Abstract
Reduction of the remaining residual cardiovascular risk is a clinical unmet need currently being addressed through a combination of further reduction of plasma concentrations of low-density lipoproteins (LDLs) and increasing plasma concentrations of high-density lipoproteins (HDLs). This brief review sets out the so-called HDL hypothesis and summarises the clinical results of the family of drugs, which function to raise plasma HDL concentration through inhibition of cholesteryl ester transfer proteins (CEPT).
Keywords: Apolipoprotein AI, cholesteryl ester transfer protein, high-density lipoprotein, low-density lipoprotein
The concentration of plasma low-density lipoprotein cholesterol (LDL-C) is reduced, while that of total high-density lipoprotein cholesterol (HDL-C) is increased, following inhibition of cholesteryl ester transfer protein (CETP). This combined effect has made inhibition of CETP an attractive pharmacological approach for reducing the residual incidence of cardiovascular disease (CVD) remaining after optimal LDL-lowering therapy. However, since HDLs represent a complex dynamic heterogeneous family of particles varying in size, composition and function, the concept is not without difficulties. CVD has been shown to alter the particle complexity, in terms of both relative abundance of size/density and composition. The effects of raising the plasma concentration of HDL-C on a background of ‘disease modified’ are largely unknown. Randomised clinical trials to date have failed to provide evidence of benefit for this approach. The CETP inhibitor, dalcetrapib, which showed no harmful effect, also had no ability to reduce LDL-C and the study may be considered as providing strong evidence that HDL raising per se is not an effective approach in reducing CVD. The remaining members of the CETP inhibitor family, currently in Phase III studies, are able to reduce plasma LDL-C and may, thus, provide a beneficial effect on CVD, as long as it is not reduced through the adverse effects of raising plasma HDL-C, which may well be dysfunctional. Subsequent analysis of these large randomised controlled trials, due to be published in 2016/17, may allow us to further understand the effect of CVD on the complex metabolism of HDL-C.
The Birth of the HDL Hypothesis
It is a well-established fact that elevated plasma concentrations of low-density lipoprotein-cholesterol (LDL-C) is one of the most important risk factors for developing coronary artery disease (CAD), and, eventually, coronary heart disease (CHD)[1] and other forms of atherosclerotic cardiovascular disease (CVD). Targeting LDL-C reduction has been effective in lowering CVD risk, through the use of HMG-CoA reductase inhibitors (statins) for both primary and secondary CVD prevention as the first-line therapy, resulting in reduced CV events and overall mortality[2,3]. However, despite reduction in LDL-C, 18–41 % with moderate doses of statins and 40–60 % with higher doses or more potent statins, there remains a significant residual cardiovascular risk. In the late 1970s the inverse relationship between plasma concentration of HDL-C and CVD risk was identified[4] and subsequent prospective data from the Framingham Heart and ARIC studies further supported this idea[5,6]. It was proposed that CHD risk was inversely related to plasma concentration of HDL-C, owing to the ability of HDL particles to remove cholesterol from developing atherosclerotic lesions, and thus, the HDL hypothesis was conceived. Subsequent in vivo studies, in which plasma HDL-C was raised by infusion or transgenic expression of human apolipoprotein AI (ApoAI) in rabbit and mouse models of atherosclerosis demonstrated a potent atheroprotective effect[7–9]. With this wide array of potential benefits, raising plasma HDL-C was seen as a promising new drug target.
Raising Plasma Concentration of HDL-C
Although lifestyle changes, such as vigorous exercise, smoking cessation and weight loss have been shown to moderately increase plasma concentrations of HDLs[10–13], individuals with low plasma HDL-C are more likely to respond to pharmacological treatment that increases HDL. Whilst statins, fibrates and some thiazolidenediones have been shown to modestly increase plasma concentrations of HDL-C[14–16], nicotinic acid or niacins have been used to provide a more robust increase by 15–16 %[17,18]. Niacin increases plasma HDL-C by inhibiting the putative hepatocyte HDL-C catabolism receptor, preventing HDL-C catabolism, and thereby increasing the half-life of circulating HDL-C[18]. However, neither of the two large randomised controlled clinical trials, AIM-HIGH and HPS2-THRIVE, were able to demonstrate a difference in the primary end point despite favourable changes in HDL-C concentration[17,18]. Although these data may question the ability to provide a cardioprotective effect through elevating plasma HDL-C, nicotinic acid and niacins have dramatic side effects, such as flushing, which may well compromise any benefits observed.
