Abstract
Background
Tightness of hip flexor muscles has been recognized as a risk factor for various musculoskeletal injuries in the lower extremities.
Purpose
The purpose of this study was to examine the acute effects of two hip flexor stretching techniques (dynamic and hold-relax proprioceptive neuromuscular facilitation, HR-PNF) on hip extension (ROM), knee joint position sense (JPS) and balance in healthy college age students who exhibit tightness in hip flexor muscles.
Study Design
Pretest-posttest randomized experimental groups.
Methods
Thirty-six healthy college age students (mean = 22.37 years) with tight hip flexors participated in this study. Hip extension ROM, knee joint position sense and dynamic balance were tested pre- and post-stretching using a digital inclinometer, an iPod touch and the Y-Balance test, respectively. Subjects were randomly divided into dynamic and HR-PNF stretching groups. Three-way mixed analysis of variance was utilized to explore if an interaction existed between the groups in tested variables.
Results
There was a significant effect of time on hip extension ROM in both groups (p < 0.001). There was also a significant effect of stretch type on hip extension ROM (p = 0.004) favoring hold-relax over dynamic stretching group. There was a non-significant effect of time on mean knee joint position replication error in both groups. There was a significant main effect of time on the Y-Balance test's mean distance of reach to posteromedial and posterolateral directions (p < 0.001). There was also a significant main effect of directions of reach on distances achieved (p < 0.001) favoring posterolateral over posteromedial, and the latter over anterior direction.
Conclusions
The results of this study demonstrated the effectiveness of both HR-PNF and dynamic stretching techniques which resulted in a significant acute improvement in hip extension ROM and dynamic balance measures, with HR-PNF being more effective than dynamic stretch. However, there were no significant improvements in knee joint position replication over time in either stretching group.
Level of Evidence
2b
Keywords: Dynamic balance, dynamic stretching, hold-relax proprioceptive neuromuscular facilitation, knee joint position sense, tight hip flexor
INTRODUCTION
Tightness of hip flexor muscles (i.e. iliopsoas and rectus femoris) evaluated through hip extension ROM measurement, has been recognized as a risk factor for various musculoskeletal injuries (e.g., knee and hamstrings) in the lower extremities.1-7 ROM is defined as the degree of movement within a joint, and it can be active (reached by voluntary skeletal muscles’ contraction) or passive (achieved by external mean such as gravity).8 Restricted hip flexor mobility has been clinically defined as the inability of the individual to achieve full hip extension during the modified Thomas test position.8 Tight hip flexors is an impairment that has been found in both symptomatic individuals (individuals with lower quarter or extremity disorders and functional limitations) and those individuals who are asymptomatic.6,9 Lack of flexibility may result in early muscle fatigue or altered movement patterns.5 Therefore, hip flexor muscle tightness is believed to have negative impact on dynamic balance as well as on biomechanics of lower extremities which, in turn, can increase the risk of falls.10,11
Hip flexor muscle tightness has been negatively correlated with dynamic balance performance in junior high school students.10 Several authors have suggested an association between diminished balance and injury.12-16 Balance and joint position sense (JPS) are proprioceptive parameters that rely on contributions from visual, vestibular and peripheral receptors that are found in skin, joints, muscles and ligaments.17-24 Proprioception provides the body with conscious and subconscious JPS and motion, and is essential for knee joint functioning to maintain optimal control (balance) of lower extremities while performing daily physical activities.25-27 JPS is an aspect of proprioception that plays an important role in functional dynamic stability of joints through the action of the muscles and ligaments around them throughout their ROM.26,28-30 Reduced contributions from sensory proprioceptive receptors may diminish the protective reflex mechanisms of muscles which, in turn, could predispose individuals to musculoskeletal disorders by altering the control of movement.31.32
Since tightness of hip flexors is associated with balance dysfunction, and because the proprioceptive aspect of JPS is one of the mechanisms that contributes to maintenance of balance, it is reasonable to question if restricted hip flexors have unfavorable effects on the knee's JPS. The action of rectus femoris muscle on both joints (as hip flexor and knee extensor) provides further support for this notion.33 Similar to the relationship between tight hip flexors and lower extremity injuries, abnormal knee JPS has also been linked to several orthopedic and musculoskeletal conditions in knee joint.34-37 These factors combined may highlight the role of hip flexor tightness as a key component related to reduced balance, diminished knee JPS and increased risk of lower extremity injury.
In rehabilitation practice, stretching of hip flexor muscles has been acknowledged as effective in addressing limited hip extension ROM.6,38 A variety of stretching techniques have been described in the literature including dynamic, static (active or passive), and proprioceptive neuromuscular facilitation (PNF) to address this impairment.6,39 Dynamic stretching is a controlled movement that uses the active ROM of the joint while moving without exceeding extensibility limits of the individual.40 Dynamic stretching incorporates a concomitant active contraction of antagonist muscles which may lead to benefits to those muscles that are not experienced with static stretching.6 Therefore, and due to its distinct benefits on muscular performance, dynamic stretching may be the preferred stretching technique.41-43 Proprioceptive neuromuscular facilitation (PNF) stretching on the other hand, is considered one of the most effective stretching techniques used to improve ROM, particularly in respect to short-term changes in ROM.44,45 PNF type stretching can be defined as a combination of isometric contraction and passive lengthening of the target muscle or group of muscles.46 There are three known techniques for PNF stretching procedures. These three techniques include contract and relax (CR), hold and relax (HR), and contract-relax with antagonist contraction technique (CR-AC).47-49
The purpose of this study was to examine the acute effects of two hip flexor stretching techniques (dynamic and HR-PNF) on hip extension ROM, knee JPS and balance in healthy college age students who exhibit tightness in hip flexor muscles. The authors also aimed to determine which one of these techniques has a greater influence on hip extension ROM, knee JPS and dynamic balance. It was hypothesized that significant differences in hip extension ROM, knee JPS and balance measurements would result between pre and post stretching intervention protocols. Additionally, it was hypothesized that significant differences would occur in these measurements between the two stretching groups at post intervention time point.
METHODS
The study sample consisted of thirty-six college age students (25 males, 11 females ). The primary criterion for inclusion to this study was the presence of tightness of hip flexor muscles (THF). THF in the current study was identified as a subject demonstrating a bilateral hip (i.e. unilateral THF was excluded) hip extension angle between +5 ° to + 15 ° above the horizon during the modified Thomas test. Subjects with lower extremity injuries or pain, orthopedic, neurological, cardiovascular abnormalities, or surgeries, as well as a history of participating in a proprioceptive or balance training programs in the prior six months were excluded from participating in this study. This experiment was approved by the human subject's review board of Western Washington University. A written informed consent, health history and physical activity questionnaire forms were provided to each participant prior to data collection.
