Abstract
Background
Limb salvage surgery with vascular reconstruction is currently considered as the standard treatment for extremity soft tissue sarcoma (STS), showing equivalent oncologic outcome compared with amputation. In this retrospective study, the surgical and functional outcomes after arterial or venous reconstruction in limb salvage surgery for STS were analyzed.
Methods
Consecutive patients who underwent vascular resection and reconstruction as part of limb salvage surgery for extremity STS from July 2009 to June 2015 were included in this study. Incidence of surgical complication, graft patency, and patients' functional outcome were reviewed.
Results
During the study period, 14 arteries and 13 veins were reconstructed in 17 patients (artery only in 4, vein only in 3, artery and vein in 10). Autologous great saphenous vein (GSV) was the most commonly used vascular conduit in both arterial and venous reconstruction (78.6% and 77.0%). The patency of synthetic graft was significantly lower than that of the autologous vein conduit (log rank test, P = 0.001). Among 15 patients with tumors in lower extremity, 13 were ambulatory after limb salvage surgery. During median follow up of 23.3 months (interquartile range 39.9 months), 2 patients (11.7%) needed amputation of the initially salvaged limb due to local recurrence.
Conclusion
Limb salvage surgery of soft tissue tumor combined with vascular reconstruction showed favorable functional outcome with good local control. Autologous vein conduit is preferred over synthetic graft both in arterial and venous reconstruction.
Keywords: Blood Vessels, Limb Salvage, Extremities, Sarcoma
Graphical Abstract
INTRODUCTION
Soft tissue sarcoma (STS) is a rare malignant neoplasm that accounts for less than 1% of all cancers diagnosed annually.1 Aggressive surgical excision of these tumors provides an opportunity for complete cure. When STS in the extremities invaded major blood vessels, amputation was previously considered as the treatment of choice for a complete oncologic resection rather than local excision. This was due to the high recurrence rate and hematogenous metastasis after local excision close to vascular structure. However, there was no difference in oncologic outcome between the surgical resection with adequately wide margins and the amputation.2,3 Therefore, limb salvage surgery has been preferred because patients have significantly better quality of life. Even in patients with distant metastasis, limb salvage surgery should be contemplated for long-term maintenance of a good quality of life.
The purposes of this study were to analyze the oncologic and functional outcome of patients who underwent vascular reconstructions for limb salvage in extremity sarcomas, and to define the risk factors for poor outcomes.
METHODS
This is a retrospective case series of patients with STS or locally aggressive fibromatosis in the extremities, who received simultaneous vascular resection and reconstruction at Seoul National University Hospital from July 1, 2009 to June 31, 2015. Electronic medical records and imaging studies were reviewed, including histologic type of the tumor, surgical complication, graft type, graft patency and functional outcomes.
All patients were initially evaluated by orthopedic oncology surgeons and underwent preoperative computed tomography (CT) or magnetic resonance imaging (MRI) to identify tumor invasion of major vessels. If any vascular invasion is suspected, consultation to a vascular surgeon is done. On the day before operation, preoperative duplex vein mapping of the contralateral saphenous vein is done by a registered vascular technologist. After en bloc dissection of the tumor with vascular pedicles in situ is done by the oncologic surgeon, the vascular surgeon starts to harvest the contralateral great saphenous vein (GSV) by multiple small stab incision as long as required. And after injecting a bolus of intravenous heparin, vascular clamps are applied on the proximal and distal vascular pedicles. Arterial reconstruction is done in reversed vein interposition graft, and then vein reconstruction is done if needed. After completion of the anastomosis, distal pedal flow is monitored by continuous wave Doppler. If the arterial flow is not normal, intraoperative angiography is performed. Whenever possible, vascular reconstruction was performed using contralateral GSV with a diameter greater than 3 mm in order to prevent excessive limb swelling. When it was not available, ipsilateral GSV or a prosthetic graft of expanded polytetrafluoroethylene (ePTFE) were used. Low molecular weight heparin (1 mg/kg) was given subcutaneously to all patients in the absence of postoperative bleeding until oral administration was possible. Use of antiplatelet agent or anticoagulant was determined by the surgeons' preference regardless of the type of vascular reconstruction or graft.
