Abstract
Background
Dysfunction of the lower urinary tract is the most common complication of radical hysterectomy (RH). However, there are no established treatment protocols for postoperative underactive bladder (PUB). We developed our own new program for the treatment of underactive bladder (UB) after RH and evaluated it retrospectively.
Methods
In this program, there are five steps for patients to follow according to their urinary condition. The first step is the administration of urapidil 30 mg, voiding six times at a predetermined time each day, and clean intermittent catheterization (CIC) after each voiding. As the patient’s condition improves, the number of CICs is reduced, and the medication is stopped. The last step includes voiding six times at a predetermined time each day. When the volume of residual urine (RU) is less than 100 mL, patients move on to the next step. When the volume of RU exceeds 100 mL, patients return to the previous step.
Results
Of the 75 patients who visited our department, 41 were eligible for this program. Twenty-two patients visited our department because of urinary retention (UR), and 19 patients were admitted because of increased RU. The mean RU volume was 276.3 mL (range, 150–550 mL). After completing the program, 39 (95.1%) patients no longer required CIC. The mean time to withdrawal of CIC was 25.1 weeks (range, 1–72 weeks). Thirty-six patients no longer required medical treatment, including urapidil, for PUB. Of the 5 patients who had persistent PUB after treatment, 2 patients continued CIC and urapidil, and three patients continued urapidil alone.
Conclusion
The present results demonstrate that the program of CIC in combination with urapidil is effective for the management of PUB after RH.
Keywords: Clean intermittent catheterization, radical hysterectomy, underactive bladder
Underactive bladder (UB) is a clinical entity often encountered by urologists and is often associated with significant lower urinary tract symptoms. The International Continence Society has defined detrusor underactivity as “a contraction of reduced strength and/or duration, resulting in prolonged bladder emptying and/or failure to achieve complete bladder emptying within a normal time span.”1
During surgery, the nerves involved in urinary function are sometimes injured.2 In particular, surgery involving the uterus can result in postoperative underactive bladder (PUB).3 Surgeries for malignant tumors require complete resection of the tumor and sometimes require the sacrifice of some surrounding nerves. The greater the surgical stress, the more extensive is the nerve damage, sometimes resulting in severe urinary dysfunction, such as PUB, and rectal disorders.3 In recent years, nerve-sparing surgical techniques have been developed.4 In PUB, the attenuation of micturition after catheter removal is usually recognized by the disappearance of urinary sensation and lower abdominal distention. Detrusor muscle contraction in PUB reduces dysuria or urinary retention (UR). Because the effect of drug therapies is limited, some patients require clean intermittent catheterization (CIC) to facilitate bladder emptying.3
Dysfunction of the lower urinary tract is the most common complication of radical hysterectomy (RH). However, there is no established treatment protocol for PUB. Therefore, we created our own program for PUB after RH. We formulated this program so that it can be safely followed at the generalist’s level without referral to the urologist. The final goal of this program was withdrawal from CIC and pharmacological treatment with alpha-blockers. This program was evaluated retrospectively.
MATERIALS AND METHODS
Ethics
This study was conducted at the Division of Urology, Tottori University Hospital, Tottori, Japan. The study was approved by the Tottori University Ethics Committee (no. 17A100).
Patients
Female patients who underwent RH for endometrial and cervical uterine cancer between January 2010 and April 2015 at our department were included in the study. Patients were excluded if they had active urinary tract infections (UTIs) and/or preoperative neurogenic bladder. All patients were referred to our treatment program after a diagnosis of PUB.
