Abstract
Background:
Significant macromastia is socially and physically debilitating. Reduction mammaplasty in these cases carries significant morbidity.
Methods:
Cases of inferior pedicle reduction mammaplasty performed at the breast unit, King Fahd Hospital, Jeddah, Saudi Arabia, over the last 10 years were reviewed. Inclusion criteria were cases with significant macromastia in which the distance from the supra-sternal notch to the nipple was ≥ 40 cm.
Results:
There were 26 cases of inferior pedicle reduction mammaplasty done for significant macromastia. The average age was 34.56 years (range, 16–56 years). The average sternal notch to the nipple distance was 43.08 cm (range, 40–49 cm). The average amount of breast tissue removed from the right breast was 1,057.6 g (range, 495–2,450) and from the left breast was 959.4 g (range, 445–2,100). Postoperatively, 4/26 (15.4%) had ecchymosis, 9/26 (34.6%) developed T-junction sloughing, 2/26 (7.7%) had wound infection, and 1/26 (3.8%) had unilateral partial nipple-areola complex ischemia. In 7/26 (26.9%), scars were evident and revision was performed in 4/26 (15.4%) cases. Variable degrees of upper breast flattening and bottoming were seen in most cases; however, these variations were more profound in fatty breasts and longer pedicles. The average follow-up period was 26.04 months (range, 3–68 months). All patients were satisfied with the reduced breast heaviness, but only 19/26 (73.1%) were highly satisfied with the breast shape and scars.
Conclusions:
In cases of significant macromastia, inferior pedicle reduction mammaplasty is a safe procedure. Evident scars, upper breast flattening, and bottoming adversely affect the level of satisfaction.
INTRODUCTION
Significant macromastia carries a significant physical and social morbidity.1 Different techniques have been performed to reduce the breast volume while maintaining an aesthetically acceptable shape with preservation of a viable nipple-areola complex (NAC). Free nipple graft (FNG) had been considered the safest approach in terms of nipple viability despite the flattened appearance with loss of sensation.2–5 Inferior pedicle reduction mammaplasty is considered 1 of the safe options in cases of significant macromastia.5–8
We are presenting our experience and the outcome of inferior pedicle reduction mammaplasty in cases of massive macromastia.
MATERIALS AND METHODS
From January 2008 till June 2017, the records of the breast unit at King Fahd General Hospital in Jeddah were reviewed. The search was made for cases of inferior pedicle reduction mammaplasty done for significant macromastia in which the distance from the sternal notch to the nipple (SN-N) was ≥ 40 cm. Medical records of these cases were reviewed for biographic data, admission details, operative procedures, and follow-up wound care. Level of satisfaction was assessed during the follow-up clinic visits and through telephonic interview. No specific questionnaire was used.
PREOPERATIVE PREPARATION
The procedure was discussed with the patient in addition to details about the expected scars and their location, postoperative nipple sensation, wound dehiscence, and the possibility of prolonged recovery. Standard blood tests were carried out as part of a preanesthetic clearance. A bilateral mammogram was performed for all patients ≥ 40 years. Patients < 40 years with symptoms or local findings had bilateral breast ultrasound. If the radiologic findings revealed a required follow-up in 6 months, then the procedure was postponed until the second radiologic assessment was done and cleared by radiologist.
ADMISSION AND OPERATIVE DETAILS
The patients were admitted in the morning on the same day of surgery. Skin marking was done after admission in the standard Wise pattern fashion. Minor degree of asymmetry was observed in most of the cases. Prophylactic antibiotics (1.2 gm of amoxicillin/clavulanic acid or 1 g of a first-generation cephalosporin) were given at induction of anesthesia. All the cases were performed by the same surgical team with 2 team members working simultaneously on either side of the patient.
