Abstract
Introduction:
Epidural hematoma (EDH) is a traumatic accumulation of blood between the inner table of the skull and the stripped off dural membrane and predominantly consists of venous blood in infants. The study aims to assess the outcome of pediatric EDH using King's Outcome Scale for Childhood Head Injury (KOSCHI).
Materials and Methods:
A total of 72 patients’ files were reviewed retrospectively with a diagnosis of EDH from January 2012 to December 2014. Predesigned proforma was filled using data from patient records. In addition, KOSCHI was calculated using recent telephone interviews.
Results:
Among 72 patients, 65.3% were male and 34.7% were female. Overall, road traffic accident was the most common cause (52.8%) followed by fall, assault, and sports injury. The most common symptom was more than two episodes of vomiting which was present in 51.4% of patients followed by loss of consciousness in 37.5%, ENT bleed in 33.3%, headache in 16.7%, and fits in 11.1% of patients. The median follow-up of our patients was 19 (6–40) months. Most of our patients made good recovery with 76.4% of our patients scoring 5b on KOSCHI.
Conclusion:
EDH is not uncommon among children with head injury. It should be suspected in every child with posttraumatic skull fracture or scalp hematoma. Prompt surgical intervention can give good long-term outcome.
Keywords: Craniotomy, extradural hematoma, head injury, infant, outcome
Introduction
Epidural hematoma (EDH) is a traumatic accumulation of blood between the inner table of the skull and the stripped off dural membrane and predominantly consists of venous blood in infants.[1,2] It is a grave complication of traumatic injuries to the head. In a thickly populated country like ours where current population is estimated to be over 180 million people, head injury remains to be a leading cause of morbidity and mortality in pediatric population. Falls tops road traffic accidents (RTAs) in the list of such terrible causes. These injuries to the skull and brain tissue endanger heavy bleeding and hematoma formation which can be epidural, subdural, subarachnoid, or even intracerebral. This may accidently result from a trivial injury or fall from a short height; however, possibility of nonaccidental injury should be considered.[3,4] According to chronicles, EDH accounts for 2%–3% of such traumatically headinjured children requiring hospital care.[5]
Computed tomography (CT) scan remains to be a prime diagnostic tool; however; nonspecific symptoms and crotchet nature of the disease often delay its diagnosis in pediatric population. Its presentation varies among children contingent upon Glasgow coma scale (GCS), CT findings such as degree of midline shift, associated intracranial or extracranial lesions, size of EDH which are of prognostic value.
To forestall a potentially life-threatening stage, early diagnosis and prompt surgical evacuation of radiographically significant EDH is needed. However, despite of its worldwide acknowledgment, EDH is still bizarrely presented as a neurosurgical emergency amid the children.
Materials and Methods
The study was conducted at Department of Neurosurgery, Jinnah Postgraduate Medical Center. A total of 72 patients files were reviewed retrospectively with a diagnosis of EDH from January 2012 to December 2014. All the cases were secondary to trauma. We divided children into three age-based groups; infant (0–1 year), toddler (2–4 years), schoolgoing age (5-14 years). Data was collected for each case including demographics, mode of injury, presenting symptoms, associated injuries, and radiological features of CT scan brain including site and size of hematoma [Figures 1 and 2].
Figure 1.
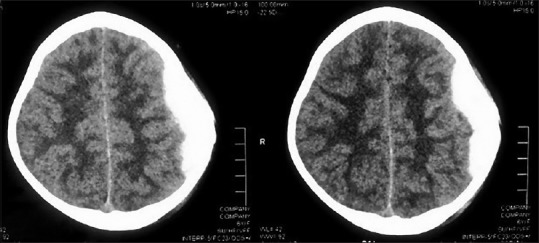
Preoperative computed tomography scan of a patient showing right parietal region extradural hematoma
Figure 2.
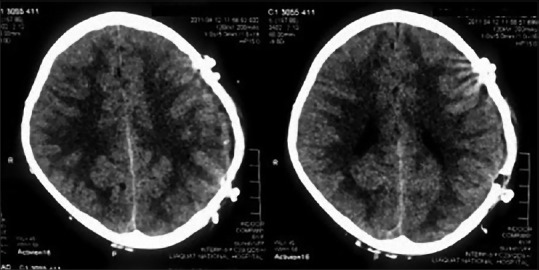
Postoperative computed tomography scan of the same patient showing complete evacuation of hematoma
Time intervals from injury to hospital presentation and then to surgery were recorded. Pre- and post-operative GCS was compared to document surgical improvement; King's Outcome Scale for Childhood Head Injury (KOSCHI) was used for long-term outcome by recent telephone interviews.
