Abstract
Background
While the global workforce is approaching gender parity, women occupy a small number of management level positions across most professions, including healthcare. Although the inclusion of women into the membership of many oncology societies has increased, the under-representation of women in leadership roles within international and national oncology societies remains relatively consistent. Moreover, the exact status of women participating as board members or presidents of oncology societies or as speakers at oncology congresses was undocumented to date.
Methods
The database used in this analysis was derived from data collection performed by the European Society for Medical Oncology for the years 2015–2016 and data analyses performed using the Statistical Analysis Software V.9.3 and R language for statistical computing V.3.4.0 by Frontier Science Foundation-Hellas. The literature search was performed by the authors.
Results
We report the presence of a gender gap within oncology. Results regarding the under-representation of women occupying leadership roles in oncology show female participation as members of the board or presidents of national and international oncology societies and as invited speakers at oncology congresses remains below 50% in the majority of societies included in this analysis. Women in leadership positions of societies was associated with a higher percentage of female invited speakers at these societies’ congresses (p=0.006).
Conclusion
The full contribution that can be attained from using the potential of women in leadership roles is currently under-realised. Examples of how gender and minority participation in organisations improves outcomes and creativity are provided from science, clinical practice and industry that show outcomes are greatly improved by collective participation of both men and women. Although there are programmes in place in many oncology organisations to improve this disparity, the gender gap is still there. Ongoing discussion may help to create more awareness in the effort to accelerate the advancement of women within oncology.
Keywords: gender, gender bias, medical oncology, workplace
Key questions.
What is already known about this subject?
Although more women are entering the global workforce, this participation has not translated to full participation at the upper management levels, including in the field of medical oncology. Leadership positions within oncology, such as presidents or board members of oncology societies and invited speakers at oncology congresses, remain predominantly held by men. Information remains sparse regarding the actual number of women participating in oncology societies and holding leadership positions in Europe, Asia Pacific and South America.
What does this study add?
This publication provides recent figures for the percentage of women occupying leadership roles across a selected cohort of international and national European, South American and Asian large oncology societies and congresses, as well as direct comparisons between major US-based and European-based international societies and congresses. The data discussed here also suggest why gender gaps still exist and speculate how to achieve a better gender parity. Examples are given of successful programmes addressing this issue, and suggestions for new ways to provide resources and support to aid women in achieving their potential.
Key questions.
How might this impact on clinical practice?
Generally, groups having a mix that includes diverse backgrounds, nationalities and genders produce better outcomes. Women often exhibit a cooperative work style that enhances the effectiveness of groups, particularly when extensive information management and decision-making are required, such as treatment recommendations formulation. Women in leadership will contribute to a people-oriented and interactive approach to the development and implementation of patient treatment policies. Policies developed by gender-balanced groups will encourage more women to practice oncology and will also reflect a female perspective that will benefit both male andfemale patients. The integration of women into all levels of oncology will ensure that the physician workforce reflects the gender diversity and cultural perception of the population it serves.
