Abstract
Objective
Supraglottic airway devices can be life-saving in the ‘cannot intubate, cannot oxygenate’ situation. The cricoid pressure (CP) is considered critical in the prevention of aspiration. The aim of this self-controlled study was to evaluate the effect of CP on the bag mask ventilation (BMV), and the placement of and the ventilation through, the ProSeal laryngeal mask airway (LMA).
Methods
In 60 adult patients undergoing elective surgery, after induction of anaesthesia, the effect of bimanual CP (≈30N) on BMV, ventilation through the ProSeal LMA, its anatomic position and airway seal pressures were evaluated. CP was released, the ProSeal LMA was reseated (appropriate position), the above assessments were repeated, and the effect of CP on the tidal volume (TV) and peak inspiratory pressure (PIP) was noted.
Results
Out of 60 patients, the bag mask ventilation with CP was adequate in 25 (41.7%) patients compared to 59 (98.3%) patients without CP; p<0.001. The ventilation via the ProSeal LMA with CP was excellent, adequate and impossible in 0.0% (0), 49.2% (29) and 50.8% (30) patients, respectively, compared to 93.3% (56), 6.7% (4), 0% (0) patients, respectively, without CP; p<0.001. Releasing CP and advancing the ProSeal LMA to its appropriate position significantly improved the ventilation and anatomic position scores; both p<0.001. Airway seal pressures improved significantly without CP compared to with CP; p<0.001). With the ProSeal LMA in a proper position, the CP application resulted in a significant decrease in the mean expired TV (489.14±91.62 vs. 355.08±104.42 mL) with an increase in PIP (16.72±5.01 vs. 30.71±6.74 cmH2O); both p<0.001.
Conclusion
The application of bimanual CP (≈30N) interferes with the bag mask ventilation and prevents both the correct placement and ventilation via the ProSeal LMA in adult patients.
Keywords: Cricoid pressure, laryngeal mask airway, ProSeal, ventilation
Introduction
Supraglottic airway devices play an important role in the airway management of patients in whom either intubation after induction of general anesthesia has failed or neither the face mask ventilation nor intubation is possible (1). Cricoid pressure (CP) is proposed as a method to prevent passive regurgitation and the aspiration of stomach contents during induction of anaesthesia in patients with a full stomach (2), and it has become a standard practice amongst anaesthesiologists during a rapid sequence induction/intubation (RSII). Previous studies report that the application of CP prevents both the correct placement of the classic laryngeal mask airway (LMA) and ventilation through it (3, 4). These studies suggest that CP be released at the time of the LMA placement and be reapplied after the LMA placement. However, these studies did not assess the adequacy of ventilation via the LMA following the reapplication of CP. In addition, the result of these studies of classic LMA cannot be extrapolated to the ProSeal LMA. A proper placement of the ProSeal LMA is hampered when CP is applied before its insertion (5).
The present study was designed to comprehensively evaluate the CP effect on the bag mask ventilation (BMV) and ventilation through the ProSeal LMA. The effect of CP applied after an appropriate placement of the ProSeal LMA with regard to its anatomic positioning and ventilation characteristics were also addressed. The findings from this study would provide useful clinical inputs in the airway management of the ‘cannot intubate, cannot oxygenate’ situation of patients at risk of gastric aspiration. The study hypothesis was that the application of bimanual CP may adversely affect the ventilation by facemask and ProSeal LMA. The aim of this prospective, self-controlled study was to evaluate the effect of bimanual CP on the bag mask ventilation, placement of and ventilation through the ProSeal LMA in adult patients undergoing elective surgery under general anaesthesia.
Methods
The study was approved by the Institute’s ethics committee (Ref: IEC/VMMC/SJH/Nov 13/4) and registered with the Clinical Trials Registry India (CTRI/2007/15/005981). After obtaining informed written consent from the patients, this prospective, self-controlled study was performed in 60 adults, aged 18–65 years and classified as Grade I and II physical status according to the American Society of Anesthesiologists, undergoing elective surgery, in whom the neuromuscular block was indicated as part of the anaesthetic procedure. Patients with pathology of the neck, upper respiratory tract or upper alimentary tract; gastro-esophageal reflux disease; a risk of pulmonary aspiration of gastric contents; anticipated difficult intubation, mouth opening <2.5 cm, the body mass index >30 kg m−2, reactive airway disease, and who were pregnant were excluded.
