Abstract.
We conducted a nationally representative cross-sectional study of 875 health-care facilities (HCFs) to determine water, sanitation, and health-care waste disposal service levels in Bangladesh for doctors, staff, and patients/caregivers in 2013. We calculated proportions and prevalence ratios to compare urban versus rural and government versus other HCFs. We report World Health Organization (WHO)-defined basic HCF service levels. The most common HCF was nongovernmental private (80%, 698/875), with an average of 25 beds and 12 admissions per day. There was an improved water source inside the HCF for doctors (79%, 95% confidence intervals [CI]: 75, 82), staff (59%, 95% CI: 55, 64), and patients/caregivers (59%, 95% CI: 55, 63). Improved toilets for doctors (81%, 95% CI: 78, 85) and other staff (73%, 95% CI: 70, 77) were more common than for patients/caregivers (54%, 95% CI: 50, 58). Forty-three percentage (434/875) of HCFs had no disposal method for health-care waste. More urban than rural and more government than other HCFs had an improved water source on the premises and improved toilets for staff. WHO-defined basic service levels were detected in > 90% of HCFs for drinking water, among 46–77% for sanitation, and 68% for handwashing at point of care but 26% near toilets. Forty-seven percentage of HCFs attained basic health-care waste management service levels. Patient/caregiver access to water, sanitation, and hygiene facilities is inadequate in many HCFs across Bangladesh. Improving facilities for this group should be an integral part of accreditation.
INTRODUCTION
As part of Sustainable Development Goal 3.8, access to universal health coverage is a global priority whereby people are encouraged to seek health-care facility (HCF)–based health services with an emphasis on service quality (http://www.who.int/servicedeliverysafety/areas/qhc/quality-uhc/en/). Health-care facilities in low- and middle-income countries (LMICs) are often the focal point of epidemics and emerging infectious diseases, including those from antimicrobial-resistant organisms.1,2 Improving HCF water, sanitation and hygiene (WASH) facilities; environmental cleanliness; and infection control programs can reduce disease transmission, provide a safe environment, and support delivery of quality services that are people-centered.
Providing policy makers with data that represent a national overview can highlight areas for attention, to advocate for HCF funding. A nationally representative study of HCFs conducted in Bangladesh in 2014 that focused on service provision reported that a small number of WASH indicators3 and other studies examining features of HCFs that impact nosocomial infections in Bangladesh have concentrated on government and tertiary care HCFs.4–6 Recently, the WHO developed a WASH ladder for HCFs and proposed survey questions for future national HCF assessment.7
To guide policy to improve service delivery in HCFs, we analyze representative cross-sectional data from Bangladesh on water and sanitation facilities and health-care waste management practices. This builds on a recent report on HCF handwashing facilities and practices.8 An observational study in three public tertiary care HCFs highlighted the high frequency of family caregivers providing patient care and their poor handwashing practices,5 suggesting that for Bangladesh and potentially other LMICs, facilities for this patient care group should also be considered during policy formulation. We report WASH facilities for patients, family caregivers, ward staff, nurses and doctors, and health-care waste management. We examine differences among rural versus urban and among government versus other (independent, private, and nongovernmental organization [NGO]) HCFs to inform resource allocation and as baseline for future HCF monitoring efforts.
MATERIALS AND METHODS
Sampling method.
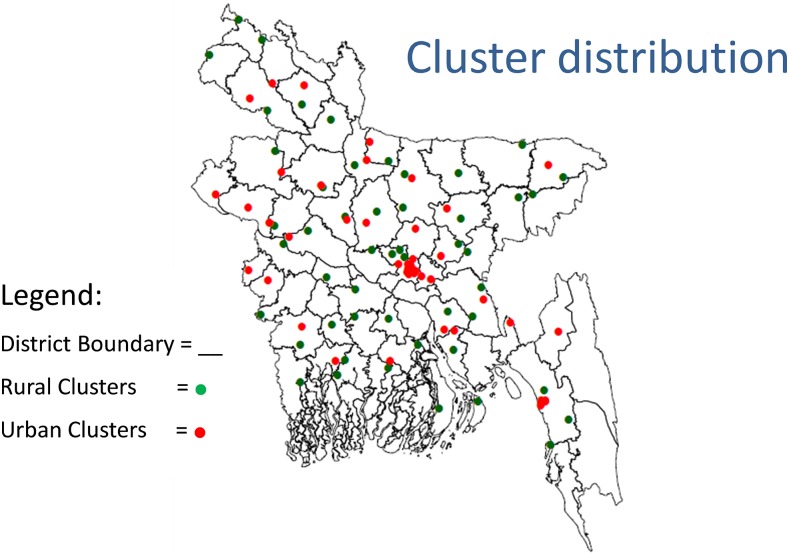
This study comprised the HCF component of a five population group (HCFs, households, schools, restaurants/street food vendors, and traditional birth attendants) survey on WASH facilities, practices, and knowledge.9 We randomly selected 50 rural and 50 urban clusters using probability proportional to size population sampling (Figure 1).9 From each cluster, we sampled nine HCFs each from the initial 75 clusters and eight HCFs from each of the remaining 25 clusters from July to October 2013. An HCF was eligible if it provided on-site overnight inpatient health-care service, had at least one patient admitted on the day of interview and the facility head or delegate gave informed consent for participation in the study.
Figure 1.
Distribution of geographic clusters. This figure appears in color at www.ajtmh.org.
Data collection.
