Abstract
The aging of workforces combined with the prevalence of age-related chronic diseases has generated interest in whether large numbers of older workers will need workplace accommodations. This research applied work functioning theory to examine accommodation availability, need and use in workers with arthritis, diabetes, or no chronic disabling diseases; factors associated with accommodation needs; and the relationship of accommodation needs met, unmet or exceeded to job outcomes. Participants were aged 50–67 years, employed, and had arthritis (n = 631), diabetes (n = 286), both arthritis/diabetes (n = 111) or no chronic disabling conditions (healthy controls n = 538). They were recruited from a national panel of 80,000 individuals and a cross-sectional survey was administered online or by telephone. Questionnaires assessed demographics, health, work context, workplace accommodations, and job outcomes. Chi-square analyses, analyses of variance, and regression analyses compared groups. Respondents were similar in many demographic and work context factors. As expected, workers with arthritis and/or diabetes often reported poorer health and employment outcomes. Yet, there were few differences across health conditions in need for or use of accommodations with most participants reporting accommodations needs met. In keeping with work functioning theory, unmet accommodation needs were largely related to work context, not health. Workers whose accommodation needs were exceeded reported better job outcomes than those with accommodation needs met. Findings highlight both work context and health in understanding workplace accommodations and suggest that many older workers can meet accommodation needs with existing workplace practices. However, additional research aimed at workplace support and the timing of accommodation use is needed.
The aging of workforces in many developed countries has generated concerns about worker shortages and lost expertise (American Association of Retired Persons (AARP), 2002; Mermin, Johnson, & Murphy, 2007; Nyce & Schieber, 2005). Research addressing these issues has examined longer working trajectories; alterations to the nature of employment like increased opportunities for bridged retirement; and the impact of policy changes dissolving mandatory retirement (Beehr, 2014; Cooke, 2006; Ekerdt, 2010; Feldman & Beehr, 2011; Kooij, de Lange, Jansen, & Dikkers, 2008; Nilsson, Hydbom & Rylander, 2011; Wang, Zhan, Liu, & Shultz, 2008). Working longer is also in keeping with the desire of many older workers who want or need to remain in the labor force beyond a traditional retirement age of 65 years (Park, 2011; Pignal, Arrowsmith & Ness, 2010). However, with increasing age there is a greater likelihood of chronic diseases that can cause disability and that can make working difficult (Brault, Hootman, Helmick, Theis & Armour, 2009; Ilmarinen, 2001; Martin, Freedman, Schoeni, &Andreski, 2009; Perruccio, Power, & Badley, 2007; Smith, Bielecky, & Mustard, 2012).
Among the most common age-related, chronic conditions are arthritis and diabetes. Both conditions are of growing importance not only because their prevalence is associated with ageing, but also because they are linked to population increases in obesity and decreases in physical activity that can mean earlier disease onset and more years spent living with a disability (Leveille, Wee, & Iezzoni, 2005; Lipscombe & Hux, 2007; Perruccio et al., 2007). Individuals with arthritis and diabetes often report being concerned about whether they will be able to sustain work over time, and report elevated job strain and depression that are associated with disruption to employment (Gignac et al., 2012; Gignac, Sutton & Badley, 2007; Lacaille, White, Backman & Gignac, 2007; Polonsky, 2000; Watkins et al., 2000).
To date, research examining employment among those living with arthritis and diabetes has largely drawn on a medical model for guidance. Studies have examined the high incidence of work disability among those living with the conditions and disease factors associated with temporarily or permanently giving up work (Allaire, Wolfe, Niu, LaValley, & Michaud, 2005; Burton, Morrison, Maclean, & Ruderman, 2006; Kanavos, van den Aardweg, & Schurer, 2012; Li, Gignac, & Anis, 2006; Vijan, Hayward & Langa, 2004; Zhang et al., 2010). Relatively little research has adopted a biopsychosocial approach. A biopsychosocial framework is of growing interest because it places disease within the wider context of a person’s life (WHO, 2001). Disability is not thought to arise solely from a health condition, but from the interplay of health (e.g., pain), personal factors (e.g., age, education, individual perceptions), and social and environmental factors (e.g., social support, physical barriers), all of which can make the performance of life activities difficult (WHO, 2001).
An example of a biopsychosocial theory relevant to employment is work functioning theory (Sandqvist & Henriksson, 2004). The theory posits that occupational activities are valued by individuals and that these activities are closely linked to a person’s psychological, social, and financial well-being. The theory was developed to address the observation that there are often increased levels of work disability related to age or health that can impact work performance. Yet, functioning at work is not entirely explained by age or disease symptoms. It is also related to personal factors, work context, and workplace practices that may support work performance or impede it (De Rijk, 2013; Kristman et al., 2016; Sandqvist & Henriksson, 2004).
To date, work functioning theory has mostly been applied to work injuries and return to work; clinical rehabilitation practice; and the measurement of concepts like work ability (Kristman et al., 2016; Loisel & Côté, 2013; Pransky, 2013; Sandqvist & Henriksson, 2004; Tengland, 2011). This study is the first to apply work functioning theory to examine the need for, use of, and unmet needs for organization-level policies and practices that are often broadly available to help employees accommodate their personal needs. It includes policies and practices like flexible hours, special equipment, ergonomic changes, modified job duties, and altered work hours. Although these practices can be used for a variety of reasons, they may be particularly beneficial to enhance the job performance of workers who are managing chronic conditions like arthritis and diabetes. By examining workplace accommodations, we gain a more nuanced understanding of worker needs, factors contributing to having accommodation needs met, unmet or exceeded, and the relationship of accommodations to employment outcomes among older workers with arthritis and diabetes.
Arthritis, Diabetes and Previous Employment Research
Studies of workforce participation among individuals with arthritis find that absenteeism and presenteeism (i.e., reduced work performance) are considerable problems. Leaves of absence of 3 months or more are relatively common and range from one-third to over 50% of individuals (Allaire et al., 2005; Boonen, 2006; Burton et al., 2006; Kaptein et al., 2009). Work disability (i.e., permanently giving up one’s job) and at-work productivity costs are high and are estimated to be two to four times greater than direct health care costs, making arthritis among the costliest diseases in many developed countries (Allaire et al., 2005; Li et al., 2006; Public Health Agency of Canada, 2010; Yelin et al., 2004; Zhang et al., 2010).
Studies also find that diabetes can have a negative impact on employment (Glasgow & Eakin, 1998; Herquelot, Guéguen, Bonenfant, & Dray-Spira, 2011; Latif 2009). Estimates are that more than 50% of those with diabetes are of working age with most new cases being diagnosed among baby boomers (born 1946–1964) (Public Health Agency of Canada, 2011; Shaw, Sicree, & Zimmet, 2010). A study of five European countries (France, Germany, Italy, Spain, United Kingdom) found that the indirect costs of diabetes related to reduced productivity, absenteeism, early retirement and the use of social benefits exceeded direct health care costs by a factor of at least 2:1 and cost approximately €98.4 billion in 2010 (Kanavos, et al., 2012).
Although different in their pathology, arthritis and diabetes are of shared interest for several reasons. Both diseases are chronic, have no cure, and can cause disability. Yet, they may not have a continuous impact on employment. Instead, they often result in episodic or intermittent disability, symptom exacerbation (e.g., flares), or complications that occasionally affect work activities (Galarneau & Radulescu, 2009; Gignac, Cao, Tang, & Beaton, 2011; Gignac et al., 2012; Glasgow & Eakin, 1998; Herquelot et al., 2011; Latif, 2009; Vijan et al., 200). Longitudinal data spanning nearly 5 years from employed women and men living with arthritis highlighted that disability was episodic for nearly three quarters of participants (Gignac et al., 2011). The intermittent nature of arthritis and diabetes is significant for several reasons. On the one hand, it points to the importance of not stigmatizing older workers with chronic conditions as being an inevitable drain on workplace and health resources. On the other hand, longitudinal research with a sample of individuals with arthritis found that many of those with intermittent disability did not pursue accommodations to help manage disability at work until they had pronounced and consistent disability or experienced a crisis (Gignac & Cao, 2009; Gignac et al., 2011). Delays in accessing accommodations raise concerns that older workers may be doing “too little; too late,” which could negatively impact their jobs and result in greater absenteeism, lost productivity and job disruptions, and even threaten the ability to remain employed. In addition, some research finds considerable ageism in workplaces with older workers being perceived negatively, especially in terms of performance and adaptability (Bal, Reiss, Rudolph, & Baltes, 2011; Henkens, 2005; Ng & Feldman, 2013). Perceived ageism may mean that older workers hesitate to draw attention to accommodation needs and are less likely to use existing policies and practices.
Research examining workplace accommodations among individuals with arthritis or diabetes is uncommon. A small number of studies exist in samples of individuals with arthritis and find that accommodation use is relatively low, despite individuals reporting pain, fatigue, and functional limitations at work (Dhanhani, Gignac, Beaton, Su, & Fortin, 2015; Chen et al., 2007; Gignac, Cao, & McAlpine, 2015; Yelin, Sonneborn, & Trupin, 2000). Research has not examined whether the absence of accommodation use reflects a lack of accommodation availability or need. Because accommodation policies are set at an organization level and are available to all workers, and because we expect workers with arthritis and diabetes to be employed in a wide range of jobs, we do not expect differences in reports of accommodation availability among workers with arthritis, diabetes and no chronic diseases. However, in keeping with previous research, workers with arthritis and diabetes are expected to report greater pain, fatigue and health variability (Allaire et al., 2005; Burton et al., 2006; Kaptein et al., 2009; Latif, 2009). As such, more workers with arthritis and diabetes are expected to report a need for workplace accommodations than older workers with no chronic disabling diseases. However, it is unclear whether they will report greater use of accommodations. If older workers are reluctant to draw attention to their health or delay using accommodations because of variability in health symptoms, we may see no differences in accommodation use compared to workers with no chronic diseases even when accommodations are available.
Hypothesis 1a: Workers aged 50 or more who live with arthritis or diabetes will report greater pain, fatigue, and health variability compared to workers who do not have any chronic disabling diseases.
Hypothesis 1b: Older workers who live with arthritis or diabetes will report similar levels of accommodation availability as workers who do not have any chronic, disabling diseases.
Hypothesis 1c: Older workers who live with arthritis or diabetes will report greater need for accommodations at work than older workers who do not have any chronic disabling diseases.
Hypothesis 1d: Older workers who live with arthritis and diabetes will be similar in their use of accommodations at work when compared to older workers who do not have any chronic disabling diseases.
Work Functioning Theory and Workplace Accommodations
As noted, work functioning theory highlights that disability at work needs to be understood as a dynamic interplay among the person, his or her work activities, and the surrounding environment (De Rijk, 2013; Kristman et al., 2016; Loisel & Côté, 2013; Pransky, 2013; Sandqvist & Henriksson, 2004; Tengland, 2011). Applied to older workers with arthritis and/or diabetes, work functioning theory underscores the importance of considering not only the presence of a chronic condition, but also the need for accommodations in conjunction with accommodation availability and use, which are key aspects of the work environment. Specifically, some workers will report that their accommodation needs are met with existing policies. That is, they need adaptations like flexible hours or more breaks and that these accommodations are available and have been used. Other workers may report needing some accommodations, but that these are not available, or they are reluctant to use them. These workers have unmet accommodation needs. Finally, it is possible that some individuals will report that they do not need some workplace accommodations. However, their workplace has put in place accommodation practices and they may draw on them in the absence of a health need. These individuals could be thought to have their accommodation needs exceeded. We would expect that older workers who have arthritis and diabetes would be more likely to have unmet accommodation needs and less likely to have accommodation needs exceeded compared to workers with no chronic disabling diseases.