Correct application of bimanual CP was practiced before starting the study by applying a force of approximately 3 kg on a weighing scale. In this technique, the CP (≈3 kg force) was applied with fingers of one hand, while the other hand was placed beneath the cervical vertebra to support the neck. Revalidation of the force applied for CP was done after each case by reproducing the force applied, and the reading was noted by an observer not involved in the study. One investigator (SP) applied CP. A second anaesthesiologist performed the bag mask ventilation, ProSeal LMA insertion and the assessment of lung ventilation and ProSeal LMA position. Another anaesthesiologist recorded the observed variables.
All patients fasted overnight. Alprazolam 0.25 mg/0.5 mg (<50 kg/>50 kg body weight, respectively) was given orally the night before and 2 hours before surgery. In the operation theatre, standard monitoring with electrocardiography, non-invasive blood pressure, oxygen saturation, end tidal carbon dioxide and airway pressure were established.
The patient’s head was kept in the sniffing position, and the cricoid cartilage was identified. Anaesthesia was induced with propofol 2 mg kg−1 and fentanyl 2 μg kg−1. Vecuronium 0.1 mg kg−1 was administered for neuromuscular blockade. Ventilation via bag mask commenced with oxygen, nitrous oxide and isoflurane 0.6% for 3 min. The adequacy of ventilation via bag mask was observed. An adequate ventilation was defined as the chest expansion with satisfactory compliance and normal square-wave capnogram. If it was not possible to ventilate adequately via face mask, the subject was excluded. After an adequate BMV was determined, CP was applied and the BMV was again assessed.
The ProSeal LMA was inserted 3 minutes following vecuronium injection, using the introducer tool (6). The size of the Proseal LMA was as per the manufacturer’s recommendation. The ProSeal LMA was inserted until the appreciation of resistance (Position 1). The cuff was inflated with air to a pressure of 60 cmH2O using a manometer with CP and the introducer tool in place. The air inflation volume was noted. A summarized protocol is presented in Figure 1.
Figure 1.
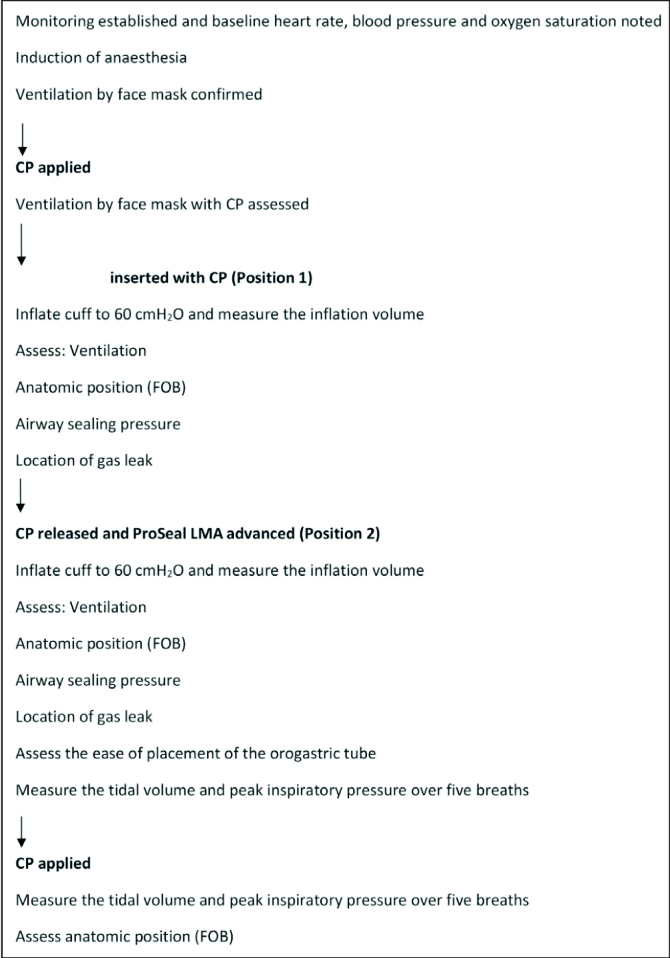
Summarized protocol
CP: cricoid pressure; LMA: laryngeal mask airway
The ProSeal LMA was connected to the circle system, and the ventilation via ProSeal LMA was assessed by a 3-point ventilation score described by Keller and colleagues (7): 1=Excellent, chest expansion without obvious gas leakage; 2=Adequate, chest expansion with obvious gas leakage; 3=Impossible, minimal chest expansion and considerable gas leakage.