CETP as a Novel Drug Target to Raise Plasma Concentration of HDLs.
Development of a novel target for elevating plasma HDL-C concentration was derived from analysis of the understanding of the biochemistry of HDL metabolism and particle dynamics. CETP is a hydrophobic glycoprotein which can catalyse the transfer of cholesteryl esters, generated by lecithin:cholesterol acyltransferase (LCAT), principally in larger α-HDLs, to other lipoproteins in exchange for triglycerides (TGs), derived primarily from very low-density lipoproteins (VLDL) or chylomicrons[19] (Figure 1). This process of lipid exchange has been shown to increase the relative abundance of small lipid-poor preβ-HDL particles, which play a primary role in the acquisition of cholesterol from cell membranes via the ABCA1 transporter (reverse cholesterol transport)[20]. These data seeded the idea that modulation of HDL particle abundance could increase the ability to remove cholesterol from peripheral tissues, and was further supported by numerous in vivo studies where inhibition of CETP in animal models prevented cholesterol-induced atherosclerosis[21–23], whilst CETP gene transfer in mice (a species lacking CETP activity) increased lesion formation[21]. Although these findings were encouraging, subsequent studies in other models did not reiterate the protective effect of CETP inhibition shown previously[24–26]. However, these data are difficult to compare and may reflect disparity in means by which CETP is modulated and in the mechanisms involved in generating atheromatous lesions in the specific models. In an extremely elegant set of experiments, Brousseau and colleagues were able to show, that raising HDL-C using the CETP-inhibitor drug, torcetrapib, did so through an effect on delaying catabolism[27]. Both torcetrapib and niacin increase HDL by delaying catabolism, which, in turn, increases the half-life of HDL-C, but neither of these methods have led to a beneficial clinical effect. As HDLs are heterogeneous, dynamic particles, it is likely that their structure and function will be significantly modified by prolonging the circulatory half-life and would depend largely on the effect of the clinical status of the patient.
Figure 1: Schematic diagram showing activity of CETP.
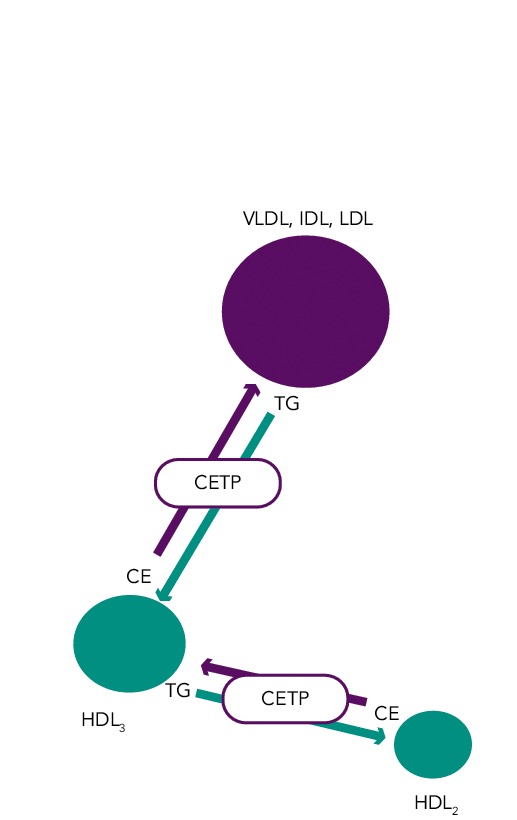
CETP modulates cholesterol ester (CE) exchange for triglycerides (TG) between HDL particles (homotypic transfer), leading to the larger HDL2 particle, and apoB-containing particles (VLDL, IDL, LDL) (heterotypic transfer).
