Abstract
Tissue engineered bone grafts based on bone marrow mesenchymal stromal cells (MSCs) are being actively developed for craniomaxillofacial (CMF) applications. As for all tissue engineered implants, the bone-regenerating capacity of these MSC-based grafts must first be evaluated in animal models prior to human trials. Canine models have traditionally resulted in improved clinical translation of CMF grafts relative to other animal models. However, the utility of canine CMF models for evaluating MSC-based bone grafts rests on canine MSCs (cMSCs) responding in a similar manner to scaffold-based stimuli as human MSCs (hMSCs). Herein, cMSC and hMSC responses to polyethylene glycol (PEG)-based scaffolds were therefore compared in the presence or absence of osteoinductive polydimethylsiloxane (PDMS). Notably, the conjugation of PDMS to PEG-based constructs resulted in increases in both cMSC and hMSC osteopontin and calcium deposition. Based on these results, cMSCs were further used to assess the efficacy of tethered bone morphogenic protein 2 (BMP2) in enhancing PEG-PDMS scaffold osteoinductivity. Addition of low doses of tethered BMP2 (100 ng/mL) to PEG-PDMS systems increased cMSC expression of osterix and osteopontin compared to both PEG-PDMS and PEG-BMP2 controls. Furthermore, these increases were comparable to effects seen with up to 5-times higher BMP2 doses noted in literature.
Keywords: canine mesenchymal stromal cells, human mesenchymal stromal cells, osteogenesis, PDMS bioactive scaffolds, BMP2
1. INTRODUCTION
Craniomaxillofacial (CMF) defects are a significant source of trauma among combat-injured military personnel and veterans 1. In addition, CMF defects are one of the most common birth defects 2–4, with approximately 1 in 700 live births being associated with a cleft or palate deformity 3. Such defects are often associated with substantial pain, aesthetic concerns, and high cost of treatment, which generally includes surgical procedures, dental treatment, speech therapy, and counseling 5. Surgical interventions generally require the use of autografts or allografts, such as allogeneic bone or demineralized bone matrix 4,6–9. However, each of these graft sources has inherent disadvantages, such as donor site morbidity and prolonged post-operative pain for autografts, immune rejection and disease transmission for allografts, and limited availability for both.
Tissue engineering is a promising alternative to autograft- or allograft-based treatment of CMF bone defects 4,6,9–12. In the context of tissue engineering, scaffolds intended to support bone regeneration have been developed from numerous materials, including ceramics 13–20, synthetic polymers 21–23, and metals 24–26. In many cases, these scaffolds are seeded with bone marrow mesenchymal stromal cells (MSCs) 27, a multipotent cell type capable of differentiating into osteogenic, chondrogenic, and adipogenic lineages. In MSC-based bone scaffold approaches, the biomaterial is generally modified to support a strong and specific osteogenic response from associated MSCs, often through the inclusion of bioactive glass 17,28–30, hydroxyapatite (HAp) 13–16, or osteoinductive growth factors 31,32.
As for all tissue engineered bone grafts, the bone-regenerating capacity of these MSC-based constructs must first be evaluated in animal models prior to human trials. Canine models have traditionally been associated with improved clinical translation of CMF grafts and devices relative to small animal models (such as rodents) 33,34 as well as larger animal models (such as rabbit, sheep, and goat) 34–36. This improved translation potential results in part from the greater similarity between human and canine bone remodeling, bone composition, and dentition 35,37. However, extending canine CMF models to the evaluation of MSC-based bone scaffolds also requires a high degree of correlation in the osteogenic responses of canine MSCs (cMSCs) and human MSCs (hMSCs) to scaffold-based stimuli. Currently, limited evidence exists to support the conclusion that cMSCs respond similarly to 3D osteogenic environments as their human counterparts 38. Thus, a primary goal of the current study is to compare the osteogenic responses of cMSCs and hMSCs to equivalent 3D scaffold environments.
In comparing cMSC to hMSC responses, polyethylene glycol (PEG) scaffolds as well as PEG-polydimethylsiloxane (PEG-PDMS) constructs 39–41 were utilized. Notably, while PEG-only scaffolds are generally considered relatively inert, they have been found to support osteoblastic differentiation when coupled with silica- or siloxane- based additives such as PDMS 39–44. Indeed, PEG-PDMS constructs have previously been shown to stimulate progenitor cells to undergo highly specific osteogenic lineage progression even in the absence of osteogenic media supplements, and the PDMS phase has been shown to intrinsically induce mineralization 39–41. Beyond these points, the use of acrylate-derivatized PEG as the scaffold base allows for the covalent incorporation of additional stimuli, a feature which has been used extensively to increase PEG scaffold bioactivity 45–47. Specifically, to enhance the intrinsic osteoinductive strength of PEG-PDMS scaffolds, growth factors such as recombinant bone morphogenic protein 2 (BMP2) can potentially be conjugated into the scaffold network.
BMP2 is known to play a significant role in the initial stages of bone healing as well as in the later stages of osteogenesis 48–50, and both cMSCs and hMSCs undergo osteoblastic differentiation in response to exogenous BMP2 51,52. However, the large doses of BMP2 (as high as 1.5 mg/mL scaffold 53) often administered to counter its rapid in vivo clearance have been associated with high treatment costs as well as significant complications, including inflammation, tumor development, and ectopic bone formation 54–56. To reduce the levels of BMP2 needed to trigger desired cell responses, BMP2 can be covalently tethered within scaffolds 31,32,57. In contrast to physical incorporation, this method prevents cell internalization of BMP2, allowing for repeated signaling between the cell and the ligand, and prolongs BMP2 retention within the scaffold 31. Indeed, 200–500 ng/mL of tethered BMP2 has previously been shown to induce MSC osteoblastic differentiation 31,50,58,59, and 60–100 ng/mL has been reported to have an significant osteogenic effects on cMSCs 51. Thus, a second goal of the current work is to utilize validated cMSCs to assess the efficacy of tethered, low-dose BMP2 in enhancing the intrinsic osteogenic capacity of PEG-PDMS scaffolds.
Toward these ends, two sets of experiments were conducted in the current study: the first focused on comparing cMSC and hMSC osteogenic responses to equivalent 3D scaffold environments and the second focused on utilizing cMSCs to evaluate the increase in PEG-PDMS scaffold osteoinductivity following incorporation of low-dose, tethered BMP2. In each study, MSCs were cultured in various scaffold formulations in the absence of osteogenic media supplements. After 21 days of culture, levels of osteogenic transcription factors runx2 or osterix, bone ECM proteins collagen I (Col-1) and osteopontin (OPN), and mineralization were evaluated.
2. MATERIALS AND METHODS
2.1. Preparation of diacrylate-terminated PEG and methacrylate-terminated star PDMS
Diacrylate-terminated PEG (PEG-DA, Mn = 3.4 kDa) and methacrylate-terminated star PDMS (PDMSstar-MA, Mn = 2 kDa) were prepared according to previously described protocols 39–41,60. The acrylation of PEG-DA and methacrylation of PDMSstar-MA were each confirmed to be > 95% by 1H-NMR.
2.2. Synthesis of acrylate-derivatized RGDS and acrylate-derivatized BMP2
Acrylate-derivatization of the cell adhesion peptide RGDS (American Peptide) and recombinant human BMP2 (carrier free; R&D Systems) was achieved by reaction with acryloyl-PEG-succinimidyl valerate (ACRL-PEG-SVA, 3.4 kDa; Laysan Bio) at a 1:1 molar ratio or a 1:6 molar ratio, respectively 61,62. Both mixtures were reacted in 50 mM sodium bicarbonate buffer, pH 8.5, for 2 h at room temperature (RT) under constant agitation. The reaction products (ACRL-PEG-RGDS) and (ACRL-PEG-BMP2) were separately purified by overnight dialysis against double deionized water (dIH2O) using 3,500 MWCO or 5,000 MWCO Snakeskin Dialysis tubing (Thermo Scientific), respectively. ACRL-PEG-RGDS was lyophilized and stored at −20 °C until use. ACRL-PEG-BMP2 was filter-sterilized, stored at 4°C, and used within 1 h of purification.
2.3. Evaluation of scaffold material properties
Precursor solutions containing 10 wt% PEG-DA and 1 mM ACRL-PEG-RGDS were prepared in phosphate buffered saline (PBS). Photoinitiator, consisting of a 30 wt% solution of 2,2-dimethyl-2-phenyl-acetophenone in N-vinylpyrrolidone, was added to each precursor solution at a concentration of 10 µL/mL. To a subset of solutions, PDMSstar-MA was then added to 2 wt %. The mixtures were vortexed and filter sterilized using 0.22-µm polyethersulfone (PES) filters. Sterile ACRL-PEG-BMP2 was also added to a subset of precursor solutions to achieve a final BMP2 concentration of 100 ng/mL. In total, four distinct solutions were obtained (each containing 1 mM ACRL-PEG-RGDS and photoinitiator): (i) 10 wt % PEG-DA (PEG), (ii) 10 wt% PEG-DA + 2 wt% PDMS-MA (PEG-PDMS), (iii) 10 wt% PEG-DA + 100 ng/mL ACRL-PEG-BMP2 (PEG-BMP2) and (iv) 10 wt% PEG-DA + 2 wt% PDMS-MA + 100 ng/mL ACRL-PEG-BMP2 (PEG-PDMS-BMP2). These formulations were separately poured into 0.75 mm-thick, UV transparent, rectangular molds and polymerized by exposure to long-wave UV light (∼6 mW/cm2, 365 nm; Spectroline) for 6 min. After polymerization, the hydrogel slabs were washed in PBS and incubated for 24 h at RT to allow the gels to reach equilibrium swelling.
