morphology; abnormal placentation and amniotic fluid composition. |
||
| SULT2B1 | Null/KO MGI:5432568 (unpublished) |
Endocrine (steroids)
disturbed cholesterol metabolism and levels. |
No report/references was found for 17βHSD3, 17βHSD6, 17βHSD8, 3βHSD1, 3βHSD2, DHRS11, STS, SULT2A1, SULT1A1.
The human AKR1C3/17βHSD5 KO refers to mice with disrupted AKR1C18, however, functional conservation between the four human AKR1Cs and the eight mouse AKR1Cs in unclear (Sudeshna et al., 2013).
Reference ID refers to the Mouse Genome Informatics (MGI; www.informatics.jax.org. Accessed on date: February 2018) (Blake et al., 2017).
Caron et al. (1997), 2Huang et al. (2012), 3Hu et al. (2002), 4Liu et al. (2005), 5Bair and Mellon (2004), 6Nemoto et al. (2000), 7 Fisher et al. (1998), 8Honda et al. (1998), 9Hakkarainen et al. (2015), 10Saloniemi et al. (2010) and Järvensivu et al. (2018), 11Rantakari et al. (2008), 12Zhongyi et al. (2007), 13Baes et al. (2000), 14Shehu et al. (2008), 15Jokela et al. (2010), 16Shang et al. (2002), 17Driessen et al. (2000) and Sahu et al. (2015); 18Li et al. (2010) and Rauschenberger et al. (2010); 19Li et al. (2010); Rauschenberger et al. (2010), 20Dickinson et al. (2016), 21Rantakari et al. (2010); Kemilainen et al. (2016); 22Tang et al. (2010), 23Tang et al. (2010), 24Kim et al. (2005), 25Piekorz et al. (2005), 26Ishida et al. (2007), 27Mahendroo et al. (1996), 28Mahendroo et al. (2001), 29Dickinson et al. (2016), 30Qian et al. (2001) and Tong et al. (2005).
Androgens and progestogens can be further metabolized by aldo-ketoreductases (AKRs) and 5α-reductases (SRD5As; Figure 2). Cytoplasmic AKRs (AKR1C1, 1C2, 1C3/17βHSD5 and 1C4) have broad substrate specificity with non-stereo-selective 3α/3βHSD, 17- and 20-ketosteroid reductase activities (Table 2; Penning et al., 2004; Steckelbroeck et al., 2010). Together with the fact that they have wide tissue distribution (only AKR1C4 is restricted), AKR1Cs contribute to make intracrine networks flexible and intricate (Rižner and Penning, 2014; Sinreih et al., 2014).
SRD5As convert 3-keto Δ4 androstene and pregnene to 5α-reduced steroids (androstanes and pregnanes), hence they are important in progestogen, androgen (DHT production) and neurosteroid metabolism (Di Costanzo et al., 2009). SRD5A1 and 3 are widely expressed, in contrast to SRD5A2. Human 5β-reductase activity, catalyzed by AKR1D1, is restricted to the liver, where 5β-steroids are directed to clearance/catabolism. However, some 5β-compounds are neuroactive and recent studies indicate the presence of AKR1D1 in placenta and myometrium (Jin et al., 2011). With the exclusion of their neuroactivity (Paragraph 4.6), 5β-steroids will not be further considered.
The sulphatase pathway is finally responsible for the balance between sulpho-conjugated and free steroids. Sulpho-conjugated steroids (-S) possess higher water solubility, increased stability and longer half-life than unconjugated compounds (e.g., 10–12 h vs. 20–30 min for estrogens), and although they cannot bind steroid-receptors, they serve as a reservoir for the formation of biologically active steroids (Reed et al., 2005). Sulphotransferases (SULTs) are phase-I detoxifying enzymes that use bis-phospho-nucleotide 3′-phospho-adenosine-5′-phosphate- (PAP)-sulfate as donor to conjugate 3β-hydroxyl steroids (e.g., estrogens, DHEA, P5, cholesterol; red circles in Figure 2) with a sulfate group (Strott, 2002; Rižner, 2016). Distinct SULTs have different specificities toward substrates, with SULT1E1 being the major estrogen sulphating enzyme (with little contribution of SULT1A1), and SULT2A1 being specific for DHEA (but also for P5, 17OHP5 and A5) (Table 2). Steroid sulphatase (STS) is a membrane-bound microsomal enzyme that catalyzes the hydrolysis of sulfate ester bonds from sulphated-steroids (cholesterol-S, P5-S, 17OHP5-S, DHEA-S, E1-S) (Mueller et al., 2015; Rižner, 2016), thus releasing unconjugated compounds.
Although sulphated-3α-hydroxysteroids are not thoroughly studied, they are detected in biospecimens (AN-S, 3αDIOL-S; Table 1 and orange circles in Figure 2). They are most likely produced by SULT2A1 (active on 3α-hydroxy bile acids) (Strott, 2002; Rižner, 2016) but no 3α-stereo specific sulphatase is known to date. Some intracellular sulphated-steroids are converted to other compounds without prior desulphation (Sánchez-Guijo et al., 2016).
In conclusions, intracrinology presents redundant and complex pathways, which generate compounds with various activities. Genetic variants in intracrine genes are associated with various diseases (classically endocrine and not; Table 5). Even in the absence of the enzymatic machinery to metabolize cholesterol (StAR, steroidogenic factor, CYP17A1 and CYP11A1), DHEA, P5 and especially their sulphated-conjugates have high blood concentrations (Table 1), and are used to generate all other steroids in peripheral tissues.
Table 5.
Diseases associated with gene variants in intracrine enzymes.
| Name | Affected system or tissue Disease | Phenotype | OMIM ID# References |
|---|---|---|---|
| StAR |
Endocrine system Lipoid adrenal hyperplasia |
Deficiency of adrenal or gonadal steroids | OMIM: 2017101 |
| All individuals are phenotypic females | |||
| Infant mortality (mineral- & glucocorticoid deficiency | |||
| CYP11A1 |
Endocrine system Congenital adrenal insufficiency, with 46XY sex reversal |
Acute adrenal insufficiency in infancy or childhood | OMIM: 6137431 |
| Abnormality of cholesterol metabolism | |||
| Absence of secondary sex characteristics | |||
| Reproductive (ass∧) | SNPs∧∧ associated with endometrial cancer | 2 | |
| Bone (ass∧) | SNPs associated with skeletal adverse events to AI | 3 | |
| CNV (ass∧) | SNPs associated with neurological disturbances | 4 | |
| CYP17A1 | Endocrine system Congenital adrenal insufficiency (17α-hydroxyl. deficiency) | Excessive corticosteroids leading to hypertension Low aldosterone synthesis Abnormal sex determination and secondary sex characteristics, amenorrhea |
OMIM: 2021101 |
| GIT (ass∧) | SNPs associated with risk of cancer in the CRC## | 5 | |
| Reproductive (ass∧) | SNPs associated with endometrial cancer | 6 | |
| CYP19A1 | Reprod Endocrin**Aromatase deficiency | Pseudo hermaphroditism in female | OMIM: 613546 |
| Cystic ovaries, delayed bone maturation, adiposity | |||
| Aromatase excess syndrome | Heterosexual precocity and gynecomastia in males | OMIM: 139300 | |
| Isosexual precocity in females | |||
| Reproductive (ass∧) | SNPs associated with endometrial cancer and ovarian cancer risks, endometriosis risk and risk to develop preeclampsia | 6−14 | |
| Bone (ass∧) | SNPs associated with osteoporosis and fracture risk | 15, 16 | |
| Lung (ass∧) | SNPs associated with lung cancer | 17 | |
| GIT (ass∧) | SNPs associated with gastric cancer | 18 | |
| 3βHSD1 | Endocr syst*(ass∧) | SNPs associated with hypertension | 19 |
| Skin (ass∧) | SNPs associated with acne susceptibility | 20 | |
| 3βHSD2 | Endocrine system & Reprod Endocrin Congenital adrenal insufficiency (3β-HSD2 deficiency) | Impaired steroid biosynthesis | OMIM: 2018101 |
| Low cortisol, aldosterone, P androgens, estrogens. | |||
| Male new-borns exhibit pseudo hermaphroditism | |||
| Incomplete masculinization of the external genitalia | |||
| Affected females can have partial verification | |||
| Urogenital (ass∧) | SNPs associated with bladder cancer | 21 | |
| 17βHSD1 | Reproductive (ass∧) | SNPs associated with E2 levels and with endometriosis, cancer risk, abortion | 22−25 |
| 17βHSD3 | Reprod Endocrin ketosteroidreductase deficiency of testis | Males: pseudo hermaphroditism, gynecomastia | OMIM: 2643001 |
| Infertility | |||
| 17βHSD4 |
CNS and Reprod Endocrin Perrault syndrome 1 |
Ovarian dysgenesis, amenorrhea, low estrogens | OMIM: 233400 |
| Sensorineural deafness, | |||
| Neurologic manifestations (mild mental retardation) | |||
|
CNS D-bifunctional protein deficiency |
Abnormal peroxisomal fatty acid beta-oxidation | OMIM: 261515 | |
| Deterioration of nervous system functions | |||
| Infantile-onset of hypotonia, seizures, and abnormal facial features, death before the age of 2 years | |||
| 17βHSD6 | Reproductive (ass∧) | SNPs associated with PCOS*** | 26 |
| 17βHSD9 |
Eye Fundus albipunctatus |
Fleck retina disease, night blindness, delayed cone and rod photopigment regeneration. | OMIM: 136880 |
| 17βHSD10 |
CNS HSD10 mitochondrial disease |
X-linked neurodegenerative disorder | OMIM: 300438 |
| Multisystemic features, mitochondrial dysfunction | |||
| Turner type X-linked mental retardation | Moderate to profound mental retardation Macrocephaly and variable skeletal features | OMIM: 300706 | |
| 17βHSD12 | Reproductive (ass∧) | (Male) SNPs associated with prostate cancer | 27 |
| Lung (ass∧) | SNPs associated with pulmonary function | 28 | |
| 17βHSD15 |
Eye and CNS Retinal dystrophy, juvenile cataracts, short stature |
Decreased visual acuity, retinitis pigmentosa | OMIM: 616108 |
| Psychomotor delays from early childhood, lack of fine motor skills and coordination, learning difficulties, facial dysmorphism | |||
| AKR1C1 | Lymphocytes (ass∧) | SNPs associated with non-Hodgkin lymphoma | 29 |
| Lung (ass∧) | SNPs associated with lung cancer | 29 | |
| CNS (ass∧) | SNPs associated with panic disorders | 29 | |
| AKR1C2 | Reprod Endocrin 46XY sex reversal 8 | Males: ambiguous external genitalia, cryptorchidism | OMIM: 614279 |
| Disturbed endocrine features | |||
| Endocr. syst. (ass∧) | SNPs associated with weight-gain predisposition | 29 | |
| Lung (ass∧) | SNPs associated with lung cancer | 29 | |
| AKR1C3 | Reproductive (ass∧) | SNPs associated with T levels and PCOS | 29,30 |
| Lymphocytes (ass∧) | SNPs associated with large B cell lymphoma | 29 | |
| Lung (ass∧) | SNPs associated with lung cancer | 29 | |
| Leukocytes (ass∧) | SNPs associated with lung childhood leukemia | 29 | |
| Urogenital (ass∧) | SNPs associated with bladder cancer | 29 | |
| CNS (ass∧) | SNPs associated with amyotrophic lateral sclerosis | 29 | |
| AKR1C4 | Reprod Endocrin 46XY sex reversal 8 | Males: ambiguous external genitalia, cryptorchidism | OMIM 614279 |
| Disturbed endocrine features | |||
| – (ass∧) | SNPs associated with responses to anthracycline | 29 | |
| CNS (ass∧) | SNPs associated with paranoia risk | 29 | |
| SRD5A1 | Reproductive (ass∧) | Haplotypes associated with PCOS and hirsutum | 31 |
| SRD5A2 | Reprod Endocrin Pseudovaginal perineoscrotal hypospadias | Males: pseudo hermaphroditism, ambiguous genitalia, cryptorchidism, small prostate | OMIM: 264600 |
| No Mullerian structures, masculinization at puberty | |||
| No breast development or menstruation at puberty | |||
| Abnormal plasma DHT (and T) level | |||
| Reproductive (ass∧) | Haplotypes associated with PCOS | 31 | |
| Bone (ass∧) | SNPs associated with low bone mineral density | 32 | |
| SRD5A3 |
CNS Type Iq congenital glycosylation disorder |
Developmental delay, midline brain malformations | OMIM: 612379 |
| Variable extents of visual loss | |||
|
CNS Kahrizi syndrome |
Mental retardation, delayed motor development, speech impairment, coarse facial features | OMIM: 612713 | |
| STS |
Skin X-linked ichthyosis |
Cutaneous manifestations: dark brown, polygonal scales and generalized dryness | OMIM: 30810040 |
|
Bone bone dysplasia |
Chondrodysplasia punctata and bone dysplasia | 33 | |
| SULT1E1 | Reproductive (ass∧) | SNP associated with estrogen dependent diseases | 34 |
| SULT2A1 | Reproductive (ass∧) | SNP associated with DHEA-S, androgens and PCOS | 40,35 |
| SULT2B1 |
Skin congenital autosomal recessive ichthyosis |
Generalized desquamation, dry scaly skin, hyperkeratosis, erythema | OMIM: 604125 |
| SULT1A1 | Reproductive (ass∧) | SNPs associated with endometrial cancer | 11,36 |
| Bone (ass∧) | SNPs associated with low bone mineral density | 32 | |
| GIT (ass∧) | SNPs associated with risk of cancer in the GIT | 37−38 | |
| – (ass∧) | SNPs associated with activity and termostability | 37,39 |
Selected papers reporting association between SNPs and diseases are reported. Association studies with enzymes involved in steroid signaling but not discusses in the present review exist (for some references, see Doherty et al., 2005; Freedman et al., 2009; Miller and Auchus, 2011; Mueller et al., 2015).
Endocr syst: Endocrine system.
Reprod Endocrin: Reproductive endocrinology.
PCOS: polycystic ovarian syndrome.
ass: association studies, case controls.
SNP: single nucleotide polymorphism.
OMIM: Online Mendelian Inheritance in Man. McKusick-Nathans Institute of Genetic Medicine, Johns Hopkins University (Baltimore, MD). (https://omim.org/. Accessed on date: February 2018).
CRC: colorectal cancer.
Miller and Auchus (2011), 2Terry et al. (2010), 3Rodríguez-Sanz et al. (2015), 4Deng et al. (2016), 5Zeng et al. (2016), 6Olson et al. (2007), 7Berstein et al. (2006), 8Kitawaki et al. (2002), 9Lundin et al. (2012), 10Thompson et al. (2016), 11Gulyaeva et al. (2008), 12Setiawan et al. (2009), 13Zacher et al. (2016), 14Shimodaira et al. (2012), 15Fontein et al. (2014), 16Masi et al. (2001), 17Zhang et al. (2013), 18Cho et al. (2012), 19Shimodaira et al. (2010), 20Yang et al. (2013), 21Andrew et al. (2012), 22Tsuchiya et al. (2005), 23Huber et al. (2005), 24Setiawan et al. (2004), 25Shi et al. (2016), 26Jones et al. (2009), 27Audet-Walsh et al. (2012), 28Loth et al. (2014), 29Alshogran (2017), 30Qin et al. (2006), 31Goodarzi et al. (2006), 32Zarrabeitia et al. (2007), 33Wöhrle et al. (1990), 34Adjei et al. (2003), 35Goodarzi et al. (2007), 36Ashton et al. (2010), 37Lilla et al. (2007), 38Xiao et al. (2014), 39Sun et al. (2005), and 40Mueller et al. (2015).
Bold text indicates the system affected, italics text indicates the name of the disease.
Drug development
Natural hormones have been historically used as drugs, and depending on definitions, approximately 90 marketed drugs share a steroidal core (see https://www.drugbank.ca). Steroids (T, E2, cortisol, DHEA), simple derivatives (ethinylestrogen, prednisolone) or more complex analogs (abiraterone, fulvestrant) are used in various conditions. This old-and-proven steroidal chemistry based approach is used even in modern era.
By targeting steroid intracrine metabolism, the effects of steroids can be modulated locally. Table 3 overviews the available drugs targeting intracrine enzymes and their developmental status. CYP19A1 (aromatase) inhibitors, currently at their third generation, started to be used for breast cancer during the 80's of last century (Lønning and Eikesdal, 2013), and was followed by drugs able to target other enzymes (CYP11A1, CYP17A1, SRD5As; Table 3).
Table 3.
Drugs targeting intracrine enzymes.
| Inhibitor name (if known); (Drug Bank ID#) | |||||
|---|---|---|---|---|---|
| Developmental phase& | Approved drugs | ||||
| Name | Discovery | Preclinical indication | Clinical indication | Inhibitor name | Indication |
| CYP11A1 | ✓ | ✓ | ✓ | Aminoglutethimide (DB00357##) |
Cushing's syndrome Breast cancer |
| CYP17A1 | ✓ | ✓ | ✓ | Abiraterone (DB05812) |
Prostate cancer, metastatic, castration-resistant |
| CYP19A1 | ✓ | ✓ | Letrozole (DB01006)(19, 22, 24) |
Anastrozole | Breast cancer: adjuvant treatment, metastatic |
| (DB01217) | |||||
| Letrozole | |||||
| (DB01006) | |||||
| Exemestane | Breast cancer, palliative | ||||
| (DB00990) | |||||
| Formestane1 | |||||
| Testolactone* | |||||
| (DB00894) | |||||
| Anastrozole (DB01217) (20, 23) |
|||||
| Exemestane (DB00990) 21 |
|||||
| Advanced stage endometrial cancer, NSCLC∧, LAM∧∧ | |||||
| 3βHSD1 | ✓ | ✓ | ✓ | Trilostane* (DB01108) |
Cushing's syndrome (veterinary use) |
| 3βHSD2 | ✓ | ✓ | ✓ | Trilostane* (DB01108) |
Cushing's syndrome (veterinary use) |
| 17βHSD1 | ✓ | Endometriosis2,3 | |||
| Endometrial cancer4 | |||||
| Breast cancer5,6 | |||||
| Endometrial hyperplasia7 | |||||
| 17βHSD2 | 8,9 | ||||
| 17βHSD3&& | Prostate cancer10 | ||||
| 17βHSD7 | 11 | ||||
| AKR1C1 | 12 | ||||
| AKR1C2 | 12 | ||||
| AKR1C3 | ✓ | ✓ | ASP-952113 Prostate cancer** |
||
| BAY 1128688 Endometriosis*** |
|||||
| AKR1C4 | 12 | ||||
| SRD5A1 | ✓ | ✓ | ✓ | Dutasteride (DB01126) | Prostatic hyperplasia (benign) |
| SRD5A2 | ✓ | ✓ | ✓ | Finasteride (DB01216) | Prostatic hyperplasia (benign) |
| Dutasteride (DB01126) | |||||
| SRD5A3 | ✓ | ✓ | ✓ | Dutasteride (DB01216) | Prostatic hyperplasia (benign) |
| STS | ✓ | ✓ | Irosustat (DB02292) | ||
| Endometrial cancer 14,15 | |||||
| Breast cancer14−17 | |||||
| E2MATE/PLG2001 | |||||
| Endometriosis18 | |||||
| SULT1E1 | ✓ | ✓ | ✓ | Cyclizine (DB01176) | antistaminic for nausea/vomiting |
‘Clinical phase’, i.e., in phase I, II or III trial; ‘Preclinical phase’ refers to in vivo testing; ‘Discovery phase’ any previous phase with some candidate compounds.
Drug Bank ID if the compound is deposited in Drug Bank database (www.drugbank.ca/drugs. Accessed on date: February 2018) (Wishart et al., 2018).
Aminoglutethimide (ID: DB00357) is an important inhibitor of CYP11A1 with inhibitory activity on CYP19A1 as well.
No longer on the market.
17βHSD3 is testis specific and the reactions catalyzed by this enzyme are not reported in Figure 2.
This trial for prostate cancer was prematurely terminated (www.clinicaltrials.gov, NCT01352208).
Phase I trial is concluded (www.clinicaltrials.gov, NCT02434640. Accessed on date: February 2018) and a phase II trial started 2016 (http://adisinsight.springer.com/drugs/800041929).
NSCLC: non-small cell lung cancer
LAM: lymphangioleiomyomatosis
Perez Carrion et al. (1994), 2Arnold and Einspanier (2013), 3Delvoux et al. (2014), 4Konings et al. (2017), 5Järvensivu et al. (2018), 6Husen et al. (2006), 7Saloniemi et al. (2010), 8Gargano et al. (2015), 9Soubhye et al. (2015) 10Day et al. (2013), 11 Wang et al. (2017), 12BroŽic et al. (2011), 13 Kikuchi et al. (2014), 14Purohit and Foster (2012), 15Pautier et al. (2017), 16Palmieri et al. (2017a), 17Palmieri et al. (2017b), 18Pohl et al. (2014), 19Ma et al. (2004), 20Rose et al. (2000), 21Lindemann et al. (2014), 22Slomovitz et al. (2015), 23 NCT00932152; 25Lu et al. (2017).
More recently, there is a re-emerging interest in developing novel intracrine drugs. A number of compounds are in their clinical phases, like STS inhibitors (Maltais and Poirier, 2011; Woo et al., 2011; Purohit and Foster, 2012; Pohl et al., 2014; Pautier et al., 2017) or inhibitors of AKR1C3/17βHSD5, which are of particular interest because this enzyme has crucial role in androgen/estrogen and prostaglandin biosynthesis (Penning, 2017). Bayer's AKR1C3/17βHSD5 inhibitor BAY 1128688 has a modified estrogen core, it interferes with both pathways, and is in phase II clinical trial for endometriosis (Bothe et al., 2017). Astellas Pharma potent and selective AKR1C3/17βHSD5 inhibitor ASP-9521 had only modest effect in a phase II study on prostate cancer as single drug, but combination therapy approaches remain to be studied (Kikuchi et al., 2014; Loriot et al., 2014).
HSD inhibitors are being studied in the area of hormone-dependent diseases, with 11βHSD inhibitors being in clinical trials for metabolic disorders (Ye et al., 2017) and 17βHSD inhibitors approaching the clinical phase for a number of gynecological indications (Table 3; Abdelsamie et al., 2017).
Intracrinology in peripheral tissues
In this paragraph, intracrinology of endometrium, GIT, bone, lungs, and CNS is reviewed. To comprehensively understand the ability of these tissues and systems to generate estrogens and other steroids, we have performed a systematic search of all original papers published in English until June 2018 that described the levels of intracrine enzymes (those indicated in Table 2-mRNA, protein or activity) in healthy tissues. In total 177 if the four extra ref are allowed papers were reviewed, and for details of this search, see Supplemental panel: “Systematic Review.” The results of this systematic review are summarized in Tables 6–8 and are briefly overviewed in each section dedicated to the distinct tissues or systems. Reports describing the enzymes in cultured cells or cell lines were excluded (may have been discussed elsewhere, though). Each section follows then with a non-systematic overview of the role of intracrinology in pathophysiology. A brief non-systematic description of the intracrinology of the skin, immune system and adipose tissue is also given. We will not describe the intracrinology of breast, prostate and liver (where steroid catabolism is the most relevant aspect), and we redirect the reader to recent reviews (Foster et al., 2008a; Luu-The et al., 2008; Luu-The and Labrie, 2010; Labrie and Labrie, 2013; Labrie, 2015; Mueller et al., 2015; Zhao et al., 2016; Hilborn et al., 2017; Penning, 2017).
Table 6.
Expression of intracrine enzymes in endometrium–results of the systematic search.
| Name | Menopausal status | ||||
|---|---|---|---|---|---|
| Technique# | Pre | Post | References | ||
| StAR | mRNA | RT-PCR | yes | yes | Bukulmez et al., 2008a; Attar et al., 2009; Sinreih et al., 2017b& |
| CYP11A1 | mRNA | RT-PCR | yes | n.d. | Tsai et al., 2001; Rhee et al., 2003; Attar et al., 2009; Sinreih et al., 2013; Huhtinen et al., 2014 |
| RT-PCR | no | n.d. | Rhee et al., 2003 | ||
| CYP17A1 | mRNA | RT-PCR | yes | n.d. | Tsai et al., 2001; Attar et al., 2009; Huhtinen et al., 2014 |
| RT-PCR | no | n.d. | Rhee et al., 2003 | ||
| IHC | no | no | Watanabe et al., 1995 | ||
| CYP19A1 | mRNA | RT-PCR | yes | yes | Dheenadayalu et al., 2002; Brosens et al., 2004; Matsuzaki et al., 2006; Pathirage et al., 2006; Smuc et al., 2006, 2009; Dassen et al., 2007; Bukulmez et al., 2008b; Attar et al., 2009; Smuc and Rizner, 2009; Lépine et al., 2010; Cornel et al., 2012; Huhtinen et al., 2012a; Delvoux et al., 2014; Sinreih et al., 2017a |
| RT-PCR | no | no | Bulun et al., 1993, 1994; Watanabe et al., 1995; Noble et al., 1996, 1997; Kitawaki et al., 1999; Bacallao et al., 2008; Colette et al., 2009 | ||
| ISH | no | n.d. | Watanabe et al., 1995 | ||
| Protein | IHC | yes | yes | Maentausta et al., 1990; Kitaoka et al., 2004; Maia et al., 2006, 2007; Hudelist et al., 2007; Vouk et al., 2011; Miller et al., 2012a | |
| IHC | no | no | Watanabe et al., 1995; Kitawaki et al., 1999; Velasco et al., 2006; Acién et al., 2007; Jeon et al., 2007; Bukulmez et al., 2008b; Colette et al., 2009 | ||
| WB | N.d. | yes | Knapp et al., 2013 | ||
| activity | no | no | Bulun et al., 1993; Watanabe et al., 1995; Noble et al., 1997 | ||
| activity | yes | yes | Tseng et al., 1982; Yamaki et al., 1985; Taga et al., 1990; Yamamoto et al., 1990a,b, 1993a,b; Jongen et al., 2005; Purohit et al., 2008 | ||
| 3βHSD1 | mRNA | RT-PCR | yes | yes | Rhee et al., 2003; Vani et al., 2007; Attar et al., 2009; Smuc et al., 2009; Gibson et al., 2013; Sinreih et al., 2013 |
| Protein* | IHC | yes | n.d. | Rhee et al., 2003; Vani et al., 2007 | |
| IHC | no | no | Watanabe et al., 1995 | ||
| 3βHSD2 | mRNA | RT-PCR | yes | yes | Tsai et al., 2001; Attar et al., 2009; Huhtinen et al., 2014; Osinski et al., 2018 |
| 17βHSDs | |||||
| oxidative activity | yes | yes | Tseng and Gurpide, 1974; Pollow et al., 1975a,b, 1976; Polow et al., 1975; Tseng et al., 1977; Lane, 1990; Kitawaki et al., 2000; Utsunomiya et al., 2001; Delvoux et al., 2007, 2009; Cornel et al., 2012 | ||
| reductive activity | yes | yes | Maentausta et al., 1990; Delvoux et al., 2007, 2009, 2014; Bacallao et al., 2008 | ||
| no | no | Utsunomiya et al., 2001 | |||
| 17βHSD1 | mRNA | RT-PCR | yes | yes | Zeitoun et al., 1998; Dassen et al., 2007; Smuc et al., 2007, 2009; Bacallao et al., 2008; Huhtinen et al., 2012a; Colette et al., 2013; Delvoux et al., 2014; Sinreih et al., 2017a; Osinski et al., 2018 |
| NB | yes | n.d. | Zeitoun et al., 1998 | ||
| RT-PCR | no | no | Casey et al., 1994; Utsunomiya et al., 2001 | ||
| Protein | IHC | yes | yes | Maentausta et al., 1990&; Mäentausta et al., 1991; Li et al., 2003; Dassen et al., 2007; Colette et al., 2013; Mori et al., 2015; He et al., 2016; Sinreih et al., 2017a | |
| IHC | no | no | Utsunomiya et al., 2001 | ||
| 17βHSD2 | mRNA | RT-PCR | yes | yes | Mäentausta et al., 1991; Zeitoun et al., 1998; Kitawaki et al., 2000, 2002; Utsunomiya et al., 2001; Matsuzaki et al., 2006; Smuc et al., 2006, 2007, 2009; Carneiro et al., 2007; Dassen et al., 2007; Vani et al., 2007; Bacallao et al., 2008; Hevir et al., 2011b; Huhtinen et al., 2012a; Colette et al., 2013; Delvoux et al., 2014; Sinreih et al., 2017a; Osinski et al., 2018 |
| NB | yes | n.d. | Zeitoun et al., 1998 | ||
| Protein | IHC | yes | yes | Scublinsky et al., 1976; Ciuffi et al., 1982; Utsunomiya et al., 2001; Dassen et al., 2007; Colette et al., 2013; Cornel et al., 2017; Sinreih et al., 2017a | |
| 17βHSD4 | mRNA | RT-PCR | yes | yes | Dassen et al., 2007; Smuc et al., 2009; Huhtinen et al., 2012a; Delvoux et al., 2014 |
| NB | yes | n.d. | Möller et al., 1999 | ||
| 17βHSD6 | mRNA | RT-PCR | yes | n.d. | Huang and Luu-The, 2000; Huhtinen et al., 2012a |
| 17βHSD7 | mRNA | RT-PCR | yes | yes | Smuc et al., 2007, 2009; Smuc and Rizner, 2009; Lépine et al., 2010; Cornel et al., 2012; Huhtinen et al., 2012a; Delvoux et al., 2014 |
| 17βHSD8 | mRNA | RT-PCR | yes | yes | Smuc and Rizner, 2009; Smuc et al., 2009 |
| 17βHSD10 | mRNA | RT-PCR | yes | n.d. | Huhtinen et al., 2012a |
| 17βHSD12 | mRNA | RT-PCR | yes | yes | Smuc and Rizner, 2009; Smuc et al., 2009; Lépine et al., 2010; Cornel et al., 2012; Huhtinen et al., 2012a; Delvoux et al., 2014 |
| 17βHSD14 | mRNA | RT-PCR | yes | n.d. | Huhtinen et al., 2012a; Sinreih et al., 2017a |
| AKR1Cs | |||||
| AKR1C1 | mRNA | RT-PCR | yes | yes | Rizner et al., 2006; Smuc and Rizner, 2009; Smuc et al., 2009; Hevir et al., 2011b; Sinreih et al., 2013 |
| AKR1C2 | mRNA | RT-PCR | yes | yes | Hevir et al., 2011b; Sinreih et al., 2013 |
| AKR1C3/17 βHSD5 |
mRNA | RT-PCR | yes | yes | Penning et al., 2000; Rizner et al., 2006; Vani et al., 2007; Smuc and Rizner, 2009; Smuc et al., 2009; Hevir et al., 2011b; Cornel et al., 2012; Huhtinen et al., 2012a; Sinreih et al., 2013; Delvoux et al., 2014 |
| Protein | IHC | yes | yes | Pelletier et al., 1999; Ito et al., 2006; Vani et al., 2007; Smuc and Rizner, 2009; Zakharov et al., 2010 | |
| SRD5As | |||||
| SRD5A1 | mRNA | RT-PCR | yes | yes | Carneiro et al., 2008; Hevir et al., 2011b; Sinreih et al., 2013; Huhtinen et al., 2014 |
| Protein | IHC | yes | yes | Ito et al., 2002; Carneiro et al., 2008; Tanaka et al., 2015 | |
| SRD5A2 | mRNA | RT-PCR | yes | yes | Carneiro et al., 2008; Hevir et al., 2011b; Sinreih et al., 2013; Huhtinen et al., 2014 |
| Protein | IHC | yes | yes | Ito et al., 2002; Carneiro et al., 2008; Tanaka et al., 2015 | |
| SRD5A3 | RT-PCR | yes | n.d. | Huhtinen et al., 2014 | |
| Sulphatase pathway | |||||
| STS | mRNA | RT-PCR | yes | yes | Tanaka et al., 2003; Utsunomiya et al., 2004; Smuc et al., 2006, 2007, 2009; Dalla Valle et al., 2007; Dassen et al., 2007; Bacallao et al., 2008; Smuc and Rizner, 2009; Lépine et al., 2010; Colette et al., 2013; Huhtinen et al., 2014; Piccinato et al., 2016b; Sinreih et al., 2017a |
| RT-PCR | no | no | Miki et al., 2002 | ||
| Comp-RT | yes | n.d. | Yanaihara et al., 2001 | ||
| Protein | IHC | yes | yes | Yanaihara et al., 2001; Utsunomiya et al., 2004; Dassen et al., 2007; Cornel et al., 2017; Sinreih et al., 2017a | |
| IHC | no | no | Miki et al., 2002 | ||
| activity | yes | yes | Warren and French, 1965; Prost and Adessi, 1983; Adessi et al., 1984; Platia et al., 1984; Yamamoto et al., 1990a, 1993a; Tanaka et al., 2003; Bacallao et al., 2008; Purohit et al., 2008; Delvoux et al., 2009 | ||
| IHC | no | no | Utsunomiya et al., 2004 | ||
| SULT1E1 | mRNA | RT-PCR | yes | yes | Yamamoto et al., 1993a; Miki et al., 2002; Tanaka et al., 2003; Utsunomiya et al., 2004; Smuc et al., 2006, 2007; Dassen et al., 2007; Bacallao et al., 2008; Smuc and Rizner, 2009; Lépine et al., 2010; Hevir et al., 2011a, 2013; Colette et al., 2013; Piccinato et al., 2016b; Sinreih et al., 2017a |
| NB | yes | n.d. | Rubin et al., 1999 | ||
| Protein | IHC | yes | yes | Miki et al., 2002; Utsunomiya et al., 2004; Hudelist et al., 2007; Cornel et al., 2017; Sinreih et al., 2017a | |
| activity | yes | yes | Tanaka et al., 2003; Utsunomiya et al., 2004; Bacallao et al., 2008; Purohit et al., 2008 | ||
| SULT1A1 | mRNA | RT-PCR | yes | yes | Hevir et al., 2011a, 2013 |
| SULT1A1 | NB | yes | n.d. | Rubin et al., 1999*** | |
| SULT2A1 | NB | no | n.d. | Rubin et al., 1999 | |
| SULT2B1 | mRNA | RT-PCR | yes | yes | Hevir et al., 2011a, 2013 |
Primary/original references were analyzed and reviews were excluded (and are cited ad hoc in the text). The table report only the enzymes whose expression was assessed in reviewed studies**.
Technique abbreviations. For mRNA detection, NB: northern blot; ISH: in situ hybridisation; RT-PCR: reverse transcription semi or quantitative PCR; Comp-RT: competitive RT-PCR. For protein detection: IHC: immunohistochemistry; WB: western blotting. For enzyme activity measurement: activity.
Most commercially available antibodies do not distinguish between 3βHSD1 and 3βHSD1.
No publication was found describing the expression of 17βHSD9, 11, 13, 15, DHRS11 and AKR1C4.
The same study also detected expression of SULT1A3 (Rubin et al., 1999).
n.d.: not determined.
Protein level was measured by radioimmunoassay.
