Abstract
The most frequent presentation of esophageal cancer is adenocarcinoma and squamous cell carcinoma. In recent years, the latter has decreased its incidence increasing the adenocarcinoma. Currently, another type of tumor with a much lower incidence has been described, which has a neuroendocrine component along with another exocrine glandular component and has been classified since 2010 as mixed adenoneuroendocrine carcinoma (MANEC). We present the case of a 68-year-old male with a history of dyspepsia and epigastric pain who after performing a gastroscopy, was diagnosed with a malignant neoplasm of the esophagus. The patient underwent a total esophagectomy with reconstruction by tubular gastroplasty with cervical anastomosis. The final result of the piece after immunohistochemistry revealed that the tumor was composed of one component of adenocarcinoma in 60% together with another component compatible with neuroendocrine in 40%. With these findings and according to the World Health Organization classification of 2010 was diagnosed as esophageal MANEC. MANECs are rare tumors, described in other locations of the digestive tract, the esophagus being an infrequent location. Its preoperative diagnosis is difficult, and it is not until the final analysis of the complete piece by means of specific immunohistochemical techniques when its diagnosis can be established. Its treatment is fundamentally surgical, whereas the adjuvant therapeutic schemes with chemotherapy are not well defined at present because of their low incidence.
KEYWORDS: Adenocarcinoma mixed tumor, collision tumor, esophagus, gastroesophageal junction, mixed adenoneuroendocrine carcinoma
INTRODUCTION
Esophageal cancer accounts for approximately 1.7% of total cancer deaths. It is the fourth cause of death due to malignant neoplasia of the digestive tract.[1] Ninety-five percent of esophageal cancers correspond to adenocarcinomas and/or squamous cell carcinomas. Less frequently, lymphomas, sarcomas, melanoma metastases, or neuroendocrine carcinomas have been described in this location.[2]
Mixed adenoneuroendocrine carcinoma (MANEC) is rare, and their location in the esophagus is exceptional. Stomach, Vater's ampulla, large intestine, rectum and even gastric mucosa with ectopic location are described in the literature.[2,3,4,5,6]
Next, we present a patient undergoing abdominal esophagectomy whose histopathological result revealed a MANEC.
CASE REPORT
A 68-year-old male with a history of epigastric pain and dyspepsia was admitted to our center for study. Physical examination and blood tests showed no alterations. An upper digestive endoscopy was performed in which a neoformative lesion was found, located at 38 cm of the dental arch, at the level of the gastroesophageal junction to which a biopsy was performed. The biopsy was positive for adenocarcinoma and could not be ruled out by the immunohistochemical study of neuroendocrine differentiation.
A cervical-thoraco-abdominal CT scan was performed as an extension study in which no disseminated disease was evident, except for small subcentimeter adenopathies in the gastrohepatic ligament. A transhiatal esophagectomy was performed with cervical anastomosis using tubular gastric plasty [Figure 1]. The immunohistochemical study revealed a mixed tumor formed by an infiltrative adenocarcinoma of the intestinal type moderately differentiated (60% of the tumor lesion) and by a well-differentiated neuroendocrine carcinoma (40% of the tumor surface studied) [Figure 2]. Four metastatic adenopathies from a total of 19 dissected lymph nodes were identified. The neoplasm invaded all the layers and presented perineural and vascular invasion. According to the international qualification of the AJCC (2010) it corresponded to a tumor stage T3N2M0. Immunohistochemistry was positive for synaptophysin and chromogranin (neuroendocrine component). In accordance with the current World Health Organization (WHO) classification of 2010, it was classified as MANEC of esophageal localization. After the intervention, the patient presented a favorable postoperative period, being discharged on the 10th day of admission.
Figure 1.
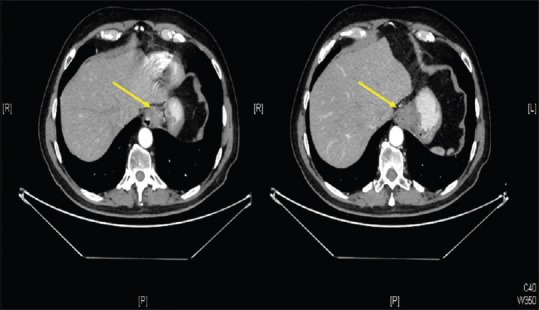
Computed tomography Scan. Yellow arrow shows the esophagus tumor
Figure 2.
