Abstract
Objectives:
Despite screening, disparities exist in cervical cancer incidence and outcomes. Demographic factors are associated with diagnosis at advanced stage (AS), but less is known about geographic factors. We sought to investigate risk factors for developing AS cervical cancer in Alabama.
Methods:
We identified women treated for cervical cancer from 2005–2015 at our institution. Stages II-IV were considered AS. ZIP codes were categorized by federal Rural-Urban Commuting Area (RUCA) Codes, and 16 historically underserved counties were categorized as Black Belt Rural (BBR). Utilizing data from the American College of Obstetricians and Gynecologists (ACOG), we identified women’s health provider locations. We explored associations between stage and multiple factors using logistic regression.
Results:
Of 934 patients, 29.2% were black, 52.7% had AS cancer and 63.4% lived in urban areas. Average distance to nearest ACOG Fellow in urban, rural and BBR areas was 5.0, 10.6 and 13.7 miles, respectively. Black race, public insurance and age >65 were associated with increased risk of AS cancer. Living in a rural area trended towards higher risk but was not significant. When stratified by race, insurance status and age were associated with AS cancer in white women only.
Conclusions:
Living further from a women’s health provider or in a rural area was not associated with a higher risk of AS cervical cancer. Black women had a higher risk of AS than white women regardless of age, insurance status and geography. Disparities in cervical cancer are multifactorial and necessitate further research into socioeconomic, biologic and systems causes.
Keywords: cervical cancer, racial disparity, geographic disparity, health disparities, rural health, public health
Précis:
Black race remains a significant risk factor for development of advanced stage cervical cancer, while geography was not shown to affect stage at diagnosis.
Introduction
Cervical cancer is a worldwide public health problem causing significant morbidity and mortality. It is the second most common cancer among women and accounts for almost 300,000 deaths worldwide per year [1, 2]. In the United States, more than 12,000 new women are diagnosed annually [3, 4]. Despite widespread screening and increasing uptake of human papillomavirus (HPV) vaccination, over half of new diagnoses are advanced stage (AS) which carries high rates of morbidity and mortality as well as increased risk of recurrence [4, 5].
Similar to other healthcare disparities, the contributing factors to disparities in cervical cancer outcomes are multifactorial [2, 6]. Poverty, insurance status and race have all been shown to negatively affect HPV vaccination series completion rates, Pap screening rates and follow-up and treatment of abnormal Pap smear results [7–10]. Furthermore, disparities in stage at diagnosis, guideline-adherent care and outcomes have been demonstrated for cervical cancer [10–13]. Low socioeconomic status (SES), lack of access to reliable transportation, lack of health insurance and minority race have been shown to be associated with a diagnosis of AS cervical cancer [2, 14, 15]. In the United States, there is wide geographical variation in cervical cancer incidence and mortality rates with the highest rates seen in Appalachia, the South Atlantic, and lower Mississippi Valley. Alabama occupies the southernmost part of Appalachia [16, 17]. We have previously demonstrated the impact of distance from a comprehensive cancer center on overall survival in women diagnosed with cervical cancer, which highlights the importance of geographic location in obtaining and completing high quality cancer treatment [11]. Geographic measures such as the distance to nearest women’s health provider and residing in a rural area are potentially modifiable barriers to both prevention and treatment of cervical cancer; however, less is known about the effects of these factors on stage at diagnosis and their interaction with other factors that impact cervical cancer outcomes. Thus, we evaluated the geographic and sociodemographic risk factors for development of AS cervical cancer in our state.
Methods
Our institutional tumor registry was queried to identify a cohort of women treated for cervical cancer from 2005–2015 at the University of Alabama at Birmingham. Patients diagnosed with American Joint Committee on Cancer (AJCC) Stages II-IV were considered to have AS cervical cancer. ZIP codes were defined as rural or urban based on 2010 federal Rural-Urban Commuting Area (RUCA) Codes [18]. ZIP codes were further categorized as Black Belt Rural (BBR) if they were in one of 16 Black Belt counties, which are particularly medically underserved and rural with demonstrated disparities in other health outcomes whose population is approximately 50 percent African American (Figure 1) [19–23]. Utilizing data from the American College of Obstetricians and Gynecologists (ACOG), we identified practice locations of ACOG Fellows in the state. A total of 442 ACOG Fellows were identified including 383 Fellows, 44 Junior Fellows, 8 Associate Members and 7 Senior Status Fellows. This was used as a proxy for women’s health care providers. Estimated patient travel distance individually and combined with RUCA Codes have been used by other investigators to evaluate geospatial effects of residence on cancer outcomes [24]. Insurance status was classified as public, private or uninsured. Public insurance included Medicaid, Medicare, Tricare and Indian Health Services. There were 29 patients excluded from analysis due to unknown insurance status. Associations between stage and multiple factors including age, race, minimum distance between patient and nearest provider in miles, rurality, income and insurance status were explored using logistic regression using an alpha level of 0.05 for significance. SAS statistical software was used for analysis (SAS v9.4, SAS Institute, Cary, NC). This project was approved by our Institutional Review Board.