Endometrium
The actions of steroid hormones in the endometrium are mediated by hormone-receptors via the classical mechanisms, although non-genomic and rapid signaling are also present (Groothuis et al., 2007; Zwart et al., 2011; Flach and Zwart, 2016; Hewitt et al., 2016). Estrogens and P control the menstrual cycle (Groothuis et al., 2007; Andersen and Ezcurra, 2014) and the endometrium during the window of implantation (WOI), occurring in the mid-luteal phase (Wang and Dey, 2006).
In rats, the WOI is characterized by high E2 plasma levels, and endometrial ERα and PR expression shows specific and varying cytosolic/nuclear patterns (Singh et al., 1996). ERα and PR expression decreases after ovulation and in preimplantation stages in both mice (Vasquez and DeMayo, 2013) and primates (Macaca mulatta) (Ghosh et al., 1999).
Rodent genetic models unraveled some molecular mechanisms underlying the estrogen-dependency of these processes. ERα-KO mice are infertile, no implantation occurs, endometrium is hypoplastic and estrogen response is absent (Couse and Korach, 1999; Walker and Korach, 2004). Not only its absence, but also sustained estrogen signaling has deleterious effects on endometrial receptivity, as recapitulated by mice with uterine COUP-TFII ablation. These mice exhibit increased estrogen signaling and asynchrony between embryo competency and uterine receptivity with consequent implantation defects. This effect is rescued by treatment with the antiestrogen ICI-182780 (Lee et al., 2010). Additionally, the duration of E2 exposure and its dosage affect endometrial receptivity and WOI length in mice (Ma et al., 2003).
Available human data, mostly obtained in the context of assisted reproduction technologies (ART), also indicate that steroid stimulation retards or shortens the luteal phase, the WOI, causes shifts in the appearance of pinopodes (a classical WOI marker) and causes asynchrony between ovarian and menstrual cycles (Devroey et al., 2004).
Intracrinology in healthy endometrium–systematic search
Initial studies on steroid hormone metabolism in the endometrium date back to 1965 with first demonstration of the STS activity, followed by investigation on the oxidative and reductive 17βHSD activities (Table 6).
Both pre and postmenopausal tissues possess oxidative and reductive 17βHSD activities and the expression of 17βHSD1, 2, 4, 6, 7, 8, 10, 12, 14, and AKR1C3/17βHSD5 was detected at the mRNA or protein levels. Sulphatase pathway (STS and SULT1E1; recently reviewed by Rižner, 2016), CYP19A1, 3βHSDs, SRD5As and AKR1Cs are also present, indicating that human endometrium can metabolize sulphated-compounds and DHEA to form androgens and estrogens.
Few 17βHSDs have been characterized by IHC. The low expression of 17βHSD1 poses sensitivity problems using standard detection methods (Cornel et al., 2017), and few authors reported endometrial absence of 17βHSD1 (Table 6). Type 1 17βHSD localizes in the cytoplasm of epithelial cells (Dassen et al., 2007; Colette et al., 2013; Mori et al., 2015; Sinreih et al., 2017a) and it is also detected in primary stroma cells cultured in vitro (Aghajanova et al., 2009; Mori et al., 2015). Type 2 17βHSD, AKR1C3/17βHSD5 and 3βHSD1 give strong reactivity in the glandular epithelium (Rhee et al., 2003; Ito et al., 2006; Dassen et al., 2007; Vani et al., 2007; Smuc and Rizner, 2009; Zakharov et al., 2010; Colette et al., 2013; Mori et al., 2015; Sinreih et al., 2017a).
CYP19A1 as well has low expression and some authors detected this enzyme only in association with diseases (see below and recently reviewed by Rižner, 2013). Although CYP19A1 immunoreactivity was initially associated with stroma cells (Watanabe et al., 1995), subsequent investigations showed also glandular expression (Kitawaki et al., 1999; Hudelist et al., 2007) and laser-capture-microdissected stroma/epithelial components detected CYP19A1 mRNA in both cell types (Matsuzaki et al., 2006).
The mRNA of those enzymes converting cholesterol to DHEA (CYP11A1, CYP17A1, StAR) and (ovarian) 3βHSD2 was reported in recent studies, suggesting that the endometrium can produce steroids from cholesterol (Table 6).
Intratissue steroid levels
Endometrial steroid levels were recently profiled by LC-MS. E2 levels differ between tissue and serum during the menstrual cycle, being up to five-times higher in tissue than in serum during the proliferative phase and 1.5-fold higher in the luteal period (Huhtinen et al., 2012a, 2014). T levels were lower in tissue than in serum with no cyclic changes. The levels P and P5 (and their 17-hydroxy derivatives) did not vary between serum and tissue, indicating that, contrarily to estrogens, progestogen intra-tissue levels are determined by passive diffusion from the blood (Huhtinen et al., 2014).
Intracrinology and reproduction
Animal models show not only that intracrine enzymes are expressed in the endometrium, but also they vary the expression levels during the endometrial phases and during implantation, as shown already during the 80's in rhesus monkeys for the oxidizing 17βHSD activity (Kreitmann et al., 1979).
In rodents, STS activity measured with [3H]E1-S in 6-days pregnant rats was lower around the implantation site compared with non-implantation sites (Loza, 1995). In situ hybridisation signal of 17βHSD7 mRNA varied spatio-temporally throughout implantation and early gestation, being initially detected on luminal epithelium around the implantation site and absent in decidua (embryonic day, Ed5.5). At Ed8 and Ed9.5, 17βHSD7 expression increased in the decidua capsularis (the part that interacts with the trophoblast) and later (after E9) in the junctional zone of the developing placenta and in the spongiotrophoblasts (Nokelainen et al., 2000).
A brilliant study in mice showed that decidualization is dependent on local E2 produced through CYP19A1. CYP19A1 expression increased during pregnancy and decidualization was unaffected by ovariectomy. In contrast, treatment with the aromatase inhibitor (AI) letrozole impaired decidualization and decreased decidual marker expression (e.g., PRP, BMP2 and CX43) (Das et al., 2009).
In human endometrium, 17βHSD2 and SULT1E1 are induced by P as their expression peaks in the luteal phase (Rubin et al., 1999; Tseng and Mazella, 2002; Utsunomiya et al., 2004; Dassen et al., 2007; Huhtinen et al., 2012a; Colette et al., 2013; Piccinato et al., 2016b). Since both enzymes decrease intra-tissue estrogen levels, their up-regulation is one of the mechanisms of the uterine antiestrogenic effects of P. The P-dependency of 17βHSD2 and SULT1E1 was recapitulated in vitro using explant cultures and primary cells (Tseng and Mazella, 2002; Dassen et al., 2007; Piccinato et al., 2016b). Luteal peak expression of other SULTs (1A1 and 2B1) was also reported (Rubin et al., 1999; Koizumi et al., 2010). Some reports also suggested that STS expression increased in the luteal phase (Tanaka et al., 2003; Piccinato et al., 2016b) with a potential role during decidualization (Tseng and Mazella, 2002). Mid-luteal phase endometrium shows also peaking expression of 3βHSD1 (mRNA and protein) (Rhee et al., 2003; Vani et al., 2007).
Two studies on human ectopic pregnancies explored the endometrium around the implanted blastocyst. Expression of 3βHSD1 (mRNA and protein) was highest in decidua obtained from ectopic pregnancies (Rhee et al., 2003) and in a study on 23 tubal pregnancies, 17βHSD1 showed highest immunoreactivity at the fetal-maternal interface (Li et al., 2003), suggestive for a role of these enzymes in the nidation site.
Endometriosis
Endometriosis, an estrogen-dependent benign disorder affecting up to 10% of reproductive-aged women, is associated with pelvic pain, infertility, decreased life-quality and important health care/social costs (Simoens et al., 2011, 2012; De Graaff et al., 2013, 2015, 2016; Vercellini et al., 2014). Endometriosis is characterized by the growth of endometrium-like tissue outside the uterus (ectopic locations), beside the ovaries (endometrioma), as peritoneal implants, or as deep-lesions infiltrating peritoneal organs (deep endometriosis).
The expression of intracrine enzymes in endometriosis was reviewed in 2012, (Huhtinen et al., 2012b) and among other studies, 20 papers published between 1996 and 2009 specifically described the levels of intracrine enzymes in eutopic and ectopic endometrium from patients and control women. With the exclusion of one study that included over 100 patients (Colette et al., 2009), the rest included small study populations, and in most cases, the various endometriosis types (ovarian, peritoneal and deep infiltrating) were pooled together. Various techniques were used (RT-qPCR, immunohistochemistry, enzyme activity assay). Overall, no clear conclusion could be drawn from these studies. Comparing endometriosis with controls, CYP19A1 was up-regulated (six studies), unchanged (three studies) and one study found no expression of this gene. With respect to oxidative and reductive 17βHSDs, 17βHSD1 was reported up-regulated (three studies), 17βHSD2 was reported down-regulated or unchanged and two studies reported an up-regulation of 17βHSD7 and 12 in endometriosis vs. controls (Huhtinen et al., 2012b).
Subsequent investigations also continued to report inconsistent results. No change in mRNA (Delvoux et al., 2014) or increased expression of CYP19A1 in ovarian endometriosis vs. controls (Huhtinen et al., 2012a) were reported. An increased expression of CYP19A1 was also described using in vitro spheroids derived from endometrial stroma cells from patients compared with controls (Mori et al., 2015).
The mRNA expression of 17βHSD1 was higher in endometriosis compared with normal tissue using patient biopsies as well as spheroid cultures derived from endometrial stroma cells of patients and controls (Delvoux et al., 2014; Mori et al., 2015). One study assessing the three endometriosis types separately (60 patients in total) described that the increased 17βHSD1 level was restricted to endometrioma during the secretory phase of the menstrual cycle (Huhtinen et al., 2012a), whereas a second study on 79 patients and 41 controls, found no change in 17βHSD1 level, but described an increased 17βHSD1/2 ratio (Colette et al., 2013).
Regarding 17βHSD2, recent investigations reported both unchanged (Delvoux et al., 2014) and down-regulated mRNA in patient biopsies compared with controls (Huhtinen et al., 2012a; Colette et al., 2013). No variations were found in 17βHSD4, 5, 7 and 12 (Smuc et al., 2009; Delvoux et al., 2014) but an increased level of 17βHSD6 mRNA was detected in endometriosis compared with controls (Huhtinen et al., 2012a).
A few studies reported detectable levels of the enzymes involved in the generation of DHEA from cholesterol (StAR, CYP11A1 and CYP17A1) in endometriosis (Tsai et al., 2001; Rhee et al., 2003; Bukulmez et al., 2008a; Attar et al., 2009; Sinreih et al., 2013, 2017b; Huhtinen et al., 2014), suggesting that, in contrast to eutopic endometrium, endometriosis is able to produce steroids from cholesterol. However, it has also been argued that the presence of paracrine confounders of ovarian origin in studies using endometriomas could bias the results (Noël et al., 2011).
The contribution of STS, SULT1E1 and other SULTs was investigated by numerous studies and also in this case, conclusions are unclear (recently reviewed, Rižner, 2016). A recent investigation using 78 specimens described increased STS levels in endometriosis vs. control samples and found that the overall balance between STS and SULT1E1 differed between eutopic and ectopic tissue, implying an unbalanced flux of sulpho-conjugated estrogens in this disease (Piccinato et al., 2016b). The same research group also described an aberrant regulation of the enzymes involved in the estrogen oxidative metabolism in endometriosis (Piccinato et al., 2016a).
Although the level of the single enzymes in the intracrine machinery varies with apparently no clear association with the disease condition, the intracrinological nature of endometriosis was recently proven by comparison between serum and tissue levels of steroids in 60 patients (eutopic and ectopic endometrium) and 16 controls. Although E2 changed cyclically in eutopic tissue, E2 levels remained constant in the lesions and inversely correlated with the mRNA level of 17βHSD2 and 17βHSD6 suggesting an impairment in E2 deactivation to E1. P levels were equal in serum and control tissues, but resulted higher in patients and correlated with high 3βHSD2 mRNA. T, low in the tissue of controls, was over 13-times more concentrated at ectopic locations and correlated with low expression of SRD5A3 (Huhtinen et al., 2012a, 2014).
Endometrial cancer (EC)
EC is the most common gynecological malignancy in western society and 80% of all cases are estrogen-driven (Amant et al., 2005; Morice et al., 2015). Major serum steroids are increased in patients with EC, including several substrates for intracrine E2 synthesis (Lépine et al., 2010; Audet-Walsh et al., 2011). In addition, tissue-steroid levels differ between cancer, normal tissue and serum and correlate with the levels of specific intracrine enzymes (see below) (Tanaka et al., 2015).
A systematic review recently explored all studies published between 1990 and 2017 assessing the expression of 17βHSD1, 2, STS, SULT1E1, and CYP19A1, with results that describe unbalanced intracrine regulation and important inter-patient variability (Cornel et al., 2018). Most studies compared cases with controls or tumor tissue with adjacent normal endometrium. Compared with normal tissue (from controls or adjacent to tumor), 17βHSD1 was found increased in EC (Cornel et al., 2012), decreased (Smuc and Rizner, 2009; Lépine et al., 2010) and undetected (Utsunomiya et al., 2001, 2003); 17βHSD2 was found decreased (Utsunomiya et al., 2003, 2004) or increased (Lépine et al., 2010; Cornel et al., 2012; Sinreih et al., 2013); AKR1C3/17βHSD5 was found unchanged (Cornel et al., 2012; Sinreih et al., 2013), increased (Ito et al., 2016) and decreased (Zakharov et al., 2010); 17βHSD7 both decreased (Smuc and Rizner, 2009) and unchanged (Lépine et al., 2010; Cornel et al., 2012) and 17βHSD12 was unchanged (Smuc and Rizner, 2009; Cornel et al., 2012) or increased in tumors vs. controls (Lépine et al., 2010). One recent report described decreased 17βHSD14 levels in tumor compared with adjacent tissue (Sinreih et al., 2017a). Controversial results apply to CYP19A1, described as increased (Watanabe et al., 1995; Utsunomiya et al., 2001, 2004; Smuc and Rizner, 2009) and unchanged (Jongen et al., 2005; Pathirage et al., 2006; Cornel et al., 2012). STS/SULT1E1 expression is also inconsistent in different studies (recently reviewed in Mueller et al., 2015; Rižner, 2016).
Recent studies exploring the association between enzyme levels and tumor characteristics found a correlation between STS with tumor grade and lymphovascular invasion (Sinreih et al., 2017a) and described an association between high CYP19A1 or 17βHSD1 and poor patient prognosis (Segawa et al., 2005; Cornel et al., 2017).
Other investigations emphasized the potential antiestrogenic and protective roles of androgens and P. Formation of DHT (via conversion of A4 to T by AKR1C3/17βHSD5 and of T to DHT by SRD5As) has potential antiestrogenic action because it devoids tissue from T (substrate of CYP19A1 yielding E2) and because it has direct endometrial antiproliferative effects via AR (Ito et al., 2016). Similar to the AKR1C3/17βHSD5 data reported earlier, results on SDR5A expression are inconclusive as SRD5A2 was down-regulated in a study on 47 tumor specimens compared with adjacent normal tissue (Sinreih et al., 2013), but both SRD5A1 and SRD5A2 resulted unchanged in another study on 122 tumors (although only five controls were studied) (Tanaka et al., 2015). This last study found however increased androgen levels (T and DHT) in tissue vs. blood. High DHT levels were restricted to samples with high SRD5A1 immunohistochemical staining. In addition, AR and SRD5A1 positivity was associated with good patient prognosis (Tanaka et al., 2015). The prognostic value of AR is confirmed by independent investigations (Tangen et al., 2016).
P is well-known for its antiestrogenic action, PR positivity is a good prognostic marker (Tangen et al., 2014) and P synthesis and metabolism are disturbed in EC (Sinreih et al., 2013). Interestingly, in a study on 47 tumors and adjacent normal tissues, EC had decreased StAR and CYP11A1 mRNA levels, indicative of diminished de novo steroid synthesis (Sinreih et al., 2013, 2017b). At the same time, EC showed decreased SRD5A2 and increased 17βHSD2 indicative of a diminished rate of conversion of P to 5αDHP and of 20αDHP to 5α-pregnan-20-ol-3-one, but increased conversion of 20αDHP to P (see Figure 2).
Other endometrial/gynecological disorders
Although literature is scarce, a potential role of intracrinology is postulated for ovarian cancer (Ito et al., 2016), for adenomyosis and fibroids (Rižner, 2016), for sarcoma, where CYP19A1 expression may have prognostic significance (Kitaoka et al., 2004) and among infertile women (Brosens et al., 2004).
Intracrine drug targets
Endometriosis: blocking the systemic estrogen signaling via P, or GnRH agonist is standard care (Vercellini et al., 2014). Blocking the intracrine E2 generation is the future approach with on-going preclinical/clinical research.
STS inhibition showed promising results. Irosustat (Table 3) inhibited up to 100% the formation of free steroids using ex-vivo material from 27 patients (Purohit et al., 2008) and STS inhibition showed good results in a mouse model of endometriosis, where decreased size and weight of the lesions was observed (Colette et al., 2011). A phase-I clinical trial on 24 volunteers proved the safety of the STS inhibitor E2MATE (PLG2001), which reduced STS activity by over 90% and induced changes in endometrial markers (both alone or co-administered with norethindrone acetate) (Pohl et al., 2014).
Inhibitors of 17βHSD1 are in preclinical phase, and promising results are described using a primate model of endometriosis, where decreased behavior/pain symptoms were reported (Arnold and Einspanier, 2013) and using ex-vivo material from endometriosis patient (over 70% of the patients showed over 80% of enzyme inhibition) (Delvoux et al., 2014).
AKR1C3/17βHSD5 inhibition can interfere with E2, androgen synthesis, and reduce prostaglandin-associated inflammation/proliferation and an inhibitor has recently entered a phase II trial for endometriosis (Table 3). Overall, AIs have limited efficacy for endometriosis (Ferrero et al., 2011; Dunselman et al., 2014),
EC: only in case of advanced stage/metastatic disease hormonal care is given (progestogen, tamoxifen or AIs). AIs alone have limited efficacy with low response rates (Rose et al., 2000; Ma et al., 2004; Lindemann et al., 2014). Promising data were obtained using dual regimen (AI and mTOR inhibitor; Slomovitz et al., 2015) and additional trials on combinatory regimen are on-going. STS inhibitors showed promising results in a mouse subcutaneous model of EC, with decreased tumor growth by 48–67% (Foster et al., 2008b). However, a phase II trial on advanced stage EC was stopped because of the absence of added benefit compared with progestogen treatment (Purohit and Foster, 2012; Pautier et al., 2017).
Preclinical studies on 17βHSD1 inhibitors showed promising results in a mouse model of endometrial hyperplasia (Saloniemi et al., 2010;Järvensivu et al., 2015) and in various models of EC (Konings et al., 2018).
Endometrium: conclusions
The ability to synthesize DHEA from cholesterol (reported by few studies) needs confirmation. However, the endometrium possesses the enzymatic machinery to metabolize sulphated-compounds and DHEA and form androgens and estrogens, (although this contention is wrangled by other authors: Labrie and Labrie, 2013; Labrie, 2015). Further, the endometrium can metabolize androgens and progestogens via AKR1Cs and SRD5As to produce a wide range of compounds, including estrogens (Table 6 and Figure 3). The morphological changes during the menstrual cycle are accompanied by cyclic changes in intracrine steroid and enzyme levels, indicating that steroid exposure needs to be cyclically regulated to support endometrial physiology.
Figure 3.
Effect of steroids (mainly estrogens) and intracrine networks in central nervous system, lungs, digestive system, uterus and bone. Italics and by brackets are those metabolism/reactions that need conformation by independent authors (because validated at the mRNA level only or in few studies). * EC, epithelial cells; **SMC, smooth muscle cells; #Chol, cholesterol. The drawing was kindly generated by Dr. Margaretha A. Skowron (Department of Urology, University Düsseldorf, Germany) for this review.
Gastrointestinal tract (GIT) and digestive system (DS)
ERα and ERβ are expressed throughout the GIT and DS (esophagus, stomach, colon, gallbladder, pancreas) and epidemiological studies show important influence of sex hormones in DS physiology and disturbances, with a clear gender-dependency. In the duodenum, estrogens regulate bicarbonate secretion (Nayeb-Hashemi and Kaunitz, 2009; Tuo et al., 2011). This is an important defense mechanism of the mucosa against acids discharged from the stomach, and men develop duodenal ulcer two/three-times more often than premenopausal women (Wu et al., 2008). Such estrogen protective effect is recapitulated in animal studies exposed to estrogens and anti-estrogens, and is mediated by a rapid action (i.e., non genomic) of ERα on membrane ion channels (Smith et al., 2008).
ERα, ERβ and GPER mediate important effects on the pancreatic beta-cells during adaptation to insulin resistance periods (e.g., pregnancy, puberty, obesity; Nadal et al., 2011). In mice, ERα signaling regulates proliferation of beta-cell during development and after injury (Yuchi et al., 2015).
Men are also more likely than women to develop cancer in the esophagus, stomach and colon. Accordingly, estrogen treatment for prostate cancer decreases the incidence of gastric cancer and menopausal status in women is associated with colorectal cancer CRC risk (Freedman et al., 2007; Kennelly et al., 2008; Hogan et al., 2009; Duell et al., 2010). ERβ results oncoprotective at several GIT sites (Kennelly et al., 2008; Barzi et al., 2013; Caiazza et al., 2015) and low expression correlate with high CRC stage in mice and with poor differentiated gallbladder cancer in humans (Hogan et al., 2009).
The association between estrogens and DS cancer risk is however controversial. The Women's Health Initiative and other large studies showed that combined estrogens plus P hormone replacement therapy (HRT) decreases CRC risk, but increases that of gallbladder. In addition, CRC during HRT has a higher grade (Kennelly et al., 2008; Hogan et al., 2009; Rennert et al., 2009; Foster, 2013; Mueller et al., 2015). However, a recent randomized, placebo-controlled trial enrolling over 10,000 women receiving estrogens alone vs. placebo found no difference in CRC incidence (Lavasani et al., 2015). Such complexity is recapitulated in animal studies where estrogens and androgens can have distinct and opposite effects on colitis and CRC (Amos-Landgraf et al., 2014; Heijmans et al., 2014). Overall, the association between DS disturbances/cancers with estrogens depends on the moment in life, extent and nature (endogenous or exogenous) of exposure and is influenced by the relative balance of the receptors (Foster, 2013). Similarly, androgens influence DS pathophysiology via complex and unclear mechanisms involving classical, membrane signaling, level of free and SHBG bound T (Roshan et al., 2016).
The lack of clear conclusion and the fact that the levels of circulating endogenous estrogens in women do not influence CRC risk indicates that intracrine steroids may have a predominant role irrespective of their circulating levels (Sato et al., 2009; Falk et al., 2015).
Intracrinology in healthy GIT–systematic search
In total, 29 original papers were retrieved that described the levels of the intracrine enzymes in the GIT, published from the late 80's (Table 7 and Supplemental panel: “Systematic Review”).
Table 7.
Expression of intracrine enzymes in the gastrointestinal tract (GIT)-results of the systematic search.
| Gene | Detection | Gastrointestinal tract | ||||||
|---|---|---|---|---|---|---|---|---|
| Molecule | Technique# | St* | References | S.I.* | References | L.I.* | References | |
| CYP11A1 | Protein | IHC | no | Saitoh et al., 1992 | n.d. | n.d. | ||
| CYP19A1 | Protein | Activity | n.d. | n.d. | yes | English et al., 2000 | ||
| CYP19A1 | Protein | IHC | no | Saitoh et al., 1992 | n.d. | yes | English et al., 2000 | |
| WB | no | Saitoh et al., 1992 | n.d. | n.d. | ||||
| HSD17B oxidative activity | n.d. | n.d. | yes | English et al., 1999 | ||||
| HSD17B reductive activity | n.d. | n.d. | yes | English et al., 1999 | ||||
| 17βHSD1 | mRNA | RT-PCR | no | Oduwole et al., 2003a | n.d. | yes | Rawłuszko et al., 2011 | |
| NB | n.d. | no | Casey et al., 1994 | no | Casey et al., 1994 | |||
| ISH | n.d. | no | Oduwole et al., 2002 | no | Oduwole et al., 2002 | |||
| Protein | WB | n.d. | n.d. | yes | Rawłuszko et al., 2011 | |||
| 17βHSD2 | mRNA | RT-PCR | yes | Oduwole et al., 2003a; Frycz et al., 2015 | n.d. | n.d. | ||
| NB | n.d. | yes | Casey et al., 1994 | yes | Casey et al., 1994 | |||
| ISH | n.d. | yes | Oduwole et al., 2002 | yes | Oduwole et al., 2002, 2003b | |||
| Protein | IHC | n.d. | n.d. | yes | English et al., 2000; Mueller et al., 2015 | |||
| WB | yes | Frycz et al., 2015 | n.d. | yes | English et al., 2000; Mueller et al., 2015 | |||
| 17βHSD4 | mRNA | NB | n.d. | yes | Möller et al., 1999 | yes | Möller et al., 1999 | |
| Protein | IHC | n.d. | n.d. | yes | English et al., 2000; Mueller et al., 2015 | |||
| WB | n.d. | n.d. | yes | English et al., 2000; Mueller et al., 2015 | ||||
| 17βHSD10 | mRNA | RT-PCR | n.d. | n.d. | yes | De Preter et al., 2012 | ||
| 17βHSD12 | mRNA | RT-PCR | n.d. | yes | Sakurai et al., 2006 | n.d. | ||
| NB | n.d. | yes | Sakurai et al., 2006 | no | Sakurai et al., 2006 | |||
| Protein | IHC | yes | Sakurai et al., 2006 | yes | Sakurai et al., 2006 | yes | Sakurai et al., 2006 | |
| AKR1C3 | mRNA | Comp-RT | yes | Frycz et al., 2016 | n.d. | n.d. | ||
| NB | yes | Frycz et al., 2016 | yes | Lin et al., 1997 | yes | Lin et al., 1997 | ||
| Protein | IHC | yes | Miller et al., 2012b; Chang et al., 2013 | yes | Chang et al., 2013 | yes | Chang et al., 2013 | |
| SRD5A1 | Protein | IHC | yes | Aumüller et al., 1996 | yes | Aumüller et al., 1996 | yes | Aumüller et al., 1996 |
| SRD5A2 | Protein | IHC | yes | Aumüller et al., 1996 | yes | Aumüller et al., 1996 | yes | Aumüller et al., 1996 |
| STS | mRNA | RT-PCR | n.d. | no | Miki et al., 2002 | yes | Dalla Valle et al., 2007 | |
| RT-PCR | – | – | no | Miki et al., 2002 | ||||
| Protein | IHC | n.d. | no | Miki et al., 2002 | no | Miki et al., 2002; Sato et al., 2009 | ||
| Protein | Activity | n.d. | n.d. | yes | Munroe and Chang, 1987 | |||
| SULT1E1 | mRNA | RT-PCR | no | Nishimura and Naito, 2006 | yes | Miki et al., 2002; Nishimura and Naito, 2006 | yes | Miki et al., 2002; Teubner et al., 2007; Riches et al., 2009 |
| – | – | no | Nishimura and Naito, 2006 | |||||
| NB | n.d. | yes | Her et al., 1996 | n.d. | ||||
| Protein | IHC | no | Chen et al., 2003; Teubner et al., 2007 | yes | Miki et al., 2002; Teubner et al., 2007 | yes | Miki et al., 2002; Teubner et al., 2007; Sato et al., 2009 | |
| WB | n.d. | yes | Her et al., 1996; Chen et al., 2003; Teubner et al., 2007; Riches et al., 2009 | no | Chen et al., 2003 | |||
| Activity | no | Chen et al., 2003; Teubner et al., 2007 | yes | Teubner et al., 2007 | yes | Teubner et al., 2007 | ||
| SULT2A1 | mRNA | RT-PCR | no | Nishimura and Naito, 2006 | yes | Nishimura and Naito, 2006 | no | Nishimura and Naito, 2006 |
| ISH | yes | Tashiro et al., 2000 | n.d. | n.d. | ||||
| NB | n.d. | yes | Her et al., 1996 | n.d. | ||||
| Protein | IHC | no | Teubner et al., 2007 | yes | Teubner et al., 2007 | yes | Teubner et al., 2007 | |
| WB | yes | Tashiro et al., 2000; Chen et al., 2003 | yes | Her et al., 1996; Chen et al., 2003; Teubner et al., 2007; Riches et al., 2009 | yes | Chen et al., 2003; Teubner et al., 2007; Riches et al., 2009 | ||
| WB | n.d. | n.d. | no | Chen et al., 2003 | ||||
| Activity | yes | Tashiro et al., 2000 | yes | Chen et al., 2003; Teubner et al., 2007 | yes | Chen et al., 2003; Teubner et al., 2007 | ||
| Activity | no | Teubner et al., 2007 | – | – | ||||
| SULT1A1 | mRNA | RT-PCR | yes | Nishimura and Naito, 2006 | yes | Nishimura and Naito, 2006 | yes | Nishimura and Naito, 2006 |
| Protein | IHC | yes | Teubner et al., 2007 | yes | Teubner et al., 2007 | yes | Teubner et al., 2007 | |
| WB | yes | Teubner et al., 2007 | yes | Teubner et al., 2007; Riches et al., 2009 | yes | Teubner et al., 2007; Riches et al., 2009 | ||
| Activity | yes | Teubner et al., 2007 | yes | Teubner et al., 2007 | yes | Teubner et al., 2007 | ||
| SULT2B1 | mRNA | RT-PCR | no | Nishimura and Naito, 2006 | yes | Nishimura and Naito, 2006 | no | Nishimura and Naito, 2006 |
| NB | n.d. | n.d. | no | Meloche and Falany, 2001 | ||||
Primary/original references were analyzed and reviews were excluded (and are cited ad hoc in the text). The table report only the enzymes whose expression was assessed in reviewed studies**.
St: stomach; S.I.: small intestine; L.I.: large intestine.
Technique abbreviations. For mRNA detection, NB: northern blot; ISH: in situ hybridisation; RT-PCR: reverse transcription quantitative (or semi-quantitative) PCR; Comp-RT: competitive RT-PCR assay; NB: northern blotting. For protein detection: IHC: immunohistochemistry; WB; western blotting; activity: enzyme activity measurement.
**No publication was found describing the expression of StAR, 3βHSD1, 3βHSD2, 17βHSD6, 7, 8, 9, 11, 13, 14 15, DHRS11, AKR1C1 AKR1C2 and AKR1C4.
n.d.: not determined.
Stomach intracrinology.
The stomach is an endocrine tissue, and in rodents it produces steroids starting at birth and throughout adulthood (Kobayashi et al., 2013). Human gastric mucosa expresses 17βHSD1, 2, 12 and AKR1C3/17βHSD5 (Table 7). The mRNA for 17βHSD2 in mucosa surface and glandular epithelium inversely correlates with age in both genders (Oduwole et al., 2003a). Luminal gastric mucosa has strong AKR1C3/17βHSD5 immunoreactivity that decreases toward the gastric pits (Chang et al., 2013). Weak immunoreactivity for 17βHSD12 localizes in the fundic glands and in the squamous epithelium of the esophagus (Sakurai et al., 2006).
Sulphatases in parietal cells of the gastric glands have a protective role in detoxification. Estrogenic SULT1E1 is not expressed whereas data for SULT2A1 are inconsistent. SULT2A1 was detected in the gastric mucosa in a study on seven subjects (Tashiro et al., 2000), but it was low/absent in other studies on 39 (Teubner et al., 2007) and 23 subjects (Chen et al., 2003).
Small intestine: duodenum–jejunum–ileum.
Due to its high exposure to food components and harmful xenobiotics, the duodenum expresses several phase I/II enzymes including DHEA/estrogenic SULT1E1, 2A1, 1A1 (Table 7). Protein and enzyme activity of SULT1E1 and 2A1 are present in human jejunum and ileum but absent in duodenum (Teubner et al., 2007), mRNA and protein levels vary with no relation either with age or gender (Her et al., 1996; Nishimura and Naito, 2006). In a study on 23 subjects, SULT1E1 and 2A1 varied inter-individually and between different intestine tracts (Chen et al., 2003). The duodenal mucosa expresses 17βHSD2, but not 17βHSD1 (Casey et al., 1994; Oduwole et al., 2003a) and shows strong luminal AKR1C3/17βHSD5 (Chang et al., 2013) and weak 17βHSD12 immunoreactivity (Sakurai et al., 2006) that decreases toward the Brunner's gland (Chang et al., 2013).
Large intestine: colon, cecum, rectum
The intracrinology of healthy colon mucosa and its relation to CRC was recently reviewed (Foster, 2013). Studies dating from 1987 demonstrated the presence of CYP19A1, 17βHSD reductive and oxidative enzymatic activities, plus the expression of 17βHSD1, 2, 4, CYP19A1, STS and SULT1E1 (Table 7). Most 17βHSDs tend to have higher levels at the surface than in cryptal epithelial cells as indicated for 17βHSD2 mRNA (Oduwole et al., 2002; Foster, 2013), and for the immunoreactivity of AKR1C3/17βHSD5 (very strong; Chang et al., 2013) and 17βHSD12 (weak; Sakurai et al., 2006).
Pancreas
Radiolabelled substrates demonstrated the presence of CYP19A1 and SRD5A activities in human pancreatic tissue (Iqbal et al., 1983), which expresses 17βHSD2, 12, STS, SULT1E1 (Casey et al., 1994; Miki et al., 2002; Sakurai et al., 2006; Dalla Valle et al., 2007). High levels of AKR1C3/17βHSD5 localized in pancreatic ductules (acini and islets of Langerhans resulted negative; Chang et al., 2013).
Association with diseases
SNPs in genes controlling estrogen synthesis, response and deactivation are associated with GIT cancers (Freedman et al., 2009; Cho et al., 2012; Zeng et al., 2016) and AKR1C4 is a candidate gene in hereditary CRC (Gylfe et al., 2013; Table 5). Also variations in the expression of these genes associate with GIT disturbances. Low 17βHSD10 levels are associated with aberrant butyrate β-oxidation and ulcerative colitis (De Preter et al., 2012). The epithelial 17βHSD2 level is low in case of stomach, duodenal cancer and chronic gastritis, though it is high in regenerating epithelium close to active gastritis and ulcers (Oduwole et al., 2003a). In a study on 34 gastric tumors and adjacent healthy tissue, the mRNA and protein levels of 17βHSD2 and AKR1C3/17βHSD5 were down-regulated in cancer (Frycz et al., 2015, 2016). Some studies showed lower oxidative 17βHSD activity and mRNA level of 17βHSD2 (and 4) in CRC vs. adjacent normal tissue, suggesting a protective role of estrogen deactivation. However, another study on 35 women and 39 men found that high 17βHSD2 levels were associated with poor prognosis in female patients with distal CRC (reviewed in Foster, 2013). Also 17βHSD1 level measured by RT-qPCR and western blotting in specimens from 52 patients was lower in CRC than adjacent normal mucosa (Rawłuszko et al., 2011). CRC show also higher CYP19A1 mRNA compared with adjacent normal mucosa (n = 31) (Sato et al., 2012).