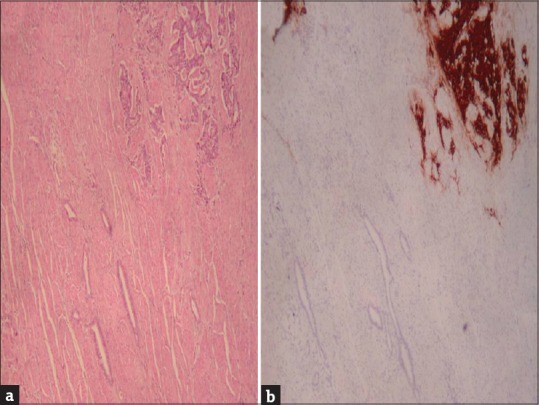
Mixed adenoneuroendocrine carcinoma. (a) Hematoxylin eosin. (b) Synaptophysin
DISCUSSION
The first reference to this type of tumor was made by Cordier in 1924.[7] Since then, it has been mentioned under different names adenocarcinoid, collision tumors, goblet cell carcinomas, and adenocarcinoma ex goblet cell.[8,9,10,11] In 1987, Lewin applied the term mixed tumor, when both components (neuroendocrine and glandular exocrine) reach at least 30% each.[3,6,9] Calcifies them in tumor collision (the exocrine and neuroendocrine component occur in separate areas of the tumor lesion), combined tumors (both components are diffusely intermixed), and in amphicrine tumors (those tumors in which the tumor cell expresses an exocrine component and another neuroendocrine.[3,6]
In the year 2000, WHO included them within the group of endocrine neoplasms, as mixed exocrine-endocrine tumors.[1,3,12] In 2010, the WHO defined them as MANEC.[3,13] The term refers to those tumors that have one component of adenocarcinoma and another of neuroendocrine, both in a percentage of at least 30%.[7] La Rosa, in 2012, updates the classification, dividing them according to their forecast into high, intermediate and low grade depending on the differentiation of their components.[3]
Among the hypotheses about its origin, it is accepted the possibility that MANEC arise independently from 2 different precursor cells in a synchronous way or that they derive from a multipotential stem cell.[14] MANECs are 3–4 times more frequent in men than in women.[1] They do not have a specific clinic or carcinoid syndrome has been described in the literature. They can present from polypoid masses to ulcerated stenotic lesions of variable size (0.5–14 cm).
Its diagnosis is made by immunohistochemistry. Its neuroendocrine component presents positivity for synaptophysin in 75%–90%, chromogranin in 60–70%, CD56 in 50%, and for neuronal specific enolase in a variable percentage while the glandular exocrine component usually expresses specific nonneuroendocrine markers such as cytokeratins 7 and 20 and carcinoembryonic antigen.[1,8,14,15]
If the neuroendocrine component of the MANEC is well differentiated, the therapeutic schemes will be followed after the surgery as if it were an adenocarcinoma. On the other hand, if poorly differentiated, the treatment scheme will be carried out as if it were a neuroendocrine tumor. According to the WHO in 2010, surgery is the treatment of choice and the only one with a curative purpose.[16] The objective of the surgery is to achieve a complete macroscopic tumor resection. Thus, for authors such as Van Laetham, an esophagogastrectomy transthoracic would be of choice for Siewert Type I tumors while for Type II-III, a trnashiatal esophagogastrectomy or extended total gastrectomy would be recommended.[4,17] The subsequent therapeutic strategy is not well defined at present, probably due to the low incidence of these tumors. Most authors agree that their treatment is defined by the most aggressive component.[3]
However, there is no consensus among the different authors for the choice of adjuvant treatment by chemotherapy. For some authors, the use of cisplatin or carboplatin with ectoposide would be recommended.[2,18] Other authors approve the choice of cisplatin combined with fluoropyrimidines in the presence of metastatic adenopathies.[17] In our case, the patient rejected several chemotherapy lines due to their possible side effects, accepting to start the treatment with capecitabine.
