Abstract
Veterans in rural areas and veterans involved in the criminal justice system have experienced less access to, and use of, health care. However, there is limited information on the treatment needs and health care access of justice-involved veterans who live in rural areas. This study used national Veterans Health Administration data from fiscal year 2014 to examine the interactive effect of rural/urban residence and justice involvement on mental health and substance use disorder treatment entry among veterans diagnosed with mental health or substance use disorders. Of veterans residing in rural areas, 15,328 (2.5%) were justice-involved and 607,819 (97.5%) veterans had no known justice involvement. Among veterans in urban areas, 54,525 (4.3%) were justice-involved and 1,213,766 (95.7%) had no known justice involvement. Rural residence was associated with lower access to mental health or substance use disorder treatment in the non-justice-involved sample but not the justice-involved sample. Justice-involvement was associated with higher odds of entering mental health or substance use disorder treatment for veterans in rural and in urban areas. Substance use disorder treatment entry could be improved for all veterans, particularly rural veterans who are not justice-involved. Telehealth, outreach services, and integrated treatment may help address challenges to treatment entry experienced by rural veterans and justice-involved veterans.
Keywords: rural health, criminal justice, mental disorders, substance use disorders, veterans, mental health services
Among the veteran population in the US, 5.2 million – roughly 24% - live in rural areas with 2.9 million rural veterans (56%) enrolled in Veterans Health Administration (VHA) care (Department of Veterans Affairs, 2017). Although prior literature has focused on health disparities among rural veterans compared to their urban counterparts (Kondo et al., 2017), rural veterans involved in the criminal justice system are a largely understudied population who may have heightened risk for poor access and use of treatment services. Justice-involved veterans – military veterans detained by or under the supervision of the criminal justice system – who live in rural areas have lower odds of engaging in mental health treatment, and of entering and engaging in addiction treatment, compared to their urban counterparts (Finlay, Smelson, et al., 2016; Finlay et al., 2017). However, these veterans were not compared to other rural veterans with similar conditions who were not involved in the criminal justice system. Thus, our understanding of the treatment needs of justice-involved veterans in the context of the broader population of veterans served at VHA is limited. The current study aims to examine the intersection of rural residence status with justice status among veterans diagnosed with mental health or substance use disorders who sought treatment in VHA facilities.
Broader trends within VHA may explain less use of mental health and substance use disorder treatment observed among justice-involved veterans in rural areas compared to their urban counterparts; however, research findings on differences in treatment use between rural and urban veterans are mixed. Rural veterans have lower odds of receiving mental health services compared to urban veterans (Mott, Grubbs, Sansgiry, Fortney, & Cully, 2015; Teich, Ali, Lynch, & Mutter, 2017). Among veterans who were part of VHA intensive mental health care services, veterans who lived in isolated rural areas received less rehabilitation, psychotherapy, and crisis intervention services than urban veterans in the same program (Mohamed, Neale, & Rosenheck, 2009). Receipt of pharmacotherapy for alcohol or opioid use disorders was lower among veterans in rural areas compared to urban areas, regardless of justice involvement (Finlay, Binswanger, et al., 2016; Finlay, Harris, et al., 2016). Other research has found that more rural veterans had at least one mental health treatment visit compared to urban veterans (Johnson et al., 2015). Among veterans who served in recent conflicts in Iraq or Afghanistan, rural veterans had higher odds of receiving pharmacological or psychotherapy treatments for PTSD or depression than urban veterans (Hudson et al., 2014). Although not directly compared to urban residents, among rural residents who used stimulants, less than 20% received substance abuse treatment in the two-year period after study baseline (Carlson et al., 2010). Another study found similarly low rates of addiction treatment use among rural residents who used stimulants (Curran, Ounpraseuth, Allee, Small, & Booth, 2011). These studies suggest that rural residents face barriers to addiction treatment.
Studies of rural veterans and other rural residents have identified barriers to treatment. For example, bureaucratic difficulties enrolling and understanding the VHA system and a lack of understanding of eligibility requirements were cited by women veterans in rural areas as barriers to treatment in general (Brooks, Dailey, Bair, & Shore, 2016). Travel distances (Brooks et al., 2016), stigma or a lack of privacy to seek treatment (Browne et al., 2016), a mistrust of health care providers (Goins, Williams, Carter, Spencer, & Solovieva, 2005), and a lack of perceived need for substance use disorder treatment (Borders, Booth, Stewart, Cheney, & Curran, 2015) also have been identified as barriers for rural veterans. Finally, health care system barriers such as a lack of treatment options or integrated services that address the array of patients’ needs (Browne et al., 2016; Sigmon, 2014) and a dearth of primary care physicians to provide office-based pharmacotherapy for addiction treatment (Quest, Merrill, Roll, Saxon, & Rosenblatt, 2012; Rosenblatt, Andrilla, Catlin, & Larson, 2015) may explain lower rates of treatment access and use in rural areas. Among women veterans in rural areas, mental health treatment was the second most frequently requested local service (Brooks et al., 2016).
Many of the challenges faced by rural and urban residents in accessing health care may be further exacerbated by justice-involvement. For example, public transportation or transportation services for medical care are limited in rural areas (Buzza et al., 2011; Goins et al., 2005). Therefore, Veterans who have lost their driver’s license because of criminal justice-related issues may struggle to keep appointments. In urban areas, adults who were referred by the criminal justice system to outpatient methadone treatment had higher odds of delayed admission to treatment than adults who self-referred (Gryczynski, Schwartz, Salkever, Mitchell, & Jaffe, 2011), and in rural areas where substance use disorder treatment options are more limited than in urban areas (Sigmon, 2014), waitlists may be even longer. Mistrust of the health care system or health care professionals has been cited by both justice-involved populations (Howerton et al., 2007; Wainwright, McDonnell, Lennox, Shaw, & Senior, 2017) and rural populations (Goins et al., 2005) as a barrier to treatment seeking. Whether these negative attitudes are especially prominent among rural residents with justice involvement is unknown. Criminal justice related barriers to treatment cited by those on parole include previous incarceration having interrupted treatment or administrative/bureaucratic processes, stigma, and poor treatment by health care providers (Marlow, White, & Chesla, 2010).
