Abstract
Background
Despite the substantial impact on child and maternal health, breastfeeding practices for infants remain at the suboptimum level in Bangladesh. Yet the understanding of why these practices are suboptimal, especially surrounding urban slum dwelling mothers, is unclear. The purpose of this study was to assess early infant feeding practices, examine associations with maternal factors, and uncover the facilitators and barriers to early feeding practices in selected slums of Dhaka, Bangladesh.
Methods
A mixed method study was conducted from June to September 2016 using both quantitative and qualitative methods among mothers with children under the age of 6 months. The survey included 342 mother-infant pairs and 18 in-depth interviews were conducted. Univariate and multiple logistic regression was used to determine status of early infant feeding practices and factors associated with exclusive breastfeeding (EBF) within the previous 24 h. Transcripts were coded to uncover the facilitators and barriers surrounding early infant feeding practices.
Results
Sixty four percent (220/342) of mothers initiated breastfeeding within 1 h, 96.5% (330/342) reported feeding colostrum, and 36.3% (124/342) infants were EBF in the last 24 h. After adjusting for child gender, maternal age, education, diet and household income; infant’s age (adjusted odds ratio (AOR) for 61–120 days 6.42; 95% CI 3.42, 12.1; AOR for 121–180 days 45.6; 95% CI 18.33, 113.45), prelacteal feeding (AOR 2.53; 95% CI 1.14, 4.58), lack of planning for EBF during pregnancy (AOR 4.06; 95% CI 1.09, 15.12) and infants delivered by cesarean section (AOR 2.76; 95% CI 1.34, 5.67) were negatively associated with EBF. During the 18 interviews, eight mothers reported a cesarean delivery and none of these mothers initiated breastfeeding within 1 h or exclusively breastfed. Moreover, all eight mothers gave their infants prelacteal feeds.
Conclusions
The status of early infant feeding practices in Dhaka’s slums was poor. The negative impact of cesarean section on all early infant feeding practices was evident in both quantitative and qualitative analysis.
Keywords: Initial breastfeeding, Exclusive breastfeeding, Associated factors, Barriers and facilitators, Mode of delivery, Slum, Dhaka, Bangladesh
Background
Appropriate feeding for first 6 months of life is crucial for child health and survival. Breastfeeding saves lives and promotes physical and mental health throughout childhood and beyond [1–5]. Increasing infant survival by at least six times, breastfeeding impacts childhood survival significantly [1]. Moreover, infants exclusively breastfed are 14 times less likely to die in first 6 months compared to non-breastfed infants, while partially and non-breastfed children are at 5–9 times higher risk of death due to infection [1]. If breastfeeding was scaled up to near universal level (90–95%) 823,000 deaths could have been saved in low and middle-income countries (LMICs) in 2015 [6].
Despite the known positive impact of breastfeeding on infant survival and health, the rate of exclusive breastfeeding globally is low [7]. In 2015, 37% infants less than 6 months old were exclusively breastfed in LMICs [6]. In Bangladesh, for the past two decades, the prevalence of exclusive breastfeeding remained constant around 55% [8]. Additionally, in 2014 the rate of early initiation of breastfeeding was 51% and 27% of the newborn received prelacteal feeds in their first 3 days of life [8].
Bangladesh is undergoing a rapid urbanization process. The current urban population will increase by 50% in 2028. One third of this urban population live in slums and are inclined to experience negative factors of health and nutrition. According to Bangladesh Urban Health Survey 2013, health indicators are lower in urban slums compared to non-slum areas [9]. Among infants of mothers from Dhaka’s slum, 10% of infants were exclusively breastfed for 6 months, breastfeeding was initiated within 1 h in 24% of infants, and 54% of infants were given prelacteal feeds; which are much lower compared to the national rates of 55% EBF, 51% early initiation and 27% prelacteal feeds [8, 10].
Low rates of early initiation and exclusive breastfeeding are reflective of various factors influencing a mothers’ inability or reluctance to breastfeed. A mother’s experience, and in turn her child bearing and rearing, is largely embedded in social, cultural, and personal norms and perceptions. Therefore, it is difficult to generalize the determinants of early infant feeding practices. Exclusive breastfeeding for first 6 months has been found to be associated with maternal age, education, occupation, economic status, place of residence, and mother’s intention to breastfeed [11–20]. Other factors influencing exclusive breastfeeding are history of prelacteal feeding, early initiation, antenatal care visits, prenatal counseling, influence from healthcare providers, type of delivery [11, 13, 14, 16, 19, 20].
Specifically, a birth by cesarean section negatively impacts early infant feeding practies, and globally the rate of cesarean delivery is increasing. The largest absolute increase in cesarean delivery has been observed in developing countries, with an increase of 6.7% from 1990 to 2014 [21]. Moreover, within Bangladesh, cesarean delivery has increased from 4% in 2004 to 23% in 2014 [8]. The implications of cesarean delivery on early infant feeding is yet to be explored within the Bangladesh context.
Moreover, qualitative studies found that maternal perception influenced early infant feeding practices in different areas of Bangladesh and other low and middle income countries [22–25]. Such influencing factors vary, not only in the context of different countries but also in different settings within country. An explanatory study conducted among slum dwellers in Dhaka revealed poor practice of initiation of breastfeeding within 1 h of birth [25]. Still the perceived barriers and facilitators of exclusive breastfeeding among the mothers with children less than 6 months of age need to be explored. A recent study from Bangladesh Urban Health Survey (BDHS) 2014 data revealed that less educated and housewife mothers are more inclined to exclusive breastfeeding [26]. Therefore, given the limited evidence surrounding feeding practices in Dhaka’s slums, the study investigated the status of early feeding practices in infants less than 6 months, examined factors associated with such practices, and uncovered the facilitators and barriers to early infant feeding practices in selected slums of Dhaka, Bangladesh.
Methods
Study design and sample selection
A mixed method study was conducted using both quantitative and qualitative methods in two conveniently selected slums, Korail and Sat Tala slum, in Dhaka. Korail slum is one of the largest slums and has approximately 15,000 households, while Sat Tala slum has nearly 6500 households, and 342 mothers with children under the age of 6 months were studied. Household listing in the selected area was carried out to identify the household with eligible participants prior to interview. All eligible households with children less than 6 months in the selected area were visited and mother infant dyads were interviewed and evaluated for nutritional status. Qualitatively, 18 mothers were purposively selected from both slums and interviewed with an in-depth interview guide.
Sample size calculation: Sample size for quantitative method was calculated based on current exclusive breastfeeding rate as an indicator of early infant feeding practice at 90% confidence level, 5% precision and with a design effect of 1.2 [8]. Estimated sample size was 324 and with a 10% attrition rate required sample size was 360.
Selection of variables
Independent variables were selected based on extensive literature review. Relevant child characteristics for early infant feeding were child age, gender, birth order, immunization status and infant’s nutritional status. Maternal characteristics assessed were age, education, occupation, age at first pregnancy, planning for EBF during pregnancy, maternal depressive symptoms, number of antenatal care visit, postnatal care visit, place of delivery, assisted delivery by trained professionals, mode of delivery, maternal dietary diversity (24-h recall), maternal nutritional status, initiation of breastfeeding and practice of giving prelacteal feeds. Household characteristics considered were monthly income, asset index as a proxy indicator of household wealth, and household food consumption (7 days recall). Exclusive breastfeeding coded as a binary outcome and used as a dependent variable.
