Abstract
Background:
Venous thromboembolism is a common complication in patients with glioma. The clotting factor von Willebrand factor (VWF) is a highly adhesive procoagulant molecule that mediates platelet adhesion to endothelial and subendothelial surfaces. In the current analysis, we examined The Cancer Genome Atlas (TCGA) data to assess the effect of VWF gene expression on prognosis in patients with lower grade gliomas (LGGs).
Methods:
For newly diagnosed gliomas, we evaluated the association between and overall survival in the genomic data commons TCGA LGG dataset in TCGA. Survival data of the glioma subgroup were extracted for analysis and generation of Kaplan–Meier curves for overall survival.
Results:
Lower grade gliomas with less VWF gene expression had significantly better survival than those with more VWF gene expression (hazard ratio 0.64, 95% confidence interval 0.44–0.92, P 0.015 log rank test). The effect of VWF gene expression on survival was even more evident when the sample was analyzed as three groups (P = 0.00019). IDH1, TP53, and ATRX mutations are present in 40% or more adult LGGs.
Conclusion:
The deleterious prognostic effect of VWF expression in LGGs is not surprising, given its role in other cancers. Therefore, VWF gene expression may be a clinically important risk marker in LGG.
Keywords: Glioblastoma, glioma, survival, von Willebrand factor
INTRODUCTION
Malignant brain tumors are accompanied by hypercoagulability. Glioblastoma multiforme (GBM), the most common primary tumor of the central nervous system, is associated with heightened coagulation and venous thromboembolism (VTE). The circulating substance inducing the hypercoagulability is uncertain. Anticoagulants are frequently administered to GBM patients, although these agents increase the risk of intracerebral hemorrhage.[1]
Venous thromboembolism is a common complication in patients with glioma.[2] VTE may be a prognostic factor for these patients.[3] Thrombin an enzyme in blood plasma, causes the clotting of blood by converting fibrinogen to fibrin. In lower grade gliomas (LGGs), thrombin is a growth stimulant. Intracerebral infusion of argatroban, a specific thrombin inhibitor, reduces brain edema and neurologic deficits in a rat glioma model. Thrombin immunoreactivity is found in cultured rat glioma cells and human glioblastoma. In addition, thrombin induces glioma cell proliferation in vitro; whereas argatroban reduces glioma mass.[4]
Another clotting factor, von Willebrand factor (VWF), is a highly adhesive procoagulant molecule that mediates platelet adhesion to endothelial and subendothelial surfaces. Normally VWF is expressed exclusively in endothelial cells and megakaryocytes. However, a few studies have reported V detection in cancer cells of nonendothelial origin including osteosarcoma and glioma,[5] and VWF is a prognostic factor in GBM.[6] In the current analysis, we examined The Cancer Genome Atlas (TCGA) data to assess the effect of VWF gene expression on prognosis in patients with LGGs.
METHODS
For newly diagnosed gliomas, we evaluated the association between VWF and overall survival in the genomic data commons (GDC) TCGA LGG dataset in TCGA. To access and analyze the data we used as follows:
GDC Data Portal (https://portal.gdc.cancer.gov/)
UCSC Xena browser (https://xenabrowser.net)
Oncomine (https://oncomine.org)]
cBioportal (http://cbioportal.org).
Survival data of the glioma subgroup were extracted for analysis and generation of Kaplan–Meier curves for overall survival. The optimal cutoff was identified by methods described in the R2 web-based application (http://r2.amc.nl); the method divides the sample, ascending order gene expression, into equal-sized groups. Further details have been published.[7]
Gene expression is quantitated as Fragments Per Kilobase of transcript per Million mapped reads upper quartile (fpkm-uq),which is an RNA-Seq-based expression normalization method.[8]
RESULTS
We analyzed data from 513 patients with primary LGG. The patients’ mean age was 43 ± 14 (mean ± standard deviation) years old, with 55% of the patients were male, 45% were female, 92.1% were white, 4.1% were African-American, 1.6% were Asian, 0.2% were American Indian or Alaska native, and 1.9% were unclassified. Mean survival was 7.8 years.
VWF was significantly overexpressed in LGGs, especially in astrocytomas (P = 0.008, t = 2.471, Fold Change: 1.084, data from RefSeq Genes, UCSC refGene, July 2009, hgl8, NCBI 36.1, March 2006) [Figure 1].