A trained field team collected data during unannounced visits using face-to-face interviews and environmental spot checks on practices, facilities (water supply type, location, and cleanliness; toilet type [including separate male and female access], location, numbers; internal and external HCF cleanliness; and health-care waste management), knowledge, and population characteristics using standardized questionnaires. In each HCF, we interviewed the head administrator or a physician who they nominated. From the pediatric ward (or adult female ward if there was no pediatric ward), field staff selected a nurse and a ward staff member (“ward boy” or female assistant, ayah) available at the time of survey for interview. A patient or their family caregiver on the ward who was willing to consent was interviewed. The team recorded the number of beds and number of patients admitted on the survey day. Trained field staff collected data on tablets and smart phones and uploaded to central servers every 10 days.
Sample size calculation.
We determined sample size powered to compare differences between rural and urban areas. We assumed a design effect of 12.0 (using a conservative high-level intra-cluster correlation of 0.45, based on previous household studies), power of 80%, and α of 0.05, assumed a frequency of 50% for soap and water present at a convenient handwashing location after defecation, a minimum detectable difference of 10% between rural and urban areas, and estimated that we needed 864 HCFs; therefore, we sampled 875. We intentionally over-sampled from urban areas to allow robust urban–rural comparisons.
Data analysis.
We report proportions, weighted for estimated rural and urban clusters, to represent national HCF estimates. We provide descriptive statistics for facilities for three population groups; doctors, nurses/other staff, and patients/caregivers. We report medians and interquartile ranges (IQR) for continuous variables that were skewed. We estimated prevalence ratios (PRs) and 95% confidence intervals (95% CI) to compare urban versus rural and government versus other HCFs using Poisson regression controlling for clustering.
We applied the following definitions: WHO/United Nations International Children’s Emergency Fund (UNICEF) Joint Monitoring Program for Water Supply and Sanitation categories for improved water source and improved toilet10; shallow tube wells as those < 250-feet deep; health-care waste as cotton, cloth, bandages, gloves, sanitary pads, syringes, bottles, medicine foils, plastic saline packets, blood/urine/stool/collection tubes used in clinical settings, and placentas.
We calculated the frequency of HCFs that provided basic, limited, and unimproved service levels.7 Detailed data on handwashing facilities and practices from the surveyed HCFs have been published elsewhere8; these data were extracted, where relevant, to summarize health-care hand hygiene service levels. Based on the WHO service levels,7 we summarized HCF characteristics for water supply, sanitation, hand hygiene,8 and health-care waste management adapting the survey indicators to those suggested by WHO.7
Ethical considerations.
Field workers obtained written informed consent from HCF administrators, staff members, patients, and family caregivers. The scientific research protocol for the study was reviewed and approved by an institutional review board at the International Centre for Diarrhoeal Disease Research, Bangladesh.
RESULTS
Health-care facility characteristics.
The 100 clusters included 54 of 64 districts from seven of eight Bangladesh divisions (Figure 1). Among the 875 HCFs, the most common facility was small nongovernmental private HCFs, with a median of 17 (IQR: 11, 26) beds and seven (IQR: 3, 13) admissions per day, sampled in both urban (367/443, 83%) and rural areas (331/432, 76%; Table 1). Among government facilities, subdistrict HCFs comprised 10% with a median of 43 (IQR: 31, 50) beds and 30 (IQR:19, 40) admissions per day (Table 1). Medical college/specialized HCFs (private, for profit hospitals with a teaching facility) provide the largest total number of beds of those in surveyed HCFs. There were 17,128 (61%, 95% CI: 60, 62) beds provided by these facilities of the 28,039 among all surveyed HCFs and 8,335 (51%, 95% CI: 50, 52) admissions among the total 16,457 admissions on survey day (data not shown). There were some notable variations in HCF size by category for urban and rural settings with “independent, private, and NGO” facilities more common in urban areas (PR 1.13, 95% CI: 1.07, 1.21). There were significantly more private, nongovernmental HCFs (PR 1.09, 95% CI: 1.02, 1.17) and NGO facilities (PR 2.36, 95% CI: 1.14, 4.88) in urban than rural areas, contrasting with a lower frequency of urban subdistrict-level facilities (PR 0.34, 95% CI: 0.21, 0.53; Table 1), as reported previously.8
Table 1.
HCF characteristics, Bangladesh, 2013
| Indicator | Total | Rural | Urban | No. beds | No. daily admissions |
|---|---|---|---|---|---|
| n (%) | Median (IQR) | ||||
| All HCFs | 875 | 432 | 443 | 20 (12, 32) | 8 (4, 19) |
| Government | 136 (15) | 89 (21) | 47 (11)* | 49 (31, 57) | 33 (18, 52) |
| Medical college/specialized | 3 (0) | 0 (0) | 3 (1) | 86 (16, 123) | 18 (2, 90) |
| Maternal child welfare centers | 15 (2) | 7 (2) | 8 (2) | 20 (16, 26) | 6 (4, 10) |
| District level | 26 (3) | 14 (3) | 12 (3) | 108 (100, 138) | 133 (96, 172) |
| Subdistrict level | 90 (10) | 67 (15) | 23 (5)* | 43 (31, 50) | 30 (19, 40) |
| Union subcenters | 2 (0) | 1 (0) | 1 (0) | 15 (10, 19) | 3 (1, 5) |
| Other | 739 (85) | 343 (79) | 396 (89) | 17 (11, 27) | 7 (3, 16) |
| Medical college/specialized | 7 (1) | 2 (0) | 5 (1) | 350 (111, 586) | 107 (66, 239) |
| Private | 698 (80) | 331 (76) | 367 (83)* | 17 (11, 26) | 7 (3, 13) |
| Nongovernmental organization | 34 (4) | 10 (2) | 24 (5)* | 14 (10, 20) | 5 (3, 9) |
IQR = interquartile ranges.
P < 0.05 for rural vs. urban; some columns do not add to 100% because of rounding.
Drinking water and toilet facilities.
