Abstract.
Hepatitis E virus (HEV) infection in developing countries is associated with poor hygiene, lack of clean drinking water, and inadequate sanitation. In this study, we report the first case investigation and describe the present situation of HEV outbreak within displaced persons camps in the Diffa region, Republic of Niger. The investigation showed the outbreak to be closely linked to unclean water supply, low hygiene, and sanitation facility standards. Between January and September 2017, a total of 1,917 HEV suspect cases were recorded from which 736 (38.4%) have been confirmed positive for HEV by reverse transcription polymerase chain reaction and enzyme linked immunosorbent assay. Overall, 38 (1.9%) deaths were recorded, including 17 (44.7%) pregnant women. The ongoing outbreak highlights poor drinking water quality and sanitation conditions in displaced persons camps in the Diffa region. Disease containment and patient care activities, particularly for pregnant women, may have resulted in decreased transmission of infection and deaths.
Hepatitis E virus (HEV) infection is hyperendemic in many developing countries, especially in Southeast Asia and Africa, where there is poor sanitation and weak public-health infrastructures.1,2 In developed countries, HEV infections occur through zoonotic transmission or contaminated blood products and can cause chronic hepatitis in immunocompromised individuals.3 The HEV affects approximately 20 million persons annually worldwide, causing more than 56,000 deaths.4,5 The causative agent of hepatitis E infection is the HEV, which belongs to the genus Hepevirus within the Hepeviridae family. The family is composed of four distincts genotypes, with the first two infecting exclusively humans, whereas genotypes three and four represent zoonotic agents.1,6 In humans, the infection is mainly transmitted by means of contaminated water, but also via food or blood transfusions, or vertically from mother to fetus.2,6 Most HEV infections are self-limiting, but may develop into fulminant hepatitis with a case-fatality rate of 1–2% in the total population. In pregnant women, case-fatality rates of up to 40% were observed, especially during the third trimester of pregnancy.3 To date, no licensed HEV vaccine is available, instead a recombinant vaccine (HEV239 Hecolin®; Innovax, Xiamen, China) is currently under evaluation by the World Health Organization.5,7
Previous studies described HEV outbreaks in displaced populations in East Africa, including endemics in northern Uganda with more than 10,000 cases of acute jaundice and a 2% case-fatality rate8 and in South Sudan with 5,000 reported cases and a 10% death rate among pregnant women.9 However, to date, no surveillance study has been conducted in Niger and little is known about the HEV seroprevalence in the general population.
Recently, a HEV outbreak was detected in April 2017 in the Diffa Region in Niger, near the Nigerian and Chadian border. This outbreak is still ongoing and is supposed to be an indirect consequence of the misty Boko Haram sect conflict, which contributed to a massive humanitarian crisis since 2015. As a consequence, a huge number of refugees migrated to the Diffa district, therefore, exceeding hygienic and sanitary capacities and fresh water supply.10 The confirmation of HEV cases on human samples at Institut Pasteur de Dakar in April 2017 led to the official declaration of a HEV outbreak by the national health authorities.11
This work aims to report the early case investigation and describes the ongoing HEV outbreak among displaced population in the Diffa region from April to September 2017.
Geographically, the Diffa Region is located in the extreme Southeast of the Republic of the Niger between the Lake Chad and Komadugu Yobe Rivers bordering Chad in the east and Nigeria in the south. Since 2015, this region has been continuously affected by Boko Haram attacks, triggering large scale displacement of population. According to the Office for the Coordination of Humanitarian Affairs, more than 240,000 displaced people and refugees are now living in the Diffa region as of September 2017.10
Since January 2017, the regional health authorities notified a number of abnormal cases of icteric syndrome, from which the majority were detected in a fraction of population living in a precarious situation, particularly pregnant women in refugee camp. Most of these cases were admitted to the Maternal and Child Reference Health Center of Diffa where Médecins Sans Frontières (MSF) is providing medical care assistance.
In the absence of appropriate diagnostic capacities, initially, yellow fever was suspected as the causative agent of this outbreak. However, considering a large number of cases among pregnant women and a parallel HEV outbreak in the close border region of the Republic of Chad, HEV was considered as a potential cause of signs and symptoms as well.
Subsequently, the regional health directorate of Diffa initiated a case investigation within the affected areas, including blood sample collection of suspected patients. Serum samples were sent to Institut Pasteur de Dakar for biological confirmation using RT-PCR and ELISA techniques.
Following the confirmation of positive cases for HEV, the Ministry of Public Health declared officially on 19 April an outbreak of HEV infection among displaced persons in the Diffa region which had already caused 29 deaths.
The investigation results reported the ongoing outbreak to be closely linked to an unclean water supply, poor hygiene, and sanitation facilities for the 240,000 people who are currently displaced in the Diffa region. The environmental study around the affected area showed that most of the wells and drillings were in very poor conditions and particularly insufficient for the water supply of the population. Moreover, there was a lack of adequate and sufficient latrine facilities, which cause most of the population from the camps to ease themselves in the bushes across the river.