Data collection
Face-to-face structured questionnaires were administered to mothers on infant feeding practices at birth and within the last 24 h. Early infant feeding practices were summarized as exclusively breastfed (consumed only breast milk with an exception of Oral Rehydration Solution (ORS), medicine drops, syrups); predominantly breastfed (consumed breast milk with certain liquids (water and water-based drinks, fruit juice, ritual fluids and ORS, drops or syrups (vitamins, minerals, and medicines); partially breastfed (consumed breast milk with any food or liquid); and non-breastfed (did not consume breast milk) [27]. Other information collected included sociodemographic characteristics of infant, mother and household; maternal psychological condition; environmental factors including family, workplace and social service facilities; maternal and household diet; and anthropometric measurement of infants and mothers. For qualitative data collection individual in-depth interview was conducted. A semi-structured questionnaire adopted from ProPAN 2 was used to guide the interview ProPAN is a set of research tools designed for ministries of health (MoHs), nongovernmental organizations (NGOs), and bilateral and international organizations working to improve the diets and feeding practices of children under 24 months old to prevent early childhood malnutrition [28]. ProPAN multi-module field manual provides detailed instructions on how to collect, analyze, and integrate the quantitative and qualitative data required to design and evaluate interventions. The study period was from June to September 2016.
Derived variable for analysis: Maternal depressive symptoms were measured by a 20 items self-reporting questionnaire developed by World Health Organization and previously used nationally in Bangladesh [29]. Mothers with a score of eight positive answers were categorized as having depressive symptoms. Dietary diversity was based on a 24-h recall of food consumption. Food was captured within nine pre-determined food groups, as defined by Food and Nutrition Technical Assistance (FANTA). Mothers consuming five or more food groups were categorized as having adequate dietary diversity in terms of macro- and micro-nutrients.
Household food consumption, a proxy indicator of household food security developed by World Food Program, has been validated in Bangladesh and was used in the 2009 Bangladesh Household Food Security and Nutrition Assessment Report. This composite score was based on a seven-day recall of frequency of food consumption and categorized as poor consumption (0–28), borderline consumption (28.5- < 42), acceptable low consumption (42–52) and acceptable high consumption (> 52) [30].
Household asset index was calculated using household asset data on ownership of several consumer items, access to safe drinking water, and improved sanitation [8], and households were indexed into quintiles from poorest to richest.
Data analysis
Quantitative
Data was analyzed with Stata SE Version 13.0 software. Descriptive analysis was conducted to characterize the study population by infant, maternal and household characteristics. Simple logistic regression was utilized to determine the association between each independent variable and the outcome variable, exclusive breastfeeding status, and for consideration in the final model. Results are shown as crude odds ratios and p-values. Variables considered for inclusion in the multiple logistic regression analysis were selected based on previous literature [12–15, 17–20]. Variance inflation factor (VIF) was calculated to detect multicollinearity among the variables. If the VIF of a factor was 5–10 it was considered as moderate collinearity. If the VIF > 10 it was considered severe collinearity and the predictor was removed from the model. The model with highest R square value was considered to be the final regression model. All variables with a p-value less than 0.15 in bi-variate analysis were included, after adjusting for other variables [31]. Age and gender were considered as non-modifiable factors and adjusted in the final model [31]. Associated factors with p-value < 0.05 was considered to be statistically significant.
Qualitative
To explore the facilitators and barriers to optimal early infant feeding practices for the first 6 months of life, 18 in-depth interviews with mothers were conducted in the selected slums. The sample included purposively selected participants who completed the quantitative questionnaire. Nine mothers were selected who exclusively breast fed and nine who did not, based on reported exclusive breastfeeding status within 24 h. Two trained interviewers interviewed the participants per an in-depth interview guideline that included questions surrounding ideal early infant feeding practices during the first 6 months of life [28].
All interviews were tape recorded and transcribed in Bangali the same day. Qualitative analysis was conducted thematically. Transcripts were manually reviewed and coded for topics related to infant feeding practices. Transcripts were double coded and agreement of any discordant code was achieved through discussion. Finally, a matrix was prepared based on the coding and translated into English. Barriers and facilitators were categorized in external and internal factors in the matrix. External factors were those over which the caregiver has little (if any) control and internal factors refers to those intrinsic to the caregiver [28]. No software was used for the analysis.
Results
Descriptive characteristics of the participants (from quantitative survey)
A total of 342 mothers with infants less than 6 months of age were interviewed in this study, and a study profile is described in Fig. 1. A descriptive analysis of the sample, stratified by early infant feeding practices, is presented in Table 1. The majority of mothers (90.6%) reported being housewives, and 42.9% had received primary level education. Based on 24 h recall, 52.1% of mothers’ diet lacked adequate dietary diversity (consumption of ≥5 groups). Moreover, while 70% of mothers had normal nutritional status, 10.5% were thin and 22.5% overweight/obese (BMI < 18 and BMI > 25, respectively). Among the infants, 13.7% were stunted, 7.6% were wasted, 10.8% were underweight, and 4.7% were overweight.
Fig. 1.
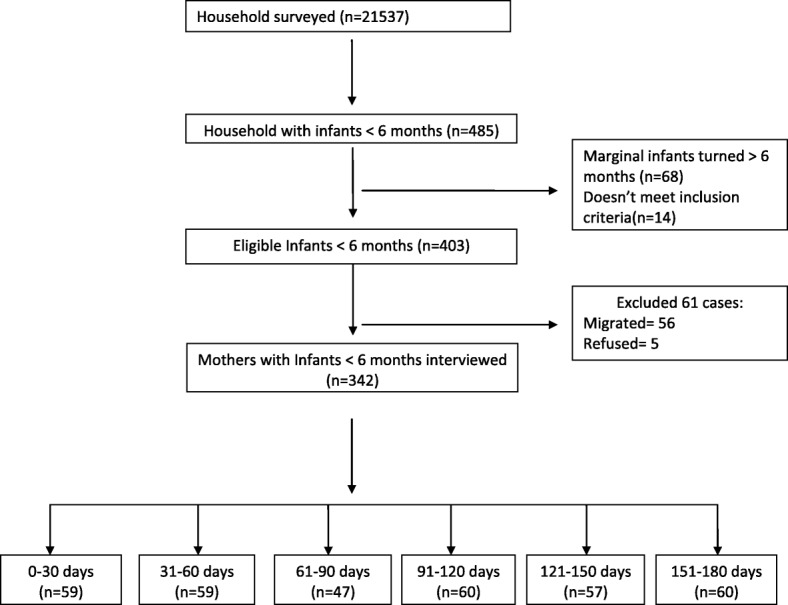
Study profile
Table 1.