Facilities for patients/caregivers were often poor and usually less common than for hospital staff, for example, for an improved water source and improved toilets (Table 2). Significantly more urban than rural HCFs had improved drinking water inside the premises; for doctors (PR 1.09, 95% CI: 1.02, 1.17), other staff (PR 1.31, 95% CI: 1.15, 1.51), patients/caregivers (PR 1.34, 95% CI: 1.18, 1.53; Table 2). The urban–rural differences were similarly observed for improved toilets for doctors (PR 1.16, 95% CI: 1.06, 1.28) and other staff (PR 1.17, 95% CI: 1.06, 1.30; Table 2).
Table 2.
Observed* HCF drinking water and toilet facilities by health-care facility category, Bangladesh, 2013
| HCF category | ||||||||
|---|---|---|---|---|---|---|---|---|
| All | Urban | Rural | PR† (95% CI) | Government | Other‡ | PR† (95% CI) | ||
| n (%§) N = 875 | 95% CI | n (%) N = 443 | n (%) N = 432 | n (%) N = 136 | n (%) N = 739 | |||
| For doctors | ||||||||
| Drinking water | ||||||||
| No water source | 2 (0.4) | −0.2, 1.0 | 0 (0) | 2 (0.5) | – | 2 (0.3) | 0 (0) | – |
| Improved water source | 854 (98) | 96, 99 | 434 (98) | 420 (98) | 1.00 (0.98, 1.02) | 132 (97) | 722 (98) | 1.00 (0.96, 1.02) |
| Located inside HCF | 721 (79) | 75, 82 | 386 (87) | 335 (78) | 1.09 (1.02, 1.17)‖ | 87 (64) | 634 (86) | 0.76 (0.67, 0.85) |
| Toilets | ||||||||
| None per HCF reporting | 103 (14) | 11, 17 | 38 (9) | 65 (15) | 0.51 (0.28, 0.94) | 1 (0.7) | 102 (14) | 0.05 (0.01, 0.36) |
| Improved toilet | 750 (81) | 78, 85 | 404 (91) | 346 (80) | 1.16 (1.06, 1.28) | 135 (99) | 615 (83) | 1.23 (1.15, 1.31) |
| For other staff | ||||||||
| Drinking water | ||||||||
| No water source | 22 (3) | 2, 6 | 8 (2) | 14 (3) | 0.53 (0.20, 1.43) | 2 (1) | 20 (3) | 0.49 (0.12, 2.05) |
| Improved water source | 611 (76) | 72, 80 | 275 (62) | 336 (78) | 0.82 (0.69, 0.98) | 123 (90) | 488 (66) | 1.32 (1.20, 1.46) |
| Located inside HCF | 596 (59) | 55, 64 | 350 (79) | 246 (57) | 1.31 (1.15, 1.51) | 49 (36) | 547 (74) | 0.51 (0.41, 0.64) |
| Toilets | ||||||||
| None per HCF reporting | 228 (29) | 26, 33 | 97 (22) | 131 (30) | 0.65 (0.49, 0.86) | 3 (2) | 225 (30) | 0.07 (0.02, 0.21) |
| Improved toilet | 675 (73) | 70, 77 | 362 (82) | 313 (72) | 1.17 (1.06, 1.30) | 134 (99) | 541 (73) | 1.39 (1.29, 1.47) |
| For patients/caregivers | ||||||||
| Drinking water | ||||||||
| No water source | 29 (4) | 2, 5 | 12 (3) | 17 (4) | 0.71 (0.29, 1.71) | 5 (4) | 24 (3) | 1.06 (0.37, 3.02) |
| Improved water source | 624 (78) | 74, 81 | 281 (63) | 343 (79) | 0.82 (0.70, 0.97) | 125 (92) | 499 (68) | 1.31 (1.19, 1.45) |
| Located inside HCF | 600 (59) | 55, 63 | 356 (80) | 244 (56) | 1.34 (1.18, 1.53) | 43 (32) | 557 (75) | 0.44 (0.34, 0.57) |
| Toilets | ||||||||
| None per HCF reporting | 67 (7) | 3, 11 | 25 (6) | 42 (10) | 0.52 (0.28, 0.98) | 1 (0.7) | 66 (9) | 0.07 (0.01, 0.48) |
| Improved toilet | 465 (54) | 50, 58 | 232 (52) | 233 (54) | 0.94 (0.80, 1.11) | 53 (39) | 412 (56) | 0.69 (0.57, 0.84) |
CI = confidence interval; HCF = health-care facility; PR = prevalence ratio.
Detected by spot checks.
PRs and 95% CI were calculated using Poisson regression models that included government vs. other and urban vs. rural location where PR for urban vs. rural < 1 indicates lower prevalence in urban settings; PR < 1 for government vs. other indicates lower prevalence in government HCFs.
Others; independent, private, and nongovernmental organization HCFs.
Weighted percentages for all HCFs.
Differences between rural and urban HCFs or government and other HCFs with P < 0.05 shown in bold.
In government HCFs, an improved water source for drinking inside the premises was significantly less common than in other HCFs but conversely for improved toilets (Table 2).
Environmental cleanliness and health-care waste management.
Between one and two-thirds of HCFs had poor cleanliness, evident as paper or food waste, excrement, or vermin around or within the facilities. The field team observed contamination with human or animal feces at or in 25% (95% CI: 21, 29) of toilets, 10% (95% CI: 7, 12) of HCF grounds, 4% (95% CI: 2, 6) of water sources, 2% (95% CI: 0, 5) of kitchens, and 1% (95% CI: 0, 1) of wards (Table 3). Rural HCF facilities were generally dirtier than urban. For example, the outside areas of urban HCFs significantly less commonly had paper or food waste than rural (PR 0.86, 95% CI: 0.76, 0.97) and urban water sources less commonly were contaminated with feces (PR 0.34, 95% CI: 0.12, 0.95; Table 3). For almost all indicators, government HCFs were significantly less clean than other HCFs (Table 3).