Figure 1:
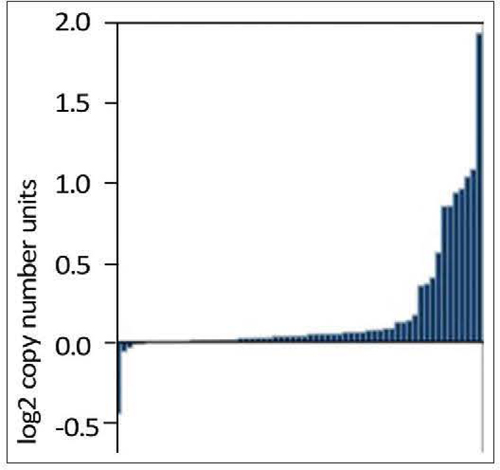
Expression of von Willebrand factor in 63 astrocytomas (The Cancer Genome Atlas-DU-7299–01A-21D-2023–01). Von Willebrand factor is significantly overexpressed (P = 0.008, t = 2.471 , fold change: 1.084). RefSeq Genes, UCSC refGene, July 2009, hg18, NCBI 36.1, March 2006
Histology of tumors and VWF expression in the current analysis are listed in Table 1. Expression of VWF was increased in astrocytomas, when compared to oligodendroglioma or oligoastrocytoma (P = 0.045, one way ANOVA). VWF was most often mutated and amplified in diffuse gliomas [Figure 2].
Table 1:
Histology and von Willebrand factor gene expression (fpkm-uq) of 510 primary tumors in this study
| n | VWF | |
|---|---|---|
| Astrocytoma | 192 | 17.8±0.07 |
| Oligoastrocytoma | 128 | 17.5±1 |
| Oligodendroglioma | 190 | 17.6±1 |
VWF: Von Willebrand factor
Figure 2:
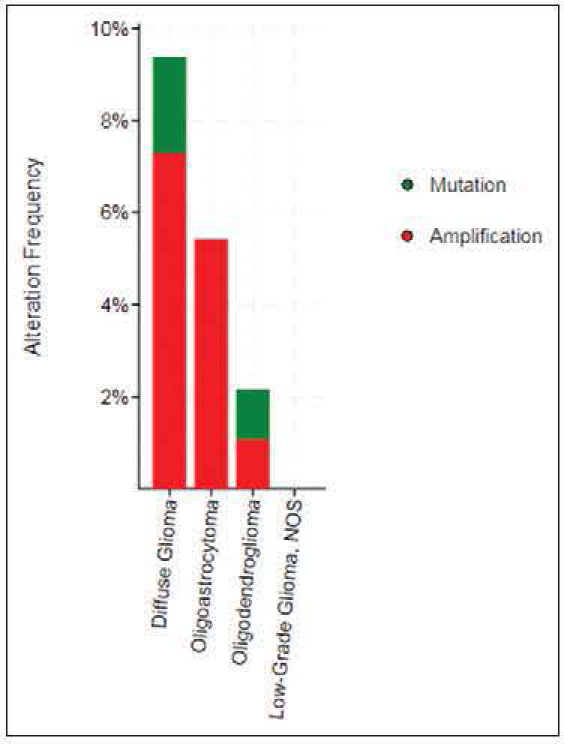
Von Willebrand factor was most often mutated and amplified in diffuse gliomas (http://cbioportal.org)
Survival of patients with astrocytomas was significantly worse than the survival of patients with oligodendroglioma or oligoastrocytoma (P = 0.0064, log rank test) [Figure 3].
