Abstract
Subdural hematoma (SDH) following labor epidural analgesia is a rare neurological complication. SDH is a late complication of this procedure; it is caused by a leak of cerebrospinal fluid that may damage the vascular structures of the brain. Persistent headache in the days after labor epidural analgesia is a nonspecific clinical symptom caused by hematoma. Preexisting vascular malformations can be a concomitant cause of headache. Clinical cases have been reported even after epidural anesthesia. The differential diagnosis includes unspecified headache, sinusitis headache, drug-induced headache, cortical vein thrombosis, fistula of the dura mater, and bacterial, viral, and aseptic meningitis.
Keywords: Accidental dural puncture, blood patch, dural fistula, epidural analgesia, subdural hematoma
Introduction
Labor pain is one of the most severe pains that women can experience. According to the American Congress of Obstetrics and Gynecology and the American Society of Anesthesiologists, mother's demand is a reason enough for the introduction of epidural analgesia in labor, provided that no contraindications exist.[1] Side effects of labor analgesia include pruritus, nausea, vomiting, headache caused by the accidental puncture of the dura mater, hypotension, malpositioning of the catheter into the intravascular compartment or subarachnoid space, and subdural hematoma (SDH).[2] This case report describes a primipara who underwent epidural analgesia during delivery and developed SDH due to the unintentional puncture of the dura mater.
Case Report
A 35-year-old primipara at 38 weeks of pregnancy underwent labor epidural analgesia. No history of neurological disorders, vascular malformations, or cerebral trauma was reported, and no contraindications to labor analgesia were found. At the beginning of labor, the patient was taken to the delivery room, a peripheral vein was cannulated, and her cardiovascular and pressure parameters were monitored. Immediately afterward, she was seated on the operating bed with her head bent over the trunk and her back bent, to allow a better opening of the vertebral spaces. The operator disinfected the skin of the lower back part corresponding to the point where she inserted the catheter, at the L2 vertebral space. After injection of local anesthetic into the skin and in the subcutaneous tissue, the anesthetist proceeded to insert the Tuohy needle. When the 18G Tuohy needle with liquid spindle was introduced, the dura mater was accidentally punctured, causing the cerebrospinal fluid (CSF) to leak.[3] The procedure was, therefore, interrupted and the patient delivered the baby naturally after 3 h. The departmental anesthesiologist performed two visits a day and every 12 h, to evaluate the patient's clinical condition and to change the current therapy. During the following day, she experienced frontal headache in orthostatic position and relieved while lying down. She also experienced neck stiffness; she became nauseated and vomited during elevation of the head from her bed from a 15° recline to a 45° recline.[4] No seizures and motor or sensory deficits were present.[4] In agreement with the existing guidelines,[5] the patient was administered the following therapy immediately after delivery: nonsteroidal analgesic drug treatment IV (ibuprofen 600 mg for three in die), IV paracetamol 1 g for three in die, oral hydration with 2500 l/die, and gastroprotection (Ranidil, 150 mg for two in die). After a 2-day stay in hospital due to such symptoms, the patient underwent brain and spinal magnetic resonance imaging (MRI). The examination revealed subdural collections with low- to medium-signal intensity in T1-dependent sequences and high signal in T2-dependant sequences, mainly located in the occipital-temporal-parietal convexity and to a lesser extent, in the contralateral convexity. The interhemispheric area was also affected. Such findings were due to intracranial hematomas. The left hematoma caused flattened gyri and narrowed sulci as well as a midline shift [Figures 1 and 2]. The neurosurgeon decided to continue the above treatment, with a 5-day follow-up, and she performed a blood patch to close the fistula. During the 5 additional days on medical treatment, the patient underwent a gradual resolution of symptoms. Follow-up MRI after 5 days showed a significant reduction of the right SDH and a mild increase of the left one due to re-bleeding. Midline shift also increased slightly, while the dural fistula resolved after the blood patch [Figures 3 and 4]. The patient was referred to the department of neurosurgery where she was followed up for another 20 days. The left hematoma did not resolve, so she underwent neurosurgical treatment. The right SDH had re-absorbed spontaneously. The surgical procedure was performed under general anesthesia. The surgeon drilled a hole in the bone next to SDH. The meninges were cut and fluids were collected with a drainage that was placed for a period of 48 h and later removed. The patient was discharged in good health after 10 days.
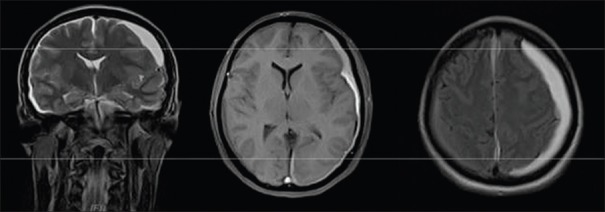
Figure 1.