Table 3.
Observed* HCF cleanliness and health-waste management by health-care facility category, Bangladesh, 2013
| HCF category | ||||||||
|---|---|---|---|---|---|---|---|---|
| All | Urban | Rural | PR† (95% CI) | Government | Other‡ | PR† (95% CI) | ||
| n (%§) | 95% CI | n (%) | n (%) | n (%) | n (%) | |||
| HCF Cleanliness | ||||||||
| Wards and rooms with: | N = 875 | – | N = 443 | N = 432 | – | N = 136 | N = 739 | – |
| Paper or food waste | 376 (48) | 44, 52 | 163 (37) | 213 (49) | 0.81 (0.69, 0.95)‖ | 101 (74) | 275 (37) | 1.92 (1.63, 2.26) |
| Sputum or betel nut waste | 152 (21) | 17, 24 | 59 (13) | 93 (22) | 0.79 (0.56, 1.09) | 73 (54) | 79 (11) | 4.80 (3.58, 6.43) |
| Human or animal feces | 6 (1) | 0, 1 | 3 (1) | 3 (1) | 1.48 (0.21, 10.45) | 4 (3) | 2 (0.3) | 11.7 (1.59, 86.7) |
| Animals or insects, live or dead | 26 (4) | 2, 6 | 8 (2) | 18 (4) | 0.54 (0.23, 1.25) | 12 (9) | 14 (2) | 4.18 (2.01, 8.69) |
| Toilets with: | N = 875 | – | N = 443 | N = 432 | – | N = 136 | N = 739 | – |
| Paper or food waste | 264 (34) | 30, 38 | 112 (25) | 152 (35) | 0.81 (0.64, 1.00) | 84 (62) | 180 (24) | 2.43 (2.02, 2.93) |
| Sputum or betel nut waste | 146 (20) | 17, 24 | 53 (12) | 93 (22) | 0.71 (0.48, 1.06) | 72 (53) | 74 (10) | 4.96 (3.64, 6.77) |
| Human or animal feces | 196 (25) | 21, 29 | 85 (19) | 111 (26) | 0.89 (0.65, 1.22) | 76 (56) | 120 (16) | 3.37 (2.69, 4.21) |
| Animals or insects, live or dead | 24 (3) | 1, 4 | 13 (3) | 11 (3) | 1.42 (0.67, 3.01) | 10 (7) | 14 (2) | 4.15 (1.94, 8.90) |
| Water sources¶ with: | N = 875 | N = 443 | N = 432 | N = 136 | N = 739 | |||
| Paper or food waste | 339 (44) | 40, 49 | 141 (32) | 198 (46) | 0.75 (0.62, 0.92) | 92 (68) | 247 (33) | 1.92 (1.60, 2.30) |
| Sputum or betel nut waste | 54 (7) | 4, 10 | 21 (5) | 33 (8) | 0.73 (0.40, 1.34) | 21 (15) | 33 (4) | 3.26 (1.97, 5.38) |
| Human or animal feces | 24 (4) | 2, 6 | 6 (1) | 18 (4) | 0.34 (0.12, 0.95) | 6 (4) | 18 (2) | 1.51 (0.61, 3.79) |
| Animals or insects, live or dead | 10 (1) | 0, 2 | 5 (1) | 5 (1) | 0.92 (0.29, 2.94) | 1 (0.7) | 9 (1.2) | 0.59 (0.08, 4.69) |
| Outside on HCF grounds with: | N = 875 | N = 443 | N = 432 | – | N = 136 | N = 739 | – | |
| Paper or food waste | 596 (73) | 69, 77 | 275 (62) | 321 (74) | 0.86 (0.76, 0.97) | 117 (86) | 479 (65) | 1.29 (1.17, 1.42) |
| Sputum or betel nut waste | 204 (27) | 23, 31 | 83 (19) | 121 (28) | 0.78 (0.59, 1.03) | 75 (55) | 129 (17) | 3.01 (2.86, 3.85) |
| Human or animal feces | 68 (10) | 7, 12 | 24 (5) | 44 (10) | 0.74 (0.45, 1.19) | 41 (30) | 27 (4) | 7.80 (5.09, 11.9) |
| Animals or insects, live or dead | 30 (4) | 2, 6 | 12 (3) | 18 (4) | 0.85 (0.43, 1.69) | 16 (12) | 14 (2) | 6.03 (3.17, 11.5) |
| HCF had kitchen | 155 (19) | 16, 23 | 69 (16) | 86 (20) | 1.27 (1.07, 1.50) | 123 (90) | 32 (4) | 21.9 (14.5, 30.4) |
| Visible in kitchen: | N = 155 | – | N = 69 | N = 86 | – | N = 123 | N = 32 | – |
| Rotten food | 20 (15) | 8, 23 | 9 (13) | 11 (13) | 1.48 (0.54, 4.07) | 19 (15) | 1 (3) | 6.05 (0.91, 40.2) |
| Human or animal feces | 3 (2) | 0, 5 | 1 (1) | 2 (2) | – | 3 (2) | 0 (0) | – |
| Animals or insects, live or dead | 14 (11) | 5, 17 | 4 (6) | 10 (12) | 0.80 (0.26, 2.42) | 14 (11) | 0 (0) | – |
| Waste Management | ||||||||
| General waste disposal location | N = 875 | – | N = 443 | N = 432 | – | N = 136 | N = 739 | – |
| Drum/dust bin | 772 (84) | 81, 87 | 415 (94) | 357 (83) | 1.12 (1.05, 1.20) | 105 (77) | 667 (90) | 0.87 (0.81, 0.94) |
| Pit | 77 (12) | 9, 15 | 21 (5) | 56 (13) | 0.42 (0.23, 0.77) | 27 (20) | 50 (7) | 2.53 (1.64, 3.91) |
| Others** | 22 (3) | 2, 5 | 6 (1) | 16 (4) | 0.34 (0.13, 0.88) | 2 (1) | 20 (3) | 0.46 (0.12, 1.79) |
| No designated area | 4 (0) | 0, 1 | 1 (0.2) | 3 (1) | 0.40 (0.05, 3.27) | 2 (1) | 2 (0.3) | 4.64 (0.48, 25.7) |
| Health-care waste disposal location# | N = 875 | – | N = 443 | N = 432 | – | N = 136 | N = 739 | – |
| Drum/dust bin | 741 (80) | 76, 83 | 403 (91) | 338 (78) | 1.15 (1.07, 1.23) | 99 (73) | 642 (87) | 0.86 (0.77, 0.95) |
| Pit | 103 (16) | 13, 19 | 30 (7) | 73 (17) | 0.45 (0.29, 0.71) | 33 (24) | 70 (9) | 2.23 (1.52, 3.28) |
| Other (river, lake, drain, and jungle)** | 18 (3) | 2, 5 | 2 (1) | 16 (4) | 0.12 (0.03, 0.50) | 2 (1) | 16 (3) | 0.51 (0.12, 2.13) |
| No designated area | 13 (1) | 0, 2 | 8 (2) | 5 (1) | 1.54 (0.44, 5.31) | 2 (1) | 11 (1) | 1.07 (0.24, 4.89) |
| Health-care waste disposal method | N = 862 | – | N = 435 | N = 427 | – | N = 134 | N = 728 | – |