2.3.1. Bulk mechanical testing
A series of 8 mm discs were prepared from the swollen hydrogel slabs using a Miltex biopsy punch. Three to four 8 mm discs were further separated into a 6 mm inner disc and an outer 8 mm ring using a 6 mm biopsy punch. The outer 8 mm rings were employed for tensile testing using a modification of the circumferential property testing technique validated by Johnson et al. 63. The 6 mm inner discs were subsequently utilized for mesh size assessments. Briefly, each ring was mounted onto an Instron 3342 by threading opposing stainless steel hooks through the segment lumen. The hooks were then uniaxially stretched at a rate of 6 mm/min until construct failure. The elastic modulus, E, of each sample, was defined as the slope of the linear region of the resulting stress–strain curve.
2.3.2. Hydrogel average mesh size
In this study, hydrogel average mesh size was characterized using an equilibrium dextran diffusion assay based on an adaptation of the methodology of Watkins et al. 64. Briefly, four 6 mm discs from each hydrogel formulation were immersed in 0.5 mL of PBS containing 50 µg/mL FITC-labeled dextran (4, 10 and 20 kDa; Sigma). Dextran was then allowed to diffuse into the hydrogels for 24 h at RT, after which each disc was gently blotted and transferred to 0.5 mL fresh PBS. After an additional 24 h at RT, the fluorescence of the PBS solution surrounding each disc was measured at ex/em 488/532 nm using a plate reader. Each fluorescence measure was converted to micrograms of dextran using dextran standard curves and then divided by gel thickness to yield a quantitative indicator of hydrogel permissivity (C). These permissivity measures were used to estimate the average mesh size (ξx) of each hydrogel type (x) relative to the PEG formulation as follows: ξx= [Cx/CPEG].
2.4. Canine tissue collection and mesenchymal stromal cell isolation
Canine MSC isolation was conducted with the approval of the Texas A&M University Institutional Animal Care and Use Committee (Animal Use Protocol 2015-0072). Primary cMSCs were isolated from three donors to partially control for age and breed effects: 1) a 14 month old, 65 lb intact male Walker hound (∼equivalent to a 16.5 year old human), 2) a 6 year old, 148 lb neutered male mixed breed (∼equivalent to a 46–49 year old human), and 3) a 3.5 year old, 47 lb neutered male mixed breed (∼equivalent to a 30 year old human). The intact versus neutered status of the male canine donors was utilized to gain initial insight into potential gender effects, since female cMSCs were unavailable to us at the time of these studies.
Under general anesthesia, a bone marrow aspirate was performed on the craniodorsal (posterior) iliac crest of each donor using a 15 gauge Illinois biopsy needle. The craniodorsal iliac crests of two additional canine donors were also separately aspirated to allow testing of response consistency to PEG-PDMS-BMP2 scaffolds. Nucleated cells were isolated from bone marrow samples using gradient centrifugation (Ficoll-Paque Plus, GE Health Care Biosciences) using previously described techniques 65. Following centrifugation at 1800 × g for 30 min, mononuclear cells were removed, washed twice with 15 mL of Hank’s Balanced Salt Solution (HBSS, Invitrogen), quantified and assessed for viability using a hemocytometer and trypan blue exclusion.
Nucleated marrow cells were plated at 30,000 cells/cm2 in 150 mm tissue culture dishes in Complete Culture Medium (CCM) containing α-MEM, 100 units/mL penicillin and 100 µg/mL streptomycin (1% PS; Invitrogen), and 10% fetal bovine serum (FBS; Atlanta Biologicals). Cells were incubated at 37 °C and 5% humidified CO2 for 24 h. Plates were washed with PBS to remove non-adherent cells followed by media exchange. This process was repeated daily for 2 additional days. Culture dishes were subsequently monitored for expansion of the primary cell population (passage 0) with media exchange performed every other day. Upon reaching 70% confluence (5–12 days), cells were lifted with 0.5% trypsin/EDTA solution (Invitrogen) and re-seeded at 100 cells/cm2 for expansion of passage 1 (P1) cells. Cells were fed every other day until 70% confluent, after which P1 cells were cryopreserved in α-MEM with 5% DMSO (Sigma-Aldrich) and 30% FBS in preparation for subsequent experiments. For cell characterization assays, P1 cells were thawed, plated at 100 cells/cm2 and expanded to 70% confluency. These cMSCs were characterized by flow cytometry for cell surface epitopes – including CD44+, CD105+, CD90+, CD9+, STRO-1−, CD34−, and CD45− (AbD Serotec or R&D Systems; Supplementary Table 1) – to confirm their MSC character. Isolated cMSCs were also confirmed to be able to differentiate down adipogenic, chondrogenic, and osteogenic lineages by standard methodologies.
2.5. Human and canine mesenchymal stromal cell culture
Primary human MSCs (hMSCs) from a healthy, 22 year old female donor were obtained from Lonza (PT-2501, Lot 7F3677) at P1. These donor cells had been confirmed by Lonza to be CD44+, CD105+, CD29+, CD166+, CD14−, CD34−, and CD45− and to undergo adipogenic, chondrogenic, or osteogenic differentiation under inductive culture conditions. To prepare for the encapsulation studies, the obtained P1 cMSCs and hMSCs were thawed and expanded at 37 °C and 5% CO2.
2.6. Fabrication and culture of cell-laden constructs
For the first set of experiments, cMSCs (passage 3–4) or hMSCs (passage 3–4) were resuspended in sterile PEG or PEG-PDMS precursor solutions at 1.5×106 cells/mL. The resulting suspensions were polymerized into hydrogels by exposure to long-wave UV light (∼6 mW/cm2, 365 nm; Spectroline) for 6 min. Each hydrogel disc (8 mm diameter) was then rinsed with sterile PBS (pH 7.4; Invitrogen) and placed in DMEM supplemented with 10% Premium-FBS (Atlanta Biologics) and 1% PS at 37 °C and 5% CO2. The discs were cultured for 21 days, with media changes every other day.
In the second set of experiments, cMSCs (passage 3–4) were encapsulated in PEG-PDMS, PEG-BMP2, or PEG-PDMS-BMP2 precursor solutions at 1.5×106 cells/mL as described above. The hydrogel discs were cultured for 21 days in DMEM supplemented with 10% Premium-FBS and 1% PS at 37 °C and 5% CO2, with media changes every other day.
2.7. Construct harvest
For both the first and second experiments, sets of sample discs were collected for protein analyses (n = 3–4 per formulation) and histological analyses (n = 3–4 per formulation) both at 24 h post-encapsulation (“day 0”) and following 21 days of culture. For protein-based assays, both endpoint and day 0 sample discs were flash-frozen in liquid N2 and stored at −80 °C. Thereafter, they were homogenized in lysis buffer (Ambion, Life Technologies), and the supernatant was collected after centrifugation. A second extraction from the gel pellet was performed by conducting three freeze-thaw cycles, followed by centrifugation to isolate the supernatant, which was combined with the supernatant obtained from the initial homogenization. DNA levels in the supernatant solutions were then measured using the PicoGreen assay (Invitrogen), with calf thymus DNA (Sigma) serving as a standard. The resulting solutions were stored at −80 °C for subsequent protein analyses. For histology, collected day 0 and endpoint samples were fixed in 10% formalin for 30 min, embedded in Tissue-Tek freezing medium, and sectioned using a cryomicrotome (20 µm thickness).
2.8. Protein level analyses
For hMSC-laden samples, the levels of osteogenic markers collagen I (Col-1) and osteopontin (OPN) were analyzed using a human multiplex immunoassay kit (R&D Systems). Briefly, hydrogel homogenates were diluted 1:1 in the kit-provided buffer and dispensed into a 96-well plate, after which magnetic bead suspensions, detection antibodies, and streptavidin-phycoerythrin were added to each sample well. The plate was then loaded into MAGPIX system (xMAP technology, Luminex), and sample concentrations for each analyte were obtained on the basis of their respective median fluorescence intensities relative to standards. Resulting protein concentration measures were then subsequently normalized to sample DNA content as determined by the PicoGreen assay (Invitrogen).
For canine samples, multiplex immunoassays for the Luminex xMAP system were unavailable for the proteins of interest. As such, the levels of Col-1 and OPN associated with the various cMSC treatment groups were analyzed using Western blot immunoassays. In brief, hydrogel homogenates were concentrated using 3,000 MWCO Amicon filter units (Millipore), followed by addition of β-mercaptoethanol and heating at 95 °C for 10 min. Concentrated proteins samples with consistent DNA levels were loaded into different wells of 8 or 12% polyacrylamide gels and separated by electrophoresis. After electrophoresis, proteins were transferred to a nitrocellulose membrane (Thermo Scientific), and the membranes were blocked with a 5% bovine serum albumin (BSA; Fisher Scientific) solution in TBST/NaN3 (25 mM Tris-HCl, pH. 7.5, 137 mM NaCl, 0.1% Tween 20, 0.05 % NaN3) for 1 h at RT. Appropriate primary antibodies (Supplementary Table 2) were diluted in 5% BSA solution in TBST/NaN3 and applied overnight at 4 °C with constant shaking.
Bound primary antibodies were detected by the application of appropriate horseradish peroxidase-conjugated or alkaline phosphatase-conjugated secondary antibodies (Jackson ImmunoResearch) for 1 h at RT, followed by the application of Luminol (Santa Cruz Biotechnology) or Novex chemiluminescent substrate (Life Technologies) respectively. Chemiluminescence was detected using a ChemiDoc™ XRS+ System equipped with Image Lab™ Software (BioRad), with exposure time controlled to avoid signal saturation. The band integrated optical density for each marker was quantified using Adobe Photoshop and normalized to the amount of loaded DNA.
For the purpose of comparison, the average DNA-normalized protein measures for each treatment group were normalized to the corresponding PEG samples (study 1) or to the corresponding PEG-PDMS controls (study 2). Following completion of the protein assessments, the hMSC and cMSC responses to PEG and PEG-PDMS scaffolds were compared. Given the strong agreement between the normalized human MAGPIX immunoassay data and the normalized canine Western blot immunoassay data, we judged it to be unnecessary to repeat the human protein measures using Western blot.