Criminal justice mandates or legal supervision also can affect treatment entry, through results are mixed as to how. Rural residents who used drugs and had a court mandate to attend treatment had three times higher odds of entering substance use disorder treatment than residents without a mandate (Oser et al., 2011). In a national sample, patients referred from the criminal justice system to substance use disorder treatment had higher odds of waiting more than one month for treatment compared to those self-referred (Andrews, Shin, Marsh, & Cao, 2013). Receipt of mental health or addiction treatment services is relatively low among criminally justice involved samples, but there are noteworthy limitations to the study methodologies. For example, in a nationally representative sample, people on probation or parole were more likely to have received substance use disorder treatment in the past 12 months as compared to the general population; however, only 28% of people on probation or parole had received alcohol or drug treatment in their lifetime (Vaughn, DeLisi, Beaver, Perron, & Abdon, 2012). Furthermore, it is unclear whether the results were limited to participants with an active mental health or substance use disorder diagnosis so appropriate use of treatment for this sample is unclear. Similarly, a longitudinal study of rural residents on probation or parole found that 69% of the sample did not use mental health services and 61% did not use addiction treatment services over 1.5 years (Mowbray, McBeath, Bank, & Newell, 2016), but is it unclear if the analyses were limited to participants with a mental health or substance use disorder diagnosis.
Among rural residents with alcohol use disorder some, but not all, types of justice involvement were associated with treatment entry. Being on probation, and being arrested and booked for drug-related charges or driving under the influence (DUI) were significantly associated with any alcohol or drug treatment received, but being on parole or being arrested and booked for other crimes (e.g., property, crimes against people, drunkenness) were not significantly linked (Booth, Curran, Han, & Edlund, 2013). Of note, 62% of the sample with justice involvement did not enter, or perceive a need for, treatment, suggesting that many justice-involved adults with alcohol use disorder are not getting needed treatment. Previous research indicated that justice-involved veterans were less likely to enter mental health and substance use disorder treatment at VHA facilities than homeless veterans (McGuire, Rosenheck, & Kasprow, 2003) and veterans with a prison history had lower odds of receiving pharmacotherapy for opioid use disorder than veterans not justice-involved (Finlay, Harris, et al., 2016).
Rural residence and justice involvement have been examined separately in relation to disparities in mental health or addiction treatment use. The literature is mixed for rural versus urban veterans and justice-involved versus non-justice-involved veterans. Furthermore, there are numerous barriers to treatment for both rural and justice-involved veterans, but it is unknown whether these factors interact and whether veterans who live in rural areas and are justice-involved have the most difficulty accessing mental health or substance use disorder treatment.
Current Study
To determine their potential multiplicative effects, we examined whether residence status and justice involved status were associated with entry into VHA mental health and substance use disorder treatment among all veterans at VHA with mental health or substance use disorder diagnoses. Based on previous literature indicating disparities in treatment use (Kondo et al., 2017), we hypothesized that veterans in urban areas would have higher odds of entering treatment compared to veterans in rural areas. We hypothesized that justice-involved veterans would have lower odds of entering treatment than other veterans because most veterans (83%) are incarcerated for crimes other than drug- or DUI-related charges (Bronson, Carson, Noonan, & Berzofsky, 2015) and previous research indicated that justice-involved veterans are less likely to enter VHA care than other veterans (Finlay, Harris, et al., 2016; McGuire et al., 2003). Finally, we also hypothesized an interaction effect such that the negative effect of justice involvement would be even more pronounced in rural areas compared to urban areas.
Method
Participants and Data Source
This is a retrospective observational study of veterans who used VHA health care services. The VHA Corporate Data Warehouse, which is a national database of electronic health records, was used to identify patients who received a mental health or substance use disorder diagnosis (excluding those in remission) during an outpatient or inpatient visit at a VHA facility in fiscal year 2014 (October 1, 2013 through September 30, 2014); these patients were included in the study. Justice-involvement, rural or urban residence, mental health and substance use disorder diagnoses, and treatment use were identified from the Corporate Data Warehouse database and from the Homeless Outreach Management and Evaluation System database, which includes information collected by VHA staff during homeless and justice outreach services. This study was approved by the Stanford University Institutional Review Board and the VA Palo Alto Research & Development committee.
Measures
Justice involvement
The VHA has two programs for justice-involved veterans. The Health Care for Reentry Veterans (HCRV) program conducts outreach with veterans in prisons, and the Veterans Justice Outreach (VJO) program conducts outreach in other criminal justice settings, primarily jails and courts (Blue-Howells, Clark, van den Berk-Clark, & McGuire, 2013). VHA staff who provide this outreach serve a variety of functions, including helping to facilitate VHA benefits paperwork, identifying and scheduling treatment at VHA facilities, and assistance in navigating the complex VHA care delivery and benefits system. In the VHA, clinic stop codes are three-digit codes that indicate the type of outpatient care and record workload that occurred during a VHA outpatient visit. Veterans were considered justice-involved if they received a 591 clinic code, indicating contact with the HCRV program, or a 592 clinic code, indicating contact with the VJO program, prior to or during fiscal year 2014. Clinic codes were drawn from the Corporate Data Warehouse database. In addition, veterans who had a Homeless Outreach Management and Evaluation System record indicating contact with the HCRV program or the VJO program also were considered justice-involved. Veterans with no known contact with HCRV or VJO are referred to in this manuscript as other veterans.
Mental health or substance use disorder diagnoses
Patients who received International Classification of Diseases-9 (ICD-9) diagnosis codes indicating mental health or substance use disorders were included in the study. Mental health diagnoses were grouped into the following categories: depressive disorders (296.2, 296.3, 301.12, 300.4, 293.83, 298.0, 311.0, 311.9, 296.9, 309.0, 309.1), PTSD (309.81), anxiety disorders (300.02, 300.0), bipolar disorder (296.x except 296.2, 296.3, and 296.9), schizophrenia (295.x except 295.5), other mental health disorders (297.0, 297.1, 297.2, 297.3, 297.8, 297.9, 298.1, 298.2, 298.3, 298.4, 298.8, 298.9), or personality disorders (301.x except 301.12). Substance use disorder diagnoses were grouped into the following categories: alcohol use disorder (291.x, 303.0, 303.9, 303.91, 303.92, 305.0, 305.01, 305.02), opioid use disorder (304.0, 304.7, 305.5), cocaine use disorder (304.2, 305.6), amphetamine use disorder (304.4, 305.7), cannabis use disorder (304.3, 305.2), sedative use disorder (304.1, 305.4), or other drug use disorders (292.0, 292.1, 292.11, 292.12, 292.2, 292.81, 292.82, 282.83, 292.84, 292.85, 292.89, 292.90, 304.5, 304.6, 304.8, 304.9, 305.3, 305.8, 305.9).