The anatomic position of the ProSeal LMA cuff was examined using a fiberoptic bronchoscope and graded by a 5-point anatomic position scoring system described by Brimacombe and Berry (8): 4=only vocal cords seen; 3=vocal cords plus the posterior epiglottis visible (glottic surface); 2=vocal cords plus the anterior epiglottis visible (vallecular surface); 1=vocal cords not seen, but adequate function; 0=vocal cords not seen and failure to function.
Determination of the airway seal pressure was done keeping the circle system gas flow at 3 L min−1 and closing the expiratory valve. The airway pressure at which the aneroid manometer dial reached equilibrium was noted (7). At this point, location of the gas leak was assessed: drainage tube (soap solution bubbling) (9); oral (audible sound); or stomach (auscultation over epigastrium). Ventilation was assisted manually between each measurement and assessment.
Next, CP was released, and the ProSeal LMA (with introducer) was advanced further until resistance was appreciated (the appropriate position, Position 2). The introducer was removed. The additional volume of air required to inflate the cuff to 60 cmH2O was noted. The adequacy of ventilation, anatomic position and seal pressure were noted as previously described. If ventilation was not possible after further advancement, the ProSeal LMA was removed and reinserted. Three attempts at reinsertion were allowed, failing which the trachea was intubated. A lubricated orogastric tube was passed through the drainage tube. Correct placement was confirmed by epigastric auscultation while 10 mL of air was injected. The orogastric tube was removed immediately after insertion.
After the evaluation, ventilation was commenced using a tidal volume (TV) of 8 mL kg−1, respiratory rate 12 breaths min−1, an inspiratory-to-expiratory ratio of 1:2, and a fresh gas flow of 3 L min−1. Expired TV and peak inspiratory pressure (PIP) were recorded during controlled ventilation, with and without CP. The readings were obtained for five consecutive breaths (sixth to tenth breath) for each situation, and the mean expired TV and PIP were calculated. Next, CP was applied and the ProSeal LMA position was reassessed by fiberoptic inspection for its dislodgement, if any, by CP.
Following completion of surgery, neuromuscular blockade was reversed with neostigmine (0.05 mg kg−1) and glycopyrrolate (0.08 mg kg−1). The ProSeal LMA was removed after return of reflexes with adequate spontaneous respiration. Adverse events such as bronchospasm, laryngospasm, airway obstruction, aspiration and blood staining of the ProSeal LMA were noted.
Statistical analysis
The first-time insertion success rate for ProSeal LMA ranges from 76% to 100%; mean 87.3% (10). Assuming an average ProSeal LMA first-time success insertion rate of 87% and a 25% decrease in the insertion success rate with CP application to be clinically important, the sample size required for the study was 51 patients, considering 90% power and 5% alpha level with one-side test. Considering a 10% dropout rate, a sample of 60 subjects was included.
Descriptive statistics were analysed with the Statistical Package for the Social Sciences version 17.0 software (SPSS Ic.; Chicago, IL, USA). Continuous variables are presented as the mean±standard deviation (SD). Categorical variables are expressed as frequencies and percentages. The comparison of normally distributed continuous variables between the groups (with and without CP) was performed using the Student’s t-test. Nominal categorical data between the groups were compared using the chi-squared test or Fisher’s exact test, as appropriate. P<0.05 was considered statistically significant.
