Abstract
Background
Although women account for a growing proportion of the oncology workforce, there is evidence they are under-represented in leadership roles. To gain further insights into this issue and extend understanding of gender challenges, the European Society for Medical Oncology Women for Oncology (W4O) Committee undertook a survey of female and male oncologists in 2016.
Design
The 2016 W4O questionnaire included questions on (1) Demographics and professional environment, (2) Gender impact on career development, (3) Challenges for career progression and inappropriate behaviour experienced in the workplace, (4) Barriers for gender parity and (5) The gender gap. Between July and September 2016, the online survey was available to male and female clinical and academic oncology healthcare professionals in the EU and internationally.
Results
Responses were analysed from 462 oncologists, of whom 76.7 % were women. Of female respondents, 45.5 % had a managerial or leadership role, compared with 65 % of male respondents (p<0.001). Men were more likely to have leadership roles, even in clinical teams with more women than men. Women respondents were more likely to consider their gender had a major impact on their career than men: 35.9 % vs 20.9 % (p<0.001). The biggest challenge to career progression for women was work and family balance (64.2%). Of female respondents, 14.4 % believed there had been significant or major progress in closing the gender pay gap compared with 39.3 % of men (p<0.001). Of female participants, 37.7 % reported they had encountered unwanted sexual comments by a superior or colleague.
Conclusions
New initiatives are needed to address under-representation of women oncologists in leadership roles, including greater and concrete promotion of work–life balance, development and leadership training for women, and more support for flexible working. The fact that over a third of women in the survey had encountered unwanted sexual comments at work is of great concern and must be urgently addressed.
Keywords: gender, gender bias, medical oncology, workplace
Key questions.
What is already known about this subject?
There is evidence that women oncologists are under-represented in leadership roles, but little information is available about how they perceive their professional environment and the specific challenges they encounter in career development, compared with their male colleagues.
What does this study add?
This study provides insight into some of the challenges facing women oncologists in career development and achieving leadership roles.
How might this impact on clinical practice?
The results of this survey will inform future European Society for Medical Oncology initiatives aimed at supporting career development for oncologists, closing the gender gap in opportunities for leadership roles and addressing other workplace challenges. The findings identify areas on which regional and national organisations and specific institutions can focus their efforts in order to improve the workplace environment.
Introduction
Women make up a growing proportion of the medical workforce, and latest data from Organisation for Economic Co-operation and Development countries show a rise in female doctors from 39.1% in 2000 to 46.5% in 2015.1 With approximately half of medical students now women, this figure is likely to increase further in the coming years.2 However, studies carried out among medical professionals consistently show that, although more women are becoming doctors, male doctors dominate leadership roles.3 4 There is also evidence of a gender pay gap, with recent UK surveys showing that full-time male doctors earn 56% more than full-time female doctors5 and male consultants earn 12% more than female consultants.6
An increasing proportion of oncologists are women.7–9 In a US audit of the oncology/haematology workforce published in 2011, there were 3716 women, representing 28.4% of the oncology/haematology workforce.7 By 2016, this had risen to 3859 women, representing 32% of the oncology/haematology workforce.8 A survey in 12 European countries showed that, between 2000 and 2012, the mean annual increase in medical oncologists was larger in female than male oncologists.9 For example, in Germany, there was an 11.9% increase in female oncologists compared with a 7.2% increase in male oncologists.9 Female membership of the European Society for Medical Oncology (ESMO) is also increasing. In 2016, 40.5% of ESMO members were women—up from 24.9% in 2004 and 35.2% in 2012—and, in 2017, 52.9% of young oncologist members of ESMO were women.10 In 2016, 37% of members of the American Society of Clinical Oncologists were women.11
In response to the rapid rise in female membership of ESMO, the Women for Oncology (W4O) initiative was established in 2013 to explore the challenges facing female oncologists and to promote equal access to career development opportunities. The W4O Committee has been tasked with generating and disseminating information on the representation of women in the oncology workforce and to raise awareness and advocate for policies aimed at ensuring balanced gender representation in leadership positions in oncology.
In 2013, the W4O Committee carried out an exploratory survey among female oncologists which showed that, while the majority of medical oncologists working on clinical teams were women, most teams were managed by men.12 Indeed, nearly half of respondents had no leadership or managerial role. The three greatest obstacles to career progression were finding a balance between work and family life, the fact that men were perceived as leaders while women were seen as team members and supporters, and cultural gender prejudice due to misconceptions about women’s family and domestic responsibilities.