Descriptive statistics of the sample stratified by percentage of exclusively breastfed, predominantly breastfed, partially breastfed and non-breastfed
| n | Exclusively breastfed % (95% CI) | Predominantly breastfed % (95% CI) | Partially breastfed % (95% CI) | Non breastfed % (95% CI) | |
|---|---|---|---|---|---|
| Infants characteristics | |||||
| Infant’s age | |||||
| 0–60 days | 118 | 70.3(61.4,78) | 13.6(8.4,21.1) | 16.1(10.4,24) | 0(0,0) |
| 61–120 days | 107 | 29.9(21.9,39.4) | 24.3(17,33.5) | 42.1(32.9,51.7) | 3.7(1.4,9.7) |
| 121–180 days | 117 | 7.7(4,14.2) | 28.2(20.7,37.2) | 61.5(52.3,70) | 2.6(0.8,7.8) |
| Gender | |||||
| Male | 178 | 38.2(31.3,45.6) | 23(17.4,29.9) | 36(29.2,43.3) | 2.8(1.2,6.6) |
| Female | 164 | 34.1(27.2,41.8) | 20.7(15.2,27.7) | 43.9(36.4,51.7) | 1.2(0.3,4.8) |
| Birth order (Reference child) | |||||
| 1st child | 145 | 37.2(29.7,45.5) | 26.2(19.6,34.1) | 34.5(27.1,42.7) | 2.1(0.7,6.3) |
| 2nd child or over | 197 | 35.5(29.1,42.5) | 18.8(13.9,24.9) | 43.7(36.8,50.7) | 2(0.8,5.3) |
| Immunization status (According to mothers’ response) | |||||
| Properly Immunized | 263 | 29.3(24.1,35.1) | 26.2(21.2,31.9) | 42.2(36.3,48.3) | 2.3(1,5) |
| Not immunized | 79 | 59.5(48.1,69.9) | 7.6(3.4,16.1) | 31.6(22.2,42.9) | 1.3(0.2,8.8) |
| Maternal characteristics | |||||
| Age | |||||
| < 18 years | 21 | 38.1(19.1,61.7) | 14.3(4.2,38.7) | 47.6(26.3,69.8) | 0(0,0) |
| ≥ 18 years | 321 | 36.1(31,41.6) | 22.4(18.2,27.3) | 39.3(34,44.7) | 2.2(1,4.5) |
| Maternal education level | |||||
| No formal education | 112 | 36.6(28.1,46) | 20.5(14,29.2) | 40.2(31.4,49.6) | 2.7(0.9,8.1) |
| Primary complete | 147 | 33.3(26.1,41.4) | 21.8(15.8,29.3) | 42.9(35,51.1) | 2(0.7,6.2) |
| secondary or above | 83 | 41(30.7,52) | 24.1(16,34.7) | 33.7(24.2,44.8) | 1.2(0.2,8.4) |
| Maternal occupation | |||||
| Housewife | 310 | 37.7(32.5,43.3) | 22.9(18.5,27.9) | 37.7(32.5,43.3) | 1.6(0.7,3.8) |
| Working mother | 32 | 21.9(10.3,40.4) | 12.5(4.50,30.2) | 59.4(40.9,75.5) | 6.3(1.4,23.2) |
| Maternal age at 1st pregnancy | |||||
| < 18 years | 98 | 34.7(25.8,44.8) | 18.4(11.8,27.5) | 45.9(36.2,56) | 1(0.1,7.1) |
| ≥ 18 years | 244 | 36.9(31,43.2) | 23.4(18.4,29.1) | 37.3(31.4,43.6) | 2.5(1.1,5.4) |
| EBF planning during pregnancy | |||||
| planned | 308 | 38.3(33,43.9) | 20.5(16.3,25.4) | 39.6(34.3,45.2) | 1.6(0.7,3.9) |
| not planned | 34 | 17.6(7.8,35.2) | 35.3(20.6,53.4) | 41.2(25.4,59) | 5.9(1.4,22) |
| Maternal depressive symptoms | |||||
| Absent | 263 | 39.2(28.9,50.6) | 17.7(10.7,28.0) | 43(32.4,54.4) | 0(0,0) |
| Present | 79 | 35.4(29.8,41.4) | 23.2(18.5,28.7) | 38.8(33,44.8) | 2.7(1.3,5.5) |
| Antenatal care (ANC) | |||||
| No or < 4 ANC visits | 106 | 28.3(20.4,37.8) | 24.5(17.2,33.8) | 44.3(35,54) | 2.8(0.9,8.6) |
| 4 visits or more | 236 | 39.8(33.7,46.3) | 20.8(16,26.5) | 37.7(31.7,44.1) | 1.7(0.6,4.5) |
| Received postnatal care services | 176 | 35.8(29,43.2) | 21.6(16.1,28.4) | 40.3(33.3,47.8) | 2.3(0.8,6) |
| Place of delivery | |||||
| Home delivery | 148 | 35.1(27.8,43.2) | 25.0(18.6,32.7) | 38.5(30.9,46.7) | 1.4(0.3,5.3) |
| Facility delivery | 194 | 37.1(30.6,44.2) | 19.6(14.6,25.8) | 40.7(34,47.8) | 2.6(1.1,6.1) |
| Delivery assisted by | |||||
| Trained professionals | 246 | 37.4(31.5,43.7) | 21.1(16.5,26.7) | 39.4(33.5,45.7) | 2(0.8,4.8) |
| Traditional birth attendant | 96 | 33.3(24.5,43.5) | 24(16.4,33.7) | 40.6(31.1,50.9) | 2.1(0.5,8.1) |
| Mode of delivery | |||||
| Normal Vaginal Delivery (NVD) | 256 | 37.5(31.7,43.6) | 21.5(16.9,27) | 39.1(33.2,45.2) | 2(0.8,4.6) |
| Cesarean Section | 86 | 32.6(23.4,43.3) | 23.3(15.4,33.5) | 41.9(31.7,52.7) | 2.3(0.6,9.1) |
| Maternal dietary diversity | |||||
| ≥ 5 food groups | 164 | 41.5(34.1,49.2) | 20.7(15.2,27.7) | 36(28.9,43.7) | 1.8(0.6,5.6) |
| < 5 group | 178 | 31.5(25,38.7) | 23(17.4,29.9) | 43.3(36.1,50.7) | 2.2(0.8,5.9) |
| Maternal BMI | |||||
| Normal (18.5–24.9) | 229 | 39.3(33.1,45.8) | 22.3(17.3,28.2) | 37.6(31.5,44.1) | 0.9(0.2,3.5) |
| Thin (< 18.5) | 36 | 25(13.1,42.4) | 11.1(4,27.1) | 61.1(43.7,76.1) | 2.8(0.4,18.7) |
| Overweight or obese (> 25) | 77 | 32.5(22.8,43.9) | 26(17.2,37.1) | 36.4(26.2,47.9) | 5.2(1.9,13.3) |
| Early initiation of breastfeeding | |||||
| ≤ 1 h after birth | 204 | 37.3(30.8,44.2) | 20.6(15.5,26.7) | 41.2(34.6,48.1) | 1(0.2,3.9) |
| > 1 h after birth | 138 | 34.8(27.2,43.2) | 23.9(17.5,31.8) | 37.7(29.9,46.1) | 3.6(1.5,8.5) |
| Prelacteal history | |||||
| No prelacteal given | 156 | 43.6(35.9,51.6) | 19.2(13.7,26.3) | 35.3(28.1,43.2) | 1.9(0.6,5.9) |
| Gave prelacteal | 186 | 30.1(23.9,37.1) | 24.2(18.5,30.9) | 43.5(36.5,50.8) | 2.2(0.8,5.6) |
| Household characteristics | |||||
| Household income | |||||
| < 10,000 | 81 | 27.2(18.4,38.1) | 25.9(17.4,36.8) | 43.2(32.7,54.4) | 3.7(1.2,11.1) |
| 10,000 to < 20,000 | 186 | 38.2(31.4,45.4) | 23.1(17.6,29.8) | 37.1(30.4,44.3) | 1.6(0.5,4.9) |
| > 20,000 | 75 | 41.3(30.6,53) | 14.7(8.2,24.9) | 42.7(31.8,54.3) | 1.3(0.2,9.2) |
| Household head | |||||
| Female head | 42 | 31(18.5,47) | 16.7(7.9,31.8) | 47.6(32.6,63.1) | 4.8(1.1,18) |
| Male head | 300 | 37(31.7,42.6) | 22.7(18.3,27.8) | 38.7(33.3,44.3) | 1.7(0.7,4) |
| Household food consumption score | |||||
| Acceptable high consumption (> 52) | 274 | 35.4(29.9,41.3) | 21.9(17.4,27.2) | 40.5(34.8,46.5) | 2.2(1,4.8) |