Introduction
The under-representation of women in leadership roles is a theme that cuts across all sectors of society, including the global workforce. While women comprise up to 42% of the world’s paid working population,1 it is estimated that just 24% of senior management positions globally are occupied by women.2
Within the healthcare sector, women comprise over 75% of the workforce in many countries, making them an important factor in the delivery of medical services.1 Looking closer, it is important to note that there are imbalances at the professional level, where the nursing and midwifery professionals are nearly 90% women, while only 25% of physicians are women.3 It is crucial to create diversity in the healthcare workforce that mirrors the general population from a gender perspective and in general terms such as racial/ethnic backgrounds, people with disabilities, as well as economically disadvantaged social backgrounds.4
A recent audit estimated that the field of oncology experienced a 3% increase in the number of oncologists per year from 2004 to 2011 in the USA. However, the same report set the number of women at 3716 (28.4%) in the composite oncologist physician workforce of 13 084 for the year 2011.5 The representation of women in oncology may also be measured by their participation in national and international medical oncology societies, where women are achieving near parity with men in terms of membership. For example, in 2015, women comprised 41.9% of the membership in the European Society for Medical Oncology (ESMO)6 while 36% of American Society of Clinical Oncology (ASCO) members as of 2016 were women.7
ESMO membership statistics 1 revealed that the number of active members had doubled, from 3788 in 2004 to 7665 in 2012, and further increased by 2015–2016 to 13 182, with the greatest rise seen in the percentage of female members, which rose from 24.9% to 35.2% to 40.5% during these years, respectively.8 This demographic shift prompted the ESMO president at that moment, Martine Piccart, to foster the Women for Oncology (W4O) initiative in 2013, which started several audits of the female work force in oncology to identify challenges and rewards specific to female oncology professionals. This resulted in the ESMO Exploratory Study on the Challenges of Female Medical Oncologists that was presented at the European Cancer Congress 2013 in Amsterdam.9
W4O survey data presented at the ESMO 2016 Congress confirmed this trend; however, while the survey revealed that progress in parity is being achieved between genders on membership levels, it highlighted the persistent discrepancies in leadership positions within these societies and in the number of women invited to speak at major meetings. This account of gender disparity within leadership positions was consistent with similar statistics on women leaders throughout the global workforce as reported by the Global gender Gap Report 201610 as well as the WHO.1
This publication reports findings from the ESMO W4O data collection that presents a current view of the proportion of women occupying leadership roles, including board members or presidents of medical oncology societies, and invited speakers at major oncology congresses. The basis of this report is an analysis of gender parity within ESMO that is expanded to a comparison with other major international societies, as well as figures from Asian, South American and European national societies.
The aim is to understand current gender disparities in oncology and to provide updated information revealing where strides forward have been taken and where change had stagnated in the journey towards achieving gender parity in oncology.
Methods
This report is based on a database comprising data collection performed by ESMO, data analysis performed by Frontier Science Foundation-Hellas and a literature search performed by the authors.
Data were collected for the years 2015–2016, with 2014 information used only when more recent data were unavailable. Information regarding the gender composition of oncology societies, both in absolute numbers and/or percentages, including board members and presidents (for 2016), and congress speakers (for 2016–2015 or if needed for 2014), was obtained via email queries. These were addressed to the society secretariat and/or the ESMO referent person who was also asked for information on the criteria used to select the congress sessions. Regarding Asian national societies, only gender information directly provided or confirmed by each society was included in the analysis. In the event that information regarding the gender of invited speakers was unavailable, the ESMO headquarters reviewed printed or online copies of the final congress programme book and derived gender information from the speakers’ names together with online biographies and/or photographs.
The analyses of presidency, board members and invited speakers included data from international societies and congresses as well as national European, South American and Asian societies and congresses.
European national societies were included on the basis of having an agreement of reciprocal membership with ESMO and Asian national oncology societies that endorsed the ESMO ASIA 2016 Congress (online supplementary table 1). International congresses were selected on the basis of being organised by ESMO, the European CanCer Organisation (ECCO), American Society of Clinical Oncology (ASCO), European Association for Cancer Research (EACR), American Association for Cancer Research (AACR), the European Society of Surgical Oncology (ESSO), European Organisation for Research and Treatment of Cancer (EORTC), the European Society for Radiotherapy and Oncology (ESTRO) and the American Society for Radiotherapy and Oncology (ASTRO). National European oncology congresses were chosen on the basis of being organised by national societies that had an agreement of reciprocal membership with ESMO.
esmoopen-2018-000423supp001.pdf (161.4KB, pdf)
Descriptive statistics of the female representation as board members and invited speakers were produced by society/congress name and geographical region. The correlations regarding the percentage of female board members or invited speakers versus the size of the society/congress and the percentage of female invited speakers versus the percentage of female board members are illustrated on a scatterplot. The Spearman correlation coefficient was used to quantify the strength of those associations.
Basic descriptive statistics were produced regarding the constitution of ESMO membership for the year 2015, including summaries of member characteristics by age and gender. Fisher’s exact test or Mann-Whitney U test was used to determine the association between the gender composition of the ESMO Executive Board members and available characteristics of ESMO members.
