Dear Sir,
Compression of the suprascapular nerve at the spinoglenoid notch may cause shoulder pain. One of the earliest descriptions of suprascapular nerve entrapment was in 1959.[1] It is an uncommon condition; hence, it is not often recognized as a cause of vague shoulder pain until there is atrophy of the infraspinatus. We report a case of atraumatic unilateral shoulder pain where a paralabral cyst was diagnosed using magnetic resonance imaging (MRI) with resultant suprascapular nerve entrapment neuropathy and subsequently treated via ultrasound-guided aspiration.
A 42-year-old man presented with atraumatic right shoulder pain for 1 month. O'Brien's test was positive and the initial clinical impression of the orthopedist was a labral tear. MRI for shoulder showed a superoposterior labral tear with a large paralabral cyst with suprascapular nerve impingement. The orthopedist referred the patient to a physiatrist for the evaluation of paralabral cyst aspiration. Physical examination of the shoulder revealed mild atrophy of the infraspinatus with no significant muscle weakness or instability, and the range of motion was full. Electromyography revealed markedly increased polyphasic waves with reduced motor recruitments in the right infraspinatus muscle and slightly increased giant waves in the right supraspinatus muscle, indicating chronic right suprascapular neuropathy which was consistent with the clinical diagnosis of suprascapular nerve entrapment by the paralabral cyst. Ultrasound (linear probe, 5–14 MHz, PLT-1005BT, Toshiba TUS-A500) showed a well-defined, homogeneously hypoechoic mildly compressible cystic lesion without vascularity measuring 18.4 mm × 10.8 mm × 24.4 mm at the spinoglenoid notch [Figure 1a]. The cystic lesion was aspirated with a 18G needle under ultrasound guidance [Figure 1b] and 3 ml of highly sticky gel like clear substance was removed. The patient's pain improved postprocedure [Figure 1c].
Figure 1.
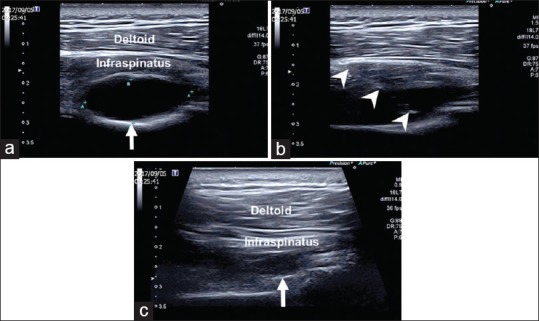
(a) A ganglion cyst (arrow) located the spinoglenoid notch. (b) Ultrasound-guided aspiration of the ganglion cyst. Arrowheads: Needle. (c) Decreased size of the ganglion cyst (arrow) postaspiration
The suprascapular nerve is a branch of the upper trunk of the brachial plexus and is a mixed sensorimotor nerve subserving motor innervation to both the supraspinatus and infraspinatus muscles and sensory innervation to the glenohumeral and acromioclavicular joints. A detailed review of the anatomy of the suprascapular nerve is available.[2] Entrapment of the suprascapular nerve at the level of the suprascapular notch will result in weakness and atrophy of both the supraspinatus and infraspinatus while entrapment at the level of the spinoglenoid notch will result in isolated infraspinatus weakness and atrophy.
Suprascapular nerve entrapment accounts for 1%–2% of shoulder pain and mainly occurs in patients under 40 years of age. There is a gender bias for males to develop ganglion compressing the suprascapular nerve.[3] Pain is the most common symptom of suprascapular nerve entrapment and the three most common causes include trauma, inflammation, and extrinsic compression.[4] The differential diagnosis is broad and include brachial plexopathy, disorders of the cervical spine, glenohumeral pathology, and rotator cuff tendinopathy.
MRI and electromyography are usually used in the evaluation of suprascapular neuropathy. Ultrasound has also been used to evaluate paralabral cysts compressing the suprascapular nerve. When ultrasound is used to evaluate such paralabral cysts, areas to be examined include the spinoglenoid notch, suprascapular notch, and infraspinatus. Paralabral cysts are most commonly located in the spinoglenoid notch.[5]
Paralabral cysts are thought to arise from the seepage of synovial fluid into the paralabral tissue as a result of a capsular defect. Fluid then accumulates due to a ball valve effect. Not surprisingly, the majority of paralabral cysts are associated with labral tears as in this case.[6]
Paralabral cysts may be managed conservatively with oral medications such as nonsteroidal anti-inflammatory drugs or percutaneous aspiration. Percutaneous aspiration may be computed tomography guided or ultrasound guided. Some authors had also reported the injection of corticosteroids after the aspiration of paralabral cysts. When conservative management has failed, it may be treated surgically by open excision or arthroscopic decompression.[7,8]
Apart from being less costly than MRI and less invasive than electromyography, ultrasound has an additional advantage of being able to provide image guidance for the aspiration of the paralabral cyst. In the current case, the patient's shoulder pain was successfully treated by ultrasound-guided aspiration of the paralabral cyst, instead of a more invasive surgical intervention.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Thompson WA, Kopell HP. Peripheral entrapment neuropathies of the upper extremity. N Engl J Med. 1959;260:1261–5. doi: 10.1056/NEJM195906182602503. [DOI] [PubMed] [Google Scholar]
- 2.Clavert P, Thomazeau H. Peri-articular suprascapular neuropathy. Orthop Traumatol Surg Res. 2014;100:S409–11. doi: 10.1016/j.otsr.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Zehetgruber H, Noske H, Lang T, Wurnig C. Suprascapular nerve entrapment. A meta-analysis. Int Orthop. 2002;26:339–43. doi: 10.1007/s00264-002-0392-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hill LJ, Jelsing EJ, Terry MJ, Strommen JA. Evaluation, treatment, and outcomes of suprascapular neuropathy: A 5-year review. PM R. 2014;6:774–80. doi: 10.1016/j.pmrj.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Hashimoto BE, Hayes AS, Ager JD. Sonographic diagnosis and treatment of ganglion cysts causing suprascapular nerve entrapment. J Ultrasound Med. 1994;13:671–4. doi: 10.7863/jum.1994.13.9.671. [DOI] [PubMed] [Google Scholar]
- 6.Piatt BE, Hawkins RJ, Fritz RC, Ho CP, Wolf E, Schickendantz M, et al. Clinical evaluation and treatment of spinoglenoid notch ganglion cysts. J Shoulder Elbow Surg. 2002;11:600–4. doi: 10.1067/mse.2002.127094. [DOI] [PubMed] [Google Scholar]
- 7.Shon MS, Jung SW, Kim JW, Yoo JC. Arthroscopic all-intra-articular decompression and labral repair of paralabral cyst in the shoulder. J Shoulder Elbow Surg. 2015;24:e7–e14. doi: 10.1016/j.jse.2014.05.017. [DOI] [PubMed] [Google Scholar]
- 8.Bathia N, Malanga G. Ultrasound-guided aspiration and corticosteroid injection in the management of a paralabral ganglion cyst. PM R. 2009;1:1041–4. doi: 10.1016/j.pmrj.2009.10.001. [DOI] [PubMed] [Google Scholar]


