Abstract
As peritoneal dialysis (PD)-related fungal infection is associated with a high mortality rate, the international guidelines recommend immediate removal of the PD catheter in conjunction with at least 2-weeks of antifungal treatment. Some authors have reported successful management of such cases without removing the PD catheter - by instilling an antifungal lock into the retained PD catheter. However, the use of antifungal locks has generally not been well accepted as the standard treatment for fungal peritonitis in PD patients. We report two cases where antifungal lock were performed in PD patients presented with PD-related fungal infection that not only had no effect on abating the infection but also causing paradoxical outcomes.
Keywords: Peritoneal dialysis (PD), Paradoxical, Fungal peritonitis, Intracatheter
1. Introduction
Fungal peritonitis is rare but has an extremely poor outcome resulting in high rates of technical failure and death [1], [2]. Leaving the PD catheter in situ was associated with significantly increased mortality [2], [3]. Therefore, the 2016 update of the International Society of PD (ISPD) Guidelines recommends that the PD catheter should be removed immediately (1C) and for appropriate antifungal agents to be administered for at least 2 weeks following PD catheter removal (2C) when fungi are identified in the PD effluent [4]. However, there have been two reports of fungal peritonitis in patients who were successfully treated by intracatheter antifungal retention of amphotericin B 1–1.5 mg combined with systemic antifungal therapy without the need for PD catheter removal [5], [6]. Moreover, a high salvage rate of central and peripheral lines; including Hickman, central venous, Broviac, and peripheral catheters using anti-fungal lock therapy has been reported with various choices of antifungal regimens such as amphotericin B, anidulafungin, caspofungin, ethanol, fluconazole, and itraconazole [7], [8], [9], [10], [11], [12], [13], [14], [15]. The authors here present 2 cases with deleterious complications when using antifungal locks in the treatment of PD-associated fungal infection.
2. Case
2.1. Case 1
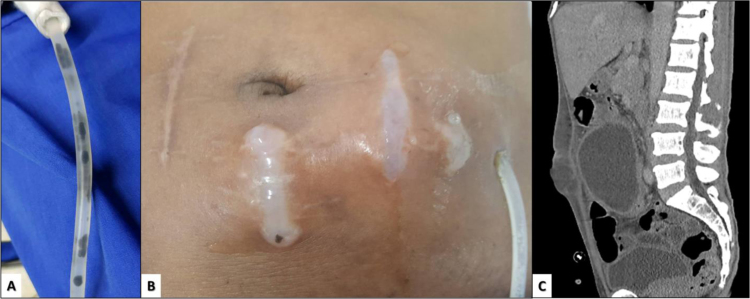
A 60-year-old man with a past medical history of diabetes, hypertension, and cerebrovascular disease was diagnosed with end-stage kidney disease from diabetes in May 2014. He commenced continuous ambulatory PD (1.5%D x 4 exchanges/day) while maintaining adequate dialysis clearance since June 2014 and has never experienced either peritonitis or exit-site infections (ESI). He had no residual renal function (RRF). During the follow-up (28 July 2017), dark-stained particles were observed inside the PD catheter lumen (Fig. 1A). The patient was clinically well with no symptoms of fever, abdominal pain, or cloudy PD effluent. Analysis of the dialysate effluent on day 0 revealed no leukocytes and there was no growth for organisms. On the same day, the dialysate and serum galactomannan (GM) index were 1.29 (<0.5) and 0.68 (<0.5), respectively, both of which were considered positive. In addition, the PCR for broad-range fungal DNA detection using internal transcribed spacer (ITS) primer and standard PCR protocol yielded a positive result [16]. Because the PCR product had only been retrieved in a small amount, gene sequencing analysis was not possible. However, the provisional diagnosis of asymptomatic fungal colonization was made. On the following day, (day +1) the primary physician administered the antifungal lock; amphotericin B (5 mg/mL in 6 mL) into the PD catheter that was subsequently prescribed once a day. On day +3, the patient developed clinical peritonitis and septicemia (temperature of 38 °C, pulse rate of 102/min, and blood pressure of 115/70 mmHg). The dialysate leukocyte went from no detectable level on day 0 up to 900/mm3 (neutrophil 70%). The serum GM index was repeated on day +3 and also showed a dramatic increase from 0.68 to 1.57 making the diagnosis of fungal peritonitis highly likely. Having confirmed all the initial test results, intravenous amphotericin B was promptly started on day +3. Urgent surgical consultation was requested resulting in the timely removal of the PD catheter on day +7. Potassium hydroxide (KOH) examination of the dark particles collected from the removed PD catheter revealed dematiaceous mold. The dialysate culture for fungus from day 0 later yielded Fusarium spp. similar to those isolated from the removed PD catheter on day +7. The patient was transferred to hemodialysis following PD catheter removal. The patient continued to improve, while intravenous amphotericin was prescribed for a total of 2 months. After discharge from hospital, the attending physician arranged a follow-up visit for the patient to reevaluate the possibility of returning to PD, but the patient developed major psychogenic trauma following their prolonged hospitalization and declined all further hospital visits. He was reported dead at home 5 months after the first report of fungal particles in the PD catheter (day +154).