To gain further insights into the current representation of women oncologists in leadership roles and to extend understanding of gender challenges to include perceptions of male oncologists, a further W4O survey with both female and male participants was performed in 2016. The aims included exploring female representation across different work environments (academia and clinics) and comparing male and female perceptions of the impact of gender on career development. The W4O Committee also wanted to explore the role of unconscious bias on gender parity in oncology and to better understand the perceived barriers to career development for women oncologists. The findings of the survey will be used to inform the activities of the ESMO W4O Committee to support the career development of women in the oncology profession.
Methods
The 2016 W4O survey was based on the 2013 questionnaire, which was updated and extended by the W4O Committee in order to address the additional goals of the new survey.
The questionnaire consisted of five sections that included questions related to (1) Demographics and professional environment, (2) Gender impact on career development, (3) Challenges for career progression and inappropriate behaviour experienced in the workplace, (4) Barriers for gender parity and (5) The gender gap.
In August 2016, the survey was made available online to male and female oncology professionals of all ages, working in a range of clinical and academic environments in the EU and internationally. It was promoted on the ESMO website, ESMO W4O and ESMO Facebook pages and through ESMO’s digital newsletters. The responses were anonymous.
Results are presented overall and by respondent’s gender and the corresponding associations are tested based on Fisher’s exact test or Mann-Whitney U test (at level of statistical significance α=5%). The Cochran-Mantel-Haenszel (CMH) test and Breslow-Day test of homogeneity were also used in cases where the joint effect of gender with other significant factors needed to be explored. Finally, multivariable ordinal logistic regression was used in order to investigate the effect of gender and a series of other respondents’ characteristics (profession, workplace, age, country, having children, covering a leadership role and experiencing unwanted sexual comments) on their beliefs. The backwards elimination method (with removal criterion p=10%) was deployed to come up with a final model with significant effects in each case. All statistical analysis was carried out in SAS V.4 (SAS Institute, Cary, North Carolina, USA) and R V.3.4.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Description of analysis population
Responses were collected from 482 participants in total, but the analysis population consisted of 462 respondents as 20 participants were excluded because they did not work directly in oncology healthcare. Of the 430 respondents who stated their gender, 330 (76.7%) were women and 100 (23.3%) were men.
The majority of the respondents were medical oncologists (69.0%); 11.4% were trainees and 5.9% were radiation oncologists. Moreover, 39.8% of respondents worked primarily at a university hospital, 21.9% at a general hospital and 14.9% at a comprehensive cancer centre. Also, 76.7% of respondents were women, of whom 67.0% were aged under 45. Of the 23.3% of respondents who were men, 39.1% were under 45.
Respondents worked mainly in Europe (71.7%), with 12.5% working in Asia, 8.6% in America, 4.4% in Africa and only 2.9% in Oceania. Of female respondents, 55.4% had children and 30.6% of them were primary carers of children while 82.6% of male respondents had children and only 1.3% were primary carers (p<0.001) (online supplementary table 1). 1
esmoopen-2018-000422supp001.pdf (274.7KB, pdf)
Professional environment
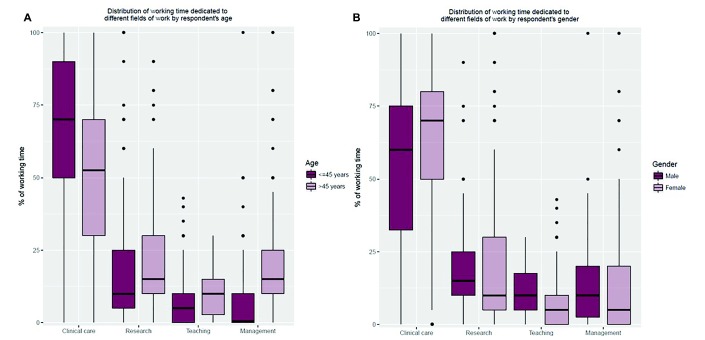
The distribution of respondents’ working time in specific fields of work is on average 60.4% clinical care, 19.6% research, 11.9% management and 8.1% teaching. Results by respondents’ gender indicate that the median working time dedicated to the fields of clinical care, teaching and management is significantly different for male and female respondents (60% for men vs 70% for women, p=0.039; 10% vs 5%, p=0.0014; and 10% vs 5%, p=0.023, respectively) (figure 1A). The distribution of working time also differs according to age for the three fields of work (figure 1B).
