Abstract
Depression is common in patients with irritable bowel syndrome (IBS), but the reported prevalence across different studies is inconsistent. This meta-analysis systematically examined the presence and severity of depressive symptoms in patients with IBS. Two investigators independently performed a literature search. The pooled depressive symptom severity was calculated using a random effects model. Subgroup, sensitivity and meta-regression analyses were conducted to examine the moderating factors of the development of depressive symptoms. Twenty four studies (n=2,837) comparing depressive symptoms between IBS patients (n=1,775) and healthy controls (n=1,062) were identified; 14 (58.3%) studies were rated as high quality. Compared to healthy controls, IBS patients had more frequent (OR=9.21, 95%CI: 4.56-18.57, P<0.001; I2=76%) and more severe depressive symptoms (n=1,480, SMD=2.02, 95%CI: 1.56-2.48, P<0.001; I2=94%). Subgroup analyses revealed that patients with all IBS subtypes had more severe depressive symptoms than controls. In addition, versions of the Hamilton Depression Rating Scale (HAM-D) and IBS diagnostic criteria were significantly associated with depressive symptom severity. Meta-regression analyses revealed that female gender, younger age and small sample size were significantly associated with more severe depressive symptoms. In conclusion, meta-analytic data showed that IBS patients had more frequent and severe depressive symptoms than healthy controls. Adequate screening and treatment for depression should be developed and implemented in this patient population.
Keywords: IBS, depressive symptoms, controlled studies, meta-analysis
Introduction
Irritable bowel syndrome (IBS) is one of the most common functional gastrointestinal (GI) diseases with the prevalence of around 20% in the general population 1-3. The Rome diagnostic criteria are the diagnostic standard for research and clinical care of IBS 4, 5. According to the predominant stool pattern, IBS is traditionally classified into four subtypes; IBS with constipation (IBS-C), IBS with diarrhea (IBS-D), mixed IBS (IBS-M) and non-subtyped IBS (IBS-U) 6. Typical symptoms of IBS include recurrent abdominal pain, bloating, change in bowel habits without detectable structural or biochemical abnormalities 7. IBS is associated with poor quality of life, impaired social functions 8, 9 and psychological-psychiatric conditions, such as depression 10; approximately 20-40% of IBS patients present with depressive symptoms 11, 12.
The close association between IBS and depression is supported by psychophysiological and neuro-imaging studies 13, 14, and this association might be related to the 'brain-gut axis' that is defined as the bidirectional connecting system through neural, neuroimmune and neuroendocrine pathways between the digestive system and the brain 15. Psychosocial factors can affect the gut physiology via the brain-gut axis in IBS 10, 16. Antidepressants are effective to some extent in treating IBS directly through the brain-gut axis independent of changes in depressive symptoms 17, 18.
The relationship between IBS and depression has not been consistent across studies. IBS has been associated with more severe depressive symptoms compared to healthy controls in some 19-22, but not all 23, 24 studies. Additionally, the association between IBS subtype and depressive symptoms is also uncertain with studies finding either an association with IBS-C 25 or IBS-D 26, 27 but not with other subtypes 25, or not at all28, 29.
Two meta-analyses 27, 30 concluded that IBS patients had more severe depressive symptoms than healthy controls, but the association between IBS subtypes and depressive symptoms was inconsistent. These studies only covered English databases and the included studies employed self-reported scales on depressive symptoms, such as the Hospitalization Anxiety and Depression Scale (HADS) and the Beck Depression Inventory (BDI). As the reliability of self-reported scales are affected by impaired insight and cognitive functions that are common in depression, investigator-rated tools, such as the Hamilton Depression Rating Scale (HAMD) 31, 32 are generally thought to be more objective and suitable for research purposes.
To the best of our knowledge, no meta-analysis or systemic review on depressive symptoms in IBS using interviewer-rated tools have been published. Thus, the aim of this study was to conduct a systematic meta-analysis to compare objectively rated depressive symptoms between IBS patients and healthy controls, and examine the association between IBS subtypes and depressive symptoms.
Methods
Search strategy
The meta-analysis was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines 33. Two authors (ZQE and WF) independently performed a literature search using both English (PubMed, PsycINFO, Embase, Cochrane Library) and Chinese (Wan Fang, SinoMed and Chinese National Knowledge Infrastructure (CNKI)) databases, from their inception to September 12, 2017 with the following search terms: ("irritable bowel syndrome" OR "colon diseases, functional" OR "functional bowel diseases" OR "IBS") AND ("depressive" OR "depression" OR "melancholia"). Furthermore, the references of included studies, meta-analyses and review papers were manually searched 27, 30, 34 to identify additional relevant studies.
Selection criteria
The search results were imported into the EndNote X7 software (Thomson Reuters, Philadelphia, PA, USA). The inclusion criteria were based on the PICOS acronym: Participants (P): Patients with IBS according to any diagnostic criteria. Intervention (I): not applicable. Comparison (C): healthy controls. Outcomes (O): depressive symptoms assessed with validated interviewer-rated scales. To assess depressive symptoms more objectively, only studies using investigator-rated scales were included. Study design (S): published case-control, cohort (only baseline data were included) and cross-sectional studies. Studies were excluded if they (1) made no comparisons between patients with IBS/IBS subtype and healthy controls; (2) did not provide meta-analyzable data on depressive symptoms. If more than one publication were published based on the same dataset, only publications with complete data were included.
Data extraction
Two reviewers (ZQE and WF) independently checked and extracted data from the studies using a pre-defined electronic Excel form: first author, year of publication, country, study design, IBS diagnostic criteria, and the assessment tools and means and standard deviations (SDs) of depressive symptoms. The first or corresponding authors were contacted for more information if relevant data were incomplete. Extracted data were analyzed independently by two reviewers (ZQE and QG). Any controversy was resolved by consensus or with the involvement of a third reviewer (WZ).