A two-sided significance level of 0.05 was used for the statistical testing. All statistical analyses were performed using the Statistical Analysis Software V.9.3 and R language for statistical computing V.3.4.0.
Results
Gender composition of ESMO membership and leadership
This analysis shows that gender demographics within ESMO are rapidly changing, with younger women representing the fastest growing segment of the membership. The proportion of women within ESMO membership has steadily grown from 20.2% in the year 2000 and has doubled according to figures for the year 2015. Evaluation of 13 082 ESMO members in 2015 revealed that women now represented 41.0% of members, with men continuing to be the majority at 59.0% of the total membership.
Further analysis of membership records from the 12 551 registered ESMO members having available age information showed that the majority (61.7%) of ESMO members were aged over 40 years, while the median age of all members was 44 years (range 22 to 97 years). Female members had a significantly lower median age compared with male members (41 years vs 47 years; p<0.001).
Looking more closely at the 4803 (38.3%) members aged 40 years or younger, there were 2489 (51.8%) women compared with 2314 (48.2%) men in this subgroup, which illustrates that the ESMO membership is growing significantly quicker from the inclusion of younger women (p<0.001).
Table 1 depicts the gender composition of the ESMO Executive Board members (reference year 2016) and the total of ESMO members (reference year 2015). Out of the 14 ESMO board members, only 2 (14.3%) were women, while of the 13 182 ESMO members, 5341 (40.5%) were women.
Table 1.
Gender representation of ESMO board members (reference year 2016) and all ESMO members (reference year 2015)
| Gender | ESMO board members—n (%) | ESMO members—n (%) |
| Male | 12 (85.7) | 7841 (59.5) |
| Female | 2 (14.3) | 5341 (40.5) |
| Total | 14 (100.0) | 13 182 (100.0) |
ESMO, European Society for Medical Oncology.
Comparison of the number of women board members of oncology societies
The presidency and board member analysis comprised data from the nine international societies listed in online supplementary table 1 (AACR, ASCO, ASTRO, EACR, ECCO, EORTC, ESMO, ESSO, ESTRO) and 44 national societies (21 European, 6 South American and 17 Asian.
Despite a clear trend towards an increase of women within the field of oncology and among the ranks of ESMO, women continue to be under-represented in senior roles within this organisation. Under-representation of women in leadership positions such as board members or presidents in oncology societies was reflected across most of the societies evaluated in this study. This analysis included the number of current board members during 2016, excluding society presidents who have been analysed separately. Ex-officio board members and members with no voting rights were also included in the analysis.
Overall, in 2016, 29 out of the 115 (25.2%) board members of all of the international societies reviewed were female oncologists, which does not differ significantly from the 27.5% (265 women out of a total of 962 board members) of Asian, European and South American national societies (p=0.66). Additionally, within the international societies there was no significant difference between the European-based (24.2% women board members) versus US-based (26.5%) societies (p=0.83).
The representation of women as board members in ESMO was not different from the representation of women oncologists on the boards of the other eight international societies (all p>0.1). However, the percentage of women named as oncology board members ranged from 7.1% for ASTRO to 46.7% for AACR. In general, societies with an emphasis on research had the highest percentage of women occupying board positions, including AACR (46.7%), EACR (40.0%) and EORTC (28.6%), as compared with more clinically oriented organisations, such as ESMO (14.3%) and ASCO (25.0%) (figure 1).
Figure 1.

Gender representation of board members in all international societies (reference year: 2016). AACR, American Association for Cancer Research; ASCO, American Society of Clinical Oncology; ASTRO, American Society for Radiotherapy and Oncology; EACR, European Association for Cancer Research; ECCO, European CanCer Organisation; EORTC, European Organisation for Research and Treatment of Cancer; ESMO, European Society for Medical Oncology; ESSO, European Society of Surgical Oncology; ESTRO, European Society for Radiotherapy and Oncology.
A significant variation between the gender composition of national boards (reference year 2016) was observed between European, South American and Asian national oncology boards (p=0.039). The European national societies had a higher percentage of female board members (33.8%) compared with the Asian (24.8%) and the South American (27.7%) national societies.