Although no clear target for drugs has been identified in the intracrine network, intracrine enzymes showed some values as biomarkers. In CRC, high STS/SULT1E1 ratio correlates with poor prognosis (Foster, 2013) and AKR1C3/17βHSD5 expression with lymph-node metastasis (Nakarai et al., 2015). In addition, AKR1C1 and AKR1C3/17βHSD5 associate with cisplatin resistance in CRC, hence inhibitors of these AKR1Cs may be used to re-sensitize patients to chemotherapy (Matsunaga et al., 2013). In a study were the levels of E1, E2 and DHEA-S were measured in CRC specimens and adjacent normal mucosa of men and women by LC-MS, intra-tumor estrogens were elevated and (in particular E1) correlated with poor prognosis. In line with an unfavorable role of intra-tissue estrogens, absence on STS was associated with long survival (Sato et al., 2009).
GIT: conclusions
Human GIT/DS is unable to metabolize cholesterol and there is no clear evidence that it expresses 3βHSDs, hence DHEA cannot be used to generate androgens and estrogens (Table 7 and Figure 3). Several SULTs are expressed throughout GIT and involved in detoxification and STS is regulated by estrogen in vitro via non-classical GPER signaling (Gilligan et al., 2017).
The role of steroids in pathology is complex, with divergent effects that depend on time, length and extent of exposure. In line with this, intracrine networks have unclear roles in pathogenesis. In the GIT these networks are strongly involved in the metabolisms of fatty acids and bile acids (outside the scope of this review).
Bone tissue and skeletal system
Bones consist of mineralized connective tissue with structural and supportive functions. The hard exterior part (cortical bone) and the trabecular and spongy cancellous tissue filling the bone interior are identical but differ in the level of mineralization. Osteoblasts, derived from multipotent mesenchymal stem cells, build the bone tissue through deposition of Type-I collagen and through the release of ions that combine chemically forming the bone mineral. Osteoclasts differentiate from hematopoietic stem cells and cause resorption of the mineralized bone mass. The balance between osteoblasts and osteoclasts regulates mineral deposition and resorption. Sex steroid hormones contribute to control bone development during puberty, contribute to bone physiology, bone mass maintenance and regulate the rate of mineral bone deposition and resorption (Svoboda et al., 2010).
The presence of the ERs as well as other hormone-receptors in normal osteoblastic cells, osteoclasts and osteoblasts is documented (Gruber et al., 2002) and estrogens and androgens stimulate bone formation and inhibit bone resorption in both males and females. During human puberty and throughout adulthood, E2 and T induce osteoblast proliferation (Kassem et al., 1998), which is mediated by IGF and GH (Riggs et al., 2002; Svoboda et al., 2010). Such human effects are well recapitulated in animal models. ERα-KO (Vidal et al., 2000) and CYP19A1-KO mice (Oz et al., 2000) exhibit low BMD in both genders and E2 treatment rescues the CYP19A1-KO phenotype (Miyaura et al., 2001). Additionally, ovariectomy stimulates osteoclast differentiation through (indirect) increased levels of IL-1, 6 and TNF in osteoblasts and other bone-derived stromal cells (Gruber et al., 2002; Svoboda et al., 2010).
Accelerated bone loss and increased osteoporotic fractures are associated with postmenopausal estrogen deficiency and low sex steroid levels elicit similar manifestations in men (Compston, 2001; Riggs et al., 2002; Syed and Khosla, 2005). Free E2 levels are associated with low lumbar spine and femoral neck bone mineral density (BMD) in both genders (Zarrabeitia et al., 2007) and estrogen therapy reduces bone loss and the risk of fracture in women with osteoporosis (Gruber et al., 2002).
Intracrinology in healthy bone–systematic search
Bone expresses CYP19A1 and 17βHSD1, and mRNA in situ hybridisation and immunohistochemistry signals were seen in lining cells, osteoblasts, chondrocytes of articular cartilage, and adipocytes adjacent to bone trabeculae in both male and female tibiae. CYP19A1 mRNA was also widely present in various bones (ribs, femurs) with inter-individual variability, but no relation with gender or age (Sasano et al., 1997). STS and 17βHSD activities were demonstrated by recovery of [3H]E1 and [3H]E2 after incubating femur-head fragments with [3H]E1-S (15 women and 12 men with osteoarthritis indicated for hip replacement). No gender-related differences were observed and E2 formation from androgens was lower than that from E1-S, indicating a predominant role of the sulphatase pathway in bone estrogen supply (Muir et al., 2004). Subsequent studies also demonstrated the presence of CYP11A1, CYP17A1, 17βHSD reductive and oxidative activity in bone tissues (Table 8). Overall, however, only six papers describing the level of intracrine enzymes in bone tissues were retrieved by the systemic search (Table 8) and most studies on bone intracrinology used in vitro cell cultures. In vitro studies were not included in our systematic review, but those on bone are briefly described in the next paragraph. These studies demonstrate the presence of a complex intracrine networks.
Table 8.
Expression of intracrine enzymes in bone, lungs and central nervous system (CNS) – results of the systematic search.
| Gene | Detection | Bone | References | Lung | References | CNS | References | |
|---|---|---|---|---|---|---|---|---|
| Molecule | Technique# | |||||||
| StAR | mRNA | RT-PCR | n.d. | yes∧ | Pezzi et al., 2003 | n.d. | ||
| CYP11A1 | mRNA | RT-PCR | yes | Rodríguez-Sanz et al., 2015 | yes∧ | Pezzi et al., 2003 | yes | Stoffel-Wagner, 2001 |
| Comp-RT | n.d. | n.d. | yes | Beyenburg et al., 1999; Watzka et al., 1999 | ||||
| Protein | WB | yes* | Rodríguez-Sanz et al., 2015 | n.d. | ||||
| CYP17A1 | mRNA | RT-PCR | yes | Rodríguez-Sanz et al., 2015 | no∧ | Pezzi et al., 2003 | yes | Stoffel-Wagner, 2001 |
| RT-PCR | – | – | no | Steckelbroeck et al., 2004b | ||||
| Protein | WB | yes* | Rodríguez-Sanz et al., 2015 | n.d. | n.d. | |||
| IHC | n.d. | n.d. | no | Steckelbroeck et al., 2004b | ||||
| Activity | n.d. | n.d. | no | Steckelbroeck et al., 2004b | ||||
| CYP19A1 | mRNA | RT-PCR | yes | Oz et al., 2001 | yes | Pezzi et al., 2003; Aresti et al., 2014; Kohno et al., 2014; Konings et al., 2017 | yes | Sasano et al., 1998; Stoffel-Wagner et al., 1998a; Stoffel-Wagner, 2001; Yague et al., 2006 |
| Comp-RT | n.d. | n.d. | yes | Stoffel-Wagner et al., 1999a | ||||
| ISH | yes | Sasano et al., 1997 | n.d. | n.d. | ||||
| Protein | IHC | yes | Sasano et al., 1997; Oz et al., 2001 | yes | Verma et al., 2013; Siegfried and Stabile, 2014; Taniuchi et al., 2014; Konings et al., 2017 | yes | Naftolin et al., 1996; Yague et al., 2006, 2010 | |
| ELISA | n.d. | yes | Aresti et al., 2014; Skjefstad et al., 2016; Tanaka et al., 2016 | n.d. | ||||
| Activity | yes | Schweikert et al., 1995 | yes | Taniuchi et al., 2014 | yes | Naftolin and MacLusky, 1982; Stoffel-Wagner, 2001 | ||
| 3βHSD1 | mRNA | RT-PCR | n.d. | yes∧ | Pezzi et al., 2003 | no | Stoffel-Wagner, 2001 | |
| 3βHSD2 | mRNA | RT-PCR | n.d. | no∧ | Pezzi et al., 2003 | no | Stoffel-Wagner, 2001 | |
| 17βHSDs | ||||||||
| HSD17B oxidative activity | yes | Muir et al., 2004 | n.d. | yes | Steckelbroeck et al., 1999, 2003; Stoffel-Wagner, 2001 | |||
| HSD17B reductive activity | yes | Muir et al., 2004 | n.d. | Tsai et al., 2001; Attar et al., 2009; Huhtinen et al., 2014 | yes | Steckelbroeck et al., 1999, 2003; Stoffel-Wagner, 2001 | ||
| 17βHSD1 | mRNA | RT-PCR | n.d. | yes | Takeyama et al., 2000; Drzewiecka et al., 2015; Konings et al., 2017) | yes | Stoffel-Wagner et al., 1999a; Stoffel-Wagner, 2001 | |
| Comp-RT | n.d. | n.d. | yes | Beyenburg et al., 2000 | ||||
| mRNA | ISH | yes | Sasano et al., 1997 | n.d. | n.d. | |||
| 17βHSD1 | Protein | Comp-RT | n.d. | n.d. | yes | Stoffel-Wagner et al., 1999b; Beyenburg et al., 2000 | ||
| IHC | yes | Sasano et al., 1997 | yes | Verma et al., 2013; Drzewiecka et al., 2015; Konings et al., 2017 | n.d. | |||
| WB | n.d. | yes | Drzewiecka et al., 2015 | n.d. | ||||
| 17βHSD2 | mRNA | RT-PCR | n.d. | yes | Takeyama et al., 2000; Simard et al., 2010; Konings et al., 2017 | no | Stoffel-Wagner, 2001 | |
| Comp-RT | n.d. | n.d. | n.d. | Stoffel-Wagner et al., 1999b; Beyenburg et al., 2000 | ||||
| NB | n.d. | n.d. | no | Casey et al., 1994 | ||||
| Protein | IHC | n.d. | yes | Verma et al., 2013 | n.d. | |||
| WB | n.d. | n.d. | ||||||
| 17βHSD3 | mRNA | RT-PCR | n.d. | n.d. | yes | Stoffel-Wagner, 2001 | ||
| Comp-RT | n.d. | n.d. | yes | Stoffel-Wagner et al., 1999b; Beyenburg et al., 2000 | ||||
| 17βHSD4 | mRNA | RT-PCR | n.d. | yes | Konings et al., 2017 | yes | Stoffel-Wagner et al., 1999a; Stoffel-Wagner, 2001; Steckelbroeck et al., 2003 | |
| Comp-RT | n.d. | n.d. | yes | Stoffel-Wagner et al., 1999b; Beyenburg et al., 2000 | ||||
| NB | n.d. | yes | Möller et al., 1999 | yes | Möller et al., 1999 | |||
| 17βHSD6 | mRNA | RT-PCR | n.d. | yes | Huang and Luu-The, 2000; Steckelbroeck et al., 2003 | |||
| 17βHSD7 | mRNA | RT-PCR | n.d. | yes | Törn et al., 2003; Konings et al., 2017 | yes | Steckelbroeck et al., 2003 | |
| 17βHSD8 | mRNA | RT-PCR | n.d. | yes | Ohno et al., 2008 | yes | Steckelbroeck et al., 2003 | |
| 17βHSD9 | mRNA | RT-PCR | n.d. | n.d. | yes | Steckelbroeck et al., 2003 | ||
| 17βHSD10 | mRNA | RT-PCR | n.d. | n.d. | yes | Steckelbroeck et al., 2003; He and Yang, 2006; Hovorkova et al., 2008 | ||
| Protein | IHC | n.d. | n.d. | yes | He et al., 2005b | |||
| C-ELISA | n.d. | n.d. | yes | Hovorkova et al., 2008 | ||||
| 17βHSD11 | mRNA | RT-PCR | n.d. | yes | Chai et al., 2003 | yes | Steckelbroeck et al., 2003 | |
| mRNA | NB | n.d. | yes | Chai et al., 2003 | n.d. | |||
| Protein | IHC | n.d. | yes | Brereton et al., 2001 | n.d. | |||
| 17βHSD12 | mRNA | RT-PCR | n.d. | yes | Sakurai et al., 2006; Konings et al., 2017 | yes | Sakurai et al., 2006 | |
| mRNA | NB | n.d. | yes | Sakurai et al., 2006 | yes | Sakurai et al., 2006 | ||
| mRNA | NB | n.d. | n.d. | no | Casey et al., 1994 | |||
| Protein | IHC | n.d. | Yes$ | Sakurai et al., 2006 | n.d. | |||
| AKR1C activity | n.d. | n.d. | yes | Steckelbroeck et al., 2010 | ||||
| AKR1C1 | mRNA | RT-PCR | n.d. | n.d. | yes | Penning et al., 2000; Stoffel-Wagner et al., 2003; Steckelbroeck et al., 2010 | ||
| AKR1C2 | mRNA | RT PCR | n.d. | n.d. | yes | Penning et al., 2000 | ||
| Comp-RT | n.d. | n.d. | yes | Stoffel-Wagner et al., 2003; Steckelbroeck et al., 2004a, 2010 | ||||
| AKR1C3 | mRNA | RT PCR | n.d. | yes | Simard et al., 2010; Konings et al., 2017 | n.d. | ||
| Comp-RT | n.d. | n.d. | yes | Stoffel-Wagner et al., 2000, 2003; Steckelbroeck et al., 2001, 2004a; Stoffel-Wagner, 2001 | ||||
| NB | n.d. | n.d. | Lin et al., 1997 | n.d. | ||||
| Protein | IHC | n.d. | yes | Miller et al., 2012b; Chang et al., 2013 | n.d. | |||
| AKR1C4 | mRNA | RT-PCR | n.d. | n.d. | no | Steckelbroeck et al., 2010 | ||
| Comp-RT | n.d. | n.d. | no | Stoffel-Wagner et al., 2000, 2003; Steckelbroeck et al., 2004a | ||||
| SRD5A1 | mRNA | Comp-RT | n.d. | n.d. | yes | Stoffel-Wagner et al., 1998b, 2000, 2003 | ||
| Protein | IHC | n.d. | yes | Aumüller et al., 1996 | yes | Aumüller et al., 1996 | ||
| activity | n.d. | n.d. | yes | Stoffel-Wagner et al., 1998b; Steckelbroeck et al., 2001 | ||||
| SRD5A2 | mRNA | Comp-RT | n.d. | n.d. | no | Stoffel-Wagner et al., 1998b, 2000 | ||
| Protein | IHC | n.d. | yes | Aumüller et al., 1996 | yes | Aumüller et al., 1996 | ||
| STS | mRNA | RT-PCR | n.d. | yes | Konings et al., 2017 | yes | Steckelbroeck et al., 2004b | |
| RT-PCR | – | no | Miki et al., 2002 | no | Miki et al., 2002 | |||
| Protein | IHC | n.d. | yes | Iida et al., 2013 | yes | Steckelbroeck et al., 2004b | ||
| IHC | – | no | Miki et al., 2002 | no | Miki et al., 2002 | |||
| Activity | yes | Muir et al., 2004 | yes | Milewich et al., 1983; Munroe and Chang, 1987 | yes | Platia et al., 1984 | ||
| SULT1E1 | mRNA | RT-PCR | yes | Svoboda et al., 2007 | yes | Miki et al., 2002; Konings et al., 2017 | yes | Miki et al., 2002; Nishimura and Naito, 2006 |
| RT-PCR | n.d. | n.d. | no | Salman et al., 2011 | ||||
| NB | n.d. | n.d. | n.d. | |||||
| Protein | IHC | n.d. | yes | Miki et al., 2002; Iida et al., 2013 | yes | Miki et al., 2002 | ||
| IHC | n.d. | – | no | Salman et al., 2011 | ||||
| WB | n.d. | yes | Riches et al., 2009 | n.d. | ||||
| Activity | n.d. | yes | Jones et al., 1992 | no | Miki et al., 2002 | |||
| SULT2A1 | mRNA | RT-PCR | n.d. | n.d. | no | Nishimura and Naito, 2006; Salman et al., 2011 3/4 Table VII continues | ||
| Protein | IHC | n.d. | yes | Riches et al., 2009 | no | Steckelbroeck et al., 2004b; Salman et al., 2011 | ||
| Activity | n.d. | n.d. | no | Steckelbroeck et al., 2004b. | ||||
| SULT1A1 | mRNA | RT-PCR | n.d. | n.d. | yes | Nishimura and Naito, 2006; Salman et al., 2011 | ||
| Protein | IHC | n.d. | n.d. | yes | Nishimura and Naito, 2006; Salman et al., 2011 | |||
| WB | n.d. | yes | Riches et al., 2009 | n.d. | ||||
| SULT2B1 | mRNA | RT-PCR | n.d. | yes | He et al., 2004, 2005a | yes | Nishimura and Naito, 2006; Salman et al., 2011 | |
| NB | n.d. | yes | He et al., 2004, 2005a | no | Meloche and Falany, 2001 | |||
| NB | – | no | Meloche and Falany, 2001 | – | ||||
| Protein | IHC | n.d. | yes | He et al., 2004, 2005a | yes | Nishimura and Naito, 2006; Salman et al., 2011 | ||
Primary/original references were analyzed and reviews were excluded (and are cited ad hoc in the text). The table report only the enzymes whose expression was assessed in reviewed studies**.
Technique abbreviations. For mRNA detection, NB: northern blot; ISH: in situ hybridisation; RT-PCR: reverse transcription quantitative (or semi-quantitative) PCR; Comp-RT: competitive RT-PCR assay; NB: northern blotting. For protein detection: IHC: immunohistochemistry; C-ELISA: competitive ELISA assay; WB: western blotting; activity: enzyme activity measurement.
CYP11A1 and CYP17A1 activities were detected in primary cells of bone.
**No publication was found describing the expression of 17βHSD13, 14, 15 and DHRS11.
Detected in fetal lung tissue.
IHC signal in bronchial epithelium.
Bone intracrinology: in vitro and in vivo
From early ‘90s, various isotopic techniques demonstrated the presence of CYP19A1, 17βHSD reductive/oxidative, 3βHSD and STS activities and the mRNA expression of 17βHSD1, 2, 4, STS, SULT1E1, CYP19A1 and SDR5A in human osteoblastic (e.g., HOS, U20S, HTB-96 and MG63) and osteosarcoma cell lines like CRL-1543 (Purohit et al., 1992; Fujikawa et al., 1997; Jakob et al., 1997; Dong et al., 1998; Saito and Yanaihara, 1998; Janssen et al., 1999; Muir et al., 2004; Svoboda et al., 2007; Dias and Selcer, 2014).
In vitro evidence using osteoblastic cells show that E2 has mitogenic effects, which is blocked by the ERα antagonist fulvestrant. Since both E1-S and DHEA-S elicit effects similar to E2, which are blocked by STS inhibition (Selcer and Difrancesca, 2012; Dias and Selcer, 2014), these studies demonstrate that conjugated steroids are activated and that DHEA is converted to E2. Studies in rat osteoblast with [14C]T demonstrated that T is converted by SRD5As and AKR1Cs to 3α/3βDIOLs, which induce proliferation via activation of ER (and not AR) (Enríquez et al., 2013).
In vitro models of osteoblast differentiation showed that various differentiation stages are accompanied by declines in STS, CYP19A1 and 17βHSD1 (Janssen et al., 1999; Dias and Selcer, 2016).
In rats, during and after sexual maturation, in situ hybridization showed that ERα and ERβ localize in osteoblasts, osteoclasts and osteocytes covering the tibia metaphysis (responsible for elongation of long bones), and co-localize with STS. Starting at sexual maturation (e.g., 7-week-old), ERs also co-localize with CYP19A1, 17βHSD1, 2 and SRD5A1 (van der Eerden et al., 2004). In addition, male transgenic mice overexpressing 17βHSD2 show disturbed IGF-I/steroid actions in bone, with growth retardation, decreased bone formation at prepuberty and decreased serum levels of IGF-I, osteocalcin and T (Shen et al., 2008).
Diseases and treatments
Genetic variants of estrogen and intracrine pathways are associated with bone disturbances (Table 5). Defects in the CYP19A1 and ERα are associated with low BMD and other skeletal disturbances (e.g., high stature, delayed bone age) and estrogen therapy ameliorates some bone abnormalities caused by CYP19A1 deficiencies in men (Smith et al., 1994; Morishima et al., 1995; Carani et al., 1997; Mullis et al., 1997; Bilezikian et al., 1998). In lumbar vertebrae, CYP19A1 levels correlate with changes in osteoporotic degree (Sasano et al., 1997).
Inhibitors of 17βHSD2 attracted attention as potential drugs to oppose the effects of low E2 on BMD, fracture and osteoporosis. Ovariectomised female macaques receiving a 17βHSD2 inhibitor display desirable bone balance, bone strength and lower bone resorption compared with untreated controls (Bagi et al., 2008). Several compounds targeting this enzyme have been developed and their use and challenges in osteoporosis were recently reviewed (Soubhye et al., 2015).
In a study on 35 chondrosarcoma biopsies (a malignant bone cancer occurring in middle aged patients), ERα (mRNA and IHC) and CYP19A1 (mRNA and activity) were demonstrated in the majority of the samples, and the AI exemestane impaired the E2- and androgen-induced proliferation of primary chondrosarcoma cells (Cleton-Jansen et al., 2005). Although AIs were proposed as novel drugs to treat this condition (Bovée et al., 2005), a pilot study on six patients with progressive disease showed no benefit of exemestane in progression-free survival compared with untreated patients (Meijer et al., 2011).
In a study of 28 osteosarcoma specimens (one of the most common bone cancers developing at young age) strong ERβ and PR immunoreactivity was seen in over 80% of the samples (and also correlated with Ki67). ERα and AR staining was seen in 30% of the samples, whereas CYP19A1 was undetected (Dohi et al., 2008). In another study, 20 osteosarcoma specimens, including 11 good responders to chemotherapy and nine poor responders, were subjected to cDNA microarray and 17βHSD10 resulted unregulated in the poor responder group. Results were further confirmed by IHC on 69 archival biopsies, hence targeting 17βHSD10 may be a valuable approach for drug (re)sensitisation (Salas et al., 2009).
Additional intracrine imbalances are described in bone diseases, such as higher androgen reducing 17βHSD activity in benign vs. malignant tumors, declines of CYP19A1 from normal bone to osteosarcoma and expression of SULT1E1 in the majority of the skeletal benign and malignant lesions, originated in bones or from primary tumors elsewhere (Svoboda et al., 2007).
Bone tissue: conclusions
In vitro, animal and human studies show that intracrinology controls bone development, benign and malignant conditions, and offer novel potential drug targets (Table 8 and Figure 3). Steroids can be synthesized in situ from cholesterol (Rodríguez-Sanz et al., 2015) and can be recruited from the serum via the sulphatase pathway. DHEA is substrate for androgen and estrogen production. The action of androgens is partly mediated by their conversion to estrogens via CYP19A1 or to estrogenic 3α/βDIOLs (Vanderschueren et al., 2008).
Lungs
Sex steroids play an important role in lung development and homeostasis. Androgens, progestogens and estrogens are present and exert genomic and non-genomic actions via their hormone-receptors. Classical ERs (with ERβ as predominant form) and membrane GPER are expressed (Couse et al., 1997; Prossnitz and Barton, 2011; Konings et al., 2017). Sex steroids remain active in the lungs throughout lifetime and modulate lung function in both a beneficial or detrimental way, extensively reviewed (González-Arenas and Agramonte-Hevia, 2012; Townsend et al., 2012; Sathish et al., 2015).
E2 and P regulate epithelial sodium channel expression in alveolar epithelial cells (Luo et al., 2015). In alveolar smooth muscle cells, E2 induces bronchodilation via the reduction of intracellular Ca2+ (Townsend et al., 2010).
Both human and animal studies support a promoting role for estrogens and inhibitory role for androgens in lung development and maturation. During gestation and neonatal period, AR is expressed in mesenchymal and epithelial cells. Androgens inhibit the production of surfactants, which starts later in male than in female neonatal lungs (Carey et al., 2007), but also support the developing lung during branching morphogenesis (Kimura et al., 2003).
Lung intracrinology in lungs–systematic search
Adult human lungs express CYP19A1 and most 17βHSDs (1, 2, 4, 7, 8, 11, 12, 17βHSD5/AKR1C3; Table 8). STS, SULT and 17βHSD1, 12 and 17βHSD5/AKR1C3 immunoreactivity localizes in the bronchial epithelium (weak for types 1 and 12, strong for type 17βHSD5) and alveolar macrophages (Sakurai et al., 2006; Miller et al., 2012b; Chang et al., 2013; Konings et al., 2017).
Intracrinology controls lung development and maturation as shown in various animal models (Boucher et al., 2009) and intracrine enzymes are expressed already during fetal stages. Human fetal lungs possess StAR, CYP11A1, 3βHSD1 mRNA (Pezzi et al., 2003), SULT1E1 activity (Jones et al., 1992) and show 17βHSD1 and 2 mRNAs expression at 13 and 20 weeks of gestational age (Takeyama et al., 2000). High mRNA levels of AR, 17βHSD2 and 17βHSD5/AKR1C3 in mid-late gestation period and adult lungs indicate the present of androgen metabolism (Simard et al., 2010). Immunoreactivity for 17βHSD11 is detected in bronchioles of 14 and 31 weeks old fetuses, whereas other structures are negative (e.g., alveoli, ciliated epithelium, acini of the trachea). The expression of 17βHSD11 increases during the second half of pregnancy and maintains similar patterns in neonatal (14 days) and adult lugs (Brereton et al., 2001).
Intracrinology and lung diseases
Altered intracrinology is involved in lung disorders already from neonatal stages toward adulthood, and SNPs in intracrine genes are associated with the onset of diseases (Zhang et al., 2013). Higher concentration of estrogens were measured by LC-MS in women with multiple-synchronous-lung adenocarcinoma compared with single adenocarcinoma (Ikeda et al., 2016) and in neoplastic tissue compared with adjacent normal lungs (Niikawa et al., 2008; Verma et al., 2013). Type 1 17βHSD mRNA, protein and activity are present in various non-small-cell-lung-cancer (NSCLC) cell lines where the mitogenic effect of E1 is abrogated by 17βHSD1 knockdown (Drzewiecka and Jagodzinski, 2012; Verma et al., 2013). In specimens from 48 NSCLC patients, 17βHSD1 expression was associated with squamous cell carcinoma and stage 3A disease (Drzewiecka et al., 2015). In another study on 103 NSCLC specimens, high 17βHSD1 immunoreactivity was associated with low intratumoural E1 and high E2:E1 ratio, whereas higher 17βHSD2 immunoreactivity was associated with high intratumoural E1. Multivariate regression analysis also demonstrated that increased 17βHSD1 immunoreactivity in tumors was an independent negative prognostic factor (Verma et al., 2013).
CYP19A1 is expressed in lung cancer and has potential therapeutic value (Niikawa et al., 2008; Verma et al., 2011; Siegfried and Stabile, 2014). A recent IHC study on 335 NSCLC specimens found an inverse association between CYP19A1 expression with disease specific survival (Skjefstad et al., 2016). Similar data, although restricted to women only, were confirmed in an independent study on 150 primary lung adenocarcinoma specimens, where CYP19A1 was found as the main driver of local estrogen supply (Tanaka et al., 2016). Another study on 110 lung adenocarcinoma specimens found an association between CYP19A1 mRNA (RT-qPCR) and poor prognosis in females, never-smokers and harboring EGFR mutations (Kohno et al., 2014). However, a recent mRNA study on 96 NSCLC patients showed that CYP19A1 in combination with ER is a good prognostic marker (Aresti et al., 2014).
STS and SULT1E1 immunoreactivity is detected in the majority of NSCLC cases, and STS is a good prognostic marker (Iida et al., 2013).
Lymphangioleiomyomatosis (LAM) is a rare, potentially fatal disease affecting predominantly young women. It is strongly hormone sensitive and it is hypothesized to originate from the uterus as lung metastasis (Prizant and Hammes, 2016). The levels of ERs, PR, AR, CYP19A1, STS, 17βHSD1 and SRD5A2 were recently assessed among 30 LAM biopsies. CYP19A1 expression resulted a useful classification marker with implication for potential therapy (Adachi et al., 2015). A recent study on specimens from 73 patients with chronic obstructive pulmonary disease (COPD) and 48 controls described an association between both CYP19A1 and 17βHSD1 with COPD (Konings et al., 2017). CYP19A1 is also implicated in interstitial pneumonia interstitial pneumonia, where local E2 concentration and CYP19A1 activity and immunoreactivity were elevated in diseased compared with normal tissue (Taniuchi et al., 2014).
Potential novel treatments
Blocking the estrogen signaling showed promising preclinical results in animal models of lung cancer (Verma et al., 2011). In humans, antiestrogen treatments (ER antagonists, GnRH, oophorectomy, P) have been used in LAM (Taveira-DaSilva and Moss, 2014) and lung cancer patients (Verma et al., 2011; Kohno et al., 2014). A phase II study on advanced NSCLC patients non-responsive to platinum-based drugs tested the dual-regimen mTOR/CYP19A1 inhibitors. Unfortunately, this study was prematurely terminated due to high toxicity (Singhal et al., 2015) and one additional trial using ER antagonist plus AI (fulvestrant and anastrozole) as consolidation therapy in postmenopausal women with advanced NSCLC (NCT00932152) was terminated due to poor recruitment.
Better results were obtained using the AI letrozole as single agent or in combination with rapamycin in a phase II trial on 17 postmenopausal women with LAM (NCT01353209). AI treatment was safe and well tolerated also in the dual drug regimen (Lu et al., 2017).
Lungs: conclusions
Steroids are involved in lung maturation, development and in susceptibility to diseases. Most 17βHSDs, STS/SULT1E1, CYP19A1 are expressed indicating the lung's ability to metabolize androgens, estrogens and progestogens. Evidence of 3βHSDs is limited to fetal tissues (Table 8 and Figure 3). Approaches aimed at decreasing local estrogens may offer future novel treatments for various lung diseases.
Brain and central nervous system (CNS)
One of the first CNS actions of sex steroids to be described is the hypothalamus-pituitary-gonadal axes control (Andersen and Ezcurra, 2014). The identification of steroid-receptors outside the hypothalamus, like hippocampus (controlling memory), prefrontal cortex, cerebellum and dopaminergic system regulation indicated that sex steroids have complex and widespread effects in the CNS. They control aggressive behavior, cognitive functions, mood, food intake, appetite, addiction, blood pressure, fine motor skills, motor coordination, pain circuit and both estrogens and androgens are neuroprotective (López and Tena-Sempere, 2015; Soma et al., 2015; McEwen and Milner, 2017). Estrogen deprivation in animals and humans is associated with development of metabolic disorders and estrogen administration has a general catabolic effect (López and Tena-Sempere, 2015). Animal experiments and KO models show that ERα mediates the major actions of estrogens in the CNS, like the metabolic control functions (Musatov et al., 2007) and the negative-feedback on the hypothalamus-pituitary-gonadal axes (Couse et al., 2003). However, both nuclear and non-nuclear ERs are relevant in distinct CNS regions (Almey et al., 2015; López and Tena-Sempere, 2015; McEwen and Milner, 2017).
Local steroid synthesis in the CNS is demonstrated in animal studies. CYP19A1-KO mice have increased ischemic damages compared with ovariectomised wild-type mice, indicating a local action of CYP19A1 (McEwen and Milner, 2017). Similar conclusions were drawn for the estrogen protective effects on stroke, Alzheimer (AD), Parkinson diseases, aggressive behavior (Soma et al., 2015; McEwen and Milner, 2017) and mice with ablation in various 17βHSDs show neuronal defects (Table 4). In rodents, CNS regions like the hippocampus and the hypothalamus express the enzymes involved in the local generation of steroids, like StAR, CYP11A1, CYP17A1, 3βHSD1, CYP19A1, 17βHSD1, SRD5A1 and 2 (mRNA and protein by immunohistochemistry or western blot), and can produce pregnenolone, DHEA, androgens and estrogens from cholesterol, as confirmed by HPLC using radiolabelled substrates and tissue cultures of brain slices (Mukai et al., 2006; Murakami et al., 2006). CYP enzymes of rat hippocampus co-localize in pyramidal neurons (CA1–CA3 regions) and granule cells (dentate gyrus) (Mukai et al., 2006; Murakami et al., 2006). Regulation of intracrine enzymes varies during development and sexual maturation, as indicated by mRNA expression (RT-qPCR) of 20 intracrine enzymes analyzed in rat hippocampus post-natal and throughout early (1 week) development (Kimoto et al., 2010).
Intracrinology in the CNS is particularly relevant because, beside the traditional pathway via the receptors, several steroids have neuroactivity and are allosteric modulators of GABAA receptors (Figure 2). Such actions are possessed also by steroids that are unable to activate the steroid hormone receptors, such as 3β- and 3α-hydroxyl sulpho-conjugates (P5-S and DHEA-S), 5β-reduced steroids (5βAN, etiocholanolone and 5β-THP isomers; Table 1), which are all GABAA negative modulators (in contrast to unconjugated 3α-hydroxysteroids) (Stoffel-Wagner, 2001; Belelli and Lambert, 2005; Agís-Balboa et al., 2006; Gibbs et al., 2006; Reddy, 2010; Steckelbroeck et al., 2010).
Intracrinology in CNS–systematic search
Intracrine enzymes are widely expressed in human CNS (Table 8) and intratissue concentrations of steroids in distinct regions differ between regions and from the levels in the blood (Mukai et al., 2006; Murakami et al., 2006; Jäntti et al., 2010). In contrast to rodents, however, the presence of the complete steroid biosynthetic pathway is not clearly demonstrated in the human CNS and contrasting data were reported (Table 8). CYP11A1 mRNA was detected in the temporal, frontal neocortex and subcortical white matter of men, women and children (Stoffel-Wagner, 2001). Low mRNA levels of CYP17A1 were detected in the hippocampus, amygdala, caudate nucleus, cerebellum, corpus callosum, spinal cord and thalamus (Stoffel-Wagner, 2001; Yu et al., 2002), but other authors found no expression of this enzyme (Steckelbroeck et al., 2004b, 2010; MacKenzie et al., 2008). No 3βHSD1 or 2 was detected in temporal lobes, hippocampus, thalamus and amygdala (Stoffel-Wagner, 2001; Steckelbroeck et al., 2010), although other authors detected low levels in amygdala, caudate nucleus, cerebellum, corpus callosum, hippocampus, spinal cord and thalamus (Yu et al., 2002).
The temporal lobes (both neocortex and white matter) have 17βHSD oxidative and reductive activities, CYP19A1 mRNA expression and activity, which is also present in hippocampus (Stoffel-Wagner et al., 1999a; Stoffel-Wagner, 2001). Temporal lobe specimens from 10 men to 12 women indicated that 17βHSD estrogen-oxidative and DHEA-reductive metabolisms are predominant, thus producing E1 and A5, respectively (Stoffel-Wagner, 2001). Regarding the different 17βHSDs, type 1, 3, and 4 mRNAs (but not type 2) were demonstrated by competitive reverse transcription-PCR in specimens from 34 women, 32 men and 10 children (Casey et al., 1994; Beyenburg et al., 2000). Subsequent studies confirmed the expression of types 4, 7, 8, 10, 11 17βHSD and AKR1C3/17βHSD5 in temporal lobes and hippocampus (Stoffel-Wagner, 2001; Steckelbroeck et al., 2003). In particular 17βHSD10 is involved in the deactivation of THP to 5αDHP, and it is an important regulator of neurological functions (Yang et al., 2016).
