Abstract
Background and Objectives:
Patients who undergo colorectal surgery have high postoperative morbidity, with ileostomates being the most disadvantaged. Recent studies assessing readmission risk factors do not provide a specific prediction model and, if so, do not focus on patients who have had colorectal surgery; thus, the results of these studies have limited applicability to our specialized practice. We wanted to develop a prediction model for readmission within 30 days of discharge after ileostomy creation.
Methods:
Patients who underwent elective ileostomy creation from 2013 to 2016 at the University of Florida were included in this retrospective study. Factors significantly associated with readmission within 30 days after discharge were identified by comparing a cohort that was readmitted within 30 days with one that was not. A practical, predictive model that stratified a patient's risk of readmission after the index procedure was developed.
Results:
A total of 86 iliostomates were included; of those, 22 (26%) were readmitted within 30 days. Factors significantly associated with readmission included preoperative steroid use, history of diabetes, history of depression, lack of a hospital social worker or postoperative ostomy education, and the presence of complications after the index procedure. A model predicting readmission within 30 days of discharge that comprised the first 4 factors was developed, with a sensitivity of 73% and a specificity of 77%.
Conclusion:
Prediction of readmission in patients who undergo ileostomy creation is possible, suggesting interventions addressing predictive factors that may help decrease the readmission rate. Prospective validation of the model in a larger cohort is needed.
Keywords: Outcome, Prediction model, Social worker, Steroid
INTRODUCTION
Approximately 600,000 patients undergo colorectal surgery annually in the United States, with an estimated 120,000 patients needing ileostomy creation.1,2 It is widely accepted that colorectal surgery has higher postoperative morbidity than noncolorectal procedures. However, the subcohort of patients with ileostomy is gaining increasing national attention because of the poorer outcomes. Although historical readmission rates for colorectal surgery range from 10% to 30%, they are much higher (up to 65%) in patients with a new ileostomy.3–5 Complications, such as bowel obstruction, surgical site infection (SSI), intra-abdominal abscess, dehydration, and stoma-related complications, have been found to be responsible for most readmissions after ileostomy creation.6 The unique challenges of this population are exacerbated by fast-track protocols; early discharge of new ileostomates continues to elicit concern for readmission risk and associated morbidity.
Because readmission within 30 days of discharge is closely scrutinized as an outcome measure and surrogate of quality with financial implications, efforts to reduce them are needed, but proven strategies are sparse.3,7,8 Objective criteria predicting the risk of readmission in this unique patient population are lacking. Current studies assessing risk factors do not provide a specific predictive model and if so, do not focus on patients who have had colorectal surgery, with limited applicability to our specialized practice.9–11 Therefore, we wanted to develop a model for predicting readmission within 30 days of discharge after elective ileostomy creation. Future efforts could then be focused on mitigating readmissions by influencing modifiable factors identified in our model.
MATERIALS AND METHODS
Patient Selection
All patients who underwent elective ileostomy during a colorectal procedure from May 2013 to January 2016 at University of Florida (UF) Health were identified and included in this single-center, retrospective cohort study. All procedures were performed by 1 of the 2 high-volume, colorectal-surgery–trained, board-certified surgeons. Patients with any missing data or those who had had additional noncolorectal procedures at the time of the index operation were excluded. Modifiable and nonmodifiable factors associated with readmission within 30 days of discharge after the index hospitalization were identified, and a practical predictive model for stratifying the patient's risk of readmission was developed. This study was approved by the UF Institutional Review Board and informed consent was waived. The study was also registered with the research registry (UIN 3356).