Hypothesis 2: More workers with arthritis and/or diabetes will have their accommodation needs unmet and fewer will have accommodation needs exceeded when compared to workers with no chronic, disabling conditions.
In addition to condition type and symptoms like pain, fatigue, and health variability being associated with accommodation needs unmet, met, or exceeded, we expect demographic factors and work context to be relevant. To date, studies have not examined a range of demographic and work context variables and their relationship to accommodation use among individuals with arthritis or diabetes. However, some research finds women report more severe disease symptoms than men (Helmick et al., 2008; Srikanth et al., 2005; van Vollenhoven, 2009; Wasef, 2004), more part-time work and more accommodation needs (Cranford, Vosko, & Zukewich, 2003; Kaptein et al., 2009; Padavic & Reskin, 2002; Wallenius et al., 2009). These findings suggest that women may have greater unmet accommodation needs than men. Moreover, although research has not examined accommodations, older adults and workers with less education are less likely to be employed when they have arthritis (Kaptein, Gignac & Badley, 2009). Greater difficulty sustaining employment in these groups could mean that age and education are relevant and that older adults and those with less education will be more likely to report unmet accommodation needs.
Work context also has not been examined in terms of accommodation needs met, unmet or exceeded. However, workers in physically demanding jobs, which may be particularly difficult for those with arthritis and diabetes; who report greater work stress; or who work part-time (and are less likely to be eligible for workplace accommodations) may have greater unmet accommodation needs, whereas those with greater job control may be more likely to report their accommodation needs met or even exceeded. Potentially relevant to having accommodation needs met, unmet or exceeded are job sector and the size of an organization. Sales and retail jobs may have fewer accommodations available whereas larger organizations may have more accommodation policies available.
Hypothesis 3a: Greater pain, fatigue and health variability are expected to be associated with having unmet accommodation needs.
Hypothesis 3b: Women, older respondents, and those with less education are expected to have more unmet accommodation needs.
Hypothesis 3c: Participants whose work is physically demanding, with greater work stress, who are employed part-time, or who work in sales and retail are expected have more unmet accommodation needs. Workers with greater job control and who are employed in larger organizations are expected to be more likely to have their accommodation needs met or exceeded.
Finally, greater age and having arthritis and/or diabetes has been found to be associated with employment outcomes like greater workplace activity limitations, more job disruptions (arriving late/leaving early; missing meetings), productivity losses and absenteeism (Allaire et al., 2005; Brault et al., 2009; Burton et al., 2006; Ilmarinen, 2001; Martin et al., 2009; Smith et al., 2012). Women also report more activity limitations in the workplace than men (Kaptein et al., 2009; Wallenius et al., 2009). Applying work functioning theory would suggest that individuals with unmet accommodation needs will report poorer employment outcomes than individuals with accommodation needs met. Having accommodation needs exceeded should allow workers to potentially avoid difficulties at work. As such, having accommodation needs exceeded should be associated with fewer activity limitations, job disruptions, productivity losses and less absenteeism compared to having accommodation needs met.
Hypothesis 4a: Living with arthritis or diabetes will be associated with greater workplace activity limitations, job disruptions, productivity losses and absenteeism
Hypothesis 4b: Older age will be associated with greater workplace activity limitations, job disruptions, productivity losses and absenteeism and being female will be associated with greater workplace activity limitations.
Hypothesis 4c: Having unmet accommodation needs will be associated with greater workplace activity limitations, job disruptions, productivity losses and absenteeism compared to having accommodation needs met.
Hypothesis 4d: Having accommodation needs exceeded will be associated with fewer workplace activity limitations, job disruptions, productivity losses and absenteeism compared to having accommodation needs met.
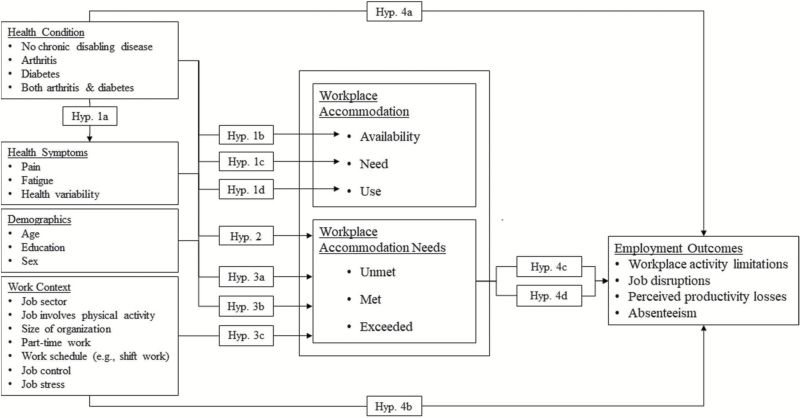
A Conceptual Model of Workplace Accommodations Using Work Functioning Theory
Figure 1 summarizes the hypotheses and presents a preliminary conceptual framework that applies work functioning theory in a novel way to better address health, demographic and work context factors that may be associated with accommodations and the relationship of accommodation needs met, unmet, and exceeded to employment outcomes. Hypothesis 1a draws on previous research and differentiates older workers with arthritis and diabetes from workers with no chronic disabling conditions in terms of pain, fatigue and health variability, while Hypotheses 1b–1d link disease condition to accommodation need, but not necessarily to accommodation availability or use. Hypothesis 2 expands on previous research and introduces concepts of accommodation needs met, unmet and exceeded. Workers with arthritis and diabetes are expected to be more likely to have accommodation needs unmet and less likely to have needs met or exceeded than adults with no chronic conditions. Hypotheses 3a–3c applies work functioning theory to posit that health factors alone are unlikely to be the only variables related to accommodation needs met, unmet or exceeded (Hypothesis 3a). Demographic factors like age, gender and education (Hypothesis 3b), as well as a wide range of work context variables like job sector, physically demanding work, the size of the workplace, part-time hours, shift work, job control and job stress may also relate to having accommodation needs met, unmet or exceeded (Hypothesis 3c). Finally, Hypotheses 4a and 4b draws on previous research that links chronic condition type, age, and gender to poorer employment outcomes. Hypotheses 4c and 4d expand on this research and apply work functioning theory to link unmet accommodation needs with poorer employment outcomes (Hypothesis 4c) and accommodation needs exceeded to better employment outcomes (Hypothesis 4d) when compared to those reporting their accommodation needs met. By applying work functioning theory to test these hypotheses, we gain not only new insights into accommodation needs and use, but also insights into factors, especially related to work context, that may be modifiable and may help improve areas of person-job fit to sustain the employment of older workers with chronic conditions.
Figure 1.
A conceptual model of workplace accommodations using work functioning theory.
METHOD
Study Design and Participants
A cross-sectional survey was used to collect data. Participants were recruited from an existing nationally representative survey panel of ~ 80,000 Canadians that was created using probability sampling. From this, we recruited a sample of workers aged 50–67 years born from 1946 to 1964 (considered the “baby boomer generation”) and which comprised workers with no chronic, disabling diseases, adults with arthritis, and adults with diabetes. Participants were eligible if born from 1946 to 1964 and employed ≥15 hr/week. Participants were labeled as healthy control respondents if they had not: (a) been diagnosed with any chronic physically or mentally disabling health conditions lasting 6 months or more; (b) experienced a disabling injury or been recovering from surgery within the past 6 months. Arthritis participants had a self-reported: (a) physician diagnosis of arthritis (e.g., osteoarthritis [OA]; inflammatory arthritis [IA] e.g., rheumatoid arthritis); and (b) an arthritis duration of ≥1 year (to ensure time working with arthritis). Diabetes participants had a self-reported: (a) physician diagnosis of Type I or II diabetes; and (b) a diabetes duration of ≥1 year. Participants were excluded if they: (a) reported being diagnosed with other chronic physically or mentally disabling health conditions (e.g., stroke, depression) prior to their arthritis or diabetes diagnosis; or (b) experienced an injury or were recovering from surgery (past 6 months). The occurrence of co-morbid conditions after diagnosis of arthritis/diabetes is challenging for establishing inclusion/exclusion criteria as both diseases result in increased risks for other conditions (Public Health Agency of Canada 2010, 2011). Hence, individuals diagnosed with other conditions after their arthritis/diabetes diagnosis were included.
Recruitment and Procedure
Potential respondents were invited by email to participate in a study aimed at better understanding the working experiences of individuals aged 50 or more years. We aimed for a quota of 500 respondents in each health condition to ensure variability in disease severity, job sector, and accommodation needs and use, and based on previous studies of workplace accommodations (Chen et al., 2007; Gignac et al., 2015; Yelin et al., 2000). Respondents were screened to meet eligibility criteria. Eligible respondents were given a choice of a telephone-administered or online questionnaire in English or French. Recruitment continued until eligible, consenting participants were found. Questionnaires took 25–30 min to complete and were administered from September to October 2014. Ethics approval was received from the University of Toronto. Informed verbal/written consent was obtained from participants.
Measures
Demographics
Information on age in years, sex (male or female), education (secondary school education or less; some postsecondary school; postsecondary education) and marital status (married/living as married; divorced; separated; widowed; never married) was collected.
Type of arthritis and diabetes
Type of arthritis was collected as OA, IA (e.g., rheumatoid arthritis) or both OA and IA. Type of diabetes was collected as Type I or Type II diabetes. For the purposes of the current study OA, IA and both OA/IA were combined into the category “arthritis” and Type I and Type II types of diabetes were combined into the category “diabetes.”
Pain
A visual analogue scale assessed pain in the last month (range 0 to 10; 0 = no pain; 10 = worst possible pain).
Fatigue
The five-item Profile of Mood States (POMS) fatigue subscale asked the extent to which participants felt worn out, fatigued, exhausted, sluggish and weary in the previous month (0 = not at all; 4 = extremely) (McNair, Douglas, Lorr, & Droppleman, 1971). Three additional items were added to balance the scale with more positive mood states and make it relevant to all respondents: full of energy, vigorous and lively. Scores were summed. Cronbach’s alpha, a measure of internal consistency, was .89 for the modified scale.
Health variability
Variability in health symptoms was assessed by asking the extent to which respondents had “variable health problems (times of good and bad health) over the past 3 months” (1 = not at all; 5 = a great deal).
Job sector
A list of 21 job sectors were provided and collapsed into six categories: (a) banking/insurance/business/technology; (b) education/health/sciences/arts; (c) construction/utilities; (d) sales/retail; (e) manufacturing/agriculture; (f) government.
Hours per week
Respondents were asked the hours worked in a typical week. For analyses these were collapsed into part-time work (less than 30 hr per week) or full-time work (more than 35 hr per week).