CETP Inhibition – Effect of Gene Polymorphisms
The human CETP gene has been mapped to chromosome 16 on the 16q21 locus, spanning about 25 kb and consisting of 16 exons and 15 introns. The current availability of DNA arrays capable of screening the entire genome for many thousands of SNPs in large cohorts has provided a new tool for studying the aetiology of complex diseases. However, the putative instrumental variables associated with alleles and clinical outcome are not always appropriate and the method is also limited by problems associated with linkage disequilibrium. Voight and colleagues reported a large Mendelian randomisation study confirming that lower CETP activity, when associated with both lower LDL-C and higher HDL-C, is associated with cardiovascular benefit[28]. Studies of CETP gene polymorphisms have been controversial. The B2 allele of the Taq1B SNP of the CETP gene (which is associated with low CETP activity and raised HDL-C) was found to be accompanied by a lower than average risk of CVD29. Further analysis showed that this association was limited to one ethnic group (Chinese)[30]. In a 10-year follow-up study of more than 18,000 women, among 350,000 SNPs, it was found that three SNPs in or close to the CETP gene (rs708272, rs432992 and rs7202364) were associated with an increase in plasma HDL-C and a reduced incidence of myocardial infarction in this population[31]. Current genetic analysis indicates that a decrease in CETP activity is correlated with a decrease in CVD risk.
Prospective Cohort Studies of CETP and CVD Risk
Measuring CETP activity is technically challenging and work by Ritsch and colleagues provides our sole reference data that there is a linear relationship between activity and concentration[32]. Prospective observational cohort studies to investigate the relationship between the plasma concentration of CETP activity or concentration and the risk of cardiovascular events generally show an inverse correlation, suggesting a negative association with CETP[33–38]. Of the three studies that evaluated populations free of CVD, two of them assayed CETP activity long-term, with a 10–15-year follow-up[33,34], whilst the other study measured concentration and had a two-year follow-up[35]. The remaining three studies considered patients with clinical CAD or CHD and measured CETP activity[36–38]. Assessment of CETP activity or mass requires purification from total plasma or serum, which is then a measurement made in the absence of the proper biological complexity of whole blood and its many affecting factors; for example, the presence of ApoC-I, an isoform of apoliprotein C that has been recently demonstrated to be an endogenous inhibitor of CETP activity[39]. Although these prospective cohort studies are strongly suggestive that low concentrations/activities of CETP may correlate with increased CVD, these data are entirely reductive and do not to address the clinical effect of CETP inhibition in an appropriate patient population.
Currently, we have limited and insufficient precise knowledge of the complex dynamics between plasma lipoproteins and activation of vascular cells and cell membranes to explain the apparent paradox between the prospective observational epidemiology and genome-wide analysis for the role of CEPT inhibition. To enter into a discourse on whether the disparity is due to confounding effects or reverse causality would be fatuous at this point.
HDL Complexity and the Effect of Disease on HDLs
The potential for disease status to change the structure and, hence, function of HDLs is of paramount importance to our understanding of the subsequent effects of raising HDL-C concentration. Interpretation and prediction of the impact of CETP inhibition is complicated by the growing awareness that the effects of HDL-C may be modified in different clinical settings. Human plasma high-density lipoprotein (HDL) particles constitute a spectrum of pseudo-micellar protein/lipid complexes, with hydrated densities within the range of 1.063 to 1.210 g/ml[40]. This spectrum may be further defined by five physicochemically-defined particle subpopulations determined by their buoyant density: HDL2b, 2a, 3a, 3b, and 3c. Compared with other lipoproteins, HDLs are protein-rich, with an average ratio protein:lipid of 1:1. Approximately 70 % of HDL protein mass is Apo AI, with Apo AII accounting for a further 15–20 %. Major components of the remaining 15–20 % of proteins are other amphipathic apolipoproteins (eg., ApoCI, ApoCIV, E, D, M and AIV), enzymes and lipid transfer proteins (eg paraoxonase (PON), PAF-acetlyhydrolase (PAFAH), LCAT, and CETP).