Statistical analysis
Data analyses were performed using the Review Manager Version 5.3 software (http://www.cochrane.org) and the Comprehensive Meta Analysis, Version 2.2.064 (http://www.Meta-Analysis.com), according to the recommendation of the Cochrane Handbook for Systematic Reviews 35. Due to the unavoidable heterogeneity in study characteristics, the random effects model was used to synthesize the data. Heterogeneity was examined by the I2 and Q statistics. Significant heterogeneity was considered when I2 values were of >50% or P<0.1 in the Q statistics 36, 37. For continuous and dichotomous outcomes SMDs and odds ratios (OR), respectively were calculated to evaluate the results' effect size (ES). ES values over 0.8, 0.5-0.8 and 0.2-0.5 constituted large, medium and small effect sizes, respectively 38. Subgroup and sensitivity analyses were conducted to explore potential sources of heterogeneity. Subgroup analyses were performed according to the following variables: 1) subtypes: IBS-C vs. IBS-D vs. IBS-M vs. IBS-U; 2) Chinese studies vs. non-Chinese studies; 3) IBS diagnostic criteria: Rome I vs. Rome II vs. Rome III; 4) treatment settings: inpatients vs. outpatients vs. mixed; 5) HAMD versions: HAMD-17 vs. HAMD-24 vs. HAMD-not reported (NR); 6) refractory vs. non-refractory IBS. Random effects meta-regression was used to evaluate the impact of continuous moderating variables, such as age, proportion of females, sample size and the Newcastle-Ottawa Scale (NOS) scores with the primary outcome 39. Potential publication bias was assessed with the funnel plots and Egger's regression test 40, 41.
Assessment of study quality
Two reviewers (ZQE and WF) independently evaluated the methodological quality of each study using the NOS 42, 43, which has a score ranging from 0 to 9 points. The total NOS score of ≥7 points were rated as high quality 44, 45.
Results
Literature search
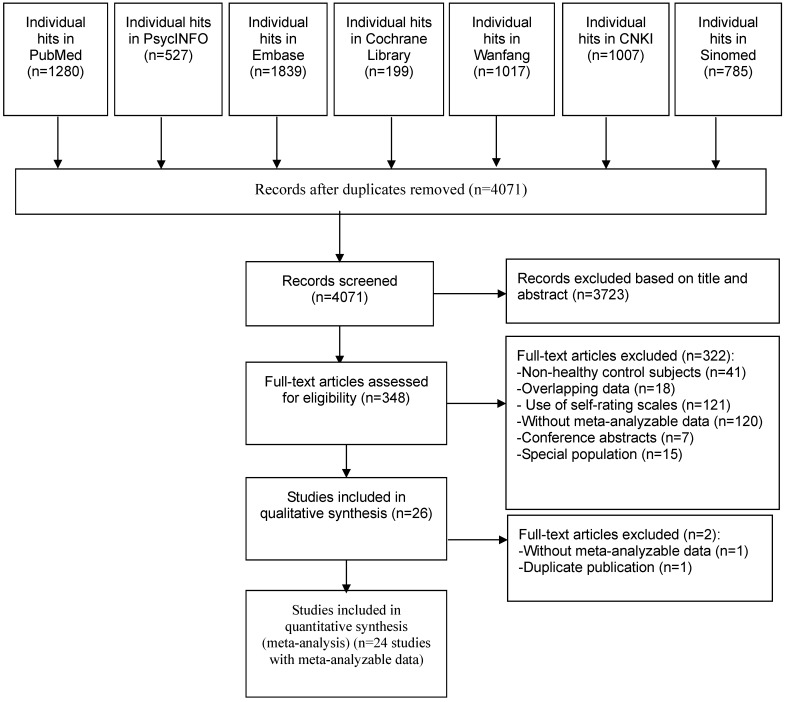
Out of 6,654 studies, 4,071 were identified after duplicate publications were removed. Eventually, 24 studies met full criteria and were included in the meta-analysis. The screening process according to the PRISMA flow diagram is presented in Figure 1. One study 46 reported data on both refractory and non-refractory IBS patients separately, therefore the data were extracted and analyzed as two separate arms. In order to avoid inflating the sample size in the control group, half numbers of healthy controls were assigned to each arm in the analyses.
Figure 1.
PRISMA flow diagram
Study characteristics
There were 2,837 subjects (1,775 IBS patients and 1,062 healthy controls) in the 24 studies (Table 1). Twenty studies were conducted in China (n=2,620) 46-65, and one each in Serbia (n=60) 66, The Netherlands (n=46) 67, United Kingdom (n=29) 68 and Turkey (n=76) 69. IBS was diagnosed using the Rome I criteria in one 69, Rome II criteria in 10 50, 56, 58-60, 62, 65-68, and Rome III criteria in 13 studies 46-49, 51-55, 57, 61, 63, 64. The severity of depressive symptoms was assessed using the Hamilton Depression Rating Scale (HAMD-17) in 5 studies 46, 61, 65, 67, 69 and HAMD-24 in 9 studies 50-53, 55, 57, 60, 63, 64, but HAMD versions that were not reported (HAMD-NR) in 10 studies 47-49, 54, 56, 58, 59, 62, 66, 68. One study included female subjects only 56. The mean age ranged from 32.9 to 63.7 years, and the proportion of males ranged from 0% to 69.6% in the patient group.
Table 1.