Prognosis depends on the stage and tumor type, with a better prognosis for those tumors without distant metastatic involvement.[14]
CONCLUSIONS
MANECs are rare tumors formed by a glandular and neuroendocrine exocrine component. Its location in the esophagus is exceptional, with few cases described in the literature. Your preoperative diagnosis is difficult. Its treatment is fundamentally surgical. Its prognosis depends on the stage and tumor type. Currently, there are no definite recommendations to establish adjuvant treatment with chemotherapy, due to the small number of these tumors.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Juanmartiñena JF, Fernández-Urién I, Córdoba A, Miranda C, Borda A. Mixed adenoneuroendocrine carcinoma (MANEC) of the gastroesophageal junction: A case report and review of the literature. Rev Esp Enferm Dig. 2017;109:160–2. doi: 10.17235/reed.2016.4315/2016. [DOI] [PubMed] [Google Scholar]
- 2.Kadhim MM, Jespersen ML, Pilegaard HK, Nordsmark M, Villadsen GE. Mixed adenoneuroendocrine carcinoma is a rare but important tumour found in the oesophagus. Case Rep Gastrointest Med. 2016;2016:9542687. doi: 10.1155/2016/9542687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.La Rosa S, Marando A, Sessa F, Capella C. Mixed adenoneuroendocrine carcinomas (MANECs) of the gastrointestinal tract: An update. Cancers (Basel) 2012;4:11–30. doi: 10.3390/cancers4010011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Briggs JC, Ibrahim NB. Oat cell carcinomas of the oesophagus: A clinico-pathological study of 23 cases. Histopathology. 1983;7:261–77. doi: 10.1111/j.1365-2559.1983.tb02240.x. [DOI] [PubMed] [Google Scholar]
- 5.Shia J, Tang LH, Weiser MR, Brenner B, Adsay NV, Stelow EB, et al. Is nonsmall cell type high-grade neuroendocrine carcinoma of the tubular gastrointestinal tract a distinct disease entity? Am J Surg Pathol. 2008;32:719–31. doi: 10.1097/PAS.0b013e318159371c. [DOI] [PubMed] [Google Scholar]
- 6.Minaya-Bravo AM, Garcia Mahillo JC, Mendoza Moreno F, Noguelares Fraguas F, Granell J. Large cell neuroendocrine – Adenocarcinona mixed tumour of colon: Collision tumour with peculiar behaviour. What do we know about these tumours? Ann Med Surg (Lond) 2015;4:399–403. doi: 10.1016/j.amsu.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cordier R. Argentaffin cells in intestinal tumors. Arch Int Med Exp. 1924;1:9–74. [Google Scholar]
- 8.Brathwaite S, Rock J, Yearsley MM, Bekaii-Saab T, Wei L, Frankel WL, et al. Mixed Adeno-neuroendocrine carcinoma: An aggressive clinical entity. Ann Surg Oncol. 2016;23:2281–6. doi: 10.1245/s10434-016-5179-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewin K. Carcinoid tumors and the mixed (composite) glandular-endocrine cell carcinomas. Am J Surg Pathol. 1987;11(Suppl 1):71–86. doi: 10.1097/00000478-198700111-00007. [DOI] [PubMed] [Google Scholar]
- 10.Capella C, La Rosa S, Uccella S, Billo P, Cornaggia M. Mixed endocrine-exocrine tumors of the gastrointestinal tract. Semin Diagn Pathol. 2000;17:91–103. [PubMed] [Google Scholar]
- 11.Holt N, Grønbæk H. Goblet cell carcinoids of the appendix. ScientificWorldJournal. 2013;2013:543696. doi: 10.1155/2013/543696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Solcia E, Klöppel G, Sobin LH. 2nd ed. Berlin, Germany: Springer; 2000. Histological Typing of Endocrine Tumours, WHO International Histological Classification of Tumours. [Google Scholar]
- 13.Rindi G, Arnold R, Bosman FT, Capella C, Kilmstra DS, Kloppel G, et al. Nomenclature and classification of neuroendocrine neoplasms of the digestive system. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon, France: IARC Press; 2010. pp. 13–4. [Google Scholar]
- 14.Maru DM, Khurana H, Rashid A, Correa AM, Anandasabapathy S, Krishnan S, et al. Retrospective study of clinicopathologic features and prognosis of high-grade neuroendocrine carcinoma of the esophagus. Am J Surg Pathol. 2008;32:1404–11. doi: 10.1097/PAS.0b013e31816bf41f. [DOI] [PubMed] [Google Scholar]
- 15.Monteiro de Melo Santos D, López-Tomassetti Fernández E, Sánchez Ramos M, Hernández Hernández JR. Improved survival with palliative surgery and chemotherapy for mixed adenoneuroendocrine carcinoma of the gastroesophageal junction with liver metastases. Cir Esp. 2017 doi: 10.1016/j.ciresp.2017.03.014. pii: S0009-739X(17) 30097-0. [DOI] [PubMed] [Google Scholar]
- 16.Veits L, Lang-Schwarz C, Volkholz H, Falkeis C, Vieth M, Schulz H, et al. Mixed adenoneuroendocrine carcinoma (MANEC) of the esophagogastric junction predominantly consisting of poorly differentiated neuroendocrine carcinoma. Endoscopy. 2013;45(Suppl 2):E16–7. doi: 10.1055/s-0032-1326113. [DOI] [PubMed] [Google Scholar]
- 17.Van Laethem JL, Carneiro F, Ducreux M, Messman H, Lordick F, Ilson DH, et al. The multidisciplinary management of gastro-oesophageal junction tumours: European Society of Digestive Oncology (ESDO): Expert discussion and report from the 16th ESMO world congress on gastrointestinal cancer, Barcelona. Dig Liver Dis. 2016;48:1283–9. doi: 10.1016/j.dld.2016.08.112. [DOI] [PubMed] [Google Scholar]
- 18.Delle Fave G, Kwekkeboom DJ, Van Cutsem E, Rindi G, Kos-Kudla B, Knigge U, et al. ENETS consensus guidelines for the management of patients with gastroduodenal neoplasms. Neuroendocrinology. 2012;95:74–87. doi: 10.1159/000335595. [DOI] [PubMed] [Google Scholar]


