Abstract
Background and Objectives:
Stabbing the head is a rare event. It may occur following an assault or self-inflicted injury. We intend to report our experience with four such cases and review narratively the relevant literature. A treatment algorithm will be delivered.
Materials and Methods:
We have reviewed four of our cases; three were stabbed to the orbit and one to the head.
Results:
Enucleation was performed in one case. Vision could be preserved in the other two and brain abscess developed in the other cases due to a retained piece of knife. We made a comparison between our cases and those limited reports in the literature to reach an algorithm.
Conclusion:
The temporal region and the orbit are the targets mostly attacked in the craniofacial stabs. Since knives have a sharp and thin edge, they may break when penetrating the skull. The damage to the brain tissue and the retained piece of knife may be missed easily by overlooking the small injury to the scalp. The suggested algorithm would be a contrast-enhanced computed tomography scan of the skull and brain and a kind of brain vascular study are necessary, considering the location of the knife in the skull and brain passing the area with crowded vasculature. The best treatment protocol is surgery accompanied by antibiotic therapy.
Keywords: Brain abscess, penetrating head wound, stab wound, traumatic aneurysm
Introduction
Penetrating craniocerebral injury is defined as head trauma caused by an object that crosses the skull bone and the underlying dura. It may be retained in the skull or exit from another point. Knives are one of the objects that may cause penetrating injury in the civilians. The exact incidence of penetrating and perforating injuries to the head in the civilian population is unknown, but current estimations indicate that bullets account for 4.6% and puncture wounds, stab, nail, etc., cause 0.4% of this kind of brain injuries.[1,2] The incidence of penetrating stab wounds to the head is so scarce that an exact treatment plan has not yet been alluded. We will present our experience with such cases, make a thorough review of the literature, and propose a treatment protocol to deal with similar casualties.
Materials and Methods
Case 1
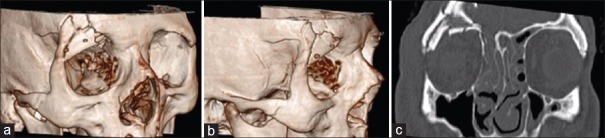
A 21-year-old male was stabbed in the rim of his right orbit. The knife was removed immediately by the offender and the victim was transferred to the emergency department. He was drowsy but cooperative and oriented. The skin laceration had sharp edges and was bandaged. Computed tomography (CT) scan [Figures 1a–c] revealed multilinear depressed skull fracture involving the rim of the orbit along the frontal bone with multiple small and in driven bone fragments into the frontal lobe, with contusion of the adjacent brain tissue and subarachnoid hemorrhage. He underwent urgent surgery with an elevation of the bone fragments, debridement of the contused brain, repair of the dura, and simultaneous reconstruction of the rim of the orbit using the autologous bone chips harvested from the clean tables of the fractured frontal bone. Wide-spectrum intravenous antibiotics were given for 3 weeks. The postoperative course was uneventful. Three D-CT scan taken after 4 months confirmed good heeling of the rim of the orbit with acceptable cosmesis.
Figure 1.
(a-c) Skull computed tomography scan with three-dimensional reconstruction showing the entrance point of the knife blade shattering the rim of the orbit and sliding into the dura. The superior rim of the right orbit and the posterior ethmoidal air cells are damaged
Case 2
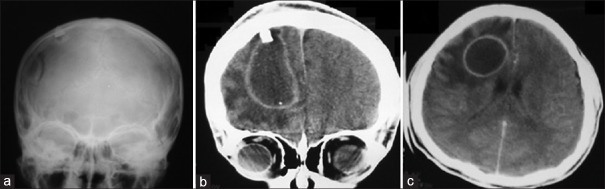
A 14-year-old boy was stabbed in the right posterior frontal region, and the knife was removed. The wound was sutured in the nearby clinic and patient discharged home with oral antibiotic capsules for 3 days only, the name of which not known. He developed fever and epilepsy after 1 week. When admitted to our hospital, he was confused, febrile, and left hemiparetic. Imaging revealed depressed frontal bone and the retained-fractured tip of the knife in skull X-ray and CT scan. Contrast-enhanced CT scan showed a large rim enhancing brain abscess in juxtaposition to the retained knife blade [Figure 2a–c]. Surgical intervention with debridement of the depressed bone fragments and foreign body, drainage of the abscess, and excision of the wall was achieved. Staphylococcus aureus was the cultured organism and could be treated with intravenous penicillin and clindamycin for 3 weeks. The contrast-enhanced CT scan taken after 2 months revealed no residue of the abscess.