2.9. Histological analyses
For samples reserved for histology, standard von Kossa staining protocols or immunohistochemical techniques were utilized to assess MSC responses to the various construct formulations.
2.9.1. Immunohistochemical staining
For immunostaining analyses, rehydrated sections were blocked for 10 min by exposure to Terminator solution (Biocare Medical). Samples were incubated at 4 °C overnight with primary antibody diluted in PBST (PBS plus 0.1 % Tween 20) containing 3% BSA. Bound primary antibody was detected using the appropriate alkaline phosphate-conjugated secondary antibody (Jackson Immunoresearch) followed by the application of chromogen Ferangi Blue (Biocare Medical) and mounting. Stained sections were imaged using a Zeiss Axiovert microscope.
2.9.2. von Kossa staining
Extracellular calcium deposition was assessed using a von Kossa staining kit (American Mastertech). Briefly, rehydrated sections were rinsed with water, after which a 5% silver nitrate solution was applied. Sections were then exposed to full-spectrum light in a humidified chamber for 1 h. After rinsing with dIH2O, sections were exposed to 5% sodium thiosulfate for 3 min, briefly rinsed with dIH2O, and mounted. Stained sections were imaged using a Zeiss Axiovert microscope.
2.9.3 Semi-quantitative staining assessment
Cell counts were carried out to semi-quantitatively evaluate immunostaining results for the intracellular proteins runx2 and osterix and the cell-surface protein AFABP. In addition, since deposited ECM remained localized around the parent cells in each construct - as is characteristic for PEG-based gels 66 - the relative levels of OPN, Col-1, and matrix mineralization (von Kossa) were also evaluated by cell counts. These counting assessments were conducted according to previously validated methods 67–70 by two independent observers. For each cell, i, in a given section, a staining intensity, di, was recorded on a scale of 0–3, 0 = “no staining” and 3 = “highest intensity among all stained samples for that species”. The cumulative staining intensity, d, for a given stain in a particular section was then calculated using the following equation: d = (Σ di)/(total cell number). Four-to-ten sections per sample and 3–4 samples per construct type were analyzed for each stain.
2.10. Statistical analyses
All data are reported as mean ± standard error of the mean. Comparison of sample means was performed by one-way ANOVA followed by Tukey’s post-hoc test (IBM-SPSS software), with significance established at p < 0.05.
3. RESULTS
3.1. MSC characterization
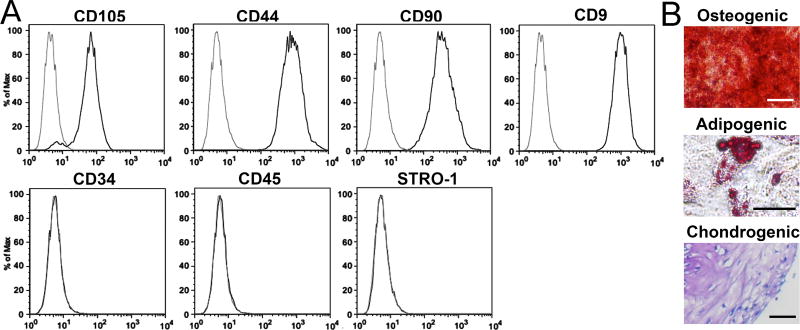
The primary human MSCs (hMSCs) used in this study were obtained from Lonza and were confirmed to express CD29, CD44, CD105, and CD166 and to not express CD14, CD34, and CD45. In addition, the hMSCs were confirmed to differentiate down the adipogenic, chondrogenic, and osteogenic lineages when cultured under recommended differentiation conditions. Similarly, flow cytometry was performed to evaluate the MSC identity of the isolated canine marrow cells per previously developed marker criteria 71,72. Specifically, canine marrow cells were evaluated for cell surface markers CD105, CD44, CD90, CD9, CD34, CD45, and STRO-1 (Figure 1A). Canine marrow cells were negative for CD34, CD45, and STRO-1, but were positive for CD105, CD90, CD44, and CD9, indicating a MSC phenotype.
Figure 1.
(A) Flow cytometry results for canine marrow stromal cells supporting the MSC character of the isolated cells. (B) Representative images for canine stromal cells cultured in osteogenic induction medium and stained with Alizarin red; canine stromal cells cultured in adipogenic induction medium and stained with Oil Red; and a canine stromal cell micromass cultures grown in chondrogenic induction medium and stained with toluidine blue. Scale bars = 100 µm. These images support the tri-lineage differentiation potential of the isolated cells.
To further assess the multipotency of the isolated cells, the canine marrow cells were cultured in osteogenic media or adipogenic media on tissue culture polystyrene for 21 days. Similarly, micromass cultures of canine marrow cells were exposed to chondrogenic media for 21 days. Figure 1B shows representative images of osteogenic, adipogenic, and chondrogenic micromass cultures stained for Alizarin Red, Oil Red O, or toluidine blue, respectively. These induction cultures demonstrate the ability of the isolated canine marrow cells to undergo osteogenic, adipogenic, and chondrogenic lineage progression. Overall, the flow cytometry results and directed differentiation cultures confirm the MSC character of the isolated canine stromal cells (hereafter referred to as cMSCs) and establish them as a viable cell source for the purposes of this study.
3.2. Canine MSC model validation
Canines are commonly used as a preclinical model for bone regeneration due to a number of similarities in pathogenesis, loading, and structure with humans 73. However, extending canine data to prediction of human outcomes is complex and based on the assumption that the involved canine cells behave in a similar way to their human counterparts. For evaluation of MSC-based bone scaffolds, this remains a parameter to be considered as cMSCs present several differences relative to hMSCs, including shorter in vitro life times, lower rates of division, and distinct differentiation potentials 74,75. We therefore compared the osteogenic responses of cMSCs and hMSCs to equivalent PEG-based scaffold environments in the presence or absence of osteoinductive PDMS.
In brief, cMSCs and hMSCs were encapsulated in PEG (10 wt%) constructs and PEG-PDMS (10 wt%, 2 wt%) constructs and cultured for 21 days. Each scaffold formulation was prepared with consistent levels of tethered RGDS to allow for cell adhesion to the scaffold network. Furthermore, characterization of the scaffolds indicated no statistical differences in the initial tensile modulus or average mesh size between the PEG and PEG-PDMS constructs (Table 1). Given the slow degradation rate of PEG and PEG-PDMS systems 41, these basal similarities allow differences in day 21 MSC responses between scaffold formulations to be attributed primarily to the presence of PDMS.
Table 1.
Comparison of the tensile modulus and relative average mesh size of the various scaffold formulations. Property results represent an average ± standard error of the mean for n = 4 samples for each construct formulation. The PEG-PDMS, PEG-BMP2 and PEG-PDMS-BMP2 formulations were included in the second phase of this study, whereas PEG versus PEG-PDMS constructs were the focus of the first phase of this work.
| Experiment | Hydrogel Formulation |
Tensile Modulus (kPa) |
Average Mesh Size Relative to PEG Control |
|---|---|---|---|
| Study 1: cMSC-hMSC comparison | PEG | 131.3 ± 1.5 | 1.00 ± 0.02 (∼5.0 nm 114) |
| PEG-PDMS | 137.8 ± 1.7 | 0.95 ± 0.03 | |
|
| |||
| Study 2: cMSC evaluation of low dose BMP2 | PEG-PDMS | 139.8 ± 2.2 | 0.97 ± 0.03 |
| PEG-BMP2 | 135.1 ± 1.7 | 0.99 ± 0.02 | |
| PEG-PDMS-BMP2 | 138.3 ± 5.1 | 0.94 ± 0.01 | |
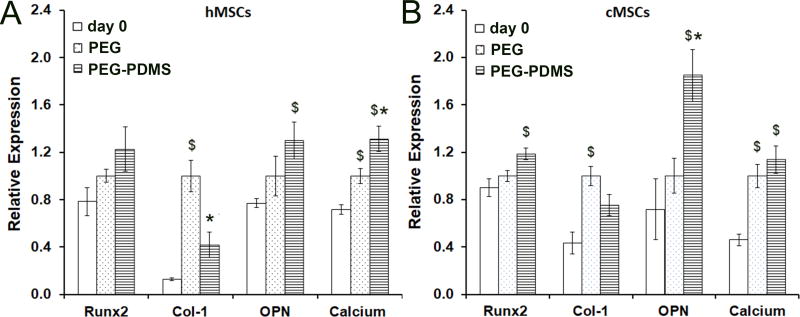
To assess cMSC and hMSC lineage progression, the levels of the early osteogenic transcription factor runx2, ECM proteins Col-1 and OPN, and matrix mineralization were all evaluated with respect to scaffold type and relative to day 0. As shown in Figure 2, the osteogenic response of cMSCs to 21 days of culture within PEG and PEG-PDMS constructs displayed a number of similarities with hMSCs. For instance, culture of both cMSCs and hMSCs in PEG constructs resulted in substantial increases in Col-1 deposition (p < 0.004) and matrix mineralization (p < 0.006) relative to day 0. PEG-PDMS scaffolds were also associated with increased levels of calcium (p < 0.001) and OPN (p < 0.010) deposition relative to day 0 for both cell types. In comparing responses to PEG versus PEG-PDMS scaffolds, the levels of runx2, OPN, and mineralization within PEG-PDMS constructs each appeared to be greater than the corresponding PEG scaffolds for both cMSCs and hMSCs. However, the only difference between PEG and PEG-PDMS constructs that rose to statistical significance was for matrix mineralization (p = 0.002). Furthermore, Col-1 levels in the PEG-PDMS constructs appeared to be significantly lower than in corresponding PEG controls for both hMSCs and cMSCs, although these differences were only significant for hMSCs (p = 0.002).
Figure 2.
Osteogenic marker levels associated with 21 days of (A) human MSC or (B) canine MSC culture within PEG or PEG-PDMS scaffolds. All data are normalized to the PEG day 21 group. ‘$’ denotes a significant difference relative to the “day 0” control. ‘*’ denotes a significant difference relative to the PEG construct group, p < 0.05.