| Acceptable food consumption (42–52) | 44 | 47.7(33,62.8) | 18.2(9.1,33) | 34.1(21.3,49.7) | 0(0,0) |
| Poor or borderline food consumption (≤ 42) | 24 | 25(11,47.4) | 29.2(13.7,51.5) | 41.7(22.9,63.1) | 4.2(0.5,27.4) |
| Toilet facility | |||||
| Improved facility | 198 | 34.8(28.5,41.8) | 22.2(16.9,28.6) | 41.9(35.2,49) | 1(0.2,4) |
| Non improved facility | 144 | 38.2(30.5,46.5) | 21.5(15.5,29.1) | 36.8(29.2,45.1) | 3.5(1.4,8.2) |
| OVERALL | 342 | 36.3(31.3,41.5) | 21.9(17.8,26.7) | 39.8(34.7,45.1) | 2.1(1,4.3) |
CI Confidence Interval
Prior to giving birth, 90% of mothers planned to exclusively breastfeed for 6 months. Approximately, 66% of mothers received ≥4 visits antenatal checks and 51.5% received a postnatal care visit. Of the 342 mothers, 71.9% delivered by a trained professional at home or at a facility and 56.7% delivered at a healthcare facility. A quarter (25.1%) of mothers had a caesarian delivery.
At the household level, 54.4% of households had a monthly income of 10,000–20,000 BDT, and 87.7% reported a male household head. Based on a seven-day recall, 21.9% of households were found to have borderline to poor food consumption.
Early initiation of breastfeeding
The study found 64.2% of mothers initiated breastfeeding within 1 h of birth. Seven of the 18 mothers who qualitatively reported early initiation explained that support from healthcare workers (i.e. midwives, traditional birth attendants, hospital staff) and in-laws (6 out of 7, 5 out of 7, respectively) facilitated their ability to initiate breastfeeding within 1 h. One mother, age 26 from Korail slum, was influenced “from TV, health worker and neighbors. .. mother and midwives told me to feed the baby and I do so. .. If midwives and family member help to hold the baby it becomes easier for mother to feed the baby early” [101062]. Two out of seven mothers mentioned about learning of early initiation of breastfeeding from TV programming.
Qualitative analysis found that 11 mothers out of 18 did not initiate breastfeeding within 1 h. The main reason for failure of early initiation was because the mother had a cesarean delivery and were unconscious, experiencing side effects of surgery, or unable to produce milk (8 out of 11 mothers). One mother, aged 23 from Korail slum, explained, “after cesarean section I was sick and there was no milk secretion for three days. .. when they gave the baby to me after three to four hours I put the baby on the breast but there was no milk” [101350]. Of the other three mothers who did not early initiate, one mother had incorrect knowledge surrounding early initiation and two, although delivered normally, could not initiate due to the lengthy infant cleaning time at the facility.
The importance of giving colostrum was widely mentioned by the mothers and 96.5% reported feeding colostrum to their infants. Qualitatively, a total of nine out of the 18 mothers stated they administered colostrum during the first 3 days. But only five of these nine mothers provided solely colostrum to their infant during the first 3 days of life, the rest also provided prelacteal feeds.
Moreover, 54.4% of mothers reported prelacteal administration, providing anything other than breastmilk to child during the first 3 days of life. Honey (23.4%), sugar water (13.7%), plain water (10.8%), and infant formula (9.9%) were the most common prelacteal feeds provided to infants. Of the 18 mothers who qualitatively responded, 11 mothers reported administering prelacteal feeds. Moreover, of these 11 mothers, five did so because of the perception of insufficient milk production and to stop the infant from crying. Formula feeding during the first 3 days after birth was mainly due to post cesarean section outcomes (sickness, unconsciousness, and/or no milk production yet) and per the doctors’ prescription. Six of the eight mothers who had a cesarean delivery, administered formula because there was no early initiation of breastfeeding and milk production has not started yet. A mother 23 years old from Korail slum described, “[the] doctor said I can breastfeed my baby but I was sick and irritated. Could not move properly. Even though I tried to breastfeed but baby was crying, I felt frustrated. They prescribed formula and I brought the formula from the hospital and fed him” [101350]. Reasons for prelacteal administration of honey or sugar water was to clear the voice, prevent cold, and sweeten the speech of the child in future. Plain water was given because mothers perceived that infant was thirsty and water would keep the child hydrated. Moreover, seven of the 18 mothers qualitatively said they gave mustard oil to infant to clear mouth and throat after birth.
Exclusive breastfeeding (EBF)
Overall 36.3% infants were exclusively breastfed within the prior 24 h and the prevalence of exclusive breastfeeding was found to decrease with the infant’s age (Fig. 2). Infants 2–4 months and 4–6 months had 5.6 (95% CI 3.14, 9.85) and 28.5 (95% CI 12.96, 62.48) times higher odds of not being exclusively breastfed, respectively, compared to infants 0–2 months. The proportion of infants predominantly, partially, and non-breastfed was 21.9%, 39.8%, and 2.1% respectively (Table 1). Common substitutes or supplements provided include plain water (52.9%), infant formula (27.2%) and homemade thin porridge (9.7%).
Fig. 2.