Figure 2.
(a) Skull X-ray showing the tip of the knife blade retained in the right frontal lobe. (b and c) Contrast-enhanced coronal and axial brain computed tomography scans showing a large brain abscess besides the blade tip
Case 3
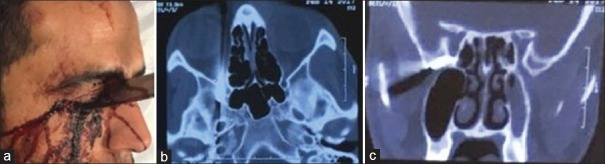
A 30-year-old was stabbed in the right eye with a big knife. He was awake and oriented, and the knife was not removed. Right globe was destructed with no vision and was frozen. The knife had penetrated the orbit along its medial wall reached the cone of the orbit and lodged in the floor of the temporal fossa just in front of the cavernous sinus [Figure 3]. The ophthalmic surgeon completed enucleation and the neurosurgeon decompressed the lesser wing through the lateral wall and the knife was removed safely and under control. The postoperative course was uneventful and he was given intravenous (IV) antibiotics for 1 week only.
Figure 3.
(a) The knife has entered the orbit through medial canthus of the right eye. (b) In the axial view of the computed tomography scan, the tip of the knife is located near the cavernous sinus. (c) The tip of the knife is seen millimeters below the optic canal
Case 4
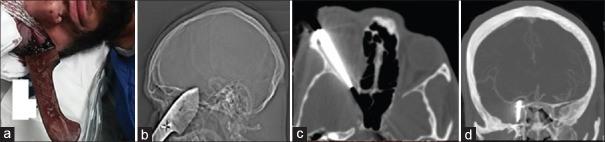
A 24-year-old male was brought to the emergency room with a knife stabbed to the left orbit. He was awake and conscious with no neurological deficit. The globe was intact with a restricted motion to all directions. Brain CT scan showed the stab trajectory along the lateral wall of the orbit penetrating to the cone of the orbit reaching the infraclinoid cavernous sinus [Figure 4a–c]. CT angiography did not show any vascular damage [Figure 4d]. A fronto-orbito-lateral craniotomy was performed and the knife could be removed carefully after appropriate decompression of the lesser and greater sphenoid wings. IV antibiotics were given for 7 days and he was discharged in good condition. In the follow-up and after 6 months, he only suffered from mild limitation in the eversion of the injured eye.
Figure 4.
(a) The knife entered from the lateral canthus of the eye in a medial direction. (b) The scout view shows a knife with a blunt tip. (c) In the axial view, the knife is seen to slide on the lateral wall of the orbit toward the optic canal. The exact location of tip is not well visible due beam hardening artifact. (d) Computed tomography angiography showing intact vasculature
Discussion
To reach a conclusion denoting the suggested treatment algorithm, it is preferred to subclassify the discussion under the categories comparing the literature with our presented cases.
Epidemiology
The exact incidence of penetrating and perforating injuries in the civilian population is unknown, and puncture wounds are responsible for only 0.4% of all brain injuries.[3] The incidence of skull stab wounds is much lower in the European context compared to developing countries such as South Africa; therefore, most of the current knowledge about the complications and management of stab wounds to the head is coming from South African literature where 597 cases have been reported during a 12-year period.[4] Our collection is from 2 different trauma centers in two major cities reviewing the referrals for more than 10 years showing either the rarity of the event or the potential mortal nature of stab wound to the skull base region.