Size of organization
Respondents were asked for the number of years they had worked for their current employer and the size of their organization. Responses were collapsed into: <50 people; 50–499 people; ≥500 people.
Job involves physical activity
Respondents were asked the extent to which their job involved physical activity or movement (e.g., bending, lifting) (1 = not at all; 5 = a great deal).
Work schedule
A single item asked about work schedules. Categories were: (a) a regular daytime schedule; (b) a regular evening shift; (c) a regular night or graveyard shift; (d) a rotating shift (changes from days to evenings to nights); (e) a split shift (two distinct periods every day); (f) on call; (g) an irregular schedule. Responses were collapsed into irregular schedule/shift work and regular schedule.
Job control
Nine items asked about control over work tasks, pace and scheduling (1 = not at all; 5 = a great deal) (Dwyer & Ganster, 1991). Example items included, “how much control do you have over how you do your work?”; “how much control do you have over how quickly or slowly you have to work?”; “how much can you choose from a variety of tasks or projects to do?” The items were a subset of the original 22-item scale. Scores were summed. Internal consistency of the adapted measure was excellent (Cronbach’s alpha = .91).
Job stress
A single item asked about respondents how stressful their work was in the past 3 months (1 = not at all; 5 = extremely).
Workplace activity limitations
The 12-item Workplace Activity Limitations Scale (WALS) measured activity limitations at work (Beaton et al., 2010; Gignac, 2005; Gignac, Cao, Lacaille, Anis, & Badley, 2008). Items assessed getting to/from/around the workplace, upper and lower mobility difficulties, concentration, scheduling and pace of work (0 = no difficulty, 3 = unable to do). Example items include asking respondents how much difficulty they have: “getting around the workplace (e.g., stairs, hallways, furniture)”; “standing for long periods of time (e.g., more than 20 min)”; “with the pace of work your job requires”; “concentrating or keeping your mind on work.” Scores were summed (Cronbach’s alpha = .83).
Job disruptions
Seven questions measured different types of job disruptions in the previous 6 months (Yes/No). Examples include experiencing “lost work time from work because of arriving late or leaving early”; “being unable to work the shift or schedule desired”; “work interruptions of greater than 20 min” (Gignac et al., 2008). Scores for the job disruptions index were summed and ranged from 0 to 7.
Health absenteeism
Respondents were asked about the number of days absent related to their health in the past 3 months. Responses were categorized into no absences versus any absences.
Perceived productivity loss
At-work productivity in the past week was measured with a global item from the Work Productivity and Activity Impairment Questionnaire (WPAI) asking participants how much their health impacted their productivity while they were working (0 = no effect; 10 = prevented working) (Reilly, Zbrozek & Dukes, 1993).
Workplace accommodations
Respondents were asked about the following workplace practices and policies that could act as accommodations: (a) flexible hours (i.e., have some flexibility in the times when work starts or finishes); (b) special equipment/adaptations (e.g., built-up keyboard); (c) modified job duties (e.g., reduced lifting); (d) altered work schedules (e.g., compressed work week); (e) more breaks and rest periods; (f) work-at-home arrangements; (g) extended health benefits (paid for by employers and not covered by provincial health insurance, e.g., some medications, physical therapy, dental); (h) paid or unpaid short-term leave (i.e., an extended absence due to health of more than 1 week and less than 3 months); (i) wellness programs (e.g., nutritional information; Dhanhani et al., 2015; Gignac et al., 2015). For each accommodation, participants were asked whether they needed the accommodation (Yes/No) and whether it was available (Yes/No/Don’t know). If an accommodation was available, respondents were asked whether they had used the accommodation in the past 12 months (Yes/No).
Workplace accommodation needs met, unmet and exceeded
Using the nine accommodation items described earlier, three groups were created to examine combinations of accommodation needs and use. Groups comprised respondents who: (a) reported congruence between the accommodations they needed and the accommodations they used (accommodation needs met); (b) reported needing more accommodations than they used (accommodation needs unmet); and (c) reported not needing some accommodations but using them anyway (accommodation needs exceeded).
Statistical analyses
The distributions of all variables were examined for normality. Correlations among variables were examined for multicollinearity. Means, standard deviations (SDs) and percentages described the sample, work context factors and accommodation availability, needs, and use by condition type. To assess Hypothesis 1a we used one-way analysis of variances (ANOVAs) to compare similarities and differences across health conditions in reports of pain, fatigue, and health variability. Hypotheses 1b–1d were tested using chi-square analyses that compared condition types by accommodation availability, need and use. Hypothesis 2 was examined using chi-square analyses comparing the condition types with accommodation needs met, unmet and exceeded. Hypothesis 3 was tested by first examining the association of accommodation needs met, unmet and exceeded with demographic, health and work context variables using bi-variable multinomial logistic regression analyses. Variables that were significant at p ≤ .05 in bi-variable analyses were included in multivariable multinomial logistic regression analyses. Finally, Hypotheses 4a–4c were tested using ordinary least-squares and logistic regression analyses to examine the association of age, gender, condition type and accommodation needs met, unmet and exceeded with employment outcomes (i.e., workplace activity limitations, job disruptions, perceived productivity losses, and absenteeism). Analyses were conducted using SAS/STAT software, version 9.3 (SAS/STAT User’s Guide, 2012), and STATA (Stata Corporation).
RESULTS
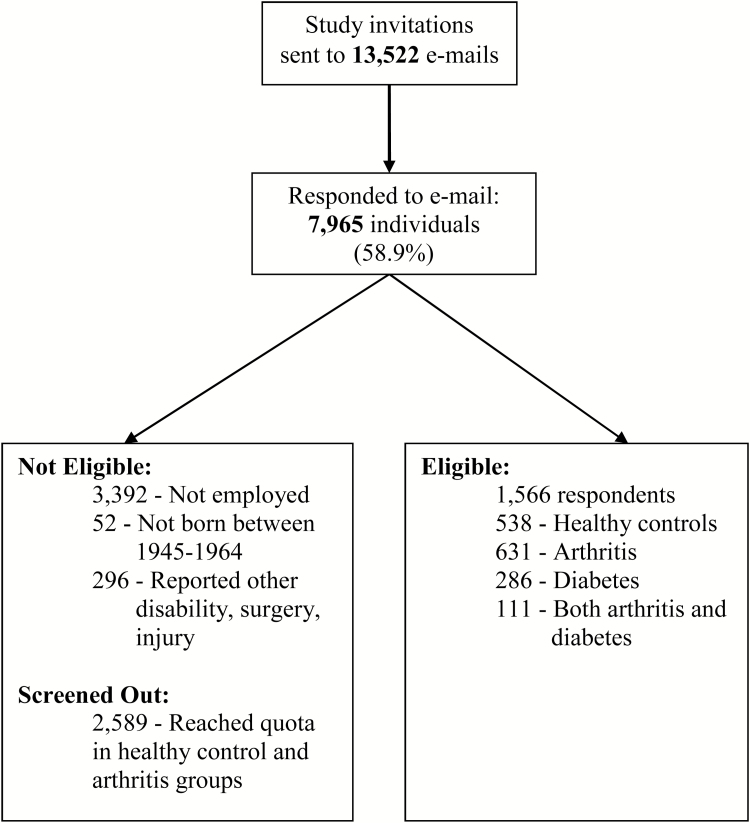
Survey invitations were sent to 13,522 emails of people born 1945–1964 with 7,965 responses (58.9%) (Figure 2). Of them, 3,740 individuals were ineligible mostly because participants were not currently employed (3,392: 53.6%) or because we reached quotas established for the healthy and arthritis groups (2,589: 40.9%). The final sample consisted of 1,566 respondents of whom 73.4% completed the online questionnaire. We did not reach a quota of 500 individuals with diabetes. However, many individuals had both arthritis and diabetes and they were included as a distinct morbidity group in our analyses. Final numbers were: healthy controls = 538; arthritis = 631; diabetes = 286; both arthritis/diabetes = 111. Among those with arthritis, 57.1% reported OA; 23.8% IA or both OA and IA; and 19.1% were unsure of their arthritis type. Among those with diabetes, 83.4% reported Type II diabetes.
Figure 2.
Summary of recruitment.
One-way ANOVAs compared the condition types in terms of sample characteristics. Groups were similar in many demographic and work context factors (Table 1). On average, participants were 59 years old. There was a greater proportion of respondents aged 60 + in the arthritis group or with both arthritis/diabetes. Consistent with the established epidemiology of these conditions, there were more women with arthritis and more men with diabetes compared to controls. There were fewer respondents with postsecondary education in the group with both arthritis/diabetes. Respondents with arthritis or both arthritis/diabetes generally reported poorer job outcomes than healthy controls with greater workplace activity limitations, F (3, 1,483) = 57.7, p < .01; job disruptions, F (3, 1,541) = 13.9, p < .01; perceived productivity losses, F (3, 1,545) = 17.8, p < .01; and absenteeism, χ2 (3, N = 1,566) = 21.7, p < .01. Unexpectedly, those with arthritis or both arthritis and diabetes also often reported poorer job outcomes than the diabetes group who generally were not significantly different from healthy controls.
Table 1.
Sample Characteristics by Condition Type (Healthy Control, Arthritis, Diabetes, Both Arthritis and Diabetes) (n = 1,566)
| Variable | Healthy, n = 538 | Arthritis, n = 631 | Diabetes, n = 286 | Both Arthritis and Diabetes, n = 111 | Total Samplea, n = 1,566 |
|---|---|---|---|---|---|
| M (SD) % | M (SD) % | M (SD) % | M (SD) % | M (SD) % | |
| Demographics | |||||
| Mean age* | 58.5 (5.1) | 59.4 (5.1)b | 59.2 (5.0) | 60.7 (4.2)b | 59.2 (5.1) |
| Gender* | |||||
| Men | 56.3 | 46.4 | 67.0 | 52.7 | 54.0 |
| Women | 43.7 | 53.6 | 33.0 | 47.3 | 46.0 |
| Education** | |||||
| Secondary or less | 13.2 | 15.6 | 19.0 | 19.8 | 15.7 |
| Some postsecondary | 16.8 | 20.4 | 20.1 | 25.2 | 19.4 |
| Postsecondary | 70.0 | 64.0 | 60.9 | 55.0 | 64.9 |
| Marital status | |||||
| Married/living as married | 70.5 | 68.0 | 66.8 | 57.7 | 67.9 |
| Divorced/separated/ widowed | 17.9 | 21.5 | 21.2 | 27.0 | 20.6 |
| Never married | 11.6 | 10.5 | 12.0 | 15.3 | 11.5 |
| Work context variables | |||||
| Job sector | |||||
| Banking/insurance/business/technology | 17.0 | 11.8 | 15.6 | 15.6 | 14.5 |
| Education/health/sciences/arts | 41.2 | 41.9 | 29.8 | 37.6 | 39.2 |
| Construction/utilities | 10.1 | 11.5 | 12.0 | 13.8 | 11.3 |
| Sales/retail | 11.4 | 16.2 | 20.6 | 17.4 | 15.4 |
| Manufacturing/agriculture | 9.1 | 9.1 | 11.0 | 7.3 | 9.3 |
| Government | 11.2 | 9.5 | 11.0 | 8.3 | 10.3 |
| Hours per week | 36.6 (12.4) | 34.7 (13.7) | 36.7 (12.5) | 35.6 (15.4) | 35.8 (13.2) |
| Size of organization | |||||
| <50 people | 23.4 | 30.1 | 29.8 | 32.1 | 27.9 |
| 50–499 people | 23.7 | 26.7 | 27.5 | 20.5 | 25.4 |
| ≥500 people | 52.9 | 43.2 | 42.7 | 47.4 | 46.7 |
| Job involves physical activity (range 1–5)* | 2.7 (1.3) | 3.1 (1.4)b | 2.8 (1.4)e | 3.0 (1.4) | 2.9 (1.4) |
| Job control (range 0–36)* | 22.1 (9.5) | 20.6 (9.9) | 19.4 (10.2)b | 19.0 (10.0)b | 20.8 (9.9) |
| Job stress (range 1–5) | 2.9 (1.0) | 2.8 (1.0) | 2.8 (1.1) | 3.0 (1.1) | 2.9 (1.0) |
| Job outcomes | |||||
| Workplace activity limitations (range 0–36)* | 2.1 (2.5) | 4.3 (4.4)b,c | 2.3 (2.8)c,d | 5.7 (4.7)b | 3.3 (3.8) |
| Job disruptions (range 0–7)* | 0.4 (1.0) | 0.9 (1.4)b | 0.6 (1.3)c,d | 1.1 (1.7)b | 0.7 (1.3) |
| Perceived productivity loss (range 0 to 10)* | 1.9 (1.7) | 2.6 (2.3)b | 2.0 (1.7)c,d | 2.9 (2.2)b | 2.3 (2.0) |
| Days absent related to health (past 3 months)* | 1.1 (3.9) | 2.6 (9.9)b | 2.2 (8.3) | 2.8 (9.7) | 2.0 (8.0) |
Note. ans vary due to missing data.