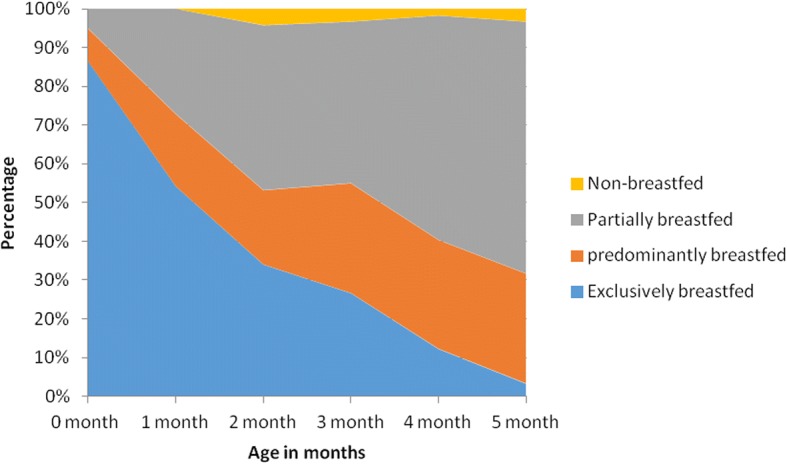
Infant feeding practices by age (Area Plot)
We found that mothers who had no or less than four antenatal care visits (OR 1.68; 95% CI 1.02, 2.76), not intending to exclusively breastfeed when pregnant (OR 2.9; 95% CI 1.17, 7.21), administered prelacteal feeds (OR 1.79; 95% CI 1.15, 2.8) and had low dietary diversity (OR 1.54; 95% CI 0.99, 2.4) were less likely to be exclusively breastfed. Infants from households with a higher asset score (OR 0.73; 95% CI 0.58, 0.9) were less likely to be non-exclusively breastfed (Table 2). There was no association found between maternal nutritional status and exclusive breastfeeding.
Table 2.
Factors associated with non-exclusive breastfeeding of infants less than 6 months
| Independent variables | OR (95% CI) | p - value | Adjusted odds Ratio (95% CI) | p - value |
|---|---|---|---|---|
| Age of infants | ||||
| 0–60 days | Reference | |||
| 61–120 days | 5.56 (3.14,9.85) | 0.00 | 6.42 (3.42,12.07) | 0.00 |
| 121–180 days | 28.46 (12.96,62.48) | 0.00 | 45.6 (18.33,113.45) | 0.00 |
| Child gender | ||||
| Female | Reference | |||
| Male | 0.84 (0.54,1.31) | 0.44 | 0.81 (0.46,1.45) | 0.48 |
| Maternal age | ||||
| ≥ 18 years | Reference | |||
| < 18 years | 0.92 (0.37,2.28) | 0.86 | 0.39 (0.12,1.22) | 0.10 |
| Maternal education | ||||
| No formal education | Reference | |||
| Primary complete | 1.15 (0.69,1.93) | 0.58 | 1.82 (0.91,3.63) | 0.09 |
| Secondary or higher | 0.83 (0.46,1.49) | 0.54 | 2 (0.89,4.51) | 0.10 |
| Antenatal visits | ||||
| 4 or more visits | Reference | |||
| No or < 4 visits | 1.68(1.02,2.76) | 0.04 | 1.41 (0.72,2.76) | 0.31 |
| Planning for EBF | ||||
| Planned EBF during pregnancy | Reference | |||
| Did not plan EBF | 2.9(1.17,7.21) | 0.02 | 4.06 (1.09,15.12 | 0.04 |
| Mode of delivery | ||||
| Normal vaginal delivery | Reference | |||
| CS | 1.24(0.74,2.08) | 0.41 | 2.76 (1.34,5.69) | 0.01 |
| Prelacteal history | ||||
| No prelacteal | Reference | |||
| Prelacteal given | 1.79(1.15,2.8) | 0.01 | 2.53 (1.4,4.58) | 0.00 |
| Maternal Dietary Diversity (MDD) | ||||
| Acceptable dietary diversity (> = 5 groups) | Reference | |||
| Low DD (< 5 food groups) | 1.54(0.99,2.4) | 0.06 | 1.55 (0.87,2.78) | 0.14 |
| Asset score | 0.73(0.58,0.9) | 0.00 | 0.81 (0.59,1.1) | 0.18 |
| HH income | ||||
| < 10,000 BDT | ||||
| 10,000–20,000 BDT | 0.6(0.34,1.07) | 0.08 | 0.48 (0.22,1.03) | 0.06 |
| > 20,000 BDT | 0.53(0.27,1.04) | 0.06 | 0.38 (0.14,1.04) | 0.06 |
OR Odds Ratio, CI Confidence Interval
In the final regression model, after adjusting for maternal age, child age and gender and household asset score, infant’s age (AOR for 2–4 months: 6.42; 95% CI: 3.42, 12.1; AOR for 4–6 months: 45.6; 95% CI 18.33, 113.45), prelacteal history (AOR 2.53; 95% CI 1.14, 4.58), not intending to exclusively breastfeed when pregnant (AOR 4.06; 95% CI 1.09, 15.12), and a cesarean delivery (AOR 2.76; 95% CI 1.34, 5.67) were all found to be risk factors for an infant not being exclusively breastfed (Table 2).
Mothers were asked if they fed their infant anything other than breastmilk since birth. Six of the 18 mothers reported exclusively breastfeeding their child. The main facilitators mentioned by the mothers were correct knowledge regarding the importance of exclusive breastfeeding, support from family, and advice and recommendation to breastfeed from health personnel (Table 3). One mother, age 19 from Korail slum, said, “. .. my parents, in-laws and neighbors also suggested me not to give anything else before six months. Sometimes I think only breastmilk is not sufficient for my baby and feel like she needs other milk or food. But I do not give other milk because doctor said not to do so” [101150]. Other facilitators mentioned by the mothers were sufficient breast milk and correct knowledge regarding the importance of exclusive breastfeeding (Table 4).
Table 3.
Barriers and facilitators for early initiation; feeding colostrum and not giving any prelacteal feeds
| Barriers | Facilitators | ||
|---|---|---|---|
| Internal | External | Internal | External |
| Thinks that breast milk become available only after 2–3 days Mother didn’t know that breast milk should be given within 1 h Put baby to breast but there was no milk secretion |
Mother was sick/unconscious took too long to bring the baby to mother after surgery Mother had difficulties to hold the baby to feed after surgery It took too long to clean the baby child was very sleepy child didn’t demand |
If mother is well Mother knew about early initiation Previous experience Knew colostrum should be given Mother trained from NGO |
Normal delivery Midwives assist to put baby on the breast Grandmother/other family member/ doctor/ midwives suggest to give breast milk as early as possible Heard this from health workers/TV/ text book |
| Thinks that honey (clear voice/prevent cold), mustard oil (to clear mouth and throat), sugar water (to clear cough) is required Did not know that other substance Should not be given no breastmilk before 3 days after delivery |
Midwives suggested honey Grandmother gave what she feels better for the child Mother was sick/unconscious Doctor /nurse/midwives prescribed infant formula Grandmother gave sugar water as believed breast milk was insufficient Child was crying too much |
Thinks only colostrum should be given up to 3 days after birth Knew that baby should not be given anything except breast milk |
Doctor/ nurse/ midwives suggest not to give anything but breast milk Another wet nurse mother fed baby when mother was sick |
Table 4.