| Bury | 105 (16) | 13, 19 | 33 (8) | 72 (17) | 0.47 (0.31, 0.73) | 25 (19) | 80 (11) | 1.50 (0.99, 2.24) |
| Burn | 268 (35) | 31, 39 | 115 (26) | 153 (36) | 0.79 (0.60, 1.04) | 69 (51) | 199 (27) | 1.81 (1.41, 2.32) |
| Incinerate | 38 (4) | 3, 6 | 19 (4) | 19 (4) | 0.97 (0.48, 1.96) | 5 (4) | 33 (5) | 0.82 (0.33, 2.05) |
| Dismantle or provide/sell to reuse | 17 (2) | 0, 3 | 11 (2) | 6 (1) | 1.65 (0.60, 4.57) | 1 (0.7) | 16 (2) | 0.37 (0.05, 2.86) |
| Nothing | 434 (43) | 39, 47 | 257 (58) | 177 (41) | 1.34 (1.09, 1.65) | 34 (25) | 400 (54) | 0.49 (0.36, 0.66) |
CI = confidence interval; HCF = health-care facility; PR = prevalence ratio.
Detected by spot checks.
PRs and 95% CI were calculated using Poisson regression models that included government vs. other and urban vs. rural location where PR for urban vs. rural < 1 indicates lower prevalence in urban settings; PR < 1 for government vs. other indicates lower prevalence in government.
Others; independent, private, and nongovernmental organization HCFs.
Weighted percentages for all HCFs.
Differences between rural vs. urban HCFs or government vs. other HCFs with P < 0.05 shown in bold.
Contamination at any water source.
Health-care waste includes cotton, cloth, bandages, gloves, sanitary pads, syringes, bottles, medicine foils, plastic saline packets, blood/urine/stool/collection tubes, and placenta.
Others include: river, dam, lake, pond, stream, canal, roadside, drain, bushes, or jungle.
Most HCFs (84%, 95% CI: 81, 87) disposed general waste into drums/dust bins, more common in urban HCFs (94% versus 83%; PR 1.12, 95% CI: 1.05, 1.20), whereas a pit was more common in rural areas (5% versus 13%; PR 0.42, 95% CI: 0.23, 0.77; Table 3). Health-care waste was similarly more commonly disposed into a drum in urban and a pit in rural areas. There was no health-care waste disposal method for 43% (95% CI: 39, 47) of HCFs. The most common disposal method was burning health-care waste among 35% (95% CI: 31, 39) of HCFs, and disposal through incineration was only observed for 4% (95% CI: 3, 6). Burying health-care waste was the second most common method, seen in 17% of rural versus 8% of urban HCFs (PR 0.47, 95% CI: 0.31, 0.73; Table 3). Government less commonly than other HCFs lacked a disposal method (25% versus 54%, PR 0.49 95% CI: 0.36, 0.66; Table 3).
WHO HCF service-level classifications.
The classification of HCFs into basic, limited, and unimproved service levels did not produce mutually exclusive categories for water (overlap between basic and limited) or for hand hygiene (for all three service-level categories; Tables 4 and 5). Among the 875 HCFs, > 90% provided basic drinking water service levels. For sanitation, only 46% provided basic service levels because of low levels of improved facilities accessible to patients/caregivers (Table 5). Basic levels for handwashing at point of care (H1) were attained for 68% (95% CI: 65, 71) of HCFs but only for 26% (95% CI: 23, 29) for patients/caregivers (H2). For health-care waste management, 47% (95% CI: 44, 50) of HCFs attained basic service levels for infectious waste treated and disposed safety (category M3; Table 5). Basic service levels for improved, useable sanitation facilities for outpatients located on the premises (category S1, PR 0.81, 95% CI: 0.68, 0.98) and water and soap within 5 m of toilets (category H2, PR 0.44, 95% CI: 0.27, 0.73) were significantly poorer in government versus other HCFs. (Note that PR and CIs for these comparisons are not shown in Table 5, but symbols are given to denote significant differences). Government HCFs had significantly better basic service levels with at least one useable, improved toilet designated for staff (category S3, PR 1.38, 95% CI: 1.28, 1.48) and fewer lacked infectious waste treatment and safe disposal (category M3, PR 0.49, 95% CI: 0.36, 0.66; Table 5). Significantly more government HCFs were categorized as having unimproved hand hygiene facilities (lacked a handwashing station, category H1; PR 1.12, 95% CI: 1.05.1.20) compared with other HCFs. Urban–rural differences were few; urban HCFs had significantly better basic sanitation service levels with at least one useable, improved toilet designated for staff (category S3, PR 1.17, 95% CI: 1.06, 1.29) than rural and conversely, more urban facilities lacked health-care waste management (category M3, PR 1.34, 95% CI: 1.09, 1.65, data not shown).
