Abstract
Background
The Lever sign has gained recent notoriety for its purported anterior cruciate ligament (ACL) diagnostics and simplicity of performance.
Purpose
The purpose of this systematic review with meta-analysis is to summarize the diagnostic accuracy of the Lever sign for use during assessment of the knee for an ACL tear in subjects with suspected acute and chronic knee injury.
Study Design
Systematic review with meta-analysis
Methods
A computer-assisted literature search of MEDLINE, CINAHL, and EMBASE databases using keywords related to diagnostic accuracy of the knee joint. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used for the search and reporting phases of the study. Quality assessment of bias and applicability was conducted using the Quality of Diagnostic Accuracy Studies (QUADAS). Mixed effects models were used to summarize accuracy.
Results
Eight articles, with only two demonstrating high quality, were included. Six of the articles were included in a meta-analysis. Diagnostic values, utilizing arthroscopy as a gold standard, were: pooled SN 0.55 (95% CI 0.22 to 0.84), pooled SP 0.89 (95% CI 0.44 to 0.99), positive likelihood ratio (+LR) 9.2 (95% CI 0.70 to 46.1), negative likelihood ratio (-LR) 0.58 (95% CI 0.18 to 1.28). Post-test probability with a positive finding (57% sampling prevalence) reached 92% (95% CI 83 to 97%). Post-test probability with a negative finding (57% sampling prevalence) reached 43% (95% CI 39 to 47%).
Conclusions
Based on limited evidence of heterogeneous methodological quality, the Lever sign can moderately change post-test probability to rule in an ACL tear. These results should be interpreted cautiously due to a limited number of studies, with small sample sizes and study quality affecting test accuracy. Future investigation should be expanded to include additional high-quality studies examining diverse clinical contexts, as they become available, to enable a more comprehensive clinical examination of this test.
Level of evidence
3a
PROSPERO Registration # CRD42018084954
Keywords: anterior cruciate ligament, diagnostic accuracy, Lever Sign, knee, sensitivity, specificity
INTRODUCTION
A tear of the anterior cruciate ligament (ACL) is a significant knee injury which can leave patients with sustained complaints of instability in daily and sporting activities as well as increasing their risk of knee osteoarthritis later in life.1,2 Current best practices for the management of symptoms in young adults propose early rehabilitation or surgery.3 Thus, there is a need for an accurate initial diagnosis based on history and physical examination, although this may be difficult to achieve.4
Diagnostic accuracy of physical examination tests for ACL tear has been extensively studied.5 The three most studied tests, the Lachman, the pivot shift and the anterior drawer test have shown overall adequate accuracy for clinical use.5-8 However, these tests also yielded lower accuracy when utilized acutely post injury compared to a chronic tear,8 when the knee has a combined lesion to the meniscus instead of an isolated ACL tear, and when the tear is partial compared to complete.5-8 Moreover, inter-rater reliability of these tests may be lower when executed by non-expert clinicians because of technical difficulties and interpretation of the outcomes.9,10
In response to these limitations, Lelli et al. proposed a new physical examination test to diagnose ACL tear called the Lever sign.11 This test requires the evaluator to place his or her fist under the calf muscle to create a “fulcrum” extending the knee while applying a moderate downward force to the distal part of the femur.11 In an intact knee, the ACL completes a lever mechanism, making the heel rise in response to the force applied to the femur.11 In an ACL-deficient knee, the heel does not rise indicating a positive Lever sign.11 In their initial study, the authors demonstrated a perfect sensitivity and specificity in a sample of acute and chronic patients with both partial and complete ACL tears.11
Several years following its introduction, this test is rapidly gaining the interest of clinicians due to its simplicity. Yet, none of the recent systematic reviews examining accuracy for ACL clinical tests have included this test to verify if subsequent studies supported the initial claims.5,8 Therefore, the purpose of this systematic review with meta-analysis is to summarize the diagnostic accuracy of the Lever sign for use during assessment of the knee for an ACL tear ACL tear in subjects with suspected acute and chronic knee injury.
METHODS
Registration
The study was registered with the International Prospective Register of Systematic Reviews (PROSPERO#CRD42018084954) on January 15, 2018. PROSPERO is a database of prospectively registered systematic reviews for health and social topics. The study was registered after the pilot search and prior to updated data search and extraction.
Data Sources
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were utilized during the search and reporting phase of this review. The PRISMA statement includes a 27-item checklist that is designed to be used as a basis for reporting systematic reviews of randomized trials,12 but the checklist can also be applied to multiple forms of research methodologies.13
A computer-assisted literature search of MEDLINE, CINAHL, and EMBASE databases was performed from inception of each respective database to December 23, 2017, and updated on April 2, 2018. The goal was to optimize the sensitivity of the search strategy,14,15 increasing the likelihood that all appropriate studies were identified. The search strategy was developed in collaboration with a medical information specialist and used controlled vocabulary and key words related to diagnostic accuracy of the lever test relative to ACL tear. Screening filters were initially used during assessment of title, abstract and full text documents. The search was further limited to humans and English or French-only publications. The search strategy for MEDLINE is provided in Appendix 1.
Selection criteria
Articles were eligible if they met all of the following criteria: 1) it included participants with suspected ACL tear/injury, 2) it included the Lever sign test to diagnose ACL tear/injury, 3) it utilized an acceptable reference standard, 4) it reported diagnostic values in sufficient detail to allow reconstruction of contingency tables, and 5) it was written in English or French.
An article was excluded if: 1) the pathology assessed was associated with a condition not located at the knee joint, 2) the study did not evaluate the Lever sign test, 3) the study did not provide sufficient detail to calculate diagnostic accuracy, 4) the clinical tests were performed on cadavers, 5) the study reported on specialized instrumentation, questionnaires or performance measures, or 6) the study was performed on infants/toddlers.
Study selection
Two reviewers (MPR, CKR) independently performed the search. Because computerized search results for diagnostic accuracy data frequently omit many relevant articles,16 the reference lists of all selected publications were checked to retrieve relevant publications that were not identified in the computerized search. Unpublished literature was also hand searched and included publications, posters, abstracts, or conference proceedings. To identify relevant articles, titles and abstracts of all identified citations were independently screened. Full-text articles were retrieved if the abstract provided insufficient information to establish eligibility or if the article passed the first eligibility screening.
All criteria were independently applied by two reviewers (MPR, CKR) to the full text of the articles that passed the first eligibility screening. Disagreements among the reviewers were discussed and resolved by consensus. Articles to be included (for meta-analysis) were determined by using clinical and statistical judgment of study heterogeneity. Clinical judgment criteria involved assessment of similarity of populations, assessment context (e.g., test performed a priori), reference standard (e.g. MRI or arthroscopy), and method in which specific tests were applied.17 In addition, after approval using clinical judgment, studies were statistically pooled for meta-analysis when ≥ 2 studies examined the Lever sign test and diagnosis with the same reference standard.
Risk of Bias/Quality Assessment
The Quality Assessment of Diagnostic Accuracy Studies tool (QUADAS), the original tool for quality assessment in diagnostic accuracy studies, was used to analyze the quality of the study. QUADAS consists of 14 items with each having a “yes”/”no”/”unclear” answer options. A “yes” score indicated sufficient information, with bias considered unlikely. A “no” score indicated sufficient information, but with potential bias from inadequate design or conduct. An “unclear” score indicated that insufficient information was provided in the article or the methodology was unclear. The total score is formed by the count of all of the criteria scored “yes”, valued as “1” whereas, “no” and “unclear” scores carried a zero score value. If a “yes” score was present for all 14 items, the maximum attainable unweighted score is 14/14. The methodological quality and risk of bias of each of the studies was independently assessed by two reviewers (MPR, SD). Disagreements among the reviewers were discussed and resolved with consensus. Inter-rater reliability was calculated with weighted Kappa.