Figure 1.
Box plots for distribution (%) of working team dedicated to different fields of work by respondent’s gender (A) and age (B).
Among female respondents, 45.5% reported that they had a managerial or leadership role, compared with 65.0% of male respondents (p<0.001). Oncologists over 45 years old were more likely to lead their teams than oncologists under the age of 45 (79.9% vs 30.6%, p<0.001). Of note, the association of leadership role with gender is not significant when adjusted for age group (CMH, p=0.23; Breslow-Day, p=0.35): for respondents less than 45 years old, 28.6% of women and 41.7% of men had a leadership role (p=0.17), while for respondents of 45 years old and older, 79.6% of women and 80.4% of men had a leadership role (p>0.99).
Overall, in most cases (59.4%), there were more women in a respondent’s work team than men, but a woman was responsible for the team in only 35.3% of cases. Men were more likely to lead, even in teams where there were fewer men than women (male leaders in 53.8% of teams with more women than men and in 82.3% of teams with more men).
Gender impact on career development
The impact of the respondent’s gender on his/her career was considered to have major or moderate significance—35.9%/36.3% respectively of female responders, compared with 20.9%/19.8% respectively of male respondents (p<0.001) (figure S1).
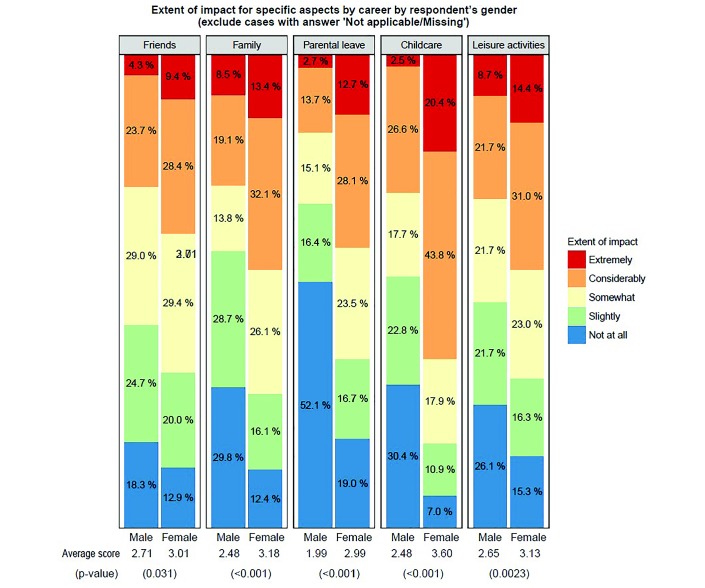
Data on the impact of a respondent’s career on specific aspects of her/his daily life are presented in figure 2. Responses show that a woman’s career was significantly more likely to affect her friends, family and marriage, and time dedicated to childcare, parental leave and leisure activities than was the case for a man (all p<0.05).
Figure 2.
Impact of career on daily life.