Results
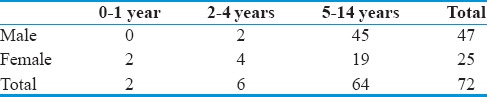
Among 72 patients, 65.3% (n = 47) were male and 34.7% (n = 25) were female. EDH was most common among schoolgoing age with 88.9% of our patients included in this age group [Table 1].
Table 1.
Gender-specific distribution of age groups
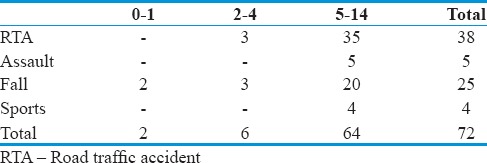
Overall, RTA was the most common cause (52.8%) followed by fall (34.7%), assault (6.9%), and sports injury (5.5%). In age group 0–1 year, fall was the only reason. In age group 2–4 years, 50% of cases were due to RTA and 50% were due to fall. In age group 5–14 years, RTA was the most common cause followed by fall. A history of assault and sports injuries was only seen in this age group [Table 2].
Table 2.
Age-specific distribution of cause of injury
The most common symptom was more than two episodes of vomiting which was present in 51.4% (n = 37) of patients followed by loss of consciousness (LOC) in 37.5% (n-27), ENT bleed in 33.3% (n = 24), headache in 16.7% (n = 12), and fits in 11.1% (n = 8) of patients. Other unusual symptoms such as crying, irritability, localized weakness, vertigo, and unusual limb movements were evident in 12.5% (n = 9) of patients.
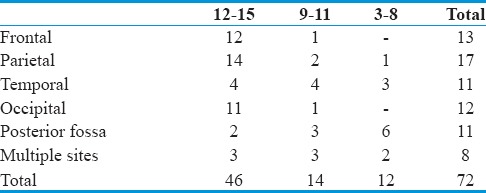
Presenting GCS of 63.8% (n = 46) patients was mildly disturbed (12–15) and out of which 76% scored 15; 19.4% (n = 14) had moderately disturbed GCS (9–11), and 16.7% (n = 12) had severely disturbed (3–8) GCS. The pupils were bilaterally equal and reactive in 79.2% (n = 57) of patients while 16.7% (n = 12) had anisocoria and 4.2% (n = 3) had fixed dilated pupils. On CT scan brain, most common site of EDH was in parietal region (23.6%) followed by frontal (18%) and occipital (16.7%) regions [Table 3]. Among 72 patients, 90.2% (n = 65) needed emergency craniotomy for evacuation of hematoma. Median hospital stay of the patients was 5 (3–8) days. Patients with EDH in the frontal region had the shorter hospital stay (mean = 3.8 ± 0.3 days) while post fossa EDH had the longest hospital course (mean = 7.2 ± 0.5 days).
Table 3.
Site-specific Glasgow coma scale at presentation
The overall mortality rate of the study was 8.3% (n = 6). Among the patients who passed away, three had temporal EDH, two had posterior fossa EDH, and one had EDH in occipital region. One patient required redo craniotomy for recollection of hematoma postoperatively.
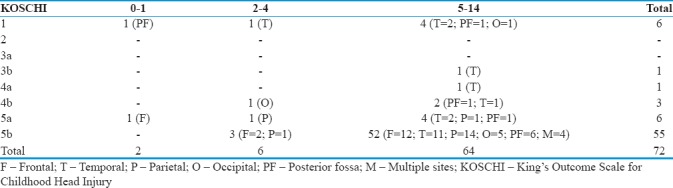
The median follow-up of our patients was 19 (6–40) months. Most of our patients made good recovery with 76.4% of our patients scoring 5b on KOSCHI [Table 4].
Table 4.
Outcome of patients according to King's Outcome Scale for Childhood Head Injury (site of hematoma is showed in parenthesis)
Discussion
Similar to other studies, overall male preponderance was reported.[6] Male predominance in schoolgoing age highlights their careless behavior in sports, increase physical activity inordinate outgoing nature and outdoor activities.[5,7] Bike riding from early age signalizes the fact that RTA is the most common cause among boys. Whereas at younger ages (0–4 years), females predominate in our study, that may be attributed to the lack of parental care and sense of gender discrimination toward female child in our society. Fall from lap is the most common mode of injury and high ratio of assault in female as compare to males further contribute to it.