Design of the Study
A pretest-posttest randomized experimental groups design was used for this study. The current study utilized two treatment groups: group A performed a dynamic stretching (DS) protocol while group B underwent HR-PNF stretching protocol. Hip extension ROM, knee JPS (constant error, CE) and dynamic balance (% distance of reach) were the dependent variables measured pre- and post-stretching (immediately-post and after five minutes for hip extension ROM) protocols. Pre- and post-intervention time points, type of stretching technique and side for hip extension ROM, knee angle for JPS and direction for dynamic balance performance were the three independent variables in this study. A general warm up protocol which consisted of five minutes of light jogging on a treadmill at a comfortable self-selected pace was used before stretching in both groups.
Dynamic stretching (DS) protocol
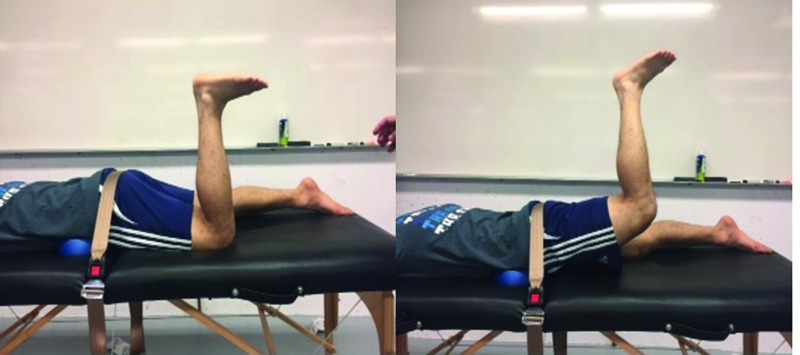
In group A, subjects lay prone with stabilizing strap placed at the posterior inferior iliac spine (PSIS) to stabilize the hips to the massage table. Then, they started actively extending the hip (knee flexed at ≈90 °) of the target limb until stretch was felt in anterior thigh (Figure 1). Subjects repeated this exercise for 10 times within a 20-second period (1 rep. in 2 seconds) followed by a 10 second rest period. This was repeated 6 times for each limb. The duration and frequency of this technique (i.e. total dosing of stretching = 120 seconds) was adapted from previous studies and followed the guidelines of the American College of Sports Medicine.6,43,50,51
Figure 1.
Dynamic stretching technique used for stretching hip flexor muscles.
Hold-relax PNF stretching protocol
In group B, subjects lay supine on a treatment table and holding one knee to the chest and letting the other leg to extend freely toward the floor at the end of table. This protocol was adapted from a previous study (Figure 2).39 The hip of interest was moved gently toward the floor (knee flexed at 90 °) until a mild stretch sensation was felt. Then, subject performed a sub-maximal voluntary isometric contraction by hip flexor muscles for 10 seconds against a examiner resistance of ≈ 20 lbs. applied by using a microFET2, padded hand-held dynamometer (Hoggan Health Industries Inc., Salt Lake City, UT, USA). The leg was then passively moved by the examiner to the new ROM and held for 20 seconds; repeated six times per limb.
Figure 2.
Hold-relax proprioceptive neuromuscular facilitation (HR-PNF) stretching technique used for stretching hip flexor muscles.
Following completion of the stretching, hip extension ROM, knee JPS and dynamic balance measurements were obtained. The same investigator and co-investigators performed the same tasks throughout the study.
Data Collection Procedures
Instrumentation
A PRO 3600 digital Protractor (Jewell Construction LLC, Manchester, NH, USA) inclinometer and an Apple iPod touch 5th generation device (Apple Inc., Cupertino, CA, USA), integrated with custom-made application software were used to measure hip extension ROM and knee JPS in both experimental groups, respectively. Intra-rater reliability for the hip extension ROM (The modified Thomas test) measurement was assessed by a pilot work prior to the initiation of the study in a sample of 10 subjects. An excellent degree of reliability was found between test and retest measurements (ICC < 0.96). Validity of this test is established by controlling lumbopelvic movement (i.e. pelvic tilt) during testing of the participants.52 The custom-made application software forms from a 3-axis tri-axial accelerometer and a three-axis gyroscope. The data from the accelerometer was used to calculate the angle of the device with respect to gravity.53 The accuracy of the measurements within the iPod touch device was reported to be 0.49-0.50 °.54 Intra-rater reliability for the hip extension ROM measurements was assessed by a pilot work prior to the initiation of the study in a sample of 10 subjects. An excellent degree of reliability was found between test and retest measurements (ICC<0.96). The Y-Balance Test (YBT) using the Y-Balance test kit (Perform Better Inc., West Warwick, RI, USA) was utilized to measure DB. The Y-Balance test kit includes three poles that extend to anterior (ANT), posterolateral (PL), and posteromedial (PM) directions in relation to the stance foot. Participants were instructed to stand on the center of the Y figure during testing and slide the blocks outward into these three directions.55
Measurement techniques and procedures
To achieve the required level of randomization during testing procedures, the order of hip extension ROM, knee JPS and DB testing was randomized (via computer software) for all subjects to reduce the learning effects.
Hip Extension ROM. The modified Thomas test was used to measure hip extension ROM.8 The following steps were used during the test: the participants were instructed to sit as close to the edge (i.e. the gluteal folds at the edge) of the table as possible; subjects pulled their knees to their chest and then gently rolled backward on the table; while maintaining this position, one of the lower limbs was released, allowing the hip to extend toward the floor; the free hand was used to help holding the other knee to the chest. This position enabled both the leg and knee of the limb being measured to hang off the edge of the table freely unsupported. While the subject kept a posterior pelvic tilt, the examiner assistant placed one of his hands (four fingers) under the lumbar spine to ensure that the lumbar spine was flat. The examiner observed and palpated the thigh to ensure that it was completely relaxed and positioned the knee joint at about 80-90 ° of flexion, then placed the digital inclinometer on the middle point of the anterior aspect of the thigh being tested (Figure 3). The middle point on the thigh was identified as the midway between trochanterion and the lateral epicondyle of the femur. During the pre- and immediately-post and five-min-post intervention time points, hip extension ROM was measured three times, and the average was used for statistical analysis. This measurement was taken by the same examiner to improve reliability of measures.
Figure 3.
Hip extension range of motion (ROM) measurement test using a digital inclinometer (Jewell Construction LLC, Manchester, NH, USA).