Predictive Factors Analyzed
Variables analyzed for correlation to readmission included (A) baseline factors: age, gender, body mass index (BMI), marital status, primary insurance, primary language, distance to hospital, and mobility status; (B) preoperative factors: smoking, steroid use, Charlson comorbidity index, comorbidities (31 individual comorbidities assessed), American Society of Anesthesiologists (ASA) score, diagnosis leading to surgery, presence of malignancy, use of anticoagulants, request for medical and cardiac clearance, discussion with family regarding high operative risk, and ostomy marking; (C) operative details for index procedure: surgical procedure, year of surgery, surgical approach (open, laparoscopic, or robotic), and reason for ostomy creation; (D) postoperative factors: ostomy teaching, weekdays versus weekend teaching, implementation of enhanced recovery after surgery protocol (ERAS), narcotic use, time to diet advancement, time between diet and discharge, a hospital social worker's assistance in planning for discharge, weekday or weekend discharge, social and family support at home (full-time vs part-time), phone calls by patient after discharge, weekday or weekend readmission, length of index hospital stay, and cost of index hospitalization; and (E) complications after index procedure: urinary retention, deep space SSI, ileus, bowel obstruction, and high ileostomy output.
Outcomes Assessed
Outcome variables included readmission, length of readmission stay, cost of readmission, and duration between discharge and readmission. If the readmission was caused by dehydration or high ostomy output, the following factors were assessed at various time points during the index hospitalization and at discharge: volumes of ostomy output, intravenous fluids (IVF), and urine output per day; time of IVF discontinuation relative to discharge; oral intake per day at discharge; ostomy output per day at discharge; electrolyte intake; and serum creatinine. In addition, the following factors were assessed upon readmission: volumes of ostomy, IVF, and urine output per day; electrolytes; serum creatinine.
Cost Analysis
Costs comprising both direct and indirect costs for the index hospitalization were obtained and defined in U.S. dollars. Direct costs were calculated to reflect the actual incurred expense. Indirect costs were obtained, and a stepdown method was used to allocate indirect costs to the patient. (For example, the finance department utility costs were allocated to the finance department before the total costs were allocated to the hospitalization and other direct cost centers.)
Statistical Analysis
SPSS software was used for statistical analysis (SPSS Statistics for Windows, Version 21.0; IBM, Armonk, NY, USA). Student's t test, ANOVA and χ2 and Fisher's exact tests were used for statistical analysis, as appropriate. Univariate analysis followed by a stepwise multivariate logistic regression was used to identify a best-fit model for developing a model for prediction of readmission within 30 days after discharge. The research herein is reported in line with criteria for Strengthening the Reporting of Cohort Studies in Surgery (STROCSS).12
RESULTS
Patient Population
A total of 86 patients who underwent creation of an ileostomy during the study period were included. There was an equal number of men and women (43 each) with a mean age of 54 years and mean BMI of 26 kg/m2. Most patients had private insurance (45%) or Medicare (41%), whereas a minority had Medicaid (10%) or were uninsured (4.5%). Most patients were ambulatory (89%), and a minority were dependent (5.8%) or wheelchair or bed bound (4.6%). Most patients had an ASA score of 3 (73%); the rest were ASA 2 (17%) and ASA 4 (9%). The mean Charlson comorbidity index was 2.4, and preoperative medical clearance related to comorbidities was obtained in 39%. All patients had an ileostomy for proximal diversion of a distal anastomosis either from a low anterior resection (LAR) (64%) or ileoanal anastomosis (36%). The underlying reasons for resection were colorectal malignancy (53%), inflammatory bowel disease (IBD) (27%), and other benign causes (20%). The average time for diet inception after the index procedure was postoperative day 2.7, whereas the average time between diet inception and discharge was 5.5 days. The average length of stay after the index procedure (ileostomy creation) was 9.3 days, with a mean cost of $30,918.
