Abstract
Introduction
Pseudomonas aeruginosa has the ability to acquire plasmids and other mobile genetic elements that confer resistance to antibiotics. Bacterial genes encoding different β-lactamases (bla), such as metallo-β-lactamases (MBLs) and extended-spectrum β-lactamases (ESBL), can confer resistance to multiple classes of β-lactam antibiotics.
Case presentation
An 83 year old female was admitted in 2012 to the Peruvian Naval Hospital, Centro Médico Naval ‘Cirujano Mayor Santiago Távara’ (CEMENA), in Lima, Peru. A midstream urine sample was collected and sent to the local CEMENA laboratory for routine urine culture. P. aeruginosa was isolated and initial antibiotic susceptibility testing showed it to be sensitive to imipenem. The clinicians started a course of meropenem, but the patient did not improve. After 5 days, a second urine culture was performed and a P. aeruginosa was isolated again, but this time the strain showed resistance to imipenem. The treatment course was changed to fosfomycin and the patient improved. Phenotypic and molecular laboratory testing to characterize the antibiotic resistance were performed, demonstrating the presence of both MBL and ESBL genes.
Conclusion
To our knowledge, this is the first report of a P. aeruginosa XDR clinical isolate that co-expresses an MBL (VIM-2), OXA-1 beta-lactamase and the ESBL (GES-1) in Peru. It is also the first report of a VIM carbapenemase in Peru.
Keywords: carbapenemase, metallo-β-lactamase
Introduction
Pseudomonas aeruginosa has been well recognized as a cause of nosocomial infection worldwide, principally in urinary tract infections, pneumonias and intra-abdominal infections [1]. Multi-drug resistant (MDR), extensively drug-resistant (XDR), and pan-drug resistant (PDR) bacterial infections have been associated with increased length of hospital stay, multiple morbidities, increased cost of hospitalization and high mortality rates ranging from 50 to 60 % [1–3]. Opportunistic species of the genus Pseudomonas have the ability to acquire foreign genetic materials, such as plasmids and other mobile genetic elements. Bacterial genes encoding different β-lactamases (bla), such as metallo-β-lactamases (MBLs) and extended-spectrum β-lactamases (ESBL), can confer resistance to multiple classes of β-lactam antibiotics.
MBLs are classified as Ambler class B beta-lactamases based on enzymatic activity that requires a metal ion co-factor to hydrolyze β-lactam antibiotics, including carbapenems. There are more than nine types of MBL, such as IMP, VIM, and NDM that have been reported worldwide including in Africa, Asia, Europe, and the Americas; while others like SPM and GIM have only circulated in specific countries such as Brazil and Germany [4]. We report here the first case of an extensively drug-resistant (XDR) Pseudomonas aeruginosa from an 83 year-old female in Lima, Peru that simultaneously expresses the VIM-2, GES-1 and OXA-1 beta-lactamases.
Case report
An 83 years old female was admitted in 2012 to the Peruvian Naval Hospital, Centro Médico Naval ‘Cirujano Mayor Santiago Távara’ (CEMENA), in Lima, Peru, with complaints of low back pain, vomiting and intestinal obstruction. The patient had a history of high blood pressure, type 2 diabetes mellitus, chronic renal disease and multiple urinary tract infections. In addition, she had a prolapsed bladder with a prior history of hysterectomy. At the time of admission, the patient was taking loperamide, amlodipine and ranitidine.
As part of her initial work-up, a midstream urine sample was collected and sent to the local CEMENA laboratory for routine urine culture. P. aeruginosa was isolated and initial antibiotic susceptibility testing showed it to be sensitive to imipenem. The clinicians started a course of meropenem at 500 mg IV q12h based on her renal function, but the patient did not improve. After 5 days, a second urine culture was performed, isolating P. aeruginosa that was now resistant to imipenem. She was then changed to renaldosed fosfomycin at 0.8 g IV q12h with noted improvement and clearance of her infection.