Production of 5α-androstane and pregnane neurosteroids is mediated by the action of SRD5As and AKR1Cs (Figure 2). SRD5A1 (not type 2) mRNA and enzyme activity were demonstrated in temporal neocortex and subcortical white matter, hippocampus, cerebellum, hypothalamus (Steckelbroeck et al., 2001; Stoffel-Wagner, 2001), and AKR1C4 mRNA was detected in both hippocampus and temporal lobe (Stoffel-Wagner, 2001). AKR1C1 and AKR1C2 are widely expressed in CNS and since no specific inhibitors directed against AKR1C1 to 4 could completely inhibit AKR1C brain activity, the involvement of an unidentified enzyme is suggested (Steckelbroeck et al., 2010). Isomeric 5β-neurosteroids require the action of AKR1D1, and it is unknown whether AKR1D1 is expressed in CNS, or liver 5β-steroids reach peripheral regions via the circulation (Jin et al., 2011).
The sulphatase pathway in the CNS is relevant because (although recent studies are revisiting this paradigm; Qaiser et al., 2017), sulphated-steroids do not cross the blood-brain barrier. Therefore, sulphated neurosteroids like DHEA-S and P5-S need to be generated locally, and in line with this, their level in the CNS is independent from the level in the blood (Rajkowski et al., 1997) and varies throughout distinct brain regions (especially hippocampus and hypothalamus) (Jäntti et al., 2010).
STS and SULTs are widely expressed, with no gender-related differences (Table 8) (Kríz et al., 2008a,b; Mueller et al., 2015). SULT1A1 has high expression especially in specimens isolated from cerebellum, occipital and frontal lobes (Salman et al., 2009). No brain region expresses SULT2A1, whereas contrasting data exist for SULT2B1 and SULT1E1 (Table 8).
Diseases and treatments
Steroid metabolism is deviated in schizophrenia (Bicikova et al., 2013) and aberrations and unbalances of intracrine enzymes are associated with neurological disorders (Luchetti et al., 2011 and see Table 5). In a study of 49 patients with AD, prefrontal cortex mRNA levels of 17βHSD1, CYP19A1 and AKR1C2 increased at late stages (Luchetti et al., 2011). STS and SULT activities, measured by radioimmunoassay and GC-MS in 55 human brain tumor specimens, varied between tumor types (Kríz et al., 2008b). Immunoreactivity for AKR1C3/17βHSD5 was low in medulloblastomas (n = 10 analyzed), high in 37 glial neoplasms and 18 meningiomas and was absent in intracranial schwannoma (n = 7) (Park et al., 2010). A recent screening of a chemical library of steroid inhibitors using three low grade pediatric glioma cell lines found that inhibition of 17βHSD3 blocked cell growth and induced apoptosis in vitro (Ajeawung et al., 2013)
Type 10 17βHSD is associated with AD and is a potential target in diseases like AD, Parkinson, and an X-linked mental retardation, that may arise from the impaired degradation of branched chain fatty acid, isoleucine or aberrant neurosteroid (THP) metabolism (Lim et al., 2011; Yang et al., 2016).
STS has been implicated in ADHD and a recent mouse study indicates that genetic and pharmacological manipulations of the STS axis influence the inhibitory processes and give rise to improvements in response control (Davies et al., 2014). A recent animal experiment using a model of autoimmune encephalomyelitis showed high SULT1A1 mRNA expression in laser-captured-micro-dissected white matter astrocytes, suggesting that deactivation of estrogens (and other phenolic substrates) may be responsible for the resistance to anti-neuro-inflammatory treatments in these cells and could be possibly used as new treatments to protect CNS from inflammatory injuries (Guillot et al., 2015).
CNS: conclusions
CNS can synthesize steroids from cholesterol, although this is restricted to few brain regions. Steroid metabolism in the CNS is particular complex due to the formation of both 5α-/β-reduced and sulpho-conjugated neurosteroids (Table 8 and Figure 3).
Intracrinology in other tissues and systems
Steroid metabolism is also important in the immune system, skin and adipose tissue. A thorough review of these systems is outside the scope of this study, however, a brief mention is given below.
Immune system and inflammation
Beside corticosteroids, several other steroids affect the immune system and inflammation. A5 induces white blood cells and platelets production in bone marrow (Chen et al., 2004); estrogens and androgens control B-lymphocyte development in a sex-dependent way and modulate autoimmune diseases (McCarthy, 2000; Calippe et al., 2010; Sakiani et al., 2013).
Lipopolysaccharide-mediated proinflammatory pathway in macrophages and NF-κB activation are blocked by estrogens, which induce T-helper (Th) type 2 responses, whereas androgens stimulate type 1 responses (Iwasa et al., 2015). DHEA and DHEA-S also regulate the maturation of Th1 or Th2 cells. It was shown that plasma Th2 lymphocytes and its major secreted cytokine IL6 increase with age, and this is reversed in mice upon administration of DHEA or DHEA-S (Reed et al., 2005). Such effect was recapitulated in vitro by DHEA but not DHEA-S implicating the involvement of macrophage STS in lymphoid tissues where Th cell maturation occurs. In line with this, the effect of DHEA-S, but not DHEA, was impaired in vivo by an STS inhibitor (Reed et al., 2005). These data prompted to propose STS inhibition as a therapeutic approach for diseases associated with inappropriate immune responses and excess Th1 cytokines such as rheumatoid arthritis (Reed et al., 2005). Whether the action of DHEA is secondary to its conversion to androgens or estrogens is currently unclear. STS activity of peripheral blood leukocytes is higher in women during the follicular phase of the menstrual cycle than in women in the luteal phase or in men and it becomes highest during pregnancy, suggesting a role for P in regulating STS activity (Reed et al., 2005; Mueller et al., 2015). In vitro studies also demonstrated that STS activity is induced by cytokines such as IL6 and TNF (Mueller et al., 2015).
Opposite deregulation of the sulphatase pathway is seen in other chronic inflammatory diseases/cell types. Vascular smooth muscle cells show higher STS activity in women with mild atherosclerosis compared with women with severe disease (and male), whereas SULT1E1 activity is lower in women with severe disease (Mueller et al., 2015).
CYP19A1 is also expressed in macrophages (Konings et al., 2017) and KO mice have increased numbers of peripheral blood and bone marrow cells and inflammatory renal lesions (Shim et al., 2004). CYP19A1 inhibitors exacerbate the autoimmune lesions in a murine model of Sjögren syndrome and estrogen administration reverses such phenotype (Iwasa et al., 2015; Park et al., 2015). Opposite effects are observed in prostate, where elevated intracrine estrogens due to CYP19A1 overexpression induce inflammation and pre-malignant pathology (Ellem et al., 2009) as well as in adipose tissue (Reed et al., 2005).
Skin
The skin is the largest human organ and first barrier against pathogens where important immune functions interconnected with intracrine steroid metabolism take place (Slominski et al., 2013). Keratinocytes and sebocytes express ERs, intracrine enzymes, and the activity of sebaceous glands is influenced by steroids as indicated by the sebum production at andrenarche (Slominski et al., 2013). CYP17A1, CYP19A1, 17βHSD1, 2, 3, 4 (and enzymes metabolizing corticosteroid - outside the scope of this review) are detected in human skin. Some genes are under the influence of vitamin D and sebocytes can synthesize T from adrenal precursors (Hughes et al., 1997; Thiboutot et al., 1998; Slominski et al., 2013). Low 17βHSD oxidative metabolism characterizes sebaceous glands from skin areas prone to develop acne compared with other locations, suggesting a protective role of the oxidative metabolism against androgen excess (Fritsch et al., 2001). Sulphatase pathway is present in the skin (Reed et al., 2005; Simard et al., 2005), and genetic variants in STS and SULTs are associated with skin disturbances, most likely because of unbalanced steroid accumulation (Table 5).
Adipose tissue
The adipose tissue is one of the most complex endocrine organs that besides secreting leptin and adiponectin, is a site of steroid metabolism, it establishes interaction with the CNS for glucose and lipid metabolism control, energy homeostasis and inflammation. The implication of sex steroids in adipose tissue is demonstrated by the different fat distribution that characterizes men and women (Mauvais-Jarvis et al., 2013; Varlamov et al., 2014; López and Tena-Sempere, 2015, 2016; Palmer and Clegg, 2015). ER-KO and CYP19A1-KO mice develop obesity with human-like phenotypes (López and Tena-Sempere, 2015). Estrogens protect against metabolic syndrome and men lacking endogenous estrogens (CYP19A1 or ER-α deficiency) develop hypertriglyceridemia, glucose intolerance and insulin resistance (Kim et al., 2014). In adipose tissue of men, 17βHSD2 levels and androgen inactivation correlate with BMI (Fouad Mansour et al., 2015). A mouse study also showed that increased unsulphated-estrogen availability due to loss of SULT1E1 improved metabolic function in a model of type 2 diabetes, which leads to speculations about a potential role of SULT1E1 inhibition for this disease - at least in women (Gao et al., 2012).
Fat consists of different tissue types (white and brown) and different regional depots with distinct physiological, intracrinological characteristics and distinct relations with pathologies and metabolic disorders (Blouin et al., 2009; Mauvais-Jarvis et al., 2013). White adipose tissue is mainly subcutaneous (abdomen) or visceral (surrounding the inner organs), this last being associated with metabolic risks. A plethora of investigations demonstrated the ability of adipose tissue to aromatise androgens into estrogens and that the intra-tissue steroid levels are higher than the levels in blood (Bélanger et al., 2002). Androgenic and estrogenic 17βHSD activity and the mRNA for 17βHSD1, 2, 3, 7, 12, AKR1C3/17βHSD5 were detected in both intra-abdominal and subcutaneous fat (Bélanger et al., 2002; Quinkler et al., 2004; Bellemare et al., 2009; Wang et al., 2013).
Both subcutaneous and visceral fat tissue of women expresses the androgenic 17βHSD3 (generally considered testis specific) indicating that adipose tissue in women is substantially androgenic. Such characteristic in the visceral depot increased with increasing BMI, suggesting a link between central obesity and metabolic diseases (Corbould et al., 2002).
Additionally, several enzymes (AKR1C2, AKR1C3/17βHSD5, CYP19A1, STS and SULT1E1) vary throughout adipocyte differentiation and maturation (Quinkler et al., 2004; Bellemare et al., 2009; Blouin et al., 2009; Mueller et al., 2015).
Conclusions and recommendations
Intracrinology consists of a complex and intricate network of alternative and redundant pathways that generate, deactivate steroids in peripheral tissues and ultimately control steroid exposure in a tissue specific manner. A number of compounds have that ability to bind and activate more than one nuclear receptors thus exerting multiple biological actions. Blood steroids represent a reservoir of substrates that support these intracrine networks. Studies retrieved by the systematic search demonstrated that most investigations rely on RT-PCR or IHC to detect enzyme and protein, and frequently without multiple-technique confirmation of the data. Since both techniques present limitations, and antibodies for IHC often perform sub-optimally (detection limit is not sufficient to detect some intracrine enzymes, crossreactivity between isoforms) these techniques are not always suitable to infer the real biological role of a reaction/enzyme.
However, the recent technological advances in steroid profiling together with an improved knowledge of intracrine enzymes and the possibility to validate data using multiple approaches (RNA, protein, activity, steroid profiling) create today unprecedented opportunities to expand our understanding of intracrinology, its relation with endocrinology and to exploit this knowledge in patient care. Improved multiplex platforms allowing to profile in peripheral tissues all steroids depicted in Figure 2 are awaited and will elucidate the relevant tissue-specific networks. It is envisaged that novel prognostic markers and drug targets will become of clinical relevance soon.
We should however be aware that the redundant actions of intracrine enzymes, their substrate promiscuity, the existence of alternative pathways and the patient-to-patient variability might result in drug insensitivity. Dual/triple inhibitors will help solving this problem. In addition, in order to optimize research on novel drugs, the classical preclinical drug discovery pipelines (safety, pharmacokinetics and dynamics), should encompass parallel research lines to learn how to pre-select potentially responsive patients.
Finally, since we know that steroidal and intracrine drugs might have profound effects on the CNS, it is desirable to have in depth research on the neurological effects of potential novel drugs during the nonclinical phase of drug development. This will facilitate to select suitable compounds to the clinical development.
Author contributions
GK drafted the study, prepared figures, tables, intermediate versions, final version and approved final version. LB drafted part of the study, contributed to intermediate versions and approved final version. KC drafted part of the study, contributed to intermediate versions and approved final version. BD contributed to intermediate versions and approved final version. TL drafted part of the study, contributed to intermediate versions and approved final version. PK contributed to intermediate versions and approved final version. MB contributed to intermediate versions and approved final version. RK contributed to intermediate versions and approved final version. SX drafted part of the study, contributed to intermediate versions and approved final version. AR drafted the study, prepared figures, tables, intermediate versions, final version and approved final version.
Conflict of interest statement
PK and TL are employees of Forendo Pharma Ltd. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We are grateful to Dr. Margaretha A Skowron (Department of Urology, University Düsseldorf, Germany) for graphic arts.
We also would like to thank the management and curator of the online databases we made use of, namely: the database of chemical molecules PubChem (www.ncbi.nlm.nih.gov; pubchem.ncbi.nlm.nih.gov) maintained by the National Center for Biotechnology Information (NCBI; National Library of Medicine/United States National Institutes of Health - NIH); Chemical Abstracts Service (CAS), maintained by the American Chemical Society (www.cas.org); Human Metabolome Data Base (HMDB, www.hmdb.ca), funded and maintained by Genome Canada; Chemical Book (www.chemicalbook.com), funded by industrial partners; Chemical Entities of Biological Interest (ChEBI; www.ebi.ac.uk/chebi/init.do), curated by the European Bioinformatics Institute of the European Molecular Biology Laboratory (EMBL); drug and drug target database Drugbank (www.drugbank.ca/drugs), University of Alberta and The Metabolomics Innovation Centre; GeneCards (www.genecards.org), developed and maintained by the Crown Human Genome Center at the Weizmann Institute of Science; Online Mendelian Inheritance in Man® (OMIM®, https://omim.org/), McKusick-Nathans Institute of Genetic Medicine, Johns Hopkins University (Baltimore, MD); Mouse Genome Informatics (MGI; www.informatics.jax.org), Mouse Genome Database at the Mouse Genome Informatics website, The Jackson Laboratory, Bar Harbor, Maine.
Glossary
Abbreviations
- [3H]
tritiated hydrogen
- [14C]
radioactive carbon
- AD
Alzheimer disease
- ADHD
attention deficit hyperactivity disorder
- AI
aromatase inhibitor
- AKR
aldo-ketoreductase
- AR
androgen-receptor
- ART
assisted reproduction technology
- BMD
bone mineral density
- BMP-2
bone morphogenetic protein 2
- COPD
chronic obstructive pulmonary disease
- COUP-TFII
chicken-ovalbumin-upstream-promoter-transcription-factor II
- CNS
central nervous system
- CRC
colorectal cancer
- CX43
connexin 43
- DS
digestive system
- Ed
embryonic day
- EC
endometrial cancer
- EndRet
endoplasmic reticulum
- ER
estrogen-receptor
- Fdx
ferredoxin
- FdR
ferredoxin reductase
- GC-MS
gas-chromatography tandem mass-spectrometry
- GnRH
gonadotropin releasing hormone
- GH
growth hormone
- GIT
gastrointestinal tract
- GPER
G protein-coupled estrogen-receptor
- HPLC
high performance liquid-chromatography
- HRT
hormone-replacement-therapy
- hCG
human chorionic gonadotropin
- IGF1
insulin-like growth factor 1
- IHC
immunohistochemistry
- IL-1
interleukin-1
- IL-6
interleukin-6
- KO
knock-out
- LC-MS
liquid-chromatography tandem mass-spectrometry
- mTOR
mammalian target of rapamycin
- NAPDH
nicotine-adenine-dinucleotide-phosphate
- NSCLC
non-small cell lung cancer
- PAIN
phenomena of pan-assay interfering compounds
- PAP
bis-phospho-nucleotide-3′-phospho-adenosine-5′-phosphate
- PCOC
poly cystic ovarian syndrome
- POR
P450 oxidoreductase
- RT-qPCR
reverse-transcriptase quantitative polymerase-chain-reaction
- SF1
steroidogenic factor 1
- SHBG
sex hormone binding globulin
- SNP
single nucleotide polymorphism
- SRD
short-chain dehydrogenase
- Th
T-helper
- TNF
tumor necrosis factor
- VEGF
vascular endothelial growth factor
- WB
western blot/blotting
- WOI
window of implantation.
Footnotes
Funding. The present study was sponsored by the Dutch Cancer Society (KWF Kankerbestrijding: www.kwf.nl), contract number UM-13-5782 granted to AR.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2018.00940/full#supplementary-material
References
- Abdelsamie A. S., van Koppen C. J., Bey E., Salah M., Börger C., Siebenbürger L., et al. (2017). 17β-HSD1 inhibitor with sub-nanomolar IC50 for a proof-of-principle study. Eur. J. Med. Chem. 127, 944–957. 10.1016/j.ejmech.2016.11.004 [DOI] [PubMed] [Google Scholar]
- Acién P., Velasco I., Gutiérrez M., Martínez-Beltrán M. (2007). Aromatase expression in endometriotic tissues and its relationship to clinical and analytical findings. Fertil. Steril. 88, 32–38. 10.1016/j.fertnstert.2006.11.188 [DOI] [PubMed] [Google Scholar]
- Adachi K., Miki Y., Saito R., Hata S., Yamauchi M., Mikami Y., et al. (2015). Intracrine steroid production and mammalian target of rapamycin pathways in pulmonary lymphangioleiomyomatosis. Hum. Pathol. 46, 1685–1693. 10.1016/j.humpath.2015.02.019 [DOI] [PubMed] [Google Scholar]
- Adessi G. L., Prost O., Agnani G., Petitjean A., Burnod J. (1984). Estrone sulfatase activity in normal and abnormal endometrium. Arch. Gynecol. 236, 13–18. 10.1007/BF02114864 [DOI] [PubMed] [Google Scholar]
- Adjei A. A., Thomae B. A., Prondzinski J. L., Eckloff B. W., Wieben E. D., Weinshilboum R. M. (2003). Human estrogen sulfotransferase (SULT1E1) pharmacogenomics: Gene resequencing and functional genomics. Br. J. Pharmacol. 139, 1373–1382. 10.1038/sj.bjp.0705369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aghajanova L., Hamilton A., Kwintkiewicz J., Vo K. C., Giudice L. C. (2009). Steroidogenic enzyme and key decidualization marker dysregulation in endometrial stromal cells from women with versus without endometriosis. Biol. Reprod. 80, 105–114. 10.1095/biolreprod.108.070300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agís-Balboa R. C., Pinna G., Zhubi A., Maloku E., Veldic M., Costa E., et al. (2006). Characterization of brain neurons that express enzymes mediating neurosteroid biosynthesis. Proc. Natl. Acad. Sci. U.S.A. 103, 14602–14607. 10.1073/pnas.0606544103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajeawung N. F., Maltais R., Jones C., Poirier D., Kamnasaran D. (2013). Viability screen on pediatric low grade glioma cell lines unveils a novel anti-cancer drug of the steroid biosynthesis inhibitor family. Cancer Lett. 330, 96–105. 10.1016/j.canlet.2012.11.034 [DOI] [PubMed] [Google Scholar]
- Almey A., Milner T. A., Brake W. G. (2015). Estrogen receptors in the central nervous system and their implication for dopamine-dependent cognition in females. Horm. Behav. 74, 125–138. 10.1016/j.yhbeh.2015.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshogran O. Y. (2017). Pharmacogenetics of aldo-keto reductase 1C (AKR1C) enzymes. Expert Opin. Drug Metab. Toxicol. 13, 1063–1073. 10.1080/17425255.2017.1376648 [DOI] [PubMed] [Google Scholar]
- Amant F., Moerman P., Neven P., Timmerman D., Van Limbergen E., Vergote I. (2005). Endometrial cancer. Lancet 366, 491–505. 10.1016/S0140-6736(05)67063-8 [DOI] [PubMed] [Google Scholar]
- Amos-Landgraf J. M., Heijmans J., Wielenga M. C., Dunkin E., Krentz K. J., Clipson L., et al. (2014). Sex disparity in colonic adenomagenesis involves promotion by male hormones, not protection by female hormones. Proc. Natl. Acad. Sci. U.S.A. 111, 16514–16519. 10.1073/pnas.1323064111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen C. Y., Ezcurra D. (2014). Human steroidogenesis: implications for controlled ovarian stimulation with exogenous gonadotropins. Reprod. Biol. Endocrinol. 12:128. 10.1186/1477-7827-12-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrew A. S., Hu T., Gu J., Gui J., Ye Y., Marsit C. J., et al. (2012). HSD3B and gene-gene interactions in a pathway-based analysis of genetic susceptibility to bladder cancer. PLoS ONE 7:e51301. 10.1371/journal.pone.0051301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aresti U., Carrera S., Iruarrizaga E., Fuente N., Marrodan I., de Lobera A. R., et al. (2014). Estrogen receptor 1 gene expression and its combination with estrogen receptor 2 or aromatase expression predicts survival in non-small cell lung cancer. PLoS ONE 9:e109659 10.1371/journal.pone.0109659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold C., Einspanier A. (2013). Medical treatment improves social behavior in a primate endometriosis model (Callithrix jacchus). J. Med. Primatol. 42, 112–119. 10.1111/jmp.12042 [DOI] [PubMed] [Google Scholar]
- Ashton K. A., Proietto A., Otton G., Symonds I., McEvoy M., Attia J., et al. (2010). Polymorphisms in genes of the steroid hormone biosynthesis and metabolism pathways and endometrial cancer risk. Cancer Epidemiol. 34, 328–337. 10.1016/j.canep.2010.03.005 [DOI] [PubMed] [Google Scholar]
- Attar E., Tokunaga H., Imir G., Yilmaz M. B., Redwine D., Putman M., et al. (2009). Prostaglandin E2 via steroidogenic factor-1 coordinately regulates transcription of steroidogenic genes necessary for estrogen synthesis in endometriosis. J. Clin. Endocrinol. Metab. 94, 623–631. 10.1210/jc.2008-1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audet-Walsh É., Bellemare J., Lacombe L., Fradet Y., Fradet V., Douville P., et al. (2012). The impact of germline genetic variations in hydroxysteroid (17-beta) dehydrogenases on prostate cancer outcomes after prostatectomy. Eur. Urol. 62, 88–96. 10.1016/j.eururo.2011.12.021 [DOI] [PubMed] [Google Scholar]
- Audet-Walsh E., Lepine J., Gregoire J., Plante M., Caron P., Tetu B., et al. (2011). Profiling of endogenous estrogens, their precursors, and metabolites in endometrial cancer patients: association with risk and relationship to clinical characteristics. J. Clin. Endocrinol. Metab. 96, E330–E339. 10.1210/jc.2010-2050 [DOI] [PubMed] [Google Scholar]
- Aumüller G., Eicheler W., Renneberg H., Adermann K., Vilja P., Forssmann W. G. (1996). Immunocytochemical evidence for differential subcellular localization of 5 alpha-reductase isoenzymes in human tissues. Acta Anat. (Basel). 156, 241–252. 10.1159/000147852 [DOI] [PubMed] [Google Scholar]
- Bacallao K., Leon L., Gabler F., Soto E., Romero C., Valladares L., et al. (2008). In situ estrogen metabolism in proliferative endometria from untreated women with polycystic ovarian syndrome with and without endometrial hyperplasia. J. Steroid Biochem. Mol. Biol. 110, 163–169. 10.1016/j.jsbmb.2008.03.031 [DOI] [PubMed] [Google Scholar]
- Baes M., Huyghe S., Carmeliet P., Declercq P. E., Collen D., Mannaerts G. P., et al. (2000). Inactivation of the peroxisomal multifunctional protein-2 in mice impedes the degradation of not only 2-methyl-branched fatty acids and bile acid intermediates but also of very long chain fatty acids. J. Biol. Chem. 275, 16329–16336. 10.1074/jbc.M001994200 [DOI] [PubMed] [Google Scholar]
- Bagi C. M., Wood J., Wilkie D., Dixon B. (2008). Effect of 17β-hydroxysteroid dehydrogenase type 2 inhibitor on bone strength in ovariectomized cynomolgus monkeys. J. Musculoskelet. Neuronal Interact. 8, 267–280. [PubMed] [Google Scholar]
- Bair S. R., Mellon S. H. (2004). Deletion of the mouse P450c17 gene causes early embryonic lethality. Mol. Cell. Biol. 24, 5383–5390. 10.1128/MCB.24.12.5383-5390.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balk S. P., Knudsen K. E. (2008). AR, the cell cycle, and prostate cancer. Nucl. Recept. Signal. 6:e001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barzi A., Lenz A. M., Labonte M. J., Lenz H. J. (2013). Molecular pathways: estrogen pathway in colorectal cancer. Clin. Cancer Res. 19, 5842–5848. 10.1158/1078-0432.CCR-13-0325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bélanger C., Luu-The V., Dupont P., Tchernof A. (2002). Adipose tissue intracrinology: potential importance of local androgen/estrogen metabolism in the regulation of adiposity. Horm. Metab. Res. 34, 737–745. 10.1055/s-2002-38265 [DOI] [PubMed] [Google Scholar]
- Belelli D., Lambert J. J. (2005). Neurosteroids: endogenous regulators of the GABA(A) receptor. Nat. Rev. Neurosci. 6, 565–575. 10.1038/nrn1703 [DOI] [PubMed] [Google Scholar]
- Bellemare V., Faucher F., Breton R., Luu-The V. (2005). Characterization of 17α-hydroxysteroid dehydrogenase activity (17α-HSD) and its involvement in the biosynthesis of epitestosterone. BMC Biochem. 6:12. 10.1186/1471-2091-6-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellemare V., Laberge P., Noel S., Tchernof A., Luu-The V. (2009). Differential estrogenic 17β-hydroxysteroid dehydrogenase activity and type 12, 17β-hydroxysteroid dehydrogenase expression levels in preadipocytes and differentiated adipocytes. J. Steroid Biochem. Mol. Biol. 114, 129–134. 10.1016/j.jsbmb.2009.01.002 [DOI] [PubMed] [Google Scholar]
- Berstein L., Zimarina T., Imyanitov E., Kovalevskij A., Maximov S., Pujol P., et al. (2006). Hormonal imbalance in two types of endometrial cancer and genetic polymorphism of steroidogenic enzymes. Maturitas 54, 352–355. 10.1016/j.maturitas.2006.04.017 [DOI] [PubMed] [Google Scholar]
- Beyenburg S., Stoffel-Wagner B., Watzka M., Blumcke I., Bauer J., Schramm J., et al. (1999). Expression of cytochrome P450scc mRNA in the hippocampus of patients with temporal lobe epilepsy. Neuroreport 10, 3067–3070. 10.1097/00001756-199909290-00035 [DOI] [PubMed] [Google Scholar]
- Beyenburg S., Watzka M., Blumcke I., Schramm J., Bidlingmaier F., Elger C. E., et al. (2000). Expression of mRNAs encoding for 17β-hydroxisteroid dehydrogenase isozymes 1, 2, 3 and 4 in epileptic human hippocampus. Epilepsy Res. 41, 83–91. 10.1016/S0920-1211(00)00130-3 [DOI] [PubMed] [Google Scholar]
- Bicikova M., Hill M., Ripova D., Mohr P., Hampl R. (2013). Determination of steroid metabolome as a possible tool for laboratory diagnosis of schizophrenia. J. Steroid Biochem. Mol. Biol. 133, 77–83. 10.1016/j.jsbmb.2012.08.009 [DOI] [PubMed] [Google Scholar]
- Bilezikian J. P., Morishima A., Bell J., Grumbach M. M. (1998). Increased bone mass as a result of estrogen therapy in a man with aromatase deficiency. N. Engl. J. Med. 339, 599–603. 10.1056/NEJM199808273390905 [DOI] [PubMed] [Google Scholar]
- Blake J. A., Eppig J. T., Kadin J. A., Richardson J. E., Smith C. L., Bult C. J., et al. (2017). Mouse Genome Database (MGD)-2017: community knowledge resource for the laboratory mouse. Nucleic Acids Res. 45, D723–D729. 10.1093/nar/gkw1040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blouin K., Nadeau M., Mailloux J., Daris M., Lebel S., Luu-The V., et al. (2009). Pathways of adipose tissue androgen metabolism in women: depot differences and modulation by adipogenesis. Am. J. Physiol. Endocrinol. Metab. 296, E244–E255. 10.1152/ajpendo.00039.2008 [DOI] [PubMed] [Google Scholar]
- Bothe U., Busemann M., Steinmeyer A., Droescher P., Fischer O. M., Peters M., et al. (2017). First time disclosure of BAY 1128688: a novel AKR1C3 inhibitor for the treatment of endometriosis, in 254th ACS National Meeting & Exposition (Washington, DC: ). [Google Scholar]
- Boucher E., Provost P. R., Plante J., Tremblay Y. (2009). Androgen receptor and 17β-HSD type 2 regulation in neonatal mouse lung development. Mol. Cell. Endocrinol. 311, 109–119. 10.1016/j.mce.2009.06.012 [DOI] [PubMed] [Google Scholar]
- Bovée J. V., Cleton-Jansen A. M., Taminiau A. H., Hogendoorn P. C. (2005). Emerging pathways in the development of chondrosarcoma of bone and implications for targeted treatment. Lancet Oncol. 6, 599–607. 10.1016/S1470-2045(05)70282-5 [DOI] [PubMed] [Google Scholar]
- Brereton P., Suzuki T., Sasano H., Li K., Duarte C., Obeyesekere V., et al. (2001). Pan1b (17βHSD11)-enzymatic activity and distribution in the lung. Mol. Cell. Endocrinol. 171, 111–117. 10.1016/S0303-7207(00)00417-2 [DOI] [PubMed] [Google Scholar]
- Brosens J., Verhoeven H., Campo R., Gianaroli L., Gordts S., Hazekamp J., et al. (2004). High endometrial aromatase P450 mRNA expression is associated with poor IVF outcome. Hum. Reprod. 19, 352–356. 10.1093/humrep/deh075 [DOI] [PubMed] [Google Scholar]
- BroŽic P., Turk S., Rizner T. L., Gobec S. (2011). Inhibitors of aldo-keto reductases AKR1C1-AKR1C4. Curr. Med. Chem. 18, 2554–2565. 10.2174/092986711795933713 [DOI] [PubMed] [Google Scholar]
- Bukulmez O., Hardy D. B., Carr B. R., Auchus R. J., Toloubeydokhti T., Word R. A., et al. (2008a). Androstenedione up-regulation of endometrial aromatase expression via local conversion to estrogen: potential relevance to the pathogenesis of endometriosis. J. Clin. Endocrinol. Metab. 93, 3471–3477. 10.1210/jc.2008-0248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukulmez O., Hardy D. B., Carr B. R., Word R. A., Mendelson C. R. (2008b). Inflammatory status influences aromatase and steroid receptor expression in endometriosis. Endocrinology 149, 1190–1204. 10.1210/en.2007-0665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulun S. E., Economos K., Miller D., Simpson E. R. (1994). CYP19 (aromatase cytochrome P450) gene expression in human malignant endometrial tumors. J. Clin. Endocrinol. Metab. 79, 1831–1834. [DOI] [PubMed] [Google Scholar]