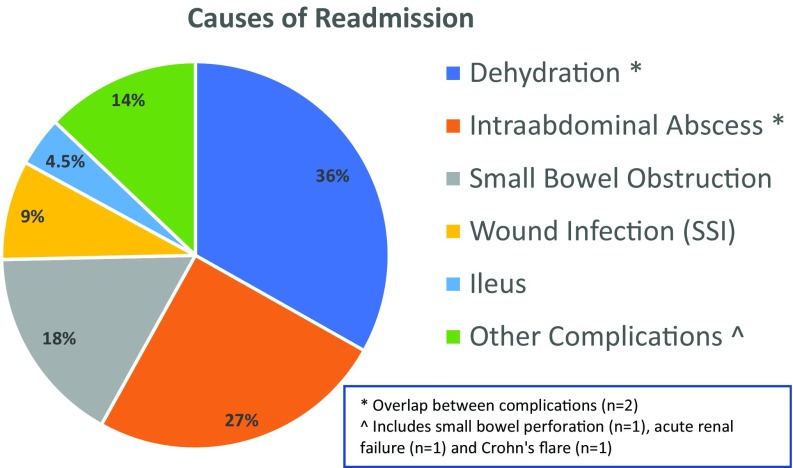
Twenty-two patients (26%) were readmitted within 30 days after discharge after the index procedure. Mean time interval from discharge to readmission was 8.5 days, with one-fifth of the patients (20%) readmitted on weekends. The average length of hospital stay for readmission was 5 days, at a cost of $13,839. Readmissions were most commonly caused by dehydration from high ostomy output (36%), deep space SSI (27%), or small bowel obstruction (18%), as depicted in Figure 1. Baseline characteristics of the patients who were and were not readmitted were similar (Table 1).
Figure 1.
Causes of postoperative readmission within 30 days of discharge.
Table 1.
Comparison of Baseline Characteristics in the Nonreadmitted Versus the Readmitted Groups
| Baseline Characteristics | Not Readmitted Group (Mean) | Readmitted Group (Mean) | P |
|---|---|---|---|
| Age (years) | 54 | 52 | .67 |
| Gender (% male) | 48 | 54 | .82 |
| BMI (kg/m2) | 26 | 27 | .69 |
| Marital status (% married) | 20 | 41 | .46 |
| Mobility status (%) | |||
| Ambulatory | 90 | 86 | .87 |
| Dependent | 5.3 | 9.1 | .82 |
| Wheelchair/bedbound | 4.7 | 4.9 | .92 |
Factors Associated with Postoperative Readmission Within 30 Days of Discharge
A comparison was made of 69 pre-, intra- and postoperative variables in the patients who were and were not readmitted (Table 2). Of all variables analyzed, the following factors were associated with a significantly higher rate of readmission: preoperative steroid use, history of diabetes, history of depression, lack of formal postoperative ostomy education, and lack of discharge planning by a social worker. In addition, development of complications during the index hospitalization, such as bowel obstruction, high ostomy output, deep space SSI, urinary retention, and other complications (small bowel perforation, Crohn's disease flare, and acute renal failure) were significantly associated with readmission, as shown in Table 2. Of note, an attempt was made to wean all patients from steroids before surgery; however, 7 patients (8%) had to continue low-dose steroids (<10 mg/day prednisone) because of prolonged steroid use and inability to wean. Inability to wean from steroids was not an indication alone for proximal diversion but was analyzed as a predictive factor for readmission.
Table 2.