Qualitatively, studies that exhibit higher QUADAS values are associated with less risk of design bias than those of lower values. Studies were stratified as “high quality/low risk of bias” if the QUADAS score was ≥10/14, and “low quality/high risk of bias” of the study score < 10/14. This dichotomizing stratification level was chosen since it has been utilized successfully previously and no other strategy is advocated to discriminate low and high bias diagnostic accuracy studies.18-23
Data extraction and analysis
One reviewer (MPR) independently extracted information and data regarding study population, setting, examiner, duration of symptoms, mechanism of injury, test performance, diagnostic reference-standard, and number of true positives, false positives, false negatives, and true negatives for calculation of sensitivity (SN), specificity (SP), positive likelihood ratios (+LR), and negative likelihood ratios (-LR) when not provided. Extracted data was verified by the other study authors (CKR, SD).
It has been suggested that post-test probability can be altered to a minimal degree with +LRs of 1 to 2 or -LRs of 0.5 to1, to a small degree with +LRs of 2 to 5 or -LRs of 0.2 to 0.5, to a moderate degree with +LRs of 5 to 10 and -LRs of 0.1 to 0.2) and to a large and almost conclusive degree with +LRs greater than 10 and -LRs less than 0.1.24 Pretest probability is defined as the probability of the target pathology before a diagnostic test result is known. It represents the probability that a specific patient, with a specific past history, presenting to a specific clinical setting, with a specific symptom complex, has a specific pathology.24
STATISTICAL METHODS
Meta-Analysis
Der-Simionian and Laird25 mixed effects models, which incorporate both between and within study heterogeneity, were used to produce summary estimates of SN, SP, LR+, LR-, PPV, and NPV. An I-squared value of > 50% and Cochrane's-Q p-value of < 0.10 were the criteria to indicate significant between-study heterogeneity, of SN and SP and likelihood ratios respectfully. Publication bias was not formally tested due to low power of the tests with limited included studies.26 All analyses were conducted in R version 3.4.2 (package: mada, http://cran.r-project.org/).
RESULTS
Selection of Studies
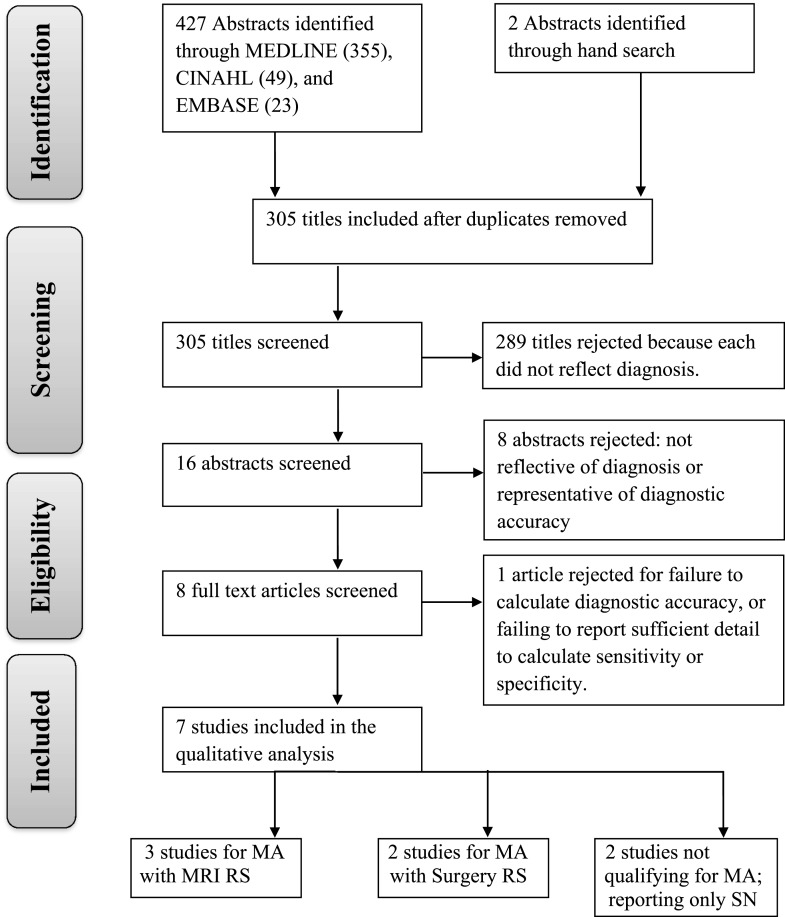
The systematic searches of MEDLINE, CINAHL, and EMBASE, as well as hand search, netted 305 abstracts after duplicates were removed. Abstract and full text review reduced the acceptable papers to eight11,27-33 (Figure 1 and Table 1). Abstract screening inter-rater agreement was κ=0.80 (95% CI: 0.60 to 0.94) and full text agreement was κ=0.92 (95% CI: 0.85 to 0.99); both indicating almost perfect agreement. The search strategy utilized for MEDLINE is listed in Appendix I. Excluded studies are listed in Appendix II.
Figure 1.
Flow diagram for study.
TABLE 1.
Demographics and risk of bias in included studies.
| Study | Level of Evidence | Study Design | Risk of Bias (QUADAS) | Subjects; Gender; Mean Age; Duration of Symptoms | Mechanism of Injury |
|---|---|---|---|---|---|
| Chong et al. (2017)27 | III | Cohort study | High | 33 patients diagnosed with ACL injury at least 72 hours prior to examination Females (n=12) Mean age: 30.6 ± 17.0 (15–60) years (females) 30.9 ± 14.3 (11–62) years (males) Injury onset: knee injury was not sustained within 72 hours prior to data collection |
NR |
| Deveci et al. (2015)28 | IV | Cohort study | High | 117 patients diagnosed with ACL tear based on symptoms, physical exam and (+) 1.5T MRI Females (n=21) Mean age: 25.8 ± 5.9 (17–45) years Injury onset: 8.7 (4–25) weeks |
NR |
| Jarbo et al. (2017)29 | II | Cohort study (diagnosis) | Low | 102 patients with acute (≤4 weeks) symptomatic knees Females (n=44) Mean age: 23 years Injury onset: within 4 weeks of their injury or the onset of symptoms |
NR |
| Lichtenberg et al. (2018)33 | II | Cohort study (diagnosis) | High | 94 patients with trauma to the knee. Patients with locking knee complaints or previous ACL were excluded. Females (n=37) Mean age: 34 ± 15 years Injury onset: ranging from acute ( < 3 weeks) to chronic ( > 12 weeks) |
Trauma to the knee |
| Lelli et al. (2014)11 | IV | Cohort study | High | 400 patients Group A (acute injury, (+) MRI for complete ACL rupture); 29 females; 27 years Group B (chronic injury, (+) MRI for complete ACL rupture); 35 females; 26 years Group C (acute injury with (+) MRI for partial ACL rupture); 24 females; 26.8 years Group D (chronic injury with (+) MRI for partial ACL rupture; 31 females; 25.9 years Mean age: 26.4 ± 14.9 years Injury Onset:
|
NR |
| Massey et al. (2017)31 | II | Cohort study | Low | 91 patients after a knee injury with subjective swelling, or an objective effusion 30 females Mean age: 28 ± 11 years Injury onset: NR |
Noncontact or contact knee injury |
| Mulligan et al. (2017)30 | III | Cohort study | High | 60 patients with complaint of knee pain (<7/10) 22 females Mean age: 42 ± 13.4 (18-65) years Injury onset: 55 ± 80 (1-304) days |
NR |
| Thapa et al. (2015)32 | II | Cohort study | High | 80 patients with complaints of knee symptoms of giving way/locking/pain 30 females Mean age: 32.12 (21-42) years Injury onset: NR |
Sports activities (62.8%) |
NR, not reported; QUADAS, Quality Assessment of Diagnostic Accuracy Studies scores; studies were stratified as “high quality/low risk of bias” if the QUADAS score was ≥10/14, and “low quality/high risk of bias” of the study score < 10/14.