bGroup is significantly different from the “Healthy control” group, p < .05.
cGroup is significantly different from the “Both Arthritis and Diabetes” group, p < .05.
dGroup is significantly different from the “Arthritis” group, p < .05.
Chi-square or one-way analysis of variance (ANOVA) significant difference, *p < .01; **p < .05.
There was partial support for Hypothesis 1a (Table 2). Individuals with arthritis or both arthritis/diabetes reported greater pain, F (3, 1,558) = 100.9, p < .01; fatigue, F (3, 1,516) = 10.0, p < .01; and health variability, F (3, 1,554) = 25.1, p < .01, than healthy controls. Respondents with diabetes reported significantly more health variability, F (1, 1,554) = 9.7, p < .01 and more pain, F (1, 1,558) = 9.6, p < .01), than healthy controls, but did not report greater fatigue.
Table 2.
Differences in Health Variables and Accommodation Availability by Condition Type (Healthy Control, Arthritis, Diabetes, Both Arthritis and Diabetes) (n = 1,566)
| Variable | Healthy, n = 538 | Arthritis, n = 631 | Diabetes, n = 286 | Both Arthritis and Diabetes, n = 111 | Total Samplea, n = 1,566 |
|---|---|---|---|---|---|
| M (SD) % | M (SD) % | M (SD) % | M (SD) % | M (SD) % | |
| Pain (range 0–10)* | 2.6 (1.7) | 4.4 (2.2)b | 3.0 (1.9)d | 4.6 (2.3)b | 3.5 (2.2) |
| Fatigue (range 0–32)* | 11.5 (6.4) | 13.0 (6.8)b | 12.3 (6.2) | 15.0 (6.6)b | 12.5 (6.6) |
| Health variability (past 3 months) (range 1–5)* | 1.7 (0.9) | 2.1 (1.1)b | 1.9 (0.9)b,c,d | 2.4 (1.1)b | 2.0 (1.0) |
| Availability of workplace policies/accommodations* | |||||
| None available | 4.8 | 6.5 | 11.1 | 17.1 | 7.6 |
| 1–2 available | 14.4 | 17.5 | 17.7 | 13.4 | 16.2 |
| ≥3 available | 80.8 | 70.0 | 71.2 | 69.5 | 76.2 |
Note. a ns vary due to missing data.
bGroup is significantly different from the “Healthy control” group, p < .05.
cGroup is significantly different from the “Both Arthritis and Diabetes” group, p < .05.
dGroup is significantly different from the “Arthritis” group, p < .05.
Chi-square or one-way ANOVA significant difference, *p < .01.
We had hypothesized that there would be no differences in the availability of workplace accommodations across condition types (Hypothesis 1b) (Table 2). However, workers with diabetes or both arthritis/diabetes reported fewer accommodations available than healthy controls, χ2 (6, N = 1,554) = 22.4, p < 01. Despite this, about 70% or more of participants across all condition types reported three or more accommodations available in their workplace. The most widely available accommodations were flex-time, special equipment or adaptations, and extended health benefits. Least available was work-at-home arrangements.
To examine Hypothesis 1c, we compared each accommodation type reported as needed by health condition using chi-square analyses. We also created a variable assessing the total number of accommodations needed by examining sample distributions across condition type. The latter analysis resulted in three levels: those who needed no accommodations; those who needed 1–2 accommodations; those who needed three or more accommodations. We had expected to find differences in accommodation needs by condition type with healthy controls reporting fewer needs than respondents with arthritis or diabetes. However, despite differences in health and job outcomes, there were few differences across health groups in perceived need for accommodations (Table 3). The most frequently reported accommodations needed were extended health benefits followed by flexible hours. About one in five and one in four participants with arthritis or both arthritis/diabetes reported needing special equipment/adaptations, which was significantly greater than healthy controls, χ2 (3, N = 1,171) = 8.1, p < .04. Respondents with arthritis, diabetes and both arthritis/diabetes also were significantly more likely to report needing modified job duties compared to healthy controls, χ2 (3, N = 1,171) = 20.6, p < .01, although this amounted to only 17% of respondents with arthritis and fewer participants in the other disease groups. Participants with arthritis and diabetes were also more likely to report needing short-term leaves of absence, χ2 (3, N = 1,171) = 8.8, p < .03. When accommodation types were combined into a total number of accommodations needed, chi-square analyses found that 14.6% to 26.6% of respondents across the health conditions reported not needing any accommodations and fewer than 45% of respondents reported needing three or more accommodations. Differences in the levels of accommodations needed were not significant across health condition type, χ2 (6, N = 1,171) = 10.3, p = .11.
Table 3.
Percentage of Respondents Reporting Workplace Accommodations Needed and Used and Accommodation Needs Met, Unmet, or Exceeded by Condition Type (n = 1,171)
| Workplace Accommodations | Workplace Accommodations Needed % | Workplace Accommodations Used % | Workplace Accommodations % | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Healthy Control | Arthritis | Diabetes | Both A&D | Healthy Control | Arthritis | Diabetes | Both A&D | Healthy Control | Arthritis | Diabetes | Both A&D | ||
| Flexible hours/flex-time | 36.4 | 36.6 | 39.1 | 33.3 | 31.4 | 31.4 | 31.8 | 23.8 | Accommodation needs | ||||
| Special equipment or adaptationsb | 13.9 | 19.7d | 18.1 | 25.0d | 10.9 | 13.2 | 15.5 | 15.0 | Unmet | 18.3 | 23.5 | 25.4 | 29.3 |
| Modified job duties a, c | 6.9 | 17.0d | 11.8d | 16.5d | 3.4 | 9.7d | 8.8d | 8.9d | Met | 65.2 | 60.7 | 61.0 | 62.2 |
| Altered work schedule | 15.3 | 19.2 | 18.1 | 17.5 | 13.9 | 14.8 | 13.8 | 13.9 | Exceeded | 16.5 | 15.8 | 13.6 | 8.5 |
| More breaks and rest periods c | 14.2 | 19.7 | 20.8 | 18.5 | 9.4 | 16.2d | 19.0d | 13.6 | |||||
| Work-at-home arrangements | 22.8 | 21.0 | 26.8 | 15.0 | 24.1 | 22.0 | 26.8 | 16.5 | |||||
| Extended health benefits | 61.2 | 63.1 | 59.0 | 74.1 | 59.7 | 53.6 | 48.7 | 53.1 | |||||
| Short-term leave b | 18.5 | 26.2d | 26.3d | 26.8 | 14.9 | 19.9 | 23.8d | 24.4d | |||||
| Wellness program | 25.8 | 26.0 | 29.5 | 30.9 | 21.0 | 18.6 | 24.2 | 21.3 | |||||
| Total workplace accommodations needed/usede | |||||||||||||
| 0 needed/used | 26.6 | 20.5 | 20.2 | 14.6 | 24.1 | 23.1 | 25.0 | 30.5 | |||||
| 1–2 needed/used | 36.8 | 38.4 | 43.0 | 40.3 | 44.9 | 44.5 | 45.6 | 35.4 | |||||
| ≥3 needed/used | 36.6 | 41.1 | 36.8 | 45.1 | 31.0 | 32.4 | 29.4 | 34.1 | |||||
Note. Healthy control n = 396; Arthritis n = 465; Diabetes n = 228; Arthritis and Diabetes (A&D) n = 82. Samples sizes vary due to missing data and range from 1,139 to 1,167.
aNeed/Use of workplace practices/accommodations differs by condition, p < .01.
bNeed/Use of workplace practices/accommodations differs by condition, p < .05.
cUse of workplace practices/accommodations differs by condition, p < .01.
dGroup is significantly different from the “Healthy control” group, p < .05.
eChi-square tests examining disease type by levels of Workplace Practices/Accommodations needed and used, p < .07 and p < .66, respectively.
Hypothesis 1d anticipated that there would not be significant differences in accommodations used by condition type. The hypothesis was largely supported. However, compared to healthy controls, respondents with arthritis, diabetes, and both arthritis/diabetes were significantly more likely to use modified work duties, χ2 (3, N = 1,171) = 13.8, p < .01; participants with arthritis and diabetes were more likely to use additional breaks and rest periods, χ2 (3, N = 1,171) = 12.9, p < .01; and respondents with diabetes or both arthritis/diabetes were significantly more likely to have used a short-term leave of absence, χ2 (3, N = 1,171) = 9.3, p < .03. Despite this, when accommodation types were combined into three groups reflecting total levels of accommodations used (none; 1–2; 3 or more), chi-square analyses yielded no significant differences by health condition type, χ2 (6, N = 1,171) = 3.9, p = .69. About two-thirds of respondents used two or fewer accommodations in the past 12 months.
Hypothesis 2 predicted that more workers with arthritis and diabetes would have their accommodation needs unmet and fewer would have accommodation needs exceeded when compared to workers with no chronic, disabling conditions. As described earlier, we created three groups of respondents with accommodation needs met, unmet or exceeded. Chi-square analyses examined differences across the three groups by health condition (Table 3). Although approximately one quarter of participants with arthritis or diabetes and nearly 30% of those with both arthritis/diabetes had accommodation needs unmet compared to 18.3% of healthy controls, the chi-square analysis yielded no significant differences by health condition and the hypothesis was not supported, χ2 (6, N = 1,171) = 10.0, p = .12. Most participants reported having their accommodation needs met (60.7% to 65.2%). Fewer respondents reported their accommodation needs exceeded with similar percentages among healthy controls (16.5%), respondents with arthritis (15.8%) and those with diabetes (13.6%) and somewhat less among participants with both arthritis/diabetes (8.5%).