Perceived barriers and facilitators for exclusive breastfeeding
| Barriers | Facilitators | ||
|---|---|---|---|
| Internal | External | Internal | External |
| Insufficient breast milk (thinks due to inadequate diet of mother, medicine after surgery, infrequent feeding) Mother left for work Thinks baby should drink water as it feels thirsty Thinks complementary food should start after 4 months |
Grandmother did not allow breastfeeding Doctor prescribed formula Bottle feeding Maternity leave < 6 months No crèche at the workplace Workload does not permit to breastfeed at workplace |
Mother knew that child should be given only breastmilk up to 6 months Knew that other food is harmful for child health Sufficient breastmilk -Thinks breastmilk is best for baby |
Doctor suggest that baby should not be given anything else before 6 months Breast milk is free of cost Grandmother/family member helps in household work Husband support breastfeeding -bottle feeding is hazardous in terms of preparation |
Moreover, 12 of the 18 mothers interviewed reported failing to exclusively breastfeed for the first 6 months of the infant’s life. The majority of the mothers reported the perception of insufficient breastmilk as the main barrier towards exclusive breastfeeding, and mothers voiced that the infant’s cry was an indication of insufficient breastmilk. Reasons behind breastmilk insufficiency perceived by the mothers was inadequate maternal consumption of food, medicine taken after surgery, and infrequent breastfeeding. All eight mothers who had a cesarean section did not exclusively breastfeed. One mother, age 22 from Sattala slum explained, “I cannot give my baby only breast milk because after cesarean section I took antibiotics and my breast milk dried up. Baby does not get sufficient breast milk and cries a lot. Then I started Lactogen [formula]. .. baby does not want to suck the breast when there is insufficient milk” [102115]. Of the 12 mothers who did not exclusively breastfeed, nine provided their infant with formula. Seven of the 12 mothers fed their infant water, and these mothers noted the importance of exclusive breastfeeding but believed their infant was dehydrated and therefore needed water. An additional two mothers reported not being able to exclusively breastfeed due to their employment status.
Discussion
This mixed method study investigated not only the status of infant feeding practices and the associated factors, but it also uncovered the main facilitators and barriers behind such practices among mothers with infants under 6 months in the slums of Dhaka, Bangladesh. The study found that one fourth of mother had a cesarean section, and this type of delivery impacted early initiation of breastfeeding, colostrum administration, and exclusive breastfeeding. Moreover, mothers who delivered by cesarean section qualitatively explained their inability to abide by early infant feeding best practices due to their unconsciousness, sickness, pain, and prescription medication post-surgery and the subsequent need to supplement breastfeeding due to delayed or inadequate milk production.
Early initiation of breastfeeding was found to be slightly higher in our study than compared to overall national average from BDHS 2014, 64.2% and 50.8%, respectively [8]. Qualitative study found only seven out of 18 mothers initiate breastfeeding within 1 h. Of the 11 mothers who did not, eight qualitatively said they failed to because of the cesarean section. This finding echoes the 2016 finding that only 37.7% of mothers who delivered in a health facility in Bangladesh initiated within 1 h [8], which may be reflective of type of delivery. Analysis of national survey data in Nepal showed that cesarean delivery is one of the risk factors for delayed initiation of breastfeeding [32]. Delayed breastfeeding initiation has also been experienced by women who had a cesarean section in other research as well [33–36]. Maternal inability to breastfeed their child just after surgery delayed the early initiation and promoted introduction of prelacteal feeds. Moreover, breastfeeding initiation within 1 h after delivery has also been found to be a predictor of breastfeeding continuation [37–39].
As seen in other studies, 96.5% of the infants in this study were fed colostrum, yet in the qualitative analysis only nine out of 18 mothers did so. Colostrum feeding was supplemented by prelacteal feeding practices, as has been found in previous studies [22, 40]. Honey and sugar water were most widely reported prelacteal feeds given to the infants in this study. In South East Asia this a common practice to use these foods as a first thing to be provided to infants after birth [22, 40, 41]. These are also widely used as prelacteal feeds in rural Bangladesh [22, 40]. We found that infants who received prelacteal feeds were 2.5 times higher risk of not being exclusively breastfed. Prelacteal administration was also reported as a risk factor for failure to exclusively breastfed in previous studies both in Bangladesh and in other developing countries [14, 42].
Prevalence of exclusive breastfeeding in the Dhaka’s slums was found to be lower (36%) than the national prevalence (55%) of exclusive breastfeeding [8]. However, this finding is consistent with the findings from other studies in rural and slum area of Bangladesh [13, 43]. As this study found, another cross-sectional study in rural Bangladesh found a negative association between cesarean delivery and exclusive breastfeeding [13]. In-depth interviews revealed that most of the mothers (12 out of 18) reported insufficient breast milk production as one of the main reasons for being unable to exclusively breastfeed. This was the case mentioned in other formative research done in Bangladesh [40]. Moreover, all of the eight mothers within the qualitative portion of the study who had a cesarean delivery did not exclusively breastfeed their child. Inability to buy/eat nutritious food and intake of medicine after surgery was mentioned as additional reasons for insufficient breast milk which is a misconception of mothers. Only one mother correctly mentioned that after surgery infrequent feeding of her child lead to insufficient breast milk which she realized later but by that time her child became habituated to bottle feeding. This maternal perception was also reported from rural Bangladesh and from different age groups [22]. With the increasing rate of cesarean delivery nationally, it is an alarming risk for optimal early infant feeding practices. Proper implementation of Baby Friendly Hospital Initiative could be one the solutions to combat this challenge [11, 17]. Additionally, post-cesarean pain management and assisted breastfeeding initiation is believed to be helpful in improving EBF rates.
A few limitations within this study need to be noted. The definition of EBF used here according to 24 h-recall period is subject to bias and misreporting. Additionally, the data collection was conducted during the heat of summer. Therefore, maternal perception of her infant’s thirst and subsequent administration of water may have been higher than normal.
Conclusions
Early infant feeding practices among urban slum dwelling mothers in Dhaka, Bangladesh was found to be lower than the universal levels recommended by the WHO. Moreover, this study found that the cesarean section rate (25.1%) among these mothers was higher than the optimal rate for caesarean sections (10–15%) as put forth by the WHO. Cesarean delivery was found to be associated with failure to exclusively breastfeed and qualitative findings highlighted the difficulty surrounding cesarean delivery and adhering to recommended early infant feeding practices due to this type of delivery. This finding should be studied in greater depth to understand the national impact of increasing caesarean section delivery rates and the impact on early infant feeding practices as well as maternal and infant immediate and long term health.
Acknowledgements
This research project was conducted with support from Nutrition and Clinical Services Division, icddrb. We acknowledge core donors which provide unrestricted support to icddr,b for its operations and research. Icddr,b gratefully acknowledges the following donors which provide unrestricted support: Governments of the People’s Republic of Bangladesh, Canada, Sweden and the UK for providing core/unrestricted support. We gratefully acknowledge these donors for their support and commitment to icddr,b’s research efforts.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author [NC]. The data are not publicly available due to restriction according to data policy of icddr,b. The policy of icddr,b is that we should not make the availability of whole data set in the manuscript, the supplemental files, or a public repository. Institutional Review Board (IRB) of icddr,b has restrictions to disclose any personal information of the participants, and on the basis of this recommendation by the IRB, the Research & Clinical Administration and Strategy (RCAS) of icddr,b has imposed these restrictions. However, it is declared and confirmed that the part of data set related to this manuscript is available upon request.