This review included 977 subjects across the eight studies (Tables 1 & 2).11,27-33 The sample size of the studies ranged from 3327 to 400 subjects (Table 1).31 All studies were prospective in study design (Table 1). Sources of support and conflicts of interest reporting is detailed in Appendix III.
Table 2.
Characteristics of included studies.
| Study | Subjects (n) | Reference Standard | Examiners | Examination Setting | Examiner Reliability |
|---|---|---|---|---|---|
| Chong et al. (2017)27 | 33 | Arthroscopy | Experienced sports medicine orthopaedic surgeon & Experienced orthopaedic physician assistant |
Both under anaesthesia and without anaesthesia during arthroscopy |
Inter-rater Pre-anesthesia 0.30 κ; 82% agreement Post-anesthesia NA κ; 97% agreement Intra-rater 0.05 κ; 85% agreement (OS); NA κ; 67% agreement (PA) |
| Deveci et al. (2015)28 | 117 | Arthroscopy | Two orthopedic surgeons | Both under anaesthesia and without anaesthesia during arthroscopy |
0.89 to 0.96 ICC (inter-rater) |
| Jarbo et al. (2017)29 | 102 | MRI RS (n=48) Surgical GS (n=54) |
Randomly assigned undergraduate student, medical student, orthopaedic resident, or orthopaedic fellow |
Initial clinic visit (for nonsurgical patients) or under anesthesia in the operating room (for surgical patients) |
NR |
| Lichtenberg et al. (2018)33 | 94 | Arthroscopy | Orthopedic surgeon and physiotherapist |
University medical center outpatient clinic |
Inter-rater 0.82 κ; (OS and PT) |
| Lelli et al. (2014)11 | 400 | MRI | Single clinician | Surgical clinic | NR |
| Massey et al. (2017)31 | 91 | 1.5 T MRI | 2 board-certified orthopaedic surgeons |
Surgical clinic, with patient awake |
NR |
| Mulligan et al. (2017)30 | 60 | RS (n=41) Clinical test cluster |
Licensed physical | Hospital clinical setting | NR |
| GS (n=19) Surgery | Therapist with 36 years of sports physical therapy experience | ||||
| Thapa et al. (2015)32 | 80 | Arthroscopy | NR | Sports clinic in department of orthopedics |
NR |
MRI=magnetic resonance imaging, RS=reference standard, GS=gold standard, NR=not reported, n=number, T=Tesla, κ=kappa, OS=orthopaedic surgeon, PA=physician assistant, PT=physiotherapist, ICC=intraclass correlation
Quality Scores
Inter-rater agreement was κ=0.62 (95% CI: 0.48 to 0.78), indicating substantial agreement. Table 1 provides the overall risk of bias score, with two studies29,31 demonstrating low risk of bias. Details of each the individual study quality scores are presented in Appendix IV.