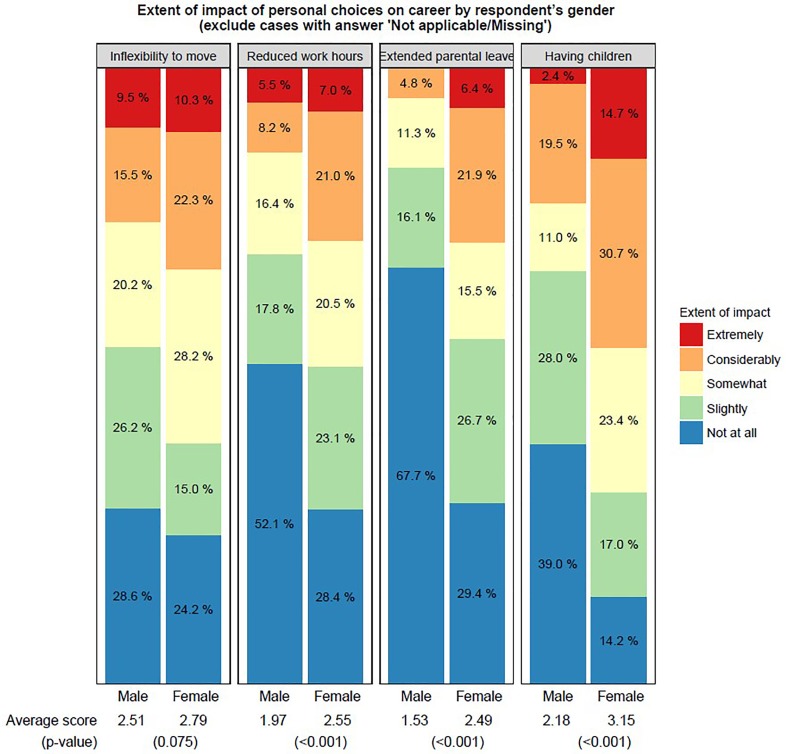
Data on the career effects of a respondent’s personal choices for moving location, having children, reducing their working hours and taking extended parental leave are summarised in figure 3. Responses showed that the career impact of choices about having children and taking extended parental leave and reduced working hours, reported by women was significantly greater than that reported by men (all three p<0.001).
Figure 3.
Impact of personal choices on career.
The statistically significant differences by responder’s gender remain significant (with the exception of impact on friends and leisure activities) even when taking into account related factors (multivariable ordinal logistic regressions presented in tables S2-S11).
Challenges for career progression and barriers for gender parity
The biggest challenges to career progression encountered by the female respondents were finding a balance between work and family (64.2%), the fact that men were perceived as natural leaders while women were perceived as team members and supporters (39.9%), and the difficulty in spending time abroad for research (31.3%) and managing and organising family commitments (30.1%) (figure S2).
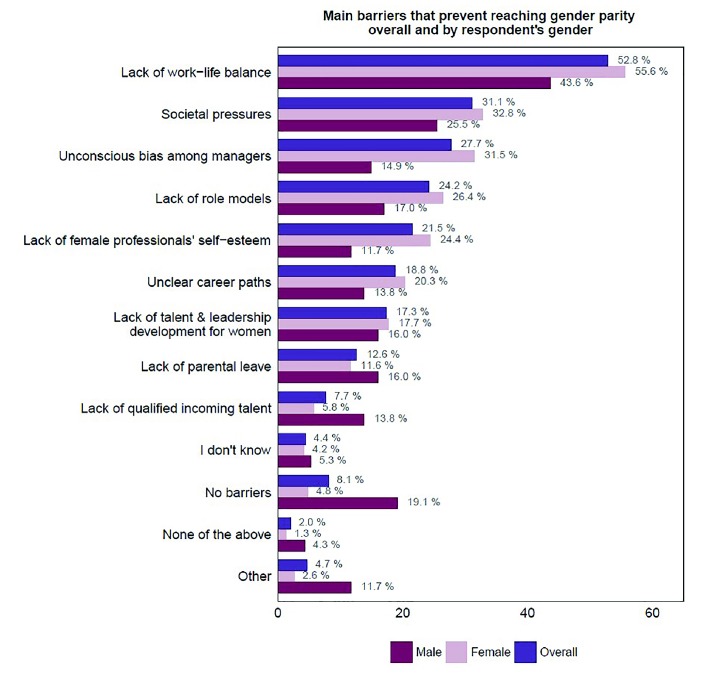
The main barriers that respondents felt prevent gender parity in the field of oncology are presented in figure 4. Overall, the greatest barrier was reported to be lack of work–life balance (52.8% of respondents), and this was the case for both female and male respondents (55.6% and 43.6%, respectively). More women (31.5%) than men (14.9%) believed that unconscious bias among managers disturbs gender parity (p=0.0015). Lack of qualified incoming talent constituted an important barrier for equality between genders for 13.8% of male respondents but for only 5.8% of female respondents (p=0.015).
Figure 4.
Barriers to gender parity overall (N=405) and by respondent’s gender (311 women and 94 men).