Abbreviations
- ANC
Antenatal care
- AOR
Adjusted Odds Ratio
- BMI
Body Mass Index
- CS
Cesarean Section
- EBF
Exclusive breastfeeding
- FANTA
Food and Nutrition Technical Assistance
- icddr,b
International Centre for Diarrhoeal Disease Research, Bangladesh
- LMICs
low and middle income countries
- MDD
Maternal Dietary Diversity
- NCSD
Nutrition and Clinical Services Division
- NVD
Normal Vaginal Delivery
- OR
Odds Ratio
- ORS
Oral Rehydration Solution
- WHO
Word Health Organization
Authors’ contributions
CC and RS conceived the research idea; TA, NC, MMI and HK contributed in development of study design. HK and NC conducted the data analysis; CC and RS assisted data analysis. HK and CC summarized the findings. CC and HK drafted the manuscript. NC, MMI and TA gave critical input to finalize the manuscript. All authors reviewed and approved the final manuscript.
Ethics approval and consent to participate
This study was approved by the icddr,b Research Review Committee and Ethical Review Committee (Protocol number PR#16022). Informed written consent was obtained from all participants prior to the interview.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Halima Khatun, Email: Halima.khatun.runa@gmail.com.
Carly A Comins, Email: carlyacomins@gmail.com.
Rajesh Shah, Email: rajesh_sah004@yahoo.com.
M Munirul Islam, Email: mislam@icddrb.org.
Nuzhat Choudhury, Email: nuzhat@icddrb.org.
Tahmeed Ahmed, Email: tahmeed@icddrb.org.
References
- 1.Sankar MJ, Sinha B, Chowdhury R, Bhandari N, Taneja S, Martines J, Bahl R. Optimal breastfeeding practices and infant and child mortality: a systematic review and meta-analysis. Acta Paediatr. 2015;104(S467):3–13. doi: 10.1111/apa.13147. [DOI] [PubMed] [Google Scholar]
- 2.Peres KG, Cascaes AM, Nascimento GG, Victora CG. Effect of breastfeeding on malocclusions: a systematic review and meta-analysis. Acta Paediatr. 2015;104(S467):54–61. doi: 10.1111/apa.13103. [DOI] [PubMed] [Google Scholar]
- 3.Lodge C, Tan D, Lau M, Dai X, Tham R, Lowe A, Bowatte G, Allen K, Dharmage S. Breastfeeding and asthma and allergies: a systematic review and meta-analysis. Acta Paediatr. 2015;104(S467):38–53. doi: 10.1111/apa.13132. [DOI] [PubMed] [Google Scholar]
- 4.Horta BL, Loret de Mola C, Victora CG. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta-analysis. Acta Paediatr. 2015;104(S467):30–37. doi: 10.1111/apa.13133. [DOI] [PubMed] [Google Scholar]
- 5.Horta BL, Loret de Mola C, Victora CG. Breastfeeding and intelligence: a systematic review and meta-analysis. Acta Paediatr. 2015;104(S467):14–19. doi: 10.1111/apa.13139. [DOI] [PubMed] [Google Scholar]
- 6.Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N, Rollins NC. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–490. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 7.Cai X, Wardlaw T, Brown DW. Global trends in exclusive breastfeeding. Int Breastfeed J. 2012;7:12. doi: 10.1186/1746-4358-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Institute of Population Research and Training (NIPORT), and MaA International I: 2015 . Bangladesh demographic and health survey 2014: key indicators. 2015. [Google Scholar]
- 9.National Institute of Population Research and Training (NIPORT), International Center for Diarrheal Disease Research (icddr b),MEASURE Evaluation. M . Bangladesh urban health survey 2013 final report NIPORT, Icddr,b and MEASURE evaluation. 2015. [Google Scholar]
- 10.Ambikapathi R, Kosek MN, Lee GO, Mahopo C, Patil CL, Maciel BL, Turab A, Islam MM, Ulak M, Bose A, et al. How multiple episodes of exclusive breastfeeding impact estimates of exclusive breastfeeding duration: report from the eight-site MAL-ED birth cohort study. Maternal & Child Nutrition. 2016;12(4):740–756. doi: 10.1111/mcn.12352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sinha B, Chowdhury R, Sankar MJ, Martines J, Taneja S, Mazumder S, Rollins N, Bahl R, Bhandari N. Interventions to improve breastfeeding outcomes: a systematic review and meta-analysis. Acta Paediatr. 2015;104(S467):114–134. doi: 10.1111/apa.13127. [DOI] [PubMed] [Google Scholar]
- 12.Elaine AY, Thomas JS, Owais A, Tirmizi N, Faruque A, Das SK, Rahman S, Schwartz B, Stein AD. Maternal prenatal attitudes and postnatal breast-feeding behaviours in rural Bangladesh. Public Health Nutr. 2015;18(04):679–685. doi: 10.1017/S1368980014000937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sundaram ME, Labrique AB, Mehra S, Ali H, Shamim AA, Klemm RD, West KP, Christian P. Early neonatal feeding is common and associated with subsequent breastfeeding behavior in rural Bangladesh. J Nutr. 2013;143(7):1161–1167. doi: 10.3945/jn.112.170803. [DOI] [PubMed] [Google Scholar]
- 14.Kim MJ, Kim YM, Yoo JH. Factors affecting exclusive breast-feeding during the first 6 months in Korea. Pediatrics international : official journal of the Japan Pediatric Society. 2013;55(2):177–180. doi: 10.1111/ped.12004. [DOI] [PubMed] [Google Scholar]
- 15.Hall J. Effective community-based interventions to improve exclusive breast feeding at four to six months in low- and low-middle-income countries: a systematic review of randomised controlled trials. Midwifery. 2011;27(4):497–502. doi: 10.1016/j.midw.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 16.Sasaki Y, Ali M, Kakimoto K, Saroeun O, Kanal K, Kuroiwa C. Predictors of exclusive breast-feeding in early infancy: a survey report from Phnom Penh, Cambodia. J Pediatr Nurs. 2010;25(6):463–469. doi: 10.1016/j.pedn.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 17.Kristiansen AL, Lande B, Overby NC, Andersen LF. Factors associated with exclusive breast-feeding and breast-feeding in Norway. Public Health Nutr. 2010;13(12):2087–2096. doi: 10.1017/S1368980010002156. [DOI] [PubMed] [Google Scholar]
- 18.Tiwari R, Mahajan PC, Lahariya C. The determinants of exclusive breast feeding in urban slums: a community based study. J Trop Pediatr. 2009;55(1):49–54. doi: 10.1093/tropej/fmn037. [DOI] [PubMed] [Google Scholar]
- 19.Santo LCE, De Oliveira LD, Giugliani ERJ. Factors associated with low incidence of exclusive breastfeeding for the first 6 months. Birth. 2007;34(3):212–219. doi: 10.1111/j.1523-536X.2007.00173.x. [DOI] [PubMed] [Google Scholar]