Results
We studied 60 patients, 16 men and 44 women. Patient characteristics are shown in Table 1. The mean±SD [range] force measured with simulated CP applied on a weighing scale was 3.10±0.21 [2.8–3.4] kg. This corresponds to a mean (range) force of 30.3 (27.5–33.3) N. Out of 60 patients, ventilation via bag mask with CP was adequate in 25 patients (41.7%) compared to 59 patients (98.3%) without CP; p<0.001.
Table 1.
Patient characteristics
| Age (yr) | 37.78±13.54 |
| Gender (M:F) | 16:44 |
| Weight (kg) | 56.98±10.78 |
| Height (cm) | 155.88±9.14 |
| Body mass index (kg m−2) | 23.39±3.64 |
Values are mean±SD or numbers, as applicable. M: male; F: female
In 1 patient, the ProSeal LMA could not be inserted with CP; it was successfully inserted after the removal of CP. The mean cuff inflation volume to attain a cuff pressure of 60 cmH2O with CP was 15.24±3.61 mL compared to 19.07±3.21 mL without CP; p<0.001. The airway seal pressures could not be determined in 30 (50%) patients when the ProSeal LMA was inserted with CP because of the inability to ventilate; in the remaining 30 patients, the airway seal pressure was 22.43±5.57 cmH2O, which increased to 29.13±5.08 cmH2O when the ProSeal LMA was appropriately positioned after the CP release; p<0.001. Statistically significant differences were found both in ventilation via ProSeal LMA and anatomic position scores with and without CP (Table 2).
Table 2.
Lung ventilation and anatomic position scores of the ProSeal LMA with and without CP
| ProSeal LMA Position with CP | ProSeal LMA Position Following Release of CP | p | |
|---|---|---|---|
| Lung ventilation | |||
| Excellent | 0 (0%) | 56 (93.3%) | <0.001 |
| Adequate | 29 (49.2%) | 4 (6.7%) | <0.001 |
| Impossible | 30 (50.8%) | 0 (0%) | <0.001 |
| Anatomic position | |||
| Score 4 | 0 (0%) | 14 (23.3%) | <0.001 |
| Score 3 | 17 (28.8%) | 31 (51.7%) | 0.011 |
| Score 2 | 9 (15.3%) | 14 (23.3%) | 0.265 |
| Score 1 | 10 (16.9%) | 1 (1.7%) | 0.005 |
| Score 0 | 23 (39.0%) | 0 (0.0%) | <0.001 |
Score 4: only vocal cords seen; Score 3: vocal cords plus posterior epiglottis visible (glottis surface); Score 2: vocal cords plus anterior epiglottis visible (vallecular surface); Score 1: vocal cords not seen, but adequate function; Score 0: vocal cords invisible and inadequate function.
Values are numbers (percent).
CP: cricoid pressure
During determination of the airway seal pressure, the incidence of gas leak from the drain tube and the mouth was comparable in both positions of the ProSeal LMA (with and without CP; p>0.05. No patient demonstrated a gas leak from the stomach in the ProSeal LMA placed with CP compared with 4 of 60 patients (6.7%) when the ProSeal LMA was advanced without CP to its proper position; p=0.041.
An orogastric tube insertion via the drainage tube was successful in the first attempt in 59 patients (98.3%) and in the second attempt in 1 patient (1.7%).
The application of CP with the ProSeal LMA in the appropriate position resulted in a statistically significant decrease in TV and increase in PIP compared to no CP; p<0.001 (Table 3). A worsening of the anatomic position score occurred when CP was applied after the placement of the ProSeal LMA in the appropriate position (Position 2). With regard to Score 1 (only vocal cords seen), there was no significant difference between the two situations, p=0.228; however, the glottic opening appeared narrower when CP was applied (Table 4). Adverse events such as bronchospasm, laryngospasm, airway obstruction, oxygen desaturation and aspiration were not observed in any patient. Mild blood staining of the ProSeal LMA was observed in 39 (65%) patients.
Table 3.