- Bulun S. E., Mahendroo M. S., Simpson E. R. (1993). Polymerase chain reaction amplification fails to detect aromatase cytochrome P450 transcripts in normal human endometrium or decidua. J. Clin. Endocrinol. Metab. 76, 1458–1463. [DOI] [PubMed] [Google Scholar]
- Caiazza F., Ryan E. J., Doherty G., Winter D. C., Sheahan K. (2015). Estrogen receptors and their implications in colorectal carcinogenesis. Front. Oncol. 5:19. 10.3389/fonc.2015.00019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calippe B., Douin-Echinard V., Delpy L., Laffargue M., Lelu K., Krust A., et al. (2010). 17β-estradiol promotes TLR4-triggered proinflammatory mediator production through direct estrogen receptor alpha signaling in macrophages in vivo. J. Immunol. 185, 1169–1176. 10.4049/jimmunol.0902383 [DOI] [PubMed] [Google Scholar]
- Carani C., Qin K., Simoni M., Faustini-Fustini M., Serpente S., Boyd J., et al. (1997). Effect of testosterone and estradiol in a man with aromatase deficiency. N. Engl. J. Med. 337, 91–95. 10.1056/NEJM199707103370204 [DOI] [PubMed] [Google Scholar]
- Carey M. A., Card J. W., Voltz J. W., Arbes S. J., Jr., Germolec D. R., Korach K. S., et al. (2007). It's all about sex: gender, lung development and lung disease. Trends Endocrinol. Metab. 18, 308–313. 10.1016/j.tem.2007.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carneiro M. M., Morsch D. M., Camargos A. F., Reis F. M., Spritzer P. M. (2008). Androgen receptor and 5α-reductase are expressed in pelvic endometriosis. BJOG 115, 113–117. 10.1111/j.1471-0528.2007.01521.x [DOI] [PubMed] [Google Scholar]
- Carneiro M. M., Morsch D. M., Camargos A. F., Spritzer P. M., Reis F. M. (2007). Expression of 17β-hydroxysteroid dehydrogenase type 2 in pelvic endometriosis. Gynecol. Endocrinol. 23, 188–192. 10.1080/09513590701200850 [DOI] [PubMed] [Google Scholar]
- Caron K. M., Soo S. C., Wetsel W. C., Stocco D. M., Clark B. J., Parker K. L. (1997). Targeted disruption of the mouse gene encoding steroidogenic acute regulatory protein provides insights into congenital lipoid adrenal hyperplasia. Proc. Natl. Acad. Sci. U.S.A. 94, 11540–11545. 10.1073/pnas.94.21.11540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey M. L., MacDonald P. C., Andersson S. (1994). 17 beta-Hydroxysteroid dehydrogenase type 2: chromosomal assignment and progestin regulation of gene expression in human endometrium. J. Clin. Invest. 94, 2135–2141. 10.1172/JCI117569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chai Z., Brereton P., Suzuki T., Sasano H., Obeyesekere V., Escher G., et al. (2003). 17β-hydroxysteroid dehydrogenase type XI localizes to human steroidogenic cells. Endocrinology 144, 2084–2091. 10.1210/en.2002-221030 [DOI] [PubMed] [Google Scholar]
- Chang T. S., Lin H. K., Rogers K. A., Brame L. S., Yeh M. M., Yang Q., et al. (2013). Expression of aldo-keto reductase family 1 member C3 (AKR1C3) in neuroendocrine tumors & adenocarcinomas of pancreas, gastrointestinal tract, and lung. Int. J. Clin. Exp. Pathol. 6, 2419–2429. [PMC free article] [PubMed] [Google Scholar]
- Chen F., Knecht K., Leu C., Rutledge S. J., Scafonas A., Gambone C., et al. (2004). Partial agonist/antagonist properties of androstenedione and 4-androsten-3β,17β-diol. J. Steroid Biochem. Mol. Biol. 91, 247–257. 10.1016/j.jsbmb.2004.04.009 [DOI] [PubMed] [Google Scholar]
- Chen G., Zhang D., Jing N., Yin S., Falany C. N., Radominska-Pandya A. (2003). Human gastrointestinal sulfotransferases: identification and distribution. Toxicol. Appl. Pharmacol. 187, 186–197. 10.1016/S0041-008X(02)00073-X [DOI] [PubMed] [Google Scholar]
- Cho L. Y., Yang J. J., Ko K. P., Ma S. H., Shin A., Choi B. Y., et al. (2012). Genetic susceptibility factors on genes involved in the steroid hormone biosynthesis pathway and progesterone receptor for gastric cancer risk. PLoS ONE 7:e47603. 10.1371/journal.pone.0047603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciuffi M., Savino L., Santini D., Buzzoni P., Scarselli G., Mazzei T. (1982). Estradiol and progestin receptors, 17-beta-hydroxysteroid-dehydrogenase and histopathologic grade in endometrial carcinoma. Tumori 68, 217–221. 10.1177/030089168206800305 [DOI] [PubMed] [Google Scholar]
- Cleton-Jansen A. M., van Beerendonk H. M., Baelde H. J., Bovee J. V., Karperien M., Hogendoorn P. C. (2005). Estrogen signaling is active in cartilaginous tumors: implications for antiestrogen therapy as treatment option of metastasized or irresectable chondrosarcoma. Clin. Cancer Res. 11, 8028–8035. 10.1158/1078-0432.CCR-05-1253 [DOI] [PubMed] [Google Scholar]
- Colette S., Defrere S., Lousse J. C., Van Langendonckt A., Gotteland J. P., Loumaye E., et al. (2011). Inhibition of steroid sulfatase decreases endometriosis in an in vivo murine model. Hum. Reprod. 26, 1362–1370. 10.1093/humrep/der079 [DOI] [PubMed] [Google Scholar]
- Colette S., Defrere S., Van Kerk O., Van Langendonckt A., Dolmans M. M., Donnez J. (2013). Differential expression of steroidogenic enzymes according to endometriosis type. Fertil. Steril. 100, 1642–1649. 10.1016/j.fertnstert.2013.08.003 [DOI] [PubMed] [Google Scholar]
- Colette S., Lousse J. C., Defrere S., Curaba M., Heilier J. F., Van Langendonckt A., et al. (2009). Absence of aromatase protein and mRNA expression in endometriosis. Hum. Reprod. 24, 2133–2141. 10.1093/humrep/dep199 [DOI] [PubMed] [Google Scholar]
- Compston J. E. (2001). Sex steroids and bone. Physiol. Rev. 81, 419–447. 10.1152/physrev.2001.81.1.419 [DOI] [PubMed] [Google Scholar]
- Corbould A. M., Bawden M. J., Lavranos T. C., Rodgers R. J., Judd S. J. (2002). The effect of obesity on the ratio of type 3, 17β-hydroxysteroid dehydrogenase mRNA to cytochrome P450 aromatase mRNA in subcutaneous abdominal and intra-abdominal adipose tissue of women. Int. J. Obes. Relat. Metab. Disord. 26, 165–175. 10.1038/sj.ijo.0801886 [DOI] [PubMed] [Google Scholar]
- Cornel K. M., Krakstad C., Delvoux B., Xanthoulea S., Jori B., Bongers M. Y., et al. (2017). High mRNA levels of 17β-hydroxysteroid dehydrogenase type 1 correlate with poor prognosis in endometrial cancer. Mol. Cell. Endocrinol. 442, 51–57. 10.1016/j.mce.2016.11.030 [DOI] [PubMed] [Google Scholar]
- Cornel K. M., Kruitwagen R. F., Delvoux B., Visconti L., Van de Vijver K. K., Day J. M., et al. (2012). Overexpression of 17β-Hydroxysteroid Dehydrogenase Type 1 Increases the exposure of endometrial cancer to 17β-Estradiol. J. Clin. Endocrinol. Metab. 97, E591–E601. 10.1210/jc.2011-2994 [DOI] [PubMed] [Google Scholar]
- Cornel K. M. C., Bongers M. Y., Kruitwagen R. P. F. M., Romano A. (2018). Local estrogen metabolism (intracrinology) in endometrial cancer: a systematic review. Mol. Cell. Endocrinol. Accepted for publication. [DOI] [PubMed] [Google Scholar]
- Couse J. F., Korach K. S. (1999). Estrogen receptor null mice: what have we learned and where will they lead us? Endocr. Rev. 20, 358–417. [DOI] [PubMed] [Google Scholar]
- Couse J. F., Lindzey J., Grandien K., Gustafsson J. A., Korach K. S. (1997). Tissue distribution and quantitative analysis of estrogen receptor-α (ERα) and estrogen receptor-β (ERβ) messenger ribonucleic acid in the wild-type and ERα-knockout mouse. Endocrinology 138, 4613–4621. 10.1210/endo.138.11.5496 [DOI] [PubMed] [Google Scholar]
- Couse J. F., Yates M. M., Walker V. R., Korach K. S. (2003). Characterization of the hypothalamic-pituitary-gonadal axis in estrogen receptor (ER) Null mice reveals hypergonadism and endocrine sex reversal in females lacking ERα but not ERβ. Mol. Endocrinol. 17, 1039–1053. 10.1210/me.2002-0398 [DOI] [PubMed] [Google Scholar]
- Dalla Valle L., Toffolo V., Nardi A., Fiore C., Armanini D., Belvedere P., et al. (2007). The expression of the human steroid sulfatase-encoding gene is driven by alternative first exons. J. Steroid Biochem. Mol. Biol. 107, 22–29. 10.1016/j.jsbmb.2007.05.004 [DOI] [PubMed] [Google Scholar]
- Das A., Mantena S. R., Kannan A., Evans D. B., Bagchi M. K., Bagchi I. C. (2009). De novo synthesis of estrogen in pregnant uterus is critical for stromal decidualization and angiogenesis. Proc. Natl. Acad. Sci. U.S.A. 106, 12542–12547. 10.1073/pnas.0901647106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dassen H., Punyadeera C., Kamps R., Delvoux B., Van Langendonckt A., Donnez J., et al. (2007). Estrogen metabolizing enzymes in endometrium and endometriosis. Hum. Reprod. 22, 3148–3158. 10.1093/humrep/dem310 [DOI] [PubMed] [Google Scholar]
- Davies W., Humby T., Trent S., Eddy J. B., Ojarikre O. A., Wilkinson L. S. (2014). Genetic and pharmacological modulation of the steroid sulfatase axis improves response control; comparison with drugs used in ADHD. Neuropsychopharmacology 39, 2622–2632. 10.1038/npp.2014.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day J. M., Foster P. A., Tutill H. J., Schmidlin F., Sharland C. M., Hargrave J. D., et al. (2013). STX2171, a 17β-hydroxysteroid dehydrogenase type 3 inhibitor, is efficacious in vivo in a novel hormone-dependent prostate cancer model. Endocr. Relat. Cancer 20, 53–64. 10.1530/ERC-12-0231 [DOI] [PubMed] [Google Scholar]
- De Graaff A. A., D'Hooghe T. M., Dunselman G. A., Dirksen C. D., Hummelshoj L., Consortium W. E., et al. (2013). The significant effect of endometriosis on physical, mental and social wellbeing: results from an international cross-sectional survey. Hum. Reprod. 28, 2677–2685. 10.1093/humrep/det284 [DOI] [PubMed] [Google Scholar]
- De Graaff A. A., Dirksen C. D., Simoens S., De Bie B., Hummelshoj L., D'Hooghe T. M., et al. (2015). Quality of life outcomes in women with endometriosis are highly influenced by recruitment strategies. Hum. Reprod. 30, 1331–1341. 10.1093/humrep/dev084 [DOI] [PubMed] [Google Scholar]
- De Graaff A. A., Van Lankveld J., Smits L. J., Van Beek J. J., Dunselman G. A. (2016). Dyspareunia and depressive symptoms are associated with impaired sexual functioning in women with endometriosis, whereas sexual functioning in their male partners is not affected. Hum. Reprod. 31, 2577–2586. 10.1093/humrep/dew215 [DOI] [PubMed] [Google Scholar]
- De Preter V., Arijs I., Windey K., Vanhove W., Vermeire S., Schuit F., et al. (2012). Impaired butyrate oxidation in ulcerative colitis is due to decreased butyrate uptake and a defect in the oxidation pathway. Inflamm. Bowel Dis. 18, 1127–1136. 10.1002/ibd.21894 [DOI] [PubMed] [Google Scholar]
- Delvoux B., D'Hooghe T., Kyama C., Koskimies P., Hermans R. J., Dunselman G. A., et al. (2014). Inhibition of type 1, 17β-hydroxysteroid dehydrogenase impairs the synthesis of 17β-estradiol in endometriosis lesions. J. Clin. Endocrinol. Metab. 99, 276–284. 10.1210/jc.2013-2851 [DOI] [PubMed] [Google Scholar]
- Delvoux B., Groothuis P., D'Hooghe T., Kyama C., Dunselman G., Romano A. (2009). Increased production of 17β-estradiol in endometriosis lesions is the result of impaired metabolism. J. Clin. Endocrinol. Metab. 94, 876–883. 10.1210/jc.2008-2218 [DOI] [PubMed] [Google Scholar]
- Delvoux B., Husen B., Aldenhoff Y., Koole L., Dunselman G., Thole H., et al. (2007). A sensitive HPLC method for the assessment of metabolic conversion of estrogens. J. Steroid Biochem. Mol. Biol. 104, 246–251. 10.1016/j.jsbmb.2007.03.006 [DOI] [PubMed] [Google Scholar]
- Deng H. Z., You C., Xing Y., Chen K. Y., Zou X. B. (2016). A Family-Based Association Study of CYP11A1 and CYP11B1 Gene Polymorphisms With Autism in Chinese Trios. J. Child Neurol. 31, 733–737. 10.1177/0883073815620672 [DOI] [PubMed] [Google Scholar]
- Devroey P., Bourgain C., Macklon N. S., Fauser B. C. (2004). Reproductive biology and IVF: ovarian stimulation and endometrial receptivity. Trends Endocrinol. Metab. 15, 84–90. 10.1016/j.tem.2004.01.009 [DOI] [PubMed] [Google Scholar]
- Dheenadayalu K., Mak I., Gordts S., Campo R., Higham J., Puttemans P., et al. (2002). Aromatase P450 messenger RNA expression in eutopic endometrium is not a specific marker for pelvic endometriosis. Fertil. Steril. 78, 825–829. 10.1016/S0015-0282(02)03324-1 [DOI] [PubMed] [Google Scholar]
- Di Costanzo L., Penning T. M., Christianson D. W. (2009). Aldo-keto reductases in which the conserved catalytic histidine is substituted. Chem. Biol. Interact. 178, 127–133. 10.1016/j.cbi.2008.10.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dias N. J., Selcer K. W. (2014). Steroid sulfatase mediated growth Sof human MG-63 pre-osteoblastic cells. Steroids 88, 77–82. 10.1016/j.steroids.2014.07.001 [DOI] [PubMed] [Google Scholar]
- Dias N. J., Selcer K. W. (2016). Steroid sulfatase in the human MG-63 preosteoblastic cell line: Antagonistic regulation by glucocorticoids and NFkappaB. Mol. Cell. Endocrinol. 420, 85–96. 10.1016/j.mce.2015.11.029 [DOI] [PubMed] [Google Scholar]
- Dickinson M. E., Flenniken A. M., Ji X., Teboul L., Wong M. D., White J. K., et al. (2016). High-throughput discovery of novel developmental phenotypes. Nature 537, 508–514. 10.1038/nature19356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty J. A., Weiss N. S., Freeman R. J., Dightman D. A., Thornton P. J., Houck J. R., et al. (2005). Genetic factors in catechol estrogen metabolism in relation to the risk of endometrial cancer. Cancer Epidemiol. Biomarkers Prev. 14, 357–366. 10.1158/1055-9965.EPI-04-0479 [DOI] [PubMed] [Google Scholar]
- Dohi O., Hatori M., Suzuki T., Ono K., Hosaka M., Akahira J., et al. (2008). Sex steroid receptors expression and hormone-induced cell proliferation in human osteosarcoma. Cancer Sci. 99, 518–523. 10.1111/j.1349-7006.2007.00673.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Y., Qiu Q. Q., Debear J., Lathrop W. F., Bertolini D. R., Tamburini P. P. (1998). 17β-hydroxysteroid dehydrogenases in human bone cells. J. Bone Miner. Res. 13, 1539–1546. 10.1359/jbmr.1998.13.10.1539 [DOI] [PubMed] [Google Scholar]
- Driessen C. A., Winkens H. J., Hoffmann K., Kuhlmann L. D., Janssen B. P., Van Vugt A. H., et al. (2000). Disruption of the 11-cis-retinol dehydrogenase gene leads to accumulation of cis-retinols and cis-retinyl esters. Mol. Cell. Biol. 20, 4275–4287. 10.1128/MCB.20.12.4275-4287.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drzewiecka H., Galecki B., Jarmolowska-Jurczyszyn D., Kluk A., Dyszkiewicz W., Jagodzinski P. P. (2015). Increased expression of 17-beta-hydroxysteroid dehydrogenase type 1 in non-small cell lung cancer. Lung Cancer 87, 107–116. 10.1016/j.lungcan.2014.12.012 [DOI] [PubMed] [Google Scholar]
- Drzewiecka H., Jagodzinski P. P. (2012). Conversion of estrone to 17-beta-estradiol in human non-small-cell lung cancer cells in vitro. Biomed. Pharmacother. 66, 530–534. 10.1016/j.biopha.2012.02.006 [DOI] [PubMed] [Google Scholar]
- Duell E. J., Travier N., Lujan-Barroso L., Boutron-Ruault M. C., Clavel-Chapelon F., Palli D., et al. (2010). Menstrual and reproductive factors, exogenous hormone use, and gastric cancer risk in a cohort of women from the European Prospective Investigation Into Cancer and Nutrition. Am. J. Epidemiol. 172, 1384–1393. 10.1093/aje/kwq321 [DOI] [PubMed] [Google Scholar]
- Dunselman G. A., Vermeulen N., Becker C., Calhaz-Jorge C., D'Hooghe T., De Bie B., et al. (2014). ESHRE guideline: management of women with endometriosis. Hum. Reprod. 29, 400–412. 10.1093/humrep/det457 [DOI] [PubMed] [Google Scholar]
- Ellem S. J., Wang H., Poutanen M., Risbridger G. P. (2009). Increased endogenous estrogen synthesis leads to the sequential induction of prostatic inflammation (prostatitis) and prostatic pre-malignancy. Am. J. Pathol. 175, 1187–1199. 10.2353/ajpath.2009.081107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endo S., Miyagi N., Matsunaga T., Hara A., Ikari A. (2016). Human dehydrogenase/reductase (SDR family) member 11 is a novel type of 17β-hydroxysteroid dehydrogenase. Biochem. Biophys. Res. Commun. 472, 231–236. 10.1016/j.bbrc.2016.01.190 [DOI] [PubMed] [Google Scholar]
- English M. A., Hughes S. V., Kane K. F., Langman M. J., Stewart P. M., Hewison M. (2000). Oestrogen inactivation in the colon: analysis of the expression and regulation of 17β-hydroxysteroid dehydrogenase isozymes in normal colon and colonic cancer. Br. J. Cancer 83, 550–558. 10.1054/bjoc.2000.1324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- English M. A., Kane K. F., Cruickshank N., Langman M. J., Stewart P. M., Hewison M. (1999). Loss of estrogen inactivation in colonic cancer. J. Clin. Endocrinol. Metab. 84, 2080–2085. 10.1210/jcem.84.6.5772 [DOI] [PubMed] [Google Scholar]
- Enríquez J., Larrea F., Santillan R., Hernandez A., Herrero B., Perez-Palacios G., et al. (2013). Neonatal rat osteoblasts bioconvert testosterone to non-phenolic metabolites with estrogen-like effects on bone cell proliferation and differentiation. Horm. Mol. Biol. Clin. Investig. 13, 41–49. 10.1515/hmbci-2012-0035 [DOI] [PubMed] [Google Scholar]
- Falk R. T., Dallal C. M., Lacey J. V., Jr., Bauer D. C., Buist D. S., Cauley J. A., et al. (2015). Estrogen metabolites are not associated with colorectal cancer risk in postmenopausal women. Cancer Epidemiol. Biomarkers Prev. 24, 1419–1422. 10.1158/1055-9965.EPI-15-0541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrero S., Gillott D. J., Venturini P. L., Remorgida V. (2011). Use of aromatase inhibitors to treat endometriosis-related pain symptoms: a systematic review. Reprod. Biol. Endocrinol. 9, 89. 10.1186/1477-7827-9-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher C. R., Graves K. H., Parlow A. F., Simpson E. R. (1998). Characterization of mice deficient in aromatase (ArKO) because of targeted disruption of the cyp19 gene. Proc. Natl. Acad. Sci. U.S.A. 95, 6965–6970. 10.1073/pnas.95.12.6965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flach K. D., Zwart W. (2016). The first decade of estrogen receptor cistromics in breast cancer. J. Endocrinol. 229 R43–56. 10.1530/JOE-16-0003 [DOI] [PubMed] [Google Scholar]
- Fontein D. B., Houtsma D., Nortier J. W., Baak-Pablo R. F., Kranenbarg E. M., van der Straaten T. R., et al. (2014). Germline variants in the CYP19A1 gene are related to specific adverse events in aromatase inhibitor users: a substudy of Dutch patients in the TEAM trial. Breast Cancer Res. Treat. 144, 599–606. 10.1007/s10549-014-2873-2 [DOI] [PubMed] [Google Scholar]
- Foster P. A. (2013). Oestrogen and colorectal cancer: mechanisms and controversies. Int. J. Colorectal Dis. 28, 737–749. 10.1007/s00384-012-1628-y [DOI] [PubMed] [Google Scholar]
- Foster P. A., Reed M. J., Purohit A. (2008a). Recent developments of steroid sulfatase inhibitors as anti-cancer agents. Anticancer. Agents Med. Chem. 8, 732–738. 10.2174/187152008785914815 [DOI] [PubMed] [Google Scholar]
- Foster P. A., Woo L. W., Potter B. V., Reed M. J., Purohit A. (2008b). The use of steroid sulfatase inhibitors as a novel therapeutic strategy against hormone-dependent endometrial cancer. Endocrinology 149, 4035–4042. 10.1210/en.2008-0223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fouad Mansour M., Pelletier M., Boulet M. M., Mayrand D., Brochu G., Lebel S., et al. (2015). Oxidative activity of 17β-hydroxysteroid dehydrogenase on testosterone in male abdominal adipose tissues and cellular localization of 17β-HSD type 2. Mol. Cell. Endocrinol. 414, 168–176. 10.1016/j.mce.2015.06.016 [DOI] [PubMed] [Google Scholar]
- Freedman N. D., Ahn J., Hou L., Lissowska J., Zatonski W., Yeager M., et al. (2009). Polymorphisms in estrogen- and androgen-metabolizing genes and the risk of gastric cancer. Carcinogenesis 30, 71–77. 10.1093/carcin/bgn258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman N. D., Chow W. H., Gao Y. T., Shu X. O., Ji B. T., Yang G., et al. (2007). Menstrual and reproductive factors and gastric cancer risk in a large prospective study of women. Gut 56, 1671–1677. 10.1136/gut.2007.129411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritsch M., Orfanos C. E., Zouboulis C. C. (2001). Sebocytes are the key regulators of androgen homeostasis in human skin. J. Invest. Dermatol. 116, 793–800. 10.1046/j.1523-1747.2001.01312.x [DOI] [PubMed] [Google Scholar]
- Frycz B. A., Murawa D., Borejsza-Wysocki M., Marciniak R., Murawa P., Drews M., et al. (2015). Expression of 17β-hydroxysteroid dehydrogenase type 2 is associated with some clinicopathological features in gastric cancer. Biomed. Pharmacother. 70, 24–27. 10.1016/j.biopha.2014.12.042 [DOI] [PubMed] [Google Scholar]
- Frycz B. A., Murawa D., Borejsza-Wysocki M., Wichtowski M., Spychala A., Marciniak R., et al. (2016). Transcript level of AKR1C3 is down-regulated in gastric cancer. Biochem. Cell Biol. 94, 138–146. 10.1139/bcb-2015-0096 [DOI] [PubMed] [Google Scholar]
- Fujikawa H., Okura F., Kuwano Y., Sekizawa A., Chiba H., Shimodaira K., et al. (1997). Steroid sulfatase activity in osteoblast cells. Biochem. Biophys. Res. Commun. 231, 42–47. 10.1006/bbrc.1996.6038 [DOI] [PubMed] [Google Scholar]
- Gangloff A., Shi R., Nahoum V., Lin S. X. (2003). Pseudo-symmetry of C19 steroids, alternative binding orientations, and multispecificity in human estrogenic 17β-hydroxysteroid dehydrogenase. FASEB J. 17, 274–276. 10.1096/fj.02-0397fje [DOI] [PubMed] [Google Scholar]
- Gao J., He J., Shi X., Stefanovic-Racic M., Xu M., O'Doherty R. M., et al. (2012). Sex-specific effect of estrogen sulfotransferase on mouse models of type 2 diabetes. Diabetes 61, 1543–1551. 10.2337/db11-1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gargano E. M., Allegretta G., Perspicace E., Carotti A., Van Koppen C., Frotscher M., et al. (2015). 17β-Hydroxysteroid dehydrogenase Type 2 inhibition: discovery of selective and metabolically stable compounds inhibiting both the human enzyme and its murine ortholog. PLoS ONE 10:e0134754. 10.1371/journal.pone.0134754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh D., Dhara S., Kumar A., Sengupta J. (1999). Immunohistochemical localization of receptors for progesterone and oestradiol-17 beta in the implantation site of the rhesus monkey. Hum. Reprod. 14, 505–514. 10.1093/humrep/14.2.505 [DOI] [PubMed] [Google Scholar]
- Gibbs T. T., Russek S. J., Farb D. H. (2006). Sulfated steroids as endogenous neuromodulators. Pharmacol. Biochem. Behav. 84, 555–567. 10.1016/j.pbb.2006.07.031 [DOI] [PubMed] [Google Scholar]
- Gibson D. A., McInnes K. J., Critchley H. O., Saunders P. T. (2013). Endometrial Intracrinology–generation of an estrogen-dominated microenvironment in the secretory phase of women. J. Clin. Endocrinol. Metab. 98, E1802–E1806. 10.1210/jc.2013-2140 [DOI] [PubMed] [Google Scholar]
- Gilligan L. C., Gondal A., Tang V., Hussain M. T., Arvaniti A., Hewitt A. M., et al. (2017). Estrone sulfate transport and steroid sulfatase activity in colorectal cancer: implications for hormone replacement therapy. Front. Pharmacol. 8:103. 10.3389/fphar.2017.00103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Arenas A., Agramonte-Hevia J. (2012). Sex steroid hormone effects in normal and pathologic conditions in lung physiology. Mini Rev. Med. Chem. 12, 1055–1062. 10.2174/138955712802762194 [DOI] [PubMed] [Google Scholar]
- Goodarzi M. O., Antoine H. J., Azziz R. (2007). Genes for enzymes regulating dehydroepiandrosterone sulfonation are associated with levels of dehydroepiandrosterone sulfate in polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 92, 2659–2664. 10.1210/jc.2006-2600 [DOI] [PubMed] [Google Scholar]
- Goodarzi M. O., Shah N. A., Antoine H. J., Pall M., Guo X., Azziz R. (2006). Variants in the 5α-reductase type 1 and type 2 genes are associated with polycystic ovary syndrome and the severity of hirsutism in affected women. J. Clin. Endocrinol. Metab. 91, 4085–4091. 10.1210/jc.2006-0227 [DOI] [PubMed] [Google Scholar]
- Groothuis P. G., Dassen H. H., Romano A., Punyadeera C. (2007). Estrogen and the endometrium: lessons learned from gene expression profiling in rodents and human. Hum. Reprod. Update 13, 405–417. 10.1093/humupd/dmm009 [DOI] [PubMed] [Google Scholar]
- Gruber C. J., Tschugguel W., Schneeberger C., Huber J. C. (2002). Production and actions of estrogens. N. Engl. J. Med. 346, 340–352. 10.1056/NEJMra000471 [DOI] [PubMed] [Google Scholar]
- Guillot F., Garcia A., Salou M., Brouard S., Laplaud D. A., Nicot A. B. (2015). Transcript analysis of laser capture microdissected white matter astrocytes and higher phenol sulfotransferase 1A1 expression during autoimmune neuroinflammation. J. Neuroinflammation 12, 130. 10.1186/s12974-015-0348-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulyaeva L. F., Mikhailova O. N., PustyInyak V. O., Kim I. V., IV., Gerasimov A. V., Krasilnikov S. E., et al. (2008). Comparative analysis of SNP in estrogen-metabolizing enzymes for ovarian, endometrial, and breast cancers in Novosibirsk, Russia. Adv. Exp. Med. Biol. 617, 359–366. 10.1007/978-0-387-69080-3_34 [DOI] [PubMed] [Google Scholar]
- Gylfe A. E., Katainen R., Kondelin J., Tanskanen T., Cajuso T., Hanninen U., et al. (2013). Eleven candidate susceptibility genes for common familial colorectal cancer. PLoS Genet. 9:e1003876. 10.1371/journal.pgen.1003876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakkarainen J., Jokela H., Pakarinen P., Heikela H., Katkanaho L., Vandenput L., et al. (2015). Hydroxysteroid (17β)-dehydrogenase 1-deficient female mice present with normal puberty onset but are severely subfertile due to a defect in luteinization and progesterone production. FASEB J. 29, 3806–3816. 10.1096/fj.14-269035 [DOI] [PubMed] [Google Scholar]
- He D., Frost A. R., Falany C. N. (2005a). Identification and immunohistochemical localization of Sulfotransferase 2B1b (SULT2B1b) in human lung. Biochim Biophys Act. 1724, 119–126. 10.1016/j.bbagen.2005.03.018 [DOI] [PubMed] [Google Scholar]
- He D., Meloche C. A., Dumas N. A., Frost A. R., Falany C. N. (2004). Different subcellular localization of sulphotransferase 2B1b in human placenta and prostate. Biochem. J. 379, 533–540. 10.1042/bj20031524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He W., Gauri M., Li T., Wang R., Lin S. X. (2016). Current knowledge of the multifunctional 17β-hydroxysteroid dehydrogenase type 1 (HSD17B1). Gene 588, 54–61. 10.1016/j.gene.2016.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He X. Y., Wegiel J., Yang Y. Z., Pullarkat R., Schulz H., Yang S. Y. (2005b). Type 10, 17β-hydroxysteroid dehydrogenase catalyzing the oxidation of steroid modulators of gamma-aminobutyric acid type A receptors. Mol. Cell. Endocrinol. 229, 111–117. 10.1016/j.mce.2004.08.011 [DOI] [PubMed] [Google Scholar]
- He X. Y., Yang S. Y. (2006). Roles of type 10, 17β-hydroxysteroid dehydrogenase in intracrinology and metabolism of isoleucine and fatty acids. Endocr. Metab. Immune Disord. Drug Targets 6, 95–102. 10.2174/187153006776056639 [DOI] [PubMed] [Google Scholar]
- Heijmans J., Wielenga M. C., Rosekrans S. L., van Lidth de Jeude J. F., Roelofs J., Groothuis P., et al. (2014). Oestrogens promote tumorigenesis in a mouse model for colitis-associated cancer. Gut 63, 310–316. 10.1136/gutjnl-2012-304216 [DOI] [PubMed] [Google Scholar]
- Her C., Szumlanski C., Aksoy I. A., Weinshilboum R. M. (1996). Human jejunal estrogen sulfotransferase and dehydroepiandrosterone sulfotransferase: immunochemical characterization of individual variation. Drug Metab. Dispos. 24, 1328–1335. [PubMed] [Google Scholar]
- Hevir N., Ribic-Pucelj M., Lanisnik Rizner T. (2013). Disturbed balance between phase I and II metabolizing enzymes in ovarian endometriosis: a source of excessive hydroxy-estrogens and ROS? Mol. Cell. Endocrinol. 367, 74–84. 10.1016/j.mce.2012.12.019 [DOI] [PubMed] [Google Scholar]
- Hevir N., Sinkovec J., Rizner T. L. (2011a). Disturbed expression of phase I and phase II estrogen-metabolizing enzymes in endometrial cancer: lower levels of CYP1B1 and increased expression of S-COMT. Mol. Cell. Endocrinol. 331, 158–167. 10.1016/j.mce.2010.09.011 [DOI] [PubMed] [Google Scholar]
- Hevir N., Vouk K., Sinkovec J., Ribic-Pucelj M., Rizner T. L. (2011b). Aldo-keto reductases AKR1C1, AKR1C2 and AKR1C3 may enhance progesterone metabolism in ovarian endometriosis. Chem. Biol. Interact. 191, 217–226. 10.1016/j.cbi.2011.01.003 [DOI] [PubMed] [Google Scholar]
- Hewitt S. C., Winuthayanon W., Korach K. S. (2016). What's new in estrogen receptor action in the female reproductive tract. J. Mol. Endocrinol. 56 R55–71. 10.1530/JME-15-0254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilborn E., Stal O., Jansson A. (2017). Estrogen and androgen-converting enzymes 17β-hydroxysteroid dehydrogenase and their involvement in cancer: with a special focus on 17β-hydroxysteroid dehydrogenase type 1, 2, and breast cancer. Oncotarget 8, 30552–30562. 10.18632/oncotarget.15547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan A. M., Collins D., Baird A. W., Winter D. C. (2009). Estrogen and gastrointestinal malignancy. Mol. Cell. Endocrinol. 307, 19–24. 10.1016/j.mce.2009.03.016 [DOI] [PubMed] [Google Scholar]
- Honda S., Harada N., Ito S., Takagi Y., Maeda S. (1998). Disruption of sexual behavior in male aromatase-deficient mice lacking exons 1 and 2 of the cyp19 gene. Biochem. Biophys. Res. Commun. 252, 445–449. 10.1006/bbrc.1998.9672 [DOI] [PubMed] [Google Scholar]
- Hovorkova P., Kristofikova Z., Horinek A., Ripova D., Majer E., Zach P., et al. (2008). Lateralization of 17β-hydroxysteroid dehydrogenase type 10 in hippocampi of demented and psychotic people. Dement. Geriatr. Cogn. Disord. 26, 193–198. 10.1159/000151778 [DOI] [PubMed] [Google Scholar]
- Hu M. C., Hsu N. C., El Hadj N. B., Pai C. I., Chu H. P., Wang C. K., et al. (2002). Steroid deficiency syndromes in mice with targeted disruption of Cyp11a1. Mol. Endocrinol. 16, 1943–1950. 10.1210/me.2002-0055 [DOI] [PubMed] [Google Scholar]
- Huang C. C., Shih M. C., Hsu N. C., Chien Y., Chung B. C. (2012). Fetal glucocorticoid synthesis is required for development of fetal adrenal medulla and hypothalamus feedback suppression. Endocrinology 153, 4749–4756. 10.1210/en.2012-1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang X. F., Luu-The V. (2000). Molecular characterization of a first human 3(α->β)-hydroxysteroid epimerase. J. Biol. Chem. 275, 29452–29457. 10.1074/jbc.M000562200 [DOI] [PubMed] [Google Scholar]
- Huber A., Keck C. C., Hefler L. A., Schneeberger C., Huber J. C., Bentz E. K., et al. (2005). Ten estrogen-related polymorphisms and endometriosis: a study of multiple gene-gene interactions. Obstet. Gynecol. 106, 1025–1031. 10.1097/01.AOG.0000185259.01648.41 [DOI] [PubMed] [Google Scholar]
- Hudelist G., Czerwenka K., Keckstein J., Haas C., Fink-Retter A., Gschwantler-Kaulich D., et al. (2007). Expression of aromatase and estrogen sulfotransferase in eutopic and ectopic endometrium: evidence for unbalanced estradiol production in endometriosis. Reprod. Sci. 14, 798–805. 10.1177/1933719107309120 [DOI] [PubMed] [Google Scholar]