The majority of almost all society boards consisted of men. For all societies with large board size (N>20), more than 60% of the members were men. Only six societies had more female than male board members; of these, two were Asian (MyOS: 72% women, N=18; PSMO: 56%, N=9), one was South American (SOMPU: 64%, N=11) and three were European (AIOM: 57%, N=7; MAGYOT: 80%, N=5; UMOS: 60%, N=5).
The percentage of female board members of European national societies varied from 0% for the OEGHO to 80% for the MAGYOT.
On review of Asian and South American national societies, a strikingly disparate range for the proportion of female board members emerged, from 0% for the AOU or SLACOM, to 72% of the MyOS and 64% in the SOMPU boards.
It should be noted that the percentage of women acting as board members showed an association with the size of the society, which approached statistical significance (p=0.051).
Representation of women as presidents of oncology societies
As could be anticipated with women being under-represented at the board member level, few oncology societies had women presidents. In 2016, of the 53 international and national societies analysed, 48 (90.6%) presidents were men, with just 5 (9.4%) female presidents.
An apparent but not statistically significant association was observed between having a female president and the percentage of women board members of societies; societies having a female president also had 38.2% of women board members, whereas 26.6% of women occupied board positions in societies having a male president (p=0.084).
The direction of this association, even though non-significant, suggests that the integration of women into the boards of societies opens the door to placement in additional leadership positions.
Representation of women as invited speakers at oncology congresses
A third indicator of the assimilation of women into leadership roles within the field of oncology is their representation as invited speakers at national and international congresses.
The analysis of invited speakers represented data from 6 international congresses (AACR, ASCO, EACR, ECCO, ESMO, ESSO), 9 European national congresses, 3 South American national congresses and 17 Asian national congresses held during 2015–2016.
Overall, women represented less than one-third of invited speakers. Out of the total of 5496 invited speakers, 3876 (70.5%) were men and 1620 (29.5%) were women. Women remained under-represented as speakers compared with men at the international and all national (European, South American and Asian) congresses assessed.
There was no difference when comparing female representation as invited speakers in all international (30.3%) versus in all national congresses (28.9%) (p=0.27).
However, focusing only on the international congresses, a direct comparison of American-based versus European-based international congresses revealed a greater proportion of women speakers at American-based (33.1%) versus European-based (27.5%) international congresses (p=0.004) (analytical percentage by congress shown in figure 2).
Figure 2.

Gender representation in all international congresses (reference year 2016). AACR, American Association for Cancer Research; ASCO, American Society of Clinical Oncology; EACR, European Association for Cancer Research; ECCO, European CanCer Organisation; ESMO, European Society for Medical Oncology; ESSO, European Society of Surgical Oncology.
As shown in table 2, within the major international congresses held during 2016, women represented approximately one-third of invited speakers at most congresses (32.4% AACR, 34% ASCO and 32.9% ECCO). Lower representation was seen in EACR, ESMO and ESSO, where women represented 27.5%, 26.2% and 10.9%, respectively, of the invited speakers at the respective congresses.
Table 2.
Comparison of the percentage of women as invited speakers between the ESMO congress and other international congresses (reference year 2016)
| Comparison | P values |
| ESMO (N=588) vs Europe-based congresses | |
| ESMO vs ECCO (N=422) (26.2% vs 32.9%) | 0.021 |
| ESMO vs EACR (N=69) (26.2% vs 27.5%) | 0.77 |
| ESMO vs ESSO (N=91) (26.2% vs 10.9%) | 0.001 |
| ESMO (N=588) vs US-based congresses | |
| ESMO vs ASCO (N=485) (26.2% vs 34.0%) | 0.006 |
| ESMO vs AACR (N=683) (26.2% vs 32.4%) | 0.019 |
Bold values indicate where the p value is significant.
AACR, American Association for Cancer Research; ASCO, American Society of Clinical Oncology; EACR, European Association for Cancer Research; ECCO, European CanCer Organisation; ESMO, European Society for Medical Oncology; ESSO, European Society of Surgical Oncology.