Figure 1. Traditional Counties of the Alabama Black Belt.
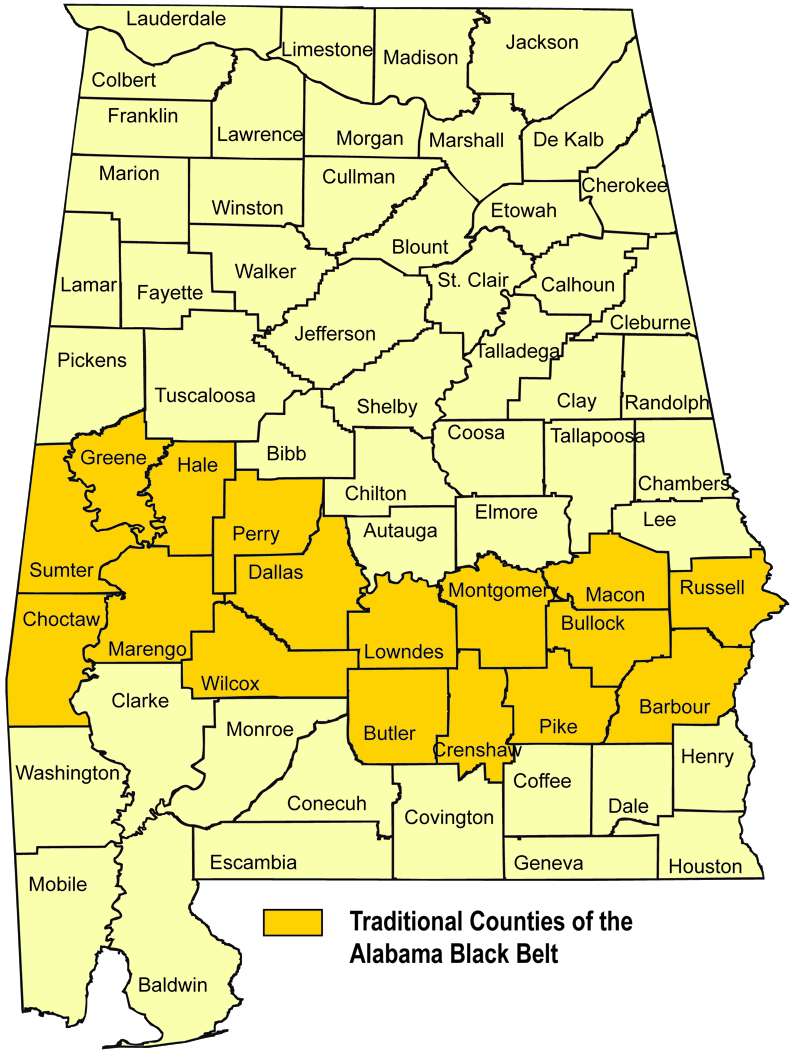
Source: Center for Business and Economic Research, The University of Alabama
Results
After exclusions, we identified 934 patients for the analysis. Of these, 273 (29.2%) patients were black and 661 (70.8%) were white. Mean age at diagnosis was 49.8 (SD 14.7). There were 493 patients with AS cervical cancer including: 197 (21.1%) Stage II, 210 (22.5%) Stage III and 86 (9.2%) Stage IV. 592 (63.4%) lived in urban areas and 342 (36.6%) in rural areas, including 85 in BBR areas (Table 1). Mean distance to the nearest women’s health provider for patients in urban, rural and BBR areas was 5.0, 10.6 and 13.7 miles, respectively. Black women were significantly more likely to have public insurance compared to white women (P <0.001) (Table 2).