Knee JPS test. Subjects were instructed to sit comfortably on the edge of table with shank hanging 90 ° from horizontal and including 2cm of space between the table and the popliteal fossa. iPod was strapped to the lateral side of the subject's dominant leg about 2.4 cm above the lateral malleolus and secured via a Neoprene sleeve with hook and loop Velcro fasteners (Figure 4).54 Once testing began, the iPod provided all audio feedback to guide the subject through their position-reposition task. The task consisted of three trials to both 30 ° and 60 ° of knee extension (total of six trials) which were randomized by the application. Throughout all testing, subjects were asked to wear tight clothes as well as keep their eyes closed in order to eliminate external cues. A customized LabVIEW (National Instruments Corporation, Austin, TX, USA) program was used to calculate the accuracy of the reproduction of each knee joint angle. The accuracy of the reproduction of JPS was represented as a constant error. Constant error refers to the calculated value of deviation from the target angle.56
Figure 4.
Knee joint position sense (JPS) measurement using iPod touch device (Apple Inc., Cupertino, CA, USA) integrated with custom-made application software.
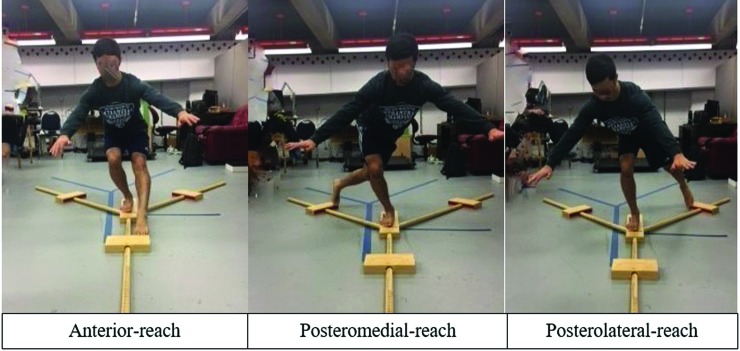
Dynamic balance test. The Y Balance Test (YBT) procedures as used in a previous study conducted by Gribble et al. were utilized to measure and represent dynamic balance performance (DB) during pre- and post-interventions measurements in the current study.57 The participants pushed the moving rectangular pieces using their contralateral legs while maintaining a single-leg stance on the stance foot on the center of piece of the Y figure. Participants pushed these moving pieces to the farthest point possible on each pole with their reaching foot (Figure 5). The distances of reach were recorded to the nearest quarter of centimeter. Next, these distances were normalized to the length of subjects’ legs.57 The sequence of reach directions was randomized using a computer software to evade sequencing effects on the collected data. Participants were given one to two practice trials, then they were instructed to perform three trials in each direction (i.e. ANT, PM and PL) and 15 seconds of rest were given between each trial. The mean value of the three trials during the pre-and post-interventions measurements was used for statistical analysis.
Figure 5.
The Y-Balance Test.
Statistical Analysis
Mean and standard deviation (SD) values for hip extension ROM, knee JPS replication error CE and scores of DB performance during the pre- and post-intervention time points for both groups were calculated. A 3-way mixed analysis of variance (ANOVA) was utilized to test statistically significant differences (SPSS version 21.0). The ANOVA was conducted to compare the group (dynamic stretching vs HR-PNF stretching), time (pre-stretching vs post-stretching), and side of limb (right vs right for hip extension ROM). For the knee JPS, angle (30 ° vs 60 ° in knee JPS) was used instead of the side of limb. For the Y-balance test, the direction (ANT vs PM vs PL) substituted the side of limb. If statistical significance with the two-way interaction or main effects existed, then a pairwise comparison was performed, and Bonferroni correction was applied. Additionally, a partial-eta (η2 p) squared was calculated to determine the effect size. Statistical significance was set at an alpha level of 0.05.
RESULTS
The study sample consisted of thirty-six college age students (24 males, 11 females, mean age 22.37 ± 1.63 years, height 171.05 ± 9.64 cm, and weight 72 ± 13.70 kg). A statistical power analysis based on a previous study and calculated using G* power 3.1 software (Heinrich Heine University, Düsseldorf, Germany) revealed that 18 participants per group would result in an estimated power of 0.80 to observe significant differences with the alpha level set to 0.05.6 Due to equipment malfunction of the JPS measuring device (iPod failed to record or save the measurement), the data of one male participant was excluded from statistical analysis.
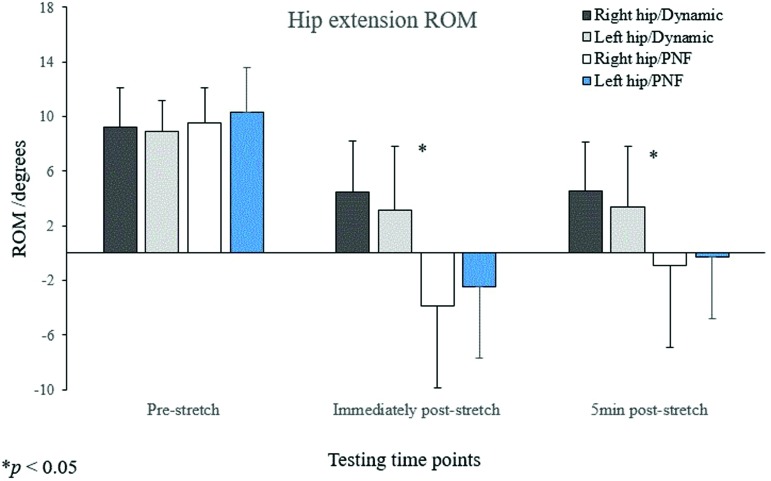
Pre- and post-stretching values of hip extension ROM are shown in Table 1. There was a significant two-way interaction between the side of limb and stretch type (F [1, 33] = 8.154, p = 0.007, η2p = 0.198) indicating to a greater improvement in hip extension ROM on both left and right sides in HR-PNF group compared to DS group ( p = 0.001 and p = 0.035, respectively) (Figure 6). A significant two-way interaction was found between the time and stretch type (F [2, 66] = 20.870, p < 0.001, η2p = 0.387) indicating a greater improvement in HR-PNF compared to DS group occurred in hip extension ROM during immediately-post stretch and post-five-min-stretch time points (p < 0.001 and p = 0.005, respectively). In the HR-PNF stretching group, immediately-post stretching values of hip extension ROM were better than pre-stretching and post-5 min stretching (p < 0.001). In DS group, both immediately-post and post-five-min stretching values were better than pre-test stretching values (p < 0.001).
Table 1.