Dynamics and physiology
Penetrating craniocerebral injury is defined as the damage caused by an object that crosses the thickness of skull bone and dura mater. It may exit from another point after passing through and through. Penetrating agent can be a missile or nonmissile penetrant. Nonmissile penetrants can be of high velocity (>100 m/s) or low velocity. High-velocity nonmissile penetrants can penetrate the skull, but low-velocity ones usually cause laceration/maceration of the scalp. High-velocity nonmissile penetrations may be caused by perforating instruments or bone fragments shattered from the skull that penetrate the brain.[5] A list of objects that can cause nonmissile penetrating trauma and reported in the literature include knives, crochet hooks, knitting needles, breech pins, umbrella bibs, crowbars, iron rods, pitchforks, car antenna, pairs of scissors, and even screwdrivers.[6] The force needed to pierce through skin is roughly estimated to be 49 N. Meanwhile, 540 N energy is needed for penetrating the parietal bone by a sharp object. The temporal bone, as one of the thinnest parts of the skull, can be penetrated with 255 N energy.[7] The knives that can bear such a large amount of energy to penetrate through the skull must be rigid and sharp enough [Figures 3 and 4]. The knife with such characteristics is often made of steel or metal, with a sharp tip, and a rigid wide handle which could increase the penetrating force (cases 3 and 4). Knives create a classic slot fracture.[8] Stab wounds to the head are mostly seen in violence associated with alcohol intoxication, unintended situations, and rare self-inflicted events.[9]
Head is a less favorable site for knife attacks. According to Martin Bauer's study on head stab wounds in a European center, patients who were stabbed to the head had been stabbed to other parts of the body at least once. The prevalence of a single stab wound to the head is significantly higher in male attackers in South African reports.[10,11] Strangely enough, all our cases were wounded only in the skull.
The frontal bone is the most anterior, the thickest, and most achievable target for attacker, but the other parts of the skull such as the orbit and squamous part of temporal bone are thinner, making them more vulnerable and an attractive target for the expert attackers[12] as in three of our cases.
Diagnosis
When an object penetrates the skull, it injures the brain in the entrance, along the entrance gutter and in the exit.[13]
Victims are usually visited at a primary trauma center or a general hospital by a junior physician who may not be aware of the medical and legal importance of such kind of trauma. These injuries are the result of aggression and murder attempts (all our 4 cases). In our second case, the patient was treated as a simple scalp laceration, and no attempt was made to further investigate the possibility of retained object.
Most of the patients with stab wound to the head are in a good general condition. They are awake, responsive, and hemodynamically stable[14] except for the possible neurological deficits.[15]
The knife can be retained within or removed from the skull. There is a more likelihood of breakage of the knife as it passes deeper through the skull[16] or the whole knife would be stuck within the cranium There may also be multiple puncture sites on the skin. The scalp presentation of a stab injury is usually a small linear cut, and the wound may be hidden by hair so that the depth of the injury cannot be exactly evaluated as in our first case. Palpation of the injured skin is essential in cases of depressed fractures.