Fig. 1.
A) Dark particle inside the peritoneal catheter lumen in Case 1 B) Subcutaneous and tunnel abscesses with surrounding inflamed and swollen skin in Case 2 C) Computerized tomography demonstrates soft tissue collection under the inflamed skin.
2.2. Case 2
A 55-year-old Thai male farmer with ESRD due to long-standing hypertension who had been on CAPD (1.5%D x 4 exchanges/day) for 2 years presented at the PD clinic with acute abdominal pain and bloody dialysate. He had a recent history of culture-negative peritonitis on day −55 having received a 2-week course of intravenous cefazolin 1 gm/day and ceftazidime 1 gm/day. He reported no previous episodes of exit-site infection (ESI) and had a urine output of 500–1500 mL/day. Physical examination on day 0 (10 Dec 17) was unremarkable except for mild generalized abdominal tenderness. The dialysate cell count on day 0 showed numerous erythrocytes and leukocyte 1200/mm3, 70% of which were neutrophils. He was initially diagnosed with PD-related peritonitis and received a combination of intraperitoneal cefazolin and ceftazidime on the same day resulting in partial resolution of the abdominal pain. On day +12, culture from the PD effluent on day 0 came back positive for Trichosporon asahii. He was diagnosed with fungal peritonitis requiring administration of intravenous amphotericin B, 0.5 mg/kg/day and oral fluconazole 200 mg/day. However, the patient refused to transfer to hemodialysis because he lived in a remote rural area where no hemodialysis facility was available. After discussing about the risks and benefits with the patient a daily antifungal lock of amphotericin B; 5 mg/mL in 6 mL was commenced on day +18 in order to preserve the PD catheter. Although the PD effluent became clear and the dialysate leukocyte gradually decreased, the leukocyte still persisted at more than 100/mm3 with neutrophil predominance. On day +35, despite combined systemic antifungal therapy and intracatheter antifungal locks, the patient developed-increased abdominal pain. On examination, there was a localized erythematous swelling (10 ×10 cm) with marked tenderness and fluctuation along the subcutaneous tunnel of the PD catheter and incisional scar (Fig. 1B). Computerized tomography of the whole abdomen was performed on day +52 displaying a large subcutaneous fluid collection (Fig. 1C). At that stage, the patient was likely having refractory fungal peritonitis with tunnel and subcutaneous abscesses. Following surgical consult, the PD catheter was removed on day +53. The removed PD catheter demonstrated multiple clumps of clear-colored particles adhered to the internal surface (Fig. 1B). KOH smear of the intraluminal scrape revealed yeast-like organism with septated hyphae and arthroconidia. Culture from the catheter scrape on day +53 also isolated Trichosporon asahii. The patient and family refused long-term hemodialysis but agreed only to continuation of oral antifungal treatment. He was discharged from the hospital on day +72 and eventually the patient passed away at home on day +105.