Hypothesis 3 predicted that having accommodation needs unmet, met, or exceeded would not only be related to health, but also would be associated with age, gender, education and a range of work context variables. The hypothesis was examined in two steps. First, bivariable multinomial regression analyses were conducted with demographic, health, and work context factors as predictor variables where each was examined separately with a two-level outcome that compared accommodation needs unmet with accommodation needs met, as well as accommodation needs exceeded with accommodation needs met. Table 4 presents the estimates (b), standard errors (SE), odds ratios (OR) and p-values for each analysis of each outcome and the overall findings. Findings revealed that, compared to respondents who reported their accommodation needs met, respondents with unmet needs had significantly greater pain, b = 0.12, p < .01; fatigue, b = 0.04, p < .01; and health variability, b = 0.25, p < .01. They also reported more physically demanding work, b = 0.17, p < .01; greater job stress, b = 0.25, p < .01; and less job control, b = −0.05, p < .05. They were more likely to be working in health/education/sciences, OR = 2.22, p < .01; sales/retail, OR = 2.60, p < .01; or utilities/construction, OR = 2.08, p < .05 rather than banking/insurance/business/technology. Compared to full-time workers, part-time workers were more likely to have unmet needs instead of needs met, OR = 1.58, p < .03. Irregular shift workers also were more likely to have unmet needs compared to regular shift workers, OR = 1.44, p < .05. Compared to respondents who had their accommodation needs met, respondents who had their accommodation needs exceeded, reported significantly less fatigue, b = −0.03, p < .05 and health variability, b = −0.41, p < .01 and reported work as being less physically demanding, b = −0.14, p < .05, and having greater job control, b = 0.04, p < .01, than respondents who reported their accommodation needs met.
Table 4.
Bivariable Multinomial Regression Analyses of Demographic, Health, and Work Context Factors Associated With Workplace Accommodation Needs Unmet, Met and Exceeded
| Variable | Unmet Needs (n = 217) vs. Needs Met (n = 632) | Needs Exceeded (n = 156) vs. Needs Met (n = 632) | p | ||||
|---|---|---|---|---|---|---|---|
| b | SE | OR | b | SE | OR | ||
| Age | 0.01 | 0.01 | 1.01 | 0.01 | 0.02 | 1.01 | .63 |
| Gender (female) | 0.28 | 0.14 | 1.32 | −0.20 | 0.17 | 0.82 | .04 |
| Education | .30 | ||||||
| Postsecondary complete | −0.35 | 0.18 | 0.70 | 0.02 | 0.24 | 1.02 | |
| Some postsecondary | −0.18 | 0.23 | 0.83 | 0.22 | 0.28 | 1.25 | |
| Pain | 0.12** | 0.03 | 1.13 | −0.07 | 0.04 | 0.93 | <.001 |
| Fatigue | 0.04** | 0.01 | 1.04 | −0.03* | 0.01 | 0.97 | <.001 |
| Health variability | 0.25** | 0.07 | 1.28 | −0.41** | 0.10 | 0.66 | <.001 |
| Health condition | .13 | ||||||
| Arthritis | 0.33 | 0.17 | 1.39 | 0.03 | 0.19 | 1.03 | |
| Diabetes | 0.40 | 0.21 | 1.49 | −0.13 | 0.24 | 0.88 | |
| Both arthritis and diabetes | 0.52 | 0.28 | 1.68 | −0.61 | 0.43 | 1.54 | |
| Job sector | .09 | ||||||
| Education/health/sciences/arts | 0.80** | 0.28 | 2.22 | −0.30 | 0.26 | 0.74 | |
| Construction/utilities | 0.95** | 0.32 | 2.60 | −0.41 | 0.35 | 0.66 | |
| Sales/retail | 0.73* | 0.31 | 2.08 | −0.02 | 0.29 | 0.98 | |
| Manufacturing/agriculture | 0.54 | 0.36 | 1.72 | −0.15 | 0.34 | 0.86 | |
| Government | 0.54 | 0.33 | 1.72 | −0.32 | 0.32 | 0.72 | |
| Work physically demanding | 0.17** | 0.05 | 1.19 | −0.14* | 0.06 | 0.87 | <.001 |
| Size of employer | |||||||
| <100 employees | 0.08 | 0.15 | 1.08 | 0.29 | 0.18 | 1.34 | .24 |
| Part-time hours | 0.46** | 0.17 | 1.58 | 0.21 | 0.21 | 1.23 | .03 |
| Work schedule (irregular shift work) | 0.37* | 0.16 | 1.44 | 0.04 | 0.19 | 1.04 | .06 |
| Job control | −0.05** | 0.01 | 0.95 | 0.04** | 0.01 | 1.04 | <.001 |
| Work stress | 0.25** | 0.07 | 1.28 | −0.06 | 0.08 | 0.94 | <.001 |
Note. Sample sizes vary from 996 to 1,167 due to different number of missing values for different variables. Reference groups for gender; education; condition; job sector; size of employer, work hours and shift work are: men; secondary or less; healthy; banking/insurance/business/ technology; ≥100 employees; full time and regular shift.
Asterisks denote comparisons between two groups, *p < .05, **p < .01. p-value column denotes overall significance level across all groups.
Multivariable multinomial regression analyses next examined all predictor variables significant at p < .05 comparing accommodation needs met with accommodation needs unmet and accommodation needs met with accommodation needs exceeded (Table 5). Health variables were not significantly associated with unmet or exceeded accommodation needs. Instead, findings indicated that work context variables were related to accommodations. Specifically, participants who worked part-time, OR = 1.72, p < .01; reported less job control, OR = 0.97, p < .01; and more work stress, OR = 1.26, p < .01 were more likely to have unmet accommodation needs as opposed to accommodation needs met. Participants with greater health variability were less likely to have accommodation needs exceeded as compared to needs met, OR = 0.70, p < .01, whereas respondents who reported greater job control were more likely to have accommodation needs exceeded, OR = 1.03, p < .01.
Table 5.
Multivariable Multinomial Regression Analyses of Demographic, Health, and Work Context Factors Associated With Workplace Accommodation Needs Unmet, Met, and Exceeded (n = 1,005)
| Variable | Unmet Needs (n = 217) vs. Needs Met (n = 632) | Needs Exceeded (n = 156) vs. Needs Met (n = 632) | p | ||||
|---|---|---|---|---|---|---|---|
| b | SE | OR | b | SE | OR | ||
| Gender (female) | −0.04 | 0.18 | 0.97 | −0.26 | 0.20 | 0.77 | .44 |
| Pain | 0.06 | 0.05 | 1.06 | 0.02 | 0.05 | 1.02 | .47 |
| Fatigue | 0.00 | 0.02 | 1.00 | 0.01 | 0.02 | 1.01 | .94 |
| Health variability | 0.07 | 0.09 | 1.08 | −0.36** | 0.12 | 0.70 | .01 |
| Health condition | .51 | ||||||
| Arthritis | 0.07 | 0.23 | 1.07 | 0.32 | 0.25 | 1.37 | |
| Diabetes | 0.39 | 0.26 | 1.48 | 0.39 | 0.29 | 1.23 | |
| Both arthritis and diabetes | 0.44 | 0.35 | 1.55 | 0.20 | 0.49 | 1.22 | |
| Job sector | .79 | ||||||
| Education/health/sciences/arts | 0.56 | 0.34 | 1.75 | −0.27 | 0.31 | 0.76 | |
| Construction/utilities | 0.69 | 0.38 | 1.99 | −0.08 | 0.39 | 0.92 | |
| Sales/retail | 0.39 | 0.38 | 1.48 | 0.06 | 0.35 | 1.06 | |
| Manufacturing/agriculture | 0.42 | 0.42 | 1.53 | −0.08 | 0.38 | 0.92 | |
| Government | 0.43 | 0.38 | 1.53 | −0.23 | 0.36 | 0.80 | |
| Work physically demanding | 0.06 | 0.07 | 1.07 | −0.04 | 0.08 | 0.96 | .51 |
| Part-time hours | 0.54* | 0.22 | 1.72 | 0.27 | 0.26 | 1.31 | .04 |
| Work schedule (irregular shift) | −0.01 | 0.19 | 0.99 | 0.06 | 0.23 | 1.07 | .96 |
| Job control | −0.03** | 0.01 | 0.97 | 0.03** | 0.01 | 1.03 | <.001 |
| Work stress | 0.23* | 0.09 | 1.26 | 0.09 | 0.10 | 1.09 | .05 |
Notes. Unmet needs, n = 217; Needs met, n = 632; Needs exceeded, n = 156. Reference groups for gender; condition; job sector; work hours and shift work are: men; healthy; banking/insurance/ business/technology; full time and regular shift.
Asterisks denote comparisons between two groups, *p < .05, **p < .01. p-value column denotes overall significance level across all groups.
Hypotheses 4a–4c further investigated the combination of health and work context as important to older workers’ employment by examining factors associated with job outcomes using ordinary least squares and logistic regression analyses. Specifically, accommodation needs met, unmet and exceeded were included as predictor variables along with age, gender, and health condition and their association examined with workplace activity limitations, job disruptions, productivity losses, and absenteeism (Table 6). Findings showed support for Hypothesis 4a in that age, gender and health condition type were significantly related to several job outcomes. Specifically, younger age was associated with fewer workplace activity limitations, b = −0.06, p < .01; job disruptions, b = −0.03, p < .01; and productivity losses, b = −0.05, p < .01 and being less likely to report absenteeism, OR = 0.94, p < .01. Compared to men, women reported greater workplace activity limitations, b = 0.54, p < .01 and more productivity losses, b = 0.41, p < .01. Compared to healthy controls, having arthritis, b = 2.2, p < .01 or both arthritis/diabetes, b = 3.42, p < .01, was significantly associated with greater workplace activity limitations. Compared to healthy controls, those with arthritis, b =.37, p < .01; diabetes, b = 0.22, p < .05; or with both arthritis/diabetes, b = 0.51, p < .01, had greater job disruptions. Also, those with arthritis, b = 0.71, p <.01, and both arthritis and diabetes, b = 0.78, p < .01, had higher productivity loss compared to health controls. All health conditions were associated with absenteeism. Those with arthritis, OR = 1.65, p < .01; diabetes, OR = 1.78, p < .01; and both arthritis/diabetes, OR = 2.27, p <.01, were more likely to report absenteeism compared to healthy controls. Partial support was found for Hypothesis 4b that predicted having accommodation needs unmet would be related to poorer job outcomes. Respondents with unmet accommodation needs had greater workplace activity limitations than respondents with accommodation needs met, b = 0.95, p < .01. However, there were no significant differences in job disruptions, productivity losses or absenteeism between those with accommodation needs unmet versus met. Greater support was found for Hypothesis 4c, which compared to respondents who had their accommodation needs met to those with accommodation needs exceeded. Respondents who reported their accommodation needs exceeded had fewer workplace activity limitations, b = −0.85, p < .01; job disruptions, b = −0.38, p < .01; and productivity losses, b = −0.66, p < .01.