Comparison of Predictive Factors in the Readmitted Versus Nonreadmitted Groups
| Factors Analyzed | Not Readmitted Group (Mean) | Readmitted Group (Mean) | P |
|---|---|---|---|
| Preoperative Factors | |||
| ASA score, % | |||
| II | 20 | 9% | .07 |
| III | 67 | 91 | |
| IV | 13 | 0 | |
| Charlson comorbidity index | 2.37 | 2.54 | .75 |
| Smoking (%) | 19 | 14 | .75 |
| Steroid use (%) | 3 | 23 | .04 |
| History of diabetes (%) | 8 | 27 | .04 |
| History of depression (%) | 17 | 32 | 0.03 |
| Diagnosis (%) | |||
| Malignancy | 52 | 54 | 0.87 |
| Benign IBD | 30 | 25 | 96 |
| Benign non-IBD | 18 | 21 | 0.95 |
| Anticoagulant use (%) | 94 | 95 | .99 |
| Request for medical/cardiac clearance (%) | 37 | 45 | .68 |
| Discussion with family regarding high operative risk (%) | 17 | 18 | .00 |
| Ostomy marking/education with stoma nurse (%) | 89 | 91 | .00 |
| Distance to hospital (miles) | 25 | 80 | .06 |
| Operative Factors (Index Procedure) | |||
| Procedure (%) | |||
| LAR with coloanal anastomosis | 60 | 68 | .67 |
| Total proctocolectomy with ileoanal anastomosis | 40 | 32 | |
| Surgical approach (%) | |||
| Open | 37 | 41 | .83 |
| Laparoscopic | 49 | 50 | |
| Robotic | 14 | 9 | |
| Reason for ileostomy creation (%) | |||
| Low pelvic coloanal anastomosis | 60 | 68 | .67 |
| Ileoanal anastomosis | 40 | 32 | |
| Postoperative Factors | |||
| Formal ostomy teaching (%) | |||
| Performed | 95 | 70 | .04 |
| Weekend teaching | 40 | 0a | .03 |
| ERAS protocol implemented (%) | 50 | 60 | .34 |
| Time to diet advancement (postoperative days) | 2.9 | 1.9 | .46 |
| Time between diet advancement and discharge (postoperative days) | 4.9 | 6.9 | .29 |
| Social worker planning for discharge (%) | 82 | 57 | .05 |
| Weekend discharge (%) | 30 | 6 | .06 |
| Social/family support at home (%) | |||
| Full-time | 68 | 77 | .77 |
| Part-time | 18 | 9 | .09 |
| Phone calls by patient after discharge (% yes) | 51 | 64 | .46 |
| Length of index hospital stay (days) | 9.0 | 10.1 | .57 |
| Cost of index hospitalization ($) | 30,412 | 32,393 | .71 |
| Complications during index admission (%) | |||
| High ostomy output | 17 | 46 | .02 |
| Small bowel obstruction | 2 | 18 | .01 |
| SSI | 3 | 9 | .27 |
| Deep space infection/abscess | 5 | 32 | .002 |
| Ileus | 6 | 18 | .19 |
| Urinary Retention | 6 | 27 | .02 |
| Other Complications | 19 | 68 | .0001 |
Bold P-values indicate statistically significant differences (P < .05).
an = 1 in the weekend group that got readmitted.
Readmission for Dehydration
Since dehydration was the most common cause of readmission, a subgroup analysis to identify factors specifically associated with a readmission for dehydration was performed. None of the 16 factors studied achieved significance.12 These included time-to-diet inception, time to discharge, time to discontinuation of IVF, oral liquid intake, ileostomy output, and urine output at different time points before discharge (24 and 48 h before discharge) and laboratory evaluation before discharge from the index procedure. However, upon readmission, the patients had a significantly higher white blood cell count, serum blood urea nitrogen level, and a lower sodium level, consistent with dehydration.12 Patients also needed significantly more IVF upon readmission.