As presented earlier, infants are reportedly rare in this series (2.7%) because Dura adheres too tightly to the overlaying bone in this age.[4] Some studies even show greater number of EDH in infantile age group.[7] Most common mode of injury was RTA (52.7%) whereas in other studies, fall outweighs other causes.[7,8] Lack of proper traffic regulations and bike riding at young ages among boys contribute to this. As with other studies, RTA and assault increase with the increase in age.[9,10] However, in our study, RTA remains almost constant till the age 14 where it peaks and assault tends to rise with age. Sports injuries account only for 5.5% of cases that is possibly due to decreasing level of interest toward sports.
Browne and Lam found that 45.5% of patients had isolated EDH with no associated injury and fall as a major factor.[6] Our study showed favorably comparable results with 38.8% (n = 28) isolated EDH and fall contributed half of such cases. Risk of EDH tends to multiply four times with skull fractures.[11] Occurrence of cranial fracture has been testified from 48%–90% in pediatric age;[12,13,14] however, in this series, it was only 33.3% (n = 24). Whether it contributes to the formation of EDH is a matter of consideration. Difference in elasticity coefficient of dura and skull bone explains the mechanism of dural separation and accumulation of EDH without fracture. Associated extracranial injuries are found to 68.1% (n = 49) as compared to 85% of Browne and Lam[6] work and even reportedly rare in some studies.[8] Only 2.7% of cases had subdural hematoma that is contrary to 14.3% in one Australian series in pediatric age specifically in infants.[6] Scalp hematoma is considered to be an imperative sign for suspecting EDH;[14] in our study, 48 (66.7%) out of 72 EDH were associated with scalp hematoma or lacerations.
Most common presenting symptom in our series were LOC and vomiting; Zhong et al. reported headache and vomiting as the one of the common symptom,[7] but we found headache in only 16.7% (n = 12) of cases. A history of head trauma with LOC and vomiting strongly points toward the diagnosis. Unusual symptoms such as fits, irritability, localized weakness, vertigo, and unusual limb movements were evident in 12.5% of patient's population that is interestingly not reported by any other series.
Regional preponderance as with other series was found to be toward parietal region.[8,9] Right parietal region contributes more than half to this. Overall right side is more frequently involved as has been proven in literature.[14] Similar to Gerlach's work, after parietal, frontal EDH was most common.[8] EDH rarely involves posterior fossa. As compared to 8.5% of cases in other literature,[8,15] our data inferred only 4.2% post fossa EDH. It is due to the fact that dura attaches more firmly to the posterior vault as compared to anterior half. As in Giovanni's series, all patients with post fossa made good recovery while other literature does not stand in favor of this.[12]
Temporal EDH is reportedly rare in the literature.[13] It may be attributed to the fact that indentation of middle meningeal artery in temporal bone in adults is not seen in children. However, in our study, about one quarter of the hematomas involved the temporal region.
As Gerlach et al. reported, around 50% of surgical intervention was performed within 6 h of injury; with mean time interval from injury to surgery of 4.5 (2–15) h, our study favorably relates with other literature.[8,9] Nonspecific symptoms and crotchet nature of the disease often delay its diagnosis and management.[16]
Mortality rate varies in different literature from 0% to 12% and even higher in pre-CT era.[1,17,18] Mortality rate in our study was 8.3% and strongly associated with male gender, none of the female died. West China hospital study reported 66% of deceased were male and majority of the death were due to fall,[7] while RTA was the leading cause of death in our study. In one study, children <4 years had mortality of 16.7%, 6.3% in age 4–10 years, and 7.4% in children older than 10 years.[9] The overall outcome in different studies shows complete recovery in 82.9%–94.8% of patients on GOS and mRS.[6,7,17] In this series, 76% of cases recover fully on KOSCHI.