Figure 3:
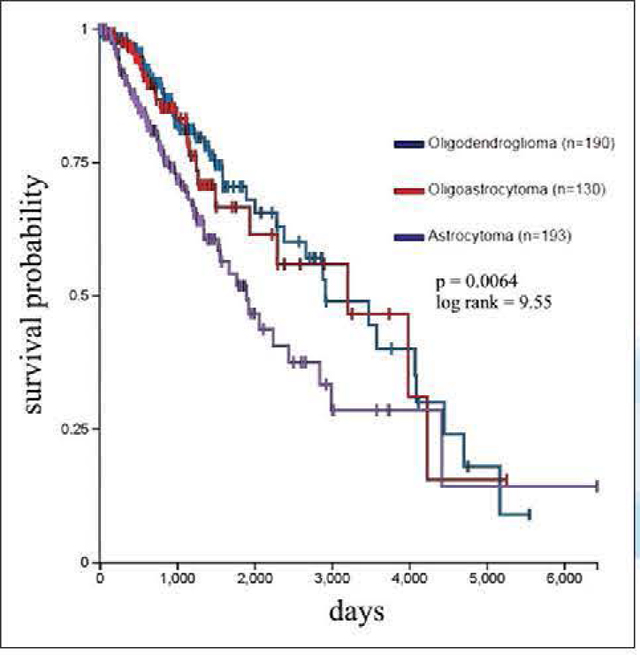
Survival of lower grade glioma by histology in 513 patients. Survival of astrocytomas was significantly worse than oligodendroglioma or oligoastrocytoma (P = 0.0064, log rank test)
Survival versus VWF gene expression is shown in Figure 4. Lower grade gliomas with less VWF gene expression had significantly better survival than those with more VWF gene expression (hazard ratio 0.64, 95% confidence interval 0.44–0.92, P = 0.015 log rank test). The effect of VWF gene expression on survival was even more evident when the sample was analyzed as three groups (P = 0.00019).
Figure 4:
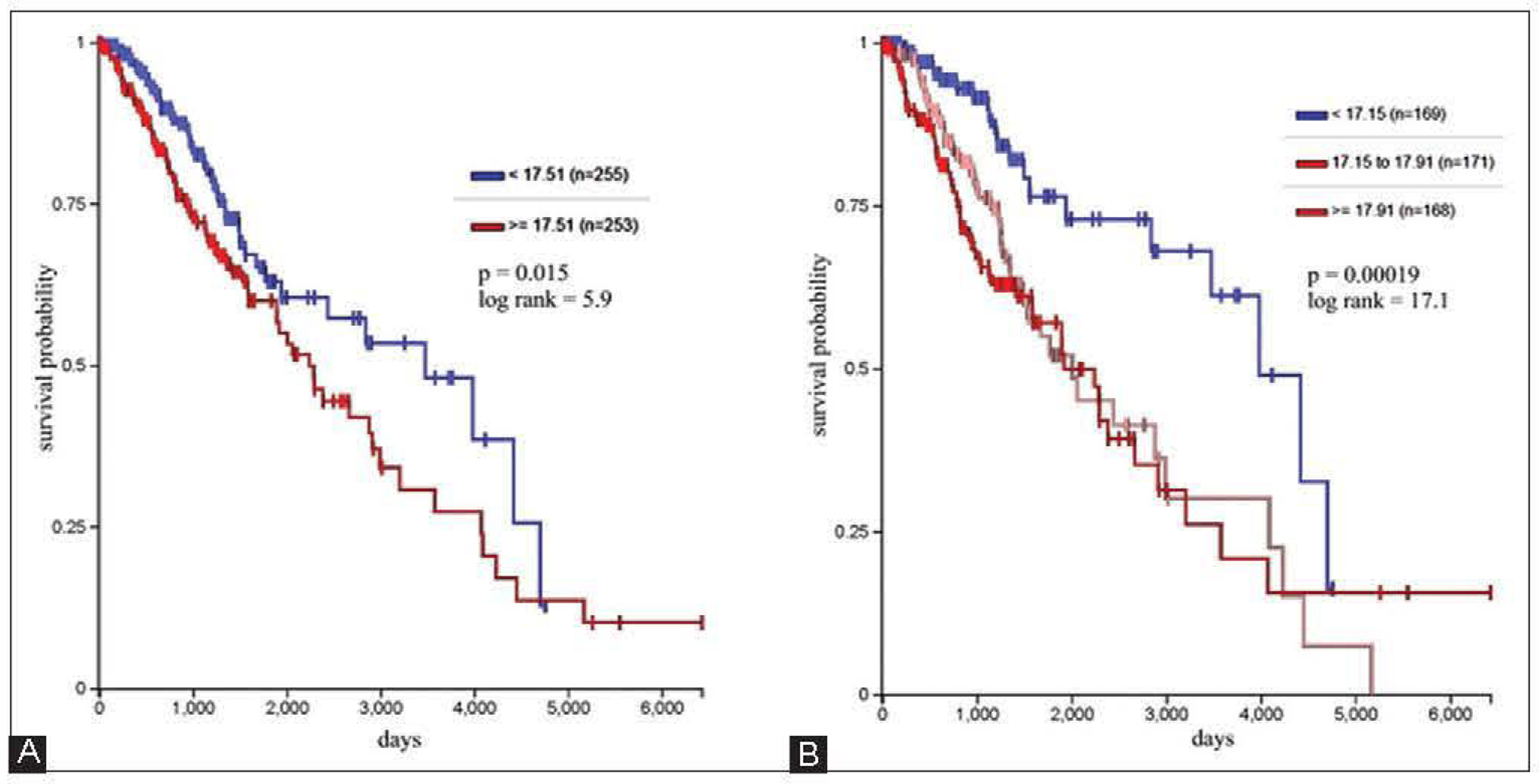
Survival versus Von Willebrand factor gene expression in 508 patients. (A) Lower grade gliomas with less Von Willebrand factor gene expression had significantly better survival than those with more VWF gene expression (hazard ratio 0.64, 95% confidence interval 0.44–0.92, P = 0.015 log rank test). (B) The effect of Von Willebrand factor gene expression on survival was even more evident when the sample was analyzed as three groups (P = 0.00019)
IDHI, TP53, and ATRX mutations are present in 40% or more adult LGGs.[9,10] Among these tumors, as noted above, patients with astrocytomas have poorer survival than patients with oligoastrocytomas or oligodendrogliomas; prognosis of oligoastrocytomas or oligodendrogliomas is approximately equivalent. When we analyzed the data with Cox regression, expression had a significant effect on survival (P = 0.02) that was unrelated to the effect of IDH1 expression (P = 0.062), TP53 expression (P = 0.135), independent of ATRX expression (P = 0.021), and histology (astrocytoma versus ohgoastrocytoma and oligodendroglioma, P = 0.002).
DISCUSSION
Lower grade glioma is a uniformly fatal disease of young adults with survival averaging approximately 7 years.
Although LGG patients have better survival than patients with high-grade (WHO Grade III/IV) glioma, almost all LGGs eventually progress to high-grade glioma and death. Data from the surveillance, epidemiology and end Results program of the National Cancer Institute suggest that for the majority of LGG patients, overall survival has not significantly improved over the past three decades.[11]