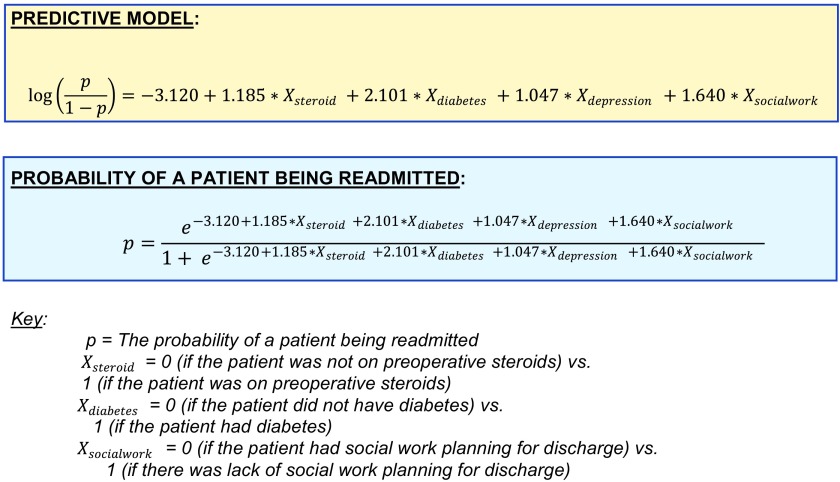
Prediction Model for Postoperative Readmission Within 30 Days of Discharge
A model of postoperative readmission within 30 days of discharge was created (Figure 2), with a sensitivity of 73% and specificity of 77% was created. The factors associated with readmission in the final model were preoperative use of steroids (OR 3.27), preoperative history of depression (OR 2.85), preoperative history of diabetes (OR 3.34), and lack of a social worker planning for discharge after the index procedure (OR 5.15), as shown in Table 3.
Figure 2.
Prediction model for readmission within 30 days of discharge after ileostomy.
Table 3.
Practical Interpretation of the Effect of Predictors in the Model on Readmission
| Predictor Variable | Parameter Estimatea | Increase in Risk of Readmission, If Present | Interpretationb |
|---|---|---|---|
| Steroid use | 1.185 | 3.27-fold | Patients using steroids have a 3.27-fold increase in readmission risk over those not using steroids. |
| History of diabetes | 1.206 | 3.34-fold | Patient with diabetes have a 3.34-fold increase in readmission risk over those without diabetes. |
| History of depression | 1.047 | 2.85-fold | Patients with depression have a 2.849-fold increase in readmission risk over those without depression. |
| Lack of case worker planning for discharge | 1.640 | 5.15-fold | Patients who have no social worker planning for discharge have a 5.155-fold higher readmission risk over a patient who had a social worker planning for discharge. |
aIntercept was −3.120. Thus, the average probability of readmission for a patient who does not use steroids, does not have diabetes and depression, and has a social worker planning for discharge is 4.416%.
bProvided all other predictor variables in the equation are held constant.
DISCUSSION
Readmission rates for patients who undergo colorectal surgery range from 10% to 30%,3,4 which is consistent with our overall colorectal surgery readmission rate (18%) for the study period. However, readmission rates for ileostomates are reported to be as high as 65% and often are not stated in the literature.5 We have published our efforts to reduce the readmission rate in this patient population.5 Other centers have reported success with different novel outpatient approaches to the same concern.13 However, with the intensification of financial pressure on health care systems to avoid readmission after the enactment of the Affordable Care Act of 2010, an objective method of predicting readmissions in this population was needed. This study highlights the causes of and the factors associated with readmission for patients who undergo creation of an ileostomy at a high-volume tertiary care center. We also developed a prediction model for readmission within 30 days of discharge specific to this patient subset, which highlights the role of preoperative optimization of patient's comorbidities, weaning them off steroids, and formal involvement of ostomy nurses and social workers in the discharge planning process.
Our findings agree with an validate those of previous studies, as preoperative steroid use, history of diabetes or depression, and complications after the index procedure have been individually identified as risk factors for readmission after general surgery procedures.9–11 A new ileostomy and steroid use were identified as a risk factor for readmission in other patients such as those with IBD,14 as was the case in our study. A recent systematic review identified older age, presence of comorbidities, preoperative immunosuppression, and postoperative complications as risk factors for readmission within 30 days of discharge.11 The Centers for Medicare and Medicaid Services (CMS) has also identified risk factors associated with readmission,15 but the data are not disease or specialty specific. CMS limits clinical relevance to individual practitioners, beyond overcoming reimbursement challenges.