Table 1.
Patient Characteristics
| Stage 1 | Stage II-V | Total | |
|---|---|---|---|
| Counts, N (%) | 441 (47) | 493 (53) | 934 |
| Age, mean (SD) | 47 (14.7) | 52 (14.3) | |
| Race | |||
| Black, N (%) | 125 (45) | 150 (55) | 273 |
| White, N (%) | 401 (61) | 260 (39) | 661 |
| Region | |||
| Urban, N (%) | 278 (48) | 296 (52) | 592 |
| Rural, N (%) | 125 (45) | 150 (55) | 342 |
| BBR, N (%) | 38 (45) | 47 (55) | 85 |
| Mean Income | $42,013 | $40,700 |
BBR – black belt rural
Table 2.
Insurance Status by Age, Race, and Rurality
| Private N (%) |
Public N (%) |
Uninsured N (%) |
Total | P value | |
|---|---|---|---|---|---|
| 346 (37) | 431 (46) | 128 (14) | 905 | ||
| Race | <0.0001 | ||||
| Black | 71 (27) | 160 (61) | 32 (12) | 263 | |
| White | 275 (43) | 271 (42) | 96 (15) | 642 | |
| Age | <0.0001 | ||||
| Age ≤50 | 239 (47) | 183 (36) | 91 (18) | 513 | |
| Age 50–65 | 88 (35) | 130 (52) | 34 (13) | 252 | |
| Age >65 | 19 (14) | 118 (84) | 3 (2) | 140 | |
| Rurality | 0.02 | ||||
| Rural | 117 (33) | 187 (53) | 47 (13) | 351 | |
| Urban | 229 (41) | 244 (44) | 81 (15) | 554 |
In the crude analysis, black race (OR 1.46; 95% CI 1.09–1.94), public insurance (compared to private, OR 1.80; 95% CI 1.35–2.40) and age >65 years (OR 1.95; 95% CI 1.34–2.85) were associated with increased risk of being diagnosed with AS cervical cancer. A shorter minimum distance to nearest women’s health provider did not have a significant effect on risk of AS disease (OR 0.995; 95% CI 0.98–1.01). Living in a rural (including BBR) area trended towards a higher risk of AS but was not statistically significant (OR 1.19; 95% CI 0.91–1.56) (Table 3). A significant interaction between race and insurance status on the outcome (P = 0.03) was noted; therefore, we conducted a stratified analysis by race. When stratified by race and adjusted for multiple factors in multivariate analysis, insurance status (both uninsured and public insurance) and older age were both associated with AS cancer in white women but not black women (Table 4).
Table 3.
Odds of Being Diagnosed with Advanced Stage Cervical Cancer
| Crude OR | 95% CI | |
|---|---|---|
| Age >65 vs. ≤50 | 1.95*** | 1.34–2.84 |
| Black vs. White | 1.46* | 1.09–1.94 |
| Rural vs. Urban | 1.19 | 0.91–1.56 |
| Shorter distance to provider | 0.99 | 0.98–1.01 |
| Uninsured † | 1.40 | 0.93–2.10 |
| Public Insurance† | 1.80*** | 1.35–2.4 |
| Higher income | 0.93 | 0.85–1.03 |
compared to women with private insurance
P-value:
= < 0.001
= < 0.05
Table 4.
Adjusted Odds of Being diagnosed with Advanced Stage Cervical Cancer – Stratified by Race
| Adjusted OR | 95% CI | |
|---|---|---|
| White | ||
| Age >65 vs. ≤50 | 1.70* | 1.03–2.83 |
| Rural vs. Urban | 0.99 | 0.68–1.46 |
| Uninsured† | 1.69* | 1.05–2.71 |
| Public insurance† | 1.93* | 1.34–2.69 |
| Black | ||
| Age >65 vs. ≤50 | 1.18 | 0.57–2.43 |
| Rural vs. Urban | 1.70 | 0.75–3.86 |
| Uninsured† | 0.77 | 0.32–1.82 |
| Public insurance† | 0.83 | 0.46–1.52 |
compared to women with private insurance
P-value:
= < 0.05
Discussion
In our analysis, AS cervical cancer was diagnosed in over half of cases, which indicates that there are ample opportunities for improvement in both prevention and early detection. We examined distance to nearest women’s health provider with the hypothesis that this can affect both primary and secondary prevention leading to delayed diagnosis. As expected, distance to nearest women’s health provider was greater in both rural and BBR ZIP codes. Interestingly, this longer distance was not associated with a higher risk of AS disease, with neither closer distance to the nearest provider or rurality associated with AS disease. Previous studies have shown that women who live in rural areas live farther from Pap screening and treatment services, and that lack of access to reliable transportation is associated with a higher likelihood of AS disease [2, 14, 15]. Furthermore, other studies have demonstrated the negative impact of distance from treatment facility for patients after diagnosis of both ovarian and cervical cancer [11, 25, 26]. However, this analysis indicates that other factors, namely race, age and insurance status, had a stronger influence on outcomes than did geography in our population.