Expired tidal volume and peak inspiratory pressure with and without CP with the ProSeal LMA in proper position
| With CP | Without CP | p | |
|---|---|---|---|
| Tidal volume (mL) | 355.08±104.42 | 489.14±91.62 | <0.001 |
| Peak inspiratory pressure (cmH2O) | 30.71±6.74 | 16.72±5.01 | <0.001 |
Values are mean±SD. CP: cricoid pressure
Table 4.
Anatomic position scores of the ProSeal LMA in proper position (Position 2) with and without CP
| Anatomic position | ProSeal LMA in proper position | ||
|---|---|---|---|
| With CP | Without CP | p | |
| Score 4 | 9 (15.0%) | 14 (23.3%) | 0.228 |
| Score 3 | 16 (26.7%) | 31 (51.7%) | 0.004 |
| Score 2 | 29 (48.3%) | 14 (23.3%) | 0.005 |
| Score 1 | 4 (6.7%) | 1 (1.7%) | 0.364 |
| Score 0 | 2 (3.3%) | 0 (0.0%) | 0.496 |
Values are numbers (percent). CP: cricoid pressure; LMA: laryngeal mask airway
Discussion
This study evaluated the effect of bimanual CP (≈30 N) on BMV, and on the placement and ventilation through a ProSeal LMA. We used the bimanual method of applying CP, as CP without a neck support results in flexion of the head (11). The flexion of the head may make the LMA placement more difficult. Single-handed CP has been found to prevent the placement and ventilation via the LMA more often compared to bimanual CP (12).
In the event of a ‘cannot intubate’ scenario, the manual face mask ventilation of the lungs with oxygen with continued CP application is an imperative (13). We found that CP significantly hampered BMV compared to no CP (41.7% vs. 98.3%, respectively). The magnitude of airway obstruction depends on the force that is applied to the cricoid. Hartsilver and Vanner (13) recommended reduction in the CP force on experiencing difficulty in BMV and a complete release of CP if the difficulty persists.
We found that advancing the ProSeal LMA to its appropriate position (Position 2) after release of CP significantly improved the ventilation scores. The placement of the ProSeal LMA with and without CP resulted in an excellent or adequate ventilation in 49.2% vs. 100% patients respectively. Impaired ventilation was attributed to an excessive gas leak and airway obstruction.
Li et al. (5) reported excellent or adequate ventilation via ProSeal LMA with CP in 28% patients as compared to 100% patients in whom CP was not applied. Previous studies confirm impairment of ventilation via the classic LMA, when CP was applied prior to device insertion (12, 14, 15). Application of CP may cause laryngeal obstruction due to cricoid cartilage deformation or tilting resulting in a vocal cord closure (13). Tilting of the cricoid cartilage resulting in airway obstruction is more likely to occur with classic LMA placement, as its tip lies behind the upper part of the cricoid (16). Indeed, a CP of 30 N has been found to be effective in occluding the oesophageal entrance in anaesthetised and paralysed patients (17).
We observed that the anatomic position scores improved significantly when the ProSeal LMA was advanced to its appropriate position (Position 2) after the release of CP. The anatomic position score was 0 (vocal cords not seen and failure to function) in 23/59 patients (39.0%) with the ProSeal LMA placed after the application of CP (Position 1) compared to 0/60 patients (0%) when the ProSeal LMA was moved to its appropriate position (Position 2) after CP was released; p<0.001. CP prevented a deep enough placement of the ProSeal LMA mask, resulting in an inadequate seal. The tongue base was commonly seen fibreoptically. This was reflected clinically in a majority of patients with impossible lung ventilation (minimal chest expansion, marked air leak). This suggests that the application of CP before the ProSeal LMA placement impedes its advancement to appropriate position.