Study Characteristics
Detail on subject sex, mean age, duration of symptoms, and mechanism of injury are listed in Table 1. The clinicians performing the examination and the setting in which the examination was performed are listed in Table 2. The reference standards utilized, as well as the professional training of the clinicians performing the Lever sign are also listed in Table 2.
META-ANALYSIS
Six studies11,29-33 qualified for meta-analysis (Tables 1-3). Three studies (n=234 subjects) utilized arthroscopy as a gold standard in surgical candidates,30,32,33 while three studies (n=539 subjects) utilized MRI as a reference standard.11,29,31
TABLE 3.
Pooled diagnostic properties for the diagnosis of Lever sign for ACL tear/injury.
| # studies (sample size) | SN (95% CI) | SP (95% CI) | +LR (95% CI) | -LR (95% CI) | Post-Test Change for (+) Result | Post-Test Change for (-) Result | |
|---|---|---|---|---|---|---|---|
| Surgery | 330,32,33 (n=234) |
0.55 (0.22, 0.84) |
0.89 (0.44, 0.99) |
9.2 (0.70, 46.1) |
0.58 (0.18, 1.28) |
Pretest=57% Posttest=92% |
Pretest=57% Posttest=43% |
| MRI (High quality studies only) | 229,31 (n=139) |
0.77 (0.55, 0.90) |
0.91 (0.55, 0.99) |
13.1 (1.9, 52.4) |
0.28 (0.14, 0.46) |
Pretest=54% Posttest=94% |
Pretest=54% Posttest=25% |
| MRI (all studies) | 311,29,31 (n=539) |
0.95 (0.34, 1.0) |
0.97 (0.58, 1.0) |
128 (0.97, 832.0) |
0.18 (0.00, 1.0) |
Pretest=70% Posttest=100% |
Pretest=70% Posttest=30% |
DerSimoninian-Laird mixed-effects models used throughout. SN=sensitivity, SP=specificity, + LR=positive likelihood ratio, -LR=negative likelihood ratio, (+)=positive, (-)=negative, PPV=positive predictive value, NPV=negative predictive value, CI=confidence interval, MRI=magnetic resonance imaging, n=number
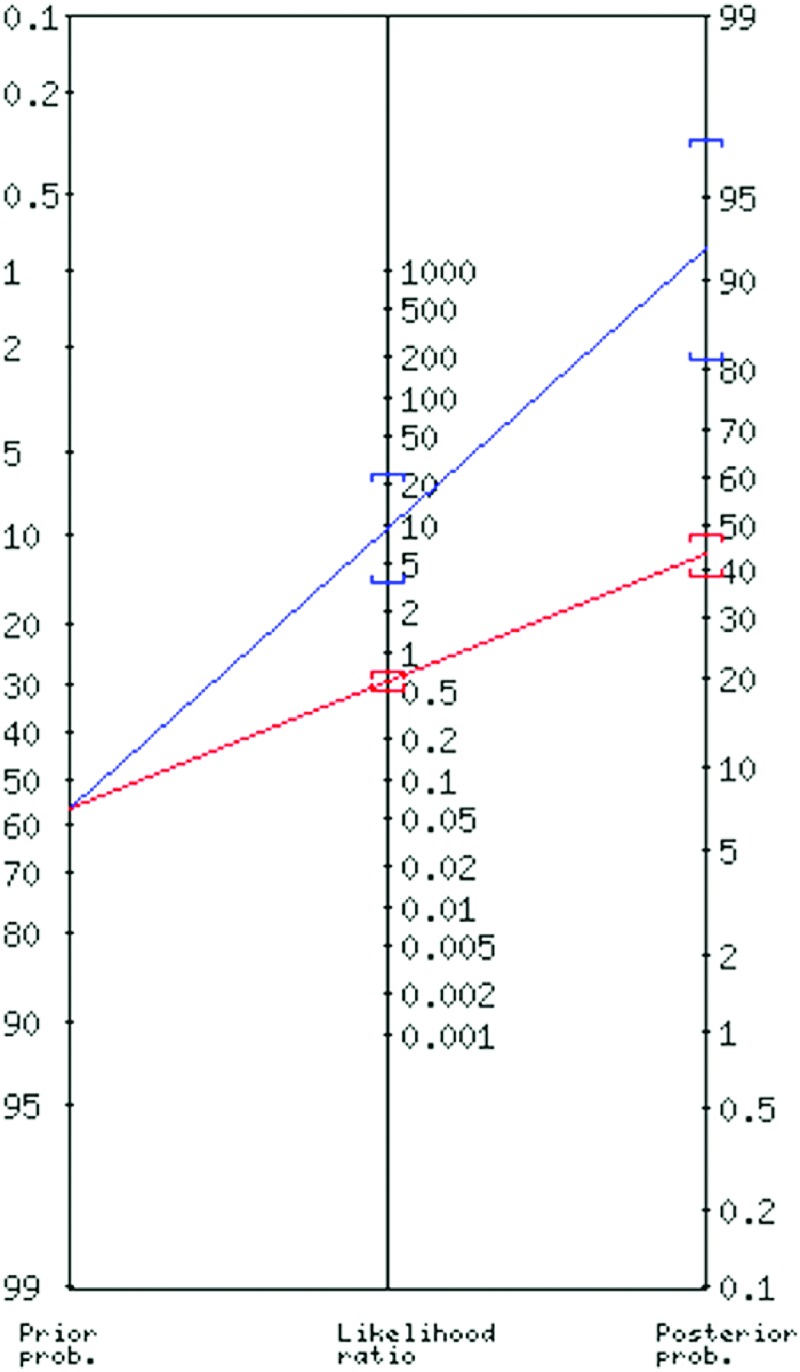
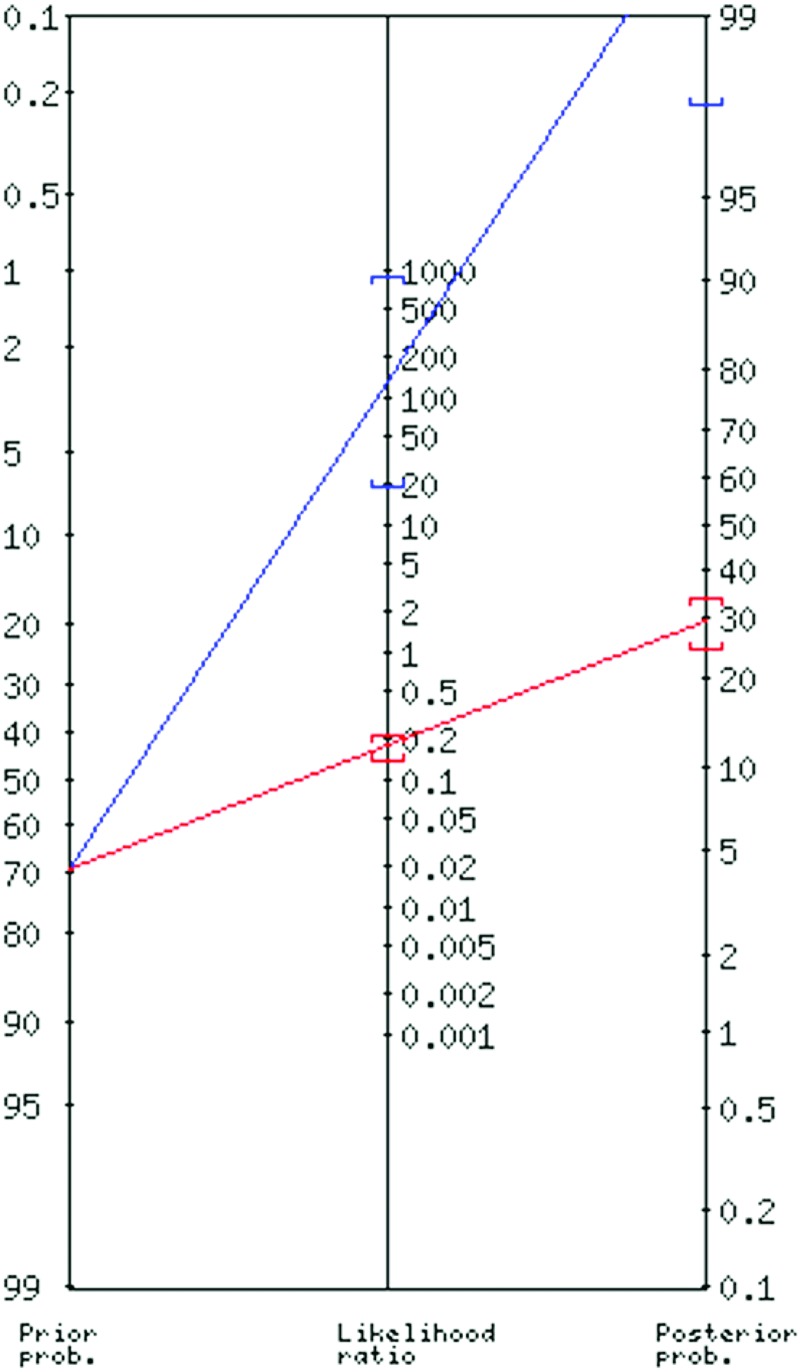
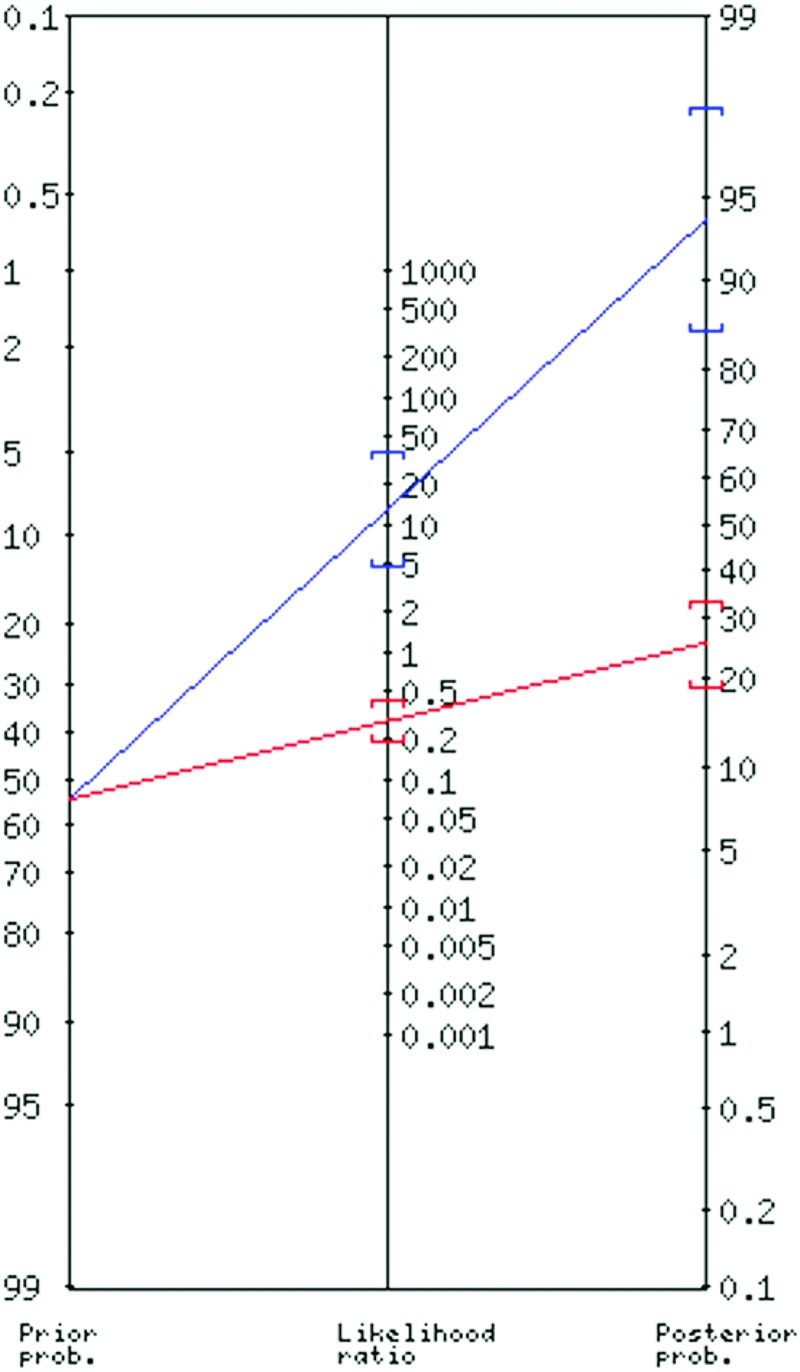
Figures 2 through 4 illustrate pre- to post-test probability changes utilizing the Lever sign with arthroscopy and MRI reference standards, respectively. Diagnostic accuracy and probability shifts were calculated utilizing MRI as a reference standard with high quality/low risk of bias studies29,31 only (Figure 2) and with all studies11,29,31 (one additional study was low quality/high risk of bias). Pre- to post-test probability for positive and negative findings on the Lever sign are presented in Table 3. As shown in this table, the adding of one high risk of bias study11 substantially change the estimates.