During surgery, all patients were in supine position with arms abducted 90 degrees. Standard skin preparation with antiseptic technique was performed. Electrocautery was used for dissection throughout the procedure. A wide-base inferior pedicle was dissected and gently covered till the excess U-shaped tissue was removed. The width of the pedicle is not measured; it varies between cases based on the breast size and shape. Two cases had axillary breast and fibroadenomas that were removed at the time of surgery. One case had excision of extensive hidradenitis suppurativa in the inferior part of the breast. The excised excess breast tissue was not sent for a pathologic assessment since any suspicious clinical/radiologic findings were dealt with preoperatively. For symmetry, the residual breast mound was relied on rather than excising equal grams from both sides; however, the excised breast tissue was always weighed. Wounds were sutured in 2 layers, Coated Vicryl (polyglactin 910) sutures were used for interrupted suturing of the dermal layer, and Monocryl (poliglecaprone 25) sutures were used for continuous suturing of the subcuticular layer. The skin was approximated with Steri-strips, and no drains were used. Local infiltration of Marcain (bupivacaine hydrochloride) 0.25% subcutaneously in the scars was done. NAC color was inspected for any changes followed by the application of a pressure dressing utilizing large crepe bandages left intact for 1 week unless accidentally removed early by the patient. Oral antibiotics (amoxicillin/clavulanic acid 1 g twice daily or a first-generation cephalosporin) were given for 1 week and oral analgesics. Iron supplements were prescribed postoperatively when the preoperative hemoglobin level was ≤ 12 g/dl. All cases were discharged from the hospital 6–8 hours after surgery.
During the first postoperative clinic visit (1 week after surgery), the heavy dressing was removed and the steri-strips were changed. Use of Steri-strips was maintained for 3 weeks. The patient was instructed to resume full shower hygiene and to wear a supportive bra for 6 weeks.
RESULTS
There were 26 cases of inferior pedicle reduction mammaplasty done for significant macromastia. All patients’ neck and shoulder pain and brassiere grooving attributed to excessive breast weight (Fig. 1). The average age was 34.56 years (range, 16–56 years). All the cases, except 3, were Saudi; 50% of all were married and parous. Four cases (15.4%) were diabetic on oral hypoglycemic agents with an average glycated hemoglobin (HbA1c) of 6.8%. Two (7.7%) cases were smokers. Six (23%) cases had a history of benign breast diseases, and 4 (15.4%) underwent previous lumpectomy for benign lesions. Most of the patients (15/26; 57.7%) had dark-skinned complexion with evidence of previous small scarring (on different body parts) pattern consistent with typical scarring in dark-skinned complexions. The average weight was 85.08 kg (range, 61.1–115 kg), average height was 158.57 cm (range, 145.5–177 cm) and average body mass index was 33.65 kg/m2 (range, 25.4–42.3 kg/m2). The average SN-N distance was 43.08 cm (range, 40–49 cm).
Fig. 1.
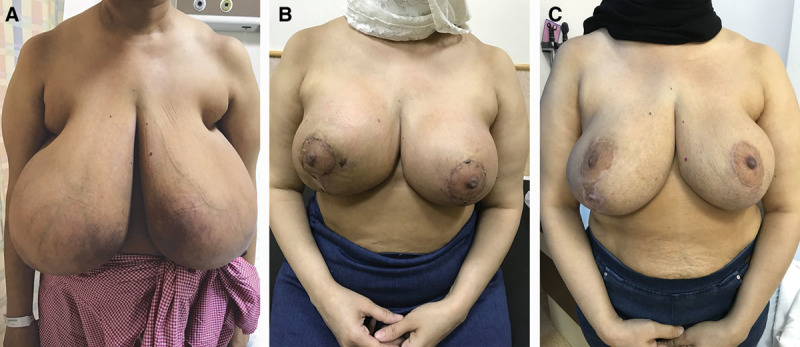
A, A 43-year-old diabetic patient; SN-N distance was 46 cm. Note the narrow breast base compared with the enlarged lower part with dilated vessels and skin irritation on the medial side. B, Four weeks postsurgery, 1,860 and 1,620 g removed from the right and left side, respectively. Slight residual ecchymosis seen on the right side. C, Eleven months postsurgery. Highly satisfied with the weight reduction but slightly unhappy about the right vertical scar.