The representation of women as speakers at national congresses also differed significantly from 24.4% in Asian versus 33.5% in European versus 34.4% in South American congresses (p<0.0001).
While the proportion of women invited speakers at congresses was not associated with the size of the congress (p=0.47), a high participation by women as board members of oncology societies seemed to translate to greater representation of women as speakers at congresses. A significant positive association was found between the percentage of women members of oncology society boards and the percentage of women invited speakers at congresses organised by these societies (p=0.006). This association was based on 32 societies having available information for both invited speakers and board members (figure 3).
Figure 3.
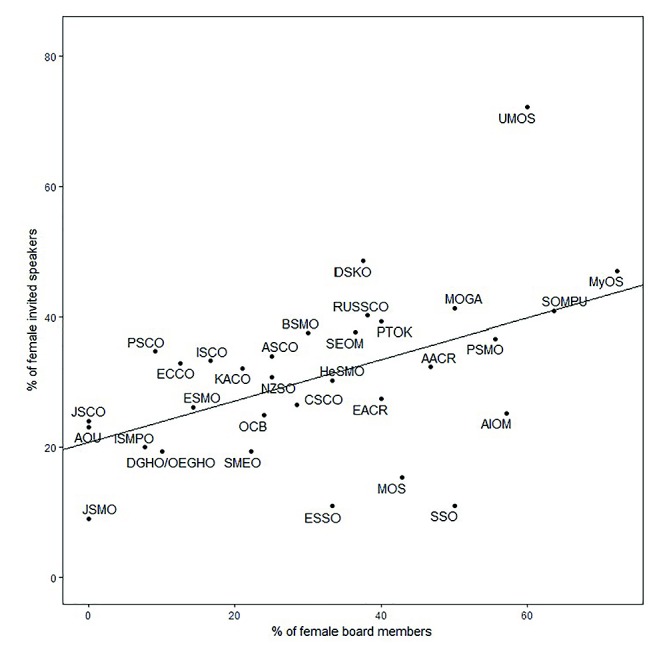
Scatterplot of the percentage of female invited speakers versus the percentage of female board members. Note: Societies DGHO and OEGHO constitute one category/society. Please see appendix for definitions of abbreviations.
To illustrate this point, in 2016 AACR had a female president, 47% of board members were women and the AACR congress had one of the higher percentages (32%) of female speakers. Among European national societies, the UMOS board comprised 60.0% women and the highest percentage (72%) of female speakers at their congress. A high proportion (47.0%) of female speakers was observed in the MyOS and MOGA (41%) congresses, which was reflected in board member female composition of 72% and 50%, respectively.
Discussion
This report demonstrates the existence of a gender gap that is not narrowing within the leadership in oncology. Although women are entering the field and participating as members of oncology societies, this has not translated into more women occupying positions as board members, presidents of these societies or as invited expert speakers at congresses organised by international and national oncology societies. The gender composition of oncology society boards impacts the representation of women as invited speakers; however, the female membership of a society does not seem to be a factor in the number of women invited as congress speakers.
Women currently constitute the majority of ESMO members under the age of 40, but they continue to occupy a very small percentage of leadership positions within ESMO and most other oncology societies. In 2016, just 2 (14.3%) of the 14 ESMO board members were women.
Further, a survey of several well-known US academic journals revealed that 5.9% of first authors in 1970 were women, while 29.3% female first-authors published in 2004 (p<0.001). A last author comparison showed 3.7% were women in 1970 and 19.3% in 2004. Additionally, only 1.5% of guest editorials were authored by women in 1970, which rose to the tiny proportion of 11.4% by 2004.11
A growing body of evidence demonstrates that individuals with diverse backgrounds increase both innovation and creativity within groups.12 Taking an example from the corporate world, financial performance was improved in gender-diverse teams, which outperformed non-diverse teams in terms of average economic growth, return on equity, debt/equity ratios, greater market share, higher sales revenue and increased profits overall.13 One analysis found that race-based and gender-based diversity improved economic growth but was important in understanding human interactions.14
The need for gender parity at all levels of organisations is nowhere as apparent as within medical science, where collaborative working groups that are gender heterogeneous produce better quality science.15 Gender parity in leadership comes closest to being attained in research-oriented oncology societies, for example, AACR and EACR, which have female board representation of 46.7% and 40.0%, respectively. In addition, AACR has the only female president among international societies, as well as a female CEO, identified by this audit. In contrast, the SLACOM, OEGHO, AOU, JSCO, JSMO and the HKCTS had no female representation on their boards within the reference period of this article.