- Hughes S. V., Robinson E., Bland R., Lewis H. M., Stewart P. M., Hewison M. (1997). 1,25-dihydroxyvitamin D3 regulates estrogen metabolism in cultured keratinocytes. Endocrinology 138, 3711–3718. 10.1210/endo.138.9.5406 [DOI] [PubMed] [Google Scholar]
- Huhtinen K., Desai R., Stahle M., Salminen A., Handelsman D. J., Perheentupa A., et al. (2012a). Endometrial and endometriotic concentrations of estrone and estradiol are determined by local metabolism rather than circulating levels. J. Clin. Endocrinol. Metab. 97, 4228–4235. 10.1210/jc.2012-1154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huhtinen K., Saloniemi-Heinonen T., Keski-Rahkonen P., Desai R., Laajala D., Stahle M., et al. (2014). Intra-tissue steroid profiling indicates differential progesterone and testosterone metabolism in the endometrium and endometriosis lesions. J. Clin. Endocrinol. Metab. 99 E2188–2197. 10.1210/jc.2014-1913 [DOI] [PubMed] [Google Scholar]
- Huhtinen K., Stahle M., Perheentupa A., Poutanen M. (2012b). Estrogen biosynthesis and signaling in endometriosis. Mol. Cell. Endocrinol. 358, 146–154. 10.1016/j.mce.2011.08.022 [DOI] [PubMed] [Google Scholar]
- Husen B., Huhtinen K., Poutanen M., Kangas L., Messinger J., Thole H. (2006). Evaluation of inhibitors for 17β-hydroxysteroid dehydrogenase type 1 in vivo in immunodeficient mice inoculated with MCF-7 cells stably expressing the recombinant human enzyme. Mol. Cell. Endocrinol. 248, 109–113. 10.1016/j.mce.2005.11.042 [DOI] [PubMed] [Google Scholar]
- Ihlenfeldt W. D., Bolton E. E., Bryant S. H. (2009). The PubChem chemical structure sketcher. J. Cheminform. 1:20. 10.1186/1758-2946-1-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iida S., Kakinuma H., Miki Y., Abe K., Sakurai M., Suzuki S., et al. (2013). Steroid sulphatase and oestrogen sulphotransferase in human non-small-cell lung carcinoma. Br. J. Cancer 108, 1415–1424. 10.1038/bjc.2013.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda K., Shiraishi K., Yoshida A., Shinchi Y., Sanada M., Motooka Y., et al. (2016). Synchronous multiple lung adenocarcinomas: estrogen concentration in peripheral lung. PLoS ONE 11:e0160910. 10.1371/journal.pone.0160910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal M. J., Greenway B., Wilkinson M. L., Johnson P. J., Williams R. (1983). Sex-steroid enzymes, aromatase and 5 alpha-reductase in the pancreas: a comparison of normal adult, foetal and malignant tissue. Clin. Sci. 65, 71–75. 10.1042/cs0650071 [DOI] [PubMed] [Google Scholar]
- Ishida M., Choi J. H., Hirabayashi K., Matsuwaki T., Suzuki M., Yamanouchi K., et al. (2007). Reproductive phenotypes in mice with targeted disruption of the 20α-hydroxysteroid dehydrogenase gene. J. Reprod. Dev. 53, 499–508. 10.1262/jrd.18125 [DOI] [PubMed] [Google Scholar]
- Ito K., Miki Y., Suzuki T., McNamara K. M., Sasano H. (2016). In situ androgen and estrogen biosynthesis in endometrial cancer: focus on androgen actions and intratumoral production. Endocr. Relat. Cancer 23 R323–335. 10.1530/ERC-15-0470 [DOI] [PubMed] [Google Scholar]
- Ito K., Suzuki T., Akahira J., Moriya T., Kaneko C., Utsunomiya H., et al. (2002). Expression of androgen receptor and 5α-reductases in the human normal endometrium and its disorders. Int. J. Cancer 99, 652–657. 10.1002/ijc.10394 [DOI] [PubMed] [Google Scholar]
- Ito K., Utsunomiya H., Suzuki T., Saitou S., Akahira J., Okamura K., et al. (2006). 17β-hydroxysteroid dehydrogenases in human endometrium and its disorders. Mol. Cell. Endocrinol. 248, 136–140. 10.1016/j.mce.2005.11.038 [DOI] [PubMed] [Google Scholar]
- Iwasa A., Arakaki R., Honma N., Ushio A., Yamada A., Kondo T., et al. (2015). Aromatase controls Sjogren syndrome-like lesions through monocyte chemotactic protein-1 in target organ and adipose tissue-associated macrophages. Am. J. Pathol. 185, 151–161. 10.1016/j.ajpath.2014.09.006 [DOI] [PubMed] [Google Scholar]
- Jakob F., Siggelkow H., Homann D., Kohrle J., Adamski J., Schutze N. (1997). Local estradiol metabolism in osteoblast- and osteoclast-like cells. J. Steroid Biochem. Mol. Biol. 61, 167–174. 10.1016/S0960-0760(97)80009-X [DOI] [PubMed] [Google Scholar]
- Janssen J. M., Bland R., Hewison M., Coughtrie M. W., Sharp S., Arts J., et al. (1999). Estradiol formation by human osteoblasts via multiple pathways: relation with osteoblast function. J. Cell. Biochem. 75, 528–537. [DOI] [PubMed] [Google Scholar]
- Jäntti S. E., Tammimaki A., Raattamaa H., Piepponen P., Kostiainen R., Ketola R. A. (2010). Determination of steroids and their intact glucuronide conjugates in mouse brain by capillary liquid chromatography-tandem mass spectrometry. Anal. Chem. 82, 3168–3175. 10.1021/ac902321z [DOI] [PubMed] [Google Scholar]
- Järvensivu P., Heinosalo T., Hakkarainen J., Kronqvist P., Saarinen N., Poutanen M. (2018). HSD17B1 expression induces inflammation-aided rupture of mammary gland myoepithelium. Endocr. Relat. Cancer 25, 393–406. 10.1530/ERC-17-0476 [DOI] [PubMed] [Google Scholar]
- Järvensivu P., Saloniemi-Heinonen T., Awosanya M., Koskimies P., Saarinen N., Poutanen M. (2015). HSD17B1 expression enhances estrogen signaling stimulated by the low active estrone, evidenced by an estrogen responsive element-driven reporter gene in vivo. Chem. Biol. Interact. 234, 126–134. 10.1016/j.cbi.2015.01.008 [DOI] [PubMed] [Google Scholar]
- Jeon Y. T., Park S. Y., Kim Y. B., Kim J. W., Park N. H., Kang S. B., et al. (2007). Aromatase expression was not detected by immunohistochemistry in endometrial cancer. Ann. N. Y. Acad. Sci. 1095, 70–75. 10.1196/annals.1397.010 [DOI] [PubMed] [Google Scholar]
- Jin Y., Mesaros A. C., Blair I. A., Penning T. M. (2011). Stereospecific reduction of 5β-reduced steroids by human ketosteroid reductases of the AKR (aldo-keto reductase) superfamily: role of AKR1C1-AKR1C4 in the metabolism of testosterone and progesterone via the 5β-reductase pathway. Biochem. J. 437, 53–61. 10.1042/BJ20101804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokela H., Rantakari P., Lamminen T., Strauss L., Ola R., Mutka A. L., et al. (2010). Hydroxysteroid (17β) dehydrogenase 7 activity is essential for fetal de novo cholesterol synthesis and for neuroectodermal survival and cardiovascular differentiation in early mouse embryos. Endocrinology 151, 1884–1892. 10.1210/en.2009-0928 [DOI] [PubMed] [Google Scholar]
- Jones A. L., Hume R., Bamforth K. J., Coughtrie M. W. (1992). Estrogen and phenol sulfotransferase activities in human fetal lung. Early Hum. Dev. 28, 65–77. 10.1016/0378-3782(92)90007-4 [DOI] [PubMed] [Google Scholar]
- Jones M. R., Mathur R., Cui J., Guo X., Azziz R., Goodarzi M. O. (2009). Independent confirmation of association between metabolic phenotypes of polycystic ovary syndrome and variation in the type 6, 17β-hydroxysteroid dehydrogenase gene. J. Clin. Endocrinol. Metab. 94, 5034–5038. 10.1210/jc.2009-0931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongen V. H., Thijssen J. H., Hollema H., Donker G. H., Santema J. G., Van der Zee A. G., et al. (2005). Is aromatase cytochrome P450 involved in the pathogenesis of endometrioid endometrial cancer? Int. J. Gynecol. Cancer 15, 529–536. 10.1111/j.1525-1438.2005.15320.x [DOI] [PubMed] [Google Scholar]
- Kancheva L., Hill M., Vcelakova H., Vrbikova J., Pelikanova T., Starka L. (2007). The identification and simultaneous quantification of neuroactive androstane steroids and their polar conjugates in the serum of adult men, using gas chromatography-mass spectrometry. Steroids 72, 792–801. 10.1016/j.steroids.2007.06.006 [DOI] [PubMed] [Google Scholar]
- Kassem M., Okazaki R., Harris S. A., Spelsberg T. C., Conover C. A., Riggs B. L. (1998). Estrogen effects on insulin-like growth factor gene expression in a human osteoblastic cell line with high levels of estrogen receptor. Calcif. Tissue Int. 62, 60–66. 10.1007/s002239900395 [DOI] [PubMed] [Google Scholar]
- Kemilainen H., Adam M., Maki-Jouppila J., Damdimopoulou P., Damdimopoulos A. E., Kere J., et al. (2016). The hydroxysteroid (17β) dehydrogenase family gene HSD17B12 Is involved in the prostaglandin synthesis pathway, the ovarian function, and regulation of fertility. Endocrinology 157, 3719–3730. 10.1210/en.2016-1252 [DOI] [PubMed] [Google Scholar]
- Kennelly R., Kavanagh D. O., Hogan A. M., Winter D. C. (2008). Oestrogen and the colon: potential mechanisms for cancer prevention. Lancet Oncol. 9, 385–391. 10.1016/S1470-2045(08)70100-1 [DOI] [PubMed] [Google Scholar]
- Kikuchi A., Furutani T., Azami H., Watanabe K., Niimi T., Kamiyama Y., et al. (2014). In vitro and in vivo characterisation of ASP9521: a novel, selective, orally bioavailable inhibitor of 17β-hydroxysteroid dehydrogenase type 5 (17βHSD5; AKR1C3). Invest. New Drugs 32, 860–870. 10.1007/s10637-014-0130-5 [DOI] [PubMed] [Google Scholar]
- Kim J. H., Cho H. T., Kim Y. J. (2014). The role of estrogen in adipose tissue metabolism: insights into glucose homeostasis regulation. Endocr. J. 61, 1055–1067. 10.1507/endocrj.EJ14-0262 [DOI] [PubMed] [Google Scholar]
- Kim S., Thiessen P. A., Bolton E. E., Chen J., Fu G., Gindulyte A., et al. (2016). PubChem substance and compound databases. Nucleic Acids Res. 44, D1202–D1213. 10.1093/nar/gkv951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim T. S., Maeda A., Maeda T., Heinlein C., Kedishvili N., Palczewski K., et al. (2005). Delayed dark adaptation in 11-cis-retinol dehydrogenase-deficient mice: a role of RDH11 in visual processes in vivo. J. Biol. Chem. 280, 8694–8704. 10.1074/jbc.M413172200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimoto T., Ishii H., Higo S., Hojo Y., Kawato S. (2010). Semicomprehensive analysis of the postnatal age-related changes in the mRNA expression of sex steroidogenic enzymes and sex steroid receptors in the male rat hippocampus. Endocrinology 151, 5795–5806. 10.1210/en.2010-0581 [DOI] [PubMed] [Google Scholar]
- Kimura Y., Suzuki T., Kaneko C., Darnel A. D., Akahira J., Ebina M., et al. (2003). Expression of androgen receptor and 5α-reductase types 1 and 2 in early gestation fetal lung: a possible correlation with branching morphogenesis. Clin. Sci. 105, 709–713. 10.1042/CS20030236 [DOI] [PubMed] [Google Scholar]
- Kitaoka Y., Kitawaki J., Koshiba H., Inoue S., Ishihara H., Teramoto M., et al. (2004). Aromatase cytochrome P450 and estrogen and progesterone receptors in uterine sarcomas: correlation with clinical parameters. J. Steroid Biochem. Mol. Biol. 88, 183–189. 10.1016/j.jsbmb.2003.11.013 [DOI] [PubMed] [Google Scholar]
- Kitawaki J., Kado N., Ishihara H., Koshiba H., Kitaoka Y., Honjo H. (2002). Endometriosis: the pathophysiology as an estrogen-dependent disease. J. Steroid Biochem. Mol. Biol. 83, 149–155. 10.1016/S0960-0760(02)00260-1 [DOI] [PubMed] [Google Scholar]
- Kitawaki J., Koshiba H., Ishihara H., Kusuki I., Tsukamoto K., Honjo H. (2000). Progesterone induction of 17β-hydroxysteroid dehydrogenase type 2 during the secretory phase occurs in the endometrium of estrogen-dependent benign diseases but not in normal endometrium. J. Clin. Endocrinol. Metab. 85, 3292–3296. 10.1210/jcem.85.9.6829 [DOI] [PubMed] [Google Scholar]
- Kitawaki J., Kusuki I., Koshiba H., Tsukamoto K., Fushiki S., Honjo H. (1999). Detection of aromatase cytochrome P-450 in endometrial biopsy specimens as a diagnostic test for endometriosis. Fertil. Steril. 72, 1100–1106. 10.1016/S0015-0282(99)00424-0 [DOI] [PubMed] [Google Scholar]
- Knapp P., Chabowski A., Blachnio-Zabielska A., Walentowicz-Sadlecka M., Grabiec M., Knapp P. A. (2013). Expression of estrogen receptors (alpha, beta), cyclooxygenase-2 and aromatase in normal endometrium and endometrioid cancer of uterus. Adv. Med. Sci. 58, 96–103. 10.2478/v10039-012-0055-1 [DOI] [PubMed] [Google Scholar]
- Kobayashi H., Yoshida S., Sun Y. J., Shirasawa N., Naito A. (2013). Postnatal development of gastric aromatase and portal venous estradiol-17β levels in male rats. J. Endocrinol. 218, 117–124. 10.1530/JOE-13-0074 [DOI] [PubMed] [Google Scholar]
- Kohno M., Okamoto T., Suda K., Shimokawa M., Kitahara H., Shimamatsu S., et al. (2014). Prognostic and therapeutic implications of aromatase expression in lung adenocarcinomas with EGFR mutations. Clin. Cancer Res. 20, 3613–3622. 10.1158/1078-0432.CCR-13-2683 [DOI] [PubMed] [Google Scholar]
- Koizumi M., Momoeda M., Hiroi H., Hosokawa Y., Tsutsumi R., Osuga Y., et al. (2010). Expression and regulation of cholesterol sulfotransferase (SULT2B1b) in human endometrium. Fertil. Steril. 93, 1538–1544. 10.1016/j.fertnstert.2009.01.075 [DOI] [PubMed] [Google Scholar]
- Konings G. F., Cornel K. M., Xanthoulea S., Delvoux B., Skowron M. A., Kooreman L., et al. (2018). Blocking 17β-hydroxysteroid dehydrogenase type 1 in endometrial cancer: a potential novel endocrine therapeutic approach. J. Pathol. 244, 203–214. 10.1002/path.5004 [DOI] [PubMed] [Google Scholar]
- Konings G. F., Reynaert N. L., Delvoux B., Verhamme F. M., Bracke K. R., Brusselle G. G., et al. (2017). Increased levels of enzymes involved in local estradiol synthesis in chronic obstructive pulmonary disease. Mol. Cell. Endocrinol. 443, 23–31. 10.1016/j.mce.2016.12.001 [DOI] [PubMed] [Google Scholar]
- Kreitmann O., Kreitmann-Gimbal B., Bayard F., Hodgen G. D. (1979). 17 beta-hydroxysteroid dehydrogenase in monkey endometrium: characterization of enzyme activity, and effects of estradiol alone or in combination with progesterone. Steroids 34, 693–703. 10.1016/0039-128X(79)90139-9 [DOI] [PubMed] [Google Scholar]
- Kríz L., Bicikova M., Hampl R. (2008a). Roles of steroid sulfatase in brain and other tissues. Physiol. Res. 57, 657–668. [DOI] [PubMed] [Google Scholar]
- Kríz L., Bicikova M., Mohapl M., Hill M., Cerny I., Hampl R. (2008b). Steroid sulfatase and sulfuryl transferase activities in human brain tumors. J. Steroid Biochem. Mol. Biol. 109, 31–39. 10.1016/j.jsbmb.2007.12.004 [DOI] [PubMed] [Google Scholar]
- Laatikainen T., Laitinen E. A., Vihko R. (1971). Secretion of free and sulfate-conjugated neutral steroids by the human testis. Effect of administration of human chorionic gonadotropin. J. Clin. Endocrinol. Metab. 32, 59–64. 10.1210/jcem-32-1-59 [DOI] [PubMed] [Google Scholar]
- Labrie F. (1991). Intracrinology. Mol. Cell. Endocrinol. 78, C113–C118. 10.1016/0303-7207(91)90116-A [DOI] [PubMed] [Google Scholar]
- Labrie F. (2015). All sex steroids are made intracellularly in peripheral tissues by the mechanisms of intracrinology after menopause. J. Steroid Biochem. Mol. Biol. 145, 133–138. 10.1016/j.jsbmb.2014.06.001 [DOI] [PubMed] [Google Scholar]
- Labrie F., Labrie C. (2013). DHEA and intracrinology at menopause, a positive choice for evolution of the human species. Climacteric 16, 205–213. 10.3109/13697137.2012.733983 [DOI] [PubMed] [Google Scholar]
- Lane G. (1990). The histochemistry of isocitric and oestradiol-17 beta dehydrogenases in the endometrium of postmenopausal women treated with oestrogens and progestogens. Histochem. J. 22, 45–50. 10.1007/BF01962878 [DOI] [PubMed] [Google Scholar]
- Laplante Y., Rancourt C., Poirier D. (2009). Relative involvement of three 17β-hydroxysteroid dehydrogenases (types 1, 7 and 12) in the formation of estradiol in various breast cancer cell lines using selective inhibitors. Mol. Cell. Endocrinol. 301, 146–153. 10.1016/j.mce.2008.08.026 [DOI] [PubMed] [Google Scholar]
- Lavasani S., Chlebowski R. T., Prentice R. L., Kato I., Wactawski-Wende J., Johnson K. C., et al. (2015). Estrogen and colorectal cancer incidence and mortality. Cancer 121, 3261–3271. 10.1002/cncr.29464 [DOI] [PubMed] [Google Scholar]
- Lee D. K., Kurihara I., Jeong J. W., Lydon J. P., DeMayo F. J., Tsai M. J., et al. (2010). Suppression of ERα activity by COUP-TFII is essential for successful implantation and decidualization. Mol. Endocrinol. 24, 930–940. 10.1210/me.2009-0531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lépine J., Audet-Walsh E., Gregoire J., Tetu B., Plante M., Menard V., et al. (2010). Circulating estrogens in endometrial cancer cases and their relationship with tissular expression of key estrogen biosynthesis and metabolic pathways. J. Clin. Endocrinol. Metab. 95, 2689–2698. 10.1210/jc.2010-2648 [DOI] [PubMed] [Google Scholar]
- Li C., Chen P., Palladino A., Narayan S., Russell L. K., Sayed S., et al. (2010). Mechanism of hyperinsulinism in short-chain 3-hydroxyacyl-CoA dehydrogenase deficiency involves activation of glutamate dehydrogenase. J. Biol. Chem. 285, 31806–31818. 10.1074/jbc.M110.123638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Qin L., Xiao Z. J., Wang Y. L., Herva R., Leng J. H., et al. (2003). Expression of P450 aromatase and 17β-hydroxysteroid dehydrogenase type 1 at fetal-maternal interface during tubal pregnancy. J. Steroid Biochem. Mol. Biol. 87, 241–246. 10.1016/j.jsbmb.2003.09.013 [DOI] [PubMed] [Google Scholar]
- Lilla C., Risch A., Verla-Tebit E., Hoffmeister M., Brenner H., Chang-Claude J. (2007). SULT1A1 genotype and susceptibility to colorectal cancer. Int. J. Cancer 120, 201–206. 10.1002/ijc.22156 [DOI] [PubMed] [Google Scholar]
- Lim Y. A., Grimm A., Giese M., Mensah-Nyagan A. G., Villafranca J. E., Ittner L. M., et al. (2011). Inhibition of the mitochondrial enzyme ABAD restores the amyloid-beta-mediated deregulation of estradiol. PLoS ONE 6:e28887. 10.1371/journal.pone.0028887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H. K., Jez J. M., Schlegel B. P., Peehl D. M., Pachter J. A., Penning T. M. (1997). Expression and characterization of recombinant type 2, 3 α-hydroxysteroid dehydrogenase (HSD) from human prostate: demonstration of bifunctional 3α/17β-HSD activity and cellular distribution. Mol. Endocrinol. 11, 1971–1984. [DOI] [PubMed] [Google Scholar]
- Lindemann K., Malander S., Christensen R. D., Mirza M. R., Kristensen G. B., Aavall-Lundqvist E., et al. (2014). Examestane in advanced or recurrent endometrial carcinoma: a prospective phase II study by the Nordic Society of Gynecologic Oncology (NSGO). BMC Cancer 14:68. 10.1186/1471-2407-14-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Yao Z. X., Bendavid C., Borgmeyer C., Han Z., Cavalli L. R., et al. (2005). Haploinsufficiency of cytochrome P450, 17β-hydroxylase/17,20 lyase (CYP17) causes infertility in male mice. Mol. Endocrinol. 19, 2380–2389. 10.1210/me.2004-0418 [DOI] [PubMed] [Google Scholar]
- Lønning P. E., Eikesdal H. P. (2013). Aromatase inhibition 2013: clinical state of the art and questions that remain to be solved. Endocr. Relat. Cancer 20, R183–R201. 10.1530/ERC-13-0099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- López M., Tena-Sempere M. (2015). Estrogens and the control of energy homeostasis: a brain perspective. Trends Endocrinol. Metab. 26, 411–421. 10.1016/j.tem.2015.06.003 [DOI] [PubMed] [Google Scholar]
- López M., Tena-Sempere M. (2016). Estradiol and brown fat. Best Pract. Res. Clin. Endocrinol. Metab. 30, 527–536. 10.1016/j.beem.2016.08.004 [DOI] [PubMed] [Google Scholar]
- Loria R. M., Graf M. R. (2012). 17α-androstenediol-mediated oncophagy of tumor cells by different mechanisms is determined by the target tumor. Ann. N. Y. Acad. Sci. 1262, 127–133. 10.1111/j.1749-6632.2012.06602.x [DOI] [PubMed] [Google Scholar]
- Loriot Y., Fizazi K., Jones R. J., Van den Brande J., Molife R. L., Omlin A., et al. (2014). Safety, tolerability and anti-tumour activity of the androgen biosynthesis inhibitor ASP9521 in patients with metastatic castration-resistant prostate cancer: multi-centre phase I/II study. Invest. New Drugs 32, 995–1004. 10.1007/s10637-014-0101-x [DOI] [PubMed] [Google Scholar]
- Loth D. W., Soler Artigas M., Gharib S. A., Wain L. V., Franceschini N., Koch B., et al. (2014). Genome-wide association analysis identifies six new loci associated with forced vital capacity. Nat. Genet. 46, 669–677. 10.1038/ng.3011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loza M. C. (1995). Hydrolysis of estrone sulfate in uterine minces of the 6-days pregnant rat. J. Steroid Biochem. Mol. Biol. 52, 277–280. 10.1016/0960-0760(94)00177-N [DOI] [PubMed] [Google Scholar]
- Lu C., Lee H. S., Pappas G. P., Dilling D. F., Burger C. D., Shifren A., et al. (2017). A Phase II Clinical Trial of an Aromatase Inhibitor for Postmenopausal Women with Lymphangioleiomyomatosis. Ann. Am. Thorac. Soc. 14, 919–928. 10.1513/AnnalsATS.201610-824OC [DOI] [PubMed] [Google Scholar]
- Luchetti S., Bossers K., Van de Bilt S., Agrapart V., Morales R. R., Frajese G. V., et al. (2011). Neurosteroid biosynthetic pathways changes in prefrontal cortex in Alzheimer's disease. Neurobiol. Aging 32, 1964–1976. 10.1016/j.neurobiolaging.2009.12.014 [DOI] [PubMed] [Google Scholar]
- Lundin E., Wirgin I., Lukanova A., Afanasyeva Y., Krogh V., Axelsson T., et al. (2012). Selected polymorphisms in sex hormone-related genes, circulating sex hormones and risk of endometrial cancer. Cancer Epidemiol. 36, 445–452. 10.1016/j.canep.2012.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo L., Deng J., Wang D. X., He J., Deng W. (2015). Regulation of epithelial sodium channel expression by oestradiol and progestogen in alveolar epithelial cells. Respir. Physiol. Neurobiol. 216, 52–62. 10.1016/j.resp.2015.06.001 [DOI] [PubMed] [Google Scholar]
- Luu-The V., Belanger A., Labrie F. (2008). Androgen biosynthetic pathways in the human prostate. Best Pract. Res. Clin. Endocrinol. Metab. 22, 207–221. 10.1016/j.beem.2008.01.008 [DOI] [PubMed] [Google Scholar]
- Luu-The V., Labrie F. (2010). The intracrine sex steroid biosynthesis pathways. Prog. Brain Res. 181, 177–192. 10.1016/S0079-6123(08)81010-2 [DOI] [PubMed] [Google Scholar]
- Ma B. B., Oza A., Eisenhauer E., Stanimir G., Carey M., Chapman W., et al. (2004). The activity of letrozole in patients with advanced or recurrent endometrial cancer and correlation with biological markers–a study of the National Cancer Institute of Canada Clinical Trials Group. Int. J. Gynecol. Cancer 14, 650–658. 10.1111/j.1048-891X.2004.14419.x [DOI] [PubMed] [Google Scholar]
- Ma W. G., Song H., Das S. K., Paria B. C., Dey S. K. (2003). Estrogen is a critical determinant that specifies the duration of the window of uterine receptivity for implantation. Proc. Natl. Acad. Sci. U.S.A. 100, 2963–2968. 10.1073/pnas.0530162100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKenzie S. M., Dewar D., Stewart W., Fraser R., Connell J. M., Davies E. (2008). The transcription of steroidogenic genes in the human cerebellum and hippocampus: a comparative survey of normal and Alzheimer's tissue. J. Endocrinol. 196, 123–130. 10.1677/JOE-07-0427 [DOI] [PubMed] [Google Scholar]
- Maentausta O., Peltoketo H., Isomaa V., Jouppila P., Vihko R. (1990). Immunological measurement of human 17β-hydroxysteroid dehydrogenase. J. Steroid. Biochem. 36, 673–680. [DOI] [PubMed] [Google Scholar]
- Mäentausta O., Sormunen R., Isomaa V., Lehto V. P., Jouppila P., Vihko R. (1991). Immunohistochemical localization of 17 beta-hydroxysteroid dehydrogenase in the human endometrium during the menstrual cycle. Lab. Invest. 65, 582–587. [PubMed] [Google Scholar]
- Mahendroo M. S., Cala K. M., Hess D. L., Russell D. W. (2001). Unexpected virilization in male mice lacking steroid 5 alpha-reductase enzymes. Endocrinology 142, 4652–4662. 10.1210/endo.142.11.8510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahendroo M. S., Cala K. M., Russell D. W. (1996). 5 alpha-reduced androgens play a key role in murine parturition. Mol. Endocrinol. 10, 380–392. [DOI] [PubMed] [Google Scholar]
- Maia H., Jr., Pimentel K., Casoy J., Correia T., Freitas L. A., Zausner B., et al. (2007). Aromatase expression in the eutopic endometrium of myomatous uteri: the influence of the menstrual cycle and oral contraceptive use. Gynecol. Endocrinol. 23, 320–324. 10.1080/09513590701321565 [DOI] [PubMed] [Google Scholar]
- Maia H., Jr., Pimentel K., Silva T. M., Freitas L. A., Zausner B., Athayde C., et al. (2006). Aromatase and cyclooxygenase-2 expression in endometrial polyps during the menstrual cycle. Gynecol. Endocrinol. 22, 219–224. 10.1080/09513590600585955 [DOI] [PubMed] [Google Scholar]
- Maltais R., Poirier D. (2011). Steroid sulfatase inhibitors: a review covering the promising 2000-2010 decade. Steroids 76, 929–948. 10.1016/j.steroids.2011.03.010 [DOI] [PubMed] [Google Scholar]
- Manenda M. S., Hamel C. J., Masselot-Joubert L., Picard M. E., Shi R. (2016). Androgen-metabolizing enzymes: A structural perspective. J. Steroid Biochem. Mol. Biol. 161, 54–72. 10.1016/j.jsbmb.2016.02.021 [DOI] [PubMed] [Google Scholar]
- Marchais-Oberwinkler S., Wetzel M., Ziegler E., Kruchten P., Werth R., Henn C., et al. (2011). New drug-like hydroxyphenylnaphthol steroidomimetics as potent and selective 17β-hydroxysteroid dehydrogenase type 1 inhibitors for the treatment of estrogen-dependent diseases. J. Med. Chem. 54, 534–547. 10.1021/jm1009082 [DOI] [PubMed] [Google Scholar]
- Masi L., Becherini L., Gennari L., Amedei A., Colli E., Falchetti A., et al. (2001). Polymorphism of the aromatase gene in postmenopausal Italian women: distribution and correlation with bone mass and fracture risk. J. Clin. Endocrinol. Metab. 86, 2263–2269. 10.1210/jc.86.5.2263 [DOI] [PubMed] [Google Scholar]
- Matsunaga T., Hojo A., Yamane Y., Endo S., El-Kabbani O., Hara A. (2013). Pathophysiological roles of aldo-keto reductases (AKR1C1 and AKR1C3) in development of cisplatin resistance in human colon cancers. Chem. Biol. Interact. 202, 234–242. 10.1016/j.cbi.2012.09.024 [DOI] [PubMed] [Google Scholar]
- Matsuzaki S., Canis M., Pouly J. L., Dechelotte P. J., Mage G. (2006). Analysis of aromatase and 17β-hydroxysteroid dehydrogenase type 2 messenger ribonucleic acid expression in deep endometriosis and eutopic endometrium using laser capture microdissection. Fertil. Steril. 85, 308–313. 10.1016/j.fertnstert.2005.08.017 [DOI] [PubMed] [Google Scholar]
- Mauvais-Jarvis F., Clegg D. J., Hevener A. L. (2013). The role of estrogens in control of energy balance and glucose homeostasis. Endocr. Rev. 34, 309–338. 10.1210/er.2012-1055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy M. (2000). The “gender gap” in autoimmune disease. Lancet 356, 1088 10.1016/S0140-6736(05)74535-9 [DOI] [PubMed] [Google Scholar]
- McEwen B. S., Milner T. A. (2017). Understanding the broad influence of sex hormones and sex differences in the brain. J. Neurosci. Res. 95, 24–39. 10.1002/jnr.23809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijer D., Gelderblom H., Karperien M., Cleton-Jansen A. M., Hogendoorn P. C., Bovee J. V. (2011). Expression of aromatase and estrogen receptor alpha in chondrosarcoma, but no beneficial effect of inhibiting estrogen signaling both in vitro and in vivo. Clin. Sarcoma Res. 1:5. 10.1186/2045-3329-1-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meloche C. A., Falany C. N. (2001). Expression and characterization of the human 3 beta-hydroxysteroid sulfotransferases (SULT2B1a and SULT2B1b). J. Steroid Biochem. Mol. Biol. 77, 261–269. 10.1016/S0960-0760(01)00064-4 [DOI] [PubMed] [Google Scholar]
- Miki Y., Nakata T., Suzuki T., Darnel A. D., Moriya T., Kaneko C., et al. (2002). Systemic distribution of steroid sulfatase and estrogen sulfotransferase in human adult and fetal tissues. J. Clin. Endocrinol. Metab. 87, 5760–5768. 10.1210/jc.2002-020670 [DOI] [PubMed] [Google Scholar]
- Milewich L., Garcia R. L., Johnson A. R. (1983). Steroid sulfatase activity in human lung tissue and in endothelial pulmonary cells in culture. J. Clin. Endocrinol. Metab. 57, 8–14. 10.1210/jcem-57-1-8 [DOI] [PubMed] [Google Scholar]
- Miller P. B., Parnell B. A., Bushnell G., Tallman N., Forstein D. A., Higdon H. L, III., et al. (2012a). Endometrial receptivity defects during IVF cycles with and without letrozole. Hum. Reprod. 27, 881–888. 10.1093/humrep/der452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller V. L., Lin H. K., Murugan P., Fan M., Penning T. M., Brame L. S., et al. (2012b). Aldo-keto reductase family 1 member C3 (AKR1C3) is expressed in adenocarcinoma and squamous cell carcinoma but not small cell carcinoma. Int. J. Clin. Exp. Pathol. 5, 278–289. [PMC free article] [PubMed] [Google Scholar]
- Miller W. L., Auchus R. J. (2011). The molecular biology, biochemistry, and physiology of human steroidogenesis and its disorders. Endocr. Rev. 32, 81–151. 10.1210/er.2010-0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindnich R., Moller G., Adamski J. (2004). The role of 17 beta-hydroxysteroid dehydrogenases. Mol. Cell. Endocrinol. 218, 7–20. 10.1016/j.mce.2003.12.006 [DOI] [PubMed] [Google Scholar]
- Miyaura C., Toda K., Inada M., Ohshiba T., Matsumoto C., Okada T., et al. (2001). Sex- and age-related response to aromatase deficiency in bone. Biochem. Biophys. Res. Commun. 280, 1062–1068. 10.1006/bbrc.2001.4246 [DOI] [PubMed] [Google Scholar]
- Moeller G., Adamski J. (2006). Multifunctionality of human 17β-hydroxysteroid dehydrogenases. Mol. Cell. Endocrinol. 248, 47–55. 10.1016/j.mce.2005.11.031 [DOI] [PubMed] [Google Scholar]
- Moeller G., Adamski J. (2009). Integrated view on 17β-hydroxysteroid dehydrogenases. Mol. Cell. Endocrinol. 301, 7–19. 10.1016/j.mce.2008.10.040 [DOI] [PubMed] [Google Scholar]
- Möller G., Leenders F., van Grunsven E. G., Dolez V., Qualmann B., Kessels M. M., et al. (1999). Characterization of the HSD17B4 gene: D-specific multifunctional protein 2/17β-hydroxysteroid dehydrogenase IV. J. Steroid Biochem. Mol. Biol. 69, 441–446. 10.1016/S0960-0760(99)00066-7 [DOI] [PubMed] [Google Scholar]
- Morgat A., Axelsen K. B., Lombardot T., Alcantara R., Aimo L., Zerara M., et al. (2015). Updates in Rhea–a manually curated resource of biochemical reactions. Nucleic Acids Res. 43, D459–D464. 10.1093/nar/gku961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mori T., Ito F., Matsushima H., Takaoka O., Koshiba A., Tanaka Y., et al. (2015). Dienogest reduces HSD17β1 expression and activity in endometriosis. J. Endocrinol. 225, 69–76. 10.1530/JOE-15-0052 [DOI] [PubMed] [Google Scholar]
- Morice P., Leary A., Creutzberg C., Abu-Rustum N., Darai E. (2015). Endometrial cancer. Lancet 387, 1094–1108. 10.1016/S0140-6736(15)00130-0 [DOI] [PubMed] [Google Scholar]
- Morishima A., Grumbach M. M., Simpson E. R., Fisher C., Qin K. (1995). Aromatase deficiency in male and female siblings caused by a novel mutation and the physiological role of estrogens. J. Clin. Endocrinol. Metab. 80, 3689–3698. [DOI] [PubMed] [Google Scholar]