Statistical analysis
All statistical analysis was performed using SPSS software version 23 (IBM Corp., Armonk, NY, USA). The Kaplan-Meier method was used to estimate overall survival probability as well as the rates of arterial or venous graft patency. The results were considered significant if the P value was less than 0.05 with confidence intervals (CI) of 95%.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of Seoul National University Hospital (approval No. 1802-127-926).
RESULTS
A total of 17 patients received major vascular reconstruction after en bloc resection of the extremity STS. The median age was 47 years (range, 15–80 years) and there were 8 males (47.1%) and 9 females (52.9%). The characteristics of the extremity STS were listed in Table 1, including the sites of the tumors, the histologic types of the sarcomas, the tumor grade, and tumor status. The most common site of the primary tumor was thigh in 70.6%, and the most frequent histologic type was osteosarcoma in 3 (17.7%), followed by synovial sarcoma, chondrosarcoma, and fibromatosis. One third of the tumors were recurrent tumors. The mean tumor size in the largest dimension was 10.2 cm (range, 5.5–16.5 cm). The tumor was resected en bloc with free resection margins.
Table 1. The characteristics of the extremity tumors.
| Site of tumor | Patients (n = 17), No. (%) | |
|---|---|---|
| Lower extremity | ||
| Thigh | 12 (70.6) | |
| Calf | 2 (11.7) | |
| Inguinal | 1 (5.9) | |
| Upper extremity | ||
| Axilla | 1 (5.9) | |
| Upper arm | 1 (5.9) | |
| Histologic type of sarcoma | ||
| Osteosarcoma | 3 (17.7) | |
| Synovial sarcoma | 2 (11.7) | |
| Chondrosarcoma | 2 (11.7) | |
| Fibromatosis | 2 (11.7) | |
| Ewing sarcoma | 1 (5.9) | |
| Pleomorphic spindle cell sarcoma | 1 (5.9) | |
| Angiosarcoma | 1 (5.9) | |
| Myxoid malignant fibrous histocytoma | 1 (5.9) | |
| Undifferentiated sarcoma | 1 (5.9) | |
| Malignant hemangiopericytoma | 1 (5.9) | |
| Fibrohistiocytoma | 1 (5.9) | |
| Hemangioendoendothelioma | 1 (5.9) | |
| Tumor grade | ||
| FNCLCC gr1a | 0 | |
| FNCLCC gr2 | 8 (47.1) | |
| FNCLCC gr3 | 5 (29.4) | |
| Unclassified | 4 (23.5)b | |
| Tumor | ||
| Primary | 11 (64.7) | |
| Recurred | 6 (35.3)c | |
aFrench Federation Nationale des Centres de Lutte Contrele Cancer. bTwo cases of fibromatosis were included. cTwo cases of fibromatosis were included.
The characteristics of vessel reconstruction was summarized in Tables 2 and 3. A total of 14 arteries and 13 veins were reconstructed in 17 patients after en bloc resection (both artery and vein in 10, artery only in 4, and vein only in 3). The most common reconstruction method was femoral-femoral interposition graft in 9 patients (52.9%). Among them, 8 patients had arterial and venous reconstructions simultaneously and one patient required only arterial reconstruction. The most commonly used conduit was autologous GSV in both arterial (11/14, 78.6%) and venous reconstruction (10/13, 77.0%). In the other patients, ringed ePTFE graft was used (6/27, 22.2%). During the postoperative period, 5 early thrombotic occlusions within 1 month after reconstruction developed, including 2 arterial and 3 venous reconstruction (Table 4). Thrombectomy was successfully done in 2 arterial thromboses. Conservative therapy was done in venous thrombosis. There were no infections related to the vascular grafts. Fluid collection occurred in 5 patients without surgical wound infection.