Table 4.
Criteria used for assigning WHO HCF service levels7 using data from surveyed HCFs,* Bangladesh, 2013
| Water | Sanitation | |||||
|---|---|---|---|---|---|---|
| W1 | W2 | W3 | S1 | S2 | S3 | S4 |
| Improved† main water source | Improved and on premises (on HCF grounds) | Water available from main source at time of survey | Improved toilets/latrines† for patients [for patients/caregivers not outpatient wards/clinics] located on premises and usable‡ at time of visit | At least one toilet designated for women/girls [for patients/caregivers] and have facilities to manage menstrual needs [menstrual hygiene management data not collected] | At least one toilet designated for staff | At least one toilet meets the needs of people with limited mobility [not collected] |
| Handwashing§ | Health-care waste management | – | – | |||
| H1 | H2 | M1 | M2 | M3 | – | – |
| Hand hygiene stations (basin with water and soap or alcohol-based hand rub) at points of care (we asked and observed the presence of handwashing locations in chamber/room/ward/duty ward) | Hand hygiene stations (basin with water and soap) available within 5 m of toilets | Waste safely segregated in consultation area [not collected] | Sharps waste treated and disposed of safely [not collected] | Infectious waste treated and disposed of safely [data on infectious and noninfectious waste but not sharps and no data on separate bins for these]. Safe disposal methods relevant for Bangladesh HCFs; bury, burn, and incinerate | – | – |
HCF = health-care facility.
Square brackets used to denote deviation from WHO definition.
Joint monitoring program definition of improved water source (W1–W3) and improved latrine (S1–S4).12
(S1) WHO definition of useable functional toilet; the hole or pit unblocked, water available for flush/pour flush toilets, no cracks, or leaks in the toilet structure. Sufficient privacy; toilet stall with walls without major holes, door unlocked when not in use (or for which a key is available at any time), and can be locked from the inside [data on sufficient privacy not collected].
Detailed data on HCF hand hygiene has been published elsewhere.8
Table 5.
WHO-designated HCF service levels7 and proportion of surveyed HCFs meeting service levels (N = 875)
| WHO classification* | Basic service | Limited service | Unimproved/no facility | |||
|---|---|---|---|---|---|---|
| Indicator description | N (%) | Indicator description | N (%) | Indicator description | N (%) | |
| Water | ||||||
| W1 | Improved main water supply at the facility in the outpatient area | 854 (98) | Improved main water supply at the facility | 854 (98) | An unimproved or no water source (W1) OR an improved water source (W1) that is more than 500 m from the facility (W2) | 21 (2) |
| W2 | Improved and on premises | 849 (97) | A “no” response for ANY (W2, W3) | 5 (0) | ||
| W3 | Available from main source at time of survey (W3) | 849 (97) | ||||
| Sanitation | ||||||
| S1 | Improved facilities for outpatients at the facility located on premises and usable at time of visit | 402 (46)† | Improved facilities but not usable | 23 (3) | Unimproved or no facilities | 450 (51) |
| S2 | At least one toilet designated for women/girls to manage menstrual needs | 176 (24) | A “no” response for ANY (S2, S3, S4) | – | N/A | N/A |
| S3 | At least one useable, improved toilet designated for staff | 674 (77)ठ| ||||
| S4 | At least one toilet meets the needs of people with limited mobility | Not collected | ||||
| Hand hygiene | ||||||
| H1 | Hand hygiene stations (water and soap or alcohol-based hand rub) at points of care | 597 (68) | Hand hygiene stations at either points of care (H1) or toilets (H2), but not both | 528 (60) | No hand hygiene stations available or available without soap or water or alcohol-based hand rub | 728 (83)‡ |
| H2 | Hand hygiene (water and soap) available within 5 m of toilets | 225 (26)† | ||||
| Health-care waste management | ||||||
| M1 | Waste safely segregated in consultation room | Not collected | Bins are in place but not used effectively. | Not collected | There are no bins for sharps and infectious waste | Not collected |
| M2 | Sharps waste treated and disposed of safely | Not collected | Waste is segregated but either infectious or sharps waste (or both) are not disposed of safely | Not collected | Waste is not safely treated and disposed | Not collected |
| M3 | Infectious waste treated and disposed of safely | 411 (47)‡‖ | Waste is not safely treated and disposed | 464 (53)‡‖ | ||
HCF = health-care facility; PR = prevalence ratio.
WHO definitions described in Table 4; detailed data on HCF hand hygiene has been published elsewhere.8
Compared facilities using Poisson regression models that included urban vs. rural and government vs. other HCFs where PR < 1 for government and P < 0.05.
Where PR > 1 for government and P < 0.05.
Where PR > 1 for urban and P < 0.05.
Where PR < 1 for urban and P < 0.05.