The average hemoglobin level before surgery was 12.1 g/dl (range, 9.8–14.3 g/dl); none of the patients required a blood transfusion intraoperatively or postoperatively. The average duration of surgery was 2.94 hours (range, 2–4.2 hours). The average amount of breast tissue removed from the right and left breast was 1057.6 g (range, 495–2,450) and 959.4 g (range, 445–2,100), respectively. One patient had extensive hidradenitis suppurativa involving most of the skin of the lower surface of the breast; it was completely excised at the beginning of the procedure before exposing the pedicle (Fig. 2).
Fig. 2.

A, A 29-year-old diabetic patient; SN-N distance was 48 cm. B, A supine view showing the inframammary area with extensive skin hidradenitis suppurativa. C, Three weeks postsurgery; 2,450 and 2,100 g were removed from the right and left side, respectively.
Postoperatively, of 26 cases, 4 (15.4%) had ecchymosis and 9 (34.6%) had developed T-junction sloughing. None of the diabetic patients developed wound infection, but wound infection was seen in 2 (7.7%) cases of the nondiabetic cases.
One patient had a history of bilateral congenital nipple retraction and 2 right-sided centrally located lactational abscesses that were surgically drained a few years back (Fig. 3A). A failed trial of nipple eversion was attempted during her reduction mammaplasty, which may have added an extra-insult to the nipple vascularity; she ended up with a partial right NAC ischemia and loss (Fig. 3B). One patient experienced unilateral diminished nipple sensation, whereas 1 patient developed more nipple sensitivity; the remaining 23 cases (88.5%) had normal nipple sensation. Symmetry was maintained in all cases. In 7/26 (26.9%) cases, scars were evident and revision was performed in 4(15.4%) of them. It was observed that patients with a darker complexion had more evident scars than patients with a lighter complexion. Variable degrees of flattening of the upper breast and bottoming were seen in most cases, but it was more evident in fatty breasts and long pedicles.
Fig. 3.
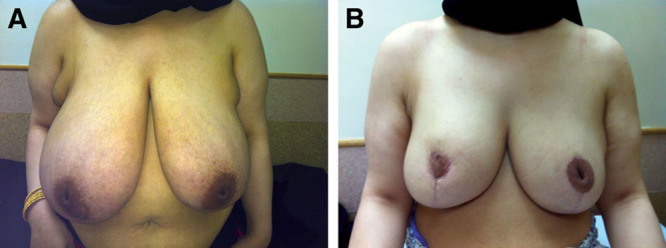
A, A 38-year-old diabetic patient; SN-N distance was 48 cm. Note the bilateral nipple retraction and the right circum-areolar scar of the previous abscess drainage. B, Six months postsurgery; 1,600 and 1,300 g were removed from the right and left side, respectively. Note partial loss of the right NAC. Bilateral axillary breasts were also excised during her surgery.
The average follow-up period was 26.04 months (range, 3–68 months). Fat necrosis manifested as soft lumps underneath the scars (periareolar or vertical) in 3/26 cases (11.5%), these 3 patients developed a temporary anxiety due to their concern about a possible malignancy; radiologic assessment performed alleviated the patients’ anxiety. All patients were happy about the reduced breast heaviness, but their satisfaction with the breast shape and scars was variable: 19/26 (73.1%) were highly satisfied, 3/26 (11.5%) were satisfied, 2/26 (7.7%) found the results acceptable but were not satisfied, and 2/26 (7.7%) were completely dissatisfied.
DISCUSSION
Large pendulous breasts affected the body image of our patients and severely limited their clothing options. Moreover, it was socially embarrassing especially for single, young women who were planning to get married. The average body mass index of our cases was 33.65 kg/m2, indicating most were overweight. Some patients had already reduced their weight, but they did not notice a change in their breast’s size. Another point to consider in overweight women is how much the breast size should be reduced. It is very important to address the body image and the proportion of body parts before the procedure; this is especially the case with patients having a large abdominal girth. Undercorrection/removing less breast tissue in these cases is advisable to avoid a disproportional appearance of the breasts as compared with the abdomen.