Most knives which are able to penetrate the skull are metal and radiopaque. Further evaluations such as head CT scan or plain radiograph can be obtained after stabilizing patient's condition. CT scan is diagnostic if there is a suspicion of fracture or retained piece of foreign body and knife in stab injuries. The imaging helps in identifying the extent of skull fractures, retained pieces of weapons, hemorrhages, ischemia, brain edema, and depth of penetration even if the knife is removed. In plain X-rays, the length and depth of retained knife or a piece of it can also be seen. Magnetic resonance imaging (MRI) can be performed if no retained piece of metal is present.[17]
Evaluation of vascular structures is also mandatory, especially if the tract of entrance passes along the areas with crowded vasculature.[18] If the clinical condition of the patient is stable, angiographic studies are suggested before surgical intervention. Vascular studies are even more valuable if there is a retained piece of knife or any evidence of vascular injury in brain CT scan. Both CT angiography and digital subtraction angiography (DSA) can be performed, but since most penetrating knives are metal, the artifact in CT angiography might conceal the traumatic aneurysm or the vessels in spasm. DSA, on the other hand, can provide a dynamic picture of the vasculature; therefore, spasm and thrombosis could be easier to identify. It is suggested to perform an early angiography before removing the foreign body and repeat it to find late aneurysm formation even after years of injury in some cases.[19]
Management/treatment algorithm
The management strategy for these injuries is primarily surgical.[20] The step-wise evaluation of the patient, as addressed by de Holanda LF et al.,[25] includes resuscitation, close evaluation of the scalp by looking for the site of penetration, their number, and shape followed by thorough neurological examination. The next step is imaging consisting of skull X-rays and CT scan of the brain. MRI is not required unless in the late phases for further evaluation, and when the physician is assured that no metal object is retained in the orbit or intracranial space.[21]
The incidence of skull penetrating injuries with stab is so low that most treatment algorithms are based on case reports and case series. The main goal of surgical treatment in penetrating injuries is to remove the object in a safe manner, debridement of damaged parenchyma, removal of hematoma, and closure of the injured dura and skin as in our series.[22] Most cases in the literature were surgically treated through craniotomy.[20] Craniotomy should be set wide enough to facilitate removal of the knife with minimal or no pivotal movement and also to facilitate the control of possible abrupt bleeding. The superior and inferior sagittal sinuses are vulnerable to stab wounds in the mid-sagittal plane in the frontal and parietal bone. The cavernous sinus is vulnerable in stabs to the anterior temporal fossa and the orbit. The petrosal and the sigmoid sinus could be damaged if the penetrating knife faces backward in the posterior temporal fossa. If the wall of the sinus or a major artery is damaged, the bleeding can be catastrophic.[23] Constant compression, fibrin glue, and fascia are currently more advised than artificial materials for repairing the dura or the sinus.[24]
Blind removal of the knife can damage the neural tissue and may cause secondary injury to the brain and the adjacent vessels even though anecdotal cases of removing the offending agent in the radiology department has also been reported.[25] Hence, stabilizing the head, adequate craniotomy and neuronavigation with the aid of CT scan can be helpful in removing the penetrated piece of knife with minimal damage.
Most of the authors recommend prophylactic antibiotics as a mainstay of treatment because penetrating objects are contaminated. The prophylactic antibiotics should cover a combination of Gram-positive, Gram-negative, and anaerobic bacteria. The duration of antibiotherapy is still controversial. There is a clear consensus that the antimicrobial prophylactic therapy should be continued for at least 72 h after surgery if any foreign objects remained in the scalp, skull, orbit, or central nervous system.[26] Antiepileptic medication should be started in cases of parenchymal lesions, hematoma, injury to eloquent areas of the brain such as the temporal or the frontal lobe, Glasgow Coma scale of 9 or less, and if any posttraumatic seizure occurred. The duration of antiepileptic administration is not well delineated, but if no seizure occurs in the acute phase, the medication can be discarded after 1 week.[26]