DISCUSSION
With LMICs striving to provide universal health coverage, there will be increased demand for HCF-based services; thus, the quality of these facilities will come under greater scrutiny (https://www.washinhcf.org/action-plan, accessed July 4, 2018). Data from this 2013 cross-sectional study highlights areas for attention. We detected very high levels of HCFs that provided WHO-defined basic water service for all population groups, more common than that found in 2014. This is likely explained by the types of HCFs included in the two studies. The 2014 Bangladesh Health Facility Survey used registered HCFs as the sampling frame with a focus on selecting all seven public HCF types across seven geographic division with private and NGO facilities of at least 20 beds. Of included HCFs, 83% were public and 8% were urban.11 This contrasts with our study where 15% of HCFs were public (government) and 51% were urban based on our strategy to oversample to allow geographic comparisons. We found that improved water sources inside the HCF for each population group were significantly less common for government than for other HCFs, likely explaining the higher frequency of basic water service in our study. Microbiological water analysis was not performed, so microbiological safety could not be assessed. Recently, the importance of microbiological water safety has been recognized and included in the WHO-UNICEF indicators for water quality12; this should be considered for HCF service level determination in future iterations.
Basic sanitation services, evident as useable, improved latrines, were available for outpatients (patients/caregivers) in approximately half of the HCFs surveyed and for staff among approximately three-quarters (Table 5). The HCF survey conducted in 2014 found that 72% of HCFs had functional client latrines,3 considerably higher than the 49% found in this study for the patient/caregiver group. However, we did not collect data on facilities in outpatient wards and clinics but asked the survey respondent to show facilities for the patient/caregiver group and followed the WHO definitions for useable as closely as possible.7 The absence of adequate, useable client/patient/caregiver latrines suggests that HCF quality improvement should prioritize toilets for staff and patients. In Bangladesh HCFs, where resources are limited, family members accompanying patients provide most hands on patient care.13,14 Family caregivers are similarly an important group in India,15 Malawi,16 and potentially other LMICs. Providing facilities for this group should be accorded a high priority, based on their potential to be involved in nosocomial transmission. Facilities for patient/caregiver use should be included in future versions of WHO HCF service levels.
Basic handwashing services were available for approximately two-thirds of HCFs at point of care, but in only 27% for patient/caregiver use,8 considerably lower than the 65% reported from the 54-country study.17 Handwashing is critical for infection control to reduce disease transmission. Even when there were handwashing locations accessible to patients/caregivers, soap and water was often absent.8
Among surveyed HCFs, half had basic health-care waste management facilities (waste burnt, buried, or incinerated) and 43% had no disposal method. This is considerably better than the HCFs in Dhaka (urban) in ∼2005 where almost 90% had no management system but disposed of health-care waste with other solid waste as part of the municipal system.18 Approximately half of surveyed HCFs reported that they burned, incinerated, or buried health-care waste, in line with findings from the 2014 survey.11 Very few HCFs reported selling discarded materials, which could be an underestimate because of social desirability bias; a previous report from Bangladesh suggested that these materials can generate income.19 Awareness of the dangers and necessary infrastructure to support safe health-care waste management in low-income settings can be limited.19,20 Health-care waste disposal should be strengthened by policy and enforcement to prevent spillover of pathogens, some which can harbor antimicrobial resistance, into the environment.13
Facility cleanliness was poor. The HCF wards, water sources, and grounds were littered with refuse and toilets were often soiled with human feces; conditions in rural and government HCFs were especially poor (Table 3). The WHO HCF standards21 provide guidance on cleaning surfaces and fittings to ensure facilities are visibly clean, and on toilet cleaning, but there are no standards for ensuring trash is collected and disposed and no measures included to assess HCF service levels.7
We detected inequities in HCF WASH facilities, the most striking between high-status physicians and patient caregivers; the latter provide frequent patient care and whose support should be prioritized. In addition, rural HCFs less commonly had improved drinking water on the premises or improved toilets for one or more population group (Table 2). Government HCFs generally more commonly had WASH facilities on the premises and better health-care waste disposal but poor cleanliness (dirtier wards, toilets, and water sources). A systematic review of LMIC HCF studies examining a range of quality indicators found that private facilities were not more efficient than government, as previously assumed.22 To improve HCF WASH facilities, rural areas should be targeted for toilet facility upgrades and policy should include recommendations on facility cleanliness.
Universal health coverage goals are more likely to be attained when HCFs meet standards for physical facilities and practices. Policy should enhance and support improved HCF governance and the government should consider exploring initiatives such as the Clean and Safe HCF program that has been developed in Ethiopia23 in an effort to reduce intra-facility and intra-family infectious disease transmission.
There were some important limitations to this study. The survey was conducted in advance of WHO publishing the core indicators and questions for HCF assessment.7 Some indicators for basic service levels reported here are incomplete. However, when using these 2013 survey data to construct WHO indicators, we found areas for change and addition. We predominantly collected data on indicators that could be observed in preference to reported, to minimize social desirability/courtesy bias. However, some reported indicators were collected. Even among observable indicators (e.g., facilities designated for doctor, staff, or patient/attendant used), we relied on HCF staff to point out these to field staff, which could have led to overestimation of facility availability for some population groups. We sampled different numbers of HCFs from clusters but did not adjust for these differences. This was unlikely to impact prevalence figures or rural–urban comparisons.
CONCLUSION
More emphasis is needed on facilities for family caregivers who provide patient management in resource-poor settings. Improving facilities for this group should be an integral part of accreditation. Based on HCF WHO basic service-level indicators, effort should be taken to ensure soap is available at handwashing locations.8 Moreover, cleanliness, trash disposal, and health-care waste disposal need improvement to attain quality service delivery at HCFs, as part of universal health coverage (sustainable development goal 3.8).
Private HCFs served the community with the largest share of beds and had the highest total daily admissions; driving change needs to consider profit-based motivators and incentives, for example, cost savings and increased efficiencies to improve facility quality. Further research to determine motivators for change in government, NGO, and private HCFs of all sizes would be worthwhile in developing strategies for improvement.
We recommend revisions to WHO indicators for LMIC HCF service levels7 to include data on overall facility cleanliness and adequate trash disposal. Although not examined in this study, HCF water quality assessment could be enhanced by including indicators on continuity of water supply and whether drinking water is microbiologically safe.