Proteomic analysis of HDLs, on the other hand, has been identifying putative mechanistic information for functional observations reported in previous decades. Recent proteomic studies have identified up to 49 proteins associated with centrifugally-isolated HDL[41–44]. Studies by Vaisar and colleagues[44], investigating both total HDL and HDL3 from normocholesterolaemic control subjects and age-matched patients with CAD, identified a role for HDLs in protease inhibition in addition to an effect on complement activation, supporting findings from ten years earlier[45]. Data from a meticulous study, in which the proteome of HDL2b, 2a, 3a, 3b, and 3c, also from normocholesterolaemic subjects, were analysed, defined 28 distinct HDL-associated proteins which associated in clusters in subpopulations[46]. In this study the investigators were able to show that ApoL-I, PON1 and PON3 correlated with the capacity of HDL3 to protect against oxidation, confirming their results through measurement of the ability of HDL3 to reduce the rate of accumulation of conjugated dienes in an LDL oxidation assay. These observations confirm earlier functional studies in which PON was shown to be one of the major proteins responsible for the anti-oxidative function of HDLs[47–49]. In a recent report of a 10-year follow up of 88 type 2 diabetic patients, the incidence of cardiovascular events increased in proportion to reduced PON1 levels and activity, suggesting that PON1 may be an independent predictor of cardiovascular events in people with diabetes[49]. Modulation of the structure and function of HDL-C has been reported, initially with regard to the anti-oxidative function of the particle[50], but also with respect to the anti-inflammatory, cholesterol transfer, and anti-thrombotic function of HDL-C[51–53].
Clinical Outcomes, so Far
The first Phase III randomised controlled trial for a member of the CETP inhibitor family (Torcetrapib: ILLUMINATE; NCT00134264) began in July 2004 comparing 15,067 patients randomised to high-intensity statin alone or high-intensity statin plus torcetrapib[54]. This study was terminated early when it became clear that the drug increased the incidence of the primary CVD endpoint, despite raising HDL-C by 70 % and lowering LDL-C by 20 %. Following analysis of the trial samples collected, the authors concluded that the effect was due to an off-target rise in the concentration of an aldosterone-like factor, which resulted in an unanticipated increase in blood pressure. However, this is not entirely consistent with the fact that CHD mortality was inversely related to a raised blood pressure and the incidence of stroke was not greater in the treatment group. A second member of the CETP inhibitors, dalcetrapib, presented an opportunity to test the HDL hypothesis as this compound raised plasma HDL-C by 30–40 % but had little or no effect on LDL-C. A Phase III randomised controlled trial (Dalcetrapib: Dal-OUTCOMES; NCT00658515), involving 15,600 patients with recent acute coronary syndrome, began in 2008 but was halted in 2012, because of a perceived lack of efficacy[55]. Anacetrapib is the most potent CETP inhibitor to date and in the first clinical trial (Anacetrapib: DEFINE; NCT00685776)[56] was shown to lower LDL-C by approximately 50 % and increase HDL-C by 140 %. Although, this gross effect may reflect an extreme disturbance of HDL-C metabolism and its consequences,the DEFINE trial did not report any significant increase in CVD in the test arm. However, this study was too small to provide robust information on the clinical events[56].
Conclusion
Although two members of the CETP inhibitor drug family have clearly been removed from the drugs cabinet, it is still a fact that we do not know if the remaining members will provide a clinical benefit for patients with CVD/CHD. The two members of this family under clinical investigation, currently in Phase III randomised control trials (Anacetrapib: REVEAL; NCT01252953 and Evacetrapib: ACCELERATE; NCT01687998), are due to report in 2016/17. Results from these highly powered, multi-centre studies, will determine the success or failure of the original hypothesis that CETP inhibition is of benefit to CVD/CHD. Any chance of addressing whether success is through raising HDL-C per se is lost following the failure of Dalcetrapib, the only member of the family that had little effect of plasma LDL-C. Efficacy of either CETP inhibitor remaining in the arena, may be due to the ability of one or other of these drugs to further reduce plasma LDL-C, rather than a benefit of raising HDL-C concentration. Should the drugs fail to give a beneficial effect, the reasons will be largely unknown, but may relate to the altered kinetic of the dynamic effects that increase the circulating half-life and hence complexity of the HDL particles. The results of these studies are anticipated with gathering interest, and an additional benefit will be that they will provide an important opportunity to gain a further understanding of HDL metabolism/catabolism in disease, which will be invaluable in progressing with clinical development of these compounds.