Residence
Rural or urban residence was drawn from the Corporate Data Warehouse files based on the patient’s last known address. Type of residence was defined using the U.S. Census Bureau definition (Ratcliffe, Burd, Holder, & Fields, 2016). Urban areas were defined as having an urban core of at least 1,000 residents per square mile or 50,000 or more people in the urban nucleus. Rural areas were defined as non-urban areas.
Treatment use
All treatment use occurred within the VHA health care system. For veterans diagnosed with a mental health disorder, we counted the number of mental health outpatient visits, mental health inpatient days, and mental health residential days recorded in their electronic health record in the one-year period following their first mental health diagnosis. For veterans diagnosed with depressive disorders, PTSD, bipolar disorders, and schizophrenia we examined pharmacy records to determine whether veterans received pharmacotherapy for their diagnosed conditions. Based on the 2010 VHA clinical guidelines, we only included medications that were recommended as first line (likely to be beneficial) or second line (some benefit or trade-off between benefit and harm). Therefore, we did not calculate receipt of pharmacotherapy for other mental health disorders or personality disorders because there were no medications recommended that met our criteria. Entry to mental health treatment was coded as any use of mental health outpatient, inpatient, or residential care or any receipt of pharmacotherapy for depressive disorders, PTSD, bipolar disorder, or schizophrenia in the one-year period following first mental health diagnosis.
For veterans diagnosed with a substance use disorder, we counted the number of substance use disorder outpatient visits and substance use disorder residential days recorded in their electronic health record in the one-year period following their first substance use disorder diagnosis. For veterans diagnosed with alcohol or opioid use disorder, we examined pharmacy records to determine whether veterans received pharmacotherapy for their diagnosed conditions. As with mental health disorders, medications for alcohol or opioid use disorder were selected using VHA clinical guidelines and were limited to first or second line medications. We did not calculate receipt of pharmacotherapy for any of the substance use disorder diagnoses because there were not medications that met our criteria for inclusion. Entry to substance use disorder treatment was coded as any use of substance use disorder outpatient or residential care or any receipt of pharmacotherapy for alcohol or opioid use disorders in the one-year period following first substance use disorder diagnosis.
Patient characteristics
Demographic variables included gender; age; ethnicity/race (Hispanic, non-Hispanic: American Indian/Alaskan Native, Asian, Black, White; based on the Bureau of Census categories); marital status (single, married, separated/divorced, widowed); and homeless status (drawn from a homeless indicator variable, receipt of housing services, and ICD-9 codes for unstable housing and homelessness), which indicates a person is at-risk for or experiencing homelessness or receiving homeless services. Military-related characteristics included service in Iraq or Afghanistan (yes/no) and service-connected disability rating (None, < 50%, ≥ 50%), which reflects a VHA-determined disability occurring during or aggravated by military service. Demographic and military characteristics were coded from records collected the same day the veteran received her or his first mental health or substance use disorder diagnosis during fiscal year 2014, or if missing then was drawn from the next health care visit where that information was available. Service in Iraq or Afghanistan was drawn from the Iraq/Afghanistan Roster, which is a database of veterans who served in conflicts in Iraq or Afghanistan and enrolled in VHA care. The Deyo comorbidity index, a sum of up to 17 comorbid medical diagnoses, such as HIV, liver disease, diabetes, and congestive heart failure (Deyo, Cherkin, & Ciol, 1992) was coded from records from the one-year period after the first mental health or substance use disorder diagnosis and was a proxy for overall physical health.
Data Analysis
We examined descriptive statistics of patient characteristics and the proportion of patients diagnosed with mental health or substance use disorders, stratified by rural or urban residence and justice status. We then conducted 2 mixed effects logistic regression models with main effects for residence and justice status and the interaction of the two variables in each model, adjusting for all other patient characteristics and including a random effect for facility (N = 141 VHA medical centers). To examine entry into mental health treatment as the dependent variable, we limited the sample to veterans who were diagnosed with a mental health disorder and examined justice-involved veterans compared to other veterans (model 1). For entry into substance use disorder treatment as the dependent variable, we limited the sample to veterans who were diagnosed with a substance use disorder and compared justice-involved veterans with other veterans (model 2). Because the interaction effects were significant for most models, to facilitate interpretation, we conducted two additional mixed effects logistic regression models focused only on rural veterans. We examined the association between justice-involvement and entry into mental health or substance use disorder treatment, adjusting for all other patient characteristics and included a random effect for facility.
Results
Patient Characteristics
Of 623,147 rural VHA patients in fiscal year 2014 who were diagnosed with a mental health or substance use disorder, 15,328 (2.5%) were justice involved and 607,819 (97.5%) veterans had no known justice-related contact. Of 1,268,291 urban VHA patients in fiscal year 2014 who were diagnosed with a mental health or substance use disorder, 54,525 (4.3%) were justice-involved and 1,213,766 (95.7%) veterans had no known justice-related contact. In general, justice-involved veterans were younger, had higher rates of homelessness, and had fewer co-morbid medical conditions compared to other veterans (Table 1). More justice-involved veterans served in Iraq or Afghanistan compared to other veterans.
Table 1.