Acknowledgments:
icddr,b acknowledges with gratitude the commitment of WaterAid Bangladesh to its research efforts. icddr,b is thankful to the Governments of Bangladesh, Canada, Sweden, and the United Kingdom for providing core/unrestricted support.
REFERENCES
- 1.Jones KE, Patel NG, Levy MA, Storeygard A, Balk D, Gittleman JL, Daszak P, 2008. Global trends in emerging infectious diseases. Nature 451: 990–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allegranzi B, Bagheri Nejad S, Combescure C, Graafmans W, Attar H, Donaldson L, Pittet D, 2011. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 377: 228–241. [DOI] [PubMed] [Google Scholar]
- 3.NIPORT , 2016. Bangladesh Health Facility Survey 2014 Dhaka, Bangladesh: National Institute of Population Research and Training (NIPORT), Associates for Community and Population Research (ACPR), and ICF International. Available at: https://dhsprogram.com/pubs/pdf/SPA23/SPA23.pdf. Accessed July 4, 2018.
- 4.Bhuiyan MU, et al. 2014. Incidence of and risk factors for hospital-acquired diarrhea in three tertiary care public hospitals in Bangladesh. Am J Trop Med Hyg 91: 165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Islam MS, Luby SP, Sultana R, Rimi NA, Zaman RU, Uddin M, Nahar N, Rahman M, Hossain MJ, Gurley ES, 2014. Family caregivers in public tertiary care hospitals in Bangladesh: risks and opportunities for infection control. Am J Infect Control 42: 305–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rimi NA, Sultana R, Luby SP, Islam MS, Uddin M, Hossain MJ, Zaman RU, Nahar N, Gurley ES, 2014. Infrastructure and contamination of the physical environment in three Bangladeshi hospitals: putting infection control into context. PLoS One 9: e89085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO , 2016. Monitoring WASH in Health Care Facilities. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 8.Horng LM, Unicomb L, Alam MU, Halder AK, Shoab AK, Ghosh PK, Opel A, Islam MK, Luby SP, 2016. Healthcare worker and family caregiver hand hygiene in Bangladeshi healthcare facilities: results from the Bangladesh National Hygiene Baseline Survey. J Hosp Infect 94: 286–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alam MU, Luby SP, Halder AK, Islam K, Opel A, Shoab AK, Ghosh PK, Rahman M, Mahon T, Unicomb L, 2017. Menstrual hygiene management among Bangladeshi adolescent schoolgirls and risk factors affecting school absence: results from a cross-sectional survey. BMJ Open 7: e015508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO/UNICEF , 2015. WHO/UNICEF Joint Monitoring Programme (JMP) for Water Supply and Sanitation. Geneva, Switzerland: World Health Organization.
- 11.National Institute of Population Research and Training (NIPORT) , Associates for Community and Population Research (ACPR), and ICF International, 2016. Bangladesh Health Facility Survey 2014. Dhaka, Bangladesh: NIPORT, ACPR, and ICF International. [Google Scholar]
- 12.WHO/UNICEF , 2017. WASH in the 2030 Agenda: New Global Indicators for Drinking Water, Sanitation and Hygiene. Geneva, Switzerland: World Health Organization.
- 13.Islam MA, Islam M, Hasan R, Hossain MI, Nabi A, Rahman M, Goessens WHF, Endtz HP, Boehm AB, Faruque SM, 2017. Environmental spread of New Delhi metallo-β-lactamase-1-producing multidrug-resistant bacteria in Dhaka, Bangladesh. Appl Environ Microbiol 83: pii: e00793–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hadley MB, Roques A, 2007. Nursing in Bangladesh: rhetoric and reality. Soc Sci Med 64: 1153–1165. [DOI] [PubMed] [Google Scholar]
- 15.Bhalla A, Suri V, Kaur P, Kaur S, 2014. Involvement of the family members in caring of patients an acute care setting. J Postgrad Med 60: 382–385. [DOI] [PubMed] [Google Scholar]
- 16.Hoffman M, Mofolo I, Salima C, Hoffman I, Zadrozny S, Martinson F, Van Der Horst C, 2012. Utilization of family members to provide hospital care in Malawi: the role of Hospital Guardians. Malawi Med J 24: 74–78. [PMC free article] [PubMed] [Google Scholar]
- 17.WHO/UNICEF , 2015. Water, Sanitation and Hygiene in Health Care Facilities: Status in Low and Middle Income Countries and Way Forward. Geneva, Switzerland: World Health Organization.
- 18.Hassan MM, Ahmed SA, Rahman KA, Biswas TK, 2008. Pattern of medical waste management: existing scenario in Dhaka city, Bangladesh. BMC Public Health 8: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patwary MA, O’Hare WT, Sarker MH, 2011. An illicit economy: scavenging and recycling of medical waste. J Environ Manage 92: 2900–2906. [DOI] [PubMed] [Google Scholar]
- 20.Sarker MA, Harun-Or-Rashid M, Hirosawa T, Abdul Hai MS, Siddique MR, Sakamoto J, Hamajima N, 2014. Evaluation of knowledge, practices, and possible barriers among healthcare providers regarding medical waste management in Dhaka, Bangladesh. Med Sci Monit 20: 2590–2597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO , 2008. Essential Environmental Health Standards in Health Care. Adams J, Bartram J, Chartier Y, eds. Geneva: Switzerland: World Health Organization. [Google Scholar]
- 22.Basu S, Andrews J, Kishore S, Panjabi R, Stuckler D, 2012. Comparative performance of private and public healthcare systems in low- and middle-income countries: a systematic review. PLoS Med 9: e1001244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seman Y, 2016. Clean and Safe Health Facility Initiative (CASH) in Ethiopia. Geneva, Switzerland: World Health Organization. [Google Scholar]