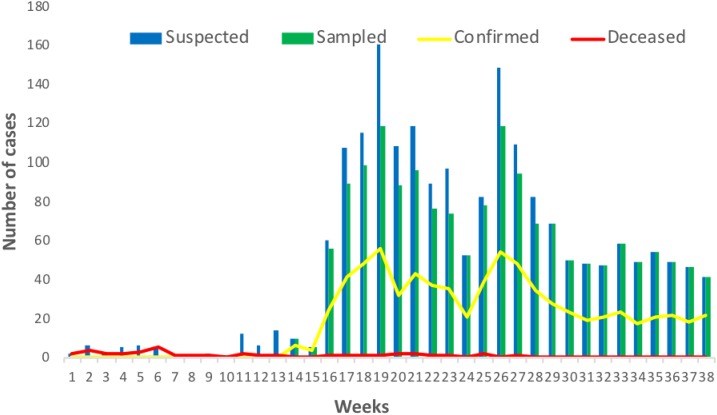
The review of hospital logbooks revealed that already in the last quarter of 2016 about 12 cases of acute jaundice symptoms have been recorded among displaced persons attending medical care although without any death. In January 2017, 18 patients, all pregnant women, presenting symptoms such as jaundice, vomiting, fever, pelvic pains, and memory loss were notified to the regional health authorities of Diffa. Of these cases, 6 (33.3%) died. Until April 2017, 46 additional cases, presenting similar symptoms were recorded, mainly pregnant, women from which 16 (34.8%) died (Figure 1).
Figure 1.
Weekly distribution of hepatitis E virus cases in the Diffa region, Niger, January to September 2017. This figure appears in color at www.ajtmh.org.
Between April and September 2017, a total of 1,633 (85.2%) HEV suspected cases were sampled, of which 736 (45.0%) have been confirmed positive for HEV using RT-PCR and the Human HEV IgM ELISA Test Kit (MyBioSource, San Diego, CA).
The case definition used for suspected cases was as follows: patients living in refugees camps 3–6 months before the outbreak declaration, and presenting acute syndromes including jaundice, dark urine, anorexia, faintness, tiredness, and sensibility of the top-right quadrant.
Most of the cases were older than 15 years with 456 (62.0%) female cases. The predominant clinical symptoms among them were jaundice, 712 (96.7%); tiredness, 603 (81.9%); and dark urine 565 (76.8%) (Table 1).
Table 1.
Characteristics of patients with hepatitis E virus infection in the Diffa region, Niger, January to September 2017
| Sampled cases N = 1,633 | Confirmed cases N = 736 | Dead cases N = 38 | |
|---|---|---|---|
| Age | |||
| < 5 | 79 (4.8%) | 12 (1.6%) | 1 (2.6%) |
| 5–14 | 209 (12.8%) | 54 (7.3%) | 1 (2.6%) |
| 15–24 | 435 (26.6%) | 181 (24.6%) | 8 (21.0%) |
| 25–34 | 521 (31.9%) | 318 (43.2%) | 22 (57.9%) |
| > 35 | 389 (23.8%) | 171 (23.2%) | 6 (15.8%) |
| Gender | |||
| Male | 676 (41.4%) | 280 (38.0%) | 2 (5.2%) |
| Female | 957 (58.6%) | 456 (62.0%) | 36 (94.8%) |
| Symptoms | |||
| Jaundice | 1,523 (93.2%) | 712 (96.7%) | 31 (81.6%) |
| Dark urine | 1,047 (64.1%) | 565 (76.8%) | 17 (44.7%) |
| Tiredness | 876 (53.6%) | 603 (81.9%) | 8 (21.0%) |
| Vomiting | 715 (43.8%) | 426 (57.9%) | 13 (34.2%) |
Overall, between January and September 2017, 1,917 HEV-suspected cases were recorded, of which 38 (1.9%) died. The great majority of these fatal cases 36 (94.8%) occurred among female patients, with half of them being pregnant (44.7%).
The humanitarian crisis in the Lake Chad region led to a large migration wave into refugee camps in the Diffa region and this may have contributed to the ongoing HEV outbreak.10 A recent study showed that in displaced persons camps, people from places with different historical epidemiologic profiles come together and reside in close quarters where conditions for disease spread are high.12 The reports of previous investigations on HEV outbreaks worldwide sustained that the infection was linked to unclean water supply, poor hygiene, and limited access to sanitation facilities, particularly in displaced persons camps.7,11 Indeed, several camps for displaced persons in the Diffa region did not have an adequate supply of drinking water and there was a lack of latrines or those in place were in poor conditions.10 Also because of insufficient potable water infrastructures, most population from camps got supplies of drinking water at the same troughs intended for animals. As HEV is a zoonotic disease, contaminated drinking water from animal could result as the main infection source. Therefore, MSF in collaboration with the Ministry of Public Health conducted awareness campaigns aiming to increase basic hygiene measures such as the use of latrines and handwashing, to contain the outbreak propagation. The large distribution of Aquatabs tablets for decontamination of well and river water contributed strongly to improve the quality of drinking water. Indeed, disinfection with Aquatabs tablets at a concentration of 33 mg per 10 L of water for 10 minutes allows the prevention of diarrhea and gastro-intestinal pains and elimination of all micro-organisms including HEV. In addition, other actions improved the infrastructures of the local water supply, in particular, the renewal of water fetching and water storage materials, and the construction of new wells and drillings.7 All these actions, in combination with improved medical care measurements, resulted in the reduction of new HEV infections and substantially decreased the death rate.