Figure 2.
Pre- to post-test probability shifts for Lever sign with arthroscopy gold standard (pooled analysis). Blue line represents positive and red line represents negative probability shifts.
Figure 4.
Pre- to post-test probability shifts for Lever sign with MRI reference standard (low and high risk of bias studies included in pooled analysis). Blue line represents positive and red line represents negative probability shifts.
Figure 3.
Pre- to post-test probability shifts for Lever sign with MRI reference standard (only low risk of bias studies in pooled analysis). Blue line represents positive and red line represents negative probability shifts.
RESULTS OF INDIVIDUAL DIAGNOSTIC STUDIES
One study29 utilized arthroscopy as a gold standard, but did not qualify for meta-analysis as the subjects were examined under anesthesia, unlike the other two studies.17,20 The prevalence of ACL tear in this study with this gold standard was 54%. Post-test probability with a positive finding was 86%, while a post-test probability with a negative finding was 16%.
Three studies11,27,28 examining those with ACL tear/injury reported only SN (Table 4). Two studies27,28 utilized arthroscopy as a reference standard, and both examined the Lever sign pre- and post-anesthesia. Chong et al.27 found a SN range of 0.82 (physician assistant examiner) to 0.88 (orthopaedic surgeon examiner) pre- and 0.97 (orthopaedic surgeon) to 1.0 (physician assistant) post-anesthesia in a group of 33 subjects with ACL tear of at least 72 hours prior to examination. Deveci et al.32 demonstrated a SN of 0.94 pre- and 0.98 post-anesthesia in a group of 117 subjects with ACL tear of a mean of 8.7 (4 to 25 weeks) from onset of injury.
Table 4.
Summary of independent articles reporting on the diagnostic accuracy of Lever sign for ACL tear/injury.
| Authors | Subjects (n) | SN/SP (95% CI) | +LR/-LR | PPV/NPV | Reference Standard | Post-Test Probability |
|---|---|---|---|---|---|---|
| Chong et al. (2017)27 | 33 |
OS 0.88 SN (NR) (pre-anesthesia); 0.97 (NR) (post-anesthesia) PA 0.82 SN (NR) (pre-anesthesia); 1.0 SN (NR) (post-anesthesia) |
NA | NA | Arthroscopy | NA |
| Deveci et al. (2015)28 | 117 | 0.94 (NR) (pre-anesthesia) 0.98 SN (NR) (post-anesthesia) |
NA | NA | Arthroscopy | NA |
| Jarbo et al. (2017)29 | 54 | 0.86 (0.68 to 0.96)/0.85 (0.64 to 0.96) | 5.4/0.16 | 0.86/0.84 | Arthroscopy | 86% with (+) test 16% with (-) test (54% pre-test prevalence) |
| Mulligan et al. (2017)30 | 41 | 44 (14 to 78)/75 (57 to 89) | 1.8/0.74 | 0.33/0.83 | Clinical test cluster | 33% with (+) test 17% with (-) test (22% pre-test prevalence) |
SN=sensitivity, SP=specificity, +LR=positive likelihood ratio, -LR=negative likelihood ratio, (+)=positive, (-)=negative, PPV=positive predictive value, NPV=negative predictive value, CI=confidence interval, n=number, NR=not reported, OS=orthopedic surgeon, PA=physician assistant, NA=not applicable
One of the studies30 utilized a separate reference standard, therefore not qualifying for meta-analysis. Besides arthroscopy as a gold standard, Mulligan et al30 also utilized a clinical test cluster as a reference standard in 41 subjects, demonstrating diagnostic values of: SN 0.44 (95% CI 0.17 0 to 0.74), SP 0.75 (95% CI 0.67 to 0.83), + LR 1.78 (95% CI 0.69 to 4.58), -LR 0.74 (95% CI 0.40 to 1.37). The prevalence of ACL tear in this study with clinical test cluster reference standard was 22%. Post-test probability with a positive finding was 33%, while a post-test probability with a negative finding was 17%.
DISCUSSION
The aim of this systematic review with meta-analysis was to summarize the diagnostic accuracy of the Lever sign when used to diagnose an ACL tear. Based on limited evidence of heterogeneous methodological quality, the Lever sign can moderately change post-test probability to rule in or rule out an ACL tear based upon studies with lower risk of bias. Interpretation of the methodological quality of the primary diagnostic studies is presented, as well as comparisons to the findings of previous meta-analyses of other ACL tests.
Methodological quality of the primary diagnostic studies and impact on accuracy
Eight primary diagnostic studies, including the original article by Lelli et al., have investigated this test. Only two studies were considered to have a low risk of bias.29,31 Out of the five other studies11,27,28,30,32, three low-quality studies11,27,28 included 644 out of the 977 patients (66%) in this systematic review.
An important bias in these three studies is the assessment of the Lever sign on cohorts including only ACL-deficient knees prior to obtaining arthroscopic surgery.11,27,28 Accordingly with QUADAS methodological assessment, this bias precludes investigators from adequate blinding when the index test was executed, which likely overestimated accuracy.34 More so, because of the absence of non ACL-deficient cases is these cohorts, only SN could be calculated. Thus, these studies only informed on the capacity of the Lever sign to assist in “ruling out” the presence of injury when the test is negative.35 Lastly, Lelli et al. measured SP of the Lever sign by evaluating the test on the healthy knees of the patients as a control.11 This represents a case-control bias which can also overestimate accuracy.34,36
This meta-analysis demonstrates the impact of low-quality studies on analysis of accuracy. The pooled estimates for positive and negative LR using MRI as a reference standard was 13.1 and 0.28 when considering only the two high-quality studies.29,31 When adding one low-quality study11 to the meta-analysis, pooled estimate for +LR increased approximately 10-fold to 128.0 and negative LR to 0.18. The addition of 400 true positives and true negatives without added false positive and false negative findings because of possible biases yielded wide 95% CI and unprecise estimates to guide clinical decision-making.
Clear utilization of blinding for test interpretation was reported in only one study29 in this review. Test interpretation with knowledge of index test findings is a significant bias in diagnostic accuracy studies. A meta-review37 and one review38 have reported that overall accuracy was higher in the presence of diagnostic review bias (person interpreting the reference standard was aware of the index test results).
These biases were also found in recent diagnostic studies investigating other ACL tests.8 Researchers are urged to follow Equator Network guidelines (http://www.equator-network.org) and QUADAS,39 in future study designs to advance our understanding of these diagnostic tests.