Patient Characteristics of Veterans with Mental Health or Substance Use Disorders by Residence and Justice Status in Fiscal Year 2014
| Characteristics | Rural | Urban | ||
|---|---|---|---|---|
|
| ||||
| Justice-involved (n = 15,328) |
Other (n =607,819) |
Justice-involved (n = 54,525) |
Other (n = 1,213,766) |
|
|
| ||||
| % | % | % | % | |
| Gender | ||||
| Female | 6 | 8 | 6 | 11 |
| Male | 94 | 92 | 94 | 89 |
| Age | ||||
| < 35 | 26 | 10 | 21 | 14 |
| 35–44 | 16 | 9 | 13 | 11 |
| 45–54 | 22 | 14 | 27 | 16 |
| 55–64 | 26 | 28 | 31 | 27 |
| 65+ | 9 | 39 | 8 | 33 |
| Hispanic | 4 | 3 | 8 | 9 |
| Non-Hispanic | ||||
| American | 3 | 2 | 1 | 1 |
| Indian/Alaskan | ||||
| Native | ||||
| Asian | 1 | 1 | 1 | 2 |
| Black/African | 15 | 10 | 37 | 25 |
| American | ||||
| White | 77 | 84 | 52 | 63 |
| Marital status | ||||
| Single | 31 | 15 | 39 | 23 |
| Married | 27 | 56 | 19 | 46 |
| Divorced/separated | 40 | 25 | 40 | 27 |
| Widowed | 2 | 4 | 3 | 4 |
| Homeless | ||||
| No | 92 | 99 | 87 | 98 |
| Yes | 8 | <1 | 13 | 2 |
| Service in Iraq or Afghanistan | ||||
| No | 71 | 85 | 79 | 82 |
| Yes | 29 | 15 | 21 | 18 |
| Service-connected disability rating | ||||
| None | 35 | 33 | 44 | 34 |
| 0–49% | 28 | 24 | 28 | 26 |
| 50–100% | 37 | 42 | 29 | 40 |
| Deyo comorbidity index | ||||
| 0 conditions | 64 | 48 | 63 | 52 |
| 1 condition | 19 | 22 | 19 | 21 |
| 2 conditions | 7 | 11 | 7 | 10 |
| 3+ conditions | 10 | 18 | 11 | 17 |
Mental health and substance use disorder diagnoses for the sample are reported in Table 2. Among veterans with mental health or substance use disorders, depression was the most common mental health disorder with 66% of rural justice-involved veterans, 62% of rural other veterans, 63% of urban justice-involved veterans, and 61% of urban other veterans with this diagnosis. PTSD and anxiety were the second and third most common mental health disorders. Less than 20% of veterans in the sample were diagnosed with bipolar disorder, schizophrenia, other mental health disorders, or personality disorders. Among veterans with substance use disorders, alcohol use disorder was the most common condition with 49% of rural justice-involved veterans, 17% of rural other veterans, 52% of urban justice-involved veterans, and 19% of urban other veterans with this diagnosis. Other drug use disorders were the second most common group of substance use disorders for all veterans. Less than 20% of justice-involved veterans (both rural and urban) and less than 6% of other veterans (rural and urban) were diagnosed with opioid, cocaine, amphetamine, cannabis, or sedative use disorders.
Table 2.
Mental Health and Substance Use Disorder Diagnoses Among Veterans by Residence and Justice Status in Fiscal Year 2014
| Diagnoses | Rural | Urban | ||
|---|---|---|---|---|
|
| ||||
| Justice-involved (n = 15,328) |
Other (n= 607,819) |
Justice-involved (n = 54,525) |
Other (n = 1,213,766) |
|
|
| ||||
| % | % | % | % | |
| Mental health diagnoses | ||||
| Depression | 66 | 62 | 63 | 61 |
| Post-traumatic stress disorder | 51 | 42 | 42 | 39 |
| Anxiety | 35 | 31 | 29 | 31 |
| Bipolar disorder | 16 | 6 | 16 | 8 |
| Schizophrenia | 7 | 3 | 10 | 5 |
| Other mental health disorders | 6 | 3 | 8 | 3 |
| Personality disorders | 12 | 3 | 11 | 3 |
| Substance use disorder diagnoses | ||||
| Alcohol use disorder | 49 | 17 | 52 | 19 |
| Opioid use disorder | 13 | 2 | 13 | 3 |
| Cocaine use disorder | 13 | 1 | 23 | 4 |
| Amphetamine use disorder | 7 | 1 | 7 | 1 |
| Cannabis use disorder | 19 | 4 | 20 | 5 |
| Sedative use disorder | 3 | 1 | 3 | 1 |
| Other drug use disorders | 29 | 4 | 33 | 6 |
| Co-occurring mental health and substance use disorder diagnoses | 56 | 16 | 58 | 19 |
Treatment Entry
Among veterans in rural areas who were diagnosed with a mental health disorder, 93% of justice-involved veterans and 80% of other veterans entered mental health treatment. Among veterans in urban areas who were diagnosed with a mental health disorder, 94% of justice-involved veterans and 83% of other veterans entered mental health treatment. Among veterans in rural areas who were diagnosed with a substance use disorder, 55% of justice-involved veterans and 20% of other veterans entered substance use disorder treatment. Among veterans in urban areas who were diagnosed with a substance use disorder, 59% of justice-involved veterans and 28% of other veterans entered substance use disorder treatment.
Rural Residence and Justice Involvement
Among veterans with a mental health disorder, the first logistic regression model examined the interaction of residence and justice status associated with entry into mental health treatment. The interaction of residence by justice status was significant (β = 0.09, standard error [SE] = 0.04, p < .001), as were the main effects for residence (β = −0.08, SE = 0.01, p < .001) and justice status (β = −0.84, SE = 0.02, p < .001), adjusting for other covariates. Justice-involved veterans, whether rural or urban residents, had higher odds of entering mental health treatment than other veterans (Figure 1). Other veterans who lived in rural areas had the lowest odds of entering treatment. The interaction effect indicated that justice-involved veterans had the same odds of entering mental health treatment regardless of residence; whereas, among other veterans, living in a rural area was associated with lower mental health treatment entry.
Figure 1.
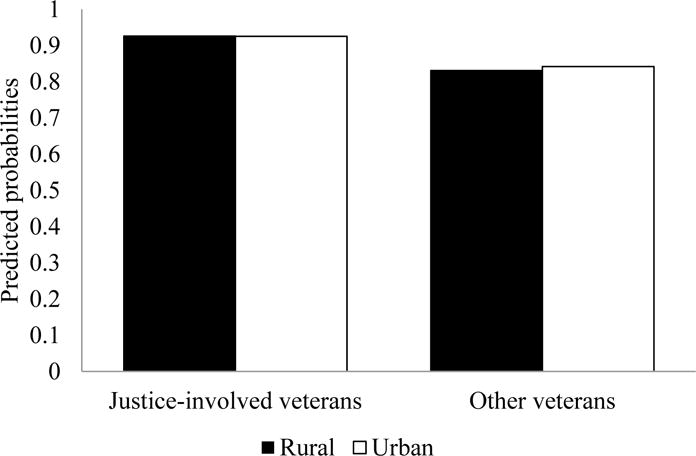
Interaction effect of justice status and residence and predicted probabilities of entry into mental health treatment among justice-involved veterans and other veterans who have mental health conditions.