Previous studies on ProSeal (5) and classic LMA (12, 14, 15, 18) report similar findings. Li et al. (5) observed the anatomic position Scores 1 and 2 in 17/50 (34%) patients with CP compared to 38/50 (76%) patients after the release of CP. Single-handed CP (30 N) impeded the placement and adequate lung ventilation through the classic LMA (12). Aoyama et al. (15) reported that the LMA mask tip was located below the cricoid cartilage at the C6 or C7 vertebra when CP was not applied and was at the C4 or C5 vertebra when CP was applied. When the cuff of the correctly positioned mask is inflated, the thyroid, arytenoid and cricoid cartilages move anteriorly, resulting in bulging of the tissues that overlie the larynx (19). However, CP prevents this characteristic bulging of the laryngeal tissue, so that the inflated cuff, positioned more proximally than usual, compresses only the arytenoid cartilages anteriorly, which leads to partial or complete airway obstruction (15). CP significantly decreased the success rate of adequate ventilation through the i-gel (100% vs. 85%) and the rate of optimal position of i-gel (98% vs. 43%) (20).
The airway seal pressure was significantly lower when CP was applied compared to the pressure obtained after the CP release (22.43±5.57 vs. 29.13±5.08 cmH2O, respectively). Similarly, Li et al. (5) found a significantly lower airway seal pressures when the ProSeal LMA insertion was done with CP (21±7 cm H2O) compared with that observed without CP (27±7 cmH2O). The sealing pressure of a supraglottic device indicates feasibility of positive pressure ventilation and protection of the airway from supra-cuff soiling, and it is an index of successful placement of LMA (7). The lower sealing pressures obtained when the ProSeal LMA was placed with CP can be potentially harmful to patients with a full stomach.
We found that a significant decrease in expired TV with CP (355.08±104.42 vs. 489.14±91.62 mL) was associated with a significant increase in PIP (30.71±6.74 cmH2O vs. 16.72±5.01 cmH2O, respectively). In contrast, Li et al. (5) found that CP applied with the ProSeal LMA in a proper position did not affect TV (501±83 vs 498±81 mL), but increased PIP from 14±2 cm H2O to 28±5 cmH2O. This discrepancy could possibly be related to differences in study methodology. Li et al. (5) used a modification of the bimanual CP technique (a gauze roll under the neck) and tidal volumes of 10 mL kg−1 compared with 8 ml/kg in our study. Asai et al. (12) recommended a temporary release of CP during the LMA placement and its reapplication immediately after the LMA placement. However, they did not assess the effect of CP on ventilation (12). The modifications of the ProSeal LMA are designed to decrease gastric inflation and prevent regurgitation and aspiration of gastric contents compared to the classic LMA. Our data do not support reapplication of CP after the ProSeal LMA placement, as this resulted in a statistically significant and a clinically important decrease in TV with a higher PIP.
Worsening of the anatomic position score assessed fibreoptically was observed when CP was applied after an appropriate ProSeal LMA placement (Position 2). Bimanual CP application (30 N) narrowed the glottis in 45.7% of patients (21). The application of CP with the LMA in place results in the caudal part of the larynx (cricoid) moving back towards the posterior pharyngeal wall. The mask shifts the cranial part of the larynx (arytenoid) anteriorly. The result is an anterior tilting of the larynx with glottis closure (21).
Supraglottic airway devices can be successfully inserted without the use of neuromuscular blocking agents (NMBAs). In the present study, an NMBA was used to assess the effect of the ProSeal LMA placement in paralysed patients on controlled ventilation that would mimic the emergency scenario of patients undergoing emergency laparotomy or Caesarean delivery. Moreover, neuromuscular blocker has been used to get a good placement of LMA (22). The ProSeal LMA was advanced to its appropriate position with the cuff inflated. In the up-down movement manoeuvre described for optimizing placement of supraglottic airway device, after the LMA has been inserted and the cuff inflated, the up-down movement is performed without deflating the cuff within the patient’s mouth (23).
Our study has limitations. CP was applied manually instead of using a cricoid yoke with a force transducer. Manual CP is more accurately placed on the cricoid cartilage and represents clinical practice. However, a uniform force is not applied in each case (13). The use of CP in RSI/I is an accepted standard of care in non-fasting patients and in those at risk of aspiration. The CP application is still widely practiced despite the studies that cite increasing concerns with regard to its safety and efficacy (24–26).