3.3 PEG-PDMS-BMP2 scaffolds for osteoblastic differentiation of canine MSCs
As a second goal of the current work, validated cMSCs were utilized to assess the efficacy of tethered, low-dose BMP2 in enhancing the intrinsic osteogenic capacity of PEG-PDMS scaffolds. A low dose of BMP2 (100 ng/mL) was selected for incorporation: 1) to reduce the potential for the undesired side effects currently associated with high dose BMP2 loading 76, and 2) based on literature indicating 100 ng/mL doses could be effective in stimulating Col-1 deposition as well as calcification 77,78.
To assess possible synergistic effects between PDMS and BMP2, the responses of cMSCs to three construct groups were compared: 1) PEG-PDMS, 2) PEG-BMP2, and 3) PEG-PDMS-BMP2. As with the incorporation of PDMS, the addition of BMP2 into the PEG network structure did not substantially impact scaffold bulk modulus or average mesh size (Table 1), again allowing focus on added bioactivity in comparing cell responses. As anticipated, cMSCs in PEG-BMP2 scaffolds displayed significantly increased Col-1 deposition (p < 0.001) relative to PEG-PDMS constructs (Figure 3). However, PEG-BMP2 networks did not stimulate statistically significant increases in runx2 or OPN relative to PEG-PDMS scaffolds. Furthermore, although the levels of the mid-term osteogenic transcription factor osterix appeared to be increased in PEG-BMP2 constructs relative to PEG-PDMS scaffolds, this difference fell below statistical significance (p = 0.269).
Figure 3.
Comparison of cMSC osteogenic responses following 21 days of culture in PEG-PDMS, PEG-BMP2, or PEG-PDMS-BMP2 scaffolds. All data are normalized to the PEG-PDMS group. ‘$’ denotes a significant difference relative to PEG-PDMS controls. ‘*’ denotes a significant difference relative to the PEG-BMP2 group.
When PDMS and BMP2 were combined, however, osterix levels increased 2.2-fold (p = 0.008) and calcium deposition increased 1.9-fold (p = 0.038) relative to pure PEG-PDMS constructs. PEG-PDMS-BMP2 scaffolds also displayed a 2.0-fold increase in OPN deposition (p < 0.009) relative to both PEG-PDMS and PEG-BMP2 constructs. That said, the addition of BMP2 to PEG-PDMS networks did not promote a significant increase in Col-1 relative to PEG-PDMS only constructs, despite the increase in Col-1 noted with BMP2 alone. The cumulative results from the first (Figure 2) and second (Figure 3) experimental sets indicate that PDMS may have a suppressive effect on Col-1 production. Representative images of Col-1, OPN, and von Kossa staining are presented in Supplementary Figure 1.
To assess the specificity of cMSC differentiation towards the osteoblastic lineage, markers for adipogenesis (AFABP) and chondrogenesis (Col-2, Col-10) were also assessed (Figure 4). Although no decrease in AFABP expression was observed in PEG-BMP2 scaffolds relative to PEG-PDMS controls (p = 0.089), PEG-PDMS-BMP2 scaffolds were associated with a significant reduction in AFABP expression relative to PEG-PDMS constructs (p = 0.001). No significant differences in Col-2 expression were noted for PEG-BMP2 or PEG-PDMS-BMP2 scaffolds relative to PEG-PDMS constructs. However, just as PDMS appeared to have a suppressive effect on Col-1 production, PDMS presence in the PEG-PDMS-BMP2 constructs was correlated with reduced levels of the hypertropic chondrocyte marker Col-10 relative to PEG-BMP2 scaffolds (p = 0.006). BMP2 is known to stimulate chondrogenic as well as osteogenic differentiation, with increases in the chondrogenic transcription factor sox9, the cartilage ECM protein Col-2, and the hypertropic chondrocytic marker Col-10 frequently being noted following low-dose BMP2 stimulation 78–81. Thus, the present AFABP and Col-10 data indicate that PDMS incorporation may improve the osteogenic specificity of BMP2 bioactivity. Representative images of Col-2 immunostaining are presented in Supplementary Figure 1.
Figure 4.
Comparison of cMSC chondrogenic or adipogenic responses following 21 days of culture in PEG-PDMS, PEG-BMP2, and PEG-PDMS-BMP2 scaffolds. Levels of Col-2, Col-10 and AFABP relative to PDMS hydrogels. All data are normalized to the PEG-PDMS group. ‘$’ denotes a significant difference relative to PEG-PDMS controls. ‘*’ denotes a significant difference relative to the PEG-BMP2 group.
Although data from a single canine donor are shown in Figures 3 & 4, confirmatory experiments with PEG-PDMS-BMP2 scaffolds were conducted for an additional two cMSC donors. A high degree of correlation in type and degree of response with respect to scaffold formulation was observed among donors for each of the markers assessed (runx2, Col-10, and AFABP; Supplementary Figure 2).
4. DISCUSSION
The success of MSC-based scaffolds for bone regeneration largely depends on the associated MSCs supporting new bone formation. Successful clinical translation of MSC-based bone grafts based on in vivo preclinical data requires not only a similarly in anatomy and healing responses between humans and the selected animal model, but also a similarity in their MSC responses to scaffold-based stimuli. However, little is known about the degree of correlation in osteogenic responses of human and canine MSCs to 3D scaffold environments. In the current study, human and canine MSCs were cultured in vitro and subjected to equivalent 3D scaffold environments for 21 days in the absence of osteogenic media supplements. Following culture, scaffolds were analyzed for protein levels of several osteogenic markers as well as for deposited calcium.
Experimental results showed a high degree of agreement in cMSC and hMSC osteogenic responses to RGDS-containing PEG and PEG-PDMS scaffolds, indicating that canine models may warrant further development as preclinical animal models for MSC-based bone graft evaluation. Specifically, the culture of cMSCs and hMSCs in PEG constructs for 21 days promoted accumulation of Col-1 and calcium deposition. Furthermore, the addition of PDMS to PEG-based constructs increased OPN production and matrix mineralization by both cMSCs and hMSCs relative to day 0. The current PEG scaffold results are consistent with previous reports demonstrating that PEG constructs containing tethered RGD were able to facilitate MSC osteogenic differentiation and matrix mineralization over time 82,83. The PEG-PDMS results also support previous work demonstrating siloxane and/or PDMS to intrinsically support matrix mineralization 39,84–86 and to have an overall osteoinductive effect on human, rabbit and murine mesenchymal progenitor cells 41,85–87. That said, the present data indicated Col-1 deposition in the PEG-PDMS constructs to be lower than that in corresponding PEG controls for both cMSCs and hMSCs. This latter result is in contrast to previous work with PEG-PDMS scaffolds and murine mesenchymal progenitor cells in which a positive correlation between Col-1 levels and PDMS incorporation was observed 41. This distinction underscores the need for appropriate animal model selection for both in vitro and in vivo testing.
In order to harness the positive effects of PDMS on calcium and OPN deposition while potentially minimizing its negative impact on Col-1 levels, low-dose BMP2 was incorporated into the PEG-PDMS constructs. Specifically, BMP2 was incorporated at 100 ng/mL, a dose ∼10,000-fold lower than that associated with the BMP2-loaded collagen sponges currently approved for certain in vivo applications 53. The incorporated BMP2 was covalently-conjugated into the scaffold network in order to take advantage of the prolonged BMP2 retention and the potential for repeated signaling that tethering introduces 31. PEG-PDMS-BMP2 scaffolds were associated with a 2.2-fold increase in osterix expression, a 2.0-fold increase in OPN production, and a 1.9-fold increase in calcium deposition relative to pure PEG-PDMS systems. These results (obtained in the absence of osteogenic media supplements) are consistent in degree with the osteogenic effects previously observed following incorporation of substantially higher doses of tethered BMP2 (200–500 ng/mL) within various scaffold systems (usually cultured in the presence of osteogenic media supplements) 31,50,59,88,89. For instance, Liu et. al. 31 reported that tethering 500 ng/ml of BMP2 into PEG-based scaffolds resulted in a ∼1.5-fold increase in calcium deposition after 12 days of culture in osteogenic induction medium. We report a 1.9-fold increase with 100 ng/mL BMP2 addition to PEG-PDMS constructs cultured for 21 days in the absence of osteogenic supplements. By way of further comparison, addition of 0.1 mg/ml of BMP2 (1000 times the current dose) to thiolated chitosan scaffolds promoted a 4-fold increase in calcium deposition after 21 days of culture in osteogenic media 90.
In contrast to matrix mineralization, the addition of BMP2 to PEG-PDMS networks did not promote a significant increase in the osteogenic ECM protein Col-1 relative to PEG-PDMS scaffolds, despite the marked increase in Col-1 noted with the incorporation of BMP2 alone. In addition, the addition of PDMS to pure PEG scaffolds appeared to reduce Col-1 deposition relative to PEG only controls. These results indicate that PDMS may have a suppressive effect on Col-1 production. Similarly, assessment of the hypertrophic chondrocytic marker Col-10 in the PEG-PDMS-BMP2 scaffolds revealed that the presence of PDMS appeared to limit the production of Col-10 stimulated by BMP2 alone. Cumulatively, the present results indicate that PEG-PDMS-BMP2 constructs successfully promote specific osteogenic differentiation of cMSCs even in the absence of osteogenic media supplements.