The second P. aeruginosa isolate was sent to the Naval Medical Research Unit No. 6 (NAMRU-6) in Callao, Peru (coded as MIS1668) for confirmation and further molecular characterization. The isolate was confirmed as P. aeruginosa by routine biochemical algorithms and antimicrobial susceptibility testing (AST) was performed using the automated Phoenix System (BD Diagnostics). MIC results were interpreted using the Clinical Laboratory Standards Institute guidelines (CLSI M100-S23) [5]. The isolate was found to be resistant to all antibiotics on the NMIC/ID-124 Phoenix panel (Table 1). Additional antibiotic susceptibilities were tested using the disk diffusion test (DDT) for colistin 10 µg, imipenem 10 µg, and ticarcillin–clavulanic acid 75/10 µg, with only sensitivity to colistin exhibited, thus meeting the criteria for an extensively drug-resistant (XDR) isolate according to the international guidelines [6].
Table 1. Antimicrobial susceptibility results.
| Antibiotic | MIC (µg ml−1)* | Interpretation† |
|---|---|---|
| Cefepime (FEP) | >16 | R |
| Ceftazidime (CAZ) | >16 | R |
| Meropenem (MEM) | >8 | R |
| Aztreonam (ATM) | >16 | R |
| Piperacillin–Tazobactam (TZP) | >64/4 | R |
| Tobramycin (NN) | >8 | R |
| Amikacin (AN) | >32 | R |
| Gentamicin (GM) | >8 | R |
| Levofloxacin (LVX) | >4 | R |
| Ciprofloxacin (CIP) | >2 | R |
| Imipenem (IPM) | 6 | R |
| Ticarcillin–Clavulanic acid (TIM) | 6 | R |
| Colistin (CL) | 15 | S |
*MIC: Minimum inhibitory concentration. Results for IPM, TIM and CL correspond to DDT (mm).
†Results obtained according CLSI2013. S, Susceptible; R, Resistant.
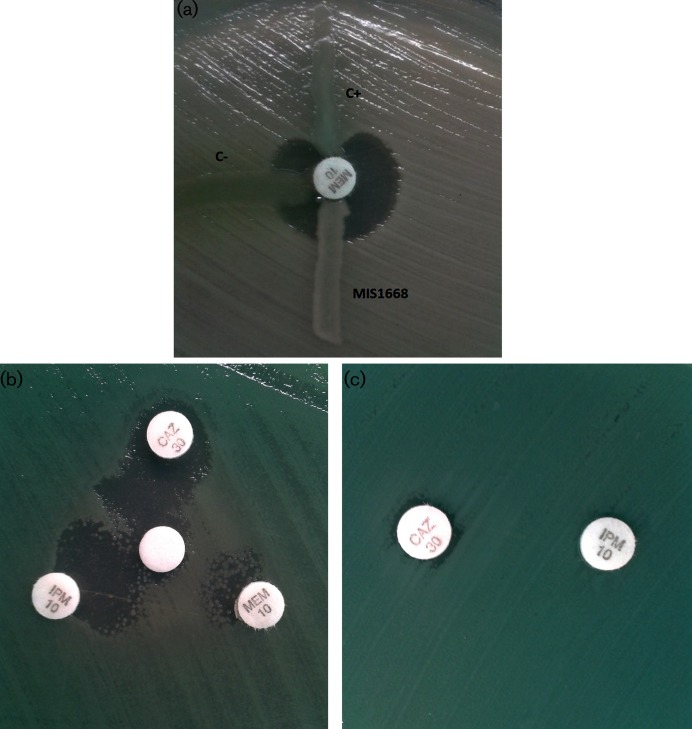
Since the MIS1668 isolate was carbapenem-resistant, we used the modified Hodge test (MHT) assay to screen for carbapenemase activity with Klebsiella pneumoniae ATCC 700603 [7]. A P. aeruginosa harboring the blaIMP-16 gene and P. aeruginosa ATCC 27853 were also used as positive and negative controls, respectively. Surprisingly, MIS1668 was determined to be negative for carbapenemase activity by MHT (Fig. 1a). Thus, we subsequently characterized the isolate using the disk diffusion synergy test (DDST) using EDTA disks with imipenem, meropenem and ceftazidime disks placed 15 mm center-to-center of each disk using the method described by Radice et al. [8]. Although MHT was negative, DDST showed synergy when subjecting the isolate to all disks (Fig. 1b), indicating the presence of an MBL enzyme being inhibited by chelation of the metal ion required for activity by the added EDTA. Synergy between imipenem and ceftazidime was observed only in the presence of the EDTA disk, a pattern similar to activity exhibited by the GES enzyme (Fig. 1c) [9].