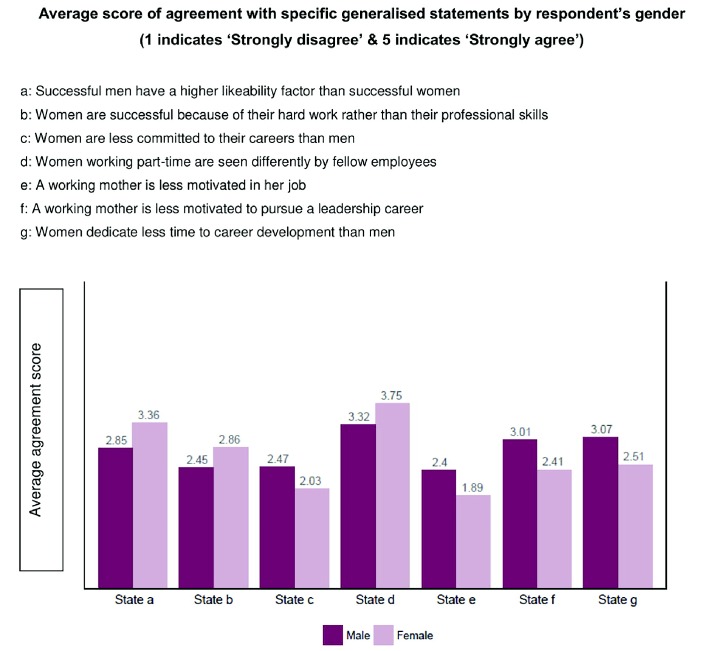
Responses to a series of generalised statements about attitudes to working women, based on experiences previously reported by ESMO members, varied between female and male participants in the survey (figure 5 provides average scores of agreement). For example, 53.8% of women agreed or strongly agreed with the statement that successful men have a higher likeability factor than successful women, compared with 29.7% of men (p<0.001). In contrast, 14.3% of female respondents agreed or strongly agreed with the statement that women are less committed to their careers than men, compared with 22.4% of male respondents (p=0.0017). Similarly, 22.3% of women in the survey agreed or strongly agreed with the statement that a working mother is less motivated to pursue a leadership career, compared with 44.1% of men who took part in the survey (p<0.001).
Figure 5.
Agreement with specific generalised statements.
Additional findings are derived from the joint assessment of related factors (tables S12-S18). The belief that women are less committed to their careers than men is significantly more prevalent for respondents working in general versus university hospitals.
Overall, 173/362 (47.8%) of participants who answered the question believed that there had been no or minor progress in closing the gender gap in the workplace since they started working, 32.0% believed there had been moderate progress and 20.2% significant or major progress. Among female respondents, only 14.4% believed there had been significant or major progress compared with 39.3% of male respondents (p<0.001).
The impression of unequal opportunities between men and women in the workplace was shared by 54.7% of all respondents (64.6% of female respondents vs 22.6% of male respondents; p<0.001), but 65.1% of respondents felt that their organisation practised ‘equal pay for equal work’ (58.3% of female respondents vs 87.1% of male respondents; p<0.001).
Of female participants, 37.7% reported that they had encountered unwanted sexual comments by a superior or colleague. These comments took the form of generalised sexist remarks and behaviours (69.0%), inappropriate sexual advances (19.8%), subtle bribery to engage in sexual behaviours (8.6%), coercive advances (1.7%) and threats to engage in sexual behaviours (0.9%).
Suggestions to address gender parity
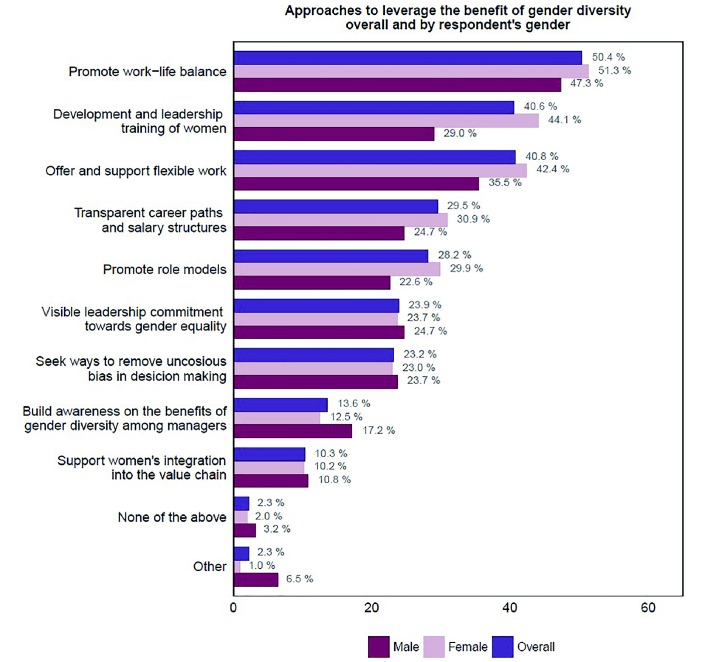
To address gender parity, female and male respondents indicated that the three most important approaches were promotion of work–life balance (51.3% vs 47.3%, respectively, not significant), development and leadership training for women (44.1% vs 29%, respectively, p=0.011), and the offer of support for flexible working (42.4% vs 35.5% respectively, not significant). Additional suggestions are shown in figure 6.