Characteristics of the studies included in the meta-analysis
| Authors | Country | N | Design, n (IBS/control) |
Assessment scales on depressive symptoms | Patients with IBS | Healthy controls | NOS scores |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IBS diagnostic criteria | Subject type | Mean age (yrs) | Male (%) | Subject type | Mean age (yrs) | Male (%) | ||||||
| Akkus et al, 2004 | Turkey | 82 | Case control, 32/50 |
HAMD-17 | Rome I | Outpatients | 44.8 | 59.4 | Hospital staff; Healthy volunteers |
47.6 | 44.0 | 7 |
| Chen and Wang et al, 2007 | China | 60 | Case control, 30/30 |
HAMD | Rome II | Inpatients; Outpatients |
NR | 40.0 | Health examination population; Healthy volunteers | NR | 43.3 | 8 |
| Chen and Zou et al, 2007 | China | 54 | Case control, 27/27 |
HAMD-24 | Rome II | Outpatients | 40.3 | 44.4 | Health examination population | 37 | 48.2 | 6 |
| Gonçalves de Medeiros et al, 2012 | United Kingdom | 27 | RCT, 21/8 |
HAMD | Rome II | Outpatients | 39.9 | 23.8 | Healthy volunteers | 32.3 | 75.0 | 6 |
| Hao et al, 2015 | China | 50 | Case control, 30/20 |
HAMD | Rome III | Inpatients | 38C | 53.3 | Health examination population | 42C | 55.0 | 8 |
| Jin et al, 2004 | China | 58 | RCT, 36/22 |
HAMD-17 | Rome II | Inpatients; Outpatients |
42.7 | 44.4 | Health examination population | 41.1 | 59.1 | 5 |
| Kilkens et al, 2013 | Netherlands | 46 | Case control, 23/23 | HAMD-17 | Rome II | Outpatients | 32.9 | 39.1 | Healthy volunteers | 28.6 | 39.1 | 8 |
| Li and Chen et al, 2015 | China | 140 | Case control, 70/70 | HAMD-24 | Rome III | Outpatients | 51.0 | 48.6 | Health examination population | 49 | 50.0 | 7 |
| Li et al, 2015 | China | 64 | Case control, 32/32 | HAMD-24 | Rome III | Inpatients; Outpatients |
40.8 | 34.4 | Health examination population; Healthy volunteers | 39 | 31.3 | 8 |
| Liu et al, 2013 | China | 801 | Cross-sectional, 601/100 | HAMD-17 | Rome III | Outpatient | 38.3 | 49.5 | Health examination population | 39.7 | 45.0 | 7 |
| Mao et al, 2010 | China | 96 | Case control, 56/40 | HAMD | Rome III | Inpatients | 35.2 | 32.1 | Health examination population | 32.2 | 35.0 | 6 |
| Mu et al, 2003 | China | 60 | Case control, 30/30 | HAMD | Rome II | Outpatients | NR | 33.3 | Hospital staff | NR | 40.0 | 5 |
| Shi et al, 2012 | China | 90 | Case control, 60/30 |
HAMD-24 | Rome III | Inpatients; Outpatients |
NR | 30.0 | Health examination population | NR | 66.7 | 8 |
| Shi and Zhang et al, 2012 | China | 57 | Case control, 32/25 | HAMD-17 | Rome III | Outpatients | 40.0 | 40.6 | NR | 39.2 | 56.0 | 6 |
| Song et al, 2015 | China | 204 | Case control, 102/102 | HAMD-24 | Rome III | Outpatients | 48.1 | 38.2 | Health examination population | 42.3 | 42.2 | 7 |
| Tian et al, 2011 | China | 30 | Case control, 20/10 | HAMD | Rome III | NR | 45C | 55.0 | Health examination population | 42C | 60.0 | 7 |
| Tosic-Golubovic et al, 2010 | Serbia | 60 | Case control, 30/30 | HAMD | Rome II | Outpatients | 43.9 | 50.0 | Community | 41.6 | 50.0 | 8 |
| Wan et al, 2005 | China | 50 | Case control, 30/20 | HAMD | Rome II | Outpatients | 37.0 | 0 | Hospital staff; Patient's relative; Students | 38 | 0 | 6 |
| Wang et al, 2012 | China | 116 | Case control, 56/60 | HAMD-24 | Rome II | Inpatients; Outpatients |
NR | NR | Health examination population; Patient's relative | NR | NR | 6 |
| Wang et al, 2014 | China | 260 | Case control, 150/110 | HAMD | Rome III | NR | NR | 41.3 | Health examination population; Patient's relative | NR | NR | 8 |
| Xu et al, 2012 | China | 134 | Case control, 69/65 | HAMD-24 | Rome III | Inpatients; Outpatients |
NR | 42.0 | Hospital staff; Patient's relative | NR | 50.8 | 8 |
| Xu et al, 2014 | China | 215 | Case control, 112/103 | HAMD-24 | Rome III | Outpatients | 63.7 | 69.6 | Healthy volunteers | 56.3 | 57.3 | 5 |
| Xu et al, 2017 | China | 66 | Cross-sectional, 46/20 | HAMD-24 | Rome III | Outpatients | 34.2 | 49.1 | Healthy volunteers | 29.5 | 60.0 | 8 |
| Zhang et al, 2007 | China | 115 | Case control, 80/35 | HAMD | Rome II | NR | 20-73 | 55.0 | NR | 20-60 | 45.7 | 5 |
a Only data from IBS subjects and healthy control groups were extracted if there were multiple study arms.
b Rome I/II/III are standard criteria for diagnosis of IBS.
c median age.
HAMD=Hamilton Depression Rating Scale; IBS= irritable bowel syndrome; NR=not reported; NOS=Newcastle-Ottawa Scale; yrs=years; RCT=randomized controlled trial.
Quality assessment
The NOS score assessing quality of the studies ranged from 4 to 8 points (Supplemental Table 1); 58.3% of studies (n=14) 46, 48-50, 52-55, 57, 63, 64, 66, 67, 69 were assessed as “high quality” (NOS≥7).
Primary outcome
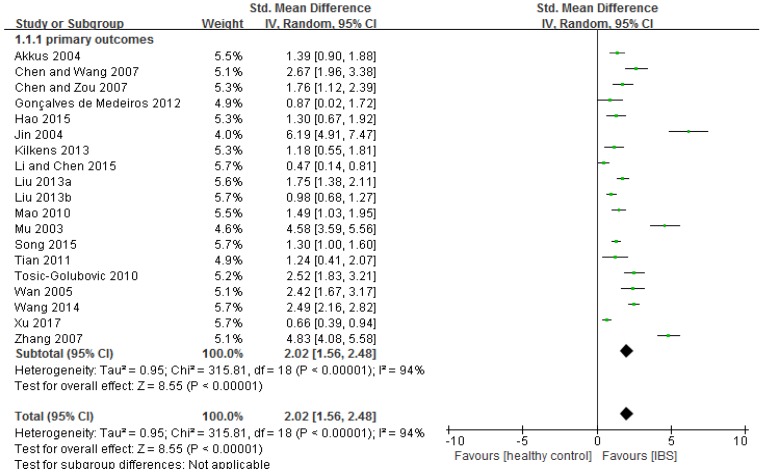
Compared to healthy controls, IBS patients had more severe depressive symptoms (n=1,480, SMD=2.02, 95%CI: 1.56-2.48, P<0.001; Figure 2). The funnel plot showed asymmetry, while Egger's regression test showed publication bias (P=0.005). Sensitivity analysis revealed that the significance in bias remained (n=1,334, SMD=1.51, 95%CI: 1.16-1.86, P<0.001) after excluding three outlying studies (i.e., SMD>3) 59, 62, 65. Subgroup analyses further revealed that the significance remained in all of the 18 subgroup analyses (Table 2; Supplemental figure 3). In addition, IBS diagnostic criteria (p=0.01) and HAMD versions (p=0.002) were significantly associated with more severe depressive symptoms compared with the control group (Table 2). In meta-regression analyses younger age (slope=-0.033, p<0.001), proportion of female gender (slope=0.021, p<0.001) and small sample size (slope=-0.002, p<0.001) were significantly associated with more severe depressive symptoms. NOS scores did not have significant impact on the primary outcome (slope =0.095, P=0.08).