3. Discussion
PD catheter removal is the mainstay for the treatment of complicated infection in PD, including fungal peritonitis. While emergent PD catheter removal has been suggested to improve patient outcomes in many studies, some authors recommend delayed removal in light of the potential benefits to enable peritoneal lavage using antifungal agents in the first few days. Moreover, there were some reports in which patients with fungal peritonitis were treated successfully by utilizing a combination of systemic antifungal therapy and intracatheter antifungal lock therapy without the need for PD catheter removal [6], [17], [18] given the fact that several options for treating fungal peritonitis in PD patients were possible. Although the ISPD guidelines 2016 recommends immediate peritoneal catheter removal if fungi are identified in the PD effluent, the level of evidence is graded as “low”, and the guidelines do not mention about intracatheter antifungal locks nor do they discourage this practice. Hence, antifungal locks may be considered as an option for fungus-related infection for PD patients in some centers particularly when PD catheter removal is not feasible or has been refused by the patient. Anyhow, according to these present cases, antifungal locks may not always be successful and could result in paradoxical complications.
The first scenario was an asymptomatic particle-stained PD catheter that was confirmed to be caused by Fusarium spp. colonization. The optimal management regarding this condition remains uncertain. There was one report of successful fungal particle elimination from the PD catheter in asymptomatic patients using an amphotericin lock [19]. However, the majority of authors suggest immediate removal of the PD catheter with or without antifungal treatment [20], [21], [22], [23]. Immediate occurrence of peritonitis and fungemia by the same organism on the next day following anti-fungal lock therapy in this present case suggests that the episode was likely aggravated by the introduction of an antifungal agent into the PD catheter lumen. Antifungal agents may break down a stable fungal mycelium on the inner surface of the PD catheter causing a spread of fungal hyphae into the peritoneal cavity and blood circulation.
The observation of positive GM index in both serum and PD effluent on day 0 in the case of the subclinical Fusarium spp. colonization was another learning point from the first case. This cross-reactivity has been previously reported in a series of 9 hematological patients with invasive fusariosis of whom the blood or body fluid was positive for GM without any evidence of Aspergillus infection. The cross-reactivity was also confirmed in the same study by showing that supernatant from the Fusarium isolate could also give a positive GM index result with standard Aspergillus enzyme immunoassay [24]. GM index was also used for earlier diagnosis of invasive fusariosis in another study showing that the GM index could be positive for 10 days prior to the clinical diagnosis using conventional methods [25]. Our finding point out that in the case of the asymptomatic particle-stained PD catheter, the test for GM index not only from the PD effluent but also from serum can hasten the diagnosis of fungal colonization by Aspergillus spp. and some other fungi including Fusarium spp.
The second scenario was a straight-forward situation where a case of definite fungal peritonitis was treated conservatively by systemic and intracatheter antifungal lock therapy without PD catheter removal. This practice was homologous to the successful cases in previous reports [5], [6], [17], [18]. Because the infections had not been present at the beginning of peritonitis, subsequent infections in the second case may have resulted from fungal invasion through the PD catheter. The use of antifungal locks might not directly lead to such complications but in our opinion this treatment may cause a delay in definitive PD catheter removal which might lead to the paradoxical outcome.
In conclusion, we presented examples of paradoxical experiences utilizing antifungal locks in two different scenarios of PD-related fungal infections. Despite utilizing the benefits of PD catheter salvage and avoiding PD catheter removal in frail patients, antifungal locks are subject to potentially hazardous complications. Unless the PD catheter removal is not feasible or medically contraindicated, the use of antifungal locks in either a particle-stained PD catheter being left in place or frank peritonitis should be discouraged.
Acknowledgements
This study was supported by the Rachadaphisek Sompot Endorsement Fund (CU-GRS_60_12_30_05), Chulalongkorn University, the National Research Council of Thailand (2558-113 156/2560), and Thailand Research Foundation IRG5780017), Thailand (156/2560). We are special thanks to Ms. Margaret Clarke for her manuscript editing.
Acknowledgments
Conflict of interest
The authors declare no conflicts of interest. The authors alone are responsible for the content of the study.