Program for PUB
The program involved five steps. The first step included the administration of urapidil 30 mg, voiding six times at a predetermined time each day, and CIC after each voiding. The second step involved the administration of urapidil 30 mg, voiding six times at a predetermined time each day, and CIC three times per day after voiding. The third step involved the administration of urapidil 30 mg, voiding six times at a predetermined time each day, and CIC once per day after voiding. The fourth step involved treatment with urapidil 30 mg and voiding six times at a predetermined time each day. From the fourth step to the last step, residual urine was measured at the outpatient clinic visit for the prescription of oral urapidil, and the amount of residual urine was the key factor: when patients’ residual urine became less than 100 mL, they stopped urapidil. The last step involved voiding six times at a predetermined time each day. When the volume of residual urine was less than 100 mL, patients were asked to move on to the next step. When the volume of residual urine exceeded 100 mL, patients were asked to return to the previous step (Fig. 1).
Fig. 1.

Program for postoperative underactive bladder. The first step is taking urapidil 30 mg, voiding six times per day, and CIC after each voiding. The last step is voiding six times per day. If the volume of residual urine is over 100 mL, patients return to the previous step. CIC, clean intermittent catheterization
RESULTS
Of the 75 patients who visited our department during the study period, 41 were eligible for this program. All patients reported reduced bladder sensation and required urethral catheterization or CIC because of UR or increased residual urine (RU). The mean patient age was 48.3 years (range, 31–71 years). Thirty-nine patients were diagnosed with cervical cancer (stage I: 21 patients, stage II: 18 patients), and two had endometrial uterine cancer. All patients underwent RH and pelvic lymph node dissection, with or without ovariectomy. None of the patients underwent nerve-sparing surgery. The mean number of postoperative days to urethral catheter removal was 7.4 days (range, 6-16 days). Twenty-two patients visited our department because of UR, and 19 patients were admitted because of increased RU. The mean RU volume was 276.3 mL (range, 150–550 mL). Thirty-six patients started Step 1. Five patients could not use urapidil because of low blood pressure, so they started the program with voiding six times per day and CIC after each voiding (Table 1).
Table 1.
Patients’ characteristics
| N = 41 | ||
| Age, y (range) | 48.3 (31–72) | |
| Cervical cancer | Stage Ib | 2 |
| Endometrial cancer | Stage Ib1 | 16 |
| Stage Ib2 | 5 | |
| Stage IIa | 3 | |
| Stage IIb | 15 | |
| Time to removal of urethral catheter, days (range) | 7.4 (6–16) | |
| Initial treatment | CIC + urapidil | 36 |
| CIC only | 5 | |
| Urinary dysfunction | Urinary retention | 22 |
| Increased residual urine | 19 | |
| Mean residual urine volume, mL (range) | 276.3 (50–550) | |
CIC, clean intermittent catheterization; y, years.
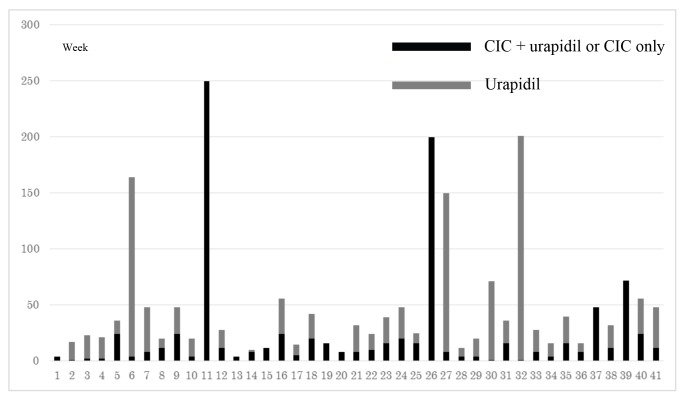
After completing the program, 39 (95.1%) patients no longer required CIC after voiding. The mean time to withdrawal of CIC was 25.1 weeks (range, 1–72 weeks). Thirty-six patients no longer required medical treatment, including urapidil, after this program. Five patients required ongoing medical treatment for PUB; two patients continued CIC and urapidil, and three continued urapidil alone (Fig. 2, Table 2).
Fig. 2.