Figure 2.
Depressive symptoms in IBS: forest plot of HAMD total scores
Table 2.
Subgroup analyses of moderating variables of the primary outcome
| subgroups | Study arms (subjects) | SMDs (95%CI) | I2 (%) | Pha | P-value for each subgroup | P-value across subgroups |
|---|---|---|---|---|---|---|
| Overall | 18 (1480) | 2.02 (1.56, 2.48) | 94 | <0.001 | <0.001 | NA |
| Subtypes | ||||||
| IBS-C | 6 (145) | 2.38 (1.10, 3.67) | 95 | <0.001 | 0.0003 | 0.81 |
| IBS-D | 7(253) | 2.08 (1.46, 2.70) | 86 | <0.001 | <0.001 | |
| IBS-M | 3(27) | 2.50 (1.86, 3.14) | 26 | 0.26 | <0.001 | |
| IBS-U | 2(33) | 2.21 (1.69, 2.72) | 0 | 0.66 | <0.001 | |
| Study setting | 0.12 | |||||
| China | 14 (1374) | 2.17 (1.62, 2.71) | 95 | <0.001 | <0.001 | |
| Other countriesb | 4 (106) | 1.50 (0.86, 2.15) | 74 | 0.008 | <0.001 | |
| IBS diagnosis criteria | 0.01 | |||||
| Rome I | 1 (32) | 1.39 (0.90, 1.88) | NA | NA | <0.001 | |
| Rome II | 9 (307) | 2.95 (1.95, 3.95) | 93 | <0.001 | <0.001 | |
| Rome III | 8 (1141) | 1.30 (0.85, 1.74) | 92 | <0.001 | <0.001 | |
| Patients | 0.15 | |||||
| Inpatients | 2 (86) | 1.42 (1.05, 1.79) | 0 | 0.62 | <0.001 | |
| Outpatients | 11 (1078) | 1.57 (1.14, 1.99) | 91 | <0.001 | <0.001 | |
| Mixed | 2 (66) | 4.39 (0.94, 7.84) | 95 | <0.001 | 0.01 | |
| NR | 3 (250) | 2.85 (1.16, 4.54) | 95 | <0.001 | 0.0009 | |
| HAM-D version | 0.002 | |||||
| HAMD-17 | 4 (692) | 2.06 (1.19, 2.94) | 94 | <0.001 | <0.001 | |
| HAMD-24 | 4 (311) | 1.00 (0.51, 1.49) | 87 | <0.001 | <0.001 | |
| NR | 10 (477) | 2.42 (1.74, 3.10) | 92 | <0.001 | <0.001 | |
| IBS severity | 0.11 | |||||
| Refractory IBS | 3 (208) | 3.43 (1.50, 5.36) | 96 | <0.001 | 0.0005 | |
| Non-refractory IBS | 16 (1272) | 1.80 (1.32, 2.27) | 94 | <0.001 | <0.001 |
a P-value of heterogeneity analysis.
b One study each in Turkey, Serbia, Netherlands, and in the United Kingdom.
NA=Not applicable; NR=Not reported; SMDs=Standard mean differences; IBS-C=Constipation-predominant Irritable Bowel Syndrome; IBS-D=Diarrhea-predominant irritable bowel syndrome; IBS-M=Mixed Irritable Bowel Syndrome; IBS-U=Un-subtyped Irritable Bowel Syndrome; Rome I/II/III=A standardize criteria for diagnosis of IBS; HAM-D=Hamilton Depression Rating Scale.
Secondary outcomes
The Hamilton Depression Rating Scale (HAM-D) contains six separate factors, namely factor I (anxiety/somatization), factor II (weight), factor III (cognitive disturbance), factor IV (diurnal variation), factor V (psychomotor retardation) and factor VI (sleep disturbances) 70-73. Compared to healthy controls, IBS patients had significantly higher scores in most HAM-D factors (SMD=4.03 to 13.54, 95%CI: 1.28-22.45, P<0.001; I2=41% to 99%, Supplemental Figure 2): anxiety/somatization (SMD=4.03), weight (SMD=4.78), psychomotor retardation (SMD=4.23) and sleep disturbances (SMD=13.54).