In terms of mechanism, a combination of substrate-based stimuli along with growth factor signaling could potentially underlie the enhanced MSC osteogenic response noted for the PEG-PDMS-BMP2 scaffolds, although the present work cannot definitively state the relative contributions of each. In terms of substrate-based stimuli, Si-based additives have generally been demonstrated to be osteoinductive through increasing HAp deposits 39,85,86,91,92 as well as through altering the local nanotopography and hydrophobicity experienced by MSCs 93. In terms of BMP2 signaling, BMPs exert their effects through binding to cell surface receptors and forming a heterotetrameric complex comprised of two dimers of type I and type II receptors. The formation of this complex initiates a signal transduction cascade which results in functional changes within the cell without the need for BMP internalization or translocation to the nucleus 94,95. Further supporting this mechanism of signal transduction, Liu et al. demonstrated enhanced osteogenic differentiation (osteocalcin, OPN, and BMP2 expression) in MSCs treated with tethered-BMP2 relative to MSCs treated with equivalent levels of soluble BMP2 31. This enhanced bioactivity of conjugated BMP2 relative to soluble BMP2 is believed to result from the prolonged signaling enabled by tethering, which hinders of BMP2 uptake and/or degradation 31. Given the similar bulk tensile moduli and average mesh size across scaffold formulations, the beneficial MSC response noted in the PDMS-BMP2 scaffolds likely reflects the combined effects of cellular interactions with tethered BMP2, the induced HAp deposits, and the material nanostructure. However, addition studies would be needed to confirm these potential mechanisms of action. Future work utilizing nanoscale mechanical testing with atomic force microscopy could help decouple the contributions from these factors.
A few limitations to the present study merit comment. First, the current work focused solely on hMSCs and cMSCs and did not investigate potential species differences among supporting cell types (e.g. osteoblasts osteoclasts, osteocytes, and macrophages) that are also important for regeneration. It should be noted, however, that although some species differences have been found for human versus canine MSCs 38,96 and macrophages 97, the overall degree of similarity between bone composition 98, cell and tissue response to stimuli 99–107, and pathological outcomes 108–111 between these two species highlights a significant overlap in behaviors. Furthermore, evaluation of additional hMSC and cMSC donors may be needed for definitive conclusions to be made regarding inter-species similarity in the osteoinductive effects of PEG-PDMS scaffolds. This is due to conflicting literature regarding age and gender effects on MSC osteogenic responses, with some studies indicating significant differences with age and gender 112 and others reporting a lack of significant differences in age and gender 113. As such, future work will confirm hMSC and cMSC responses to PEG-PDMS and PEG-PDMS-BMP2 scaffolds utilizing additional donors to more fully control for both age and gender.
5. CONCLUSIONS
The current study investigated, for the first time, the correlation between the osteogenic responses of cMSCs and hMSCs cultured within PEG scaffolds containing osteoinductive PDMS. The similarity in the osteogenic responses observed between cMSCs and hMSCs provides strong initial support for the use of cMSCs for the in vitro evaluation of MSC-based bone grafts. Using cMSCs, we further evaluated the efficacy of low-dose, tethered BMP2 in enhancing the osteoinductivity of PEG-PDMS scaffolds. The combined presence of PDMS and BMP2 significantly increased osterix, OPN, and mineralization levels relative to PEG-PDMS scaffolds while reducing the chondrogenic effects of BMP2 alone. These data suggest that low-dose BMP2 can be effective in driving osteogenesis when coupled with an intrinsically osteoinductive material.
Supplementary Material
Acknowledgments
The authors acknowledge the NIH NIBIB, the NIH NIDCR, and the AKC-CHF for funding.
References
- 1.Chan RK, Siller-Jackson A, Verrett AJ, Wu J, Hale RG. Ten years of war: a characterization of craniomaxillofacial injuries incurred during operations Enduring Freedom and Iraqi Freedom. J Trauma Acute Care Surg. 2012;73(6 Suppl 5):S453–8. doi: 10.1097/TA.0b013e3182754868. [DOI] [PubMed] [Google Scholar]
- 2.Wehby GL, Cassell CH. The impact of orofacial clefts on quality of life and healthcare use and costs. Oral Dis. 2010;16(1):3–10. doi: 10.1111/j.1601-0825.2009.01588.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dixon MJ, Marazita ML, Beaty TH, Murray JC. Cleft lip and palate: understanding genetic and environmental influences. Nat Rev Genet. 2011;12(3):167–78. doi: 10.1038/nrg2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zuk PA. Tissue Engineering Craniofacial Defects With Adult Stem Cells? Are We Ready Yet? Pediatric Research. 2008;63(5):478–486. doi: 10.1203/PDR.0b013e31816bdf36. [DOI] [PubMed] [Google Scholar]
- 5.Greenberg AMPJ. Craniomaxillofacial Reconstructive and Corrective Bone Surgery Principles of Internal Fixation Using AO/ASIF Technique. Spinger; 2002. [Google Scholar]
- 6.Kretlow JD, Young S, Klouda L, Wong M, Mikos AG. Injectable biomaterials for regenerating complex craniofacial tissues. Adv Mater. 2009;21(32–33):3368–93. doi: 10.1002/adma.200802009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhumiratana S, Vunjak-Novakovic G. Concise review: personalized human bone grafts for reconstructing head and face. Stem Cells Transl Med. 2012;1(1):64–9. doi: 10.5966/sctm.2011-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goodrich JT, Sandler AL, Tepper O. A review of reconstructive materials for use in craniofacial surgery bone fixation materials, bone substitutes, and distractors. Childs Nerv Syst. 2012;28(9):1577–88. doi: 10.1007/s00381-012-1776-y. [DOI] [PubMed] [Google Scholar]
- 9.Pagni G, Kaigler D, Rasperini G, Avila-Ortiz G, Bartel R, Giannobile WV. Bone repair cells for craniofacial regeneration. Adv Drug Deliv Rev. 2012;64(12):1310–9. doi: 10.1016/j.addr.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mao JJ, Giannobile WV, Helms JA, Hollister SJ, Krebsbach PH, Longaker MT, Shi S. Craniofacial tissue engineering by stem cells. J Dent Res. 2006;85(11):966–79. doi: 10.1177/154405910608501101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hollister SJ, Lin CY, Saito E, Lin CY, Schek RD, Taboas JM, Williams JM, Partee B, Flanagan CL, Diggs A, et al. Engineering craniofacial scaffolds. Orthod Craniofac Res. 2005;8(3):162–73. doi: 10.1111/j.1601-6343.2005.00329.x. [DOI] [PubMed] [Google Scholar]
- 12.Bhumiratana S, Vunjak-Novakovic G. Concise Review: Personalized Human Bone Grafts for Reconstructing Head and Face. Stem Cells Translational Medicine. 2012;1(1):64–69. doi: 10.5966/sctm.2011-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Byrd HS, Hobar PC, Shewmake K. Augmentation of the craniofacial skeleton with porous hydroxyapatite granules. Plastic and reconstructive surgery. 1993;91(1):15–22. [PubMed] [Google Scholar]
- 14.David L, Argenta L, Fisher D. Hydroxyapatite cement in pediatric craniofacial reconstruction. Journal of Craniofacial Surgery. 2005;16(1):129–133. doi: 10.1097/00001665-200501000-00026. [DOI] [PubMed] [Google Scholar]
- 15.Jackson IT, Yavuzer R. Hydroxyapatite cement: an alternative for craniofacial skeletal contour refinements. British journal of plastic surgery. 2000;53(1):24–29. doi: 10.1054/bjps.1999.3236. [DOI] [PubMed] [Google Scholar]
- 16.Byrd HS, Hobar PC, Shewmake K. Augmentation of the craniofacial skeleton with porous hydroxyapatite granules. Plast Reconstr Surg. 1993;91(1):15–22. discussion 23-6. [PubMed] [Google Scholar]
- 17.Greenspan DC. Bioactive ceramic implant materials. Current Opinion in Solid State and Materials Science. 1999;4(4):389–393. [Google Scholar]
- 18.Montjovent MO, Mathieu L, Schmoekel H, Mark S, Bourban PE, Zambelli PY, Laurent-Applegate LA, Pioletti DP. Repair of critical size defects in the rat cranium using ceramic-reinforced PLA scaffolds obtained by supercritical gas foaming. J Biomed Mater Res A. 2007;83(1):41–51. doi: 10.1002/jbm.a.31208. [DOI] [PubMed] [Google Scholar]
- 19.Suominen E, Kinnunen J. Bioactive glass granules and plates in the reconstruction of defects of the facial bones. Scand J Plast Reconstr Surg Hand Surg. 1996;30(4):281–9. doi: 10.3109/02844319609056406. [DOI] [PubMed] [Google Scholar]
- 20.Schneider G, Blechschmidt K, Linde D, Litschko P, Korbs T, Beleites E. Bone regeneration with glass ceramic implants and calcium phosphate cements in a rabbit cranial defect model. J Mater Sci Mater Med. 2010;21(10):2853–9. doi: 10.1007/s10856-010-4143-0. [DOI] [PubMed] [Google Scholar]