The second logistic regression model examined residence and justice-involved status among veterans diagnosed with a substance use disorder. The interaction term of residence by justice status was significant (β = 0.28, SE = 0.03, p < .001) and there were significant main effects for residence (β = −0.33, SE = 0.01, p < .001) and justice status (β = 1.07, SE = 0.01, p < .001), adjusting for other covariates. Justice-involved veterans, whether they lived in urban or rural areas, had higher odds of entering substance use disorder treatment than other veterans (Figure 2). Other veterans who lived in rural areas had the lowest odds of entering treatment. The interaction term indicated that justice-involved veterans who lived in rural areas had lower odds of entering substance use disorder treatment compared to justice-involved veterans who lived in urban areas. Among other veterans a similar pattern was observed: Veterans in rural areas had lower odds of entering substance use disorder treatment. Because of these differences by geographic location, we analyzed veterans in rural areas separately in the remaining models (results for veterans in urban areas are reported in the Appendix).
Figure 2.
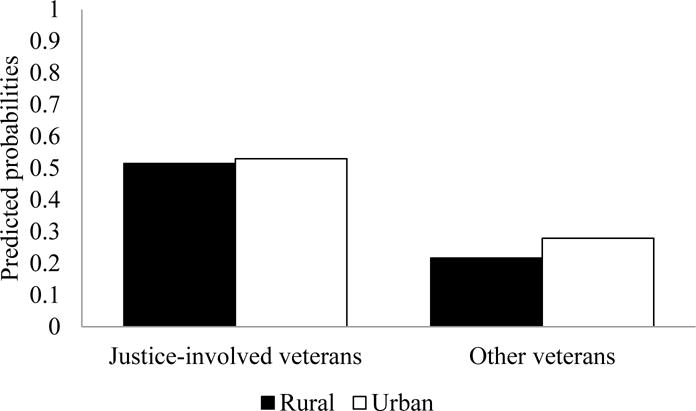
Interaction effect of justice status and residence and predicted probabilities of entry into substance use disorder treatment among justice-involved veterans and other veterans who have substance use disorder conditions.
Treatment Entry Among Rural Veterans
Among rural veterans with a mental health disorder, justice-involved veterans had 2.59 times higher odds (95% confidence interval [CI] = 2.42-2.77) of entering mental health treatment compared to other veterans (Table 3). Other patient factors associated with entry into mental health treatment included being female, being from an ethnic or racial minority group, using homeless services or being at-risk for homelessness, serving in Iraq or Afghanistan, having a service-connected disability rating, or having comorbid medical conditions.
Table 3.
Patient Characteristics Associated with Mental Health or Substance Use Disorder Treatment Entry Among Rural Veterans in Fiscal Year 2014
| Characteristics | Mental health treatment entry | Substance use disorder treatment entry | ||
|---|---|---|---|---|
|
| ||||
| OR | 95% CI | OR | 95% CI | |
| Justice-involved (ref: no) | 2.59*** | [2.42–2.77] | 3.61*** | [3.45–3.77] |
| Gender (ref: male) | 1.19*** | [1.15–1.22] | 1.24*** | [1.17–1.31] |
| Age, years (ref: <35) | ||||
| 35–44 | 0.95** | [0.92–0.99] | 0.87*** | [0.82–0.92] |
| 45–54 | 0.88*** | [0.85–0.91] | 0.68*** | [0.65–0.72] |
| 55–64 | 0.70*** | [0.67–0.73] | 0.40*** | [0.38–0.43] |
| 65+ | 0.41*** | [0.40–0.42] | 0.21*** | [0.20–0.22] |
| Race/ethnicity (ref: non-Hispanic White) | ||||
| American Indian/Alaskan Native | 1.06 | [1.00–1.12] | 1.07 | [0.96–1.18] |
| Asian | 1.15*** | [1.08–1.24] | 0.92 | [0.80–1.06] |
| Black/African American | 1.20*** | [1.17–1.23] | 1.40*** | [1.35–1.47] |
| Hispanic | 1.05* | [1.01–1.10] | 1.06 | [0.98–1.14] |
| Not married (ref: married) | 0.97*** | [0.96–0.99] | 0.88*** | [0.85–0.90] |
| Homeless (ref: no) | 2.80*** | [2.47–3.17] | 2.64*** | [2.45–2.86] |
| Service in Iraq/Afghanistan (ref: no) | 1.07*** | [1.04–1.10] | 0.97 | [0.92–1.01] |
| Service-connected disability rating (ref: no) | ||||
| < 50% | 1.12*** | [1.10–1.14] | 1.04* | [1.00–1.08] |
| ≥ 50% | 1.83*** | [1.80–1.86] | 1.09*** | [1.06–1.13] |
| Comorbid medical conditions | 1.10*** | [1.09–1.10] | 1.06*** | [1.04–1.07] |
Note. OR = odds ratio; CI = confidence interval.
p < .05.
p < .01.
p < .001.
Among rural veterans diagnosed with a substance use disorder, justice-involved veterans had 3.61 times higher odds (95% CI = 3.45-3.77) of entering substance use disorder treatment than other veterans. Other patient factors associated with entry into substance use disorder treatment included being female, being under age 35, being Black/African American, using homeless services or being at-risk for homelessness, having a service-connected disability rating, or having comorbid medical conditions.
Discussion
The current study examined the associations of rurality of residence and justice status with treatment access among veterans at VHA with mental health or substance use disorder diagnoses. Although main and interaction effects were observed, results largely contradicted hypotheses. Justice-involved veterans had higher odds of entering mental health and substance use disorder treatment than other veterans. The only difference by residence observed for justice-involved veterans was that urban veterans had higher odds of entering substance use disorder treatment compared to rural veterans. For other veterans, urban veterans had higher odds of entering mental health and substance use disorder treatment compared to rural veterans, consistent with prior literature (Mohamed et al., 2009; Mott et al., 2015; Teich et al., 2017).