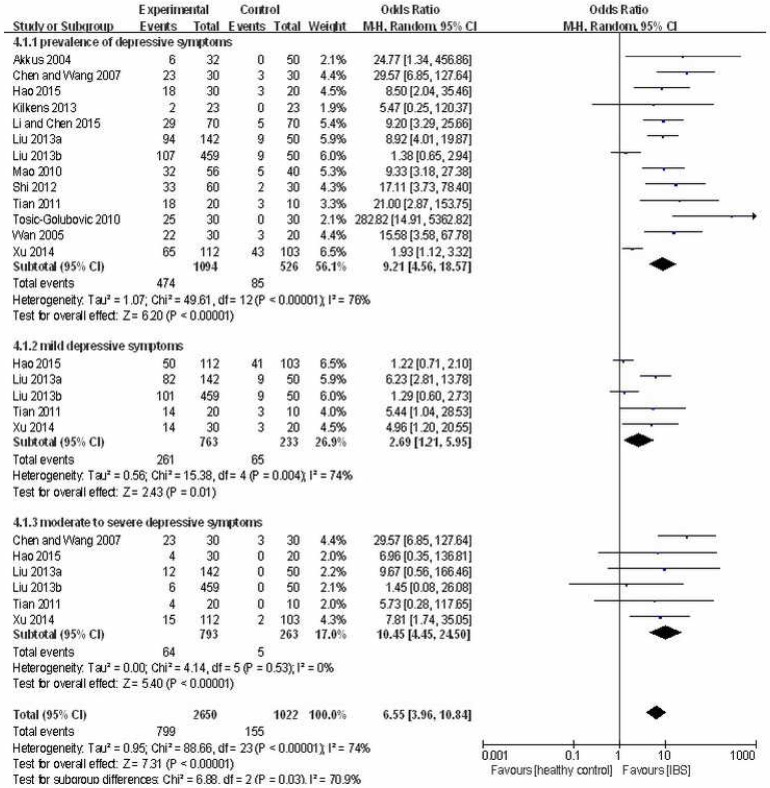
Prevalence of depressive symptoms (HAM-D total score > 7) in IBS patients was higher than in healthy controls (OR=9.21, 95%CI: 4.56-18.57, P<0.001; I2=76%, Figure 3). In addition, there was higher prevalence of mild depressive symptoms (HAM-D total score: 8-19) (OR=2.69, 95%CI: 1.21-5.95, P=0.01; I2=74%, Figure 3) as well as moderate to severe depressive symptoms (HAM-D total score ≥ 20) (OR=10.45, 95%CI: 4.45-24.50, P<0.001; I2=0%, Figure 3) in the IBS group than in the control group.
Figure 3.
Forest plot of the prevalence of depressive symptoms in IBS patients versus healthy controls
Discussion
This was the first meta-analysis on the frequency and severity of depressive symptoms measured by rater-administered scales in IBS. In psychiatric research the HAM-D is the most widely used scale of depressive symptoms with good psychometric properties 74, 75. All studies in this meta-analysis measure the presence and severity of depressive symptoms using HAM-D scales, which significantly decreases the heterogeneity attributed to different assessment instruments.
In this study, compared to healthy controls IBS patients had more severe depressive symptoms overall (SMD=2.02) and also in specific domains, namely anxiety/somatization (SMD=4.03), weight (SMD=4.78), psychomotor retardation (SMD=4.23) and sleep disturbances (SMD=13.54). Further, depressive symptoms were more frequent in IBS patients (OR=9.21), particularly moderate to severe depressive symptoms (OR=10.45). Both frequency and severity of depressive symptoms were higher in this study than in other meta-analyses 27, 30, which may be due to several reasons. First, this study focused more broadly on depressive symptoms rather than major depressive disorder. Second, studies of this meta-analysis only used the HAMD scales, which maintained the homogeneity of assessment compared to other meta-analyses that covered studies employing different self-reported tools to evaluate depressive symptoms 27, 30. It is likely that patients who had severe to very severe depressive symptoms were unable to complete self-reported scales and were therefore excluded from studies included in previous meta-analyses. Using rater-administered scales is more likely to include patients with wider range of severity which could lead to a larger effect size in this study.
In this study all IBS subtypes were associated with increased risk of the development of depressive symptoms. Patients with IBS-M showed the largest effect size (SMD = 2.50; 95% CI, 1.86-3.14), which is different from studies that found IBS-C/IBS-D with the largest effect size 18, 25, 26. Possible factors for this discrepancy may relate to the different number of included studies and measures of depressive symptoms across meta-analyses.
Subgroup and meta-regression analyses found that HAM-D versions (HAMD-17, HAMD-24 and HAMD-NR), IBS diagnostic criteria (ROME I, ROME II and ROME III), younger age, female gender and small sample size were significantly associated with more severe depressive symptoms. In terms of gender differences, earlier studies 76 found that women with IBS had more severe IBS symptoms and lower quality of life than men, regardless of diagnostic criteria used. In addition, the prevalence of IBS in women is approximately 1.5 to 3 fold higher than in men 77-80. Further, in IBS patients with severe symptoms (>3 Manning criteria), 80% are women. The consensus in the literature is that women have more anxiety and depressive symptoms than men with IBS 81, which is supported by the current study, but not others 30.
IBS occurs in all age groups 82 although around half of those with IBS develop initial symptoms before age of 35 years 83. As the prevalence of IBS and severity of pain usually decrease after the age of 50 years 84, there may be less depressive symptoms in older patients, which is consistent with our findings. Different sample sizes could influence the power to detect significant results 38, which could account for the association between sample size and the prevalence of depressive symptoms. The findings of clinical trials with small sample size are usually not stable, thus results of small studies should be interpreted with caution 85.
A previous study 30 showed no significant association between IBS diagnostic criteria and severity of depressive symptoms. However, in this study patients diagnosed according to Rome II or Rome III criteria had more severe depressive symptoms than healthy controls, while no significant difference was found between those diagnosed with Rome I criteria and controls. Reasons for the discrepancy may include the different depression scales used (self-reported scales vs. interviewer-rated scales) and the differences between the three diagnostic criteria in terms of the frequency and severity of IBS symptoms. For example, more IBS symptoms and stringent severity were adopted in Rome II than Rome III criteria, while Rome III criteria contain more items on the socioeconomic burden of IBS than Rome II 86. Further, only one study using Rome I was included in this meta-analysis.
The results of this meta-analysis should be interpreted with caution due to several methodological limitations. First, studies included in the meta-analysis focused on depressive symptoms, but not major depressive disorder. The prevalence studies of major depressive disorder in IBS needs more sophisticated methodology. Second, there was publication bias in the meta-analysis. Third, high heterogeneity remained in some subgroup analyses. Fourth, relevant variables related to IBS, such as pharmacotherapy, were not examined due to incomplete information. Finally, most studies were conducted in China, which may lead to selection bias.
In conclusion, patients with IBS of all subtypes had more frequent and severe depressive symptoms than healthy controls, particularly female and younger patients. Regular screening on depressive symptoms and effective interventions should be developed for this patient population.