Retrospective nature of our study limits the availability of clinical or radiological data, but as it is relatively a large case study with follow-up to get overall outcome of the patients, it overcomes its limitedness. Keeping in mind, its variability of presentation and grave prognosis in reasonable number of cases, it is recommended to evaluate and suspect EDH in every child with a history of RTA or fall.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW, et al. Surgical management of acute epidural hematomas. Neurosurgery. 2006;58(3 Suppl):S7–15. [PubMed] [Google Scholar]
- 2.Jamous MA, Abdel Aziz H, Al Kaisy F, Eloqayli H, Azab M, Al-Jarrah M. Conservative management of acute epidural hematoma in a pediatric age group. Pediatr Neurosurg. 2009;45:181–4. doi: 10.1159/000218200. [DOI] [PubMed] [Google Scholar]
- 3.Greenes DS, Schutzman SA. Occult intracranial injury in infants. Ann Emerg Med. 1998;32:680–6. doi: 10.1016/s0196-0644(98)70067-8. [DOI] [PubMed] [Google Scholar]
- 4.Shugerman RP, Paez A, Grossman DC, Feldman KW, Grady MS. Epidural hemorrhage: Is it abuse? Pediatrics. 1996;97:664–8. [PubMed] [Google Scholar]
- 5.Paiva WS, Andrade AF, Mathias Júnior L, Guirado VM, Amorim RL, Magrini NN, et al. Management of supratentorial epidural hematoma in children: Report on 49 patients. Arq Neuropsiquiatr. 2010;68:888–92. doi: 10.1590/s0004-282x2010000600011. [DOI] [PubMed] [Google Scholar]
- 6.Browne GJ, Lam LT. Isolated extradural hematoma in children presenting to an emergency department in Australia. Pediatr Emerg Care. 2002;18:86–90. doi: 10.1097/00006565-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Zhong W, Sima X, Huang S, Chen H, Cai B, Sun H, et al. Traumatic extradural hematoma in childhood. Childs Nerv Syst. 2013;29:635–41. doi: 10.1007/s00381-012-1971-x. [DOI] [PubMed] [Google Scholar]
- 8.Gerlach R, Dittrich S, Schneider W, Ackermann H, Seifert V, Kieslich M. Traumatic epidural hematomas in children and adolescents: Outcome analysis in 39 consecutive unselected cases. Pediatr Emerg Care. 2009;25:164–9. doi: 10.1097/PEC.0b013e31819a8966. [DOI] [PubMed] [Google Scholar]
- 9.Ben Abraham R, Lahat E, Sheinman G, Feldman Z, Barzilai A, Harel R, et al. Metabolic and clinical markers of prognosis in the era of CT imaging in children with acute epidural hematomas. Pediatr Neurosurg. 2000;33:70–5. doi: 10.1159/000028990. [DOI] [PubMed] [Google Scholar]
- 10.Herrera EJ, Viano JC, Aznar IL, Suarez JC. Postraumatic intracranial hematomas in infancy. A 16-year experience. Childs Nerv Syst. 2000;16:585–9. doi: 10.1007/s003810000340. [DOI] [PubMed] [Google Scholar]
- 11.Quayle KS, Jaffe DM, Kuppermann N, Kaufman BA, Lee BC, Park TS, et al. Diagnostic testing for acute head injury in children: When are head computed tomography and skull radiographs indicated? Pediatrics. 1997;99:E11. doi: 10.1542/peds.99.5.e11. [DOI] [PubMed] [Google Scholar]
- 12.Pasaoglu A, Orhon C, Koç K, Selçuklu A, Akdemir H, Uzunoglu H. Traumatic extradural haematomas in pediatric age group. Acta Neurochir (Wien) 1990;106:136–9. doi: 10.1007/BF01809456. [DOI] [PubMed] [Google Scholar]
- 13.Rocchi G, Caroli E, Raco A, Salvati M, Delfini R. Traumatic epidural hematoma in children. J Child Neurol. 2005;20:569–72. doi: 10.1177/08830738050200070501. [DOI] [PubMed] [Google Scholar]
- 14.Ciurea AV, Kapsalaki EZ, Coman TC, Roberts JL, Robinson JS, 3rd, Tascu A, et al. Supratentorial epidural hematoma of traumatic etiology in infants. Childs Nerv Syst. 2007;23:335–41. doi: 10.1007/s00381-006-0230-4. [DOI] [PubMed] [Google Scholar]
- 15.Prasad GL, Gupta DK, Sharma BS, Mahapatra AK. Traumatic pediatric posterior fossa extradural hematomas: A tertiary-care trauma center experience from India. Pediatr Neurosurg. 2015;50:250–6. doi: 10.1159/000438488. [DOI] [PubMed] [Google Scholar]
- 16.Boran BO, Boran P, Barut N, Akgun C, Celikoglu E, Bozbuga M. Evaluation of mild head injury in a pediatric population. Pediatr Neurosurg. 2006;42:203–7. doi: 10.1159/000092355. [DOI] [PubMed] [Google Scholar]
- 17.Jung SW, Kim DW. Our experience with surgically treated epidural hematomas in children. J Korean Neurosurg Soc. 2012;51:215–8. doi: 10.3340/jkns.2012.51.4.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dhellemmes P, Lejeune JP, Christiaens JL, Combelles G. Traumatic extradural hematomas in infancy and childhood. Experience with 144 cases. J Neurosurg. 1985;62:861–4. doi: 10.3171/jns.1985.62.6.0861. [DOI] [PubMed] [Google Scholar]