The importance of having equal female representation in the oncology physician workforce was underscored in a recent paper, which pointed out that women practice medicine differently than men and are more likely to adhere to clinical guidelines. These investigators found that patients treated by female physicians had lower 30-day mortality rates (p<0.001) and fewer 30-day readmissions (p<0.001) than patients treated by male physicians.16
The proportion of elderly in the global populations is rapidly increasing17 and, together with treatment advances, means that more patients will need care for chronic conditions and more healthcare professions, particularly in oncology, will be needed. A recent audit disclosed that within the USA, the median age of oncologists was higher than that of physicians overall and a large proportion of practising oncologists were older than 65 years. However, they also found fewer women enter the oncology field.5 Female patients may benefit from receiving medical treatment from female clinicians, and this advantage should also be extended to women, who comprise approximately 50% of the oncology population.18 It has been noted that both men and women show gender preferences, particularly for intimate examinations.19
Oncology includes women and men of diverse races, ethnicities and cultures working towards the common goal of providing optimal care for patients with cancer. Inclusion of women in international guideline development improves gender responsiveness of the health-sector workforce, making panel member diversity key in producing guidelines that are relevant to patient-specific considerations.20
A survey brought forward by the W4O Committee reported that the lack of work–family balance was cited as the main barrier to achieving gender parity in leadership roles by 52.8% of male and female respondents. Perception-based barriers to leadership also carried importance, with 39.9% and 22.8% of female participants responding that men are perceived as natural leaders while women are perceived more as a team members and supporters, and that cultural gender prejudice exists due to misconceptions about family and domestic responsibilities of women, respectively.21
These findings are supported by a survey of academic clinical department chairs who cited the constraints of traditional gender roles, manifestations of sexismin the medical environment, and lack of effective mentors as elements affecting the integration of women into leadership roles at universities. They also raised the possibility that women may devote more time to teaching and clinical activity.22
Overcoming internalised or unconscious bias manifested by both genders remains an intangible challenge that affects women and prevents some from seeking senior positions. Women may be regarded as less competent than men, even when their experience and qualifications are equivalent.23 Women must contend with behavioural double standards that describe men striving for leadership positions as ‘ambitious and direct’, whereas women exhibiting the same behaviours are labelled ‘bossy or rude’.24 It is important to note that implicit gender bias favouring men does not necessarily arise from explicitly held beliefs, with many people being genuinely unaware that this bias or generally stereotypes are affecting their decisions.25
The W4O Committee is taking steps to stimulate diversity regarding gender and also including individuals of different races, social backgrounds and those with physical disabilities. ESMO, the reference oncology society used here, is not alone in providing preceptorship, mentor, sponsor and leadership programmes.
Aiming to overcome the barriers of work–life balance and ensuring family-friendly frameworks, ESMO has begun to provide day-care during the larger ESMO congresses so participants can benefit from educational and networking activities while knowing their children are cared for by qualified adults.
Other programmes are in place to support members in career advancement with advice provided by a gender-diverse faculty. Gender balance has already been achieved in the ESMO Leaders Generation Programme of 2017, which comprises eight female and seven male oncologists who learnt the skills for successful leadership.
In addition to these programmes, ESMO also provides fellowships consisting of financial and professional support. Although women and men are equally encouraged to apply, the recipients in 2017 in clinical research were all men, whereas the translational research fellowships were women. Among the recipients of palliative care fellowships, six of eight were men and all were of diverse nationalities. ESMO may help in decreasing this gender disparity by ensuring men and women get the same opportunities.