Complications
Primary brain tissue injury mainly occurs as hemorrhage and necrosis of the neural tissue,[27] damage of the adjacent vascular structures presenting as vessel rupture, ischemia, and early or late aneurysm formation,[28] epidural or subdural hematomas, and countercoup injuries all have been described to occur with knives.[29] Any retained part of the penetrating agent can act as a hemostat and removing it may be catastrophic.[30]
Secondary brain damage is caused at the time of removing the knife, either by the assailant at the scene or by the medical personnel without having any control on the field of injury. The damage is the result of pivotal movement of the knife within the penetration gutter. The typical secondary damage consists of edema, inflammation, problems in vascular supply, and perfusion which happens in a week after trauma.[31]
Since the squamous plate of temporal bone is the least resistant part of the skull bone, the stab can be in driven deeper through this part. Haworth and De Villiers introduced a method to evaluate severe and fatal damages caused by deep stab injuries through the temporal plate. He divided the temporal fossa into anterior and posterior parts. The anterior part contains the cavernous sinus, the carotid artery, the sella turcica, and the third to sixth cranial nerves. These structures are very sensitive and deeply seated at the base of the skull. The containment of the posterior part is brain stem and basilar artery. The angle of entrance of the knife is of great importance because these structures are more deeply located than the anterior structures and are secured by adjacent bony structures.[32]
Antibiotics
It is suggested that delay of debridement of the stab penetrating wound more than 48 h can lead to increased chance of infection.[33] There is no good level of evidence to advise the need for postoperative long-term antibiotic therapy in such cases even though short-term antibiotic administration against Gram-negative, Gram-positive, and anaerobic organisms is advised for at least 72 h after surgery. Tetanus vaccination should also be considered according to the WHO protocol for vaccination.[34] Penetrating objects such as knives passing through air sinuses or the oropharynx may cause infection at the site of penetration and brain abscess as in our case 1.[35]
Vascular complications occur in 30% of cranial penetrating injuries with an approximate incidence of aneurysm formation in 15%, carotid-cavernous fistula in 7%, other types of arteriovenous fistula in 4%, occlusion of major vessels in 4%, transection in 3%, and severe vasospasm in 3%. Deeper penetration and involvement of petrous bone are associated with higher rate of vascular complications. Aneurysm formation is seen in stabs that enter somewhere near the pterion or cross the midline and are associated with intracerebral hematoma.[36] The retained piece of knife may tamponade the injured vessel and prevent bleeding that is why special care must be taken at the time of removing the object. Damage to the venous sinuses may lead in thrombosis and secondary bleeding.[37]
The frontal lobes are large enough to prevent penetrating objects to reach deep vital structures and hence stab wounds to this area may often be without neurological deficits. If parts of corpus callosum are damaged, disconnection syndrome may develop.
The orbit, as a cone-shaped space, directs the stabbed knives toward its weakest point located in front of the carotid artery and cavernous sinus. The orbital content may be intact at the time of examination and the patient may suffer no neurologic deficit, but the intracranial structures may be damaged. Transorbital stab wounds with thin and long objects are more dangerous because less energy is needed for the object to penetrate deeper.