Table 2. The characteristics of reconstructed vessels.
| Characteristics | Patients (n = 17), No. (%) | ||
|---|---|---|---|
| Resected vessel | |||
| Artery | 4 (23.5) | ||
| Vein | 3 (17.6) | ||
| Artery and Vein | 10 (58.9) | ||
| Graft used for reconstruction | |||
| Substitute for arterial reconstruction | 14 | ||
| Ipsilateral GSV | 5 (35.7) | ||
| Contralateral GSV | 6 (42.9) | ||
| ePTFE | 3 (21.4) | ||
| Substitute for venous reconstruction | 13 | ||
| Ipsilateral GSV | 4 (30.8) | ||
| Contralateral GSV | 6 (46.1) | ||
| ePTFE | 3 (23.1) | ||
GSV = great saphenous vein, ePTFE = expanded polytetrafluoroethylene.
Table 3. The characteristics of performed bypass.
| Bypass performed | Artery | Vein | Artery and vein | Patients (n = 17), No. (%) | |
|---|---|---|---|---|---|
| Lower Extremity | |||||
| Ilio-femoral | 1 | 1 (5.9) | |||
| Femoro-femoral | 1 | 8 | 9 (52.9) | ||
| Popliteo-popliteal | 1 | 2 | 1 | 4 (23.5) | |
| Popliteo-tibial | 1 | 1 (5.9) | |||
| Upper Extremity | |||||
| Axillo-brachial | 1 | 1 (5.9) | |||
| Brachio-brachial | 1 | 1 (5.9) | |||
Table 4. The characteristics of the occluded grafts.
| Occluded graft | Early occlusiona | Late occlusion | Total No. (%) | |
|---|---|---|---|---|
| Type of revascularization | ||||
| Arterial | 2 | 1 | 3/14 (21.4) | |
| Venous | 3 | 2 | 5/13 (38.5) | |
| Vascular substitute | ||||
| Great saphenous vein | 2 | 1 | 3/21 (14.3) | |
| Synthetic graft | 3 | 2 | 5/6 (83.3) | |
aEarly occlusion is ‘within 1 month after surgery.’
Median follow-up duration was 23.3 months (interquartile range 39.9 months). Two patients (11.7%) required amputation of the initially salvaged limb due to local recurrence, and later died of tumor. Nine patients (53%) were alive without recurrence, and six were alive with recurrence. The local recurrence rate after 2 years was 47%, and the overall limb salvage rate was 88.2% (15/17).