When stratified by race, having public insurance and being uninsured were associated with AS cancer in white women but not black women. However, black women had a higher risk of AS cancer than white women regardless of age, insurance status, or geography. Our analysis is consistent with previous data showing that significant racial disparities exist, and that black race remains one of the strongest predictors of worse outcomes for women with cervical cancer [13, 27]. This is important in the context of recent analyses that demonstrate that racial disparities in cervical cancer are historically underestimated [13, 17]. The high rate of public insurance or lack of insurance among women diagnosed with cervical cancer in our series, as well as the association of insurance status with AS cervical cancer in white women reinforces the fact that funding status is an influential determinant of health disparities. Eliminating racial disparity, improving access to care and increasing insurance coverage are key determinants to the success in prevention and treatment of cervical cancer [8, 9, 28].
The strengths of our study include a large number of cases from a high-volume cancer center, minimal changes in management of AS disease over the study period and a wide range of variables available for analysis [29]. However, there are several limitations. While our tumor registry accounts for about 30% of the population in our state with cervical cancer, use of a single institution tumor registry may limit the sociodemographic distribution of patients and does not identify those treated elsewhere within the state. Further, histologic cancer type was not available for this analysis, which could affect results as non-squamous cancers are more likely to present at advanced stage. The use of ACOG data to identify women’s health providers may underestimate the number of medical professionals who provide preventive treatment for women, especially in rural areas. However, abnormal screening results require referral to physicians who offer biopsy or excisional procedures. These providers should be best identified by ACOG data. Our data do not include information regarding patient or provider mobility during the study period which could alter the geographic relationships between providers and patients over time. Women of racial/ethnic groups other than white and black were excluded due to their low numbers, and data were not available to control for individual medical comorbidities. Generalizability of these results may be limited as our results are representative of the outcomes resulting from screening, diagnosis and treatment within our state’s healthcare delivery system.
Conclusion
Our study demonstrates that access to care is a complex concept that cannot be equated solely to distance to care. There are other person-level mediators of access to care such as access to transportation which may make distance more or less important depending on the population in question. Furthermore, there may be a threshold above or below which distance becomes a vital mediator of access. Such evaluations are outside the scope of our investigation. However, this concept underlines the fact that attempts to identify and eliminate outcomes disparities must involve multiple disciplines including basic science, public health, epidemiology and clinical medicine and be specific to the target population. For example, HPV subtype and histologic differences by race have been demonstrated in cervical cancer, highlighting the importance of promoting racially diverse models for investigation of tumor biology and response to treatments [30, 31]. Improvements in public health infrastructure to eliminate barriers to screening, early diagnosis and high-quality cancer therapy must be advocated for at the local, state and national levels. Race, socioeconomic status and insurance status are determinants of initiation of HPV vaccination, adherence to screening guidelines and access to appropriate treatment. All of these should be targets for reducing incident cancer cases [7–9]. Stage at diagnosis, rates of guideline-adherent care and mortality are worse for non-white women [32]. Eliminating health disparities will require committed investigation to elucidate more targeted sources of inequitable care and outcomes [2, 6, 33].
Acknowledgments
Funding: Funding support was provided in part by NIH 3P30CA013148–43S3 to CAL; P30 CA13148 to SB and P50 CA098252 to SB and CAL.
Role of the Funding Source
Dr. Leath is supported by NIH 3P30CA013148–43S3. Dr. Bae is supported by NIH P30 CA13148. Both receive funding from NIH P50 CA098252. This research was not funded by any other source.