Most of the stabs are removed by the assailant, but if it remains in place for >48 h, focal inflammatory reaction around the retained object may end up with the development of brain abscess (our case 2).
Conclusion
We have learned from our cases and the limited data in the literature that (a) the penetrating knives are usually sharp and may cause little injury to the skin so any sharp object with enough energy colliding the skull should be evaluated at least with a plain CT scan. (b) The gold standard treatment is surgery. (c) The present literature supports the administration of antibiotics and antiepileptics for unknown period of time after surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Haworth CS, de Villiers JC. Stab wounds to the temporal fossa. Neurosurgery. 1988;23:431–5. doi: 10.1227/00006123-198810000-00004. [DOI] [PubMed] [Google Scholar]
- 2.MacEwen CJ, Fullarton G. A penetrating orbitocranial stab wound. Br J Ophthalmol. 1986;70:147–9. doi: 10.1136/bjo.70.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Callaghan PT, Jones MD, James DS, Leadbeatter S, Holt CA, Nokes LD, et al. Dynamics of stab wounds: Force required for penetration of various cadaveric human tissues. Forensic Sci Int. 1999;104:173–8. doi: 10.1016/s0379-0738(99)00115-2. [DOI] [PubMed] [Google Scholar]
- 4.Yamashita M, Abrahäo N, Júnior, Lamachia C. Suicide attempt by introducing 2 nails in the head. Case report. Arq Neuropsiquiatr. 1998;56:317–9. doi: 10.1590/s0004-282x1998000200026. [DOI] [PubMed] [Google Scholar]
- 5.Chibbaro S, Tacconi L. Orbito-cranial injuries caused by penetrating non-missile foreign bodies. Experience with eighteen patients. Acta Neurochir (Wien) 2006;148:937–41. doi: 10.1007/s00701-006-0794-5. [DOI] [PubMed] [Google Scholar]
- 6.Nathoo N, Boodhoo H, Nadvi SS, Naidoo SR, Gouws E. Transcranial brainstem stab injuries: A retrospective analysis of 17 patients. Neurosurgery. 2000;47:1117–22. doi: 10.1097/00006123-200011000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Nathoo N, Nadvi SS. Traumatic intracranial aneurysms following penetrating stab wounds to the head: Two unusual cases and review of the literature. Cent Afr J Med. 1999;45:213–7. doi: 10.4314/cajm.v45i8.8487. [DOI] [PubMed] [Google Scholar]
- 8.Adams RF, Anslow P, Talbot K. Screwdriver headache: A case of traumatic intracranial hypotension. Clin Radiol. 2001;56:676–80. doi: 10.1053/crad.1999.0461. [DOI] [PubMed] [Google Scholar]
- 9.Weber W. Quantitative investigations concerning penetrating wounds of the human skull (author's transl) Z Rechtsmed. 1974;74:111–6. doi: 10.1007/BF02114697. [DOI] [PubMed] [Google Scholar]
- 10.Cemil B, Tun K, Yiǧenoǧlu O, Kaptanoǧlu E. Attempted suicide with screw penetration into the cranium. Ulus Travma Acil Cerrahi Derg. 2009;15:624–7. [PubMed] [Google Scholar]
- 11.Bauer M, Patzelt D. Intracranial stab injuries: Case report and case study. Forensic Sci Int. 2002;129:122–7. doi: 10.1016/s0379-0738(02)00271-2. [DOI] [PubMed] [Google Scholar]
- 12.du Trevou MD, van Dellen JR. Penetrating stab wounds to the brain: The timing of angiography in patients presenting with the weapon already removed. Neurosurgery. 1992;31:905–11. doi: 10.1227/00006123-199211000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Khalil N, Elwany MN, Miller JD. Transcranial stab wounds: Morbidity and medicolegal awareness. Surg Neurol. 1991;35:294–9. doi: 10.1016/0090-3019(91)90008-w. [DOI] [PubMed] [Google Scholar]
- 14.DiMaio VJ, DiMaio D. Forensic Pathology. 2nd ed. Boca Raton: CRC Press; 2001. p. 207. [Google Scholar]
- 15.Bhootra BL. Retained intra cranial blade-medicolegal perspectives. J Forensic Leg Med. 2007;14:31–4. doi: 10.1016/j.jcfm.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 16.Exadaktylos AK, Stettbacher A, Bautz PC, Terries J. The value of protocol-driven CT scanning in stab wounds to the head. Am J Emerg Med. 2002;20:295–7. doi: 10.1053/ajem.2002.33784. [DOI] [PubMed] [Google Scholar]
- 17.Lindenberg R. Trauma of meninges and brain. In: Minckler J, editor. Pathology of the Nervous System. Vol. 2. New York: McGraw-Hill; 1971. p. 1721. [Google Scholar]