References
- 1.Miles R., Hawley C.M., McDonald S.P., Brown F.G., Rosman J.B., Wiggins K.J. Predictors and outcomes of fungal peritonitis in peritoneal dialysis patients. Kidney Int. 2009;76(6):622–628. doi: 10.1038/ki.2009.202. [DOI] [PubMed] [Google Scholar]
- 2.Wang A.Y., Yu A.W., Li P.K., Lam P.K., Leung C.B., Lai K.N. Factors predicting outcome of fungal peritonitis in peritoneal dialysis: analysis of a 9-year experience of fungal peritonitis in a single center. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2000;36(6):1183–1192. doi: 10.1053/ajkd.2000.19833. [DOI] [PubMed] [Google Scholar]
- 3.Ram R., Swarnalatha G., Neela P., Murty K.V. Fungal peritonitis in patients on continuous ambulatory peritoneal dialysis: a single-centre experience in India. Nephron Clin. Pract. 2008;110(4):c207–c212. doi: 10.1159/000167867. [DOI] [PubMed] [Google Scholar]
- 4.Li P.K., Szeto C.C., Piraino B., de Arteaga J., Fan S., Figueiredo A.E. ISPD Peritonitis Recommendations: 2016 Update on Prevention and Treatment. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 2016;36(5):481–508. doi: 10.3747/pdi.2016.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.S.H. Lee, S.S. Chiang, S.J. Hseih, H.M. Shen, Successful treatment of fungal peritonitis with intracatheter antifungal retention, in: Proceedings of the Advances in peritoneal dialysis Conference on Peritoneal Dialysis, 1995, Vol. 11, pp. 172–175. [PubMed]
- 6.Tsai T.J., Chen Y.M., Hsieh B.S., Chen W.Y., Yen T.S. Can intracatheter retention of antifungal agents cure fungal peritonitis? Two cases successfully treated without catheter removal. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 1991;11(4):355–356. [PubMed] [Google Scholar]
- 7.Ozdemir H., Karbuz A., Ciftci E., Dincaslan H.U., Ince E., Aysev D. Successful treatment of central venous catheter infection due to Candida lipolytica by caspofungin-lock therapy. Mycoses. 2011;54(5):e647–e649. doi: 10.1111/j.1439-0507.2010.01964.x. [DOI] [PubMed] [Google Scholar]
- 8.Blackwood R.A., Klein K.C., Micel L.N., Willers M.L., Mody R.J., Teitelbaum D.H. Ethanol locks therapy for resolution of fungal catheter infections. Pediatr. Infect. Dis. J. 2011;30(12):1105–1107. doi: 10.1097/INF.0b013e31822c84a4. [DOI] [PubMed] [Google Scholar]
- 9.Arnow P.M., Kushner R. Malassezia furfur catheter infection cured with antibiotic lock therapy. Am. J. Med. 1991;90(1):128–130. doi: 10.1016/0002-9343(91)90518-3. [DOI] [PubMed] [Google Scholar]
- 10.Johnson D.C., Johnson F.L., Goldman S. Preliminary results treating persistent central venous catheter infections with the antibiotic lock technique in pediatric patients. Pediatr. Infect. Dis. J. 1994;13(10):930–931. doi: 10.1097/00006454-199410000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Benoit J.L., Carandang G., Sitrin M., Arnow P.M. Intraluminal antibiotic treatment of central venous catheter infections in patients receiving parenteral nutrition at home. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 1995;21(5):1286–1288. doi: 10.1093/clinids/21.5.1286. [DOI] [PubMed] [Google Scholar]
- 12.Viale P., Petrosillo N., Signorini L., Puoti M., Carosi G. Should lock therapy always be avoided for central venous catheter-associated fungal bloodstream infections? Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2001;33(11):1947–1948. doi: 10.1086/323554. (author reply 9-51) [DOI] [PubMed] [Google Scholar]
- 13.Castagnola E., Marazzi M.G., Tacchella A., Giacchino R. Broviac catheter-related candidemia. Pediatr. Infect. Dis. J. 2005;24(8):747. doi: 10.1097/01.inf.0000172929.23419.cb. [DOI] [PubMed] [Google Scholar]