- Mueller J. W., Gilligan L. C., Idkowiak J., Arlt W., Foster P. A. (2015). The regulation of steroid action by sulfation and desulfation. Endocr. Rev. 36, 526–563. 10.1210/er.2015-1036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muir M., Romalo G., Wolf L., Elger W., Schweikert H. U. (2004). Estrone sulfate is a major source of local estrogen formation in human bone. J. Clin. Endocrinol. Metab. 89, 4685–4692. 10.1210/jc.2004-0049 [DOI] [PubMed] [Google Scholar]
- Mukai H., Tsurugizawa T., Ogiue-Ikeda M., Murakami G., Hojo Y., Ishii H., et al. (2006). Local neurosteroid production in the hippocampus: influence on synaptic plasticity of memory. Neuroendocrinology 84, 255–263. 10.1159/000097747 [DOI] [PubMed] [Google Scholar]
- Mullis P. E., Yoshimura N., Kuhlmann B., Lippuner K., Jaeger P., Harada H. (1997). Aromatase deficiency in a female who is compound heterozygote for two new point mutations in the P450arom gene: impact of estrogens on hypergonadotropic hypogonadism, multicystic ovaries, and bone densitometry in childhood. J. Clin. Endocrinol. Metab. 82, 1739–1745. 10.1210/jc.82.6.1739 [DOI] [PubMed] [Google Scholar]
- Munroe D. G., Chang P. L. (1987). Tissue-specific expression of human arylsulfatase-C isozymes and steroid sulfatase. Am. J. Hum. Genet. 40, 102–114. [PMC free article] [PubMed] [Google Scholar]
- Murakami G., Tanabe N., Ishii H. T., Ogiue-Ikeda M., Tsurugizawa T., Mukai H., et al. (2006). Role of cytochrome p450 in synaptocrinology: endogenous estrogen synthesis in the brain hippocampus. Drug Metab. Rev. 38, 353–369. 10.1080/03602530600724068 [DOI] [PubMed] [Google Scholar]
- Musatov S., Chen W., Pfaff D. W., Mobbs C. V., Yang X. J., Clegg D. J., et al. (2007). Silencing of estrogen receptor alpha in the ventromedial nucleus of hypothalamus leads to metabolic syndrome. Proc. Natl. Acad. Sci. U.S.A. 104, 2501–2506. 10.1073/pnas.0610787104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadal A., Alonso-Magdalena P., Soriano S., Ripoll C., Fuentes E., Quesada I., et al. (2011). Role of estrogen receptors alpha, beta and GPER1/GPR30 in pancreatic beta-cells. Front Biosci (Landmark Ed) 16, 251–260. 10.2741/3686 [DOI] [PubMed] [Google Scholar]
- Naftolin F., Horvath T. L., Jakab R. L., Leranth C., Harada N., Balthazart J. (1996). Aromatase immunoreactivity in axon terminals of the vertebrate brain. An immunocytochemical study on quail, rat, monkey and human tissues. Neuroendocrinology 63, 149–155. 10.1159/000126951 [DOI] [PubMed] [Google Scholar]
- Naftolin F., MacLusky N. J. (1982). Aromatase in the central nervous system. Cancer Res 42, 3274s–3276s. [PubMed] [Google Scholar]
- Nakarai C., Osawa K., Akiyama M., Matsubara N., Ikeuchi H., Yamano T., et al. (2015). Expression of AKR1C3 and CNN3 as markers for detection of lymph node metastases in colorectal cancer. Clin. Exp. Med. 15, 333–341. 10.1007/s10238-014-0298-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayeb-Hashemi H., Kaunitz J. D. (2009). Gastroduodenal mucosal defense. Curr. Opin. Gastroenterol. 25, 537–543. 10.1097/MOG.0b013e328330da7b [DOI] [PubMed] [Google Scholar]
- Nemoto Y., Toda K., Ono M., Fujikawa-Adachi K., Saibara T., Onishi S., et al. (2000). Altered expression of fatty acid-metabolizing enzymes in aromatase-deficient mice. J. Clin. Invest. 105, 1819–1825. 10.1172/JCI9575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niikawa H., Suzuki T., Miki Y., Suzuki S., Nagasaki S., Akahira J., et al. (2008). Intratumoral estrogens and estrogen receptors in human non-small cell lung carcinoma. Clin. Cancer Res. 14, 4417–4426. 10.1158/1078-0432.CCR-07-1950 [DOI] [PubMed] [Google Scholar]
- Nishimura M., Naito S. (2006). Tissue-specific mRNA expression profiles of human phase I metabolizing enzymes except for cytochrome P450 and phase II metabolizing enzymes. Drug Metab. Pharmacokinet. 21, 357–374. 10.2133/dmpk.21.357 [DOI] [PubMed] [Google Scholar]
- Noble L. S., Simpson E. R., Johns A., Bulun S. E. (1996). Aromatase expression in endometriosis. J. Clin. Endocrinol. Metab. 81, 174–179. [DOI] [PubMed] [Google Scholar]
- Noble L. S., Takayama K., Zeitoun K. M., Putman J. M., Johns D. A., Hinshelwood M. M., et al. (1997). Prostaglandin E2 stimulates aromatase expression in endometriosis-derived stromal cells. J. Clin. Endocrinol. Metab. 82, 600–606. 10.1210/jc.82.2.600 [DOI] [PubMed] [Google Scholar]
- Noël J. C., Anaf V., Borghese B., Vaiman D., Fayt I., Chapron C. (2011). The steroidogenic factor-1 protein is not expressed in various forms of endometriosis but is strongly present in ovarian cortical or medullary mesenchymatous cells adjacent to endometriotic foci. Fertil. Steril. 95, 2655–2657. 10.1016/j.fertnstert.2011.01.131 [DOI] [PubMed] [Google Scholar]
- Nokelainen P., Peltoketo H., Mustonen M., Vihko P. (2000). Expression of mouse 17β-hydroxysteroid dehydrogenase/17-ketosteroid reductase type 7 in the ovary, uterus, and placenta: localization from implantation to late pregnancy. Endocrinology 141, 772–778. 10.1210/endo.141.2.7309 [DOI] [PubMed] [Google Scholar]
- Oduwole O. O., Isomaa V. V., Nokelainen P. A., Stenback F., Vihko P. T. (2002). Downregulation of estrogen-metabolizing 17 beta-hydroxysteroid dehydrogenase type 2 expression correlates inversely with Ki67 proliferation marker in colon-cancer development. Int. J. Cancer 97, 1–6. 10.1002/ijc.1567 [DOI] [PubMed] [Google Scholar]
- Oduwole O. O., Makinen J. M., Isomaa V. V., Karttunen T. J., Vihko P. T. (2003a). Sex steroid metabolism in human gastric mucosa: 17 beta-hydroxysteroid dehydrogenase type 2 in normal, inflamed and neoplastic gastric tissues. Anticancer Res. 23, 3889–3897. [PubMed] [Google Scholar]
- Oduwole O. O., Makinen M. J., Isomaa V. V., Pulkka A., Jernvall P., Karttunen T. J., et al. (2003b). 17β-hydroxysteroid dehydrogenase type 2: independent prognostic significance and evidence of estrogen protection in female patients with colon cancer. J. Steroid Biochem. Mol. Biol. 87, 133–140. 10.1016/j.jsbmb.2003.08.008 [DOI] [PubMed] [Google Scholar]
- Ohno S., Nishikawa K., Honda Y., Nakajin S. (2008). Expression in E. coli and tissue distribution of the human homologue of the mouse Ke 6 gene, 17β-hydroxysteroid dehydrogenase type 8. Mol. Cell. Biochem. 309, 209–215. 10.1007/s11010-007-9637-9 [DOI] [PubMed] [Google Scholar]
- Olson S. H., Bandera E. V., Orlow I. (2007). Variants in estrogen biosynthesis genes, sex steroid hormone levels, and endometrial cancer: a HuGE review. Am. J. Epidemiol. 165, 235–245. 10.1093/aje/kwk015 [DOI] [PubMed] [Google Scholar]
- Osinski M., Wirstlein P., Wender-Ozegowska E., Mikolajczyk M., Jagodzinski P. P., Szczepanska M. (2018). HSD3B2, HSD17B1, HSD17B2, ESR1, ESR2 and AR expression in infertile women with endometriosis. Ginekol. Pol. 89, 125–134. 10.5603/GP.a2018.0022 [DOI] [PubMed] [Google Scholar]
- Oz O. K., Millsaps R., Welch R., Birch J., Zerwekh J. E. (2001). Expression of aromatase in the human growth plate. J. Mol. Endocrinol. 27, 249–253. 10.1677/jme.0.0270249 [DOI] [PubMed] [Google Scholar]
- Oz O. K., Zerwekh J. E., Fisher C., Graves K., Nanu L., Millsaps R., et al. (2000). Bone has a sexually dimorphic response to aromatase deficiency. J. Bone Miner. Res. 15, 507–514. 10.1359/jbmr.2000.15.3.507 [DOI] [PubMed] [Google Scholar]
- Palmer B. F., Clegg D. J. (2015). The sexual dimorphism of obesity. Mol. Cell. Endocrinol. 402, 113–119. 10.1016/j.mce.2014.11.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmieri C., Stein R. C., Liu X., Hudson E., Nicholas H., Sasano H., et al. (2017a). IRIS study: a phase II study of the steroid sulfatase inhibitor Irosustat when added to an aromatase inhibitor in ER-positive breast cancer patients. Breast Cancer Res. Treat. 165, 343–353. 10.1007/s10549-017-4328-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmieri C., Szydlo R., Miller M., Barker L., Patel N. H., Sasano H., et al. (2017b). IPET study: an FLT-PET window study to assess the activity of the steroid sulfatase inhibitor irosustat in early breast cancer. Breast Cancer Res. Treat. 166, 527–539. 10.1007/s10549-017-4427-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park A. L., Lin H. K., Yang Q., Sing C. W., Fan M., Mapstone T. B., et al. (2010). Differential expression of type 2, 3α/type 5, 17β-hydroxysteroid dehydrogenase (AKR1C3) in tumors of the central nervous system. Int. J. Clin. Exp. Pathol. 3, 743–754. [PMC free article] [PubMed] [Google Scholar]
- Park Y. S., Gauna A. E., Cha S. (2015). Mouse models of primary Sjogren's syndrome. Curr. Pharm. Des. 21, 2350–2364. 10.2174/1381612821666150316120024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathirage N., Di Nezza L. A., Salmonsen L. A., Jobling T., Simpson E. R., Clyne C. D. (2006). Expression of aromatase, estrogen receptors, and their coactivators in patients with endometrial cancer. Fertil. Steril. 86, 469–472. 10.1016/j.fertnstert.2005.12.057 [DOI] [PubMed] [Google Scholar]
- Pautier P., Vergote I., Joly F., Melichar B., Kutarska E., Hall G., et al. (2017). A Phase 2, randomized, open-label study of irosustat versus megestrol acetate in advanced endometrial cancer. Int. J. Gynecol. Cancer 27, 258–266. 10.1097/IGC.0000000000000862 [DOI] [PubMed] [Google Scholar]
- Pearson Murphy B. E., Steinberg S. I., Hu F. Y., Allison C. M. (2001). Neuroactive ring A-reduced metabolites of progesterone in human plasma during pregnancy: elevated levels of 5 alpha-dihydroprogesterone in depressed patients during the latter half of pregnancy. J. Clin. Endocrinol. Metab. 86, 5981–5987. 10.1210/jcem.86.12.8122 [DOI] [PubMed] [Google Scholar]
- Pelletier G., Luu-The V., Tetu B., Labrie F. (1999). Immunocytochemical localization of type 5, 17β-hydroxysteroid dehydrogenase in human reproductive tissues. J. Histochem. Cytochem. 47, 731–738. 10.1177/002215549904700602 [DOI] [PubMed] [Google Scholar]
- Penning T. M. (2017). Aldo-Keto Reductase (AKR) 1C3 inhibitors: a patent review. Expert Opin. Ther. Pat. 27, 1329–1340. 10.1080/13543776.2017.1379503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penning T. M., Burczynski M. E., Jez J. M., Hung C. F., Lin H. K., Ma H., et al. (2000). Human 3α-hydroxysteroid dehydrogenase isoforms (AKR1C1-AKR1C4) of the aldo-keto reductase superfamily: functional plasticity and tissue distribution reveals roles in the inactivation and formation of male and female sex hormones. Biochem. J. 351, 67–77. 10.1042/bj3510067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penning T. M., Jin Y., Steckelbroeck S., Lanisnik Rizner T., Lewis M. (2004). Structure-function of human 3 alpha-hydroxysteroid dehydrogenases: genes and proteins. Mol. Cell. Endocrinol. 215, 63–72. 10.1016/j.mce.2003.11.006 [DOI] [PubMed] [Google Scholar]
- Perez Carrion R., Alberola Candel V., Calabresi F., Michel R. T., Santos R., Delozier T., et al. (1994). Comparison of the selective aromatase inhibitor formestane with tamoxifen as first-line hormonal therapy in postmenopausal women with advanced breast cancer. Ann. Oncol. 5(Suppl. 7), S19–S24. [PubMed] [Google Scholar]
- Pezzi V., Mathis J. M., Rainey W. E., Carr B. R. (2003). Profiling transcript levels for steroidogenic enzymes in fetal tissues. J. Steroid Biochem. Mol. Biol. 87, 181–189. 10.1016/j.jsbmb.2003.07.006 [DOI] [PubMed] [Google Scholar]
- Piccinato C. A., Neme R. M., Torres N., Sanches L. R., Cruz Derogis P. B., Brudniewski H. F., et al. (2016a). Increased expression of CYP1A1 and CYP1B1 in ovarian/peritoneal endometriotic lesions. Reproduction 151, 683–692. 10.1530/REP-15-0581 [DOI] [PubMed] [Google Scholar]
- Piccinato C. A., Neme R. M., Torres N., Sanches L. R., Derogis P., Brudniewski H. F., et al. (2016b). Effects of steroid hormone on estrogen sulfotransferase and on steroid sulfatase expression in endometriosis tissue and stromal cells. J. Steroid Biochem. Mol. Biol. 158, 117–126. 10.1016/j.jsbmb.2015.12.025 [DOI] [PubMed] [Google Scholar]
- Piekorz R. P., Gingras S., Hoffmeyer A., Ihle J. N., Weinstein Y. (2005). Regulation of progesterone levels during pregnancy and parturition by signal transducer and activator of transcription 5 and 20α-hydroxysteroid dehydrogenase. Mol. Endocrinol. 19, 431–440. 10.1210/me.2004-0302 [DOI] [PubMed] [Google Scholar]
- Platia M. P., Fencl M. D., Elkind-Hirsch K. E., Canick J. A., Tulchinsky D. (1984). Estrone sulfatase activity in the human brain and estrone sulfate levels in the normal menstrual cycle. J. Steroid Biochem. 21, 237–241. 10.1016/0022-4731(84)90275-9 [DOI] [PubMed] [Google Scholar]
- Pohl O., Bestel E., Gotteland J. P. (2014). Synergistic effects of E2MATE and norethindrone acetate on steroid sulfatase inhibition: a randomized phase I proof-of-principle clinical study in women of reproductive age. Reprod. Sci. 21, 1256–1265. 10.1177/1933719114522526 [DOI] [PubMed] [Google Scholar]
- Pollow K., Lubbert H., Jeske R., Pollow B. (1975a). Studies on 17β-hydroxysteroid dehydrogenase in human endometrium and endometrial carcinoma. Acta Endocrinol. 79, 146–156. [DOI] [PubMed] [Google Scholar]
- Pollow K., Lubbert H., Pollow B. (1975b). Studies on 17 beta-hydroxysteroid dehydrogenase in human endometrium and endometrial carcinoma. III. Partial purification and characterization of the microsomal enzyme. Acta Endocrinol (Copenh) 80, 355–364. [PubMed] [Google Scholar]
- Pollow K., Lubbert H., Pollow B. (1976). On the mitochondrial 17β-hydroxysteroid dehydrogenase from human endometrium and endometrial carcinoma: characterization and intramitochondrial distribution. J. Steroid Biochem. 7, 45–50. 10.1016/0022-4731(76)90163-1 [DOI] [PubMed] [Google Scholar]
- Polow K., Lubbert H., Boquoi E., Kreutzer G., Jeske R., Pollow B. (1975). Studies on 17β-hydroxysteroid dehydrogenase in human endometrium and endometrial carcinoma I. Subcellular distribution and variations of specific enzyme activity. Acta Endocrinol (Copenh) 79, 134–145. [PubMed] [Google Scholar]
- Prehn C., Moller G., Adamski J. (2009). Recent advances in 17β-hydroxysteroid dehydrogenases. J. Steroid Biochem. Mol. Biol. 114, 72–77. 10.1016/j.jsbmb.2008.12.024 [DOI] [PubMed] [Google Scholar]
- Prizant H., Hammes S. R. (2016). Minireview: lymphangioleiomyomatosis (LAM): the “Other” steroid-sensitive cancer. Endocrinology 157, 3374–3383. 10.1210/en.2016-1395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prossnitz E. R., Barton M. (2011). The G-protein-coupled estrogen receptor GPER in health and disease. Nat. Rev. Endocrinol. 7, 715–726. 10.1038/nrendo.2011.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prost O., Adessi G. L. (1983). Estrone and dehydroepiandrosterone sulfatase activities in normal and pathological human endometrium biopsies. J. Clin. Endocrinol. Metab. 56, 653–661. 10.1210/jcem-56-4-653 [DOI] [PubMed] [Google Scholar]
- Purohit A., Flanagan A. M., Reed M. J. (1992). Estrogen synthesis by osteoblast cell lines. Endocrinology 131, 2027–2029. 10.1210/endo.131.4.1396346 [DOI] [PubMed] [Google Scholar]
- Purohit A., Foster P. A. (2012). Steroid sulfatase inhibitors for estrogen- and androgen-dependent cancers. J. Endocrinol. 212, 99–110. 10.1530/JOE-11-0266 [DOI] [PubMed] [Google Scholar]
- Purohit A., Fusi L., Brosens J., Woo L. W., Potter B. V., Reed M. J. (2008). Inhibition of steroid sulphatase activity in endometriotic implants by 667 COUMATE: a potential new therapy. Hum. Reprod. 23, 290–297. 10.1093/humrep/dem308 [DOI] [PubMed] [Google Scholar]
- Qaiser M. Z., Dolman D. E. M., Begley D. J., Abbott N. J., Cazacu-Davidescu M., Corol D. I., et al. (2017). Uptake and metabolism of sulphated steroids by the blood-brain barrier in the adult male rat. J. Neurochem. 142, 672–685. 10.1111/jnc.14117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian Y. M., Sun X. J., Tong M. H., Li X. P., Richa J., Song W. C. (2001). Targeted disruption of the mouse estrogen sulfotransferase gene reveals a role of estrogen metabolism in intracrine and paracrine estrogen regulation. Endocrinology 142, 5342–5350. 10.1210/endo.142.12.8540 [DOI] [PubMed] [Google Scholar]
- Qin K., Ehrmann D. A., Cox N., Refetoff S., Rosenfield R. L. (2006). Identification of a functional polymorphism of the human type 5, 17β-hydroxysteroid dehydrogenase gene associated with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 91, 270–276. 10.1210/jc.2005-2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinkler M., Sinha B., Tomlinson J. W., Bujalska I. J., Stewart P. M., Arlt W. (2004). Androgen generation in adipose tissue in women with simple obesity–a site-specific role for 17β-hydroxysteroid dehydrogenase type 5. J. Endocrinol. 183, 331–342. 10.1677/joe.1.05762 [DOI] [PubMed] [Google Scholar]
- Rajkowski K. M., Robel P., Baulieu E. E. (1997). Hydroxysteroid sulfotransferase activity in the rat brain and liver as a function of age and sex. Steroids 62, 427–436. 10.1016/S0039-128X(97)00013-5 [DOI] [PubMed] [Google Scholar]
- Rantakari P., Lagerbohm H., Kaimainen M., Suomela J. P., Strauss L., Sainio K., et al. (2010). Hydroxysteroid (17{beta}) dehydrogenase 12 is essential for mouse organogenesis and embryonic survival. Endocrinology 151, 1893–1901. 10.1210/en.2009-0929 [DOI] [PubMed] [Google Scholar]
- Rantakari P., Strauss L., Kiviranta R., Lagerbohm H., Paviala J., Holopainen I., et al. (2008). Placenta defects and embryonic lethality resulting from disruption of mouse hydroxysteroid (17-beta) dehydrogenase 2 gene. Mol. Endocrinol. 22, 665–675. 10.1210/me.2007-0257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauschenberger K., Scholer K., Sass J. O., Sauer S., Djuric Z., Rumig C., et al. (2010). A non-enzymatic function of 17β-hydroxysteroid dehydrogenase type 10 is required for mitochondrial integrity and cell survival. EMBO Mol. Med. 2, 51–62. 10.1002/emmm.200900055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawłuszko A. A., Horbacka K., Krokowicz P., Jagodzinski P. P. (2011). Decreased expression of 17β-hydroxysteroid dehydrogenase type 1 is associated with DNA hypermethylation in colorectal cancer located in the proximal colon. BMC Cancer 11:522. 10.1186/1471-2407-11-522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy D. S. (2010). Neurosteroids: endogenous role in the human brain and therapeutic potentials. Prog. Brain Res. 186, 113–137. 10.1016/B978-0-444-53630-3.00008-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed M. J., Purohit A., Woo L. W., Newman S. P., Potter B. V. (2005). Steroid sulfatase: molecular biology, regulation, and inhibition. Endocr. Rev. 26, 171–202. 10.1210/er.2004-0003 [DOI] [PubMed] [Google Scholar]
- Rege J., Karashima S., Lerario A. M., Smith J. M., Auchus R. J., Kasa-Vubu J. Z., et al. (2016). Age-dependent increases in adrenal cytochrome b5 and serum 5-androstenediol-3-sulfate. J. Clin. Endocrinol. Metab. 101, 4585–4593. 10.1210/jc.2016-2864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rennert G., Rennert H. S., Pinchev M., Lavie O., Gruber S. B. (2009). Use of hormone replacement therapy and the risk of colorectal cancer. J. Clin. Oncol. 27, 4542–4547. 10.1200/JCO.2009.22.0764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee H. S., Oh S. H., Ko B. J., Han D. M., Jeon B. H., Park H., et al. (2003). Expression of 3β-hydroxysteroid dehydrogenase and P450 side chain cleavage enzyme in the human uterine endometrium. Exp. Mol. Med. 35, 160–166. 10.1038/emm.2003.22 [DOI] [PubMed] [Google Scholar]
- Riches Z., Stanley E. L., Bloomer J. C., Coughtrie M. W. (2009). Quantitative evaluation of the expression and activity of five major sulfotransferases (SULTs) in human tissues: the SULT “pie”. Drug Metab. Dispos. 37, 2255–2261. 10.1124/dmd.109.028399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggs B. L., Khosla S., Melton L. J., III. (2002). Sex steroids and the construction and conservation of the adult skeleton. Endocr. Rev. 23, 279–302. 10.1210/edrv.23.3.0465 [DOI] [PubMed] [Google Scholar]
- Rižner T. L. (2013). Estrogen biosynthesis, phase I and phase II metabolism, and action in endometrial cancer. Mol. Cell. Endocrinol. 381, 124–139. 10.1016/j.mce.2013.07.026 [DOI] [PubMed] [Google Scholar]
- Rižner T. L. (2016). The important roles of steroid sulfatase and sulfotransferases in gynecological diseases. Front. Pharmacol. 7:30. 10.3389/fphar.2016.00030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rižner T. L., Penning T. M. (2014). Role of aldo-keto reductase family 1 (AKR1) enzymes in human steroid metabolism. Steroids 79, 49–63. 10.1016/j.steroids.2013.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizner T. L., Smuc T., Rupreht R., Sinkovec J., Penning T. M. (2006). AKR1C1 and AKR1C3 may determine progesterone and estrogen ratios in endometrial cancer. Mol. Cell. Endocrinol. 248, 126–135. 10.1016/j.mce.2005.10.009 [DOI] [PubMed] [Google Scholar]
- Rižner T. L., Thalhammer T., Ozvegy-Laczka C. (2017). The importance of steroid uptake and intracrine action in endometrial and ovarian cancers. Front. Pharmacol. 8:346. 10.3389/fphar.2017.00346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Sanz M., Garcia-Giralt N., Prieto-Alhambra D., Servitja S., Balcells S., Pecorelli R., et al. (2015). CYP11A1 expression in bone is associated with aromatase inhibitor-related bone loss. J. Mol. Endocrinol. 55, 69–79. 10.1530/JME-15-0079 [DOI] [PubMed] [Google Scholar]
- Rose P. G., Brunetto V. L., VanLe L., Bell J., Walker J. L., Lee R. B. (2000). A phase II trial of anastrozole in advanced recurrent or persistent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol. Oncol. 78, 212–216. 10.1006/gyno.2000.5865 [DOI] [PubMed] [Google Scholar]
- Roshan M. H., Tambo A., Pace N. P. (2016). The role of testosterone in colorectal carcinoma: pathomechanisms and open questions. EPMA J. 7, 22. 10.1186/s13167-016-0071-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosner W., Hankinson S. E., Sluss P. M., Vesper H. W., Wierman M. E. (2013). Challenges to the measurement of estradiol: an endocrine society position statement. J. Clin. Endocrinol. Metab. 98, 1376–1387. 10.1210/jc.2012-3780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin G. L., Harrold A. J., Mills J. A., Falany C. N., Coughtrie M. W. (1999). Regulation of sulphotransferase expression in the endometrium during the menstrual cycle, by oral contraceptives and during early pregnancy. Mol. Hum. Reprod. 5, 995–1002. 10.1093/molehr/5.11.995 [DOI] [PubMed] [Google Scholar]
- Sahu B., Sun W., Perusek L., Parmar V., Le Y. Z., Griswold M. D., et al. (2015). Conditional ablation of retinol dehydrogenase 10 in the retinal pigmented epithelium causes delayed dark adaption in mice. J. Biol. Chem. 290, 27239–27247. 10.1074/jbc.M115.682096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito H., Yanaihara T. (1998). Steroid formation in osteoblast-like cells. J. Int. Med. Res. 26, 1–12. 10.1177/030006059802600101 [DOI] [PubMed] [Google Scholar]
- Saitoh Y., Sasano H., Naganuma H., Ohtani H., Sasano N., Ohuchi A., et al. (1992). De novo expression of aromatase in gastric carcinoma. Light and electron microscopic immunohistochemical and immunoblot study. Pathol. Res. Pract. 188, 53–60. 10.1016/S0344-0338(11)81156-8 [DOI] [PubMed] [Google Scholar]
- Sakiani S., Olsen N. J., Kovacs W. J. (2013). Gonadal steroids and humoral immunity. Nat. Rev. Endocrinol. 9, 56–62. 10.1038/nrendo.2012.206 [DOI] [PubMed] [Google Scholar]
- Sakurai N., Miki Y., Suzuki T., Watanabe K., Narita T., Ando K., et al. (2006). Systemic distribution and tissue localizations of human 17β-hydroxysteroid dehydrogenase type 12. J. Steroid Biochem. Mol. Biol. 99, 174–181. 10.1016/j.jsbmb.2006.01.010 [DOI] [PubMed] [Google Scholar]
- Salas S., Jezequel P., Campion L., Deville J. L., Chibon F., Bartoli C., et al. (2009). Molecular characterization of the response to chemotherapy in conventional osteosarcomas: predictive value of HSD17B10 and IFITM2. Int. J. Cancer 125, 851–860. 10.1002/ijc.24457 [DOI] [PubMed] [Google Scholar]
- Salman E. D., Faye-Petersen O., Falany C. N. (2011). Hydroxysteroid sulfotransferase 2B1b expression and localization in normal human brain. Horm. Mol. Biol. Clin. Investig. 8, 445–454. 10.1515/HMBCI.2011.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salman E. D., Kadlubar S. A., Falany C. N. (2009). Expression and localization of cytosolic sulfotransferase (SULT) 1A1 and SULT1A3 in normal human brain. Drug Metab. Dispos. 37, 706–709. 10.1124/dmd.108.025767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saloniemi T., Jarvensivu P., Koskimies P., Jokela H., Lamminen T., Ghaem-Maghami S., et al. (2010). Novel hydroxysteroid (17β) dehydrogenase 1 inhibitors reverse estrogen-induced endometrial hyperplasia in transgenic mice. Am. J. Pathol. 176, 1443–1451. 10.2353/ajpath.2010.090325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez-Guijo A., Neunzig J., Gerber A., Oji V., Hartmann M. F., Schuppe H. C., et al. (2016). Role of steroid sulfatase in steroid homeostasis and characterization of the sulfated steroid pathway: Evidence from steroid sulfatase deficiency. Mol. Cell. Endocrinol. 437, 142–153. 10.1016/j.mce.2016.08.019 [DOI] [PubMed] [Google Scholar]
- Sasano H., Takashashi K., Satoh F., Nagura H., Harada N. (1998). Aromatase in the human central nervous system. Clin. Endocrinol. (Oxf). 48, 325–329. 10.1046/j.1365-2265.1998.00390.x [DOI] [PubMed] [Google Scholar]
- Sasano H., Uzuki M., Sawai T., Nagura H., Matsunaga G., Kashimoto O., et al. (1997). Aromatase in human bone tissue. J. Bone Miner. Res. 12, 1416–1423. 10.1359/jbmr.1997.12.9.1416 [DOI] [PubMed] [Google Scholar]
- Sathish V., Martin Y. N., Prakash Y. S. (2015). Sex steroid signaling: implications for lung diseases. Pharmacol. Ther. 150, 94–108. 10.1016/j.pharmthera.2015.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato R., Suzuki T., Katayose Y., Miura K., Shiiba K., Miki Y., et al. (2012). Aromatase in colon carcinoma. Anticancer Res. 32, 3069–3075. [PubMed] [Google Scholar]
- Sato R., Suzuki T., Katayose Y., Miura K., Shiiba K., Tateno H., et al. (2009). Steroid sulfatase and estrogen sulfotransferase in colon carcinoma: regulators of intratumoral estrogen concentrations and potent prognostic factors. Cancer Res. 69, 914–922. 10.1158/0008-5472.CAN-08-0906 [DOI] [PubMed] [Google Scholar]
- Schweikert H. U., Wolf L., Romalo G. (1995). Oestrogen formation from androstenedione in human bone. Clin. Endocrinol. (Oxf). 43, 37–42. 10.1111/j.1365-2265.1995.tb01890.x [DOI] [PubMed] [Google Scholar]
- Scublinsky A., Marin C., Gurpide E. (1976). Localization of estradiol 17β dehydrogenase in human endometrium. J. Steroid Biochem. 7, 745–747. 10.1016/0022-4731(76)90174-6 [DOI] [PubMed] [Google Scholar]
- Segawa T., Shozu M., Murakami K., Kasai T., Shinohara K., Nomura K., et al. (2005). Aromatase expression in stromal cells of endometrioid endometrial cancer correlates with poor survival. Clin. Cancer Res. 11, 2188–2194. 10.1158/1078-0432.CCR-04-1859 [DOI] [PubMed] [Google Scholar]
- Selcer K. W., Difrancesca H. M. (2012). Characterization of steroid sulfatase in the MC3T3-E1 mouse pre-osteoblastic cell line. Steroids 77, 696–702. 10.1016/j.steroids.2012.02.024 [DOI] [PubMed] [Google Scholar]
- Setiawan V. W., Doherty J. A., Shu X. O., Akbari M. R., Chen C., De Vivo I., et al. (2009). Two estrogen-related variants in CYP19A1 and endometrial cancer risk: a pooled analysis in the epidemiology of endometrial cancer consortium. Cancer Epidemiol. Biomarkers Prev. 18, 242–247. 10.1158/1055-9965.EPI-08-0689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setiawan V. W., Hankinson S. E., Colditz G. A., Hunter D. J., De Vivo I. (2004). HSD17B1 gene polymorphisms and risk of endometrial and breast cancer. Cancer Epidemiol. Biomarkers Prev. 13, 213–219. 10.1158/1055-9965.EPI-03-0241 [DOI] [PubMed] [Google Scholar]
- Shang E., Lai K., Packer A. I., Paik J., Blaner W. S., de Morais Vieira M., et al. (2002). Targeted disruption of the mouse cis-retinol dehydrogenase gene: visual and nonvisual functions. J. Lipid Res. 43, 590–597. [PubMed] [Google Scholar]
- Shehu A., Mao J., Gibori G. B., Halperin J., Le J., Devi Y. S., et al. (2008). Prolactin receptor-associated protein/17β-hydroxysteroid dehydrogenase type 7 gene (Hsd17b7) plays a crucial role in embryonic development and fetal survival. Mol. Endocrinol. 22, 2268–2277. 10.1210/me.2008-0165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen Z., Peng Z., Sun Y., Vaananen H. K., Poutanen M. (2008). Overexpression of human hydroxysteroid (17β) dehydrogenase 2 induces disturbance in skeletal development in young male mice. J. Bone Miner. Res. 23, 1217–1226. 10.1359/jbmr.080322 [DOI] [PubMed] [Google Scholar]
- Shi L., Yang X., Dong X., Zhang B. (2016). Polymorphism of HSD17B1 Ser312Gly with Cancer Risk: Evidence from 66,147 Subjects. Twin Res. Hum. Genet. 19, 136–145. 10.1017/thg.2016.6 [DOI] [PubMed] [Google Scholar]
- Shim G. J., Warner M., Kim H. J., Andersson S., Liu L., Ekman J., et al. (2004). Aromatase-deficient mice spontaneously develop a lymphoproliferative autoimmune disease resembling Sjogren's syndrome. Proc. Natl. Acad. Sci. U.S.A. 101, 12628–12633. 10.1073/pnas.0405099101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizu K. (1979). Metabolism of [17-2H]pregnenolone into 5-[17β-2H, 17α-18O]androstene-3β, 17α-diol and other products by incubation with the microsomal fraction of boar testis under 18O2 atmosphere. Biochim. Biophys. Acta 575, 37–45. 10.1016/0005-2760(79)90128-0 [DOI] [PubMed] [Google Scholar]
- Shimodaira M., Nakayama T., Sato I., Sato N., Izawa N., Mizutani Y., et al. (2012). Estrogen synthesis genes CYP19A1, HSD3B1, and HSD3B2 in hypertensive disorders of pregnancy. Endocrine 42, 700–707. 10.1007/s12020-012-9699-7 [DOI] [PubMed] [Google Scholar]
- Shimodaira M., Nakayama T., Sato N., Aoi N., Sato M., Izumi Y., et al. (2010). Association of HSD3B1 and HSD3B2 gene polymorphisms with essential hypertension, aldosterone level, and left ventricular structure. Eur. J. Endocrinol. 163, 671–680. 10.1530/EJE-10-0428 [DOI] [PubMed] [Google Scholar]
- Siegfried J. M., Stabile L. P. (2014). Estrongenic steroid hormones in lung cancer. Semin. Oncol. 41, 5–16. 10.1053/j.seminoncol.2013.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simard J., Ricketts M. L., Gingras S., Soucy P., Feltus F. A., Melner M. H. (2005). Molecular biology of the 3β-hydroxysteroid dehydrogenase/Δ5-Δ4 isomerase gene family. Endocr. Rev. 26, 525–582. 10.1210/er.2002-0050 [DOI] [PubMed] [Google Scholar]
- Simard M., Plante J., Boucher M., Provost P. R., Tremblay Y. (2010). Type 2 and 5, 17β-hydroxysteroid dehydrogenases and androgen receptor in human fetal lungs. Mol. Cell. Endocrinol. 319, 79–87. 10.1016/j.mce.2009.12.007 [DOI] [PubMed] [Google Scholar]