Multiple prognostic factors have been described: Tumor histology, grade, location contrast enhancement, patient age, performance status, and seizure history [12] Survival probability in patients with a glioma having a high median tumor blood flow (mTBF) has been shown to be lower in patients with a glioma having a low mTBF.[13] Recently, tumor genome has proven to be a prognostic factor,[9,10] as well as F13Al copy number segments.[14]
Armand Trousseau first reported the relationship between malignant tumors and coagulation in 1865. Trousseau diagnosed the syndrome in himself 2 years later, dying soon afterward of gastric cancer. Recent findings suggest that genetic pathways within tumor cells might trigger thrombotic phenomena, worsening prognosis.[15]
The deleterious prognostic effect of VWF expression in LGGs is not surprising, given its role in other cancers, Von Willebrand factor fibers promote cancer-associated platelet aggregation in malignant melanoma of mice and humans,[16] and cancer cell-derived VWF enhances the metastasis of gastric adenocarcinoma [17] A manifestation of Heyde’s syndrome may be involved.
Heyde’s syndrome is defined as gastrointestinal bleeding from angiodysplasia in the presence of aortic stenosis. The syndrome is caused by the induction of von Willebrand disease Type IIA due to depletion of vWF in blood flowing through the narrowed aortic valvular orifice. As the stenotic aortic valve constricts, blood flow through the valve is augmented to maintain cardiac output. The narrow opening and a high flow rate produces increased blood shear stress. The stress causes VWF to uncoil in the same way it would on encountering tissue damage.[18] Perhaps, the inverse correlation between von Willebrand Factor and survival in patients with glioma is another sign of this same phenomenon.
In conclusion, gene expression may be a clinically important risk marker in LGG. The risk of VTE in glioma patients is high and extends beyond the postoperative period. The procoagulant molecule tissue factor appears to play an important role, but other markers are needed.[19] VWF may represent a new marker. Although thromboembolic events lead to worse outcomes, risks of anticoagulant administration should be better defined. Further studies of VWF would be worthwhile.