Acknowledgments
Funding
The study was supported in part by grants from the Beijing Municipal Administration of Hospitals Incubating Program (code: PX2016016), the Capital City Clinical Practice and Research Funding of Beijing Municipal Science & Technology Commission (Z141107002514033; Z151100004015042), the Clinical Medicine Development Funding of Beijing Municipal Administration of Hospitals (ZYLX201403; ZYLX201607), and the Beijing Municipal Administration of Hospital's Ascent Plan (DFL20151801).
Review registration: CRD42017076997.
Supplementary Material
Supplementary figures and table.
References
- 1.Soares RL. Irritable bowel syndrome: a clinical review. World J Gastroenterol. 2014;20:12144–60. doi: 10.3748/wjg.v20.i34.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gwee K-A. Irritable bowel syndrome in developing countries-a disorder of civilization or colonization? Neurogastroenterol Motil. 2005;17:317–24. doi: 10.1111/j.1365-2982.2005.00627.x. [DOI] [PubMed] [Google Scholar]
- 3.Drossman DA, Camilleri M, Mayer EA. et al. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108–31. doi: 10.1053/gast.2002.37095. [DOI] [PubMed] [Google Scholar]
- 4.Mearin F, Lacy BE. Diagnostic criteria in IBS: useful or not? Neurogastroenterol Motil. 2012;24:791–801. doi: 10.1111/j.1365-2982.2012.01992.x. [DOI] [PubMed] [Google Scholar]
- 5.Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006;130:1377–90. doi: 10.1053/j.gastro.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Longstreth GF, Thompson WG, Chey WD. et al. Functional bowel disorders. Gastroenterology. 2006;130:1480–91. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 7.Saha L. Irritable bowel syndrome: Pathogenesis, diagnosis, treatment, and evidence-based medicine. World J Gastroenterol. 2014;20:6759–73. doi: 10.3748/wjg.v20.i22.6759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Occhipinti K, Smith JW. Irritable bowel syndrome: a review and update. Clin Colon Rectal Surg. 2012;25:46–52. doi: 10.1055/s-0032-1301759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mönnikes H. Quality of life in patients with irritable bowel syndrome. J Clin Gastroenterol. 2011;45:S98–S101. doi: 10.1097/MCG.0b013e31821fbf44. [DOI] [PubMed] [Google Scholar]
- 10.Van Oudenhove L, Levy RL, Crowell MD. et al. Biopsychosocial aspects of functional gastrointestinal disorders: how central and environmental processes contribute to the development and expression of functional gastrointestinal disorders. Gastroenterology. 2016;150:1355–67. doi: 10.1053/j.gastro.2016.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Talley NJ, Howell S, Poulton R. The irritable bowel syndrome and psychiatric disorders in the community: is there a link? Am J Gastroenterol. 2001;96:1072–9. doi: 10.1111/j.1572-0241.2001.03741.x. [DOI] [PubMed] [Google Scholar]
- 12.Kabra N, Nadkarni A. Prevalence of depression and anxiety in irritable bowel syndrome: A clinic based study from India. Indian J Psychiatry. 2013;55:77–80. doi: 10.4103/0019-5545.105520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones MP, Crowell MD, Olden KW. et al. Functional gastrointestinal disorders: an update for the psychiatrist. Psychosomatics. 2007;48:93–102. doi: 10.1176/appi.psy.48.2.93. [DOI] [PubMed] [Google Scholar]
- 14.Van Oudenhove L, Coen SJ, Aziz Q. Functional brain imaging of gastrointestinal sensation in health and disease. World J Gastroenterol. 2007;13:3438–45. doi: 10.3748/wjg.v13.i25.3438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Oudenhove L, Vandenberghe J, Demyttenaere K. et al. Psychosocial factors, psychiatric illness and functional gastrointestinal disorders: a historical perspective. Digestion. 2010;82:201–10. doi: 10.1159/000269822. [DOI] [PubMed] [Google Scholar]
- 16.Weaver KR, Sherwin LB, Walitt B. et al. Neuroimaging the brain-gut axis in patients with irritable bowel syndrome. World J Gastrointest Pharmacol Ther. 2016;7:320–33. doi: 10.4292/wjgpt.v7.i2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.ACOGI Force, Brandt LJ, Chey WD. et al. An evidence-based position statement on the management of irritable bowel syndrome. Am J Gastroenterol. 2008;104(suppl 1):S1–35. doi: 10.1038/ajg.2008.122. [DOI] [PubMed] [Google Scholar]
- 18.Ford AC, Quigley EM, Lacy BE. et al. Effect of antidepressants and psychological therapies, including hypnotherapy, in irritable bowel syndrome: systematic review and meta-analysis. Am J Gastroenterol. 2014;109:1350–65. doi: 10.1038/ajg.2014.148. [DOI] [PubMed] [Google Scholar]
- 19.Seminowicz DA, Labus JS, Bueller JA. et al. Regional gray matter density changes in brains of patients with irritable bowel syndrome. Gastroenterology. 2010;139:48–57. doi: 10.1053/j.gastro.2010.03.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thijssen AY, Mujagic Z, Jonkers DM. et al. Alterations in serotonin metabolism in the irritable bowel syndrome. Alimentary Pharmacol Ther. 2016;43:272–82. doi: 10.1111/apt.13459. [DOI] [PubMed] [Google Scholar]
- 21.Cho HS, Park JM, Lim CH. et al. Anxiety, depression and quality of life in patients with irritable bowel syndrome. Gut Liver. 2011;5:29–36. doi: 10.5009/gnl.2011.5.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sugaya N, Nomura S, Shimada H. Relationship between cognitive factors and anxiety in individuals with irritable bowel syndrome. Int J Behav Med. 2012;19:308–15. doi: 10.1007/s12529-011-9195-0. [DOI] [PubMed] [Google Scholar]