Our study builds upon previously published work9–11 by focusing on colorectal surgery with elective ileostomy creation, with broader applicability to our specialized practice. We also provide an ileostomy-specific risk calculator (prediction model) for readmission within 30 days of discharge to help identify high-risk patients before surgery, improve physician counseling, and help address risk factors before surgery. Two larger studies have attempted to identify factors associated with readmission after ileostomy creation.16,17 Dehydration was the most frequent cause of readmission in one study,17 as it was in our study but was rarely seen (3%) in another study.16 Our study differs from the others by creating a model for predicting and identifying modifiable factors, influencing which ones might help reduce the readmission rate. In addition, we looked at some risk factors that are less well known, such as the involvement of stoma nurses and hospital social workers in discharge planning. While these are previously noted as possible strategies to reduce postoperative complications and improve patient satisfaction,18 their association with readmissions is not known. The presence of social support, the ability to obtain outpatient follow-up appointments, and better understanding of postoperative care have been identified as barriers after discharge.19 It is conceivable that addressing these problems during the index hospitalization would lead to fewer readmissions. In fact, lack of social worker involvement in planning for discharge was associated with the highest risk of readmission of all factors analyzed in our series (OR, 5.15).
It is interesting to note that many factors that we thought would play a role in readmissions failed to do so. These included ASA score, Charlson comorbidity index, surgical approach and procedure type, weekend discharge, social support network at home, and the number of phone calls by a patient after discharge. Implementation of a formal ERAS protocol did not affect readmission rates, consistent with the literature.20 No dehydration-specific readmission predictor was defined, despite multiple variables analyzed at various time points before discharge. Therefore, a focus on the factors identified in this study, in addition to the conventional factors above, is needed.
Potential limitations of our study include its retrospective nature and, because it was a single center study, the relatively low number of patients eligible for inclusion. However, we were ale to formulate a readmission model with good predictive power. In addition, it is plausible that differing local practices may lead to dissimilar reasons for readmission, but the predictive factors that withstood multivariate analysis and were subsequently included in the prediction model in our study are likely to be universally applicable. Moreover, we were unable to stratify our total costs into direct and indirect costs, which would change the financial impact of a readmission. For example, we did not measure societal costs related to loss of the patient's productivity because of the readmission.
CONCLUSION
Prediction of readmission in patients undergoing an elective ileostomy creation appears possible. Modification of the variables identified, such as aggressive preoperative weaning from steroid use, better preoperative control of comorbidities, dedicated postoperative ostomy education, and hospital social worker participation in discharge planning may help decrease the ileostomy-specific readmission rate. Closer follow-up for patients that have a complication (high ostomy output, small bowel obstruction, deep space SSI, and urinary retention) in the index procedure would be prudent. Prospective validation of the model in a larger cohort is needed. Development of prediction models for disease-specific subgroups is crucial in guiding insurance providers toward clinical relevance.
Contributor Information
Atif Iqbal, Departments of Surgery.
Ilya Sakharuk, University of Florida College of Medicine, Gainesville, Florida, USA..
Lindsey Goldstein, Departments of Surgery.
Sanda A. Tan, Departments of Surgery.
Peihua Qiu, Biostatistics, University of Florida, Gainesville, Florida.
Zhaomian Li, Biostatistics, University of Florida, Gainesville, Florida.
Steven J. Hughes, Departments of Surgery.