Figure 6.
Approaches to addressing gender parity.
Discussion
The results of the 2016 W4O workplace survey indicate that in 59.4% of clinical teams, the majority of oncologists are women but a higher proportion of leadership roles are filled by male oncologists rather than female oncologists (64.7% vs 35.3%).
In addition to the quantitative findings of the survey, individual responses from some participants offer further insights into the challenges facing women oncologists in achieving leadership roles. Some selected comments from female respondents are listed below: (1) ‘welcome to apply for a job but the male candidate is more likely to be viewed favourably’; (2) ‘men being selected for higher positions despite equal or lower qualifications and skills’; (3) ‘men in leadership roles were more comfortable talking to other men’. Comments from male respondents include (1) ‘much of the fuss around gender equality is irrelevant in this current day and age’, (2) ‘main objective should be to support women so that they are good parents and pursue the career they want’, and (3) ‘we should focus more on ability and integrity and create more opportunities for those with abilities and integrity, be it female or male’.
The finding that women oncologists are less likely to play a leadership role than their male colleagues is not unusual. In a recent survey carried out by the Association of American Medical Colleges, 51% of medical teaching staff at US medical schools were women, but only 20% were full professors and even fewer were heads of department.3 In another recent US study, female cardiologists were 37% less likely to become a full professor than their male colleagues, despite a doubling in the proportion of women entering the specialty over the last 20 years.4 In an observational study of leadership roles in US obstetrics and gynaecology residency programmes accredited in 2012–2013, 20.2% of chairs were women, together with 36.1% of vice chairs, and 29.6% of division directors.13 Similar gender disparity has been demonstrated in leadership roles in academic musculoskeletal radiology14 and neuroradiology.15 Data from an ongoing prospective study of physicians 7 years after graduation from medical schools in Switzerland showed that women doctors, in particular those with children, had less career success than their male contemporaries, were less advanced in their specialty qualification and less likely to have a mentor, tended to work in small hospitals or private practice, and aspired less often to senior hospital or academic positions.16
By surveying men as well as women, the 2016 W4O survey identified distinct perceptions of the impact of gender on career and of career on daily life. A higher proportion of women than men felt that their gender affected their career and that their career affected important aspects of their daily lives, such as their family and marriage, time devoted to childcare and parental leave. A higher proportion of female than male oncologists felt that choices about having children and taking extended parental leave affected their career, though lack of work–life balance was a major issue for both groups.
Women felt that there had been less progress in bridging the gender gap than men, and they were almost twice as likely to feel that women and men do not have equal opportunities in the workplace. The need to promote work–life balance, develop leadership training for women and offer flexible working was recognised by both male and female respondents.
The disparity between female and male perceptions of the effect of gender on career opportunities is illuminating. The W4O survey suggests the need for greater awareness of the challenges faced by female oncologists across the clinical workforce and concerted efforts to address them at all levels.
ESMO is taking steps to address these needs, with programmes to support members in career advancement through preceptorship, mentor, sponsor and leadership programmes. In the 2017 Leaders Generation Programme, eight female and seven male oncologists learnt leadership skills through workshops and presentations by ESMO and external experts. Provision of childcare at the annual ESMO congress was introduced in 2017 so that lack of childcare is less of a barrier for participants wishing to engage in educational and networking opportunities. In parallel, ESMO will support national initiatives focusing on women’s careers, though legislative changes are needed in some countries. ESMO can also survey and promote gender balance, and develop initiatives that will lead to greater recognition of women in the competitive environment of academic research and education in medical oncology.