- 20.Joshi PC, Angdembe MR, Das SK, Ahmed S, Faruque ASG, Ahmed T. Prevalence of exclusive breastfeeding and associated factors among mothers in rural Bangladesh: a cross-sectional study. Int Breastfeed J. 2014;9(1):7. doi: 10.1186/1746-4358-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Betrán AP, Ye J, Moller A-B, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PLoS One. 2016;11(2):e0148343. doi: 10.1371/journal.pone.0148343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hackett KM, Mukta US, Jalal CS, Sellen DW. A qualitative study exploring perceived barriers to infant feeding and caregiving among adolescent girls and young women in rural Bangladesh. BMC Public Health. 2015;15:771. doi: 10.1186/s12889-015-2115-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hackett KM, Mukta US, Jalal CS, Sellen DW. Knowledge, attitudes and perceptions on infant and young child nutrition and feeding among adolescent girls and young mothers in rural Bangladesh. Maternal & Child Nutrition. 2015;11(2):173–189. doi: 10.1111/mcn.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matsuyama A, Karama M, Tanaka J, Kaneko S. Perceptions of caregivers about health and nutritional problems and feeding practices of infants: a qualitative study on exclusive breast-feeding in Kwale, Kenya. BMC Public Health. 2013;13:525. doi: 10.1186/1471-2458-13-525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moran AC, Choudhury N, Khan NUZ, Karar ZA, Wahed T, Rashid SF, Alam MA. Newborn care practices among slum dwellers in Dhaka, Bangladesh: a quantitative and qualitative exploratory study. BMC Pregnancy and Childbirth. 2009;9:54. doi: 10.1186/1471-2393-9-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hossain M, Islam A, Kamarul T, Hossain G. Exclusive breastfeeding practice during first six months of an infant’s life in Bangladesh: a country based cross-sectional study. BMC Pediatr. 2018;18(1):93. doi: 10.1186/s12887-018-1076-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Organization WH: Indicators for assessing infant and young child feeding practices: part 1: definitions: conclusions of a consensus meeting held 6–8 November 2007 in Washington DC, USA. 2008.
- 28.Fund PAHOUNCs . ProPAN: Process for the Promotion of Child Feeding. 2. ed. Washington, D.C: PAHO; 2013. [Google Scholar]
- 29.National Institute of Mental H, Hospital, Bangladesh WHO: Prevalence, medical care, awareness, and attitude towards mental illness in Bangladesh, vol. 20 (1). [Dhaka]: Bangladesh journal of psychiatry 2006.
- 30.Institute of Public Health Nutrition MoHaFW, Government of the People’s Republic of Bangladesh, United Nations Children’s Fund UNICEF H, 3 United Nations Plaza, New York, New York 10017, U.S.A., World Food Programme, United Nations, Via C.G.Viola 68 PdM, 00148, Rome, Italy Bangladesh Household Food Security and Nutrition Assessment Report 2009. 2009.
- 31.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code for Biology and Medicine. 2008;3(1):17. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fenske N, Burns J, Hothorn T, Rehfuess EA. Understanding child stunting in India: a comprehensive analysis of socio-economic, nutritional and environmental determinants using additive quantile regression. PLoS One. 2013;8(11):e78692. doi: 10.1371/journal.pone.0078692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pandey S, Tiwari K, Senarath U, Agho KE, Dibley MJ. Determinants of infant and young child feeding practices in Nepal: secondary data analysis of demographic and health survey 2006. Food & Nutrition Bulletin. 2010;31(2):334–351. doi: 10.1177/156482651003100222. [DOI] [PubMed] [Google Scholar]
- 34.Regan J, Thompson A, DeFranco E. The influence of mode of delivery on breastfeeding initiation in women with a prior cesarean delivery: a population-based study. Breastfeed Med. 2013;8(2):181–186. doi: 10.1089/bfm.2012.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Watt S, Sword W, Sheehan D, Foster G, Thabane L, Krueger P, Landy CK. The effect of delivery method on breastfeeding initiation from the the Ontario mother and infant study (TOMIS) III. J Obstet Gynecol Neonatal Nurs. 2012;41(6):728–737. doi: 10.1111/j.1552-6909.2012.01394.x. [DOI] [PubMed] [Google Scholar]
- 36.Dewey K. G., Nommsen-Rivers L. A., Heinig M. J., Cohen R. J. Risk Factors for Suboptimal Infant Breastfeeding Behavior, Delayed Onset of Lactation, and Excess Neonatal Weight Loss. PEDIATRICS. 2003;112(3):607–619. doi: 10.1542/peds.112.3.607. [DOI] [PubMed] [Google Scholar]
- 37.Rowe-Murray HJ, Fisher JR. Baby friendly hospital practices: cesarean section is a persistent barrier to early initiation of breastfeeding. Birth. 2002;29(2):124–131. doi: 10.1046/j.1523-536X.2002.00172.x. [DOI] [PubMed] [Google Scholar]
- 38.Meedya S, Fahy K, Kable A. Factors that positively influence breastfeeding duration to 6 months: a literature review. Women and Birth. 2010;23(4):135–145. doi: 10.1016/j.wombi.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 39.Organization WH, Unicef . Baby-friendly hospital initiative: revised, updated and expanded for integrated care. 2009. [PubMed] [Google Scholar]
- 40.Organization WH, UNICEF . Global strategy for infant and young child feeding: World Health Organization. 2003. [Google Scholar]
- 41.Haider R, Rasheed S, Sanghvi TG, Hassan N, Pachon H, Islam S, Jalal C. Breastfeeding in infancy: identifying the program-relevant issues in Bangladesh. Int Breastfeed J. 2010:521. [DOI] [PMC free article] [PubMed]
- 42.Rahi M, Taneja D, Misra A, Mathur N, Badhan S. Newborn care practices in an urban slum of Delhi. Indian J Med Sci. 2006;60(12):506. doi: 10.4103/0019-5359.28980. [DOI] [PubMed] [Google Scholar]
- 43.Patil CL, Turab A, Ambikapathi R, Nesamvuni C, Chandyo RK, Bose A, Islam MM, Ahmed AM, Olortegui MP, de Moraes ML, et al. Early interruption of exclusive breastfeeding: results from the eight-country MAL-ED study. Journal of Health, Population, and Nutrition. 2015;34(1):10. doi: 10.1186/s41043-015-0004-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author [NC]. The data are not publicly available due to restriction according to data policy of icddr,b. The policy of icddr,b is that we should not make the availability of whole data set in the manuscript, the supplemental files, or a public repository. Institutional Review Board (IRB) of icddr,b has restrictions to disclose any personal information of the participants, and on the basis of this recommendation by the IRB, the Research & Clinical Administration and Strategy (RCAS) of icddr,b has imposed these restrictions. However, it is declared and confirmed that the part of data set related to this manuscript is available upon request.