Fig. 1.
(a). Modified Hodge test for Pseudomonas aeruginosa MIS1668. C− (negative control), Pseudomonas aeruginosa ATCC 27853. C+ (positive control), Pseudomonas aeruginosa blaIMP-16. (b). Double disk diffusion test using CAZ (ceftazidime disk), IPM (imipenem disk), MEM (meropenem disk) and EDTA 1M (white disk). (c). Double disk diffusion between CAZ (ceftazidime disk) and IPM (imipenem disk).
To further characterize the carbapenem-resistance activity, we performed a combination of multiplex PCR to detect bla genes with primer sets for the MBLs (IMP, VIM, NDM), serine-carbapenemase KPC, and for other beta-lactamases (TEM, SHV, OXA, GES, VEB, PER and CTX-M) using the primers listed in Table 2. The series of multiplex PCRs clearly demonstrated positive bands for blaVIM, blaGES and blaOXA-1-like from the P. aeruginosa MIS1668 isolate with band sizes consistent with those of the controls (Fig. 2). Subsequently, we used Sanger-based sequencing (Applied Biosystems) of the amplicons followed by blast search of the sequences to confirm the blaVIM-2, blaGES-1 and blaOXA-1 gene variants (Table S1 available in the online version of this paper). Finally, we used the Diversilab Rep-PCR method (Biomerieux) to detect homogenous DNA regions in the bacterial genome to the reference strain ATCC 27853 and found the MIS1668 isolate to be 94.1 % homologous.
Table 2. Primers used to detect bla genes.
| Gene | Primer | Sequence (5′–3′) |
|---|---|---|
| blaIMP | IMP-F | GGAATAGAGTGGCTTAAYTCTC |
| IMP-R | GGTTTAAYAAAACAACCACC | |
| blaVIM | VIM-F | GATGGTGTTTGGTCGCATA |
| VIM-R | CGAATGCGCAGCACCAG | |
| blaNDM-1 | NDM-F | GGTTTGGCGATCTGGTTTTC |
| NDM-R | CGGAATGGCTCATCACGATC | |
| blaKPC | KPC-F | CGTCTAGTTCTGCTGTCTTG |
| KPC-R | CTTGTCATCCTTGTTAGGCG | |
| blaTEM | TEM-F | CATTTCCGTGTCGCCCTTATTC |
| TEM-R | CGTTCATCCATAGTTGCCTGAC | |
| blaSHV | SHV-F | AGCCGCTTGAGCAAATTAAAC |
| SHV-R | ATCCCGCAGATAAATCACCAC | |
| blaOXA-1-like | OXA-1F | GGCACCAGATTCAACTTTCAAG |
| OXA-1R | GACCCCAAGTTTCCTGTAAGTG | |
| blaGES | GES-F | AGTCGGCTAGACCGGAAAG |
| GES-R | TTTGTCCGTGCTCAGGAT | |
| blaPER | PER-F | GCTCCGATAATGAAAGCGT |
| PER-R | TTCGGCTTGACTCGGCTGA | |
| blaVEB | VEB-F | CATTTCCCGATGCAAAGCGT |
| VEB-R | CGAAGTTTCTTTGGACTCTG | |
| blaCTX-M-1,2,9 | CTX-MA1 | SCSATGTGCAGYACCAGTAA |
| CTX-MA2 | CCGCRATATGRTTGGTGGTG | |
| blaCTX-M-8,25 | CTX825F | CGCTTTGCCATGTGCAGCACC |
| CTX825R | GCTCAGTACGATCGAGCC |
Fig. 2.
Agarose gel electrophoresis corresponding to PCR for β-lactamase genes. IMP: blaIMP positive control. VIM: blaVIM positive control. NDM: blaNDM positive control. KPC: blaKPC positive control. OXA: blaOXA-1-like positive control. SHV: blaSHV positive control. TEM: blaTEM positive control. CTX-M1,2,9 and CTX-M8,25: blaCTX-M positive controls. GES: blaGES positive control. ATCC 27853: Pseudomonas aeruginosa strain used as a negative control. 123 bp: Ladder of 123 base pars. 100 bp: Ladder of 100 base pars.