Comparison of the accuracy of Lever sign to other ACL tests
The accuracy estimates from this meta-analysis must be compared with meta-analyses of other ACL tests5 to inform regarding clinical utilization of these tests. The studies in this review report a SN of 55% to 95% (depending on the gold standard), yielding negative LR of 0.18 to 0.58. This induces a small to moderate change in negative post-test probability of 14% to 40% to rule out an ACL tear when the test is negative. A SP of 88% to 97% was also reported in the included studies, yielding a positive LR of 9.2 to 128. This induces a moderate change in positive post-test probability of 30 to 35% to rule in an ACL tear when the test is positive. Because of the limited number of patients included in this meta-analysis, estimates from this review demonstrate wide 95% CI and should be interpreted cautiously. From the two high-quality studies, one found SN of 63% and SP of 90%,29 while the other found SN of 83% and SP of 80%.31
The most comprehensive meta-analysis summarizing the accuracy of other ACL tests included 28 primary studies and demonstrated the following statistics.6 For the Lachman test, SN and negative LR was 85% and 0.2, while SP and positive LR was 94% and 10.2. For the Pivot shift test, SN and negative LR was 24% and 0.90, while SP and positive LR was 98% and 8.5. For the anterior drawer test, SN and negative LR was 55% and 0.50, while SP and positive LR was 92% and 7.3. When comparing estimates and 95% CI from meta-analyses, the Lever sign may demonstrate diagnostic accuracy comparable to other ACL tests. This conclusion mirrors one high-quality study31 in this review which directly compared all ACL tests in one cohort and found no significant difference between the estimates. Video performance of the Lachman test and Lever sign are demonstrated in Figure 5, available online.
Future direction
The results from this first meta-analysis regarding diagnostic accuracy of the Lever sign show potential for its use in clinical practice. Given the available scarce evidence and low to moderate study quality, further investigation is required to match the level of understanding of the other common tests used to examine those with suspected ACL tear.5 Other high-quality diagnostic studies are required to better understand the accuracy of this test in diverse clinical contexts and in various patient profiles. Notably, it remains to be demonstrated that this test can replace other ACL tests for contexts such as acute presentation or for partial ACL tears. Also, while the test was developed as a simplified alternative to other more technically challenging tests or for evaluators with small hands compared to a patient's muscle size, only three studies have shown inter-rater reliability to be “fair” or “high”.27,28,33 Previous evidence examining ACL diagnostic tests indicates that reliability can be lowered when the evaluator is inexperienced.10 In most studies on the Lever test, there were only experienced clinicians. Future studies should assess if this test can be valid and reliable when used by clinicians with a diversity of clinical experience, with an emphasis on primary care clinicians. It is likely that the required training for this test, as well as describing optimal condition for execution (eg. cushioning of the examination table, amount of force applied), must be standardized.
Limitations
Due to heterogeneity of studies and variable reference standards only five of the seven studies qualified for meta-analysis with two different reference standards (MRI and arthroscopy). Despite moderate shifts in positive and negative post-test probability using the Lever sign compared to both reference standards, caution is warranted due to study quality. Other limitations of this study include: limiting the search strategy to only those articles written in English or French, lack of comparison of subject inclusion and exclusion across the studies and primary studies performed in settings of high pre-test probability. Lastly, only one author extracted the data points, but both of the other authors verified all data points.
CONCLUSION
This meta-analysis summarizes the diagnostic accuracy of the Lever sign when used to diagnose ACL tear. Based on limited evidence of heterogeneous methodological quality, the Lever sign can moderately change post-test probability to rule in or rule out an ACL tear in studies with lower risk of bias. These results should be interpreted cautiously due to the limited number of studies in this review, and the likelihood that small sample sizes and study quality may have affected test accuracy. The Lever sign is simple to use and could complement a complete physical examination, specifically in contexts where the traditional tests may be difficult to execute. The evidence for the Lever sign remains scarce and warrants additional investigation to guide clinical utility.
Appendix I. MEDLINE Search Strategy
(“Clinical Examination” OR “Clinical Exam”[tiab] OR Physical Examination OR “Physical Exam”[tiab] OR “Orthopedic Examination”[tiab] OR “Orthopedic Exam”[tiab] OR “musculo-skeletal examination”[tiab] OR “musculo-skeletal examination”[tiab] OR “musculoskeletal exam”[tiab] OR “musculo-skeletal exam”[tiab] OR “Clinical evaluation”[tiab] OR “Physical evaluation”[tiab] OR “musculoskeletal evaluation”[tiab] OR “musculo-skeletal evaluation”[tiab] OR “Clinical inspection”[tiab] OR “Physical inspection”[tiab] OR “musculoskeletal inspection”[tiab] OR “musculo-skeletal inspection”[tiab] OR “Sensitivity” [tiab] OR “Specificity” [tiab] OR “Accuracy” [tiab]) AND (“knee”[MeSH Terms] OR “knee joint”[MeSH Terms] OR Knee[tiab] OR knees[tiab] OR “tibiofemoral joint”[tiab] OR “Anterior Cruciate Ligament Injuries”[MeSH Terms] OR ((“Anterior Cruciate Ligament”[MeSH Terms] OR “Anterior Cruciate Ligament”[tiab] OR ACL[tiab]) AND (Injury[tiab] OR injuries[tiab] OR “injuries”[Subheading] OR tear[tiab] OR tears[tiab] OR “lacerations”[MeSH Terms] OR “lacerations”[tiab] OR “laceration”[tiab] OR “rupture”[MeSH Terms] OR “rupture”[tiab] OR “ruptures”[tiab]))) AND (randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized[tiab] OR randomised[tiab] OR randomization[tiab] OR randomisation[tiab] OR placebo[tiab] OR drug therapy[sh] OR randomly[tiab] OR trial[tiab] OR groups[tiab] OR Clinical trial[pt] OR “clinical trial”[tiab] OR “clinical trials”[tiab] OR “evaluation studies”[Publication Type] OR “evaluation studies as topic”[MeSH Terms] OR “evaluation study”[tiab] OR evaluation studies[tiab] OR “intervention studies”[MeSH Terms] OR “intervention study”[tiab] OR “intervention studies”[tiab] OR “case-control studies”[MeSH Terms] OR “case-control”[tiab] OR “cohort studies”[MeSH Terms] OR cohort[tiab] OR “longitudinal studies”[MeSH Terms] OR “longitudinal”[tiab] OR longitudinally[tiab] OR “prospective”[tiab] OR prospectively[tiab] OR “retrospective studies”[MeSH Terms] OR “retrospective”[tiab] OR “follow up”[tiab] OR “comparative study”[Publication Type] OR “comparative study”[tiab] OR “Cross sectional studies”[mesh] OR “cross sectional”[tiab]) NOT (Editorial[ptyp] OR Letter[ptyp] OR Case Reports[ptyp] OR Comment[ptyp]) NOT (animals[mh] NOT humans[mh])
Appendix II.