- 21.Wink JD, Gerety PA, Sherif RD, Lim Y, Clarke NA, Rajapakse CS, Nah H-D, Taylor JA. Sustained delivery of rhBMP-2 via PLGA microspheres: cranial bone regeneration without heterotopic ossification or craniosynostosis. Plastic and Reconstructive Surgery. 2014 doi: 10.1097/PRS.0000000000000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eppley BL, Morales L, Wood R, Pensler J, Goldstein J, Havlik RJ, Habal M, Losken A, Williams JK, Burstein F. Resorbable PLLA-PGA plate and screw fixation in pediatric craniofacial surgery: clinical experience in 1883 patients. Plastic and reconstructive surgery. 2004;114(4):850–856. doi: 10.1097/01.prs.0000132856.69391.43. [DOI] [PubMed] [Google Scholar]
- 23.Wink JD, Gerety PA, Sherif RD, Lim Y, Clarke NA, Rajapakse CS, Nah HD, Taylor JA. Sustained delivery of rhBMP-2 by means of poly(lactic-co-glycolic acid) microspheres: cranial bone regeneration without heterotopic ossification or craniosynostosis. Plast Reconstr Surg. 2014;134(1):51–9. doi: 10.1097/PRS.0000000000000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cabraja M, Klein M, Lehmann T-N. Long-term results following titanium cranioplasty of large skull defects. Neurosurgical focus. 2009;26(6):E10. doi: 10.3171/2009.3.FOCUS091. [DOI] [PubMed] [Google Scholar]
- 25.Kuttenberger JJ, Hardt N. Long-term results following reconstruction of craniofacial defects with titanium micro-mesh systems. Journal of Cranio-Maxillofacial Surgery. 2001;29(2):75–81. doi: 10.1054/jcms.2001.0197. [DOI] [PubMed] [Google Scholar]
- 26.Cabraja M, Klein M, Lehmann TN. Long-term results following titanium cranioplasty of large skull defects. Neurosurg Focus. 2009;26(6):E10. doi: 10.3171/2009.3.FOCUS091. [DOI] [PubMed] [Google Scholar]
- 27.Kruijt Spanjer EC, Bittermann GKP, van Hooijdonk IEM, Rosenberg A, Gawlitta D. Taking the endochondral route to craniomaxillofacial bone regeneration: A logical approach? J Craniomaxillofac Surg. 2017;45(7):1099–1106. doi: 10.1016/j.jcms.2017.03.025. [DOI] [PubMed] [Google Scholar]
- 28.Montjovent MO, Mathieu L, Schmoekel H, Mark S, Bourban PE, Zambelli PY, Laurent-Applegate LA, Pioletti DP. Repair of critical size defects in the rat cranium using ceramic-reinforced PLA scaffolds obtained by supercritical gas foaming. Journal of Biomedical Materials Research Part A. 2007;83(1):41–51. doi: 10.1002/jbm.a.31208. [DOI] [PubMed] [Google Scholar]
- 29.Suominen E, Kinnunen J. Bioactive glass granules and plates in the reconstruction of defects of the facial bones. Scandinavian journal of plastic and reconstructive surgery and hand surgery. 1996;30(4):281–289. doi: 10.3109/02844319609056406. [DOI] [PubMed] [Google Scholar]
- 30.Schneider G, Blechschmidt K, Linde D, Litschko P, Körbs T, Beleites E. Bone regeneration with glass ceramic implants and calcium phosphate cements in a rabbit cranial defect model. Journal of Materials Science: Materials in Medicine. 2010;21(10):2853–2859. doi: 10.1007/s10856-010-4143-0. [DOI] [PubMed] [Google Scholar]
- 31.Liu HW, Chen CH, Tsai CL, Lin IH, Hsiue GH. Heterobifunctional poly(ethylene glycol)-tethered bone morphogenetic protein-2-stimulated bone marrow mesenchymal stromal cell differentiation and osteogenesis. Tissue Eng. 2007;13(5):1113–24. doi: 10.1089/ten.2006.0209. [DOI] [PubMed] [Google Scholar]
- 32.Barati D, Shariati SRP, Moeinzadeh S, Melero-Martin JM, Khademhosseini A, Jabbari E. Spatiotemporal release of BMP-2 and VEGF enhances osteogenic and vasculogenic differentiation of human mesenchymal stem cells and endothelial colony-forming cells co-encapsulated in a patterned hydrogel. J Control Release. 2016;223:126–136. doi: 10.1016/j.jconrel.2015.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stavropoulos A, Sculean A, Bosshardt DD, Buser D, Klinge B. Pre-clinical in vivo models for the screening of bone biomaterials for oral/craniofacial indications: focus on small-animal models. Periodontol 2000. 2015;68(1):55–65. doi: 10.1111/prd.12065. [DOI] [PubMed] [Google Scholar]
- 34.Peric M, Dumic-Cule I, Grcevic D, Matijasic M, Verbanac D, Paul R, Grgurevic L, Trkulja V, Bagi CM, Vukicevic S. The rational use of animal models in the evaluation of novel bone regenerative therapies. Bone. 2015;70:73–86. doi: 10.1016/j.bone.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 35.Pearce AI, Richards RG, Milz S, Schneider E, Pearce SG. Animal models for implant biomaterial research in bone: a review. Eur Cell Mater. 2007;13:1–10. doi: 10.22203/ecm.v013a01. [DOI] [PubMed] [Google Scholar]
- 36.Liebschner MAK. Biomechanical considerations of animal models used in tissue engineering of bone. Biomaterials. 2004;25(9):1697–1714. doi: 10.1016/s0142-9612(03)00515-5. [DOI] [PubMed] [Google Scholar]
- 37.Carlisle PL, Guda T, Silliman DT, Lien W, Hale RG, Brown Baer PR. Investigation of a pre-clinical mandibular bone notch defect model in miniature pigs: clinical computed tomography, micro-computed tomography, and histological evaluation. J Korean Assoc Oral Maxillofac Surg. 2016;42(1):20–30. doi: 10.5125/jkaoms.2016.42.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bach FC, Miranda-Bedate A, van Heel FW, Riemers FM, Muller MC, Creemers LB, Ito K, Benz K, Meij BP, Tryfonidou MA. Bone Morphogenetic Protein-2, But Not Mesenchymal Stromal Cells, Exert Regenerative Effects on Canine and Human Nucleus Pulposus Cells. Tissue Eng Part A. 2017;23(5–6):233–242. doi: 10.1089/ten.TEA.2016.0251. [DOI] [PubMed] [Google Scholar]
- 39.Bailey BM, Fei R, Munoz-Pinto D, Hahn MS, Grunlan MA. PDMS(star)-PEG hydrogels prepared via solvent-induced phase separation (SIPS) and their potential utility as tissue engineering scaffolds. Acta Biomater. 2012;8(12):4324–33. doi: 10.1016/j.actbio.2012.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hou Y, Schoener CA, Regan KR, Munoz-Pinto D, Hahn MS, Grunlan MA. Photo-cross-linked PDMSstar-PEG hydrogels: synthesis, characterization, and potential application for tissue engineering scaffolds. Biomacromolecules. 2010;11(3):648–56. doi: 10.1021/bm9012293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Munoz-Pinto DJ, Jimenez-Vergara AC, Hou Y, Hayenga HN, Rivas A, Grunlan M, Hahn MS. Osteogenic potential of poly(ethylene glycol)-poly(dimethylsiloxane) hybrid hydrogels. Tissue Eng Part A. 2012;18(15–16):1710–9. doi: 10.1089/ten.tea.2011.0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Catauro M, Bollino F, Papale F, Gallicchio M, Pacifico S. Influence of the polymer amount on bioactivity and biocompatibility of SiO2/PEG hybrid materials synthesized by sol-gel technique. Mater Sci Eng C Mater Biol Appl. 2015;48:548–55. doi: 10.1016/j.msec.2014.12.035. [DOI] [PubMed] [Google Scholar]
- 43.Catauro M, Renella RA, Papale F, Vecchio Ciprioti S. Investigation of bioactivity, biocompatibility and thermal behavior of sol-gel silica glass containing a high PEG percentage. Mater Sci Eng C Mater Biol Appl. 2016;61:51–5. doi: 10.1016/j.msec.2015.11.077. [DOI] [PubMed] [Google Scholar]
- 44.Chen J, Du Y, Que W, Xing Y, Chen X, Lei B. Crack-free polydimethylsiloxane-bioactive glass-poly(ethylene glycol) hybrid monoliths with controlled biomineralization activity and mechanical property for bone tissue regeneration. Colloids Surf B Biointerfaces. 2015;136:126–33. doi: 10.1016/j.colsurfb.2015.08.053. [DOI] [PubMed] [Google Scholar]
- 45.Benoit DS, Schwartz MP, Durney AR, Anseth KS. Small functional groups for controlled differentiation of hydrogel-encapsulated human mesenchymal stem cells. Nat Mater. 2008;7(10):816–23. doi: 10.1038/nmat2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Becerra-Bayona S, Guiza-Arguello V, Qu X, Munoz-Pinto DJ, Hahn MS. Influence of select extracellular matrix proteins on mesenchymal stem cell osteogenic commitment in three-dimensional contexts. Acta Biomater. 2012;8(12):4397–404. doi: 10.1016/j.actbio.2012.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim J, Hefferan TE, Yaszemski MJ, Lu L. Potential of hydrogels based on poly(ethylene glycol) and sebacic acid as orthopedic tissue engineering scaffolds. Tissue Eng Part A. 2009;15(8):2299–307. doi: 10.1089/ten.tea.2008.0326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fassbender M, Minkwitz S, Strobel C, Schmidmaier G, Wildemann B. Stimulation of bone healing by sustained bone morphogenetic protein 2 (BMP-2) delivery. Int J Mol Sci. 2014;15(5):8539–52. doi: 10.3390/ijms15058539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sonnet C, Simpson CL, Olabisi RM, Sullivan K, Lazard Z, Gugala Z, Peroni JF, Weh JM, Davis AR, West JL, et al. Rapid healing of femoral defects in rats with low dose sustained BMP2 expression from PEGDA hydrogel microspheres. J Orthop Res. 2013;31(10):1597–604. doi: 10.1002/jor.22407. [DOI] [PubMed] [Google Scholar]