References
- 1.Gordon T, Castelli WP, Hjortland MC et al. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. 1977;62:707–14. doi: 10.1016/0002-9343(77)90874-9. [DOI] [PubMed] [Google Scholar]
- 2.Baigent C, Keech A, Kearney PM et al. Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–78. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 3.LaRosa JC, He J, Vupputuri S. Effect of statins on risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA. 1999;282:2340–6. doi: 10.1001/jama.282.24.2340. [DOI] [PubMed] [Google Scholar]
- 4.Castelli WP, Doyle JT, Gordon T et al. HDL cholesterol and other lipids in coronary heart disease. The cooperative lipoprotein phenotyping study. Circulation. 1977;55:767–72. doi: 10.1161/01.cir.55.5.767. [DOI] [PubMed] [Google Scholar]
- 5.Castelli WP, Anderson K, Wilson PW et al. Lipids and risk of coronary heart disease. The Framingham Study. Ann Epidemiol. 1992;2:23–8. doi: 10.1016/1047-2797(92)90033-m. [DOI] [PubMed] [Google Scholar]
- 6.Sharrett AR, Ballantyne CM, Coady SA et al. Atherosclerosis Risk in Communities Study Group. Coronary heart disease prediction from lipoprotein cholesterol levels, triglycerides, lipoprotein(a), apolipoproteins A-I and B, and HDL density subfractions: The Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2001;104:1108–13. doi: 10.1161/hc3501.095214. [DOI] [PubMed] [Google Scholar]
- 7.Badimon JJ, Badimon L, Galvez A et al. High density lipoprotein plasma fractions inhibit aortic fatty streaks in cholesterol-fed rabbits. Lab Invest. 1989;60:455–61. [PubMed] [Google Scholar]
- 8.Plump AS, Scott CJ, Breslow JL. Human apolipoprotein A-I gene expression increases high-density lipoprotein and suppresses atherosclerosis in the apolipoprotein E-deficient mouse. Proc Natl Acad Sci U S A. 1994;91:9607–11. doi: 10.1073/pnas.91.20.9607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubin EM, Krauss RM, Spangler EA et al. Inhibition of early atherogenesis in transgenic mice by human apolipoprotein AI. Nature. 1991;353:265–7. doi: 10.1038/353265a0. [DOI] [PubMed] [Google Scholar]
- 10.Huttunen JK, Länsimies E, Voutilainen E et al. Effect of moderate physical exercise on serum lipoproteins. A controlled clinical trial with special reference to serum high-density lipoproteins. Circulation. 1979;60:1220–9. doi: 10.1161/01.cir.60.6.1220. [DOI] [PubMed] [Google Scholar]
- 11.Kelley GA, Kelley KS, Roberts S et al. Efficacy of aerobic exercise and a prudent diet for improving selected lipids and lipoproteins in adults: a meta-analysis of randomised controlled trials. BMC Med. 2011;9:74. doi: 10.1186/1741-7015-9-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moffatt RJ, Chelland SA, Pecott DL et al. Acute exposure to environmental tobacco smoke reduces HDL-C and HDL2-C. Prev Med. 2004;38:637–41. doi: 10.1016/j.ypmed.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Contaldo F, Strazzullo P, Postiglione A et al. Plasma high-density lipoprotein in severe obesity after stable weight loss. Atherosclerosis. 1980;37:163–7. doi: 10.1016/0021-9150(80)90001-5. [DOI] [PubMed] [Google Scholar]
- 14.Boekholdt SM, Arsenault BJ, Hovingh GK et al. Levels and changes of HDL cholesterol and apolipoprotein A-I in relation to risk of cardiovascular events among statin-treated patients: a meta-analysis. Circulation. 2013;128:1504–12. doi: 10.1161/CIRCULATIONAHA.113.002670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kesäniemi YA, Grundy SM. Influence of gemfibrozil and clofibrate on metabolism of cholesterol and plasma triglycerides in man. JAMA. 1984;251:2241–6. doi: 10.1001/jama.1984.03340410049031. [DOI] [PubMed] [Google Scholar]