Justice-involved veterans had higher odds of entering mental health and substance use disorder treatment than other veterans, which may be explained by criminal justice factors, such as court mandates, or dedicated support services provided to justice-involved veterans through VHA outreach. Veterans who were justice-involved may have had court mandates or legal supervision through probation or parole, which have been previously linked with higher odds of treatment entry (Oser et al., 2011; Vaughn et al., 2012). However, even among adults with alcohol use disorder, parole was not associated with treatment entry (Booth et al., 2013), suggesting that a clear treatment need and legal supervision may not be sufficient to compel treatment attendance. Barriers to treatment such as bureaucratic processes interrupted by incarceration, stigma, and lack of trust for health care providers (Brooks et al., 2016; Goins et al., 2005; Howerton et al., 2007; Marlow et al., 2010; Wainwright et al., 2017) may have been addressed by outreach workers from the VJO and HCRV programs who help to manage paperwork and other administrative processes and can provide an initial positive experience entering VHA treatment. For example, motivational interviewing, one technique used by outreach staff, has been shown to improve treatment entry for veterans exiting jail (Davis, Baer, Saxon, & Kivlahan, 2003).
Mental Health Treatment
Entry into mental health treatment was relatively high for all veterans in the study, with an 80% or higher rate of treatment entry observed for all groups. The VHA has a variety of programs for special populations to support their use of VHA, including the Office of Rural Health (Department of Veterans Affairs, 2017), the VJO and HCRV programs (Blue-Howells et al., 2013), and Women’s Health programs (Department of Veterans Affairs, 2010). Although veterans in rural areas who were not justice-involved had the lowest rate of mental health treatment entry, the majority entered treatment. Focusing on other aspects of their treatment beyond access, such as resolution of symptoms or receipt of evidence-based practices may yield results that provide more guidance on how to improve the mental health of veterans at VHA.
Substance Use Disorder Treatment
Compared to mental health treatment, entry into substance use disorder treatment is low. Just over half of justice-involved veterans in the current study entered substance use disorder treatment. Among justice-involved populations, receipt of pharmacotherapy or psychosocial treatment for substance use disorders has been linked with reduced drug and alcohol use, retention in treatment, and reduced criminal activity and recidivism (Amato et al., 2005; Dolan et al., 2005; Gryczynski et al., 2012; Jonas et al., 2014; Mattick, Breen, Kimber, & Davoli, 2009; Rawson et al., 2004). Improved entry to substance use disorder treatment for justice-involved veterans will likely positively impact their health as well as a societal impact of crime reduction.
For other veterans, only 20% in rural areas and 28% in urban areas entered substance use disorder treatment, similar to studies of rural residents from the general population (Carlson et al., 2010; Curran et al., 2011). Treatment options are less available in rural areas (Sigmon, 2014), such as a dearth of providers with buprenorphine waivers (Quest et al., 2012; Rosenblatt et al., 2015), but clearly substance use disorder treatment options need to be improved across the VHA system. Telehealth, which patients indicate is an acceptable treatment modality (Benavides-Vaello, Strode, & Sheeran, 2013), may be one option to increase availability of substance use disorder treatment in VHA facilities and communities where options are limited. Transportation difficulties and lack of privacy that have been mentioned as barriers to treatment (Brooks et al., 2016; Browne et al., 2016; Buzza et al., 2011; Goins et al., 2005) also may be addressed by telehealth. Substance use disorder treatment has not been successfully integrated across VHA primary care or mental health services (Tracy, Trafton, Weingardt, Aton, & Humphreys, 2007), which may partially explain lower rates of addiction treatment entry in the current study. Rural residents have cited a lack of integrated treatment services that address their array of needs as a barrier to treatment (Browne et al., 2016). Veterans in the current study may be prioritizing medical or mental health care over addiction treatment. Finally, among people who use cocaine, rural residents had a significantly lower perceived need for treatment than rural residents (Borders et al., 2015). Perhaps many of these veterans in this study, particularly in rural areas, did not perceive a need for substance use disorder treatment.
Limitations
There are limitations to our study. First, we were unable to assess treatment that veterans were receiving at VA Centers or in the community. Among others, veterans who lived especially far from VHA facilities may have sought community treatment options. Future data linkage to examine non-VHA treatment use in conjunction with VHA health care use will help inform these results. Second, our methods of identifying residence status or justice status are limited. For example, last known residence may not be accurate for homeless veterans, and there may have been veterans with criminal justice involvement who did not have contact with the VJO or HCRV programs and were coded as not justice-involved. Finally, justice-involved veterans may have entered treatment because of criminal justice factors such as court mandates or probation requirements to attend mental health or substance use disorder treatment; we did not have specific information on mandated treatment requirements or veterans who self- or attorney-referred to treatment to help improve criminal justice outcomes (e.g., court sentencing). We could identify veterans who participated in treatment courts (e.g., Veterans Treatment Court, drug court) and likely had court mandates to attend mental health or substance use disorder treatment as part of their court experience, but they represented only 5% of justice-involved veterans and there was no impact on the pattern of results when they were removed from the sample. Understanding the ways in which the justice system may shape veterans’ engagement with VHA health care will be important for future research to examine more thoroughly in order to fully understand why justice-involved veterans were more likely to access care than veterans without justice involvement.
Conclusions
The majority of justice-involved and other veterans accessed mental health treatment, regardless of residence. Entry into substance use disorder treatment, however, was low, especially for rural veterans without justice involvement. Lessons may be learned from mental health settings about how to improve access to substance use disorder care for veterans. Promising strategies to improve addiction treatment access include telehealth, which may address a lack of treatment options or transportation difficulties, outreach services to help veterans navigate the VHA bureaucracy, and integration of addiction treatment into primary care and mental health care settings. Interagency coordination among the VA, community treatment providers, and other entities such as criminal justice partners may be needed to overcome the general lack of treatment resources in rural areas. Importantly, motivating veterans to initiate and actively engage in treatments (U.S. Department of Health and Human Services, 2016), along with improving access to care, is necessary to help people with mental health and substance-related conditions achieve recovery.
Supplementary Material
Acknowledgments
Andrea Finlay was funded by a VA Health Services Research & Development (HSR&D) Career Development Award (CDA 13-279). Alex Harris and Christine Timko were funded by VA HSR&D Research Career Scientist Awards (RCS 14-232 and Senior RCS 00-001, respectively). All authors were employed and funded by the Department of Veterans Affairs when this study was conducted. The views expressed are those of the authors and do not represent the position or policy of the Department of Veterans Affairs or the United States Government.
Contributor Information
Andrea K. Finlay, Center for Innovation to Implementation (Ci2i), VA Palo Alto Health Care System, and National Center on Homelessness Among Veterans, Department of Veterans Affairs
Alex H. S. Harris, Center for Innovation to Implementation (Ci2i), VA Palo Alto Health Care System, and Department of Surgery, Stanford University School of Medicine
Joel Rosenthal, Veterans Justice Programs, Department of Veterans Affairs.