Footnotes
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Norden AD, Bartolomeo J, Tanaka S, Drappatz J, Ciampa AS, Doherty LM, et al. Safety of concurrent bevacizumab therapy and anticoagulation in glioma patients. JNeurooncol 2012;106:121–5. [DOI] [PubMed] [Google Scholar]
- 2.Al Megren M, De Wit C, Al Qahtani M, Le Gal G, Carrier M. Management of venous thromboembolism in patients with glioma. Thromb Res 2017;156:105–8. [DOI] [PubMed] [Google Scholar]
- 3.Simanek R, Vormittag R, Hassler M, Roessler K, Schwarz M, Zielinski C, et al. Venous thromboembolism and survival in patients with high-grade glioma. Neuro On col 2007;9:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hua Y, Tang L, Keep RF, Schallert T, Fewel ME, Muraszko KM, et al. The role of thrombin in gliomas. J Thromb Haernost 2005;3:1917–23. [DOI] [PubMed] [Google Scholar]
- 5.Mojiri A, Stoletov K, Carrillo MA, Willetts L, Jain S, Godbout R, et al. Functional assessment of von willebrand factor expression by cancer cells of non-endothelial origin. Oncotarget 2017;8:13015–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marfia G, Navone SE, Fanizzi C, Tabano S, Pesenti C, Abdel Hadi L, et al. Prognostic value of preoperative von willebrand factor plasma levels in patients with glioblastoma. Cancer Med 2016;5 :1783–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meier K R2 Support Team. In: R2 Tutorials. Release 3.1.2 Ch. 8. 201 7. p. 73–82. [Google Scholar]
- 8.Shahriyari L Effect of normalization methods on the performance of supervised learning algorithms applied to HTSeq-FPKM-UQ data sets: 7SK RNA expression as a predictor of survival in patients with colon adenocarcinoma. BriefBioinform 201 7. doi: 10.1093/bibibbx153. [DOI] [PubMed] [Google Scholar]
- 9.Venneti S, Huse JT. The evolving molecular genetics of low-grade glioma. Adv Anat Pathol 2015;22:94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buckner J, Giannini C, Eckel-Passow J, Lachance D, Parneyi, Laack N, et al. Management of diffuse low-grade gliomas in adults - Use of molecular diagnostics. Nat Rev Neurol 2017;13:340–51. [DOI] [PubMed] [Google Scholar]
- 11.Claus EB, Walsh KM, Wieneke JK, Molinaro AM, Wiemels JL, Schildkraut JM, et al. Survival and low-grade glioma: The emergence of genetic information. Neurosurg Focus 2015;38:E6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stupp R, Janzer RC, Hegi ME, Villemure JG, Mirimanoff RO. Prognostic factors for low-grade gliomas. Semin Oneal 2003;30:23–8. [DOI] [PubMed] [Google Scholar]
- 13.Furtner J, Bender B, Braun C, Schittenhelm J, Skardelly M, Em em ann U, et al. Prognostic value of blood flow measurements using arterial spin labeling in gliomas. PLoS One 2014;9:e99616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lehrer S, Dembitzer FR, Rheinstein PH, Rosenzweig KE. In primary glioblastoma fewer tumor copy number segments of the Fl3A1 gene are associated with poorer survival. Thromb Res 2018;167:12–4. [DOI] [PubMed] [Google Scholar]
- 15.Varki A Trousseau’s syndrome: Multiple definitions and multiple mechanisms. Blood 2007;110: 1723–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bauer AT, Suckau J, Frank K, Desch A, Goertz L, Wagner AH, et al. Von willebrand factor fibers promote cancer-associated platelet aggregation in malignant melanoma of mice and humans. Blood 2015;125:3153–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang AJ, Wang M, Wang Y, Cai W, Li Q, Zhao TT, et al. Cancer cell-derived von willebrand factor enhanced metastasis of gastric adenocarcinoma. Oncogenesis 2018;7:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.BaturP StewartWJ, Isaacson JH. Increased prevalence of aortic stenosis in patients with arteriovenous malformations of the gastrointestinal tract in heyde syndrome. Arch Intern Med 2003;163:1821–4. [DOI] [PubMed] [Google Scholar]
- 19.Jenkins EO, Schiff D, Mackman N, Key NS. Venous thromboembolism in malignant gliomas. J Thromb Haemost 2010;8:221–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