- 16.Naoumova RP, Kindler H, Leccisotti L et al. Pioglitazone improves myocardial blood flow and glucose utilisation in non-diabetic patients with combined hyperlipidaemia: a randomised, double-blind, placebo-controlled study. J Am Coll Cardiol. 2007;50:2051–8. doi: 10.1016/j.jacc.2007.07.070. [DOI] [PubMed] [Google Scholar]
- 17.Boden WE, Probstfield JL, Anderson T et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365:2255–67. doi: 10.1056/NEJMoa1107579. AIM-HIGH Investigators. [DOI] [PubMed] [Google Scholar]
- 18.Landray MJ, Haynes R, Hopewell JC et al. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371:203–12. doi: 10.1056/NEJMoa1300955. HPS2-THRIVE Collaborative Group. [DOI] [PubMed] [Google Scholar]
- 19.Fielding CJ, Fielding PE. Molecular physiology of reverse cholesterol transport. J Lipid Res. 1995;36:211–28. [PubMed] [Google Scholar]
- 20.Hennessy LK, Kunitake ST, Kane JP. Apolipoprotein A-I-containing lipoproteins, with or without apolipoprotein A-II, as progenitors of pre-beta high-density lipoprotein particles. Biochemistry. 1993;32:5759–65. doi: 10.1021/bi00073a006. [DOI] [PubMed] [Google Scholar]
- 21.Marotti KR, Castle CK, Boyle TP et al. Severe atherosclerosis in transgenic mice expressing simian cholesteryl ester transfer protein. Nature. 1993;364:73–5. doi: 10.1038/364073a0. [DOI] [PubMed] [Google Scholar]
- 22.Okamoto H, Yonemori F, Wakitani K et al. A cholesteryl ester transfer protein inhibitor attenuates atherosclerosis in rabbits. Nature. 2000;406:203–7. doi: 10.1038/35018119. [DOI] [PubMed] [Google Scholar]
- 23.Sugano M, Makino N, Sawada S et al. Effects of antisense oligonucleotides against cholesteryl ester transfer protein on the development of atherosclerosis in cholesterol-fed rabbits. J Biol Chem. 1998;273:5033–36. doi: 10.1074/jbc.273.9.5033. [DOI] [PubMed] [Google Scholar]
- 24.Ritterhaus CW, Miller DP, Thomas LJ et al. Vaccine-induced antibodies inhibit CETP activity in vivo and reduce aortic lesions in a rabbit model of atherosclerosis. Arterioscler Thromb Vasc Biol. 2000;20:2106–12. doi: 10.1161/01.atv.20.9.2106. [DOI] [PubMed] [Google Scholar]
- 25.Hayek T, Masucci-Magoulas L, Jiang X et al. Decreased early atherosclerotic lesions in hypertriglyceridemic mice expressing cholesteryl ester transfer protein transgene. J Clin Invest. 1995;96:2071–74. doi: 10.1172/JCI118255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Föger B, Chase M, Amar MJ et al. Cholesteryl ester transfer protein corrects dysfunctional high-density lipoproteins and reduces aortic atherosclerosis in lecithin cholesterol acyltransferase transgenic mice. J Biol Chem. 1999;274:36912–20. doi: 10.1074/jbc.274.52.36912. [DOI] [PubMed] [Google Scholar]
- 27.Brousseau ME, Diffenderfer MR, Millar JS et al. Effects of cholesteryl ester transfer protein inhibition on high-density lipoprotein subspecies, apolipoprotein A-I metabolism and fecal sterol excretion. Arterioscler Thromb Vasc Biol. 2005;25:1057–64. doi: 10.1161/01.ATV.0000161928.16334.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Voight BF, Peloso GM, Orho-Melander M et al. Plasma HDL cholesterol and risk of myocardial infarction: a Mendelian randomisation study. Lancet. 2012;380:572–80. doi: 10.1016/S0140-6736(12)60312-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thompson A, Di Angelantonio E, Sarwar N et al. Association of cholesteryl ester transfer protein genotypes with CETP mass and activity, lipid levels and coronary risk. JAMA. 2008;299:2777–88. doi: 10.1001/jama.299.23.2777. [DOI] [PubMed] [Google Scholar]