Conclusion
To summarize, our results indicate that the application of bimanual CP (≈30N) significantly impeded the ventilation by bag mask in 58.3% of patients. If the bag mask ventilation is difficult, CP should be released. Insertion of the ProSeal LMA with CP resulted in impossible ventilation in 50.8% patients due to an incorrect placement of the ProSeal LMA. We suggest that CP be released during the ProSeal LMA placement. Based on our data, we cannot recommend reapplication of CP after an appropriate placement of the ProSeal LMA as this results in a statistically and clinically significant decrease in the tidal volume delivered to the lungs with a significant increase in the peak inspiratory pressure. We conclude that the application of bimanual CP (≈30N) interferes with the bag mask ventilation and prevents both the correct placement and ventilation through the ProSeal LMA in adults undergoing elective surgery under general anaesthesia. This has important practical implications in the airway management of the ‘cannot intubate, cannot oxygenate’ event in patients at risk of gastric aspiration.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Institute Ethics Committee, Safdarjang Hospital & VMMC.
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – S.J., S.P.; Design – S.J., S.P., P.M., G.U.; Supervision – S.P., M.P.; Data Collection and/or Processing – T.J., S.P., P.M., G.U.; Analysis and/or Interpretation – S.P., P.M., M.P.; Literature Search – S.J., S.P., P.M., G.U., M.P.; Writing Manuscript – S.P., P.M.; Critical Review – S.J., S.P., P.M., G.U.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118:251–70. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 2.Adhikary SD, Krishnan BS. The cricoid pressure. Indian J Anaesth. 2006;50:12–9. [Google Scholar]
- 3.Brimacombe J. Cricoid pressure and the laryngeal mask airway. Anaesthesia. 1991;46:986–7. doi: 10.1111/j.1365-2044.1991.tb09871.x. [DOI] [PubMed] [Google Scholar]
- 4.Griffin RM, Hatcher IS. Aspiration pneumonia and the laryngeal mask airway. Anaesthesia. 1990;45:1039–40. doi: 10.1111/j.1365-2044.1990.tb14882.x. [DOI] [PubMed] [Google Scholar]
- 5.Li CW, Xue FS, Xu YC, Liu Y, Mao P, Liu KP, et al. Cricoid pressure impedes insertion of, and ventilation through, the ProSeal laryngeal mask airway in anesthetized, paralyzed patients. Anesth Analg. 2007;104:1195–8. doi: 10.1213/01.ane.0000260798.85824.3d. [DOI] [PubMed] [Google Scholar]
- 6.Brain AI, Verghese C, Strube PJ. The LMA ‘ProSeal’-a laryngeal mask with an oesophageal vent. Br J Anaesth. 2000;84:650–4. doi: 10.1093/bja/84.5.650. [DOI] [PubMed] [Google Scholar]
- 7.Keller C, Brimacombe J, Keller K, Morris R. A comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth. 1999;82:286–7. doi: 10.1093/bja/82.2.286. [DOI] [PubMed] [Google Scholar]
- 8.Brimacombe J, Berry A. A proposed fiberoptic scoring system to standardize the assessment of the laryngeal mask airway position. Anesth Analg. 1993;76:457. [PubMed] [Google Scholar]
- 9.O’Connor CJ, Jr, Stix MS. Bubble solution diagnoses ProSeal insertion into the glottis. Anesth Analg. 2002;94:1671–2. doi: 10.1097/00000539-200206000-00065. [DOI] [PubMed] [Google Scholar]
- 10.Cook TM, Lee G, Nolan JP. The ProSeal™ laryngeal mask airway: a review of the literature. Can J Anaesth. 2005;52:739–60. doi: 10.1007/BF03021789. [DOI] [PubMed] [Google Scholar]