Dependent variables' mean and standard deviation (SD) values at pre- and post-stretching time points. * denotes a significant difference p < 0.05.
| Dependent Variable | Dynamic Stretching Group n=17 (12 males, 5 females) |
HR-PNF Stretching Group n=18 (12 males, 6 females) |
|---|---|---|
| Right hip extension ROM (°) | (mean ± SD) | (mean ± SD) |
| Pre-stretch | 9.20 ± 2.88 | 9.54 ± 2.58 |
| Immediately post-stretch | 4.46 ± 3.79 * | -3.87 ± 6.02 |
| 5-minutes post-stretch | 4.57 ± 3.60 * | -0.90 ± 6.01 |
| Left hip extension ROM (°) | ||
| Pre-stretch | 8.89 ± 2.29 | 10.34 ± 3.28 |
| Immediately post-stretch | 3.17 ± 4.64 * | -2.48 ± 5.19 |
| 5-minutes post-stretch | 3.35 ± 4.44 * | -0.26 ± 4.52 |
| Knee JPS flexion CE at 30 ° (°) | ||
| Pre-stretch | 5.99 ± 2.43 | 6.23 ± 4.91 |
| Post-stretch | 5.57 ± 3.62 | 5.26 ± 3.63 |
| Knee JPS flexion CE at 60 ° (°) | ||
| Pre-stretch | 1.03 ± 2.97 | 2.12 ± 3.28 |
| Post-stretch | 1.78 ± 2.41 | 2.67 ± 3.87 |
| Y-test/anterior (%) | ||
| Pre-stretch | 64.57 ± 6.66 | 68.30 ± 5.28 |
| Post-stretch | 65.64 ± 6.09 | 69.24 ± 5.93 |
| Y-test/posteromedial (%) | ||
| Pre-stretch | 102.47 ± 9.43 * | 105.11 ± 11.31* |
| Post-stretch | 107.83 ± 7.97 * | 108.03 ± 12.33 * |
| Y-test/posterolateral (%) | ||
| Pre-stretch | 108.90 ± 9.36 * | 112.91 ± 10.52 * |
| Post-stretch | 112.87 ± 8.68 * | 114.06 ± 11.03 * |
Significant difference at p < 0.05.
CE: Constant error, HR-PNF: Hold-relax proprioceptive neuromuscular facilitation, JPS: Joint position sense, ROM: Range of motion, Y-test: Y-Balance test.
Figure 6.
A graphical comparison of hip extension ROM (°) of right and left hips between dynamic and HR-PNF stretching groups during pre-test, immediately post-stretch, and 5-minute post-stretch time points.
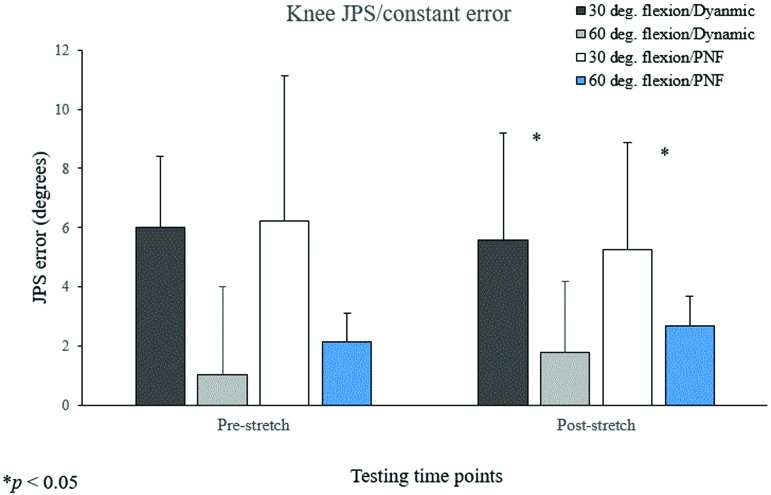
There was no significant main effect of time on mean JPS replication CE (F [1,33] = 0.003, p=0.956, η2 p<0.001) (Table 1). The only significant difference was observed in this test was between the angles of 30 ° and 60 ° over time in JPS replication error CE (i.e. average of pre- and post-combined values in both stretching groups) (F [1,33] = 51.723, p < 0.001, η2p = 0.610), with a smaller error in mean CE (1.90 ° versus 5.76 °) in 60 ° than 30 ° of knee angle, respectively (p < 0.001) (Figure 7).
Figure 7.
A graphical comparison of knee joint position sense (JPS) replication error (°) between dynamic and HR-PNF stretching groups during pre-test, post-test time points.
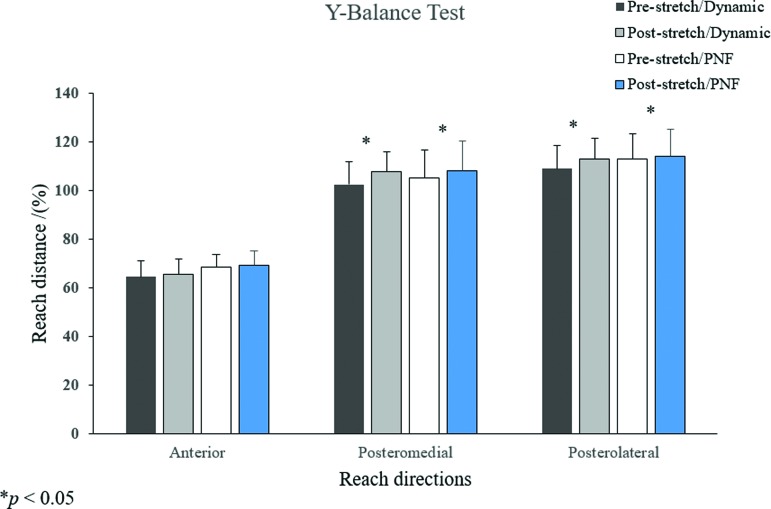
Pre- and post-stretching values for DB are shown in Table 1. There was a significant interaction between time and directions of reach (F [2, 66] = 5.653, p = 0.005, η2p. = 0.146) (Figure 8). Significantly greater distances were noticed during post-test compared to pre-test time point in distances of reach to PM and PL directions (p < 0.001). There was a significant main effect of directions of reach on the Y-Balance test values (F [1.564, 51.619] = 904.148, p < 0.001, η2p = 0.965). There was also a significant main effect of time on the Y-balance test's mean distance (F [1, 33] = 28.386, p < .001, η2p = 0.462) indicating a greater mean distance of reach during post stretching time point than during pre-stretching time point (p < 0.001).
Figure 8.
A graphical comparison of the Y-Balance test's directions of reach (%) between dynamic and HR-PNF stretching groups during pre-test, post-test time points.