Table 6.
Multivariable Regression Models Examining Age, Gender, Condition Type and Workplace Accommodation Needs Unmet, Met, and Exceeded With Employment Outcomes
| Variable | Workplace Activity Limitations (n = 1,107) | Job Disruptions (n = 1,153) | Perceived Productivity Losses (n = 1,149) | Absenteeism (n = 1,105) | |||||
|---|---|---|---|---|---|---|---|---|---|
| b | SE | b | SE | b | SE | b | SE | OR | |
| Age | −0.06** | 0.02 | −0.03** | 0.01 | −0.05** | 0.01 | −0.06** | 0.01 | 0.94** |
| Gender | 0.54* | 0.22 | 0.07 | 0.07 | 0.41** | 0.12 | 0.24 | 0.14 | 1.28 |
| Health condition | |||||||||
| Arthritis | 2.20** | 0.25 | 0.37** | 0.09 | 0.71** | 0.14 | 0.50** | 0.17 | 1.65** |
| Diabetes | 0.20 | 0.45 | 0.22* | 0.15 | 0.16 | 0.17 | 0.57** | 0.20 | 1.78** |
| Both arthritis and diabetes | 3.42** | 0.31 | 0.51** | 0.10 | 0.78** | 0.24 | 0.82** | 0.28 | 2.27** |
| Workplace accommodations | |||||||||
| Unmet needs | 0.95** | 0.27 | 0.00 | 0.09 | 0.25 | 0.14 | 0.04 | 0.17 | 1.04 |
| Needs exceeded | −0.85** | 0.31 | −0.38* | 0.10 | −0.66** | 0.17 | −0.40 | 0.22 | 0.67 |
Note. Reference groups for gender; health condition; workplace accommodations are men, healthy controls, workplace accommodation needs met. Absenteeism categorized into two groups: no absences vs. any absences.
*p < .05, **p < .01.
DISCUSSION
As workforces in many developed countries age, there is interest in retaining older workers to manage potential worker shortages and lost expertise. However, previous research suggests that the prevalence of common, age-related chronic conditions like arthritis and diabetes makes sustaining work difficult for many workers (Brault et al., 2007; Helmick et al., 2008; Ilmarinen, 2001; Martin et al., 2009). This study applied work functioning theory to develop a conceptual model that highlights the complexity of working with a chronic health condition and the value of going beyond disease factors to understand work experiences. By including the role of work context, particularly workplace accommodations, we were able to gain a more nuanced understanding of worker needs, factors contributing to having accommodation needs met, unmet or exceeded, and the relationship of accommodations to job outcomes. The findings underscore that working with pain, fatigue and health variability is common, especially among older workers with arthritis or both arthritis/diabetes. However, the results also paint a more positive picture of the potential for older workers to find ways to manage their health at work than previous studies. Need for and use of accommodations was relatively low among those with arthritis and diabetes and often no different from healthy controls. Most respondents reported at least one workplace accommodation available and about two-thirds reported their accommodation needs met in managing their health. Of interest was that unmet accommodation needs were associated with more workplace activity limitations, whereas using accommodations in advance of health needs was associated with fewer workplace activity limitations, job disruptions, and productivity losses. Additional research is needed, but the results are promising in terms of pointing to ways that workplaces may help older workers with chronic diseases sustain work.
Health Findings
Respondents were diverse in demographic, health and work characteristics with many similarities in work context across the health conditions. However, those with arthritis or both arthritis/diabetes reported poorer health and employment outcomes than healthy controls. These findings are similar to previous arthritis studies which show that, although workers with arthritis are more likely to give up employment than healthy adults, many remain working or return to work, but may struggle to manage pain, fatigue, and functional limitations in the workplace (Burton et al., 2006; Geuskens, Hazes, Barendregt, & Burdorf, 2008; Kaptein, et al., 2009; Lenssinck et al., 2013). Of interest was that respondents with diabetes were similar to healthy controls in many respects, although they reported their health as more variable. The current study suggests that many individuals with diabetes may work with little or only an occasional impact on their jobs, but difficulties with health and work become considerable with co-morbidity, such as arthritis. At the same time, we recruited fewer respondents with diabetes than other health groups. Data replicating these findings are important, as well as new research including individuals who have had to forgo employment.
Work Functioning: Theoretical and Practical Implications
Accommodation availability
This is one of the first studies that applied work functioning theory to being employed with a chronic disease and asked not only about health variables, but also the availability, need for, and use of diverse workplace accommodations. We had expected that respondents across different health conditions would be similar in their reports of the availability of accommodations in their workplace. However, respondents with both arthritis/diabetes reported less availability of accommodations than healthy controls. It is unclear why this was the case, given that respondents were largely similar in terms of job sector, size of organization, hours worked per week, and need for and use of accommodations. Most participants also reported being aware of the policies and practices available in their organization. Additional research is needed, particularly related to whether there are differences in who is given access or permission to use accommodations or whether accommodations become less available among those who frequently use them. For example, work functioning theory underscores the importance of understanding the broader workplace culture and social environment of workers, in addition to workplace policies and practices. Managers may vary in their perceptions of the legitimacy of some types of accommodations as being necessary for older workers to manage their work and health demands and may not make them available. Repeated or extensive use of an accommodation may be perceived as putting a hardship on others in the organization and supervisors may be less willing or able to provide them on an ongoing basis. If this is the case, it may have influenced perceptions of lower availability among workers, especially those with both arthritis and diabetes. Additional research examining frequency of accommodation use and the role of supervisors and coworkers in supporting accommodation needs is important. This includes international, comparative studies that examine similarities and differences in organizational practices and labor policies aimed at encouraging workplaces to support and accommodate workers with disabilities, including older workers.
Accommodation needs met, unmet and exceeded
Similar to previous studies we found that, despite health difficulties, many individuals with arthritis and/or diabetes reported relatively low levels of accommodation use (Dhanhani et al., 2015; Chen et al., 2007; Gignac et al., 2015; Yelin et al., 2000). We expanded on previous research not only by assessing the need for accommodations, but also by measuring whether accommodations were met, unmet, or exceeded. Of interest was that over 60% of respondents reported their accommodation needs were met and up to a further 16% reported their accommodation needs exceeded. These findings may be related to the episodic nature of arthritis and diabetes symptoms where many individuals may not need accommodations on a continual basis (Gignac et al., 2011). The variety of workplace practices available and the intermittent nature of symptoms also may mean that workers were able to find different ways to manage their health at work. These findings have implications for the workplace and suggest that older workers with chronic diseases may not be a drain on workplace resources, but largely may be able to manage their conditions with existing policies and practices available in Canadian workplaces. However, additional research is needed in other jurisdictions. The findings also have implications for work functioning theory and highlight the need for greater theoretical attention to changes in disability and functioning over time that may be related both to changes in health and to changes that result from adopting diverse accommodations.
Of interest was that a number of older workers used workplace accommodations in the absence of a health need. This finding is not surprising as many workplace policies and practices were created to meet diverse personal and lifestyle situations that go beyond health problems. Yet, additional research examining workers that we labeled as having accommodation needs exceeded would be useful. Although we assessed a variety of accommodation policies, we did not measure perceptions of workplace culture. It may be that, compared to respondents whose needs were met or unmet, older workers who used workplace practices in the absence of health needs perceived their workplace as having a positive and supportive culture that encouraged proactive use of accommodations and fostered workplace wellness. Additional research in this area could help inform human resource and disability management practices in workplaces, particularly research focusing on the costs of unmet needs versus proactive use of existing policies.
The importance of work context
As noted, research on arthritis and diabetes has largely adopted a medical model and focused on disease symptoms to understand workplace disability and job outcomes. In examining accommodation needs met, unmet and exceeded, and the factors associated with them, this research highlighted the importance of work context in understanding work functioning. In particular, multivariable analyses found that having accommodation needs unmet or exceeded was largely related to work context, not health. This finding supports work functioning theory and other more general biopsychosocial models of health, which emphasize that disability does not reside solely in the individual, but is a complex interaction among personal, workplace, social and environmental conditions (De Rijk, 2013; Sandqvist & Henriksson, 2004; WHO, 2001). Specific findings pointed to part-time hours as one factor associated with unmet accommodation needs. It may reflect that part-time workers are less likely to have available to them some policies and benefits like extended health benefits and flexible work hours. At the same time, part-time work may give workers with chronic health conditions greater flexibility to redress difficulties with fatigue and to meet health treatment demands, and it is often selected as a preferred job arrangement among older workers (Beehr, 2014; Cooke, 2006; Ekerdt, 2010; Feldman & Beehr, 2011; Gignac et al., 2012; Nilsson et al., 2011; Wang et al., 2008). Additional research is needed to more fully understand the role of part-time work as a barrier or facilitator to work disability and sustaining employment. It may be that respondents in this study, especially those living with arthritis and/or diabetes, did not choose part-time hours as a lifestyle choice, but found that their condition made it difficult to work full-time or that full-time jobs were not available to them. A further negative consequence of working part-time was that many were no longer eligible for some types of accommodations.
Job control also was related to accommodations with greater job control being associated with having accommodation needs exceeded and less control being related to having accommodation needs unmet. Although the current data are cross-sectional and a causal direction for the relationships are unclear, job control has been studied extensively in the workplace literature and is associated with a range of positive work outcomes (De Jonge et al., 1999; De Rijk, 2013; Karasek & Theorell, 1990; Kristman et al., 2016). The importance of job control as a predictor of accommodation use suggests that, in addition to the presence of accommodation policies, work environments that provide older workers with greater levels of control may enable them to take better advantage of accommodations, which ultimately could help older workers sustain employment.
Employment outcomes and the need for research on the timing of accommodation use
Finally, previous research on chronic diseases like arthritis and diabetes has emphasized the negative impact of age and health on presenteeism and absenteeism (Allaire et al., 2005; Boonen, 2006; Burton et al., 2006; Kaptein et al., 2009). The relationship of accommodations to job outcomes has not been extensively examined. We found that greater age, having arthritis, or both arthritis/diabetes was related to more workplace activity limitations, job disruptions, perceived productivity losses, and absenteeism. Women were also more likely to report greater workplace activity limitations and productivity losses than men. These findings are in keeping with previous studies (Allaire et al., 2005; Burton et al., 2006; Ilmarinen, 2001; Kaptein et al., 2009; Martin et al., 2009; Wallenius et al., 2009). When accommodation needs met, unmet and exceeded were added to the model, having accommodation needs unmet was significantly related to greater workplace activity limitations. There were no significant differences between having accommodation needs met or unmet in job disruptions, productivity losses or absenteeism. The lack of differences may relate to the timing of accommodation use. In the current study, it is unclear whether respondents largely avoided using accommodations until they experienced declines in job performance or health crises. Some previous research suggests that this may be the case (Gignac et al., 2011). If so, it may explain why respondents with accommodation needs met were similar to those with accommodation needs unmet in terms of many of the job outcomes examined. Increased job disruptions and productivity losses could have been the signal for some workers to initiate the use of accommodations.