The Annual Gender Gap Report of the World Economic Forum recently made a call for action to work on gender parity by revising its previous target estimate of globally achieving gender parity in pay and job opportunities from 80 years to over 170 years. They attribute this ‘glacial pace of change’ largely to unconscious bias.26 This unconscious bias must be countered by conscious attempts through sponsorship and mentorship programmes offering support to women and other under-represented groups.
Taking everything together, in oncology societies, especially ESMO, female membership is continuously growing. However, we must not automatically conclude from this that women will evolve over time to occupy leadership roles. In fact, a comparison of the number of female board members in 2014 with 2017 shows no change whatsoever has taken place.
Although the examples provided in this publication originate from ESMO initiatives, they are indicative of activities being pursued to varied degrees by many of the oncology societies today. They represent the necessary first steps towards providing mentorship and advancement initiatives for women and to incorporate women into all levels of oncology. As the pace of progress is slow, highlighting more rigorous action is needed. Overcoming conscious and unconscious biases that contribute to gender as well as other inequalities through training to recognise unconscious bias, nurturing, inclusiveness and consistency regardless of society, gender or ethnicity will be the accelerant to fuel the rapid change needed to reach this goal within our lifetime.
Acknowledgments
Writing assistance was provided by Jenny Powers and funded by ESMO.
Funding: This research was funded by ESMO.
Competing interests: EH-T is an employee of Janssen, the Pharmaceutical Company of Johnson & Johnson Europe, and a shareholder of Johnson & Johnson. DA has received research funding and/or honoraria from Roche, Merck Serono, Bayer Healthcare, Servier, BTG, Terumo, Sanofi Oncology, Eli Lilly and has participated in non-financial roles as ECCO Executive Board member, ECCO Oncopolicy Group member, EORTC Task Force member (Gastrointestinal cancers)—Global PI function with MOLOGEN, IMPALA trial (MGN 1703 as investigative agent). GC has received research funding and/or honoraria from Roche, Novartis, Pfizer and has participated in non-financial roles as a member of Steering Committee in clinical trials, member of data safety monitoring committee for clinical trials. EG has participated as Advisor for Roche, Neomed Therapeutics and Ellypses Pharma. MCG has received research funding and/or honoraria from MSD, BMS, Roche Astra Zeneca, Takeda and Eli Lilly. CR has been a consultant for BMS, Roche, Novartis, Pierre Fabre, MDS and Amgen. CS is a Scientific Consultant for SAKK (Swiss group for cancer research treatment) and has participated in non-financial roles as the ESGO Vice President, Principal Investigator for the Icon 8B Study, EUPATI Switzerland. SP has received research funding and/or honoraria from Genentech/Roche, Pfizer, Eli Lilly, MSD, Merck Serono, BMS, Novartis, Astra Zeneca, Boehringer Ingelheim, Amgen, Clovis, Regeneron, Janssen, Takeda and has participated in non-financial roles on the IASLC Board of Directors 2014–2017, SAKK lung group Vice-president, SAMO Vice-president, Froome Past President (2011–2017), ETOP Foundation Council/Scientific coordinator, ESMO president elect 2010–2021, PI ALEX trial, Genentech Steering committee, PI academic trials ETOP, EORTC/SAKK, FMH, IASLC, AACR.
Provenance and peer review: Not commissioned; internally peer reviewed.
Data on ESMO membership might vary by a few percentagepoints at specific time points because of the evolving nature ofthe ESMO database. Nevertheless, this variation does not impacton the trends brought forth in this article.
References
- 1. WHO Spotlight on statistics. Gender and health workforce statistics, 2008. [Google Scholar]
- 2. Thornton G. 2016. Women in business: turning promise into practice. Grant Thorton Individual Business Report. http://www.grantthorton.co.uk
- 3. Langer A, Meleis A, Knaul FM, et al. Women and Health: the key for sustainable development. Lancet 2015;386:1165–210. 10.1016/S0140-6736(15)60497-4 [DOI] [PubMed] [Google Scholar]
- 4. Valantine HA, Collins FS. National Institutes of Health addresses the science of diversity. Proc Natl Acad Sci U S A 2015;112:12240–2. 10.1073/pnas.1515612112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kirkwood MK, Kosty MP, Bajorin DF, et al. Tracking the workforce: the American Society of Clinical Oncology workforce information system. J Oncol Pract 2013;9:3–8. 10.1200/JOP.2012.000827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. ESMO members by age and gender database.