DISCUSSION
The purpose of this investigation was to examine the acute effects of two hip flexor stretching techniques on hip extension ROM, knee JPS and DB performance. Results showed significant improvement in hip extension ROM over time in both stretching groups. The results of the current study are consistent with results reported in numerous related studies .6,39,58-63 In a study conducted by Winters et al., researchers stated that the increase in hip extension ROM observed in their study was as a result of passive and active stretching protocols used.6 Malai et al. reported significant improvement in both right and left hip extension ROM after applying HR-PNF stretching technique on 10 individuals with tight iliopsoas muscles.39 In another study, Godges et al. demonstrated the effectiveness of both static and PNF stretching procedures on improving hip extension ROM among seven young males.58
Several possible reasons could have led to the improvement seen in hip extension ROM in both stretching groups such as increased body and muscle temperature and stimulation of nervous system, improved reciprocal inhibition of the antagonist muscles and autogenic inhibition, alteration in stiffness of musculotendinous unit, and alteration in myotatic or stretch reflex.6,40,43,45,47,63-67 However, the results of the current study were in disagreement with another study conducted by Rodacki et al .11 as the values of hip extension ROM immediately-post and post-five- min of stretching in the HR-PNF group was significantly greater than in DS group. PNF stretching technique is considered the most effective stretching technique to produce an immediate and short-term increase in ROM because it includes isometric resistance phase and followed by a static stretching phase in HR-PNF which make it an effective muscle release technique as compared to other stretching techniques.45,48,68 The results of the present study are consistent with a study conducted by Miyahara et al.69 who found a significant increase in hip flexion ROM after using static and PNF stretching protocols on thirteen healthy young male students.
The significant differences in HR-PNF group favoring immediately-post values over pre- and post-5-min stretching values, and post-5 min values over pre-stretching values can be explained by the nature and duration of effects of HR-PNF stretching technique. PNF stretch is a very effective technique for inducing an immediate and short-term increase of ROM.45 Therefore, differences were evident among these testing time points. In post-five- min time point, the effect of HR-PNF technique started to diminish over time, thus, significant difference were also noticed between immediately-post and post-five-min time points. On the contrary, in DS group, only immediately and post-five-min values were significantly greater than pre-test values. This indicates that even though DS was not as effective as HR-PNF stretching on increasing hip extension ROM, it's effect lasted longer and did not diminish as quickly as after the HR-PNF stretching technique.
The smaller mean of CE at 60 ° compared to 30 ° (1.90 ° versus 5.76 °) of knee angle may have occurred as a result of that 60 ° of knee flexion is closer to a resting position of the knee while sitting (i.e.≈90 °), therefore, the body is more familiar with replicating this position as compared to the 30 ° JPS of the knee.70 Possible reasons behind the insignificant differences noticed in the current study may be due to testing and stretching positions’ variation, the participants were young, healthy and physically active individuals who did not have proprioceptive deficits.71 Furthermore, the two stretching techniques may not have imposed adequate effect on the mechanoreceptors in all acting muscle groups around the knee to make a difference in proprioceptive acuity Lastly, large values of standard deviations for this measurement may have contributed to nonsignificant differences. The findings of this study are consistent with what have been reported in a number of other similar studies.42,71-74 Moradi et al. reported nonsignificant difference in knee JPS replication accuracy at 45 ° of knee flexion between pre- and post-static stretching in 30 soccer player (mean age 23.20 ± 1.45 years).42 Larsen and his colleagues stated the use of static stretch regimen had no effect on knee JPS (50 ° and 70 ° flexion) in 20 (6 men, 14 women) healthy young volunteers.72 A similar study demonstrated that using acute bout of passive stretch of quadriceps muscle has no effect on knee JPS (30 ° or 70 ° flexion) among untrained young males (age = 22.1 ± 2.7 years).73 Ghaffarinejad et al. also reported nonsignificant differences in knee JPS absolute error values in 20 °of flexion after stretching quadriceps, hamstrings, hip adductors, gastrocnemius and popliteus muscles.71 However, they stated significant decrease in knee JPS absolute error after statically stretching of quadriceps, hamstrings and hip adductors at 45 ° of knee flexion.71 The authors suggested stretching may have improved knee JPS by increasing proprioceptive feedback which may indirectly cause an enhancement in sensory imagery.
There were significant differences in distances of reach in both PM (pre = 103.82 %, post = 107.94 %) and PL (pre = 110.96 %, post=113.48 %) directions over time. The distance of reach during both time points to PL direction was significantly greater than the reach to PM direction which was in turn greater than the reach to ANT direction (pre=66.49 %, post=65.64 %). Improved DB performance may have occurred due to the decreased postural instability in those individuals by improving the proprioceptive feedback.71,75 It is also possible that the hold duration during HR-PNF stretching and duration of one set during DS was enough to produce this significant improvement.75 Therefore, moderate hold duration during stretching (i.e. 15-20s) may decrease the possible unfavorable reflex activity decrements.75 The results of the current study are supported by findings of several other similar studies.76-79 Handrakis et al. reported significant effect of an acute static stretching protocol on dynamic balance performance in (six men and four women aged 40-60 years) (p < 0.05).76 In a similar study, Azeem et al. have shown that both static and dynamic stretching resulted in a significant improvement in dynamic balance performance in 30 male recreational soccer players (age 17-25 years) (p < 0.001).77 Chatzopoulos and his colleagues demonstrated the superiority of dynamic over static stretching in improving balance performance using stability platform instrument in 31 female high school athletes (p < 0.05).78 Furthermore, Amiri-Khorasani reported that dynamic and combined (static and dynamic) were significantly more effective than static stretching in improving dynamic and static balance performance in 24 female soccer player (mean ± SD age = 22.08 ± 0.77 years) using the Star Balance Test.79 Contrary to the findings of this study, the results of Lim et al showed no significant difference between static, HR-PNF and no stretching groups in the mediolateral and anteroposterior directions of balance test (p < 0.05).80
The significant improvement noticed in distances of reach to PM and PL directions after stretching in both groups may also be explained by nature of the demands during reaching to these directions. Reaching to PM and PL directions involve lengthening of the hip flexors and active hip extension as compared to the anterior reach direction. It is a fact that the stretched muscles (i.e. iliopsoas and rectus femoris) are located on the anterior parts of the hips and legs.33 Therefore, more flexible muscles in these parts of the body would in turn facilitate greater ability to reach to PL direction first and PM second. Further, since concentric action of hip flexors produce hip flexion and external rotation, these muscles are stretched by hip extension and internal rotation movements (i.e. movements occurred during dynamic and HR-PNF in this study).33 Thus, during PL reach, achieving the farthest distance incorporates extension and internal rotation of the hip. On the other hand, reaching to the ANT direction would not have likely benefitted from stretching these muscles because it does not require the hips to be in an extended position but in a flexed position instead (Figure 5). Additionally, the hip and knee of stance leg is flexed while the free leg is performing the reach thus, positioning the hips behind the stance knee (to maintain balance) practically limits the reach distance to ANT direction.