Alternatively, having accommodation needs exceeded (i.e., using accommodations in advance of a difficulty or need) was related to fewer workplace activity limitations and job disruptions and less productivity loss than having accommodation needs met. Additional research is needed, particularly as we lack longitudinal data to unravel cause-effect relationships. However, the results point to potential benefits to a proactive approach in using accommodations, which may help individuals avoid workplace difficulties from occurring. The findings also have theoretical implications for enhancing work functioning theory. Although there is some attention to changes in function over time, there is little consideration of decision making related to the timing of workplace management efforts or support seeking (Sandqvist & Henriksson, 2004).
Notably, there were no differences in absenteeism related to having accommodation needs met or exceeded. The reason may be because health-related absences were relatively low, although they are in keeping with other studies (Lenssinck et al., 2013). It also may be that some absenteeism is necessary and beneficial to those with arthritis and diabetes to maintain good health, to enable individuals to seek treatment, and to ultimately sustain employment. Further information about the reasons for absenteeism would illuminate whether absences are in response to problems with health or are part of good health habits and regular treatment.
Study Limitations
Several study limitations need acknowledgment. As noted, the cross-sectional nature of the data precluded examination of changes and clarifying the temporal relationships between use of accommodations and health and job outcomes. Longitudinal studies would improve the assessment of cause and effect and allow us to further statistically test our conceptual model, including the role of accommodations as a mediator between health and employment outcomes. Longitudinal research would also help address potential healthy worker effects where older workers whose health is poorer or who are unable to access accommodations may be more likely to give up work. As such, future studies need to better understand the accommodation experiences of those who have left employment as well as those who remain working. However, it is noteworthy that participants with arthritis and diabetes were working with considerable pain, fatigue, and health variability, which is in keeping with samples from other studies. This study is also limited in using a survey methodology and self-report to assess health and workplace variables, which may have introduced a number of sources of sample and response biases into the data (Becker, 2005; Podsakoff, MacKenzie, & Podsakoff, 2012). Although self-report data are frequently used in epidemiological studies and, where available, we included measures with reported validity, additional research would be beneficial to further assess the validity and generalizability of the findings, especially in international settings. We also focused on workers aged 50+ years, which limits the generalizability of the findings. Including respondents of different ages, as well as variables like ethnicity, would enable insights into whether findings are unique or similar across age and culture and would enhance our conceptual model. Important in future studies is also to include employer and co-worker perspectives on older workers with chronic diseases and organizational willingness and ability to provide accommodations over time.
CONCLUSION
In conclusion, our study is among the first to apply work functioning theory to examine the use of existing workplace practices among baby boomers with different health conditions. The findings suggest that, regardless of whether workers had common age-related health conditions, their accommodation needs were often met by existing policies and may not be an additional drain on workplace resources. Moreover, having accommodation needs unmet or exceeded was largely related to workplace factors like job control, which may be modifiable in many workplaces. Finally, future research and theoretical attention are needed related to better understanding the timing of accommodation use and whether proactive adoption of workplace practices can improve health and employment outcomes.
ACKNOWLEDGMENTS
This research was funded by a grant from the Canadian Institutes of Health Research (CIHR) MOP#130427. The Institute for Work and Health operates with the support of the Province of Ontario. The views expressed herein are those of the authors and do not necessarily reflect those of the Province of Ontario.
REFERENCES
- Allaire S. H., Wolfe F., Niu J., LaValley M., & Michaud K (2005). Work disability and its economic effect on 55-64-year-old adults with rheumatoid arthritis. Arthritis Care and Research, 53, 603–608. doi:10.1002/art.21326 [DOI] [PubMed] [Google Scholar]
- American Association of Retired Persons (A.A.R.P.) (2002). Beyond 50: A report to the nation on trends in health security. Washington, DC: Author. [Google Scholar]
- Bal A. C., Reiss A. E., Rudolph C. W., & Baltes B. B (2011). Examining positive and negative perceptions of older workers: A meta-analysis. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 66, 687–698. doi:10.1093/geronb/gbr056 [DOI] [PubMed] [Google Scholar]
- Beaton D. E., Tang K., Gignac M. A. M., Lacaille D., Badley E. M., Anis A. H., & Bombardier C (2010). Reliability, validity and responsiveness of five at-work productivity measures in persons with rheumatoid arthritis or osteoarthritis: A 12-month multi-centre study. Arthritis Care & Research, 62, 28–37. doi:10.1002/acr.20011 [DOI] [PubMed] [Google Scholar]
- Becker T. E. (2005). Potential problems in the statistical control of variables in organizational research: A qualitative analysis with recommendations. Organizational Research Methods, 8, 274–289. doi:10.1177/1094428105278021 [Google Scholar]
- Beehr T. A. (2014). To retire or not to retire: That is not the question. Journal of Organizational Behaviour, 35, 1093–1108. doi:10.1002/job.1965 [Google Scholar]
- Boonen A. (2006). A review of work-participation, cost-of-illness and cost-effectiveness studies in ankylosing spondylitis. Nature Clinical Practice Rheumatology, 2, 546–553. doi:10.1038/ncprheum0297 [DOI] [PubMed] [Google Scholar]
- Brault M. W., Hootman J., Helmick C. G., Theis K. A. & Armour B. S (2009). Prevalence and most common causes of disability among adults-United States, 2005. Morbidity and Mortality Weekly Report, 58, 421–426. [PubMed] [Google Scholar]
- Burton W., Morrison A., Maclean R. & Ruderman E (2006). Systematic review of studies of productivity loss due to rheumatoid arthritis. Occupational Medicine, 56, 18–27. doi:10.1093/occmed/kqi171 [DOI] [PubMed] [Google Scholar]
- Chen J. C., Linnan L., Callahan L. F., Yelin E. H., Renner J. B., & Jordan J. M (2007). Workplace policies and prevalence of knee osteoarthritis: The Johnston county osteoarthritis project. Occupational & Environmental Medicine, 9, 798–805. doi:10.1136/oem.2006.030148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke M. (2006). Policy changes and the labour force participation of older workers: Evidence from six countries. Canadian Journal on Aging, 25, 387–400. doi:10.1353/cja.2007.0015 [DOI] [PubMed] [Google Scholar]
- Cranford C. J., Vosko L. F., & Zukewich N (2003). Precarious employment in the Canadian labour market: A statistical portrait. Just Labour, 3 Retrieved from http://justlabour.journals.yorku.ca/index.php/justlabour/article/view/164 [Google Scholar]
- De Jonge J., Van Breukelen G. J., Landeweerd J. A., & Nijhuis F. J. N (1999). Comparing group and individual level assessments of job characteristics in testing the job demand-control model: A multilevel approach. Human Relations, 52, 95–122. doi:10.1023/ A:1016924517061 [Google Scholar]
- De Rijk A. (2013). Work disability theories: A taxonomy for researchers. In: Loisel P. & Anema J. R. (Eds.), Handbook of work disability (pp. 475–499). New York, NY: Springer Publishing. doi: 69.156.147.253 [Google Scholar]
- Dhanhani A. M. A., Gignac M. A., Beaton D. E., Su J. & Fortin P. R (2015). Job accommodation availability and utilization among people with lupus: An examination of workplace activity limitations and work context factors. Arthritis Care and Research, 61, 378–385. doi:10.1002/acr.22662 [DOI] [PubMed] [Google Scholar]
- Dwyer D. J. & Ganster D. C (1991). The effects of job demand and control on employee attendance and satisfaction. Journal of Organizational Behaviour, 12, 595–608. doi:10.1002/job.4030120704 [Google Scholar]
- Ekerdt D. J. (2010). Frontiers of research on work and retirement. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 65, 69–80. doi:10.1093/geronb/gbp109 [DOI] [PubMed] [Google Scholar]
- Feldman D. C., & Beehr T. A (2011). A three-phase model of retirement decision making. American Psychologist, 66, 193–203. doi:10.1037/a0022153 [DOI] [PubMed] [Google Scholar]
- Galarneau D. & Radulescu M (2009). Employment among the disabled. Perspectives on Labour and Income, 10. Ottawa, ON, Canada: Statistics Canada. [Google Scholar]
- Geuskens G. A., Hazes J. M. W., Barendregt P. J. & Burdorf A (2008). Predictors of sick leave and reduced productivity at work among persons with early inflammatory joint conditions. Scandinavian Journal of Work, Environment and Health, 34, 420–429. Retrieved from http://www.jstor.org/stable/40967739 [DOI] [PubMed] [Google Scholar]
- Gignac M. A. (2005). Arthritis and employment: An examination of behavioural coping efforts to manage workplace activity limitations. Arthritis Care & Research, 53, 328–336. doi:10.1002/art.21169 [DOI] [PubMed] [Google Scholar]
- Gignac M. A. M., Backman C. L., Kaptein S., Lacaille D., Beaton D. E., Hofstetter C., & Badley E. M (2012). Tension at the borders: Perceptions of role overload, conflict, strain and facilitation in work, family and health roles among employed individuals with arthritis. Rheumatology, 51, 324–332. doi:10.1093/rheumatology/ker317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gignac M. A. & Cao X (2009). “Should I tell my employer and coworkers I have arthritis?” A longitudinal examination of self-disclosure in the work place. Arthritis and Rheumatism, 61, 1753–1761. doi:10.1002/art.24889 [DOI] [PubMed] [Google Scholar]
- Gignac M. A., Cao X., Lacaille D., Anis A. H. & Badley E. M (2008). Arthritis-related work transitions: A prospective analysis of reported productivity losses, work changes, and leaving the labor force. Arthritis Care and Research, 59, 1805–1813. doi:10.1002/art.24085 [DOI] [PubMed] [Google Scholar]
- Gignac M. A., Cao X. & McAlpine J (2015). Availability, need for, and use of work accommodations and benefits: Are they related to employment outcomes in people with arthritis?Arthritis Care & Research, 67, 855–864. doi:10.1002/acr.22508 [DOI] [PubMed] [Google Scholar]
- Gignac M. A., Cao X., Tang K. & Beaton D. E (2011). Examination of arthritis-related work place activity limitations and intermittent disability over four-and-a-half years and its relationship to job modifications and outcomes. Arthritis Care and Research, 63, 953–962. doi:10.1002/acr.20456 [DOI] [PubMed] [Google Scholar]