Excluded Studies (Abstract & full text review)
| Study | Title | Reason Excluded |
|---|---|---|
| Antinolfi P, et al. (2017)1 | Relationship between Clinical, MRI, and Arthroscopic Findings: A Guide to Correct Diagnosis of Meniscal Tears |
Lever test not utilized in study |
| Chong et al. (2017)2 | Evaluating Different Clinical Diagnosis of Anterior Cruciate Ligament Ruptures In Providers with Different Training Backgrounds. |
Reliability study; diagnostic accuracy not reported |
| Cinque ME, et al. (2017)3 | The Heel Height Test: A Novel Tool for the Detection of Combined Anterior Cruciate Ligament and Fibular Collateral Ligament Tears. |
Lever test not utilized in study |
| Kilinc BE, et al. (2016)4 | Evaluation of the accuracy of Lachman and Anterior Drawer Tests with KT1000 ın the follow-up of anterior cruciate ligament surgery. |
Lever test not utilized in study |
| Orlando Júnior N, et al. (2015)5 | Diagnosis of knee injuries: comparison of the physical examination and magnetic resonance imaging with the findings from arthroscopy. |
Lever test not utilized in study |
| Mouton C, et al. (2016)6 | Combined anterior and rotational knee laxity measurements improve the diagnosis of anterior cruciate ligament injuries. |
Not diagnostic accuracy study. |
| Geraets SE, et al (2015)7 | Diagnostic value of medical history and physical examination of anterior cruciate ligament injury: comparison between primary care physician and orthopaedic surgeon. |
Lever test not utilized in study |
| Srisuwanporn P, et al. (2016)8 | Accuracy of a New Stress Radiographic Device in Diagnosing Anterior Cruciate Ligament Tear. |
Not physical examination diagnostic accuracy study |
| Speziali A, et al. (2016)9 | Diagnostic value of the clinical investigation in acute meniscal tears combined with anterior cruciate ligament injury using arthroscopic findings as golden standard. |
Lever test not utilized in study |
REFERENCES
- 40.Antinolfi P Crisitiani R Manfreda F, et al. Relationship between Clinical, MRI, and Arthroscopic Findings: A Guide to Correct Diagnosis of Meniscal Tears. Joints. 2017;5(3):164-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chong AC Whitetree C Priddy MC Zimmerman PR Haeder PR Prohaska DJ. Evaluating Different Clinical Diagnosis of Anterior Cruciate Ligament Ruptures In Providers with Different Training Backgrounds. Iowa Orthop J. 2017;37:71-79. [PMC free article] [PubMed] [Google Scholar]
- 42.Cinque ME Geeslin AG Chahla J, et al. The Heel Height Test: A Novel Tool for the Detection of Combined Anterior Cruciate Ligament and Fibular Collateral Ligament Tears. Arthroscopy. 2017;33(12):2177-2181. [DOI] [PubMed] [Google Scholar]
- 43.Kilinc BE Kara A Celik H Oc Y Camur S. Evaluation of the accuracy of Lachman and Anterior Drawer Tests with KT1000 in the follow-up of anterior cruciate ligament surgery. Journal of exercise rehabilitation. 2016;12(4):363-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Orlando Junior N de Souza Leao MG de Oliveira NH. Diagnosis of knee injuries: comparison of the physical examination and magnetic resonance imaging with the findings from arthroscopy. Rev Bras Ortop. 2015;50(6):712-719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mouton C Theisen D Meyer T, et al. Combined anterior and rotational knee laxity measurements improve the diagnosis of anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2859-2867. [DOI] [PubMed] [Google Scholar]
- 46.Geraets SE Meuffels DE van Meer BL Breedveldt Boer HP Bierma-Zeinstra SM Reijman M. Diagnostic value of medical history and physical examination of anterior cruciate ligament injury: comparison between primary care physician and orthopaedic surgeon. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):968-974. [DOI] [PubMed] [Google Scholar]
- 47.Srisuwanporn P Wachiratarapadorn S Panyasakulwong R Thuntong B Cheecharern S Precha W. Accuracy of a New Stress Radiographic Device in Diagnosing Anterior Cruciate Ligament Tear. JMed Assoc Thai. 2016;99(4):394-399. [PubMed] [Google Scholar]
- 48.Speziali A Placella G Tei MM Georgoulis A Cerulli G. Diagnostic value of the clinical investigation in acute meniscal tears combined with anterior cruciate ligament injury using arthroscopic findings as golden standard. Musculoskeletal surgery. 2016;100(1):31-35. [DOI] [PubMed] [Google Scholar]
Appendix III.
Potential Sources of Support (if reported in study, statements are in quotations).
| Study | Potential Sources of Support (if reported in study) |
|---|---|
| Chong et al. (2017)27 | “Conflict of Interest Statement: This study did not receive any funding support for this research. The participants and authors of this study did not receive any payments or other personal benefit, or commitments or agreements that were related in any way to the subject of the research that was conducted. No benefits of any form have been received directly or indirectly to the subject of this article. The authors report no actual or potential conflict of interest in relation to this article.” |
| Deveci et al. (2015)28 | “Competing interests The authors declare that they have no competing interests.” |
| Jarbo et al. (2017)29 | “The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.” |
| Lelli et al. (2014)11 | No acknowledgement or reporting of sources of support or conflict of interest in manuscript |
| Lichtenberg et al. (2018)33 | The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. Ethical approval for this study was obtained from VU University Medical Center Amsterdam (MTC/2015.327). |
| Massey et al. (2017)31 | “The authors report the following potential conflicts of interest or sources of funding: J.D.H. receives support from NIA Magellan and Slack. He is a member of editorial board of Arthroscopy and Frontiers in Surgery, and a committee member of AOSSM Self-Assessment and AAOS OAFP Workgroup. P.C.M. receives support from NIA Magellan, Genzyme, Slack, DePuy, A Johnson & Johnson Company, Arthrex, and Zimmer. He is a member of editorial board of Journal of Knee Surgery and Orthobullets.com.” |
| Mulligan et al. (2017)30 | “We declare that we have no conflicts of interest in the authorship or publication of this contribution. |
| Thapa et al. (2015)32 | “Conflict of interests: None declared.” |
Appendix IV.
QUADAS Values for Included Studies.
| Article | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chong et al. (2017)27 | N | N | Y | Y | Y | Y | U | Y | Y | U | U | U | N | N | 6 |
| Deveci et al. (2015)28 | U | U | Y | Y | Y | Y | U | Y | Y | U | N | N | N | N | 6 |
| Jarbo et al. (2017)29 | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | Y | Y | N | N | 11 |
| Lichtenberg et al. (2018)33 | Y | Y | Y | U | U | Y | N | Y | Y | Y | U | Y | N | N | 8 |
| Lelli et al. (2014)11 | U | U | Y | U | Y | Y | Y | Y | N | U | U | U | N | N | 5 |
| Massey et al. (2017)31 | Y | Y | Y | U | Y | Y | N | Y | Y | Y | N | Y | Y | Y | 11 |
| Mulligan et al. (2017)30 | Y | Y | U | U | Y | N | Y | Y | Y | Y | U | Y | U | Y | 9 |
| Thapa et al. (2015)32 | Y | Y | Y | U | Y | Y | N | Y | Y | Y | N | Y | N | N | 9 |
Abbreviations: Y, yes; N, No; U, Unknown; QUADAS, Quality Assessment of Diagnostic Accuracy Studies scores; studies were stratified as “high quality/low risk of bias if the QUADAS score was ≥10/14, and “low quality/high risk of bias of the study score < 10/14.