Bilateral subdural hematoma, clearly visible on the left. Sequences, from left to right: Cor T2, Ax fluid-attenuated inversion recovery, and Ax T1
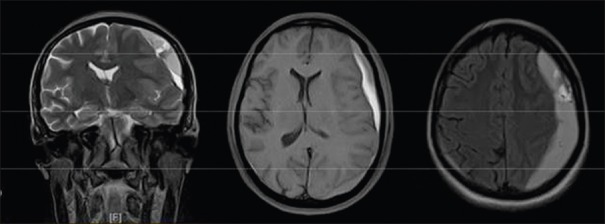
Figure 2.
Dural fistula with fluid collection in soft tissues near spinal epidural access. Sag STIR sequence
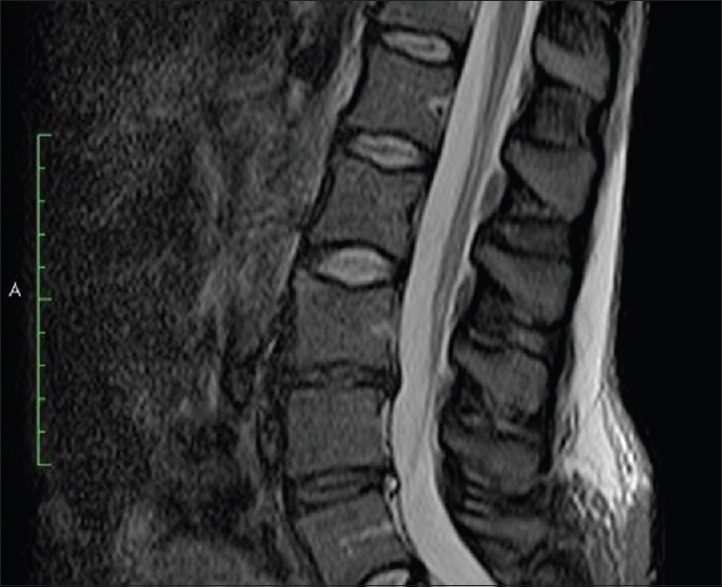
Figure 3.
Follow-up examination shows reduced right subdural hematoma and increased left subdural hematoma. Sequences, from left to right: Cor T2, Ax fluid-attenuated inversion recovery, and Ax T1
Figure 4.
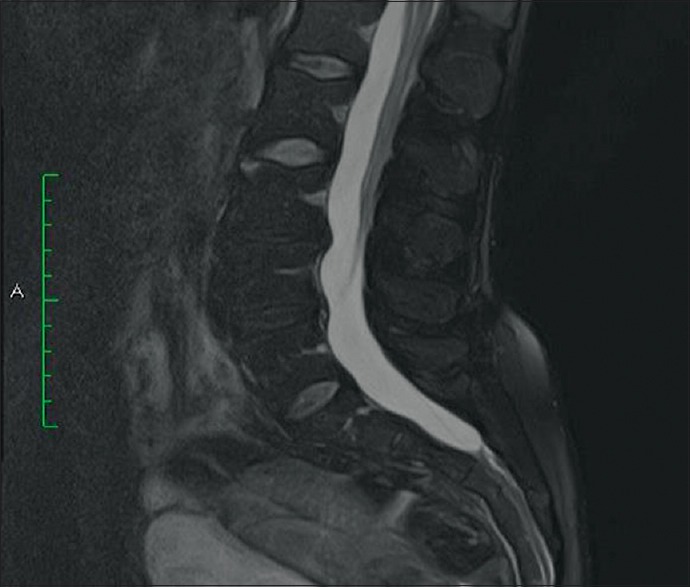
Follow-up examination shows no dural fistula and no fluid collection. Sequence Sag T2 FAT SAT
Discussion
Intracranial SDH is a rare complication.[6] A review of the existing literature was conducted in 2006 by Zeidan et al., revealing 21 cases of SDH following the accidental puncture of the dura mater, 2 of which were in the obstetric setting. The earliest diagnosis took place 2 days after the puncture, while the latest diagnosis was made after about 20 weeks.[7] Cuypers et al. recently studied intracranial subdural hematomas following neuraxial anesthesia in the obstetric population in a literature review of 56 reported cases in 2016.[8] The radiological hallmark is the typical semilunar morphology at computed tomography (CT)/MRI. The blood collection between the dura mater and the arachnoid mater is caused by the traction-induced rupture of the bridging veins between dural sinuses and cerebral cortex; this is caused by CSF hypotension. At MRI, in the acute phase, hematoma is isointense in Sequences T1-dependent sequences and hypointense in SE T2-dependent sequences. In the chronic phase, it is hypo-isointense in SE T1-dependent sequences and hyperintense in SE T2-dependent sequences.[9] Higher incidence is reported in patients with aneurysm, unknown vascular malformations, or arachnoid cysts. The mechanism underlying this condition is supposed to be a loss of CSF causing traction of vascular structures and vascular damage. Clinical signs include persistent headache, nausea, vomiting, photophobia, diplopia, focal neurological signs, and impairment of the consciousness.[10] In this case, intracranial SDH was caused by a lumbar posttraumatic dural fistula as a complication of epidural analgesia, leading to CSF hypotension and bleeding. Spinal MRI or spinal CT may detect CSF leaking area. Spinal MRI, performed with T1 and T2 sequences and fat saturation on sagittal and coronal planes, may detect the fistula causing CSF leaking; more often, it only detects the extradural CSF collection area. In the acute phase, spinal CT has higher sensitivity and specificity in comparison to spinal MRI.