- Gignac M. A., Sutton D. & Badley E. M (2007). Arthritis symptoms, the work environment, and the future: Measuring perceived job strain among employed persons with arthritis. Arthritis & Rheumatism, 57, 738–747. doi:10.1002/art.22788 [DOI] [PubMed] [Google Scholar]
- Glasgow R. E., & Eakin E. G (1998). Issues in diabetes self-management. In A. Sally , E. B. Schron , J. K. Ockene & W. L. McBee (Eds.), The handbook of health behaviour change (2nd ed., pp 435–461). New York, NY: Springer Publishing Co. [Google Scholar]
- Helmick C. G., Felson D. T., Lawrence R. C., Gabriel S., Hirsch R., Kwoh C. K., …Liang M. H (2008). Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Arthritis & Rheumatism, 58, 15–25. doi:10.1002/art.23177 [DOI] [PubMed] [Google Scholar]
- Henkens K. (2005). Stereotyping older workers and retirement: The managers’ point of view. Canadian Journal on Ageing/La Revue Canadienne du Vieillissement, 24, 353–366. doi:10.1353/cja.2006.0011 [Google Scholar]
- Herquelot E., Guéguen A., Bonenfant S. & Dray-Spira R (2011). Impact of diabetes on work cessation data from the GAZEL cohort study. Diabetes Care, 34, 1344–1349. doi:10.2337/dc10-2225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilmarinen J. E. (2001). Ageing workers. Occupational and Environmental Medicine, 58, 546. doi:10.1136/oem.58.8.546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanavos P., van den Aardweg S., & Schurer W (2012). Diabetes expenditure, burden of disease and management in 5 EU countries. London, UK: London School of Economics. [Google Scholar]
- Kaptein S. A., Gignac M. A. & Badley E. M (2009). Differences in the workforce experiences of women and men with arthritis disability: A population health perspective. Arthritis Care & Research, 61, 605–613. doi:10.1002/art.24427 [DOI] [PubMed] [Google Scholar]
- Karasek R., & Theorell T (1990). Healthy work: Stress, productivity, and reconstruction of working life. New York, NY: Basic Books. [Google Scholar]
- Kooij D., de Lange A., Jansen P., & Dikkers J (2008). Older workers’ motivation to continue to work: Five meanings of age: A conceptual review. Journal of Managerial Psychology, 23, 364–394. doi:10.1108/02683940810869015 [Google Scholar]
- Kristman V. L., Shaw W. S., Boot C. R. L., Delclos G. L., Sullivan M. J., Ehrhart M. G.,& the Hopkinton Conference Working Group on Workplace Disability Prevention. (2016). Researching complex and multi-level workplace factors affecting disability and prolonged sickness absence. Journal of Occupational Rehabilitation, 26, 399–416. doi:10.1007/s10926-016-9660-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacaille D., White M. A., Backman C. L. & Gignac M. A (2007). Problems faced at work due to inflammatory arthritis: New insights gained from understanding patients’ perspective. Arthritis Care & Research, 57, 1269–1279. doi:10.1002/art.23002 [DOI] [PubMed] [Google Scholar]
- Latif E. (2009). The impact of diabetes on employment in Canada. Health Economics, 18, 577–589. doi:10.1002/hec.1390 [DOI] [PubMed] [Google Scholar]
- Lenssinck M. L., Burdorf A., Boonen A., Gignac M. A. M., Hazes J. M. W. & Luime J. J (2013). Consequences of inflammatory arthritis for workplace productivity loss and sick leave: A systematic review. Annals of the Rheumatic Diseases, 72, 493–505. doi:10.1136/annrheumdis-2012-201998 [DOI] [PubMed] [Google Scholar]
- Leveille S. G., Wee C. C. & Iezzoni L. I (2005). Trends in obesity and arthritis among baby boomers and their predecessors 1971–2002. American Journal of Public Health, 95, 1607–1613. doi:10.2105/AJPH.2004.060418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Gignac M. A. & Anis A. H (2006). The indirect costs of arthritis resulting from unemployment, reduced performance, and occupational changes while at work. Medical Care, 44, 304–310. doi:10.1097/01.mlr.0000204257.25875.04 [DOI] [PubMed] [Google Scholar]
- Lipscombe L. L. & Hux J. E (2007). Trends in diabetes prevalence, incidence, and mortality in Ontario, Canada 1995–2005: A population-based study. Lancet, 369, 750–756. doi:10.1016/S0140-6736(07)60361-4 [DOI] [PubMed] [Google Scholar]
- Loisel P., & Côté P (2013). The work disability paradigm and its public health implications. In P. Loisel & J. R. Anema (Eds.), Handbook of work disability: Prevention and management (pp. 59–67). New York, NY: Springer Publishing Co. doi:10.1007/978-1-4614-6214-9_5 [Google Scholar]
- Martin L. G., Freedman V. A., Schoeni R. F. & Andreski P. M (2009). Health and functioning among baby boomers approaching 60. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 64B, 369–377. doi:10.1093/geronb/gbn040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNair D. M., Douglas M., Lorr M. & Droppleman L. F (1971). Manual for the profile of mood states. San Diego, CA: Educational and Industrial Testing Service. [Google Scholar]
- Mermin G. B. T., Johnson R. W. & Murphy D. P (2007). Why do boomers plan to work longer?Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 62, S286. doi:10.1093/geronb/62.5.S286 [DOI] [PubMed] [Google Scholar]
- Ng T. W. & Feldman D. C (2013). A meta-analysis of the relationships of age and tenure with innovation-related behaviour. Journal of Occupational and Organizational Psychology, 86, 585–616. doi:10.1111/joop.12031 [Google Scholar]
- Nilsson K., Hydbom A. R., & Rylander L (2011). Factors influencing the decision to extend working life or retire. Scandinavian Journal of Work, Environment & Health, 37, 473–480. Retrieved from http://www.jstor.org/stable/23064882 [DOI] [PubMed] [Google Scholar]
- Nyce S. A. & Schieber S. J (2005). The economic implications of ageing societies: The costs of living happily ever after. Cambridge, UK: Cambridge University Press. [Google Scholar]
- Padavic I., & Reskin B. F (2002). Women and men at work (2nd ed). Thousand Oaks, CA: Pine Forge Press. [Google Scholar]
- Park J. (2011). Retirement, health, and employment among those 55 plus. Perspectives on Labour and Income, Statistics Canada Catalogue, 75-001-X, 5–13. [Google Scholar]
- Perruccio A. V., Power J. D. & Badley E. M (2007). The relative impact of 13 chronic conditions across three different outcomes. Journal of Epidemiology and Community Health, 61, 1056–1061. doi:10.1136/jech.2006.047308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pignal J., Arrowsmith S. & Ness A (2010). First results from the survey of older workers, 2008. Ottawa, ON: Statistics Canada. [Google Scholar]
- Podsakoff P. M., MacKenzie S. B., & Podsakoff N. P (2012). Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology, 63, 539–569. doi:10.1146/annurev-psych-120710-100452 [DOI] [PubMed] [Google Scholar]
- Polonsky W. H. (2000). Understanding and assessing diabetes-specific quality of life. Diabetes Spectrum, 13, 36–41. [Google Scholar]
- Pransky G. (2013). Measurement of outcomes in WDP: Conceptual and methodological considerations and recommendations for measuring outcomes. In P. Loisel & J. R. Anema (Eds.), Handbook of work disability: Prevention and Management (pp. 95–106). New York, NY: Springer Publishing Co. doi:10.1007/978-1-4614-6214-9_7 [Google Scholar]
- Public Health Agency of Canada (2010). Life with Arthritis in Canada: A personal and public health challenge. Ottawa, ON: Public Health Agency of Canada. [Google Scholar]
- Public Health Agency of Canada (2011). Diabetes in Canada: Facts and figures from a public health perspective. Ottawa, ON: Public Health Agency of Canada. [Google Scholar]
- Reilly M. C., Zbrozek A. S. & Dukes E. M (1993). The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics, 4, 353. [DOI] [PubMed] [Google Scholar]
- Sandqvist J. L. & Henriksson C. M (2004). Work functioning: A conceptual framework. Work, 23, 147–157. [PubMed] [Google Scholar]
- SAS/STAT User’s Guide, Version 9.3. (2012). Cary, NC: SAS Institute Inc. [Google Scholar]
- Shaw J. E., Sicree R. A. & Zimmet P. Z (2010). Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Research and Clinical Practice, 87, 4–14. doi:10.1016/j.diabres.2009.10.007 [DOI] [PubMed] [Google Scholar]
- Smith P., Bielecky A. & Mustard C (2012). The relationship between chronic conditions and work-related injuries and repetitive strain injuries in Canada. Journal of Occupational and Environmental Medicine, 54, 841–846. doi:10.1097/JOM. 0b013e31824e11f7 [DOI] [PubMed] [Google Scholar]
- Srikanth V. K., Fryer J. L., Zhai G., Winzenberg T. M., & Hosmer D (2005). A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis & Cartilage, 13, 769–781. doi:10.1016/j.joca.2005.04.014 [DOI] [PubMed] [Google Scholar]
- Tengland P-A. (2011). The concept of work ability. Journal of Occupational Rehabilitation, 21, 275–285. doi:10.1007/s10926-010-9269-x [DOI] [PubMed] [Google Scholar]
- Vijan S., Hayward R. A. & Langa K. M (2004). The impact of diabetes on workforce participation: Results from a national household sample. Health Services Research, 39, 1653–1670. doi:10.1111/j.1475-6773.2004.00311.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Vollenhoven R. F. (2009). Sex differences in rheumatoid arthritis: More than meets the eye. BMC Medicine, 7, 1–4. doi:10.1186/1741-7015-7-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallenius M., Skomsvoll J. F., Koldingsnes W., Rødevand E., Mikkelsen C., Kaufmann C., & Kvien T. K (2009). Comparison of work disability and health-related quality of life between males and females with rheumatoid arthritis below the age of 45 years. Scandinavian Journal of Rheumatology, 38, 178–183. doi:10.1080/03009740802400594 [DOI] [PubMed] [Google Scholar]
- Wang M., Zhan Y., Liu S. & Shultz K. S (2008). Antecedents of bridge employment: A longitudinal investigation. Journal of Applied Psychology, 93, 818. [DOI] [PubMed] [Google Scholar]
- Wasef S. Z. Y. (2004). Gender differences in systemic lupus erythematosus. Gender & Medicine, 1, 12–17. doi:10.1016/S1550-8579(04)80006-8 [DOI] [PubMed] [Google Scholar]
- Watkins K. W., Connell C. M., Fitzgerald J. T., Klem L., Hickey T. & Ingersoll-Dayton B (2000). Effect of adults’ self-regulation of diabetes on quality of life outcomes. Diabetes Care, 23, 1511–1515. doi:10.2337/diacare.23.10.1511 [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) (2001). International classification of functioning, disability and health: ICF. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Yelin E., Cisternas M. G., Pasta D. J., Trupin L., Murphy L. & Helmick C. G (2004). Medical care expenditures and earnings losses of persons with arthritis and other rheumatic conditions in the United States in 1997: Total and incremental estimates. Arthritis and Rheumatism, 50, 2317–2326. doi:10.1002/art.20298 [DOI] [PubMed] [Google Scholar]
- Yelin E., Sonneborn D., & Trupin L (2000). The prevalence and impact of accommodations on the employment of persons 51–61 years of age with musculoskeletal conditions. Arthritis Care and Research, 13, 168–176. doi:10.1002/1529-0131(200006)13:3<168::AID-ANR6>3.0.CO;2-R [DOI] [PubMed] [Google Scholar]
- Zhang W., Gignac M. A., Beaton D., Tang K., Anis A. H.,& Canadian Arthritis Network Work Productivity Group. (2010). Productivity loss due to presenteeism among patients with arthritis: Estimates from 4 instruments. Journal of Rheumatology, 37, 1805–1814. doi:10.3899/jrheum.100123 [DOI] [PubMed] [Google Scholar]