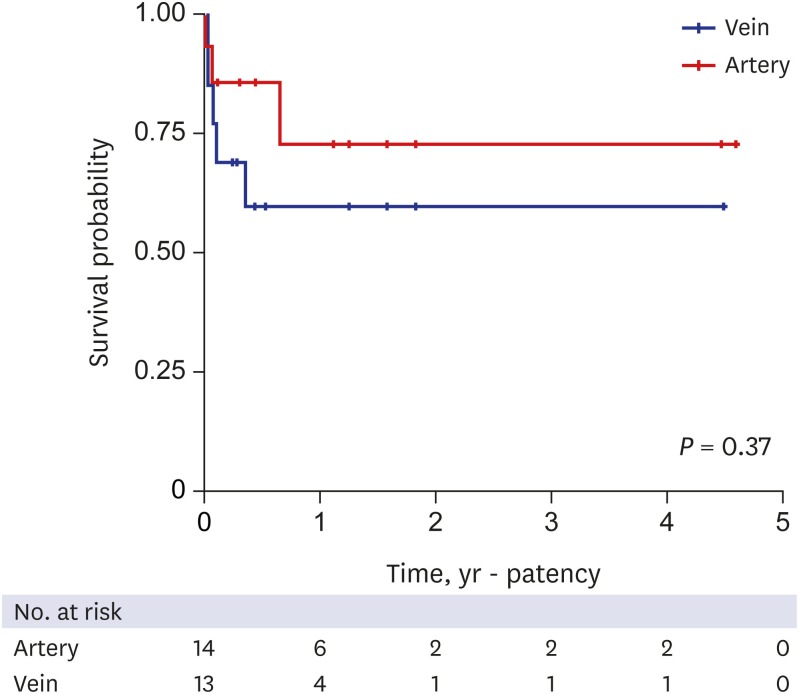
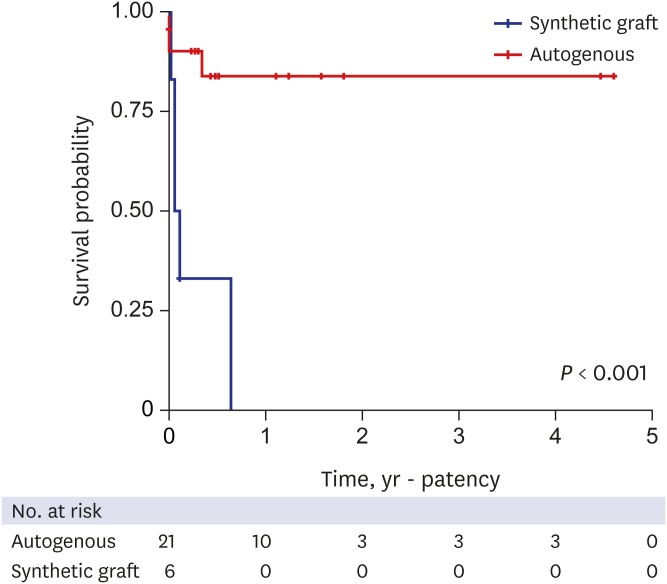
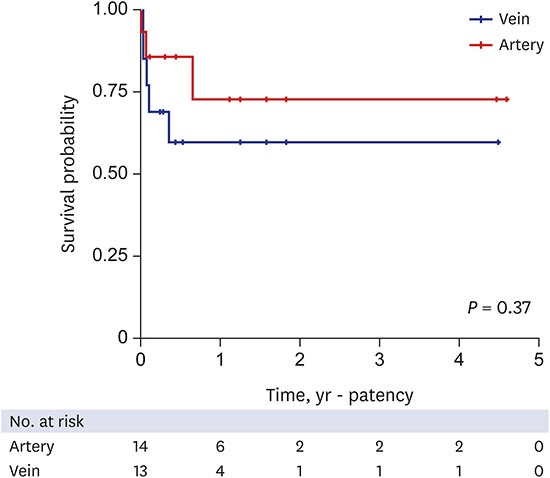
The characteristic of the occluded grafts was summarized in Table 4. With regard to the type of revascularization, occlusions occurred in 3 patients with arterial reconstruction and in 5 patients with venous reconstruction. The occlusion rate of venous reconstruction was greater than arterial reconstruction, but there was no significant difference between the two groups (P = 0.37). The Kaplan-Meyer analysis of the patency rates of arterial or venous reconstructions are illustrated in Fig. 1. The 2-year graft patency was significantly lower in synthetic graft than autologous vein (14.3% vs. 83.3%, P < 0.001) (Fig. 2).
Fig. 1. Overall patency rates of arterial or venous reconstructions.
Fig. 2. Overall patency rates according to the conduit, autologous vs. synthetic graft.
Among 15 patients with tumor in lower extremity, 13 patients (86.7%) were ambulatory without assisting devices. Vascular reconstruction after en bloc resection resulted in quite good functional outcome.
DISCUSSION
Vascular reconstruction is inevitable to perform the limb salvage surgery after resection of STS infiltrating major blood vessels. Despite the risks of increasing difficulty of surgery, longer operation time, and limited patency in some cases, the reason for doing revascularization is to avoid a severe functional impairment. Vascular surgeons often are involved as "reconstructive surgeons" during these limb salvage surgeries due to their unique skills in dealing with vessels. There has been renewed interest in the role of vascular surgeon, but there are few reports regarding that in limb salvage surgery. Vascular reconstruction has played a major role in improving the successful limb salvage surgery.