- 14.Angel-Moreno A., Boronat M., Bolanos M., Carrillo A., Gonzalez S., Perez Arellano J.L. Candida glabrata fungemia cured by antibiotic-lock therapy: case report and short review. J. Infect. 2005;51(3):e85–e87. doi: 10.1016/j.jinf.2004.08.034. [DOI] [PubMed] [Google Scholar]
- 15.Buckler B.S., Sams R.N., Goei V.L., Krishnan K.R., Bemis M.J., Parker D.P. Treatment of central venous catheter fungal infection using liposomal amphotericin-B lock therapy. Pediatr. Infect. Dis. J. 2008;27(8):762–764. doi: 10.1097/INF.0b013e318170b68b. [DOI] [PubMed] [Google Scholar]
- 16.White T.J., Bruns T., Lee S.H., Taylor J.W. Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics. In: Innis M.A., Gelfand D.H., Sninsky J.J., White T.J., editors. PCR Protocols: A Guide to Methods and Applications. Academic Press, Inc; San Diego, Califonia: 1990. pp. 315–322. [Google Scholar]
- 17.Caramori J.T., Barros e Silva M., Felipe M.J., Sadatsune T., Montelli A.C., Barretti P. Successful treatment of fungal peritonitis in CAPD by intravenous, intraperitoneal, and intracatheter administration of amphotericin B. A case report. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 1995;15(2):187–188. [PubMed] [Google Scholar]
- 18.Boer W.H., van Ampting J.M., Vos P. Successful treatment of eight episodes of Candida peritonitis without catheter removal using intracatheter administration of amphotericin B. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 2007;27(2):208–210. [PubMed] [Google Scholar]
- 19.Buchanan W.E., Quinn M.J., Hasbargen J.A. Peritoneal catheter colonization with Alternaria: successful treatment with catheter preservation. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 1994;14(1):91–92. [PubMed] [Google Scholar]
- 20.Sekkarie M., Holmes C., Ranjit U., Kauffman C.A. Grossly visible fungal colonization of a Tenckhoff catheter. A case report and literature review. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 1991;11(1):85–87. [PubMed] [Google Scholar]
- 21.Oz Y., Kiraz N., Ozkurt S., Soydan M. Colonization of peritoneal catheter with a thermophilic fungus, Thermoascus crustaceus: a case report. Med. Mycol. 2010;48(8):1105–1107. doi: 10.3109/13693781003793838. [DOI] [PubMed] [Google Scholar]
- 22.Vargemezis V., Passadakis P., Liakopoulos V., Kriki P., Kantartzi A. Fungal colonization of peritoneal catheter with persistently sterile cloudy effluent, in the absence of clinical findings of fungal peritonitis. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 2004;24(1):81–84. [PubMed] [Google Scholar]
- 23.Huang J.W., Chu T.S., Wu M.S., Peng Y.S., Hsieh B.S. Visible Penicillium spp. colonization plaques on a Tenckhoff catheter without resultant peritonitis in a peritoneal dialysis patient. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transplant. Assoc. Eur. Ren. Assoc. 2000;15(11):1872–1873. doi: 10.1093/ndt/15.11.1872. [DOI] [PubMed] [Google Scholar]
- 24.Tortorano A.M., Esposto M.C., Prigitano A., Grancini A., Ossi C., Cavanna C. Cross-reactivity of Fusarium spp. in the Aspergillus Galactomannan enzyme-linked immunosorbent assay. J. Clin. Microbiol. 2012;50(3):1051–1053. doi: 10.1128/JCM.05946-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nucci M., Carlesse F., Cappellano P., Varon A.G., Seber A., Garnica M. Earlier diagnosis of invasive fusariosis with Aspergillus serum galactomannan testing. PLoS One. 2014;9(1):e87784. doi: 10.1371/journal.pone.0087784. [DOI] [PMC free article] [PubMed] [Google Scholar]