- Simoens S., Dunselman G., Dirksen C., Hummelshoj L., Bokor A., Brandes I., et al. (2012). The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres. Hum. Reprod. 27, 1292–1299. 10.1093/humrep/des073 [DOI] [PubMed] [Google Scholar]
- Simoens S., Hummelshoj L., Dunselman G., Brandes I., Dirksen C., D'Hooghe T. (2011). Endometriosis cost assessment (the EndoCost study): a cost-of-illness study protocol. Gynecol. Obstet. Invest. 71, 170–176. 10.1159/000316055 [DOI] [PubMed] [Google Scholar]
- Singh M. M., Trivedi R. N., Chauhan S. C., Srivastava V. M., Makker A., Chowdhury S. R., et al. (1996). Uterine estradiol and progesterone receptor concentration, activities of certain antioxidant enzymes and dehydrogenases and histoarchitecture in relation to time of secretion of nidatory estrogen and high endometrial sensitivity in rat. J. Steroid Biochem. Mol. Biol. 59, 215–224. 10.1016/S0960-0760(96)00102-1 [DOI] [PubMed] [Google Scholar]
- Singhal N., Vatandoust S., Brown M. P. (2015). Phase II study evaluating efficacy and safety of everolimus with letrozole for management of advanced (unresectable or metastatic) non-small cell lung cancer after failure of platinum-based treatment: a preliminary analysis of toxicity. Cancer Chemother. Pharmacol. 75, 325–331. 10.1007/s00280-014-2644-0 [DOI] [PubMed] [Google Scholar]
- Sinreih M., Anko M., Zukunft S., Adamski J., Rizner T. L. (2014). Important roles of the AKR1C2 and SRD5A1 enzymes in progesterone metabolism in endometrial cancer model cell lines. Chem. Biol. Interact. 234, 297–308. 10.1016/j.cbi.2014.11.012 [DOI] [PubMed] [Google Scholar]
- Sinreih M., Hevir N., Rizner T. L. (2013). Altered expression of genes involved in progesterone biosynthesis, metabolism and action in endometrial cancer. Chem. Biol. Interact. 202, 210–217. 10.1016/j.cbi.2012.11.012 [DOI] [PubMed] [Google Scholar]
- Sinreih M., Knific T., Anko M., Hevir N., Vouk K., Jerin A., et al. (2017a). The significance of the sulfatase pathway for local estrogen formation in endometrial cancer. Front. Pharmacol. 8:368. 10.3389/fphar.2017.00368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinreih M., Stupar S., Cemazar L., Verdenik I., Frkovic Grazio S., Smrkolj S., et al. (2017b). STAR and AKR1B10 are down-regulated in high-grade endometrial cancer. J. Steroid Biochem. Mol. Biol.. 10.1016/j.jsbmb.2017.02.015 [DOI] [PubMed] [Google Scholar]
- Sivik T. (2012). Elucidating the Role of 17β Hydroxysteroid Dehydrogenase Type 14 in Normal Physiology and in Breast Cancer. Department of Clinical and Experimental Medicine: Linköping University (Linköping). [Google Scholar]
- Skjefstad K., Grindstad T., Khanehkenari M. R., Richardsen E., Donnem T., Kilvaer T., et al. (2016). Prognostic relevance of estrogen receptor α, β and aromatase expression in non-small cell lung cancer. Steroids 113, 5–13. 10.1016/j.steroids.2016.05.008 [DOI] [PubMed] [Google Scholar]
- Slominski A., Zbytek B., Nikolakis G., Manna P. R., Skobowiat C., Zmijewski M., et al. (2013). Steroidogenesis in the skin: implications for local immune functions. J. Steroid Biochem. Mol. Biol. 137, 107–123. 10.1016/j.jsbmb.2013.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slomovitz B. M., Jiang Y., Yates M. S., Soliman P. T., Johnston T., Nowakowski M., et al. (2015). Phase II study of everolimus and letrozole in patients with recurrent endometrial carcinoma. J. Clin. Oncol. 33, 930–936. 10.1200/JCO.2014.58.3401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A., Contreras C., Ko K. H., Chow J., Dong X., Tuo B., et al. (2008). Gender-specific protection of estrogen against gastric acid-induced duodenal injury: stimulation of duodenal mucosal bicarbonate secretion. Endocrinology 149, 4554–4566. 10.1210/en.2007-1597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith E. P., Boyd J., Frank G. R., Takahashi H., Cohen R. M., Specker B., et al. (1994). Estrogen resistance caused by a mutation in the estrogen-receptor gene in a man. N. Engl. J. Med. 331, 1056–1061. 10.1056/NEJM199410203311604 [DOI] [PubMed] [Google Scholar]
- Smuc T., Hevir N., Ribic-Pucelj M., Husen B., Thole H., Rizner T. L. (2009). Disturbed estrogen and progesterone action in ovarian endometriosis. Mol. Cell. Endocrinol. 301, 59–64. 10.1016/j.mce.2008.07.020 [DOI] [PubMed] [Google Scholar]
- Smuc T., Pucelj M. R., Sinkovec J., Husen B., Thole H., Lanisnik Rizner T. (2007). Expression analysis of the genes involved in estradiol and progesterone action in human ovarian endometriosis. Gynecol. Endocrinol. 23, 105–111. 10.1080/09513590601152219 [DOI] [PubMed] [Google Scholar]
- Smuc T., Rizner T. L. (2009). Aberrant pre-receptor regulation of estrogen and progesterone action in endometrial cancer. Mol. Cell. Endocrinol. 301, 74–82. 10.1016/j.mce.2008.09.019 [DOI] [PubMed] [Google Scholar]
- Smuc T., Rupreht R., Sinkovec J., Adamski J., Rizner T. L. (2006). Expression analysis of estrogen-metabolizing enzymes in human endometrial cancer. Mol. Cell. Endocrinol. 248, 114–117. 10.1016/j.mce.2005.10.013 [DOI] [PubMed] [Google Scholar]
- Soma K. K., Rendon N. M., Boonstra R., Albers H. E., Demas G. E. (2015). DHEA effects on brain and behavior: insights from comparative studies of aggression. J. Steroid Biochem. Mol. Biol. 145, 261–272. 10.1016/j.jsbmb.2014.05.011 [DOI] [PubMed] [Google Scholar]
- Soubhye J., Alard I. C., van Antwerpen P., Dufrasne F. (2015). Type 2, 17-beta hydroxysteroid dehydrogenase as a novel target for the treatment of osteoporosis. Future Med. Chem. 7, 1431–1456. 10.4155/fmc.15.74 [DOI] [PubMed] [Google Scholar]
- Steckelbroeck S., Jin Y., Gopishetty S., Oyesanmi B., Penning T. M. (2004a). Human cytosolic 3alpha-hydroxysteroid dehydrogenases of the aldo-keto reductase superfamily display significant 3beta-hydroxysteroid dehydrogenase activity: implications for steroid hormone metabolism and action. J. Biol. Chem. 279, 10784–10795. 10.1074/jbc.M313308200 [DOI] [PubMed] [Google Scholar]
- Steckelbroeck S., Lutjohann D., Bauman D. R., Ludwig M., Friedl A., Hans V. H., et al. (2010). Non-stereo-selective cytosolic human brain tissue 3-ketosteroid reductase is refractory to inhibition by AKR1C inhibitors. Biochim. Biophys. Act. 1801, 1221–1231. 10.1016/j.bbalip.2010.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steckelbroeck S., Nassen A., Ugele B., Ludwig M., Watzka M., Reissinger A., et al. (2004b). Steroid sulfatase (STS) expression in the human temporal lobe: enzyme activity, mRNA expression and immunohistochemistry study. J. Neurochem. 89, 403–417. 10.1046/j.1471-4159.2004.02336.x [DOI] [PubMed] [Google Scholar]
- Steckelbroeck S., Stoffel-Wagner B., Reichelt R., Schramm J., Bidlingmaier F., Siekmann L., et al. (1999). Characterization of 17β-hydroxysteroid dehydrogenase activity in brain tissue: testosterone formation in the human temporal lobe. J. Neuroendocrinol. 11, 457–464. 10.1046/j.1365-2826.1999.00363.x [DOI] [PubMed] [Google Scholar]
- Steckelbroeck S., Watzka M., Reichelt R., Hans V. H., Stoffel-Wagner B., Heidrich D. D., et al. (2001). Characterization of the 5α-reductase-3α-hydroxysteroid dehydrogenase complex in the human brain. J. Clin. Endocrinol. Metab. 86, 1324–1331. 10.1210/jcem.86.3.7325 [DOI] [PubMed] [Google Scholar]
- Steckelbroeck S., Watzka M., Reissinger A., Wegener-Toper P., Bidlingmaier F., Bliesener N., et al. (2003). Characterisation of estrogenic 17β-hydroxysteroid dehydrogenase (17β-HSD) activity in the human brain. J. Steroid Biochem. Mol. Biol. 86, 79–92. 10.1016/S0960-0760(03)00251-6 [DOI] [PubMed] [Google Scholar]
- Stelzer G., Rosen N., Plaschkes I., Zimmerman S., Twik M., Fishilevich S., et al. (2016). The GeneCards suite: from gene data mining to disease genome sequence analyses. Curr Protoc Bioinformatics 54, 1.30, 31–31, 30, 33. 10.1002/cpbi.5 [DOI] [PubMed] [Google Scholar]
- Stoffel-Wagner B. (2001). Neurosteroid metabolism in the human brain. Eur. J. Endocrinol. 145, 669–679. 10.1530/eje.0.1450669 [DOI] [PubMed] [Google Scholar]
- Stoffel-Wagner B., Beyenburg S., Watzka M., Blumcke I., Bauer J., Schramm J., et al. (2000). Expression of 5α-reductase and 3α-hydroxisteroid oxidoreductase in the hippocampus of patients with chronic temporal lobe epilepsy. Epilepsia 41, 140–147. 10.1111/j.1528-1157.2000.tb00133.x [DOI] [PubMed] [Google Scholar]
- Stoffel-Wagner B., Watzka M., Schramm J., Bidlingmaier F., Klingmuller D. (1999a). Expression of CYP19 (aromatase) mRNA in different areas of the human brain. J. Steroid Biochem. Mol. Biol. 70, 237–241. 10.1016/S0960-0760(99)00114-4 [DOI] [PubMed] [Google Scholar]
- Stoffel-Wagner B., Watzka M., Steckelbroeck S., Ludwig M., Clusmann H., Bidlingmaier F., et al. (2003). Allopregnanolone serum levels and expression of 5 alpha-reductase and 3 alpha-hydroxysteroid dehydrogenase isoforms in hippocampal and temporal cortex of patients with epilepsy. Epilepsy Res. 54, 11–19. 10.1016/S0920-1211(03)00036-6 [DOI] [PubMed] [Google Scholar]
- Stoffel-Wagner B., Watzka M., Steckelbroeck S., Schramm J., Bidlingmaier J. F., Klingmuller D. (1999b). Expression of 17β-hydroxysteroid dehydrogenase types 1, 2, 3 and 4 in the human temporal lobe. J. Endocrinol. 160, 119–126. 10.1677/joe.0.1600119 [DOI] [PubMed] [Google Scholar]
- Stoffel-Wagner B., Watzka M., Steckelbroeck S., Schwaab R., Schramm J., Bidlingmaier F., et al. (1998a). Expression of CYP19 (aromatase) mRNA in the human temporal lobe. Biochem. Biophys. Res. Commun. 244, 768–771. 10.1006/bbrc.1998.8337 [DOI] [PubMed] [Google Scholar]
- Stoffel-Wagner B., Watzka M., Steckelbroeck S., Wickert L., Schramm J., Romalo G., et al. (1998b). Expression of 5α-reductase in the human temporal lobe of children and adults. J. Clin. Endocrinol. Metab. 83, 3636–3642. [DOI] [PubMed] [Google Scholar]
- Strott C. A. (2002). Sulfonation and molecular action. Endocr. Rev. 23, 703–732. 10.1210/er.2001-0040 [DOI] [PubMed] [Google Scholar]
- Sudeshna T., Anand K., Medhamurthy R. (2013). Analysis of 20α-hydroxysteroid dehydrogenase expression in the corpus luteum of the buffalo cow: effect of prostaglandin F2-α treatment on circulating 20α-hydroxyprogesterone levels. Reprod. Biol. Endocrinol. 11:111 10.1186/1477-7827-11-111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun X. F., Ahmadi A., Arbman G., Wallin A., Asklid D., Zhang H. (2005). Polymorphisms in sulfotransferase 1A1 and glutathione S-transferase P1 genes in relation to colorectal cancer risk and patients' survival. World J. Gastroenterol. 11, 6875–6879. 10.3748/wjg.v11.i43.6875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svoboda M., Hamilton G., Thalhammer T. (2010). Steroid hormone metabolizing enzymes in benign and malignant human bone tumors. Expert Opin. Drug Metab. Toxicol. 6, 427–437. 10.1517/17425251003592129 [DOI] [PubMed] [Google Scholar]
- Svoboda M., Thalhammer T., Aust S., Arrich F., Assadian O., Toma C. D. (2007). Estrogen sulfotransferase (SULT1E1) expression in benign and malignant human bone tumors. J. Surg. Oncol. 95, 572–581. 10.1002/jso.20748 [DOI] [PubMed] [Google Scholar]
- Syed F., Khosla S. (2005). Mechanisms of sex steroid effects on bone. Biochem. Biophys. Res. Commun. 328, 688–696. 10.1016/j.bbrc.2004.11.097 [DOI] [PubMed] [Google Scholar]
- Taga S., Yoshida N., Sekiba K. (1990). Distribution and cyclic change of aromatase cytochrome P-450 activity in human uteri. J. Steroid Biochem. Mol. Biol. 37, 741–745. 10.1016/0960-0760(90)90359-S [DOI] [PubMed] [Google Scholar]
- Takeyama J., Suzuki T., Hirasawa G., Muramatsu Y., Nagura H., Iinuma K., et al. (2000). 17β-hydroxysteroid dehydrogenase type 1 and 2 expression in the human fetus. J. Clin. Endocrinol. Metab. 85, 410–416. 10.1210/jcem.85.1.6323 [DOI] [PubMed] [Google Scholar]
- Tanaka K., Kubushiro K., Iwamori Y., Okairi Y., Kiguchi K., Ishiwata I., et al. (2003). Estrogen sulfotransferase and sulfatase: Roles in the regulation of estrogen activity in human uterine endometrial carcinomas. Cancer Sci. 94, 871–876. 10.1111/j.1349-7006.2003.tb01369.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka K., Shimizu K., Kakegawa S., Ohtaki Y., Nagashima T., Kaira K., et al. (2016). Prognostic significance of aromatase and estrogen receptor beta expression in EGFR wild-type lung adenocarcinoma. Am. J. Transl. Res. 8, 81–97. [PMC free article] [PubMed] [Google Scholar]
- Tanaka S., Miki Y., Hashimoto C., Takagi K., Doe Z., Li B., et al. (2015). The role of 5α-reductase type 1 associated with intratumoral dihydrotestosterone concentrations in human endometrial carcinoma. Mol. Cell. Endocrinol. 401, 56–64. 10.1016/j.mce.2014.11.022 [DOI] [PubMed] [Google Scholar]
- Tang T., Li L., Tang J., Li Y., Lin W. Y., Martin F., et al. (2010). A mouse knockout library for secreted and transmembrane proteins. Nat. Biotechnol. 28, 749–755. 10.1038/nbt.1644 [DOI] [PubMed] [Google Scholar]
- Tangen I. L., Onyango T. B., Kopperud R., Berg A., Halle M. K., Oyan A. M., et al. (2016). Androgen receptor as potential therapeutic target in metastatic endometrial cancer. Oncotarget 7, 49289–49298. 10.18632/oncotarget.10334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangen I. L., Werner H. M., Berg A., Halle M. K., Kusonmano K., Trovik J., et al. (2014). Loss of progesterone receptor links to high proliferation and increases from primary to metastatic endometrial cancer lesions. Eur J Cancer 50, 3003–3010. 10.1016/j.ejca.2014.09.003 [DOI] [PubMed] [Google Scholar]
- Taniuchi S., Fujishima F., Miki Y., Abe K., Nakamura Y., Sato S., et al. (2014). Tissue concentrations of estrogens and aromatase immunolocalization in interstitial pneumonia of human lung. Mol. Cell. Endocrinol. 392, 136–143. 10.1016/j.mce.2014.05.016 [DOI] [PubMed] [Google Scholar]
- Tashiro A., Sasano H., Nishikawa T., Yabuki N., Muramatsu Y., Coughtrie M. W., et al. (2000). Expression and activity of dehydroepiandrosterone sulfotransferase in human gastric mucosa. J. Steroid Biochem. Mol. Biol. 72, 149–154. 10.1016/S0960-0760(00)00020-0 [DOI] [PubMed] [Google Scholar]
- Taveira-DaSilva A. M., Moss J. (2014). Management of lymphangioleiomyomatosis. F1000Prime Rep. 6, 116. 10.12703/P6-116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry K., McGrath M., Lee I. M., Buring J., De Vivo I. (2010). Genetic variation in CYP11A1 and StAR in relation to endometrial cancer risk. Gynecol. Oncol. 117, 255–259. 10.1016/j.ygyno.2010.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teubner W., Meinl W., Florian S., Kretzschmar M., Glatt H. (2007). Identification and localization of soluble sulfotransferases in the human gastrointestinal tract. Biochem. J. 404, 207–215. 10.1042/BJ20061431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiboutot D., Martin P., Volikos L., Gilliland K. (1998). Oxidative activity of the type 2 isozyme of 17β-hydroxysteroid dehydrogenase (17β-HSD) predominates in human sebaceous glands. J. Invest. Dermatol. 111, 390–395. 10.1046/j.1523-1747.1998.00322.x [DOI] [PubMed] [Google Scholar]
- Thompson D. J., O'Mara T. A., Glubb D. M., Painter J. N., Cheng T., Folkerd E., et al. (2016). CYP19A1 fine-mapping and Mendelian randomization: estradiol is causal for endometrial cancer. Endocr. Relat. Cancer 23, 77–91. 10.1530/ERC-15-0386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong M. H., Jiang H., Liu P., Lawson J. A., Brass L. F., Song W. C. (2005). Spontaneous fetal loss caused by placental thrombosis in estrogen sulfotransferase-deficient mice. Nat. Med. 11, 153–159. 10.1038/nm1184 [DOI] [PubMed] [Google Scholar]
- Törn S., Nokelainen P., Kurkela R., Pulkka A., Menjivar M., Ghosh S., et al. (2003). Production, purification, and functional analysis of recombinant human and mouse 17β-hydroxysteroid dehydrogenase type 7. Biochem. Biophys. Res. Commun. 305, 37–45. 10.1016/S0006-291X(03)00694-6 [DOI] [PubMed] [Google Scholar]
- Townsend E. A., Miller V. M., Prakash Y. S. (2012). Sex differences and sex steroids in lung health and disease. Endocr. Rev. 33, 1–47. 10.1210/er.2010-0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend E. A., Thompson M. A., Pabelick C. M., Prakash Y. S. (2010). Rapid effects of estrogen on intracellular Ca2+ regulation in human airway smooth muscle. Am. J. Physiol. Lung Cell. Mol. Physiol. 298 L521–530. 10.1152/ajplung.00287.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai S. J., Wu M. H., Lin C. C., Sun H. S., Chen H. M. (2001). Regulation of steroidogenic acute regulatory protein expression and progesterone production in endometriotic stromal cells. J. Clin. Endocrinol. Metab. 86, 5765–5773. 10.1210/jcem.86.12.8082 [DOI] [PubMed] [Google Scholar]
- Tseng L., Gurpide E. (1974). Estradiol and 20α-dihydroprogesterone dehydrogenase activities in human endometrium during the menstrual cycle. Endocrinology 94, 419–423. 10.1210/endo-94-2-419 [DOI] [PubMed] [Google Scholar]
- Tseng L., Gusberg S. B., Gurpide E. (1977). Estradiol receptor and 17 beta-dehydrogenase in normal and abnormal human endometrium. Ann. N. Y. Acad. Sci. 286, 190–198. 10.1111/j.1749-6632.1977.tb29416.x [DOI] [PubMed] [Google Scholar]
- Tseng L., Mazella J. (2002). Endometrial cell specific gene activation during implantation and early pregnancy. Front. Biosci. 7, d1566–d1574. 10.2741/A861 [DOI] [PubMed] [Google Scholar]
- Tseng L., Mazella J., Mann W. J., Chumas J. (1982). Estrogen synthesis in normal and malignant human endometrium. J. Clin. Endocrinol. Metab. 55, 1029–1031. 10.1210/jcem-55-5-1029 [DOI] [PubMed] [Google Scholar]
- Tsuchiya M., Nakao H., Katoh T., Sasaki H., Hiroshima M., Tanaka T., et al. (2005). Association between endometriosis and genetic polymorphisms of the estradiol-synthesizing enzyme genes HSD17B1 and CYP19. Hum. Reprod. 20, 974–978. 10.1093/humrep/deh726 [DOI] [PubMed] [Google Scholar]
- Tuo B., Wen G., Wei J., Liu X., Wang X., Zhang Y., et al. (2011). Estrogen regulation of duodenal bicarbonate secretion and sex-specific protection of human duodenum. Gastroenterology 141, 854–863. 10.1053/j.gastro.2011.05.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utsunomiya H., Ito K., Suzuki T., Kitamura T., Kaneko C., Nakata T., et al. (2004). Steroid sulfatase and estrogen sulfotransferase in human endometrial carcinoma. Clin. Cancer Res. 10, 5850–5856. 10.1158/1078-0432.CCR-04-0040 [DOI] [PubMed] [Google Scholar]
- Utsunomiya H., Suzuki T., Ito K., Moriya T., Konno R., Sato S., et al. (2003). The correlation between the response to progestogen treatment and the expression of progesterone receptor B and 17β-hydroxysteroid dehydrogenase type 2 in human endometrial carcinoma. Clin. Endocrinol. (Oxf). 58, 696–703. 10.1046/j.1365-2265.2003.01766.x [DOI] [PubMed] [Google Scholar]
- Utsunomiya H., Suzuki T., Kaneko C., Takeyama J., Nakamura J., Kimura K., et al. (2001). The analyses of 17β-hydroxysteroid dehydrogenase isozymes in human endometrial hyperplasia and carcinoma. J. Clin. Endocrinol. Metab. 86, 3436–3443. 10.1210/jcem.86.7.7661 [DOI] [PubMed] [Google Scholar]
- van der Eerden B. C., Lowik C. W., Wit J. M., Karperien M. (2004). Expression of estrogen receptors and enzymes involved in sex steroid metabolism in the rat tibia during sexual maturation. J. Endocrinol. 180, 457–467. 10.1677/joe.0.1800457 [DOI] [PubMed] [Google Scholar]
- Vanderschueren D., Gaytant J., Boonen S., Venken K. (2008). Androgens and bone. Curr. Opin. Endocrinol. Diabetes Obes. 15, 250–254. 10.1097/MED.0b013e3282fe6ca9 [DOI] [PubMed] [Google Scholar]
- Vani S., McDonald S. E., Williams A. R., Mason J. I., Thong K. J., Critchley H. O. (2007). Mid-luteal endometrial intracrinology following controlled ovarian hyperstimulation involving use of a gonadotrophin releasing hormone antagonist. Hum. Reprod. 22, 2981–2991. 10.1093/humrep/dem269 [DOI] [PubMed] [Google Scholar]
- Varlamov O., Bethea C. L., Roberts C. T., Jr. (2014). Sex-specific differences in lipid and glucose metabolism. Front. Endocrinol. (Lausanne). 5:241. 10.3389/fendo.2014.00241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasquez Y. M., DeMayo F. J. (2013). Role of nuclear receptors in blastocyst implantation. Semin. Cell Dev. Biol. 24, 724–735. 10.1016/j.semcdb.2013.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velasco I., Rueda J., Acien P. (2006). Aromatase expression in endometriotic tissues and cell cultures of patients with endometriosis. Mol. Hum. Reprod. 12, 377–381. 10.1093/molehr/gal041 [DOI] [PubMed] [Google Scholar]
- Vercellini P., Vigano P., Somigliana E., Fedele L. (2014). Endometriosis: pathogenesis and treatment. Nat. Rev. Endocrinol. 10, 261–275. 10.1038/nrendo.2013.255 [DOI] [PubMed] [Google Scholar]
- Verma M. K., Miki Y., Abe K., Suzuki T., Niikawa H., Suzuki S., et al. (2013). Intratumoral localization and activity of 17β-hydroxysteroid dehydrogenase type 1 in non-small cell lung cancer: a potent prognostic factor. J. Transl. Med. 11, 167. 10.1186/1479-5876-11-167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verma M. K., Miki Y., Sasano H. (2011). Aromatase in human lung carcinoma. Steroids 76, 759–764. 10.1016/j.steroids.2011.02.020 [DOI] [PubMed] [Google Scholar]
- Vidal O., Lindberg M. K., Hollberg K., Baylink D. J., Andersson G., Lubahn D. B., et al. (2000). Estrogen receptor specificity in the regulation of skeletal growth and maturation in male mice. Proc. Natl. Acad. Sci. U.S.A. 97, 5474–5479. 10.1073/pnas.97.10.5474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vouk K., Smuc T., Guggenberger C., Ribic-Pucelj M., Sinkovec J., Husen B., et al. (2011). Novel estrogen-related genes and potential biomarkers of ovarian endometriosis identified by differential expression analysis. J. Steroid Biochem. Mol. Biol. 125, 231–242. 10.1016/j.jsbmb.2011.03.010 [DOI] [PubMed] [Google Scholar]
- Walker V. R., Korach K. S. (2004). Estrogen receptor knockout mice as a model for endocrine research. ILAR J. 45, 455–461. 10.1093/ilar.45.4.455 [DOI] [PubMed] [Google Scholar]
- Wang F., Vihma V., Soronen J., Turpeinen U., Hamalainen E., Savolainen-Peltonen H., et al. (2013). 17β-Estradiol and estradiol fatty acyl esters and estrogen-converting enzyme expression in adipose tissue in obese men and women. J. Clin. Endocrinol. Metab. 98, 4923–4931. 10.1210/jc.2013-2605 [DOI] [PubMed] [Google Scholar]
- Wang H., Dey S. K. (2006). Roadmap to embryo implantation: clues from mouse models. Nat. Rev. Genet. 7, 185–199. 10.1038/nrg1808 [DOI] [PubMed] [Google Scholar]
- Wang X. Q., Aka J. A., Li T., Xu D., Doillon C. J., Lin S. X. (2017). Inhibition of 17β-hydroxysteroid dehydrogenase type 7 modulates breast cancer protein profile and enhances apoptosis by down-regulating GRP78. J. Steroid Biochem. Mol. Biol. 172, 188–197. 10.1016/j.jsbmb.2017.06.009 [DOI] [PubMed] [Google Scholar]
- Warren J. C., French A. P. (1965). DISTRIBUTION OF STEROID SULFATASE IN HUMAN TISSUES. J. Clin. Endocrinol. Metab. 25, 278–282. 10.1210/jcem-25-2-278 [DOI] [PubMed] [Google Scholar]
- Watanabe K., Sasano H., Harada N., Ozaki M., Niikura H., Sato S., et al. (1995). Aromatase in human endometrial carcinoma and hyperplasia. Immunohistochemical, in situ hybridization, and biochemical studies. Am. J. Pathol. 146, 491–500. [PMC free article] [PubMed] [Google Scholar]
- Watzka M., Bidlingmaier F., Schramm J., Klingmuller D., Stoffel-Wagner B. (1999). Sex- and age-specific differences in human brain CYP11A1 mRNA expression. J. Neuroendocrinol. 11, 901–905. 10.1046/j.1365-2826.1999.00407.x [DOI] [PubMed] [Google Scholar]
- Wishart D. S., Feunang Y. D., Guo A. C., Lo E. J., Marcu A., Grant J. R., et al. (2018). DrugBank 5.0: a major update to the DrugBank database for 2018. Nucleic Acids Res. 46, D1074–D1082. 10.1093/nar/gkx1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wishart D. S., Jewison T., Guo A. C., Wilson M., Knox C., Liu Y., et al. (2013). HMDB 3.0–the human metabolome database in 2013. Nucleic Acids Res. 41, D801–D807. 10.1093/nar/gks1065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wöhrle D., Barbi G., Schulz W., Steinbach P. (1990). Heterozygous expression of X-linked chondrodysplasia punctata. Complex chromosome aberration including deletion of MIC2 and STS. Hum. Genet. 86, 215–218. 10.1007/BF00197708 [DOI] [PubMed] [Google Scholar]
- Woo L. W., Purohit A., Potter B. V. (2011). Development of steroid sulfatase inhibitors. Mol. Cell. Endocrinol. 340, 175–185. 10.1016/j.mce.2010.12.035 [DOI] [PubMed] [Google Scholar]
- Wu H. C., Tuo B. G., Wu W. M., Gao Y., Xu Q. Q., Zhao K. (2008). Prevalence of peptic ulcer in dyspeptic patients and the influence of age, sex, and Helicobacter pylori infection. Dig. Dis. Sci. 53, 2650–2656. 10.1007/s10620-007-0177-7 [DOI] [PubMed] [Google Scholar]
- Xiao J., Zheng Y., Zhou Y., Zhang P., Wang J., Shen F., et al. (2014). Sulfotransferase SULT1A1 Arg213His polymorphism with cancer risk: a meta-analysis of 53 case-control studies. PLoS ONE 9:e106774. 10.1371/journal.pone.0106774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yague J. G., Azcoitia I., DeFelipe J., Garcia-Segura L. M., Munoz A. (2010). Aromatase expression in the normal and epileptic human hippocampus. Brain Res. 1315, 41–52. 10.1016/j.brainres.2009.09.111 [DOI] [PubMed] [Google Scholar]
- Yague J. G., Munoz A., de Monasterio-Schrader P., Defelipe J., Garcia-Segura L. M., Azcoitia I. (2006). Aromatase expression in the human temporal cortex. Neuroscience 138, 389–401. 10.1016/j.neuroscience.2005.11.054 [DOI] [PubMed] [Google Scholar]
- Yamaki J., Yamamoto T., Okada H. (1985). Aromatization of androstenedione by normal and neoplastic endometrium of the uterus. J. Steroid Biochem. 22, 63–66. 10.1016/0022-4731(85)90142-6 [DOI] [PubMed] [Google Scholar]
- Yamamoto T., Fukuoka M., Fujimoto Y., Kitawaki J., Nakakoshi M., Yoshihama M., et al. (1990a). Inhibitory effect of a new androstenedione derivative, 14α-hydroxy-4-androstene-3,6,17-trione (14α-OHAT) on aromatase activity of human uterine tumors. J. Steroid Biochem. 36, 517–21. 10.1016/0022-4731(90)90167-Q [DOI] [PubMed] [Google Scholar]
- Yamamoto T., Kitawaki J., Urabe M., Honjo H., Tamura T., Noguchi T., et al. (1993a). Estrogen productivity of endometrium and endometrial cancer tissue; influence of aromatase on proliferation of endometrial cancer cells. J. Steroid Biochem. Mol. Biol. 44, 463–468. 10.1016/0960-0760(93)90251-Q [DOI] [PubMed] [Google Scholar]
- Yamamoto T., Noguchi T., Tamura T., Kitawaki J., Okada H. (1993b). Evidence for estrogen synthesis in adenomyotic tissues. Am. J. Obstet. Gynecol. 169, 734–738. 10.1016/0002-9378(93)90654-2 [DOI] [PubMed] [Google Scholar]
- Yamamoto T., Urabe M., Naitoh K., Kitawaki J., Honjo H., Okada H. (1990b). Estrone sulfatase activity in human uterine leiomyoma. Gynecol. Oncol. 37, 315–318. 10.1016/0090-8258(90)90358-R [DOI] [PubMed] [Google Scholar]
- Yanaihara Yanaihara, T., Toma Y., Shimizu Y., Saito H., Okai T., et al. (2001). Localization and expression of steroid sulfatase in human fallopian tubes. Steroids 66, 87–91. 10.1016/S0039-128X(00)00204-X [DOI] [PubMed] [Google Scholar]
- Yang W., Wu G., Broeckel U., Smith C. A., Turner V., Haidar C. E., et al. (2016). Comparison of genome sequencing and clinical genotyping for pharmacogenes. Clin. Pharmacol. Ther. 100, 380–388. 10.1002/cpt.411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X. Y., Wu W. J., Yang C., Yang T., He J. D., Yang Z., et al. (2013). Association of HSD17B3 and HSD3B1 polymorphisms with acne vulgaris in Southwestern Han Chinese. Dermatology 227, 202–208. 10.1159/000353581 [DOI] [PubMed] [Google Scholar]
- Ye X. Y., Chen S. Y., Wu S., Yoon D. S., Wang H., Hong Z., et al. (2017). Discovery of Clinical Candidate 2-((2S,6S)-2-Phenyl-6-hydroxyadamantan-2-yl)-1-(3'-hydroxyazetidin-1-yl)ethanone [BMS-816336], an orally active novel selective 11β-Hydroxysteroid dehydrogenase type 1 inhibitor. J. Med. Chem. 60, 4932–4948. 10.1021/acs.jmedchem.7b00211 [DOI] [PubMed] [Google Scholar]
- Yu L., Romero D. G., Gomez-Sanchez C. E., Gomez-Sanchez E. P. (2002). Steroidogenic enzyme gene expression in the human brain. Mol. Cell. Endocrinol. 190, 9–17. 10.1016/S0303-7207(02)00041-2 [DOI] [PubMed] [Google Scholar]
- Yuchi Y., Cai Y., Legein B., De Groef S., Leuckx G., Coppens V., et al. (2015). Estrogen receptor α regulates β-cell formation during pancreas development and following injury. Diabetes 64, 3218–3228. 10.2337/db14-1798 [DOI] [PubMed] [Google Scholar]
- Zacher A., Kaulich K., Stepanow S., Wolter M., Kohrer K., Felsberg J., et al. (2016). Molecular diagnostics of gliomas using next generation sequencing of a glioma-tailored gene panel. Brain Pathol. 27, 146–159. 10.1111/bpa.12367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zakharov V., Lin H. K., Azzarello J., McMeekin S., Moore K. N., Penning T. M., et al. (2010). Suppressed expression of type 2, 3α/type 5, 17β-hydroxysteroid dehydrogenase (AKR1C3) in endometrial hyperplasia and carcinoma. Int. J. Clin. Exp. Pathol. 3, 608–617. [PMC free article] [PubMed] [Google Scholar]
- Zarrabeitia M. T., Hernandez J. L., Valero C., Zarrabeitia A., Amado J. A., Gonzalez-Macias J., et al. (2007). Adiposity, estradiol, and genetic variants of steroid-metabolizing enzymes as determinants of bone mineral density. Eur. J. Endocrinol. 156, 117–122. 10.1530/eje.1.02318 [DOI] [PubMed] [Google Scholar]
- Zeitoun K., Takayama K., Sasano H., Suzuki T., Moghrabi N., Andersson S., et al. (1998). Deficient 17β-hydroxysteroid dehydrogenase type 2 expression in endometriosis: failure to metabolize 17β-estradiol. J. Clin. Endocrinol. Metab. 83, 4474–4480. [DOI] [PubMed] [Google Scholar]
- Zeng C., Matsuda K., Jia W. H., Chang J., Kweon S. S., Xiang Y. B., et al. (2016). Identification of susceptibility loci and genes for colorectal cancer risk. Gastroenterology 150, 1633–1645. 10.1053/j.gastro.2016.02.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Yin Y., Niu X. M., Liu Y., Garfield D., Chen S. F., et al. (2013). CYP19A1 gene polymorphisms and risk of lung cancer. J. Int. Med. Res. 41, 735–742. 10.1177/0300060513477291 [DOI] [PubMed] [Google Scholar]
- Zhao H., Zhou L., Shangguan A. J., Bulun S. E. (2016). Aromatase expression and regulation in breast and endometrial cancer. J. Mol. Endocrinol. 57 R19–33. 10.1530/JME-15-0310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhongyi S., Rantakari P., Lamminen T., Toppari J., Poutanen M. (2007). Transgenic male mice expressing human hydroxysteroid dehydrogenase 2 indicate a role for the enzyme independent of its action on sex steroids. Endocrinology 148, 3827–3836. 10.1210/en.2007-0365 [DOI] [PubMed] [Google Scholar]
- Zwart W., Theodorou V., Kok M., Canisius S., Linn S., Carroll J. S. (2011). Oestrogen receptor-co-factor-chromatin specificity in the transcriptional regulation of breast cancer. EMBO J. 30, 4764–4776. 10.1038/emboj.2011.368 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.