STS is an aggressive tumor with a reported risk of local recurrence after surgery as high as 65%.4,5 Therefore, en bloc resection with adequate resection margin was the main operative principle for STS, and invasion of major vessels has been considered as an indication for amputation until the 1970's.6 Recently, however, great progresses in surgical skills and imaging modalities made it possible to avoid amputation. Fortner et al.7 reported the first successful vascular reconstructions in conjunction with limb salvage surgery for STS in the lower extremity. And some demonstrated that there were no significant differences in outcomes between amputated patients and the limb salvage group.8,9 Nowadays, limb salvage surgery is considered as the standard treatment of STS for better functional outcomes and quality of life.7,10
The options for vascular substitutes can be autologous or prosthetic. Currently there is no clear guideline of graft selection in vascular reconstruction. However, autologous vein graft seems to be the preferred method of reconstruction because the patency of the autologous graft was significantly superior to that of the synthetic graft.1,2
There are some technical points to mention about the vascular reconstruction after extremity sarcoma resection. First, preoperative vascular consultation and duplex imaging is performed in all patients. Second, to minimize the ischemic time of the affected limb, oncologic surgeons and vascular surgeons cooperated efficiently, such as vein harvest before tumor resection, and heparin injection before arterial clamping. And third, aggressive postoperative monitoring by the oncologist on tumor recurrence and by vascular surgeons on the patency of reconstructed vessels. Therefore, it is very important to make a good collaboration team with vascular surgeons and orthopedic oncologic surgeons.
The best conduit for bypass is the autologous saphenous vein. In this series, the patency rate of prosthetic graft was significantly poorer than the autologous vein. Usually after bypass, single or double antiplatelet agents were prescribed according to the surgeon's preference. But this data may warrant more aggressive antithrombotic therapy in this subgroup of patients with a prosthetic graft. Fortunately, there were no cases of deep vein thrombosis (DVT) or graft infection after the surgery. Postoperative antibiotics and active mechanical prevention of DVT are important.
The need for venous reconstruction after resection is still in debate. Some surgeons preferred venous reconstruction because of the risk of severe venous congestion, leg edema, and resultant decrease in arterial perfusion. Nishinari et al.11 reported that the occlusion rate of arterial reconstruction was only 4.8% and that of venous reconstruction was 13%, with no statistical significance. In this series, no significant differences have been found between the occlusion rates of arterial and venous reconstruction (P = 0.37). But there has been considerable disagreement for the necessity of simultaneous venous reconstruction,12 because of the high occlusion rate and no difference of severity of leg swelling. Tsukushi et al.13 compared the results of 12 arterial reconstructions only and 13 arterial and venous reconstructions, and reported that the rate of leg edema and functional outcomes after the operation were similar in both groups, confirming mandatory venous reconstruction was not necessary. Davis et al.14 also reported that 9 vascular reconstructions were necessary during the operations of 154 STS, and venous reconstruction was not performed. In our center, the authors usually try to reconstruct both artery and vein if the autologous vein conduit is good. But, if a prosthetic graft is to be used, vein reconstruction is not mandatory.
This study has several limitations. First, this study was a retrospective single center study with a relatively small sample size. The inherent selection bias may have limitations to generalize the findings. Second, there was no regular surveillance protocol including ankle brachial index or duplex ultrasonography. But regular physical examinations and hand-held Doppler examination were done, minimizing the risk of underdiagnosing the graft failure. Third, postoperative antiplatelet or anticoagulant medication after revascularization was not standardized, and was dependent to the surgeons' preference. Further multicenter studies are necessary to define the optimal surgical technique or conduit, especially for vein reconstruction.
Limb salvage surgery of extremity STS combined with vascular reconstruction showed favorable functional outcome with good local control. Autologous vein conduit is preferred over synthetic graft both in arterial and venous reconstruction. In order to achieve the optimal outcome of vascular reconstruction after sarcoma removal in the extremity, it is important to make a good collaboration team with vascular surgeons and orthopedic oncologic surgeons.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
Author Contributions: Conceptualization: Park DD, Cho SS, Han AR, Ha JW, Min SK. Data curation: Park DD, Cho SS, Han AR. Formal analysis: Park DD, Cho SS, Han AR. Methodology: Park DD, Choi CJ, Ahn SH, Min SI, Min SK. Writing - original draft: Park DD. Writing - review & editing: Park DD, Ha JW, Min SK.