- 30.Li YY, Wu XY, Xu J et al. Apo A5-1131T/C, FgB-455G/A, -148C/T, and CETP TaqIB gene polymorphisms and coronary artery disease in the Chinese population; a meta-analysis of 15,055 subjects. Mol Biol Rep. 2013;40:1997–2014. doi: 10.1007/s11033-012-2257-9. [DOI] [PubMed] [Google Scholar]
- 31.Ridker PM, Paré G, Parker AN et al. Polymorphism in the CETP gene region, HDL cholesterol, and risk of future myocardial infarction: Genomewide analysis among 18,245 initially healthy women from the Women’s Genome Health Study. Circ Cardiovasc Genet. 2009;2:26–33. doi: 10.1161/CIRCGENETICS.108.817304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ritsch A, Auer BM, Föger B et al. Polyclonal antibody-based immunoradiometric assay for quantitation of cholesteryl ester transfer protein. J Lipid Res. 1993;34:673–9. [PubMed] [Google Scholar]
- 33.Marschang P, Sandhofer A, Ritsch A et al. Plasma cholesteryl ester transfer protein concentrations predict cardiovascular events in patients with coronary artery disease treated with pravastatin. J Intern Med. 2006;260:151–9. doi: 10.1111/j.1365-2796.2006.01674.x. [DOI] [PubMed] [Google Scholar]
- 34.Vasan RS, Pencina MJ, Robins SJ et al. Association of circulating cholesteryl ester transfer protein activity with incidence of cardiovascular disease in the community. Circulation. 2009;120:2414–20. doi: 10.1161/CIRCULATIONAHA.109.872705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khera AV, Wolfe ML, Cannon CP et al. On-statin cholesteryl ester transfer protein mass and risk of recurrent coronary events (from the pravastatin or atorvastatin evaluation and infection therapy-thrombolysis in myocardial infarction 22 [PROVE IT-TIMI 22] study). Am J Cardiol. 2010;106:451–6. doi: 10.1016/j.amjcard.2010.03.057. [DOI] [PubMed] [Google Scholar]
- 36.Duwensee K, Breitling LP, Tancevski I et al. Cholesteryl ester transfer protein in patients with coronary heart disease. Eur J Clin Invest. 2010;40:616–22. doi: 10.1111/j.1365-2362.2010.02313.x. [DOI] [PubMed] [Google Scholar]
- 37.Ritsch A, Scharnagl H, Eller P et al. Cholesteryl ester transfer protein and mortality in patients undergoing coronary angiography: the Ludwigshafen Risk and Cardiovascular Health Study. Circulation. 2010;121:366–74. doi: 10.1161/CIRCULATIONAHA.109.875013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Robins SJ, Lyass A, Brocia RW et al. Plasma lipid transfer proteins and cardiovascular disease. The Framingham Heart Study. Atherosclerosis. 2013;228:230–6. doi: 10.1016/j.atherosclerosis.2013.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McNeal CJ, Chatterjee S, Hou J et al. Human HDL containing a novel apoC-I isoform induces smooth muscle cell apoptosis. Cardiovasc Res. 2013;98:83–93. doi: 10.1093/cvr/cvt014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Havel RJ, Eder HA, Bragdon JH. The distribution and chemical composition of ultracentrifugally separated lipoproteins in human serum. J Clin Invest. 1955;34:1345–53. doi: 10.1172/JCI103182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karlsson H, Leanderson P, Tagesson C et al. Lipoproteomics II: mapping of proteins in high-density lipoprotein using two-dimentional gel electrophoresis and mass spectrometry. Proteomics. 2005;5:1431–45. doi: 10.1002/pmic.200401010. [DOI] [PubMed] [Google Scholar]