- 23.Ålander T, Heimer G, Svärdsudd K. et al. Abuse in women and men with and without functional gastrointestinal disorders. Dig Dis Sci. 2008;53:1856–64. doi: 10.1007/s10620-007-0101-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berman S, Suyenobu B, Naliboff BD. et al. Evidence for alterations in central noradrenergic signaling in irritable bowel syndrome. Neuroimage. 2012;63:1854–63. doi: 10.1016/j.neuroimage.2012.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muscatello MR, Bruno A, Pandolfo G. et al. Depression, anxiety and anger in subtypes of irritable bowel syndrome patients. J Clin Psychol Med Settings. 2010;17:64–70. doi: 10.1007/s10880-009-9182-7. [DOI] [PubMed] [Google Scholar]
- 26.Guthrie E, Creed F, Fernandes L. et al. Cluster analysis of symptoms and health seeking behaviour differentiates subgroups of patients with severe irritable bowel syndrome. Gut. 2003;52:1616–22. doi: 10.1136/gut.52.11.1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fond G, Loundou A, Hamdani N. et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2014;264:651–60. doi: 10.1007/s00406-014-0502-z. [DOI] [PubMed] [Google Scholar]
- 28.Camilleri M, McKinzie S, Busciglio I. et al. Prospective study of motor, sensory, psychologic, and autonomic functions in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2008;6:772–81. doi: 10.1016/j.cgh.2008.02.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farzaneh N, Ghobakhlou M, Moghimi-Dehkordi B. et al. Evaluation of psychological aspects among subtypes of irritable bowel syndrome. Indian J Psychol Med. 2012;34:144–8. doi: 10.4103/0253-7176.101780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee C, Doo E, Choi JM. et al. The increased level of depression and anxiety in irritable bowel syndrome patients compared with healthy controls: systematic review and meta-analysis. J Neurogastroenterol Motil. 2017;23:349–62. doi: 10.5056/jnm16220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hedlund JL, Vieweg BW. The Hamilton rating scale for depression: a comprehensive review. Journal of Operational Psychiatry. 1979;10:149–65. [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J. et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sibelli A, Chalder T, Everitt H. et al. A systematic review with meta-analysis of the role of anxiety and depression in irritable bowel syndrome onset. Psychol Med. 2016;46:3065–80. doi: 10.1017/S0033291716001987. [DOI] [PubMed] [Google Scholar]
- 35.Higgins J E. Cochrane Handbook for Systematic Reviews of Interventions[J] Naunyn-Schmiedebergs Archiv für experimentelle Pathologie und Pharmakologie. 2011;5(2):S38. [Google Scholar]
- 36.Higgins JP, Thompson SG, Deeks JJ. et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 38.Cohen DJ. Statistical power analysis for the behavioral sciences. Technometrics. 1988;31(4):499–500. [Google Scholar]
- 39.Thompson SG, Sharp SJ. Explaining heterogeneity in meta-analysis: a comparison of methods. Stat Med. 1999;18:2693–708. doi: 10.1002/(sici)1097-0258(19991030)18:20<2693::aid-sim235>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 40.Egger M, Davey Smith G, Schneider M. et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54:1046–1055. doi: 10.1016/s0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 42.Zeng X, Zhang Y, Kwong J S. et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8:2–10. doi: 10.1111/jebm.12141. [DOI] [PubMed] [Google Scholar]
- 43.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 44.Zhou FC, Wang YY, Zheng W. et al. Prospective memory deficits in patients with depression: A meta-analysis. J Affect disord. 2017;220:79–85. doi: 10.1016/j.jad.2017.05.042. [DOI] [PubMed] [Google Scholar]
- 45.Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344:e536. doi: 10.1136/bmj.e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu BB, Jia L, Jiang SM. et al. A large sample and multi-center survey of the depression and anxiety status of patients with refractory irritable bowel syndrome in Guangdong province (in Chinese) Chin J Behav Med Brain Sci. 2013;22:140–3. [Google Scholar]
- 47.Mao HT, Tang YL. Analysis on mental status of the patients with irritable bowel syndrome (in Chinese) Clin Med Eng. 2010;17:1–2. [Google Scholar]
- 48.Hao XL, Huang XL, Gao F. Analysis on patients of ulcerative colitis with anxiety and depression (in Chinese) Xinjiang Med J; 2015. pp. 885–6. [Google Scholar]
- 49.Tian ZY, Feng LY. Anxiety and depression analysis on ulcerative colitis patients (in Chinese) Chin J Clin Ration Drug Use. 2011;04:11–2. [Google Scholar]
- 50.Chen WK, Zou YY, Li FJ. et al. Changes of psychosocial factors, enteric mucosal mast celles and 5-hydroxytryptamine in irntabIe bowel syndrome (in Chinese) World Chin J Digestol. 2007;15:46–50. [Google Scholar]
- 51.Xu YX. The clinical analysis about the relationship between IBS and psychogeny (in Chinese) Fudan Univ; 2014. [Google Scholar]
- 52.Li S. Clinical studies on the expression of IL-4 and IL-6 in intestinal mucosa and its relation with anxiety-depression of IBS-D patients (in Chinese) North China Univ Sci Tech; 2015. [Google Scholar]
- 53.Li XM, Chen P, Gao RP. et al. Comparison of the differences of anxiety and depression in the patients with various functional gastrointestinal disorders (in Chinese) Ningxia Med J. 2015;37:995–6. [Google Scholar]
- 54.Wang GZ. The Correlation Analysis of Irritable Bowel Syndrome and Depression (in Chinese) World Latest Med Inform; 2014. pp. 24–5. [Google Scholar]
- 55.Shi DW. The correlations about clinical symptoms with intestinal flora and the change of HPT in irritable bowel syndrome (in Chinese) Zhengzhou Univ; 2012. [Google Scholar]
- 56.Wan HY, Chen YL. MentaI status and dysautonomia in patients with irritable boweI syndrome (in Chinese) Chin J Clin Rehabil. 2005;9:72–3. [Google Scholar]
- 57.Xu F, Liu DS. Observation of the emotional condition in patients with irritable bowel syndrome (in Chinese) J Bengbu Med Coll. 2012;37:561–3. [Google Scholar]
- 58.Chen CY, Wang Y, Lin Q. et al. The psychological factors of patients with refractory irritable bowel syndrome (in Chinese) J Clin Psychosom Dis. 2007;13:525–6. [Google Scholar]