- 18.Amirjamshidi A, Rahmat H, Abbassioun K. Traumatic aneurysms and arteriovenous fistulas of intracranial vessels associated with penetrating head injuries occurring during war: Principles and pitfalls in diagnosis and management. A survey of 31 cases and review of the literature. J Neurosurg. 1996;84:769–80. doi: 10.3171/jns.1996.84.5.0769. [DOI] [PubMed] [Google Scholar]
- 19.Reddy KS. Essentials of Forensic Medicine. 21st ed. Hyderabad: Medical Book Company; 2002. Medicolegal aspects of wounds; p. 248. [Google Scholar]
- 20.Melvill RL, De Villiers JC. Peripheral cerebral arterial aneurysms caused by stabbing. S Afr Med J. 1977;51:471–3. [PubMed] [Google Scholar]
- 21.Kieck CF, de Villiers JC. Vascular lesions due to transcranial stab wounds. J Neurosurg. 1984;60:42–6. doi: 10.3171/jns.1984.60.1.0042. [DOI] [PubMed] [Google Scholar]
- 22.Achram M, Rizk G, Haddad FS. Angiographic aspects of traumatic intracranial aneurysms following war injuries. Br J Radiol. 1980;53:1144–9. doi: 10.1259/0007-1285-53-636-1144. [DOI] [PubMed] [Google Scholar]
- 23.Haddad FS, Haddad GF, Taha J. Traumatic intracranial aneurysms caused by missiles: Their presentation and management. Neurosurgery. 1991;28:1–7. doi: 10.1097/00006123-199101000-00001. [DOI] [PubMed] [Google Scholar]
- 24.López F, Martínez-Lage JF, Herrera A, Sánchez-Solís M, Torres P, Palacios MI, et al. Penetrating craniocerebral injury from an underwater fishing harpoon. Childs Nerv Syst. 2000;16:117–9. doi: 10.1007/s003810050025. [DOI] [PubMed] [Google Scholar]
- 25.de Holanda LF, Pereira BJ, Holanda RR, Neto JT, de Holanda CV, Giudicissi Filho M, et al. Neurosurgical management of nonmissile penetrating cranial lesions. World Neurosurg. 2016;90:420–9. doi: 10.1016/j.wneu.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 26.Wu JJ, Shih CJ. Unusual penetrating injury of the superior sagittal sinus. Surg Neurol. 1982;17:43–6. doi: 10.1016/0090-3019(82)90041-6. [DOI] [PubMed] [Google Scholar]
- 27.Kazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. J Emerg Trauma Shock. 2011;4:395–402. doi: 10.4103/0974-2700.83871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schierhout G, Roberts I. Anti-epileptic drugs for preventing seizures following acute traumatic brain injury. Cochrane Database Syst Rev. 2001:CD000173. doi: 10.1002/14651858.CD000173. [DOI] [PubMed] [Google Scholar]
- 29.Pavlidis P, Karakasi MV, Birbilis TA. Traumatic brain injury due to screwdriver assaults: Literature review and case report. Am J Forensic Med Pathol. 2016;37:291–8. doi: 10.1097/PAF.0000000000000267. [DOI] [PubMed] [Google Scholar]
- 30.31Taylor AG, Peter JC. Patients with retained transcranial knife blades: A high-risk group. J Neurosurg. 1997;87:512–5. doi: 10.3171/jns.1997.87.4.0512. [DOI] [PubMed] [Google Scholar]
- 31.Turbin RE, Maxwell DN, Langer PD, Frohman LP, Hubbi B, Wolansky L, et al. Patterns of transorbital intracranial injury: A review and comparison of occult and non-occult cases. Surv Ophthalmol. 2006;51:449–60. doi: 10.1016/j.survophthal.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 32.Di Roio C, Jourdan C, Mottolese C, Convert J, Artru F. Craniocerebral injury resulting from transorbital stick penetration in children. Childs Nerv Syst. 2000;16:503–6. doi: 10.1007/s003810000291. [DOI] [PubMed] [Google Scholar]
- 33.Mackerle Z, Gal P. Unusual penetrating head injury in children: Personal experience and review of the literature. Childs Nerv Syst. 2009;25:909–13. doi: 10.1007/s00381-009-0901-z. [DOI] [PubMed] [Google Scholar]
- 34.Lunetta P, Ohberg A, Sajantila A. Suicide by intracerebellar ballpoint pen. Am J Forensic Med Pathol. 2002;23:334–7. doi: 10.1097/00000433-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Zyck S, Toshkezi G, Krishnamurthy S, Carter DA, Siddiqui A, Hazama A, et al. Treatment of penetrating nonmissile traumatic brain injury. Case series and review of the literature. World Neurosurg. 2016;91:297–307. doi: 10.1016/j.wneu.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 36.Matsuyama T, Okuchi K, Nogami K, Hata M, Murao Y. Transorbital penetrating injury by a chopstick – Case report. Neurol Med Chir (Tokyo) 2001;41:345–8. doi: 10.2176/nmc.41.345. [DOI] [PubMed] [Google Scholar]
- 37.Gökçek C, Erdem Y, Köktekir E, Karatay M, Bayar MA, Edebali N, et al. Intracranial foreign body. Turk Neurosurg. 2007;17:121–4. [PubMed] [Google Scholar]