Although there was considerable agreement about the need for programmes to support female career development in both the 2013 and 2016 W4O surveys, some respondents in the 2016 survey were wary of encouraging initiatives for women. ‘We need attitudes that promote generic equality of opportunity rather than a (paradoxically) sexist focus on gender,’ wrote one male participant. ‘Gender equality should mean just that. I am as opposed to specialised activities and groups for women as I would be for men. Women are equal so why should we have these exclusive groups?’ asked a female respondent.
There are clearly strong opinions about how the gender gap in oncology careers should be bridged, and ongoing consultations for future strategies will be the key.
In contrast, there can be no compromise concerning the issue of sexual harassment in the workplace. The fact that the 2016 W4O survey showed that a significant proportion of women had encountered unwanted sexual comments and behaviour by superiors or colleagues is of great concern, particularly in the current climate of zero tolerance of inappropriate sexual conduct. In our survey, 37.7% of respondents had encountered unwanted sexual comments by a superior or colleague, compared with rates of sexual harassment ranging from 30% to 52% in previous studies of women in academic medicine.17
Survey limitations
There may have been selection bias in the survey, depending on those who elected to take part. Of note, the majority of the female respondents were aged under 45 (67%), while among male respondents only 39.1% were under 45.
As the denominator is not known, we cannot say what proportion of the total oncologist population worldwide, or even in Europe, is represented in our survey. The primary work place of the majority of respondents (76.7%) was in Europe, so our sample may not be representative of the oncologist profession worldwide.
Further surveys are planned, with the aim of obtaining wider representation across oncology healthcare professionals (eg, nurses, pharmacists), enlarging the geographical coverage of potential diversity and exploring variation in career opportunity and childcare availability in different countries.
In addition, data on ESMO membership might vary by a few percentage points at specific time points because of the evolving nature of the ESMO database. Nevertheless, this variation does not impact on the trends brought forth in this article.
Conclusions
Although there are generally more women oncologists in clinical teams than men, women oncologists are less likely to have leadership roles and they feel that their gender is adversely affecting their career. Women feel that less progress has been made in closing the gender gap than men and they feel affected by unequal opportunities in the workplace. The fact that over a third of women in the survey had encountered unwanted sexual comments at work is of great concern and must be urgently addressed. New initiatives are needed to address under representation of women oncologists in leadership roles, including greater promotion of work–life balance, development and leadership training for women, and more support for flexible working.
Acknowledgments
Writing assistance was provided by Jenny Bryan and funded by ESMO.
Footnotes
Funding: The 2016 Women for Oncology (W4O) survey was funded by ESMO.
Competing interests: DA has received research funding and/or honoraria from Roche, Merck Serono, Bayer Healthcare, Servier, BTG, Terumo, Sanofi Oncology, Eli Lilly and has participated in non-financial roles as ECCO Executive Board member, ECCO Oncopolicy Group member, EORTC Task Force member (Gastrointestinal cancers)—Global PI function with MOLOGEN, IMPALA trial (MGN 1703 as investigative agent). GC has received research funding and/or honoraria from Roche, Novartis, Pfizer and has participated in non-financial roles as a member of Steering Committee in clinical trials, member of data safety monitoring committee for clinical trials. MCG has received research funding and/or honoraria from MSD, BMS, Roche Astra Zeneca, Takeda and Eli Lilly. EG has participated as Advisor for Roche, Neomed Therapeutics and Ellypses Pharma. EH-T is an employee of Janssen, the Pharmaceutical Company of Johnson & Johnson Europe, and a shareholder of Johnson & Johnson. CR has been a consultant for BMS, Riche, Novartis, Pierre Fabre, MDS and Amgen. CS is a Scientific Consultant for SAKK (Swiss group for cancer research treatment) and has participated in non-financial roles as the ESGO Vice President, Principal Investigator for the Icon 8B Study, EUPATI Switzerland. SP has received research funding and/or honoraria from Genentech/Roche, Pfizer, Eli Lilly, MSD, Merck Serono, BMS, Novartis, Astra Zeneca, Boehringer Ingelheim, Amgen, Clovis, Regeneron, Janssen, Takeda and has participated in non-financial roles on the IASLC Board of Directors 2014–2017, SAKK lung group Vice-president, SAMO Vice-president, Froome Past President (2011–2017), ETOP Foundation Council/Scientific coordinator, ESMO president elect 2010–2021, PI ALEX trial, Genentech Steering committee, PI academic trials ETOP, EORTC/SAKK, FMH, IASLC, AACR.