Another possible explanation for the significant improvement in these two directions could be because of a decreased reciprocal inhibition of the gluteus maximus. It is theorized that shortened and restricted hip flexors may decrease neural drive to hip extensors (i.e. reciprocal inhibition of the gluteus maximus muscle).63 Improved function of this muscle post stretching may be a possible reason for a greater distance of reach (i.e. the reaching leg) to these directions since it is a major thigh extensor. Further, gluteus maximus contributes to maintaining balance of the body because it is a powerful muscle and most effective when the thigh is flexed (i.e. position of stance leg while reaching).33 The significant differences observed during the pre- and post-stretching time points between distances of reach to these three directions could be possibly explained by the relationship between hip joint anatomy, ROM of hip, nature of the Y-balance test and directions of reach. This thought is supported by the fact that significant differences between these directions did not change and remained over time during the post-stretching time point too.
This study was not without limitations. The age range of this study was limited to college aged-participants which limits the generalization (i.e. external validity) of its results to other populations. Knee JPS accuracy and ability of DB performance among the participants varied greatly (high standard deviations) during the baseline measurements, which may also have affected the results. In addition, repeating tests within 45-50 minutes could have had a learning effect on the performance during the DB and knee JPS tests despite randomization the order of these tests. Further studies should consider these limitations.
CONCLUSIONS
Tightness of hip flexor muscles may negatively affect dynamic balance performance but not knee joint position replication accuracy among female and male college age students. The results of the current study indicate that performing a single session of hold-relax proprioceptive neuromuscular facilitation and dynamic stretching protocols can significantly improve hip extension ROM (HR-PNF was more effective than dynamic stretch) and dynamic balance performance but are unlikely to aid in knee JPS replication accuracy. Further research is needed to understand how different types of stretching protocols can affect the variables studied in the current study.
REFERENCES
- 1.Chumanov ES Wille CM Michalski MP Heiderscheit BC. Changes in muscle activation patterns when running step rate is increased. Gait Posture. 2012;36(2):231-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delp SL Hess WE Hungerford DS Jones LC. Variation of rotation moment arms with hip flexion. J Biomech. 1999;32(5):493-501. [DOI] [PubMed] [Google Scholar]
- 3.Gabbe BJ Bennell KL Finch CF. Why are older Australian football players at greater risk of hamstring injury? J Sci Med Sport Sports Med Aust. 2006;9(4):327-333. [DOI] [PubMed] [Google Scholar]
- 4.Kolber MJ Fiebert IM. Addressing flexibility of the rectus femoris in the athlete with low back pain. Strength Cond J. 2005;27(5):66–73. [Google Scholar]
- 5.Krivickas LS Feinberg JH. Lower extremity injuries in college athletes: relation between ligamentous laxity and lower extremity muscle tightness. Arch Phys Med Rehabil. 1996;77(11):1139-1143. [DOI] [PubMed] [Google Scholar]
- 6.Winters MV Blake CG Trost JS, et al. Passive versus active stretching of hip flexor muscles in ubjects with limited hip extension: A randomized clinical trial. Phys Ther. 2004;84(9):800-807. [PubMed] [Google Scholar]
- 7.Zeller BL McCrory JL Kibler WB Uhl TL. Differences in kinematics and electromyographic activity between men and women during the single-legged squat. Am J Sports Med. 2003;31(3):449-456. [DOI] [PubMed] [Google Scholar]
- 8.Kendall FP McCreary EK Provance PG Rodgers MM Romani W. Muscles, Testing and Function: with posture and pain. 4th Ed. Baltimore, MD: Williams & Wilkins; 1993. [Google Scholar]
- 9.Offierski CM MacNab I. Hip-spine syndrome. Spine. 1983;8(3):316-321. [DOI] [PubMed] [Google Scholar]
- 10.Endo Y Sakamoto M. Relationship between lower extremity tightness and star excursion balance test performance in junior high school baseball players. J Phys Ther Sci. 2014;26(5):661-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rodacki ALF Souza RM Ugrinowitsch C Cristopoliski F Fowler NE. Transient effects of stretching exercises on gait parameters of elderly women. Man Ther. 2009;14(2):167-172. [DOI] [PubMed] [Google Scholar]
- 12.Docherty CL Valovich McLeod TC Shultz SJ. Postural control deficits in participants with functional ankle instability as measured by the balance error scoring system. Clin J Sports Med. 2006;16(3):203-208. [DOI] [PubMed] [Google Scholar]
- 13.McGuine TA Greene JJ Best T Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sports Med. 2000;10(4):239-244. [DOI] [PubMed] [Google Scholar]
- 14.Nelson ME Fiatarone MA Morganti CM Trice I Greenberg RA Evans WJ. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures. A randomized controlled trial. JAMA. 1994;272(24):1909-1914. [DOI] [PubMed] [Google Scholar]
- 15.Söderman K Alfredson H Pietilä T Werner S. Risk factors for leg injuries in female soccer players: a prospective investigation during one out-door season. Knee Surg Sports Traumatol Arthrosc. 2001;9(5):313-321. [DOI] [PubMed] [Google Scholar]
- 16.Tropp H Ekstrand J Gillquist J. Factors affecting stabilometry recordings of single limb stance. Am J Sports Med. 1984;12(3):185-188. [DOI] [PubMed] [Google Scholar]
- 17.Bisson EJ McEwen D Lajoie Y Bilodeau M. Effects of ankle and hip muscle fatigue on postural sway and attentional demands during unipedal stance. Gait Posture. 2011;33(1):83-87. [DOI] [PubMed] [Google Scholar]
- 18.Gear WS. Effect of different levels of localized muscle fatigue on knee position sense. J Sports Sci Med. 2011;10(4):725-730. [PMC free article] [PubMed] [Google Scholar]
- 19.Gribble PA Hertel J. Effect of lower-extremity muscle fatigue on postural control. Arch Phys Med Rehabil. 2004;85(4):589-592. [DOI] [PubMed] [Google Scholar]