The preservation of the NAC vascularity and sensation is considered a priority during any cosmetic breast surgery. The heavier and more ptotic the breast, the more elongated, tortuous and weak the blood vessels are, resulting in a subsequent higher risk of NAC necrosis. This is a concern if a superior pedicle technique is planned. In cases of inferior pedicle technique, the inframammary fold-to-nipple distance (which determines pedicle length) is more relevant. The inframammary fold-to-nipple distance remains relatively constant when compared with the increasing SN-N distance in progressively enlarging breasts.6 Unfortunately, pedicle length was not documented in our cases; those with shorter pedicle length had better NAC vascularity and less bottoming with subsequent better cosmetic outcome. Based on that, the inferior pedicle technique with transposition of the NAC on the pedicle should be applicable to all breast reductions regardless of the breast size.5,6
It is sometimes stated that a certain SN-N distance (≥ 40 cm) or a certain amount of glandular resection (> 2 kg per side) presents a contraindication to the use of pedicle breast-reduction techniques, thus necessitating the use of an amputation/free nipple graft technique.5 In 1963, Wise et al.9 recommended free nipple grafting in all reductions of more than 3 bra sizes. In 1989, Hawtof et al.3 showed significant complications with the inferior pedicle reduction technique and concluded that FNGs should be considered before inferior pedicles reduction technique in those cases of severe breast weight (specimen weight over 700 g) with ptosis.3 Up until 1996, the amount considered to be safely resected increased, then Chang et al.8 successfully transposed reductions of up to 5,100 g with a very low NAC necrosis rate of 1.2% over a 7-year period.8 The actual weight (in grams) of the resected tissue varies significantly depending on the glandular/fat component ratio. The more glandular component present, the heavier the weight of the resected tissue. The glandular/fat ratio is higher (and subsequently more tissue can be safely resected) in younger nulliparous women compared with older multiparous women. This might explain the variability and hence the reported safety of increased amounts to be resected.
Amputation/FNG reduction mammaplasty might be the technique of choice for selected groups: the poor-risk elderly, women with systemic disease that could affect the vascularity of the skin flaps or impair wound healing, women with previous operative procedures in the breast affecting skin flap or pedicle vascularity, and women with indications for removal of tissue in the region of the inferior pedicle.2 The principal disadvantages of the procedure relate to the quality of the grafted nipple and areola, common occurrence of flattening and hypopigmentation, eliminated potential for future breastfeeding, and reduced nipple sensation.4,5
The inframammary incision was kept as short as possible and the medial-most and lateral-most scars were well hidden. Despite careful tension-free closure, T-junction sloughing of variable degree was seen in 9/26 (34.6%) patients; in 3 of them, it was severe. None of the T-junction sloughing led to hospital readmission but this created an anxious, unpleasant recovery period for the patient. All patients healed but with some degree of scarring. Scar revision was carried out in 4 cases 6–8 months after surgery, with good cosmetic outcome.
Although breast weight was the main reason for surgery, patient satisfaction with the weight relief was later overshadowed by the scar and the breast shape. In the first postoperative week, all of them were happy about the weight relief from their neck and shoulder. A few weeks later, the patients’ attention was directed to the surgical scars and the breast appearance. Diabetics and smokers were expected to have more wound problems compared with nondiabetic and nonsmokers, but that was not a consistent finding. Scars (even the circum-areolar ones) were more evident in darker skin cases regardless of their breast size; especially in dark skin patients, this is a point that must be clearly discussed preoperatively because of the prevalence of large breasts in dark skin women. To avoid scars, Moskovitz et al.10 performed liposuction (removing an average of 1,075 cc of tissue per breast) as an alternative procedure in African American women with a high level of satisfaction.10
There are no standard guidelines about the pathologic assessment of reduction mammaplasty specimens. The reported incidence of significant pathologic findings, that is, carcinoma and atypical hyperplasia, in reduction mammaplasty specimen ranges from 0.06% to 12.8% in the United States.11 A woman living in the United States has a 12.3%, or a 1-in-8, lifetime risk of being diagnosed with breast cancer. The risk for a woman aged 50 years without cancer of being diagnosed with breast cancer over the next 10 years is 2.3% (or 1 in 43 women who are aged 50 years will be diagnosed with breast cancer by age 60 years).12 Compared with that, the age standardized rate for breast cancer in Saudi Arabia is 22.7/100,000 for female population.13 Based on this lower incidence of breast cancer in Saudi Arabia and the lack of standard pathologic guidelines, in this series the excised specimens of reduction mammaplasty were not sent for pathologic assessment.