Jessica Blue-Howells, Veterans Justice Programs, Department of Veterans Affairs.
Sean Clark, Veterans Justice Programs, Department of Veterans Affairs.
Bessie Flatley, National Center on Homelessness Among Veterans.
Christine Timko, Center for Innovation to Implementation (Ci2i), VA Palo Alto Health Care System, and Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine.
References
- Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: Available evidence to inform clinical practice and research. Journal of Substance Abuse Treatment. 2005;28:321–329. doi: 10.1016/j.jsat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Andrews CM, Shin HC, Marsh JC, Cao D. Client and program characteristics associated with wait time to substance abuse treatment entry. The American Journal of Drug and Alcohol Abuse. 2013;39(1):61–68. doi: 10.3109/00952990.2012.694515. [DOI] [PubMed] [Google Scholar]
- Benavides-Vaello S, Strode A, Sheeran BC. Using technology in the delivery of mental health and substance abuse treatment in rural communities: A review. Journal of Behavioral Health Services & Research. 2013;40(1):111–120. doi: 10.1007/s11414-012-9299-6. [DOI] [PubMed] [Google Scholar]
- Blue-Howells JH, Clark SC, van den Berk-Clark C, McGuire JF. The U.S. Department of Veterans Affairs Veterans Justice Programs and the sequential intercept model: Case examples in national dissemination of intervention for justice-involved veterans. Psychological Services. 2013;10(1):48–53. doi: 10.1037/a0029652. [DOI] [PubMed] [Google Scholar]
- Booth BM, Curran GM, Han X, Edlund MJ. Criminal justice and alcohol treatment: Results from a national sample. Journal of Substance Abuse Treatment. 2013;44:249–255. doi: 10.1016/j.jsat.2012.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borders TF, Booth BM, Stewart KE, Cheney AM, Curran GM. Rural/urban residence, access, and perceived need for treatment among African American cocaine users. Journal of Rural Health. 2015;31(1):98–107. doi: 10.1111/jrh.12092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronson J, Carson A, Noonan M, Berzofsky M. Veterans in prison and jail, 2011-12 (Report No NCJ249144) Washington, DC: 2015. Retrieved from. https://www.bjs.gov/content/pub/pdf/vpj1112.pdf. [Google Scholar]
- Brooks E, Dailey NK, Bair BD, Shore JH. Listening to the patient: Women veterans’ insights about health care needs, access, and quality in rural areas. Military Medicine. 2016;181(9):976–981. doi: 10.7205/MILMED-D-15-00367. [DOI] [PubMed] [Google Scholar]
- Browne T, Priester MA, Clone S, Iachini A, DeHart D, Hock R. Barriers and facilitators to substance use treatment in the rural south: A qualitative study. Journal of Rural Health. 2016;32(1):92–101. doi: 10.1111/jrh.12129. [DOI] [PubMed] [Google Scholar]
- Buzza C, Ono SS, Turvey C, Wittrock S, Noble M, Reddy G, Reisinger HS. Distance is relative: Unpacking a principal barrier in rural healthcare. Journal of General Internal Medicine. 2011;26(Suppl 2):648–654. doi: 10.1007/s11606-011-1762-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson RG, Sexton R, Wang J, Falck R, Leukefeld CG, Booth BM. Predictors of substance abuse treatment entry among rural illicit stimulant users in Ohio, Arkansas, and Kentucky. Substance Abuse. 2010;31(1):1–7. doi: 10.1080/08897070903442459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran GM, Ounpraseuth ST, Allee E, Small J, Booth BM. Trajectories in use of substance abuse and mental health services among stimulant users in rural areas. Psychiatric Services. 2011;62(10):1230–1232. doi: 10.1176/appi.ps.62.10.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis TM, Baer JS, Saxon AJ, Kivlahan DR. Brief motivational feedback improves post-incarceration treatment contact among veterans with substance use disorders. Drug and Alcohol Dependence. 2003;69:197–203. doi: 10.1016/s0376-8716(02)00317-4. [DOI] [PubMed] [Google Scholar]
- Department of Veterans Affairs. VHA Directive 1330.01(1): Health care services for women veterans. 2010 Retrieved from https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=5332.
- Department of Veterans Affairs. Office of Rural Health 2015–2019 strategic plan. 2017 Retrieved from https://www.ruralhealth.va.gov/
- Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Dolan KA, Shearer J, White B, Zhou J, Kaldor J, Wodak AD. Four-year follow-up of imprisoned male heroin users and methadone treatment: Mortality, re-incarceration and hepatitis C infection. Addiction. 2005;100(6):820–828. doi: 10.1111/j.1360-0443.2005.01050.x. [DOI] [PubMed] [Google Scholar]
- Finlay AK, Binswanger I, Timko C, Rosenthal J, Clark S, Blue-Howells J, Harris AHS. Criminal Justice Policy Review. 2016. Receipt of pharmacotherapy for alcohol use disorder by male justice-involved U.S. Veterans Health Administration patients. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay AK, Harris AHS, Rosenthal J, Blue-Howells J, Clark S, McGuire J, Binswanger I. Receipt of pharmacotherapy for opioid use disorder by justice-involved U.S. Veterans Health Administration patients. Drug and Alcohol Dependence. 2016;160:222–226. doi: 10.1016/j.drugalcdep.2016.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay AK, Smelson D, Sawh L, McGuire J, Rosenthal J, Blue-Howells J, Harris AHS. U.S. Department of Veterans Affairs Veterans Justice Outreach program: Connecting justice-involved veterans with mental health and substance use disorder treatment. Criminal Justice Policy Review. 2016;27(2):203–222. doi: 10.1177/0887403414562601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay AK, Stimmel M, Blue-Howells J, Rosenthal J, McGuire J, Binswanger I, Timko C. Use of Veterans Health Administration mental health and substance use disorder treatment after exiting prison: The Health Care for Reentry Veterans program. Administration and Policy in Mental Health and Mental Health Services Research. 2017;44(2):177–187. doi: 10.1007/s10488-015-0708-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goins RT, Williams KA, Carter MW, Spencer M, Solovieva T. Perceived barriers to health care access among rural older adults: A qualitative study. Journal of Rural Health. 2005;21(3):206–213. doi: 10.1111/j.1748-0361.2005.tb00084.x. [DOI] [PubMed] [Google Scholar]