- 59.Zhang YJ, Wang P, Jin JJ. et al. The relationship between gastric motility, gastrointestinal hormones and psychological factors in patients with irritable bowel syndrome (in Chinese) J Clin Internal Med. 2007;24(1):54–6. [Google Scholar]
- 60.Wang XP, Liu YT, Ren QT. Relationship of CRP with the state of anxiety and depression in irritable bowel syndrome (in Chinese) China Modern Doctor. 2012;50:146–7. [Google Scholar]
- 61.Shi QL, Zhang CC. The relationship of negative emotions with 5-HT and 5-HIAA in peripheral blood of patients with constipation-predominant irritable bowel syndrome (in Chinese) Med Frontier; 2012. pp. 10–11. [Google Scholar]
- 62.Mu B, Wang BM, Huang NX. et al. A study on psychological factor in the pat ients with IBS (in Chinese) J Tianjin Med Univ. 2003;9:543–4. [Google Scholar]
- 63.Song JZ, Wang QM, Wang C. Symptom features of irritable bowel syndrome complicated with depression (in Chinese) Chin J Digestion; 2015. pp. 590–4. [Google Scholar]
- 64.Xu XJ, Liu L, Yao SK. et al. Visceral sensitivity, gut barrier function and autonomic nerve function in patients with diarrhea-predominant irritable bowel syndrome (in Chinese) J Central South Univ (Med Sci) 2017;42:522–8. doi: 10.11817/j.issn.1672-7347.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 65.Jin DD, Xu M, Chen Z. et al. Emotional Disorders and Treatment in Patients with Refractory Irritable Bowel Syndrome (in Chinese) Chin J Gastroenterol. 2004;9:90–3. [Google Scholar]
- 66.Tosic-Golubovic S, Miljkovic S, Nagorni A. et al. Irritable bowel syndrome, anxiety, depression and personality characteristics. Psychiatr Danub. 2010;22:418–24. [PubMed] [Google Scholar]
- 67.Kilkens TO, Honig A, Maes M. et al. Fatty acid profile and affective dysregulation in irritable bowel syndrome. Lipids. 2004;39:425–31. doi: 10.1007/s11745-004-1247-x. [DOI] [PubMed] [Google Scholar]
- 68.Goncalves de Medeiros MT, de Oliveira RB, dos Santos AA. et al. The effects of sildenafil on rectal sensitivity and tone in patients with the irritable bowel syndrome. Aliment Pharmacol Ther. 2012;35:577–86. doi: 10.1111/j.1365-2036.2011.04977.x. [DOI] [PubMed] [Google Scholar]
- 69.Akkus S, Senol A, Ayvacioglu NB. et al. Is female predominance in irritable bowel syndrome related to fibromyalgia? Rheumatol Int. 2004;24:106–9. doi: 10.1007/s00296-003-0328-x. [DOI] [PubMed] [Google Scholar]
- 70.Cleary P, Guy W. Factor analysis of the Hamilton depression scale. Drugs Exp Clin Res. 1977;1:115–20. [Google Scholar]
- 71.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–96. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 72.Baumann U. Methodologic studies of the Hamilton Rating Scale for Depression. Arch Psychiatr Nervenkr. 1976;222:359–75. doi: 10.1007/BF00343243. [DOI] [PubMed] [Google Scholar]
- 73.Zimmerman M, Martinez J H, Young D. et al. Severity classification on the Hamilton depression rating scale. J Affect Disord. 2013;150:384–388. doi: 10.1016/j.jad.2013.04.028. [DOI] [PubMed] [Google Scholar]
- 74.Carneiro AM, Fernandes F, Moreno RA. Hamilton depression rating scale and montgomery-asberg depression rating scale in depressed and bipolar I patients: psychometric properties in a Brazilian sample. Health Qual Life Outcomes. 2015;13:42. doi: 10.1186/s12955-015-0235-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.López-Pina JA, Sánhez-Meca J, Rosa-Alcázar AI. The Hamilton Rating Scale for Depression: a meta analytic reliability generalization study. Int J Clin Health Psychol; 2009. p. 9. [Google Scholar]
- 76.Quigley EM, Bytzer P, Jones R. et al. Irritable bowel syndrome: the burden and unmet needs in Europe. Dig Liver Dis. 2006;38:717–23. doi: 10.1016/j.dld.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 77.Manning AP, Thompson WG, Heaton KW. et al. Towards positive diagnosis of the irritable bowel. Br Med J. 1978;2:653–4. doi: 10.1136/bmj.2.6138.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kennedy TM, Jones RH, Hungin AP. et al. Irritable bowel syndrome, gastro-oesophageal reflux, and bronchial hyper-responsiveness in the general population. Gut. 1998;43:770–4. doi: 10.1136/gut.43.6.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Drossman DA, Thompson WG, Talley NJ. et al. Identification of sub-groups of functional gastrointestinal disorders. Gastroenterol Int. 1990;3:159–72. [Google Scholar]
- 80.Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014;6:71–80. doi: 10.2147/CLEP.S40245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Longstreth GF, Wolde-Tsadik G. Irritable bowel-type symptoms in HMO examinees. Dig Dis Sci. 1993;38:1581–9. doi: 10.1007/BF01303163. [DOI] [PubMed] [Google Scholar]
- 82.Tang YR, Yang WW, Liang ML. et al. Age-related symptom and life quality changes in women with irritable bowel syndrome. World J Gastroenterol. 2012;18:7175–83. doi: 10.3748/wjg.v18.i48.7175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Maxwell PR, Mendall MA, Kumar D. Irritable bowel syndrome. Lancet. 1997;350:1691–5. doi: 10.1016/s0140-6736(97)05276-8. [DOI] [PubMed] [Google Scholar]
- 84.Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:712–21. doi: 10.1016/j.cgh.2012.02.029. [DOI] [PubMed] [Google Scholar]
- 85.Zhang Z, Xu X, Ni H. Small studies may overestimate the effect sizes in critical care meta-analyses: a meta-epidemiological study. Crit Care. 2013;17:R2. doi: 10.1186/cc11919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sperber AD, Shvartzman P, Friger M. et al. A comparative reappraisal of the Rome II and Rome III diagnostic criteria: are we getting closer to the 'true' prevalence of irritable bowel syndrome? Eur J Gastroenterol Hepatol. 2007;19:441–7. doi: 10.1097/MEG.0b013e32801140e2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figures and table.