- 42.Heller M, Stalder D, Schlappritzi E et al. Mass spectrometry-based analytical tools for the molecular protein characterisation of human plasma lipoproteins. Proteomics. 2005;5:2619–30. doi: 10.1002/pmic.200401233. [DOI] [PubMed] [Google Scholar]
- 43.Rezaee F, Casetta B, Levels JH et al. Proteomic analysis of high-density lipoprotein. Proteomics. 2006;6:721–30. doi: 10.1002/pmic.200500191. [DOI] [PubMed] [Google Scholar]
- 44.Vaisar T, Pennathur S, Green PS et al. Shotgun proteomics implicates protease inhibition and complement activation in the anti-inflammatory properties of HDL. J Clin Invest. 2007;117:746–56. doi: 10.1172/JCI26206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rosenfeld SI, Packman CH, Leddy JP. Inhibition of the lytic action of cell-bound terminal complement components by human high-density lipoproteins and apoproteins. J Clin Invest. 1983;71:795–808. doi: 10.1172/JCI110833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davidson WS, Silva GA, Chantepie S et al. Proteomic analysis of defined HDL subpopulations reveals particle-specific protein clusters: relevance to antioxidative function. Arterioscler Thromb Vasc Biol. 2009;29:870–6. doi: 10.1161/ATVBAHA.109.186031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mackness MI, Durrington PN, Mackness B. How high-density lipoprotein protects against the effects of lipid peroxidation. Curr Opin Lipidol. 2000. pp. 383–8. [DOI] [PubMed]
- 48.Laplaud PM, Dantoine T, Chapman MJ. Paraoxonase as a risk marker for cardiovascular disease: facts and hypotheses. Clin Chem Lab Med. 1998;36:431–41. doi: 10.1515/CCLM.1998.073. [DOI] [PubMed] [Google Scholar]
- 49.Ikeda Y, Inoue M, Suehiro T et al. Low human paraoxonase predicts cardiovascular events in a Japanese patients with type 2 diabetes. Acta Diabetol. 2009;46:239–42. doi: 10.1007/s00592-008-0066-3. [DOI] [PubMed] [Google Scholar]
- 50.Van Lenten BJ, Reddy ST, Navab M et al. Understanding changes in high-density lipoproteins during the acute phase response. Arterioscler Thromb Vasc Biol. 2006;26:1687–8. doi: 10.1161/01.ATV.0000232522.47018.a6. [DOI] [PubMed] [Google Scholar]
- 51.Riwanto M, Landmesser U. High density lipoproteins and endothelial functions: mechanistic insights and alterations in cardiovascular disease. J Lipid Res. 2013;54:3227–43. doi: 10.1194/jlr.R037762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bergt C, Pennathur S, Fu X et al. The myeloperoxidase product hypochlorous acid oxidises HDL in the human artery wall and impairs ABCA1-dependent cholesterol transport. Proc Natl Acad Sci U S A. 2004;101:13032–7. doi: 10.1073/pnas.0405292101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morgantini C, Natali A, Boldrini B et al. Anti-inflammatory and antioxidant properties of HDLs are impaired in type 2 diabetes. Diabetes. 2011;60:2617–23. doi: 10.2337/db11-0378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Barter PJ, Caulfield M, Eriksson M et al. ILLUMINATE Investigators. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357:2109–22. doi: 10.1056/NEJMoa0706628. [DOI] [PubMed] [Google Scholar]
- 55.Schwartz GG, Olsson AG, Abt M et al. Effects of dalcetrapib in patients with a recent acute coronary sydrome. N Eng J Med. 2012;367:2089–99. doi: 10.1056/NEJMoa1206797. [DOI] [PubMed] [Google Scholar]
- 56.Cannon CP, Shah S, Dansky HM et al. Determining the Efficacy and Tolerability Investigators. Safety of anacetrapib in patients with or at high risk for coronary heart disease. N Engl J Med. 2010;363:2406–15. doi: 10.1056/NEJMoa1009744. [DOI] [PubMed] [Google Scholar]