- 20.Gstöttner M Neher A Scholtz A Millonig M Lembert S Raschner C. Balance ability and muscle response of the preferred and nonpreferred leg in soccer players. Motor Control. 2009;13(2):218-231. [DOI] [PubMed] [Google Scholar]
- 21.Ribeiro F Mota J Oliveira J. Effect of exercise-induced fatigue on position sense of the knee in the elderly. Eur J Appl Physiol. 2006;99(4):379-385. [DOI] [PubMed] [Google Scholar]
- 22.Sotnikov POS. Primary sensory neurons in the central nervous system. Neurosci Behav Physiol. 2006;36(5):541-548. [DOI] [PubMed] [Google Scholar]
- 23.Voight ML Hardin JA Blackburn TA Tippett S Canner GC. The effects of muscle fatigue on and the relationship of arm dominance to shoulder proprioception. J Orthop Sports Phys Ther. 1996;23(6):348-352. [DOI] [PubMed] [Google Scholar]
- 24.Winter DA Patla AE Frank JS. Assessment of balance control in humans. Med Prog Technol. 1990;16(1-2):31-51. [PubMed] [Google Scholar]
- 25.Herter TM Scott SH Dukelow SP. Systematic changes in position sense accompany normal aging across adulthood. J NeuroEngineering Rehabil. 2014;11(1):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van der Wal J. The Architecture of the connective tissue in the musculoskeletal system—An often overlooked functional parameter as to proprioception in the locomotor apparatus. Int J Ther Massage Bodyw. 2009;2(4):9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bennell KL Hinman RS Metcalf BR, et al. Relationship of knee joint proprioception to pain and disability in individuals with knee osteoarthritis. J Orthop Res. 2003;21(5):792-797. [DOI] [PubMed] [Google Scholar]
- 28.Lephart SM Pincivero DM Giraldo JL Fu FH. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25(1):130-137. [DOI] [PubMed] [Google Scholar]
- 29.Miura K Ishibashi Y Tsuda E Okamura Y Otsuka H Toh S. The effect of local and general fatigue on knee proprioception. Arthrosc J Arthrosc Relat Surg. 2004;20(4):414-418. [DOI] [PubMed] [Google Scholar]
- 30.Riemann BL Lephart SM. The sensorimotor system, part II: The role of proprioception in motor control and functional joint stability. J Athl Train. 2002;37(1):80-84. [PMC free article] [PubMed] [Google Scholar]
- 31.Sjölander P Johansson H Djupsjöbacka M. Spinal and supraspinal effects of activity in ligament afferents. J Electromyogr Kinesiol. 2002;12(3):167-176. [DOI] [PubMed] [Google Scholar]
- 32.Sharma L Pai YC Holtkamp K Rymer WZ. Is knee joint proprioception worse in the arthritic knee versus the unaffected knee in unilateral knee osteoarthritis? Arthritis Rheum. 1997;40(8):1518-1525. [DOI] [PubMed] [Google Scholar]
- 33.Marieb E. N. Hoehn K. Human anatomy and physiology. 8th ed. San Francisco, CA: Pearson Benjamin Cummings; 2010. [Google Scholar]
- 34.Baker V Bennell K Stillman B Cowan S Crossley K. Abnormal knee joint position sense in individuals with patellofemoral pain syndrome. J Orthop Res. 2002;20(2):208-214. [DOI] [PubMed] [Google Scholar]
- 35.Beard DJ Kyberd PJ Fergusson CM Dodd CA. Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need for surgery? J Bone Joint Surg Br. 1993;75(2):311-315. [DOI] [PubMed] [Google Scholar]
- 36.Hurley MV. The effects of joint damage on muscle function, proprioception and rehabilitation. Man Ther. 1997;2(1):11-17. [DOI] [PubMed] [Google Scholar]
- 37.Sharma L Pai YC Holtkamp K Rymer WZ. Is knee joint proprioception worse in the arthritic knee versus the unaffected knee in unilateral knee osteoarthritis? Arthritis Rheum. 1997;40(8):1518-1525. [DOI] [PubMed] [Google Scholar]
- 38.Watt JR Jackson K Franz JR Dicharry J Evans J Kerrigan DC. Effect of a supervised hip flexor stretching program on gait in frail elderly patients. Phys Med Rehabil. 2011;3(4):330-335. [DOI] [PubMed] [Google Scholar]
- 39.Malai S Pichaiyongwongdee S Sakulsriprasert P. Immediate effect of hold-relax stretching of iliopsoas muscle on transversus abdominis muscle activation in chronic non-specific low back pain with lumbar hyperlordosis. J Med Assoc Thail. 2015;98 Suppl 5:S6-11. [PubMed] [Google Scholar]
- 40.Fletcher IM Jones B. The effect of different warm-up stretch protocols on 20 meter sprint performance in trained rugby union players. J Strength Cond Res. 2004;18(4):885-888. 10.1519/14493.1. [DOI] [PubMed] [Google Scholar]
- 41.McMillian DJ Moore JH Hatler BS Taylor DC. Dynamic vs. static-stretching warm up: the effect on power and agility performance. J Strength Cond Res. 2006;20(3):492-499. [DOI] [PubMed] [Google Scholar]
- 42.Moradi A Rajabi R Minoonejad H Aghaei M. The acute effect of static stretching of quadriceps, hamstrings and gastrocnemius muscles on knee joint position sense in football players. Phys Treat - Specif Phys Ther J. 2014;4(2):83-89. [Google Scholar]
- 43.Yamaguchi T Ishii K. Effects of static stretching for 30 seconds and dynamic stretching on leg extension power. J Strength Cond Res. 2005;19(3):677-683. [DOI] [PubMed] [Google Scholar]
- 44.Roberts JM Wilson K. Effect of stretching duration on active and passive range of motion in the lower extremity. Br J Sports Med. 1999;33(4):259-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sharman MJ Cresswell AG. Proprioceptive neuromuscular facilitation stretching: mechanisms and clinical implications. Sports Med. 2006;36(11):929-939. [DOI] [PubMed] [Google Scholar]
- 46.Marek SM. Cramer JT Fincher A L Massey LL Dangelmaier SM Purkayastha S Culbertson J Y. Acute effects of static and proprioceptive neuromuscular facilitation stretching on muscle strength and power output. J Athl Train. 2005; 40(2), 94–103. [PMC free article] [PubMed] [Google Scholar]
- 47.Youdas JW Haeflinger KM Kreun MK Holloway AM Kramer CM Hollman JH. The efficacy of two modified proprioceptive neuromuscular facilitation stretching techniques in subjects with reduced hamstring muscle length. Physiother Theory Pract. 2010;26(4):240-250. [DOI] [PubMed] [Google Scholar]
- 48.Page P. Current concepts in muscle stretching for exercise and rehabilitation. Int J Sports Phys Ther. 2012;7(1):109-119. [PMC free article] [PubMed] [Google Scholar]
- 49.Sun-Ik C Dong-Yeop L Ji-Heon H Jae-Ho Y Jin-Seop K. Effect of hold and relax technique on knee joint position awareness in normal adults. Indian J Sci Technol. 2015;8(19). [Google Scholar]