At the early stage of the outbreak, epidemiological relationship was made between a previous occurrence of HEV outbreak in the Republic of Chad, a neighboring country and that of Niger.7 However, in the absence of sequencing data and consistent epidemiological study, it will be difficult to support this hypothesis and even estimate the route of the infection.
In this study, the high number of sampled cases and confirmed cases could be attributed to the active surveillance conducted by Médecins Sans Frontières (MSF) after the outbreak declaration throughout the different refugee camps in the Diffa region. Our findings showed that among the suspected cases, jaundice and dark urine were the predominant symptoms, however their proportions in this study seems to be much higher than that reported in previous studies.5,8 Moreover, about 80% of HEV affected persons were older than 15 years, a trend reported in an earlier study5; therefore allowing to conclude that immunologically naive persons are at a higher risk of infection. The high proportion of affected women in this study may be a consequence of sociocultural practices for which water collection and water management are exclusively dedicated to women, particularly those at a mature age. On the other hand, the high mortality among pregnant women (44.8%) found in this study is much higher than that reported in previous studies.8,9 This supports the evidence of insufficient medical care for the displaced population, particularly pregnant women, which is the high risk group for HEV infection.1,6
As hepatitis E spreads mainly through contaminated water, the ongoing outbreak highlights the poor water quality and the lack of adequate sanitation facilities in displaced persons camps in the Diffa region. Strengthened measures for disease containment and medical taken care, particularly among pregnant women, have resulted in a considerable decrease of infection transmission and death. However, continuous community-based sensitization on hygiene measures and behavioral changes should be also strengthened to overcome the outbreak and prevent the dissemination of the infection.
Acknowledgments:
Besides the implication of the Ministry of Public Health of Niger, we highly acknowledge the action of Médecins Sans Frontières (MSF) for medical care and assistance in the field and also the World Health Organization for the support.
REFERENCES
- 1.Kim JH, Nelson KE, Panzner U, Kasture Y, Labrique AB, Wierzba TF, 2014. A systematic review of the epidemiology of hepatitis E virus in Africa. BMC Infect Dis 14: 308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Paschale M, et al. 2016. Epidemiology of hepatitis E virus infection during pregnancy in Benin. Trop Med Int Health 21: 108–113. [DOI] [PubMed] [Google Scholar]
- 3.Kamar N, Izopet J, Pavio N, Aggarwal R, Labrique A, Wedemeyer H, Dalton HR, 2017. Hepatitis E virus infection. Nat Rev Dis Primers 3: 17086. [DOI] [PubMed] [Google Scholar]
- 4.Gerbi GB, Williams R, Bakamutumaho B, Liu S, Downing R, Drobeniuc J, Kamili S, Xu F, Holmberg SD, Teshale EH, 2015. Hepatitis E as a cause of acute jaundice syndrome in northern Uganda, 2010–2012. Am J Trop Med Hyg 92: 411–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blasco-Perrin H, Abravanel F, Blasco-Baque V, Peron JM, 2016. Hepatitis E, the neglected one. Liver Int 36 (Suppl 1): 130–134. [DOI] [PubMed] [Google Scholar]
- 6.Scobie L, Dalton HR, 2013. Hepatitis E: source and route of infection, clinical manifestations and new developments. J Viral Hepat 20: 1–11. [DOI] [PubMed] [Google Scholar]
- 7.Green A, 2017. The omitted epidemic-hepatitis E in the Lake Chad region. Lancet 390: 443–444. [DOI] [PubMed] [Google Scholar]
- 8.Teshale EH, et al. 2010. Hepatitis E epidemic, Uganda. Emerg Infect Dis 16: 126–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention , 2013. Investigation of hepatitis E outbreak among refugees: Upper Nile, South Sudan, 2012–2013. MMWR Morb Mortal Wkly Rep 62: 581–586. [PMC free article] [PubMed] [Google Scholar]
- 10.Office for the Coordination of Humanitarian Affairs-Niger, Bulletin Humanitaire Aout , 2017. Humanitarian Response 2017 Available at: https://www.humanitarianresponse.info/en/operations/niger. Accessed September 29, 2017.
- 11.World Health Organization , 2017. Hepatite E-Niger. Disease Outbreak News 2017 Available at: http://www.who.int/csr/don/05-may-2017-hepatitis-e-niger/en/. Accessed September 17, 2017.
- 12.Azman AS, et al. 2017. High hepatitis E seroprevalence among displaced persons in South Sudan. Am J Trop Med Hyg 96: 1296–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]