The detection of the lumbar fistula allows the surgeon to perform an epidural blood patch (EBP).[11] EBP is usually successfully performed when other noninvasive treatments fail, while the effectiveness of colloidal patches or saline solutions has not been proved. Therefore, EBP is the treatment of choice in the absence of contraindications, such as sepsis or coagulopathies. The procedure consists in injecting 20 ml of autologous blood without anticoagulants in the epidural area, with the aim to develop a blood clot to close the dural fistula. The risk of a further accidental dural puncture should be taken into account. After the procedure, the patient is required to lay down for 2 h.[12] Headache after accidental puncture of the dura mater can develop in the 1st days from the epidural or at most in the 1st week. It is perceived as an occipital headache that improves in the supine position and gets worse if sitting or standing, making efforts, or leaning forward. It is possible that the headache is accompanied by nausea and discomfort of light. If after 48 h, the symptomatology worsens or does not improve, despite the medical treatment, the patient must undergo radiological instrumental investigations (CT/MRI), which can highlight the cause of CFS leakage so that it is suitable for a possible neurosurgical treatment. With reference to our case, the dural fistula was resolved after blood patch without complications[13] as well as the right SDH. Left SDH required neurosurgical treatment, with no permanent neurological outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank the patient for providing her consent to process clinical data for publication. We also thank Michela Renna (M. Sc.) for translating the manuscript.
References
- 1.Bilić N, Djaković I, Kličan-Jaić K, Rudman SS, Ivanec Ž. Epidural analgesia in labor-controversies. Acta Clin Croat. 2015;54:330–6. [PubMed] [Google Scholar]
- 2.Moschini V, Marra G, Dabrowska D. Complications of epidural and combined spinal-epidural analgesia in labour. Minerva Anestesiol. 2006;72:47–58. [PubMed] [Google Scholar]
- 3.Bisinotto FM, Dezena RA, Fabri DC, Abud TM, Canno LH. Intracranial subdural hematoma: A rare complication following spinal anesthesia: Case report. Rev Bras Anestesiol. 2012;62:88–95. doi: 10.1016/S0034-7094(12)70107-1. [DOI] [PubMed] [Google Scholar]
- 4.Nolte CH, Lehmann TN. Postpartum headache resulting from bilateral chronic subdural hematoma after dural puncture. Am J Emerg Med. 2004;22:241–2. doi: 10.1016/j.ajem.2004.02.032. [DOI] [PubMed] [Google Scholar]
- 5.Arevalo-Rodriguez I, Ciapponi A, Roqué i Figuls M, Muñoz L, Bonfill Cosp X. Posture and fluids for preventing post-dural puncture headache. Cochrane Database Syst Rev. 2016;3:CD009199. doi: 10.1002/14651858.CD009199.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scott DB, Hibbard BM. Serious non-fatal complications associated with extradural block in obstetric practice. Br J Anaesth. 1990;64:537–41. doi: 10.1093/bja/64.5.537. [DOI] [PubMed] [Google Scholar]
- 7.Zeidan A, Farhat O, Maaliki H, Baraka A. Does postdural puncture headache left untreated lead to subdural hematoma? Case report and review of the literature. Int J Obstet Anesth. 2006;15:50–8. doi: 10.1016/j.ijoa.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Cuypers V, Van de Velde M, Devroe S. Intracranial subdural haematoma following neuraxial anaesthesia in the obstetric population: A literature review with analysis of 56 reported cases. Int J Obstet Anesth. 2016;25:58–65. doi: 10.1016/j.ijoa.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Dal Pozzo G. Magnetic Resonance Compendium - Cranium e Rachide. UTET Medical Sciences S.P.A reprint; 2009. [Google Scholar]
- 10.Peralta F, Devroe S. Any news on the postdural puncture headache front? Best Pract Res Clin Anaesthesiol. 2017;31:35–47. doi: 10.1016/j.bpa.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Lee J, Lim YM, Suh DC, Rhim SC, Kim SJ, Kim KK, et al. Clinical presentation, imaging findings, and prognosis of spinal dural arteriovenous fistula. J Clin Neurosci. 2016;26:105–9. doi: 10.1016/j.jocn.2015.06.030. [DOI] [PubMed] [Google Scholar]
- 12.Ferrante E, Rubino F, Beretta F, Regna-Gladin C, Ferrante MM. Treatment and outcome of subdural hematoma in patients with spontaneous intracranial hypotension: A report of 35 cases. Acta Neurol Belg. 2018;118:61–70. doi: 10.1007/s13760-017-0845-0. [DOI] [PubMed] [Google Scholar]
- 13.Flanagan EP, Pittock SJ. Diagnosis and management of spinal cord emergencies. Handb Clin Neurol. 2017;140:319–35. doi: 10.1016/B978-0-444-63600-3.00017-9. [DOI] [PubMed] [Google Scholar]