- 11.Selwyn CJ. The “contracricoid” cuboid aid to tracheal intubation. Anaesthesia. 1982;37:345. doi: 10.1111/j.1365-2044.1982.tb01119.x. [DOI] [Google Scholar]
- 12.Asai T, Barclay K, Power I, Vaughan RS. Cricoid pressure impedes placement of the laryngeal mask airway. Br J Anaesth. 1995;74:521–5. doi: 10.1093/bja/74.5.521. [DOI] [PubMed] [Google Scholar]
- 13.Hartsilver EL, Vanner RG. Airway obstruction with cricoid pressure. Anaesthesia. 2000;55:208–11. doi: 10.1046/j.1365-2044.2000.01205.x. [DOI] [PubMed] [Google Scholar]
- 14.Ansermino JM, Blogg CE. Cricoid pressure may prevent insertion of the laryngeal mask airway. Br J Anaesth. 1992;69:465–7. doi: 10.1093/bja/69.5.465. [DOI] [PubMed] [Google Scholar]
- 15.Aoyama K, Takenaka I, Sata T, Shigematsu A. Cricoid pressure impedes positioning and ventilation through the laryngeal mask airway. Can J Anaesth. 1996;43:1035–40. doi: 10.1007/BF03011906. [DOI] [PubMed] [Google Scholar]
- 16.Brimacombe JR, Berry A. Mechanical airway obstruction after cricoid pressure with the laryngeal mask airway. Anesth Analg. 1994;55:601–2. doi: 10.1213/00000539-199403000-00039. [DOI] [PubMed] [Google Scholar]
- 17.Zeidan AM, Salem MR, Mazoit JX, Abdullah MA, Ghattas T, Crystal GJ. The effectiveness of cricoid pressure for occluding the esophageal entrance in anesthetized and paralyzed patients: An Experimental and Observational Glidescope Study. Anesth Analg. 2014;118:580–6. doi: 10.1213/ANE.0000000000000068. [DOI] [PubMed] [Google Scholar]
- 18.Brimacombe J, White A, Berry A. Effect of cricoid pressure on ease of insertion of the laryngeal mask airway. Br J Anaesth. 1993;71:800–2. doi: 10.1093/bja/71.1.166-a. [DOI] [PubMed] [Google Scholar]
- 19.Nandi PR, Nunn JF, Charlesworth CH, Taylor SJ. Radiological study of the laryngeal mask. Eur J Anaesthesiol Suppl. 1991;4:33–9. [PubMed] [Google Scholar]
- 20.Hashimoto Y, Asai T, Arai T, Okuda Y. Effect of cricoid pressure on placement of the I-gelTM: a randomised study. Anaesthesia. 2014;69:878–82. doi: 10.1111/anae.12731. [DOI] [PubMed] [Google Scholar]
- 21.Asai T, Murao K, Shingu K. Cricoid pressure applied after placement of laryngeal mask impedes subsequent fibreoptic tracheal intubation through mask. Br J Anaesth. 2000;85:256–61. doi: 10.1093/bja/85.2.256. [DOI] [PubMed] [Google Scholar]
- 22.Trikha A, Baidya DK. Routine use of laryngeal mask airway for cesarean section: Is it time to reconsider? J Obstet Anaesth Crit Care. 2016;6:1–2. doi: 10.4103/2249-4472.181053. [DOI] [Google Scholar]
- 23.Brimacombe J. Laryngeal mask anesthesia: principles and practice. 2nd ed. Philadelphia: WB Saunders; 2005. p. 166. [Google Scholar]
- 24.Kron SS. Questionable effectiveness of cricoid pressure in preventing aspiration. Anesthesiology. 1995;83:431–2. doi: 10.1097/00000542-199508000-00033. [DOI] [PubMed] [Google Scholar]
- 25.Smith KJ, Ladak S, Choi PT, Dobranowski J. The cricoid cartilage and the esophagus are not aligned in close to half of adult patients. Can J Anaesth. 2002;49:503–7. doi: 10.1007/BF03017931. [DOI] [PubMed] [Google Scholar]
- 26.Smith KJ, Dobranowski J, Yip G, Dauphin A, Choi PT. Cricoid pressure displaces the esophagus: an observational study using magnetic resonance imaging. Anesthesiology. 2003;99:60–4. doi: 10.1097/00000542-200307000-00013. [DOI] [PubMed] [Google Scholar]