Results of the postoperative underactive bladder treatment program. The number of patients who did not require CIC after this program is 39 (95.1%). The mean time to withdrawal of CIC is 25.1 (range, 1–72) weeks. Among the five patients continuing medical treatment for postoperative underactive bladder, two patients continued CIC and urapidil, and three patients continued urapidil. CIC, clean intermittent catheterization.
Table 2.
Patients who required continuing medical treatment for postoperative underactive bladder
| No. in Fig. 2 | Age (y) | UR or RU | US | DMC | Withdrawal of CIC |
| 6 | 45 | UR | No | Acontractile | Yes |
| 7 | 35 | UR | No | Acontractile | Yes |
| 11 | 32 | UR | No | Acontractile | No |
| 26 | 40 | RU | Yes | Very weak | No |
| 27 | 48 | UR | No | Very weak | Yes |
CIC, clean intermittent catheterization; DMC, detrusor muscle contraction; RU, residual urine; UR, urinary retention; US, urinary sensation; y, years.
Adverse events of this program included UTIs. Acute cystitis occurred in four patients, and acute pyelonephritis developed in one patient who subsequently required hospitalization.
DISCUSSION
The pelvic nerve plexus has visceral terminal branches that innervate the bladder. Pelvic surgery, such as RH, can cause nerve injury and lead to PUB. RH is the most common surgical treatment for uterine cervical cancer and stage II uterine endometrial cancer. After RH, it has been reported that the overall incidence of detrusor dysfunction is 8-80%.3 Sensory loss and voiding disorders are the primary conditions. Thus, some patients require urethral catheterization or CIC. For patients with UB, clinicians should consider restoring optimal bladder function and emptying. Currently, the most important treatment for UB is mechanical bladder emptying, such as CIC. Patients with an acontractile detrusor muscle void by increasing abdominal pressure, but some RU usually remains. Patients who exert high abdominal pressures while voiding may trigger a vesicoureteral reflex and develop upper urinary tract dysfunction. CIC defers the progression of upper urinary tract damage, avoids bladder overdistention, and reduces RU.2
Generally, early transient postoperative changes consist of reduced bladder capacity, detrusor underactivity, and diminished bladder sensation, which cause voiding dysfunction and may require urethral catheterization or CIC. Late changes include emptying difficulties, irritable symptoms of frequency, urgency, and urge incontinence, and reduced bladder capacity for 6-12 months or longer.5 The purpose of this program is not to shorten the treatment period, but to restore bladder function in a period equivalent to treatment without a specialist. All patients should be referred to a urologist, but this is sometimes difficult. The present study evaluated the program we developed, whose aim is to be able to do the proper treatment without the urologist.
In this program, the voiding frequency was set at six times per day because it has been traditionally suggested that the ideal or optimal frequency of CIC was every 4–6 h, with goal residual volumes of less than 500 mL.6
The pharmacological treatment of UB is limited. Muscarinic receptor agonists can sometimes be used for UB. However, six randomized trials found no significant improvement in voided volume, RU, and flow rate compared with placebo or no treatment. On the other hand, even though the level of evidence was low, alpha-blockers may constitute an acceptable first-line therapy for patients with UB7; therefore, urapidil was chosen for our program. If possible, all patients were considered for urapidil, but some of the patients could not take urapidil due to low blood pressure. There was a possibility of early recovery, but because the number in this study was small, it was difficult to compare patients who did or did not use urapidil. Therefore, it was not possible to determine if urapidil was really necessary.
In the present study, although some of the patients’ RU volumes were small, the mean time to withdrawal of CIC was 25.1 (range, 1–72) weeks. Generally, acute voiding symptoms disappear within 6–12 months after RH.5 The results of the present study suggest that bladder function recovers after approximately 6 months. However, pressure flow studies (PFS) were not performed in all cases. Therefore, it was unclear whether bladder function was actually restored.
As for cases of difficulty in withdrawal of CIC, previous reports have suggested that bladder function was delayed after postoperative radiotherapy.8 In the present study, two patients required continuing CIC. The characteristics of patients who needed to continue treatment were unknown. Surgical technique and radiation therapy were also not involved. In the future, if the number of cases increases, it may be possible to determine the characteristics of patients who fail to recover fully. This is a limitation of this study.