The presence of a wound care team in the same center might provide better care for these cases. There is a wide range of available new topical products that can treat the different stages of wound healing. It is advisable to involve the wound care team in reduction mammaplasty cases at the beginning of any wound healing problem.
CONCLUSIONS
Inferior pedicle reduction mammaplasty is a safe procedure in cases of significant macromastia. Despite the thorough preoperative discussion of the surgical outcome, patient expectation, and level of satisfaction were extremely variable.
ACKNOWLEDGMENT
The authors appreciate the efforts done by Mrs. Jill Bashore in the English language editing of the article.
Footnotes
Published online 19 June 2018.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Bostwick J. Reduction mammoplasty. In: Plastic and Reconstructive Breast Surgery. 2000:2nd ed St. Louis, Missouri: QMP; 371. [Google Scholar]
- 2.Oneal RM, Goldstein JA, Rohrich R, et al. Reduction mammoplasty with free-nipple transplantation: indications and technical refinements. Ann Plast Surg. 1991;26:117. [DOI] [PubMed] [Google Scholar]
- 3.Hawtof DB, Levine M, Kapetansky DI, et al. Complications of reduction mammaplasty: comparison of nipple-areolar graft and pedicle. Ann Plast Surg. 1989;23:3. [DOI] [PubMed] [Google Scholar]
- 4.Restifo RJ, Lalikos JF. Amputation/free nipple graft reduction mammoplasty. Oper Tech Plast Reconst Surg. 1996;3:184. [Google Scholar]
- 5.Colen SR. Breast reduction with use of the free nipple graft technique. Aesthet Surg J. 2001;21:261. [DOI] [PubMed] [Google Scholar]
- 6.Gerzenshtein J, Oswald T, McCluskey P, et al. Avoiding free nipple grafting with the inferior pedicle technique. Ann Plast Surg. 2005;55:245. [DOI] [PubMed] [Google Scholar]
- 7.Jackson IT, Bayramicli M, Gupta M, et al. Importance of the pedicle length measurement in reduction mammaplasty. Plast Reconstr Surg. 1999;104:398. [DOI] [PubMed] [Google Scholar]
- 8.Chang P, Shaaban AF, Canady JW, et al. Reduction mammaplasty: the results of avoiding nipple-areolar amputation in cases of extreme hypertrophy. Ann Plast Surg. 1996;37:585. [PubMed] [Google Scholar]
- 9.Wise RJ, Gannon JP, Hill JR. Further experience with reduction mammaplasty. Plast Reconstr Surg. 1963;32:12. [DOI] [PubMed] [Google Scholar]
- 10.Moskovitz MJ, Baxt SA, Jain AK, et al. Liposuction breast reduction: a prospective trial in African American women. Plast Reconstr Surg. 2007;119:718; discussion 727. [DOI] [PubMed] [Google Scholar]
- 11.Ambaye AB, Goodwin AJ, MacLennan SE, et al. Recommendations for pathologic evaluation of reduction mammoplasty specimens: a prospective study with systematic tissue sampling. Arch Pathol Lab Med. 2017;141:1523. [DOI] [PubMed] [Google Scholar]
- 12.DeSantis C, Ma J, Bryan L, et al. Breast cancer statistics, 2013. CA Cancer J Clin. 2014;64:52. [DOI] [PubMed] [Google Scholar]
- 13.Available at http://www.chs.gov.sa/En/HealthRecords/CancerRegistry/Pages/CancerRegistryRecords.aspx. Accessed January 27, 2018.