- 50.He X, Liu Y, Yuan X, Lu L. Enhanced healing of rat calvarial defects with MSCs loaded on BMP-2 releasing chitosan/alginate/hydroxyapatite scaffolds. PLoS One. 2014;9(8):e104061. doi: 10.1371/journal.pone.0104061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Volk SW, Diefenderfer DL, Christopher SA, Haskins ME, Leboy PS. Effects of osteogenic inducers on cultures of canine mesenchymal stem cells. Am J Vet Res. 2005;66(10):1729–37. doi: 10.2460/ajvr.2005.66.1729. [DOI] [PubMed] [Google Scholar]
- 52.Volk SW, Wang Y, Hankenson KD. Effects of donor characteristics and ex vivo expansion on canine mesenchymal stem cell properties: implications for MSC-based therapies. Cell Transplant. 2012;21(10):2189–200. doi: 10.3727/096368912X636821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Davies SD, Ochs MW. Bone morphogenetic proteins in craniomaxillofacial surgery. Oral Maxillofac Surg Clin North Am. 2010;22(1):17–31. doi: 10.1016/j.coms.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 54.Shields LBE, Raque GH, Glassman SD, Campbell M, Vitaz T, Harpring J, Shields CB. Adverse effects associated with high-dose recombinant human bone morphogenetic protein-2 use in anterior cervical spine fusion. Spine. 2006;31(5):542–547. doi: 10.1097/01.brs.0000201424.27509.72. [DOI] [PubMed] [Google Scholar]
- 55.Smucker JD, Rhee JM, Singh K, Yoon ST, Heller JG. Increased swelling complications associated with off-label usage of rhBMP-2 in the anterior cervical spine. Spine (Phila Pa 1976) 2006;31(24):2813–9. doi: 10.1097/01.brs.0000245863.52371.c2. [DOI] [PubMed] [Google Scholar]
- 56.Wong DA, Kumar A, Jatana S, Ghiselli G, Wong K. Neurologic impairment from ectopic bone in the lumbar canal: a potential complication of off-label PLIF/TLIF use of bone morphogenetic protein-2 (BMP-2) Spine J. 2008;8(6):1011–8. doi: 10.1016/j.spinee.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 57.Tabisz B, Schmitz W, Schmitz M, Luehmann T, Heusler E, Rybak JC, Meinel L, Fiebig JE, Mueller TD, Nickel J. Site-Directed Immobilization of BMP-2: Two Approaches for the Production of Innovative Osteoinductive Scaffolds. Biomacromolecules. 2017;18(3):695–708. doi: 10.1021/acs.biomac.6b01407. [DOI] [PubMed] [Google Scholar]
- 58.Liu HW, Chen CH, Tsai CL, Hsiue GH. Targeted delivery system for juxtacrine signaling growth factor based on rhBMP-2-mediated carrier-protein conjugation. Bone. 2006;39(4):825–36. doi: 10.1016/j.bone.2006.04.027. [DOI] [PubMed] [Google Scholar]
- 59.Moeinzadeh S, Barati D, He X, Jabbari E. Gelation characteristics and osteogenic differentiation of stromal cells in inert hydrolytically degradable micellar polyethylene glycol hydrogels. Biomacromolecules. 2012;13(7):2073–86. doi: 10.1021/bm300453k. [DOI] [PubMed] [Google Scholar]
- 60.Munoz-Pinto DJ, McMahon RE, Kanzelberger MA, Jimenez-Vergara AC, Grunlan MA, Hahn MS. Inorganic-organic hybrid scaffolds for osteochondral regeneration. J Biomed Mater Res A. 2010;94(1):112–21. doi: 10.1002/jbm.a.32695. [DOI] [PubMed] [Google Scholar]
- 61.Hahn MS, Miller JS, West JL. Laser scanning lithography for surface micropatterning on hydrogels. Advanced Materials. 2005;17(24):2939–2942. [Google Scholar]
- 62.Hahn MS, Miller JS, West JL. Three-dimensional biochemical and biomechanical patterning of hydrogels for guiding cell behavior. Advanced Materials. 2006;18(20):2679–2684. [Google Scholar]
- 63.Johnson CP, How T, Scraggs M, West CR, Burns J. A biomechanical study of the human vertebral artery with implications for fatal arterial injury. Forensic Sci Int. 2000;109(3):169–82. doi: 10.1016/s0379-0738(99)00198-x. [DOI] [PubMed] [Google Scholar]
- 64.Watkins AW, Anseth KS. Investigation of molecular transport and distributions in poly (ethylene glycol) hydrogels with confocal laser scanning microscopy. Macromolecules. 2005;38(4):1326–1334. [Google Scholar]
- 65.Wolfe M, Pochampally R, Swaney W, Reger RL. Isolation and culture of bone marrow-derived human multipotent stromal cells (hMSCs) Springer; 2008. pp. 3–25. [DOI] [PubMed] [Google Scholar]
- 66.Liao H, Munoz-Pinto D, Qu X, Hou Y, Grunlan MA, Hahn MS. Influence of hydrogel mechanical properties and mesh size on vocal fold fibroblast extracellular matrix production and phenotype. Acta Biomater. 2008;4(5):1161–71. doi: 10.1016/j.actbio.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Salinas CN, Anseth KS. The influence of the RGD peptide motif and its contextual presentation in PEG gels on human mesenchymal stem cell viability. J Tissue Eng Regen Med. 2008;2(5):296–304. doi: 10.1002/term.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Benoit DSW, Schwartz MP, Durney AR, Anseth KS. Small functional groups for controlled differentiation of hydrogel-encapsulated human mesenchymal stem cells. Nat Mater. 2008;7(10):816–823. doi: 10.1038/nmat2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Salinas CN, Anseth KS. The enhancement of chondrogenic differentiation of human mesenchymal stem cells by enzymatically regulated RGD functionalities. Biomaterials. 2008;29(15):2370–7. doi: 10.1016/j.biomaterials.2008.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jimenez-Vergara AC, Munoz-Pinto DJ, Hahn MS. Influence of pressurized cyclic stretch and endothelial cell presence on multipotent stem cell osteogenic commitment. Integr Biol (Camb) 2013;5(7):983–92. doi: 10.1039/c3ib20186d. [DOI] [PubMed] [Google Scholar]
- 71.Kang BJ, Ryu HH, Park SS, Koyama Y, Kikuchi M, Woo HM, Kim WH, Kweon OK. Comparing the osteogenic potential of canine mesenchymal stem cells derived from adipose tissues, bone marrow, umbilical cord blood, and Wharton's jelly for treating bone defects. J Vet Sci. 2012;13(3):299–310. doi: 10.4142/jvs.2012.13.3.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rasini V, Dominici M, Kluba T, Siegel G, Lusenti G, Northoff H, Horwitz EM, Schafer R. Mesenchymal stromal/stem cells markers in the human bone marrow. Cytotherapy. 2013;15(3):292–306. doi: 10.1016/j.jcyt.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 73.de Bakker E, Van Ryssen B, De Schauwer C, Meyer E. Canine mesenchymal stem cells: state of the art, perspectives as therapy for dogs and as a model for man. Vet Q. 2013;33(4):225–33. doi: 10.1080/01652176.2013.873963. [DOI] [PubMed] [Google Scholar]
- 74.Bertolo A, Steffen F, Malonzo-Marty C, Stoyanov J. Canine Mesenchymal Stem Cell Potential and the Importance of Dog Breed: Implication for Cell-Based Therapies. Cell Transplant. 2015;24(10):1969–80. doi: 10.3727/096368914X685294. [DOI] [PubMed] [Google Scholar]
- 75.Chow L, Johnson V, Coy J, Regan D, Dow S. Mechanisms of Immune Suppression Utilized by Canine Adipose and Bone Marrow-Derived Mesenchymal Stem Cells. Stem Cells Dev. 2017;26(5):374–389. doi: 10.1089/scd.2016.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zara JN, Siu RK, Zhang X, Shen J, Ngo R, Lee M, Li W, Chiang M, Chung J, Kwak J, et al. High doses of bone morphogenetic protein 2 induce structurally abnormal bone and inflammation in vivo. Tissue Eng Part A. 2011;17(9–10):1389–99. doi: 10.1089/ten.tea.2010.0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jorgensen NR, Henriksen Z, Sorensen OH, Civitelli R. Dexamethasone, BMP-2, and 1,25-dihydroxyvitamin D enhance a more differentiated osteoblast phenotype: validation of an in vitro model for human bone marrow-derived primary osteoblasts. Steroids. 2004;69(4):219–26. doi: 10.1016/j.steroids.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 78.Nirmal RS, Nair PD. Significance of soluble growth factors in the chondrogenic response of human umbilical cord matrix stem cells in a porous three dimensional scaffold. European Cells and Materials. 2013;26:234–251. doi: 10.22203/ecm.v026a17. [DOI] [PubMed] [Google Scholar]
- 79.Steinert AF, Proffen B, Kunz M, Hendrich C, Ghivizzani SC, Noth U, Rethwilm A, Eulert J, Evans CH. Hypertrophy is induced during the in vitro chondrogenic differentiation of human mesenchymal stem cells by bone morphogenetic protein-2 and bone morphogenetic protein-4 gene transfer. Arthritis Res Ther. 2009;11(5):R148. doi: 10.1186/ar2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kwon SH, Lee TJ, Park J, Hwang JE, Jin M, Jang HK, Hwang NS, Kim BS. Modulation of BMP-2-induced chondrogenic versus osteogenic differentiation of human mesenchymal stem cells by cell-specific extracellular matrices. Tissue Eng Part A. 2013;19(1–2):49–58. doi: 10.1089/ten.tea.2012.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Schmitt B, Ringe J, Haupl T, Notter M, Manz R, Burmester GR, Sittinger M, Kaps C. BMP2 initiates chondrogenic lineage development of adult human mesenchymal stem cells in high-density culture. Differentiation. 2003;71(9–10):567–77. doi: 10.1111/j.1432-0436.2003.07109003.x. [DOI] [PubMed] [Google Scholar]
- 82.Yang F, Williams CG, Wang DA, Lee H, Manson PN, Elisseeff J. The effect of incorporating RGD adhesive peptide in polyethylene glycol diacrylate hydrogel on osteogenesis of bone marrow stromal cells. Biomaterials. 2005;26(30):5991–8. doi: 10.1016/j.biomaterials.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 83.Burdick JA, Anseth KS. Photoencapsulation of osteoblasts in injectable RGD-modified PEG hydrogels for bone tissue engineering. Biomaterials. 2002;23(22):4315–23. doi: 10.1016/s0142-9612(02)00176-x. [DOI] [PubMed] [Google Scholar]