These patients eventually achieved self-voiding but required continuing CIC because of increased RU. The reason for these results is unknown, but these patients may have sustained extensive nerve injuries intraoperatively.
The most common complication of CIC is UTI.9 Since there was only one case of severe UTI during the study, our patient education program when patients started CIC, run by the nursing staff, was considered effective.10 In this regard, we consider that our program can be operated relatively safely.
One limitation of this study is its small number of patients, but the program is still ongoing and gradually accumulating more cases. Another limitation is the issue of long-term follow-up. Some patients discontinued follow-up. Additionally, PFS was not performed after withdrawal of CIC in all patients. The recovery of bladder function was evaluated in all patients, irrespective of whether they voided using increased abdominal pressure.
In the present study, 22 patients had UR, but only two needed continuing CIC after completing this program, indicating its usefulness in such patients. The completion of each step was decided only by the RU volume, a concept that can be easily understood and determined by the patients themselves during CIC. By educating each patient about each step in advance, the patient can make any adjustments as necessary. The implementation of this program was done without much difficulty with respect to the patients’ participation or the nurses’ and doctors’ contributions.
The present results demonstrate that the program of CIC in combination with urapidil is effective for the management of PUB after RH.
The authors declare no conflict of interest.
REFERENCES
- 1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardization of terminology of lower urinary tract function: report from the Standardisation Sub-Committee of International Continence Society. Neurourol Urodyn. 2002;21:167-78. [DOI] [PubMed] [Google Scholar]
- 2. Li X, Liao L. Updates of underactive bladder: a review of the recent literature. Int Urol Nephrol. 2016;48:919-30. [DOI] [PubMed] [Google Scholar]
- 3. Laterza RM, Sievert KD, de Ridder D, Vierhout ME, Haab F, Cardozo L, et al. Bladder function after radical hysterectomy for cervical cancer. Neurourol Urodyn. 2015;34:309-15. [DOI] [PubMed] [Google Scholar]
- 4. Wu J, Liu X, Hua K, Hu C, Chen X, Lu X, et al. Effect of neve-sparing radical hysterectomy on bladder function recovery and quality of life in patients with cervical carcinoma. Int J Gynecol Cancer. 2010;20:905-9. [DOI] [PubMed] [Google Scholar]
- 5. Chen GD, Lin LY, Wang PH, Lee HS. Urinary tract dysfunction after radical hysterectomy for cervical cancer. Gynecol Oncol. 2002;85:292-7. [DOI] [PubMed] [Google Scholar]
- 6. Aggarwal H, Zimmern PE. Underactive Bladder. Curr Urol Rep. 2016;17:17. [DOI] [PubMed] [Google Scholar]
- 7. Chang SJ, Chiang IN, Yu HJ. The effectiveness of tamsulosin in treating women with voiding difficulty. Int J Urol. 2008;15:981-5. [DOI] [PubMed] [Google Scholar]
- 8. Lin HH, Sheu BC, Lo MC, Huang SC. Abnormal urodynamic findings after radical hysterectomy or pelvic irradiation for cervical cancer. Int J Gynaecol Obstet. 1998;63:169-74. [DOI] [PubMed] [Google Scholar]
- 9. Wyndaele JJ, Brauner A, Geerlings SE, Bela K, Peter T, Bjerklund-Johanson TE. Clean intermittent catheterization and urinary tract infection: review and guide for future research. BJU Int. 2012;110(11 Pt C):E910-7. [DOI] [PubMed] [Google Scholar]
- 10. Oh SJ, Ku JH, Lim SH, Jeon HG, Son H. Effect of a “centralized intensive education system” for clean intermittent self-catheterization in patients with voiding dysfunction who start catheterization for the first time. Int J Urol. 2006;13:905-9. [DOI] [PubMed] [Google Scholar]