- 7. Connection A. ASCO: women in oncology: breaking down barriers and looking to the future, 2016:14–19. [Google Scholar]
- 8. ESMO. 2016 ESMO W4O exploratory study on the gender-related challengesof medical oncology professionals, presented at the Women forOncology session on 9 October 2016, during ESMO, 2016. [Google Scholar]
- 9. Summer 2013 presented at the ESMO Women for Oncology Forum on 28 ESMO exploratory study on the challenges for female oncologists in reaching leadership positions, 2013. [Google Scholar]
- 10. Forum WE. 2016. The Global Gender Gap Report http://reports.weforum.org/global-gender-gap-report-2016.
- 11. Jagsi R, Guancial EA, Worobey CC, et al. The "gender gap" in authorship of academic medical literature—a 35-year perspective. N Engl J Med 2006;355:281–7. 10.1056/NEJMsa053910 [DOI] [PubMed] [Google Scholar]
- 12. Fenwick GD, Neal DJ. Effect of gender composition on group performance. Gend Work Organ 2001;8:205–25. 10.1111/1468-0432.00129 [DOI] [Google Scholar]
- 13. Rohner U, Dougan B. Gender diversity and corporate performance Technical report. Zürich: Credit Suisse Research Institute, 2012. [Google Scholar]
- 14. Herring C. Does diversity pay? Amer Sociol Rev 2009;74:208–24. [Google Scholar]
- 15. Campbell LG, Mehtani S, Dozier ME, et al. Gender-heterogeneous working groups produce higher quality science. PLoS One 2013;8:e79147 10.1371/journal.pone.0079147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians. JAMA Intern Med 2017;177:206–13. 10.1001/jamainternmed.2016.7875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. WHO, 2015. Ageing and Health, Fact Sheet No. 404. http://www.who.int/mediacentre/factsheets/fs404/en/
- 18. World Cancer Research Fund International. Continuous update project;Worldwide data. [Google Scholar]
- 19. Kerssens JJ, Bensing JM, Andela MG. Patient preference for genders of health professionals. Soc Sci Med 1997;44:1531–40. 10.1016/S0277-9536(96)00272-9 [DOI] [PubMed] [Google Scholar]
- 20. Institute of Medicine of the National Academies. standards for developing trustworthy clinical practice guidelines (CPGs) In: Clinical practice guidelines we can trust, 2011. [Google Scholar]
- 21. Op Cit. ESMO W4O exploratory study on the gender-relatedchallenges of medical oncology professionals, 2016 presented at theESMO Women for Oncology Session on 9 October 2016, during ESMO, 2016. [Google Scholar]
- 22. Yedidia MJ, Bickel J. Why aren't there more women leaders in academic medicine? The views of clinical department chairs. Acad Med 2001;76:453–65. 10.1097/00001888-200105000-00017 [DOI] [PubMed] [Google Scholar]
- 23. Foschi M. Double standards for competence: theory and research. Annu Rev Sociol 2000;26:21–42. 10.1146/annurev.soc.26.1.21 [DOI] [Google Scholar]
- 24. Op Cit. ASCO: Women in oncology: breaking down barriers and looking to the future. ASCO Connection, 2016:14–19. [Google Scholar]
- 25. Moss-Racusin CA, Dovidio JF, Brescoll VL, et al. Science faculty's subtle gender biases favor male students. Proc Natl Acad Sci U S A 2012;109:16474–9. 10.1073/pnas.1211286109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. World Economic Forum, 2016. The global gender gap report. https://www.weforum.org/reports/the-global-gender-gap-report-2017
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
esmoopen-2018-000423supp001.pdf (161.4KB, pdf)