Discussion
Bacterial isolates simultaneously carrying multiple β-lactamases of different molecular classes, such as the ESBL (molecular class A or D) and MBL (molecular class B), are rare events. Such reports of P. aeruginosa isolates with genes coexisting and simultaneously encoding MBLs and ESBLs include: VIM-2 with CTX-M-2 in Uruguay, VIM-2 with OXA-10 in Croatia and IMP-1 with CTX-M-2 and IMP-1 with GES-1 in Brazil [10–12]. Also there is one report of the coexistence of VIM-2 and GES-1 in Argentina [13] within a P. aeruginosa strain very similar to the strain isolated in this case, indicating that these resistance factors could have originated in South American countries.
Although treatment efficacy for MBL in vivo remains unknown and carbapenems could still have some activity, in this case meropenem treatment clinically failed [14, 15]. It is also possible that this P. aeruginosa isolate has resistance mechanisms other than beta-lactamases, such as efflux pumps, that may be contributing to its carbapenem resistance. However, it has been shown in hospitals in Belgium that all P. aeruginosa isolates expressing VIM-2 showed high levels of cross resistance to both imipenem and meropenem as in this case [16]. However, this patient was successfully treated with fosfomycin, which works to disrupt the first step in the biosynthesis of the bacterial cell wall by the formation of the peptidoglycan precursor uridine diphosphate N-acetylmuramic acid [17]. Although there is some experience in using fosfomycin in the treatment of MDR urinary tract infections, there is less so in more invasive or systemic infection [18]. Given the ability of P. aeruginosa to easily acquire resistance to fosfomycin without a cost to its overall fitness, it would be cautious to avoid treating systemically ill patients with fosfomycin monotherapy until there is more clinical outcome data available [19, 20].
Although the MIS1668 isolate harbors a blaVIM gene encoding a carbapenemase, as detected by molecular tests, the isolate was negative for carbapenemase activity by MHT. In our case, the use of EDTA to chelate the zinc ions to allow inhibition of the enzyme demonstrated the carbapenemase phenotype but showed the importance of additional phenotypic tests in screening for a MBL and the need for molecular confirmatory testing [21].
The results of the Diversilab rep-PCR based comparison revealed that the P. aeruginosa presented here showed a 94 % homology with the reference carbapenem-sensitive ATCC 27853 strain, and indicate that this isolate has picked up an integron or possibly a gene cassette over time with a relatively conserved chromosome [22]. Although the initial isolate that was reportedly sensitive to imipenem was not saved for further testing, we presume that the isolate probably acquired genes necessary for carbapenem resistance through the sharing of plasmids at the time of treatment. However, it would be safe to assume that the antimicrobial pressure over time most probably led to the sharing of transposons between bacteria, leading to the current isolate within this particular hospital. This could be further investigated by comparing other carbapenemase-resistant P. aeruginosa isolates within Peru to see if these genes are indeed conserved and prevalent.
To our knowledge, this is the first report of a P. aeruginosa XDR clinical isolate that co-expresses an MBL (VIM-2), OXA-1, and an ESBL gene (GES-1) in Peru. It is also the first report of a VIM carbapenemase in Peru although this has been described in other countries in South America. Given its presence in other neighboring countries, the full extent of MBL prevalence in Peru is unknown and is a topic of targeted surveillance for our program and others. Most infection control programs at large hospitals in Peru are managed by professionals with strong clinical backgrounds but with limited resources to provide effective infection control monitoring and limited laboratory capability to reliably detect increasing bacterial resistance rates. Developing and strengthening reliable surveillance systems to identify isolates with genes encoding antibiotic resistance is essential in developing effective infection control polices, informing antimicrobial stewardship practices and improving overall clinical care. To further understand how these resistance mechanisms disseminate through mobile genetic elements and to develop novel interventions to counter these undesirable gene flows, robust surveillance systems are needed among laboratories in developing countries. This case illustrates the priority to establish these enhanced surveillance networks and to implement them in more resource-limited areas where multi-drug-resistant isolates may be developing and circulating.
Funding information
This work was funded by the Armed Forces Health Surveillance Global Emerging Infections Surveillance Program. Grant number 20160390182, Antimicrobial Resistance.
