Abstract
An inverted (intussuscepted) appendix is a rare finding, often mistaken for a polyp as it presents with vague symptoms. This can result in misdiagnosis and inappropriate management. Diagnosis is usually made through surgery. Rarely, endometriosis has been found as the cause of the intussusception. A 42-year-old woman presented with frequent loose stools over 2 years, an elevated calprotectin over 400 μg/g faeces (normal <110) and a serum C-reactive protein of 40 mg/l (normal <5 mg/l). Endoscopy showed an inverted appendix. Histopathology results showed inflammation and ulceration. Laparoscopic appendicectomy was performed successfully, and endometriosis was found on the inverted appendix. This is the first case reported of an inverted appendix containing endometriosis, in which the intussusception of the appendix has been diagnosed on endoscopy. This case highlights how endometriosis can involve just the appendix, without any involvement of reproductive organs. We suggest considering inverted appendix as a differential diagnosis when investigating caecal lesions.
Introduction
An inverted appendix, also referred to as intussusception, is rare, with a reported incidence of 0.01%. Endometriosis is the proliferation of endometrial tissue outside the endometrial cavity, classically involving pelvic organs and pelvic peritoneum. Rarely there can be intestinal involvement of endometriosis, reported to range from 3 to 34% [1]. An inverted appendix can be mistaken for a caecal polyp as in previous reports, which has resulted in polypectomy and colonic perforation [2]. It is usually diagnosed with surgery [3]. However, we report here an unusual case of a patient with an inverted appendix and isolated endometriosis, with the diagnosis being made through endoscopy by the nurse endoscopist.
Case Report
A 42-year-old woman had been suffering with chronic diarrhoea for two years, with elevated calprotectin over 400µg/g faeces (normal <110) and a CRP of 40 mg/l (normal <5 mg/l).
On index colonoscopy, it was reported as a large polyp in the caecum. The patient was referred to the significant polyp and early colorectal cancer (SPECC) MDT to discuss management where on reviewing the image it was felt that it was an inverted inflamed (ulcerated) appendix (Figs 1–2). A biopsy taken from the polyp showed inflammation, ulceration and some distortion. The patient had a small bowel MRI study, which excluded inflammatory small bowel disease but reported an abnormal caecum with the apparent polypoidal mass measuring 2.5 cm in diameter.
Figure 1:
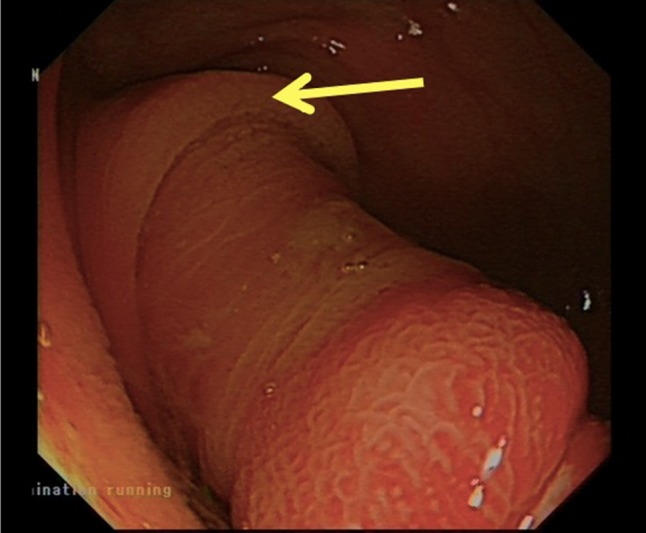
Close view of the polyp base, with appendiceal fold (arrow).
Figure 2:

Caecal polyp (inverted appendix), with wide ulceration.
The case was discussed at the colorectal MDT and recommended to have either an ileocaecal resection or a laparoscopic appendicectomy. The patient proceeded to have a laparoscopic appendicectomy with the cuff of the caecum. To facilitate this, the caecum was mobilized from the lateral wall. The inverted appendix, 50 × 30 mm in size, showed a reverse pattern of the normal mucosa. The outer surface was lined by colonic type mucosa with lymphoid aggregates. In addition the muscularis propria contained areas of endometrial glands with associated stroma and hemosiderin deposition, in keeping with endometriosis (Figs 3–5). There was no evidence of dysplasia or malignancy.
Figure 3:
At low magnification, inverted appendix lined by colonic type mucosa with underlying lymphoid aggregates.
Figure 5:
At higher magnification, endometrial glands and associated stroma present in the muscularis propria. Note the presence of a normal colonic mucosa on the right.
Figure 4:
At higher magnification, endometrial glands and stroma in the muscularis propria. Fibrosis and intervening adipose tissue seen at the centre.
Discussion
Presentation of an intussuscepted appendix can be acute or more commonly with chronic non-specific symptoms [4]. In two previous cases of inverted appendix, there was associated endometriosis on other organs and presented to the gynaecologist rather than the gastroenterology team [3, 5]. On reviewing the patient’s history, we found she did suffer with contact bleeding post coitus 5 years ago, and was investigated by gynaecology, who found that this was due to a large ectropion and cervicitis. This problem resolved with diathermy.