Patient consent: Not required.
Provenance and peer review: Not commissioned; internally peer reviewed.
For references to tables, see the ‘online supplementary table 1’ document submitted as supplementary material.
References
- 1. Organisation for Economic Co-operation and Development. 2017. The pursuit of gender equality: an uphill battle. http://www.keepeek.com/Digital-Asset-Management/oecd/social-issues-migration-health/the-pursuit-of-gender-equality/although-women-make-up-less-than-half-of-all-doctors-oecd-wide-their-share-is-growing_9789264281318-graph87-en#page3
- 2. Bates C, Gordon L, Travis E, et al. . Striving for gender equity in academic medicine careers: a call to action. Acad Med 2016;91:1050–2. 10.1097/ACM.0000000000001283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Association of American Medical Colleges, 2015. The state of women in academic medicine: the pipeline and pathways to leadership, 2015–2016. https://www.aamc.org/members/gwims/statistics
- 4. Blumenthal DM, Olenski AR, Yeh RW, et al. . Sex differences in faculty rank among academic cardiologists in the United States. Circulation 2017;135:506–17. 10.1161/CIRCULATIONAHA.116.023520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Medscape. 2018. UK doctors’ salary report. https://www.medscape.com/slideshow/uk-doctors-salary-report-6009730?src=mkm_ret_ukmd_salary2018_binleys_061218)
- 6. BBC. 2018. Top women doctors lose out in NHS pay stakes. https://www.bbc.co.uk/news/health-43077465
- 7. Kirkwood MK, Kosty MP, Bajorin DF, et al. . Tracking the workforce: the American Society of Clinical Oncology workforce information system. J Oncol Pract 2013;9:3–8. 10.1200/JOP.2012.000827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. American Society of Clinical Oncology. The state of cancer care in America, 2017: a report by the American Society of Clinical Oncology. J Oncol Pract 2017;13:e353–e394. 10.1200/JOP.2016.020743 [DOI] [PubMed] [Google Scholar]
- 9. de Azambuja E, Ameye L, Paesmans M, et al. . The landscape of medical oncology in Europe by 2020. Ann Oncol 2014;25:525–8. 10.1093/annonc/mdt559 [DOI] [PubMed] [Google Scholar]
- 10. European Society for Medical Oncology. Data gathered from ESMO membership database. [Google Scholar]
- 11. Anon. 2018. ASCO kicks off strategic planning to support women in oncology. https://gicasym.org/daily-news/asco-kicks-off-strategic-planning-support-women-oncology
- 12. European Society for Medical Oncology. 2013. ESMO exploratory study on the challenges of female medical oncologists. https://www.esmo.org/Career-Development/Women-for-Oncology/Women-Oncologists-Today
- 13. Hofler L, Hacker MR, Dodge LE, et al. . Subspecialty and gender of obstetrics and gynecology faculty in department-based leadership roles. Obstet Gynecol 2015;125:471–6. 10.1097/AOG.0000000000000628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Qamar SR, Khurshid K, Jalal S, et al. . Academic musculoskeletal radiology: influences for gender disparity. Skeletal Radiol 2018;47:381–7. 10.1007/s00256-017-2836-x [DOI] [PubMed] [Google Scholar]
- 15. Ahmadi M, Khurshid K, Sanelli PC, et al. . Influences for gender disparity in academic neuroradiology. AJNR Am J Neuroradiol 2018;39:18–23. 10.3174/ajnr.A5443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Buddeberg-Fischer B, Stamm M, Buddeberg C, et al. . The impact of gender and parenthood on physicians’ careers—professional and personal situation seven years after graduation. BMC Health Serv Res 2010;10:40 10.1186/1472-6963-10-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bates CK, Jagsi R, Gordon LK, et al. . It is time for zero tolerance for sexual harassment in academic medicine. Acad Med 2018;93:163–5. 10.1097/ACM.0000000000002050 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
esmoopen-2018-000422supp001.pdf (274.7KB, pdf)