Acknowledgements
The views expressed in this article are those of the author and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense or the U.S. Government. Some of the authors of this presentation are staff working for the Department of Defense of the United States and this work has been prepared as part of their official duties. Title 17 U.S.C. §105 provides that ‘Copyright protection under this title is not available for any work of the United States Government.’ Title 17 U.S.C. §101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Ethical statement
This study was reviewed and approved by the Institutional Review Board at the U.S. Naval Medical Research Unit No. 6 in Peru and was reviewed and approved by the ethics board at each participating institution.
Supplementary Data
Footnotes
Abbreviations: AST, Antimicrobial susceptibility testing; DDST, Disk diffusion synergy test; DDT, Disk diffusion test; ESBL, Extended-spectrum β-lactamases; MBL, Metallo-β-lactamase; XDR, Extensively drug-resistant; IMP, Imipenemase; VIM, Verona integron-encoded metallo-β-lactamase; NDM, New Delhi metallo-β-lactamase; SPM, Sao Paulo metallo-β-lactamase; GIM, German imipenemase; KPC, Klebsiella pneumoniae carbapenemase; TEM, Temoneira; SHV, Sulfhydryl variable; OXA, Oxacillinase; GES, Guiana extended spectrum; VEB, Vietnamese; PER, Pseudomonas extended resistance; CTX-M, Cefotaximase.
One supplementary table is available with the online version of this article.
References
- 1.Tang PC, Lee CC, Li CW, Li MC, Ko WC, et al. Time-to-positivity of blood culture: an independent prognostic factor of monomicrobial Pseudomonas aeruginosa bacteremia. J Microbiol Immunol Infect. 2017;50:486–493. doi: 10.1016/j.jmii.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Kang CI, Kim SH, Kim HB, Park SW, Choe YJ, et al. Pseudomonas aeruginosa bacteremia: risk factors for mortality and influence of delayed receipt of effective antimicrobial therapy on clinical outcome. Clin Infect Dis. 2003;37:745–751. doi: 10.1086/377200. [DOI] [PubMed] [Google Scholar]
- 3.Hong DJ, Bae IK, Jang IH, Jeong SH, Kang HK, et al. Epidemiology and characteristics of metallo-β-lactamase-producing Pseudomonas aeruginosa. Infect Chemother. 2015;47:81–97. doi: 10.3947/ic.2015.47.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cornaglia G, Giamarellou H, Rossolini GM. Metallo-β-lactamases: a last frontier for β-lactams? Lancet Infect Dis. 2011;11:381–393. doi: 10.1016/S1473-3099(11)70056-1. [DOI] [PubMed] [Google Scholar]
- 5.Clinical and Laboratory Standards Institute . Clinical and Laboratory Standards Institute: [Document] Wayne, PA: Clinical and Laboratory Standards Institute; 2013. [Google Scholar]
- 6.Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 7.Pasteran F, Veliz O, Rapoport M, Guerriero L, Corso A. Sensitive and specific modified Hodge test for KPC and metallo-β- lactamase detection in Pseudomonas aeruginosa by use of a novel indicator strain, Klebsiella pneumoniae ATCC 700603. J Clin Microbiol. 2011;49:4301–4303. doi: 10.1128/JCM.05602-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Radice M, Marín M, Giovanakis M, Vay C, Almuzara M, et al. Antimicrobial susceptibility testing in clinically relevant non-fermenting Gram-negative bacilli: recommendations from the Antimicrobial Agents Subcommittee of the Sociedad Argentina de Bacteriología, Micología y Parasitología Clínicas, Asociación Argentina de Microbiología. Rev Argent Microbiol. 2011;43:136–153. doi: 10.1590/S0325-75412011000200012. [DOI] [PubMed] [Google Scholar]
- 9.Pellegrino FL, Netto-dos Santos KR, Riley LW, Moreira BM. BlaGES carrying Pseudomonas aeruginosa isolates from a public hospital in Rio de Janeiro, Brazil. Braz J Infect Dis. 2006;10:251–253. doi: 10.1590/S1413-86702006000400007. [DOI] [PubMed] [Google Scholar]