In our case, we found not only an intussuscepted appendix, but more interestingly, the presence of endometriosis. Appendiceal intussusception secondary to endometriosis is extremely rare, with less than 30 cases reported in the last 50 years [6]. However, those cases involved endometriosis on other organs as well as the appendix. There are only three cases that has been previously reported in literature with isolated appendiceal endometriosis [7, 8]. However, this is the first case in which diagnosis of inverted appendix was made through endoscopy, rather than surgery. Cases have also been reported of endometriosis on the appendix, without resulting in intussusception [1].
It is important to highlight the differential diagnoses that were postulated originally; caecal polyp (epithelial lesion), mucocele of the appendix and/or associated neoplasm and inflammatory bowel disease, in view of the elevated calprotectin. The appendicectomy with local cuff of caecum can also help in the staging if it proved to be neoplastic.
Our diagnostic strategy was firstly colonoscopy, and referral to MDT, and finally MRI to rule out small bowel Crohn’s disease. Normally an inverted appendix is diagnosed through surgery and treated with laparoscopic surgery [9]. However in our case, when the inverted and ulcerated appendix was noted endoscopically, an MR Enterography was considered necessary to rule out additional lesions in the small bowel, that could explain the ulceration of the inverted appendix. Additional imaging such as CT is indicated in neoplastic lesions of the appendix but can be reserved after surgery [10]. Only by doing appendicectomy can we obtain histology with a definitive diagnosis. It was imperative we identified the lesion as an inverted appendix and not a polyp, as previous reports showed misdiagnosis and incorrect polypectomy [3]. A key point is that when the well-trained nurse endoscopist diagnosed the condition, a polypectomy was not attempted, and instead the case was referred to the SPECC MDT. A second key point is that multi-disciplinary meeting helped the patient to get the appropriate treatment in a timely manner with the correct pre-op work up.
Although endoscopic appendicectomy has been reported, this is certainly not the standard treatment for polyps on the appendiceal [2]. In fact, even with advanced endoscopic methods such as full thickness resection, appendicitis develops as a complication of the procedure in almost 10% of the cases [10].
The laparoscopic appendicectomy involved resection of the caecal cuff, believed to be the ideal procedure for intussuscepted appendix [3]. This is because the cuff provides a margin of resection for appendiceal lesions, and more importantly the risk of leaving an appendiceal stump is removed. If the stump is left behind it can cause appendicitis and intussusception. It has been previously reported of a caecal intussusception post-appendicectomy, resulting in inversion of the appendiceal stump [9]. Endoscopic techniques, mainly endoscopic full thickness resection (EFTR) cannot be recommended in our case because of the risk of complication, and ‘lesion’ size was too large to achieve complete resection [10].
Acknowledgement
The patient has given consent for her story to be published.
CONFLICT OF INTEREST STATEMENT
No conflicts of interest.
FUNDING
No sources of funding.
Ethical Approval
No ethical approval required.
References
- 1. Dainius E, Pankratjevaite L, Bradulskis S, Venskutonis D. Intussusception of the appendix and ileum endometriosis: a case report. Visceral. Medicine 2016;32:211–3. 10.1159/000445394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sriram P, Seitz U, Soehendra H. Endoscopic appendectomy in a case of appendicular intussusception due to endometriosis, mimicking a cecal polyp. Am J Gastroenterol 2000;95:1594–6. [DOI] [PubMed] [Google Scholar]
- 3. Meister T, Varilek G, Marsano L, Gates L, Al-Tawil Y, de Villiers W. Endoscopic management of rectal Dieulafoy-like lesions: a case series and review of literature. Gastrointest Endosc 1998;48:302–5. 10.1016/S0016-5107(98)70197-X. [DOI] [PubMed] [Google Scholar]
- 4. Chaar C, Wexelman B, Zuckerman K, Longo W. Intussusception of the appendix: comprehensive review of the literature. Am J Surg 2009;198:122–8. 10.1016/j.amjsurg.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 5. Gustofson R, Kim N, Liu S, Stratton P. Endometriosis and the appendix: a case series and comprehensive review of the literature. Fertil Steril 2006;86:298–303. 10.1016/j.fertnstert.2005.12.076. [DOI] [PubMed] [Google Scholar]
- 6. Dickson-Lowe R, Ibrahim S, Munthali L, Hasan F. Intussusception of the vermiform appendix. BMJ Case Rep 2015,bcr2014207584 10.1136/bcr-2014-207584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Langman J, Rowland R, Vernon-Roberts B. Endometriosis of the appendix. Br J Surg 1981;68:121–4. 10.1002/bjs.1800680218. [DOI] [PubMed] [Google Scholar]
- 8. Shen A, Stanes A. Isolated appendiceal endometriosis. J Obstet Gynaecol Can 2016;38:979–81. 10.1016/j.jogc.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 9. Danielson K. Cecocolic intussusception—a postoperative complication of appendectomy. N Engl J Med 1969;280:35–6. 10.1056/NEJM196901022800109. [DOI] [PubMed] [Google Scholar]
- 10. Schmidt A, Beyna T, Schumacher B, Meining A, Richter-Schrag H, Messmann H, et al. Colonoscopic full-thickness resection using an over-the-scope device: a prospective multicentre study in various indications. Gut 2017;67:1280–9. DOI:0.1136/gutjnl-2016-313677. [DOI] [PubMed] [Google Scholar]