REFERENCES
- 1.Anderson MJ Browning WM 3rd Urband CE Kluczynski MA Bisson LJ. A systematic summary of systematic reviews on the topic of the anterior cruciate ligament. Orthop J Sports Med. 2016;4(3) 10.1177/2325967116634074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suter LG Smith SR Katz JN, et al. Projecting lifetime risk of symptomatic knee osteoarthritis and total knee replacement in individuals sustaining a complete anterior cruciate ligament tear in early adulthood. Arthr Care Res. 2017;69(2):201-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Filbay SR Roos EM Frobell RB Roemer F Ranstam J Lohmander LS. Delaying ACL reconstruction and treating with exercise therapy alone may alter prognostic factors for 5-year outcome: an exploratory analysis of the KANON trial. Br J Sports Med. 2017;51(22):1622-1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parwaiz H Teo AQ Servant C. Anterior cruciate ligament injury: A persistently difficult diagnosis. Knee. 2016;23(1):116-120. [DOI] [PubMed] [Google Scholar]
- 5.Decary S Ouellet P Vendittoli PA Roy JS Desmeules F. Diagnostic validity of physical examination tests for common knee disorders: An overview of systematic reviews and meta-analysis. Phys Ther Sport. 2017;23:143-155. [DOI] [PubMed] [Google Scholar]
- 6.Benjaminse A Gokeler A van der Schans CP. Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther. 2006;36(5):267-288. [DOI] [PubMed] [Google Scholar]
- 7.van Eck CF van den Bekerom MP Fu FH Poolman RW Kerkhoffs GM. Methods to diagnose acute anterior cruciate ligament rupture: a meta-analysis of physical examinations with and without anaesthesia. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1895-1903. [DOI] [PubMed] [Google Scholar]
- 8.Leblanc MC Kowalczuk M Andruszkiewicz N, et al. Diagnostic accuracy of physical examination for anterior knee instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2805-2813. [DOI] [PubMed] [Google Scholar]
- 9.Lange T Freiberg A Droge P Lutzner J Schmitt J Kopkow C. The reliability of physical examination tests for the diagnosis of anterior cruciate ligament rupture--A systematic review. Man Ther. 2015;20(3):402-411. [DOI] [PubMed] [Google Scholar]
- 10.Decary S Ouellet P Vendittoli PA Desmeules F. Reliability of physical examination tests for the diagnosis of knee disorders: Evidence from a systematic review. Man Ther. 2016;26:172-182. [DOI] [PubMed] [Google Scholar]
- 11.Lelli A Di Turi RP Spenciner DB Domini M. The “Lever Sign”: a new clinical test for the diagnosis of anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2794-2797. [DOI] [PubMed] [Google Scholar]
- 12.Moher D Liberati A Tetzlaff J Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336-341. [DOI] [PubMed] [Google Scholar]
- 13.Swartz MK. The PRISMA statement: a guideline for systematic reviews and meta-analyses. J Pediatr Health Care. 2011;25(1):1-2. [DOI] [PubMed] [Google Scholar]
- 14.Wilczynski NL Haynes RB. Developing optimal search strategies for detecting clinically sound prognostic studies in MEDLINE: an analytic survey. BMC Med. 2004;2:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilczynski NL Haynes RB. Optimal search strategies for detecting clinically sound prognostic studies in EMBASE: an analytic survey. J Am Med Inform Assoc. 2005;12(4):481-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Doust JA Pietrzak E Sanders S Glasziou PP. Identifying studies for systematic reviews of diagnostic tests was difficult due to the poor sensitivity and precision of methodologic filters and the lack of information in the abstract. J Clin Epidemiol. 2005;58(5):444-449. [DOI] [PubMed] [Google Scholar]
- 17.Akobeng AK. Understanding systematic reviews and meta-analysis. Arch Dis Child. 2005;90(8):845-848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hegedus EJ Goode A Campbell S, et al. Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. Br J Sports Med. 2008;42(2):80-92; discussion 92. [DOI] [PubMed] [Google Scholar]
- 19.Reiman MP Goode AP Hegedus EJ Cook CE Wright AA. Diagnostic accuracy of clinical tests of the hip: a systematic review with meta-analysis. Br J Sports Med. 2013;47(14):893-902. [DOI] [PubMed] [Google Scholar]
- 20.Cook C Mabry L Reiman MP Hegedus EJ. Best tests/clinical findings for screening and diagnosis of patellofemoral pain syndrome: a systematic review. Physiotherapy. 2012;98(2):93-100. [DOI] [PubMed] [Google Scholar]
- 21.Reiman MP Loudon JK Goode AP. Diagnostic accuracy of clinical tests for assessment of hamstring injury: a systematic review. J Orthop Sports Phys Ther. 2013;43(4):223-231. [DOI] [PubMed] [Google Scholar]
- 22.Wright AA Hegedus EJ Lenchik L Kuhn KJ Santiago L Smoliga JM. Diagnostic accuracy of various imaging modalities for suspected lower extremity stress fractures: A systematic review with evidence-based recommendations for clinical practice. Am J Sports Med. 2016; 44(1):255-63. [DOI] [PubMed] [Google Scholar]
- 23.Reiman MP Thorborg K Goode AP Cook CE Weir A Holmich P. Diagnostic accuracy of imaging modalities and injection techniques for the diagnosis of femoroacetabular impingement/labral tear. Am J Sports Med. 2017;45(11):2665-2677. [DOI] [PubMed] [Google Scholar]
- 24.Jaeschke R Guyatt GH Sackett DL. Users' guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patientsϿ. The Evidence-Based Medicine Working Group. JAMA. 1994;271(9):703-707. [DOI] [PubMed] [Google Scholar]
- 25.DerSimonian R Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177-188. [DOI] [PubMed] [Google Scholar]
- 26.Sterne JA Gavaghan D Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53(11):1119-1129. [DOI] [PubMed] [Google Scholar]
- 27.Chong AC Whitetree C Priddy MC Zimmerman PR Haeder PR Prohaska DJ. Evaluating different clinical diagnosis of anterior cruciate ligament ruptures In providers with different training backgrounds. Iowa Orthop J. 2017;37:71-79. [PMC free article] [PubMed] [Google Scholar]
- 28.Deveci A Cankaya D Yilmaz S Ozdemir G Arslantas E Bozkurt M. The arthroscopical and radiological corelation of lever sign test for the diagnosis of anterior cruciate ligament rupture. SpringerPlus. 2015;4:830. 10.1186/s40064-015-1628-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jarbo KA Hartigan DE Scott KL Patel KA Chhabra A. Accuracy of the lever sign test in the diagnosis of anterior cruciate ligament injuries. Orthop J Sports Med. 2017;5(10) 10.1177/2325967117729809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mulligan EP Anderson A Watson S Dimeff RJ. The diagnostic accuracy of the lever sign for detecting anterior cruciate ligament injury. Int J Sports Phys Ther. 2017;12(7):1057-1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Massey PA Harris JD Winston LA Lintner DM Delgado DA McCulloch PC. Critical analysis of the lever test for diagnosis of anterior cruciate ligament insufficiency. Arthroscopy. 2017;33(8):1560-1566. [DOI] [PubMed] [Google Scholar]
- 32.Thapa SS Lamichhane AP Mahara DP. Accuracy of Lelli test for anterior cruciate ligament tear. J Inst Med. 2015;37(2):91-94. [Google Scholar]
- 33.Lichtenberg MC Koster CH Teunissen LPJ, et al. Does the Lever Sign Test Have Added Value for Diagnosing Anterior Cruciate Ligament Ruptures? Orthop J Sports Med. 2018;6(3) 10.1177/2325967118759631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Whiting PF Rutjes AW Westwood ME Mallett S, Group Q-S. A systematic review classifies sources of bias and variation in diagnostic test accuracy studies. J Clin Epidemiol. 2013;66(10):1093-1104. [DOI] [PubMed] [Google Scholar]
- 35.Hegedus EJ Stern B. Beyond SpPIN and SnNOUT: Considerations with dichotomous tests during assessment of diagnostic accuracy. J Man Manipul Ther. 2009;17(1):E1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rutjes AW Reitsma JB Di Nisio M Smidt N van Rijn JC Bossuyt PM. Evidence of bias and variation in diagnostic accuracy studies. CMAJ. 2006;174(4):469-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lijmer JG Mol BW Heisterkamp S, et al. Empirical evidence of design-related bias in studies of diagnostic tests. JAMA. 1999;282(11):1061-1066. [DOI] [PubMed] [Google Scholar]
- 38.Brealey SD Scally AJ Hahn S Godfrey C. Evidence of reference standard related bias in studies of plain radiograph reading performance: a meta-regression. Br J Radiol. 2007;80(954):406-413. [DOI] [PubMed] [Google Scholar]
- 39.Whiting P Rutjes AW Reitsma JB Bossuyt PM Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Method. 2003;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]