- 10.Ingold AJ, Castro M, Nabón A, Borthagaray G, Márquez C. VIM-2 metallo-β-lactamase gene detection in a class 1 integron associated to blaCTX-M-2 in a Pseudomonas aeruginosa clinical isolate in Uruguay: first communication. Rev Argent Microbiol. 2011;43:198–202. doi: 10.1590/S0325-75412011000300004. [DOI] [PubMed] [Google Scholar]
- 11.Sardelic S, Bedenic B, Colinon-Dupuich C, Orhanovic S, Bosnjak Z, et al. Infrequent finding of metallo-β-lactamase VIM-2 in carbapenem-resistant Pseudomonas aeruginosa strains from Croatia. Antimicrob Agents Chemother. 2012;56:2746–2749. doi: 10.1128/AAC.05212-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Polotto M, Casella T, de Lucca Oliveira MG, Rúbio FG, Nogueira ML, et al. Detection of P. aeruginosa harboring blaCTX-M-2, blaGES-1 and blaGES-5, blaIMP-1 and blaSPM-1 causing infections in Brazilian tertiary-care hospital. BMC Infect Dis. 2012;12:176. doi: 10.1186/1471-2334-12-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pasteran F, Faccone D, Petroni A, Rapoport M, Galas M, et al. Novel variant blaVIM-11 of the metallo-β-lactamase blaVIM family in a GES-1 extended-spectrum-β-lactamase-producing Pseudomonas aeruginosa clinical isolate in Argentina. Antimicrob Agents Chemother. 2005;49:474–475. doi: 10.1128/AAC.49.1.474-475.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bellais S, Mimoz O, Léotard S, Jacolot A, Petitjean O, et al. Efficacy of β-lactams for treating experimentally induced pneumonia due to a carbapenem-hydrolyzing metallo-β-lactamase-producing strain of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2002;46:2032–2034. doi: 10.1128/AAC.46.6.2032-2034.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Monogue ML, Abbo LM, Rosa R, Camargo JF, Martinez O, et al. In vitro discordance with in vivo activity: humanized exposures of ceftazidime-avibactam, aztreonam, and tigecycline alone and in combination against New Delhi metallo-β-lactamase-producing Klebsiella pneumoniae in a murine lung infection model. Antimicrob Agents Chemother. 2017;61:e00486-17. doi: 10.1128/AAC.00486-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deplano A, Rodriguez-Villalobos H, Glupczynski Y, Bogaerts P, Allemeersch D, et al. Emergence and dissemination of multidrug resistant clones of Pseudomonas aeruginosa producing VIM-2 metallo-β-lactamase in Belgium. Euro Surveill. 2007;12:E070118.2. doi: 10.2807/esw.12.03.03114-en. [DOI] [PubMed] [Google Scholar]
- 17.Kahan FM, Kahan JS, Cassidy PJ, Kropp H. The mechanism of action of fosfomycin (phosphonomycin) Ann N Y Acad Sci. 1974;235:364–386. doi: 10.1111/j.1749-6632.1974.tb43277.x. [DOI] [PubMed] [Google Scholar]
- 18.Neuner EA, Sekeres J, Hall GS, van Duin D. Experience with fosfomycin for treatment of urinary tract infections due to multidrug-resistant organisms. Antimicrob Agents Chemother. 2012;56:5744–5748. doi: 10.1128/AAC.00402-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Falagas ME, Kastoris AC, Karageorgopoulos DE, Rafailidis PI. Fosfomycin for the treatment of infections caused by multidrug-resistant non-fermenting Gram-negative bacilli: a systematic review of microbiological, animal and clinical studies. Int J Antimicrob Agents. 2009;34:111–120. doi: 10.1016/j.ijantimicag.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 20.Walsh CC, McIntosh MP, Peleg AY, Kirkpatrick CM, Bergen PJ. In vitro pharmacodynamics of fosfomycin against clinical isolates of Pseudomonas aeruginosa. J Antimicrob Chemother. 2015;70:3042–3050. doi: 10.1093/jac/dkv221. [DOI] [PubMed] [Google Scholar]
- 21.Pasteran F, Mendez T, Guerriero L, Rapoport M, Corso A. Sensitive screening tests for suspected class A carbapenemase production in species of Enterobacteriaceae. J Clin Microbiol. 2009;47:1631–1639. doi: 10.1128/JCM.00130-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Erickson KE, Otoupal PB, Chatterjee A. Gene expression variability underlies adaptive resistance in phenotypically heterogeneous bacterial populations. ACS Infect Dis. 2015;1:555–567. doi: 10.1021/acsinfecdis.5b00095. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.