Abbreviations:
- AS
Advanced Stage
- HPV
human papillomavirus
- RUCA
Rural-Urban Commuting Area Code
- BBR
Black Belt Rural
- ACOG
American College of Obstetricians and Gynecologists
- SES
Socioeconomic Status
- AJCC
American Joint Committee on Cancer
Footnotes
Declaration of Interests: CAL serves on an advisory board for Genentech/Roche and previously served on an advisory board for Celsion and Mateon Therapeutics. There are no other conflicts of interest to disclose.
IRB Status: This work was approved by the University of Alabama at Birmingham Institutional Review Board (Protocol # X160802010).
References
- [1].Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2006;24:2137–50. [DOI] [PubMed] [Google Scholar]
- [2].Collins Y, Holcomb K, Chapman-Davis E, Khabele D, Farley JH. Gynecologic cancer disparities: a report from the Health Disparities Taskforce of the Society of Gynecologic Oncology. Gynecol Oncol. 2014;133:353–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA: a cancer journal for clinicians. 2016;66:7–30. [DOI] [PubMed] [Google Scholar]
- [4].Noone AMHN, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA. SEER Cancer Statistics Review, 1975–2015. National Cancer Institute; Bethesda, MD: 2018. [Google Scholar]
- [5].National Institue of Health National Cancer Institute. Distribution of cervix uteri cancer diagnoses by stage at diagnosis, 1980–2013. NIH National Cancer Institute Cancer Trends Progress Report. [Google Scholar]
- [6].Institute of Medicine Committee on U, Eliminating R, Ethnic Disparities in Health C In: Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US) Copyright 2002 by the National Academy of Sciences. All rights reserved.; 2003. [PubMed] [Google Scholar]
- [7].Benard VB, Lawson HW, Eheman CR, Anderson C, Helsel W. Adherence to guidelines for follow-up of low-grade cytologic abnormalities among medically underserved women. Obstet Gynecol. 2005;105:1323–8. [DOI] [PubMed] [Google Scholar]
- [8].Niccolai LM, Mehta NR, Hadler JL. Racial/Ethnic and poverty disparities in human papillomavirus vaccination completion. American journal of preventive medicine. 2011;41:428–33. [DOI] [PubMed] [Google Scholar]
- [9].Widdice LE, Bernstein DI, Leonard AC, Marsolo KA, Kahn JA. Adherence to the HPV vaccine dosing intervals and factors associated with completion of 3 doses. Pediatrics. 2011;127:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Leath CA 3rd, Straughn JM Jr., Kirby TO, Huggins A, Partridge EE, Parham GP. Predictors of outcomes for women with cervical carcinoma. Gynecol Oncol. 2005;99:432–6. [DOI] [PubMed] [Google Scholar]
- [11].Barrington DA, Dilley SE, Landers EE, Thomas ED, Boone JD, Straughn JM Jr., et al. Distance from a Comprehensive Cancer Center: A proxy for poor cervical cancer outcomes? Gynecol Oncol. 2016;143:617–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Harlan LC, Greene AL, Clegg LX, Mooney M, Stevens JL, Brown ML. Insurance status and the use of guideline therapy in the treatment of selected cancers. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2005;23:9079–88. [DOI] [PubMed] [Google Scholar]
- [13].Beavis AL, Gravitt PE, Rositch AF. Hysterectomy-corrected cervical cancer mortality rates reveal a larger racial disparity in the United States. Cancer. 2017;123:1044–50. [DOI] [PubMed] [Google Scholar]
- [14].McDonald YJ, Goldberg DW, Scarinci IC, Castle PE, Cuzick J, Robertson M, et al. Health Service Accessibility and Risk in Cervical Cancer Prevention: Comparing Rural Versus Nonrural Residence in New Mexico. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ramondetta LM, Meyer LA, Schmeler KM, Daheri ME, Gallegos J, Scheurer M, et al. Avoidable tragedies: Disparities in healthcare access among medically underserved women diagnosed with cervical cancer. Gynecol Oncol. 2015;139:500–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Horner MJ, Altekruse SF, Zou Z, Wideroff L, Katki HA, Stinchcomb DG. U.S. geographic distribution of prevaccine era cervical cancer screening, incidence, stage, and mortality. Cancer Epidemiol Biomarkers Prev. 2011;20:591–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Yoo W, Kim S, Huh WK, Dilley S, Coughlin SS, Partridge EE, et al. Recent trends in racial and regional disparities in cervical cancer incidence and mortality in United States. PLoS One. 2017;12:e0172548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].United States Department of Agriculture Economic Research Service. Rural-Urban Commuting Area Codes. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/: United States Department of Agriculture Economic Research Service; 2016. [Google Scholar]