References:
- 1. Azimuddin K, Rosen L, Reed JF, Stasik JJ, Riether RD, Khubchandani IT. Readmissions after colorectal surgery cannot be predicted. Dis Colon Rectum. 2001;44:942–946. [DOI] [PubMed] [Google Scholar]
- 2. Turnbull GB. Ostomy statistics: the $64,000 question. Ostomy Wound Manage. 2003;49:22–23. [PubMed] [Google Scholar]
- 3. Paquette IM, Solan P, Rafferty JF, Ferguson MA, Davis BR. Readmission for dehydration or renal failure after ileostomy creation Dis Colon Rectum. 2013;56:974–979. [DOI] [PubMed] [Google Scholar]
- 4. Messaris E, Sehgal R, Deiling S, et al. Dehydration is the most common indication for readmission after diverting ileostomy creation. Dis Colon Rectum. 2012;55:175–180. [DOI] [PubMed] [Google Scholar]
- 5. Iqbal A, Raza A, Huang E, Goldstein L, Hughes SJ, Tan SA. Cost effectiveness of a novel attempt to reduce readmission after ileostomy creation. JSLS. 2017;Jan-Mar; 21(1):e2016.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Li LT, Mills WL, White DL, et al. Causes and prevalence of unplanned readmissions after colorectal surgery: a systematic review and meta-analysis. J Am Geriartr Soc. 2013;61:1175–1181. [DOI] [PubMed] [Google Scholar]
- 7. Datta WD, Buie AR, Maclean JA. Heine Hospital readmission rates after ileal pouch-anal anastomosis. Dis Colon Rectum. 2009;52:55–58. [DOI] [PubMed] [Google Scholar]
- 8. Bhama AR, Batool F, Collins SD, Ferraro J, Cleary RK. risk factors for postoperative complications following diverting loop ileostomy takedown. J Gastrointest Surg. 2017;21:2048–2055. [DOI] [PubMed] [Google Scholar]
- 9. Almussallam B, Joyce M, Marcello PW, et al. What factors predict hospital readmission after colorectal surgery? Am Surg. 2016;82:433–438. [PubMed] [Google Scholar]
- 10. Zhou H, Della PR, Roberts P, Goh L, Dhaliwal SS. Utility of models to predict 28-day or 30 day unplanned hospital readmissions: an updated systematic review. BMJ Open. 2016;6:e011060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alavi K, Damle RN. Risk factors for 30 day readmission after colorectal surgery: a systematic review. J Surg Res. 2016;200:200–207. [DOI] [PubMed] [Google Scholar]
- 12. Agha RA, Borrelli MR, Vella-Baldacchino M, Thavayogan R, Orgill DP, for the STROCSS Group. The STROCSS statement: Strengthening the Reporting of Cohort Studies in Surgery 2017. Int J Surg. 2017;46:198–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shaffer VO, Owi T, Kumarusamy MA, et al. Decreasing hospital readmission in ileostomy patients: results of novel pilot program. J Am Coll Surg. 2017;224:425–430. [DOI] [PubMed] [Google Scholar]
- 14. Christian KE, Jambaulikar GD, Hagan MN, et al. Predictors of early readmission in hospitalized patients with inflammatory bowel disease. Inflamm Bowel Dis. 2017;23:1891–1897. [DOI] [PubMed] [Google Scholar]
- 15. Centers for Medicare and Medicaid Services. 2014 Measure Information About the 30-Day All-Cause Hospital Readmission Measure, Calculated for the Value-Based Payment Modifier Program Baltimore, MD: CMS, April 2015. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/Downloads/2014-ACR-MIF.pdf Accessed December 2016. [Google Scholar]
- 16. Li W, Stocchi L, Cherla D. Factors associated with hospital readmission following diverting ileostomy creation. Tech Coloproctol. 2017;21:641–648. [DOI] [PubMed] [Google Scholar]
- 17. Fish DR, Mancuso CA, Garcia-Aguilar JE. Readmission after ileostomy creation: retrospective review of a common and significant event. Ann Surg. 2017;265:379–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission: current strategies and future directions. Annu Rev Med. 2014;65:471–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sutherland T, David-Kasdan JA, Beloff J, et al. Patient and provider-identified factors contributing to surgical readmission after colorectal surgery. J Invest Surg. 2016;29:195–201. [DOI] [PubMed] [Google Scholar]
- 20. Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg. 2014;38:1531–1541. [DOI] [PubMed] [Google Scholar]