- 50.Manoel ME Harris-Love MO Danoff JV Miller TA. Acute effects of static, dynamic, and proprioceptive neuromuscular facilitation stretching on muscle power in women. J Strength Cond Res. 2008;22:1528–1534 [DOI] [PubMed] [Google Scholar]
- 51.American College of Sports Medicine. ACSM's Resource manual for guidelines for exercise testing and prescription. 9th ed Baltimore: Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 52.Vigotsky AD Lehman GJ Beardsley C, et al. The modified Thomas test is not a valid measure of hip extension unless pelvic tilt is controlled. Peer J. 2016; 4:e2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Edwards ES Yin-Liang L King JH Karduna AR. Joint position sense – There's an app for that. J Biomech 2016;49(14):3529-3533. [DOI] [PubMed] [Google Scholar]
- 54.Lyons S. M. Cordell J. Gossage J. Suprak D. N. San Juan J. G. Validity and reliability of an iPod touch in measuring knee joint position sense. [Abstract]. 2017. Retrieved from ISB 2017 Congress https://isbweb.org/activities/congresses
- 55.Hertel J Braham RA Hale SA Olmsted-Kramer LC. Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(3):131-137. [DOI] [PubMed] [Google Scholar]
- 56.Vafadar AK Côté JN Archambault PS. Sex differences in the shoulder joint position sense acuity: a cross-sectional study. BMC Musculoskelet Disord. 2015;16:273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gribble PA Hertel J. Considerations for normalizing measures of the Star Excursion Balance Test. Meas Phys Educ Exerc Sci. 2003;7(2):89–100. [Google Scholar]
- 58.Godges JJ Macrae H Longdon C Tinberg C Macrae PG. The effects of two stretching procedures on hip range of motion and gait economy. J Orthop Sports Phys Ther. 1989;10(9):350-357. [DOI] [PubMed] [Google Scholar]
- 59.Halbertsma JP Göeken LN. Stretching exercises: effect on passive extensibility and stiffness in short hamstrings of healthy subjects. Arch Phys Med Rehabil. 1994;75(9):976-981. [PubMed] [Google Scholar]
- 60.McHugh MP Magnusson SP Gleim GW Nicholas JA. Viscoelastic stress relaxation in human skeletal muscle. Med Sci Sports Exerc. 1992;24(12):1375-1382. [PubMed] [Google Scholar]
- 61.Möller M Ekstrand J Oberg B Gillquist J. Duration of stretching effect on range of motion in lower extremities. Arch Phys Med Rehabil. 1985;66(3):171-173. [PubMed] [Google Scholar]
- 62.Taylor DC Dalton JD Seaber AV Garrett WE. Viscoelastic properties of muscle-tendon units. The biomechanical effects of stretching. Am J Sports Med. 1990;18(3):300-309. [DOI] [PubMed] [Google Scholar]
- 63.Willy RW Kyle BA Moore SA Chleboun GS. Effect of cessation and resumption of static hamstring muscle stretching on joint range of motion. J Orthop Sports Phys Ther. 2001;31(3):138-144. [DOI] [PubMed] [Google Scholar]
- 64.Mills M Frank B Goto S, et al. Effect of restricted hip flexor muscle length on hip extensor muscle activity and lower extremity biomechanics in college-aged female soccer players. Int J Sports Phys Ther. 2015;10(7):946-954. [PMC free article] [PubMed] [Google Scholar]
- 65.Herda TJ Herda ND Costa PB Walter-Herda AA Valdez AM Cramer JT. The effects of dynamic stretching on the passive properties of the muscle-tendon unit. J Sports Sci. 2013;31(5):479-487. [DOI] [PubMed] [Google Scholar]
- 66.Gollhofer A Rapp W. Recovery of stretch reflex responses following mechanical stimulation. Eur J Appl Physiol. 1993;66(5):415-420. [DOI] [PubMed] [Google Scholar]
- 67.Gottlieb GL Agarwal GC. Response to sudden torques about ankle in man: myotatic reflex. J Neurophysiol. 1979;42(1 Pt 1):91-106. [DOI] [PubMed] [Google Scholar]
- 68.Friemert B Bach C Schwarz W Gerngross H Schmidt R. Benefits of active motion for joint position sense. Knee Surg Sports Traumatol Arthrosc. 2006;14(6):564-570. [DOI] [PubMed] [Google Scholar]
- 69.Miyahara Y Naito H Ogura Y Katamoto S Aoki J. Effects of proprioceptive neuromuscular facilitation stretching and static stretching on maximal voluntary contraction. J Strength Cond Res. 2013;27(1):195-201. [DOI] [PubMed] [Google Scholar]
- 70.Erden Z. [Is there any difference in joint position sense among different knee angles?]. Jt Dis Relat Surg. 2009;20(1):47-51. [PubMed] [Google Scholar]
- 71.Ghaffarinejad F Taghizadeh S Mohammadi F. Effect of static stretching of muscles surrounding the knee on knee joint position sense. Br J Sports Med. 2007;41(10):684-687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Larsen R Lund H Christensen R Røgind H Danneskiold-Samsøe B Bliddal H. Effect of static stretching of quadriceps and hamstring muscles on knee joint position sense. Br J Sports Med. 2005;39(1):43-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Torres R Duarte JA Cabri JM. An acute bout of quadriceps muscle stretching has no influence on knee joint proprioception. J Hum Kinet. 2012;34:33-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Björklund M Djupsjöbacka M Crenshaw AG. Acute muscle stretching and shoulder position sense. J Athl Train. 2006;41(3):270-274. [PMC free article] [PubMed] [Google Scholar]
- 75.Costa PB Graves BS Whitehurst M Jacobs PL. The acute effects of different durations of static stretching on dynamic balance performance: J Strength Cond Res. 2009;23(1):141-147. [DOI] [PubMed] [Google Scholar]
- 76.Handrakis JP Southard VN Abreu JM, et al. Static stretching does not impair performance in active middle-aged adults. J Strength Cond Res. 2010;24(3):825-830. [DOI] [PubMed] [Google Scholar]
- 77.Azeem Z Sharma R. Comparison of dynamic and static stretching on dynamic balance performance in recreational football players. Saudi J Sports Med. 2014;14(2):134. [Google Scholar]
- 78.Chatzopoulos D Galazoulas C Patikas D Kotzamanidis C. Acute effects of static and dynamic stretching on balance, agility, reaction time and movement time. J Sports Sci Med. 2014;13(2):403-409. [PMC free article] [PubMed] [Google Scholar]
- 79.Amiri-Khorasani M. Acute effects of different stretching methods on static and dynamic balance in female football players… [including commentary by Dawn T. Gulick]. Int J Ther Rehabil. 2015;22(2):68-73. [Google Scholar]
- 80.Lim K-I Nam H-C Jung K-S. Effects on hamstring muscle extensibility, muscle activity, and balance of different stretching techniques. J Phys Ther Sci. 2014;26(2):209-213. [DOI] [PMC free article] [PubMed] [Google Scholar]