- [19].Rogers WWWR, Atkins LR, Flynt W. Alabama: The History of a Deep South State: University of Alabama Press; 1994. [Google Scholar]
- [20].Shuaib F, Foushee HR, Ehiri J, Bagchi S, Baumann A, Kohler C. Smoking, sociodemographic determinants, and stress in the Alabama Black Belt. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association. 2011;27:50–9. [DOI] [PubMed] [Google Scholar]
- [21].Patel A, Knox RJ, Logan A, Summerville K. Area Health Education Center (AHEC) programs for rural and underrepresented minority students in the Alabama Black Belt. Archives of public health = Archives belges de sante publique. 2017;75:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Gyawu R, Quansah JE, Fall S, Gichuhi PN, Bovell-Benjamin AC. Community food environment measures in the Alabama Black Belt: Implications for cancer risk reduction. Preventive medicine reports. 2015;2:689–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Alabama Maps. Center for Business and Economic Research, The University of Alabama Culverhouse College of Commerce and Business Administration. https://cber.cba.ua.edu/edata/maps/AlabamaMaps1.html. [Google Scholar]
- [24].DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, et al. Cancer statistics for African Americans, 2016: Progress and opportunities in reducing racial disparities. CA: a cancer journal for clinicians. 2016;66:290–308. [DOI] [PubMed] [Google Scholar]
- [25].Gunderson CC, Nugent EK, McMeekin DS, Moore KN. Distance traveled for treatment of cervical cancer: who travels the farthest, and does it impact outcome? International journal of gynecological cancer : official journal of the International Gynecological Cancer Society. 2013;23:1099–103. [DOI] [PubMed] [Google Scholar]
- [26].Temkin SM, Fleming SA, Amrane S, Schluterman N, Terplan M. Geographic disparities amongst patients with gynecologic malignancies at an urban NCI-designated cancer center. Gynecol Oncol. 2015;137:497–502. [DOI] [PubMed] [Google Scholar]
- [27].Rositch AF, Nowak RG, Gravitt PE. Increased age and race-specific incidence of cervical cancer after correction for hysterectomy prevalence in the United States from 2000 to 2009. Cancer. 2014;120:2032–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Robinson CL. Advisory Committee on Immunization Practices Recommended Immunization Schedules for Persons Aged 0 Through 18 Years--United States, 2016. MMWR Morbidity and mortality weekly report. 2016;65:86–7. [DOI] [PubMed] [Google Scholar]
- [29].Datta NR, Stutz E, Liu M, Rogers S, Klingbiel D, Siebenhuner A, et al. Concurrent chemoradiotherapy vs. radiotherapy alone in locally advanced cervix cancer: A systematic review and meta-analysis. Gynecol Oncol. 2017;145:374–85. [DOI] [PubMed] [Google Scholar]
- [30].Deshmukh SK, Azim S, Ahmad A, Zubair H, Tyagi N, Srivastava SK, et al. Biological basis of cancer health disparities: resources and challenges for research. American journal of cancer research. 2017;7:1–12. [PMC free article] [PubMed] [Google Scholar]
- [31].Vidal AC, Smith JS, Valea F, Bentley R, Gradison M, Yarnall KS, et al. HPV genotypes and cervical intraepithelial neoplasia in a multiethnic cohort in the southeastern USA. Cancer causes & control : CCC. 2014;25:1055–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].del Carmen MG, Montz FJ, Bristow RE, Bovicelli A, Cornelison T, Trimble E. Ethnic differences in patterns of care of stage 1A(1) and stage 1A(2) cervical cancer: a SEER database study. Gynecol Oncol. 1999;75:113–7. [DOI] [PubMed] [Google Scholar]
- [33].Goss E, Lopez AM, Brown CL, Wollins DS, Brawley OW, Raghavan D. American society of clinical oncology policy statement: disparities in cancer care. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2009;27:2881–5. [DOI] [PubMed] [Google Scholar]