References
- 1.Lawrence W., Jr Concepts in limb-sparing treatment of adult soft tissue sarcomas. Semin Surg Oncol. 1988;4(1):73–77. doi: 10.1002/ssu.2980040114. [DOI] [PubMed] [Google Scholar]
- 2.Schwarzbach MH, Hormann Y, Hinz U, Bernd L, Willeke F, Mechtersheimer G, et al. Results of limb-sparing surgery with vascular replacement for soft tissue sarcoma in the lower extremity. J Vasc Surg. 2005;42(1):88–97. doi: 10.1016/j.jvs.2005.03.017. [DOI] [PubMed] [Google Scholar]
- 3.Nagarajan R, Neglia JP, Clohisy DR, Robison LL. Limb salvage and amputation in survivors of pediatric lower-extremity bone tumors: what are the long-term implications? J Clin Oncol. 2002;20(22):4493–4501. doi: 10.1200/JCO.2002.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Williard WC, Hajdu SI, Casper ES, Brennan MF. Comparison of amputation with limb-sparing operations for adult soft tissue sarcoma of the extremity. Ann Surg. 1992;215(3):269–275. doi: 10.1097/00000658-199203000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karakousis CP, Proimakis C, Walsh DL. Primary soft tissue sarcoma of the extremities in adults. Br J Surg. 1995;82(9):1208–1212. doi: 10.1002/bjs.1800820919. [DOI] [PubMed] [Google Scholar]
- 6.Karakousis CP, Emrich LJ, Rao U, Krishnamsetty RM. Feasibility of limb salvage and survival in soft tissue sarcomas. Cancer. 1986;57(3):484–491. doi: 10.1002/1097-0142(19860201)57:3<484::aid-cncr2820570314>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 7.Fortner JG, Kim DK, Shiu MH. Limb-preserving vascular surgery for malignant tumors of the lower extremity. Arch Surg. 1977;112(4):391–394. doi: 10.1001/archsurg.1977.01370040043007. [DOI] [PubMed] [Google Scholar]
- 8.Abbas JS, Holyoke ED, Moore R, Karakousis CP. The surgical treatment and outcome of soft-tissue sarcoma. Arch Surg. 1981;116(6):765–769. doi: 10.1001/archsurg.1981.01380180025006. [DOI] [PubMed] [Google Scholar]
- 9.Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980;(153):106–120. [PubMed] [Google Scholar]
- 10.Mason GE, Aung L, Gall S, Meyers PA, Butler R, Krüg S, et al. Quality of life following amputation or limb preservation in patients with lower extremity bone sarcoma. Front Oncol. 2013;3(3):210. doi: 10.3389/fonc.2013.00210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nishinari K, Krutman M, Aguiar Junior S, Pignataro BS, Yazbek G, Zottele Bomfim GA, et al. Surgical outcomes of vascular reconstruction in soft tissue sarcomas of the lower extremities. J Vasc Surg. 2015;62(1):143–149. doi: 10.1016/j.jvs.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 12.Bonardelli S, Nodari F, Maffeis R, Ippolito V, Saccalani M, Lussardi L, et al. Limb salvage in lower-extremity sarcomas and technical details about vascular reconstruction. J Orthop Sci. 2000;5(6):555–560. doi: 10.1007/s007760070005. [DOI] [PubMed] [Google Scholar]
- 13.Tsukushi S, Nishida Y, Sugiura H, Nakashima H, Ishiguro N. Results of limb-salvage surgery with vascular reconstruction for soft tissue sarcoma in the lower extremity: comparison between only arterial and arterovenous reconstruction. J Surg Oncol. 2008;97(3):216–220. doi: 10.1002/jso.20945. [DOI] [PubMed] [Google Scholar]
- 14.Davis LA, Dandachli F, Turcotte R, Steinmetz OK. Limb-sparing surgery with vascular reconstruction for malignant lower extremity soft tissue sarcoma. J Vasc Surg. 2017;65(1):151–156. doi: 10.1016/j.jvs.2016.05.094. [DOI] [PubMed] [Google Scholar]