- Gryczynski J, Kinlock TW, Kelly SM, O’Grady KE, Gordon MS, Schwartz RP. Opioid agonist maintenance for probationers: Patient-level predictors of treatment retention, drug use, and crime. Substance Abuse. 2012;33(1):30–39. doi: 10.1080/08897077.2011.616816. [DOI] [PubMed] [Google Scholar]
- Gryczynski J, Schwartz RP, Salkever DS, Mitchell SG, Jaffe JH. Patterns in admission delays to outpatient methadone treatment in the United States. Journal of Substance Abuse Treatment. 2011;41:431–439. doi: 10.1016/j.jsat.2011.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howerton A, Byng R, Campbell J, Hess D, Owens C, Aitken P. Understanding help seeking behaviour among male offenders: Qualitative interview study. BMJ. 2007 doi: 10.1136/bmj.39059.594444.AE. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson TJ, Fortney JC, Williams JS, Austen MA, Pope SK, Hayes CJ. Effect of rural residence on use of VHA mental health care among OEF/OIF veterans. Psychiatric Services. 2014;65(12):1420–1425. doi: 10.1176/appi.ps.201300041. [DOI] [PubMed] [Google Scholar]
- Johnson CE, Bush RL, Harman J, Bolin J, Evans Hudnall G, Nguyen AM. Variation in utilization of health care services for rural VA enrollees with mental health-related diagnoses. Journal of Rural Health. 2015;31(3):244–253. doi: 10.1111/jrh.12105. [DOI] [PubMed] [Google Scholar]
- Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, Garbutt JC. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: A systematic review and meta-analysis. JAMA: Journal of the American Medical Association. 2014;311(18):1889–1900. doi: 10.1001/jama.2014.3628. [DOI] [PubMed] [Google Scholar]
- Kondo K, Low A, Everson T, Gordon CD, Veazie S, Lozier CC, Kansagara D. Health disparities in veterans: A map of the evidence. Medical Care. 2017;55(9 Suppl 2):S9–S15. doi: 10.1097/MLR.0000000000000756. [DOI] [PubMed] [Google Scholar]
- Marlow E, White MC, Chesla CA. Barriers and facilitators: Parolees’ perceptions of community health care. Journal of Correctional Health Care. 2010;16(1):17–26. doi: 10.1177/1078345809348201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Systematic Review. 2009;2009(3):1–32. doi: 10.1002/14651858.CD002209.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire J, Rosenheck RA, Kasprow WJ. Health status, service use, and costs among veterans receiving outreach services in jail or community settings. Psychiatric Services. 2003;54(2):201–207. doi: 10.1176/appi.ps.54.2.201. [DOI] [PubMed] [Google Scholar]
- Mohamed S, Neale M, Rosenheck RA. VA intensive mental health case management in urban and rural areas: Veteran characteristics and service delivery. Psychiatric Services. 2009;60(7):914–921. doi: 10.1176/appi.ps.60.7.914. [DOI] [PubMed] [Google Scholar]
- Mott JM, Grubbs KM, Sansgiry S, Fortney JC, Cully JA. Psychotherapy utilization among rural and urban veterans from 2007 to 2010. Journal of Rural Health. 2015;31(3):235–243. doi: 10.1111/jrh.12099. [DOI] [PubMed] [Google Scholar]
- Mowbray O, McBeath B, Bank L, Newell S. Trajectories of health and behavioral health services use among community corrections-involved rural adults. Social Work Research. 2016;40(1):7–18. doi: 10.1093/swr/svv048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oser CB, Leukefeld CG, Tindall MS, Garrity TF, Carlson RG, Falck R, Booth BM. Rural drug users: Factors associated with substance abuse treatment utilization. International Journal of Offender Therapy and Comparative Criminology. 2011;55(4):567–586. doi: 10.1177/0306624X10366012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quest TL, Merrill JO, Roll J, Saxon AJ, Rosenblatt RA. Buprenorphine therapy for opioid addiction in rural Washington: The experience of the early adopters. Journal of Opioid Management. 2012;8(1):29–38. doi: 10.5055/jom.2012.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratcliffe M, Burd C, Holder K, Fields A. Defining rural at the US Census Bureau (ACSGEO-1) 2016 Retrieved from https://www.census.gov/library/publications/2016/acs/acsgeo-1.html.
- Rawson RA, Marinelli-Casey P, Anglin MD, Dickow A, Frazier Y, Gallagher C, Methamphetamine Treatment Project Corporate A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction. 2004;99(6):708–717. doi: 10.1111/j.1360-0443.2004.00707.x. [DOI] [PubMed] [Google Scholar]
- Rosenblatt RA, Andrilla CH, Catlin M, Larson EH. Geographic and specialty distribution of US physicians trained to treat opioid use disorder. Annals of Family Medicine. 2015;13(1):23–26. doi: 10.1370/afm.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigmon SC. Access to treatment for opioid dependence in rural America: Challenges and future directions. JAMA Psychiatry. 2014;71(4):359–360. doi: 10.1001/jamapsychiatry.2013.4450. [DOI] [PubMed] [Google Scholar]
- Teich J, Ali MM, Lynch S, Mutter R. Utilization of mental health services by veterans living in rural areas. Journal of Rural Health. 2017;33(3):297–304. doi: 10.1111/jrh.12221. [DOI] [PubMed] [Google Scholar]
- Tracy SW, Trafton JA, Weingardt KR, Aton EG, Humphreys K. How are substance use disorders addressed in VA psychiatric and primary care settings? Results of a national survey. Psychiatric Services. 2007;58(2):266–269. doi: 10.1176/ps.2007.58.2.266. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC: Author; 2016. [PubMed] [Google Scholar]
- Vaughn MG, DeLisi M, Beaver KM, Perron BE, Abdon A. Toward a criminal justice epidemiology: Behavioral and physical health of probationers and parolees in the United States. Journal of Criminal Justice. 2012;40:165–173. doi: 10.1016/j.jcrimjus.2012.03.001. [DOI] [Google Scholar]
- Wainwright V, McDonnell S, Lennox C, Shaw J, Senior J. Treatment barriers and support for male ex-Armed Forces personnel in prison: Professional and service user perspectives. Qualitative Health Research. 2017;27(5):759–769. doi: 10.1177/1049732316636846. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