- 84.Li POC, Kokubo T, Nakanishi K, Soga N, Nakamura T, Yamamuro T. Apatite Formation Induced by Silica Gel in a Simulated Body Fluid. Journal of the American Ceramic Society. 1992;75(8):3. [Google Scholar]
- 85.Nair BP, Gangadharan D, Mohan N, Sumathi B, Nair PD. Hybrid scaffold bearing polymer-siloxane Schiff base linkage for bone tissue engineering. Mater Sci Eng C Mater Biol Appl. 2015;52:333–42. doi: 10.1016/j.msec.2015.03.040. [DOI] [PubMed] [Google Scholar]
- 86.Silva SS, Ferreira RAS, Fu L, Carlos LD, Mano JF, Reis RL, Rocha J. Functional nanostructured chitosan–siloxane hybrids. J. Mater. Chem. 2005;15(35–36):3252–61. [Google Scholar]
- 87.Obata A, Kasuga T. Stimulation of human mesenchymal stem cells and osteoblasts activities in vitro on silicon-releasable scaffolds. J Biomed Mater Res A. 2009;91(1):11–7. doi: 10.1002/jbm.a.32181. [DOI] [PubMed] [Google Scholar]
- 88.Subramanian G, Bialorucki C, Yildirim-Ayan E. Nanofibrous yet injectable polycaprolactone-collagen bone tissue scaffold with osteoprogenitor cells and controlled release of bone morphogenetic protein-2. Mater Sci Eng C Mater Biol Appl. 2015;51:16–27. doi: 10.1016/j.msec.2015.02.030. [DOI] [PubMed] [Google Scholar]
- 89.Nath SD, Abueva C, Kim B, Lee BT. Chitosan-hyaluronic acid polyelectrolyte complex scaffold crosslinked with genipin for immobilization and controlled release of BMP-2. Carbohydr Polym. 2015;115:160–9. doi: 10.1016/j.carbpol.2014.08.077. [DOI] [PubMed] [Google Scholar]
- 90.Bae IH, Jeong BC, Kook MS, Kim SH, Koh JT. Evaluation of a thiolated chitosan scaffold for local delivery of BMP-2 for osteogenic differentiation and ectopic bone formation. Biomed Res Int. 2013;2013:878930. doi: 10.1155/2013/878930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rodrigues MT, Leonor IB, Groen N, Viegas CA, Dias IR, Caridade SG, Mano JF, Gomes ME, Reis RL. Bone marrow stromal cells on a three-dimensional bioactive fiber mesh undergo osteogenic differentiation in the absence of osteogenic media supplements: the effect of silanol groups. Acta Biomater. 2014;10(10):4175–85. doi: 10.1016/j.actbio.2014.05.026. [DOI] [PubMed] [Google Scholar]
- 92.Gaharwar AK, Mihaila SM, Swami A, Patel A, Sant S, Reis RL, Marques AP, Gomes ME, Khademhosseini A. Bioactive silicate nanoplatelets for osteogenic differentiation of human mesenchymal stem cells. Adv Mater. 2013;25(24):3329–36. doi: 10.1002/adma.201300584. [DOI] [PubMed] [Google Scholar]
- 93.Ayala R, Zhang C, Yang D, Hwang Y, Aung A, Shroff SS, Arce FT, Lal R, Arya G, Varghese S. Engineering the cell-material interface for controlling stem cell adhesion, migration, and differentiation. Biomaterials. 2011;32(15):3700–11. doi: 10.1016/j.biomaterials.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 94.Wang RN, Green J, Wang Z, Deng Y, Qiao M, Peabody M, Zhang Q, Ye J, Yan Z, Denduluri S, et al. Bone Morphogenetic Protein (BMP) signaling in development and human diseases. Genes Dis. 2014;1(1):87–105. doi: 10.1016/j.gendis.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Heldin CH, Miyazono K, ten Dijke P. TGF-beta signalling from cell membrane to nucleus through SMAD proteins. Nature. 1997;390(6659):465–71. doi: 10.1038/37284. [DOI] [PubMed] [Google Scholar]
- 96.Levi B, Nelson ER, Brown K, James AW, Xu D, Dunlevie R, Wu JC, Lee M, Wu B, Commons GW, et al. Differences in osteogenic differentiation of adipose-derived stromal cells from murine, canine, and human sources in vitro and in vivo. Plast Reconstr Surg. 2011;128(2):373–86. doi: 10.1097/PRS.0b013e31821e6e49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Herrmann I, Gotovina J, Fazekas-Singer J, Fischer MB, Hufnagl K, Bianchini R, Jensen-Jarolim E. Canine macrophages can like human macrophages be in vitro activated toward the M2a subtype relevant in allergy. Dev Comp Immunol. 2018;82:118–127. doi: 10.1016/j.dci.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 98.Aerssens J, Boonen S, Lowet G, Dequeker J. Interspecies differences in bone composition, density, and quality: potential implications for in vivo bone research. Endocrinology. 1998;139(2):663–70. doi: 10.1210/endo.139.2.5751. [DOI] [PubMed] [Google Scholar]
- 99.Requicha JF, Viegas CA, Albuquerque CM, Azevedo JM, Reis RL, Gomes ME. Effect of anatomical origin and cell passage number on the stemness and osteogenic differentiation potential of canine adipose-derived stem cells. Stem Cell Rev. 2012;8(4):1211–22. doi: 10.1007/s12015-012-9397-0. [DOI] [PubMed] [Google Scholar]
- 100.Garetto LP, Chen J, Parr JA, Roberts WE. Remodeling dynamics of bone supporting rigidly fixed titanium implants: a histomorphometric comparison in four species including humans. Implant Dent. 1995;4(4):235–43. doi: 10.1097/00008505-199500440-00002. [DOI] [PubMed] [Google Scholar]
- 101.Au AY, Au RY, Demko JL, McLaughlin RM, Eves BE, Frondoza CG. Consil bioactive glass particles enhance osteoblast proliferation and selectively modulate cell signaling pathways in vitro. J Biomed Mater Res A. 2010;94(2):380–8. doi: 10.1002/jbm.a.32668. [DOI] [PubMed] [Google Scholar]
- 102.Ding X, Zhou L, Wang J, Zhao Q, Lin X, Gao Y, Li S, Wu J, Rong M, Guo Z, et al. The effects of hierarchical micro/nanosurfaces decorated with TiO2 nanotubes on the bioactivity of titanium implants in vitro and in vivo. Int J Nanomedicine. 2015;10:6955–73. doi: 10.2147/IJN.S87347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kim MH, Park K, Choi KH, Kim SH, Kim SE, Jeong CM, Huh JB. Cell adhesion and in vivo osseointegration of sandblasted/acid etched/anodized dental implants. Int J Mol Sci. 2015;16(5):10324–36. doi: 10.3390/ijms160510324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kim SE, Kim CS, Yun YP, Yang DH, Park K, Kim SE, Jeong CM, Huh JB. Improving osteoblast functions and bone formation upon BMP-2 immobilization on titanium modified with heparin. Carbohydr Polym. 2014;114:123–32. doi: 10.1016/j.carbpol.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 105.Wu X, Liu X, Wei J, Ma J, Deng F, Wei S. Nano-TiO2/PEEK bioactive composite as a bone substitute material: in vitro and in vivo studies. Int J Nanomedicine. 2012;7:1215–25. doi: 10.2147/IJN.S28101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Nie FL, Zheng YF, Wei SC, Wang DS, Yu ZT, Salimgareeva GK, Polyakov AV, Valiev RZ. In vitro and in vivo studies on nanocrystalline Ti fabricated by equal channel angular pressing with microcrystalline CP Ti as control. J Biomed Mater Res A. 2013;101(6):1694–707. doi: 10.1002/jbm.a.34472. [DOI] [PubMed] [Google Scholar]
- 107.Im GI, Qureshi SA, Kenney J, Rubash HE, Shanbhag AS. Osteoblast proliferation and maturation by bisphosphonates. Biomaterials. 2004;25(18):4105–15. doi: 10.1016/j.biomaterials.2003.11.024. [DOI] [PubMed] [Google Scholar]
- 108.Morello E, Martano M, Buracco P. Biology, diagnosis and treatment of canine appendicular osteosarcoma: similarities and differences with human osteosarcoma. Vet J. 2011;189(3):268–77. doi: 10.1016/j.tvjl.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 109.Paoloni M, Davis S, Lana S, Withrow S, Sangiorgi L, Picci P, Hewitt S, Triche T, Meltzer P, Khanna C. Canine tumor cross-species genomics uncovers targets linked to osteosarcoma progression. BMC Genomics. 2009;10:625. doi: 10.1186/1471-2164-10-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sottnik JL, Campbell B, Mehra R, Behbahani-Nejad O, Hall CL, Keller ET. Osteocytes serve as a progenitor cell of osteosarcoma. J Cell Biochem. 2014;115(8):1420–9. doi: 10.1002/jcb.24793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Fossey SL, Liao AT, McCleese JK, Bear MD, Lin J, Li PK, Kisseberth WC, London CA. Characterization of STAT3 activation and expression in canine and human osteosarcoma. BMC Cancer. 2009;9:81. doi: 10.1186/1471-2407-9-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhou S, Greenberger JS, Epperly MW, Goff JP, Adler C, Leboff MS, Glowacki J. Age-related intrinsic changes in human bone-marrow-derived mesenchymal stem cells and their differentiation to osteoblasts. Aging Cell. 2008;7(3):335–43. doi: 10.1111/j.1474-9726.2008.00377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Siegel G, Kluba T, Hermanutz-Klein U, Bieback K, Northoff H, Schafer R. Phenotype, donor age and gender affect function of human bone marrow-derived mesenchymal stromal cells. BMC Med. 2013;11:146. doi: 10.1186/1741-7015-11-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jimenez-Vergara AC, Lewis J, Hahn MS, Munoz-Pinto DJ. An improved correlation to predict molecular weight between crosslinks based on equilibrium degree of swelling of hydrogel networks. J Biomed Mater Res B Appl Biomater. 2017 doi: 10.1002/jbm.b.33942. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.