Abstract
Adolescence is a critical time point in the lifecourse. LifeLab is an educational intervention engaging adolescents in understanding DOHaD concepts, and the impact of the early life environment on future health, benefitting both their long-term health, and that of the next generation. We aimed to assess whether engaging adolescents with DOHaD concepts improves scientific literacy, and whether engagement alone improves health behaviours.
Six schools were randomised, three to intervention and three to control. Outcome measures were change in knowledge, and intended and actual behaviour in relation to diet and lifestyle. 333 students completed baseline and follow-up questionnaires. At 12 months, intervention students showed greater understanding of DOHaD concepts. No sustained changes in behaviours were identified.
Adolescents’ engagement with DOHaD concepts can be improved and maintained over 12 months. Such engagement does not itself translate into behaviour change. The intervention has consequently been revised to include additional components beyond engagement alone.
Keywords: Health Education, Behaviour Change, Scientific Literacy, Health Literacy, Randomised Control Trial
Introduction
Non-communicable diseases (NCDs), including cardiovascular disease, type 2 diabetes and some cancers account for over 70% of deaths globally and the number of deaths from NCDs is rising.1 Their prevention not only benefits individuals at risk, but reduces pressure on limited health resources.2 Behavioural risk factors are the largest contributor to the NCD burden.3
A large body of evidence shows the impact of prenatal and infant development on long-term health, and specifically on NCDs.4–6 A woman’s diet and general health as she embarks on pregnancy has profound and lasting effects on early development and on the lifelong health of her children,7 a concept core to the Developmental Origins of Health and Disease hypothesis. The health behaviours of fathers are also important both because they influence the health behaviours of their partners8 and because they affect sperm quality.9
Adolescence is increasingly recognised as an important time when lifestyle and health behaviours become embedded tracking into adulthood.10 Thus adolescence offers a window of opportunity to improve health and nutrition literacy in order to reduce later risk of NCDs, but also to pass health opportunities to the next generation.
Our systematic review of approaches to behaviour change interventions showed that successful interventions include educational components,11 because education can change attitudes, alter health-related behaviours and increase scientific and health literacy in young people.12,13 Schools have long been seen as ideal settings for such interventions (e.g.14).
However, while typical public health campaigns using transmission communication approaches (e.g. leaflets, advertising) can raise awareness and immediate behaviour change, sustaining behaviour change is challenging. The model espoused by LENScience highlights the importance of transactional communication interventions. The learning activities are interactive and develop a co-constructed understanding, building on the appreciation of the varied personal, social and cultural contexts in which students exist.15 Coupling activities which translate specific knowledge into interactive learning activities with context-specific learning,16 may improve the capacity of adolescents to obtain and understand basic health information and engage with services needed to make appropriate health decisions (i.e. their health literacy) and motivate them to change behaviour.
Knowledge of scientific principles, especially those related to human biology, critical thinking and the ability to make informed decisions about science-related issues, are attributes closely linked to health literacy. These considerations led us to develop LifeLab, an innovative ‘hands-on’ science-based approach aiming to promote health literacy through science engagement and literacy.17 The theme of LifeLab is “Me, My Health & My Children’s Health”. Feasibility work showed that participation in a science programme focusing on health, and experiencing learning within a hospital-based classroom had a positive influence on teenagers’ awareness of the importance of making healthy lifestyle choices.17
We present data from a pilot, cluster-randomised study, conducted prior to a large cluster-randomised control trial. Our primary objective was to measure, at an individual participant level, the effects of the LifeLab intervention at 12 months’ follow-up. The main outcomes were change in knowledge of DOHaD concepts, including the impact of early life environment and their effects on the students' health and that of their future children, along with change in attitudes in relation to diet and lifestyle.
Methods
Trial design
We recruited Year 9 students (aged 13-14 years) from six state, mixed gender, secondary schools (approximately 400 students) from Southampton and Hampshire, each school representing one cluster.
Following recruitment, schools returned a letter of agreement signed by the Headteacher as their consent to participation. Schools were then randomly allocated to either ‘control’ or ‘intervention’ status. Parent and pupil information sheets were provided for the schools to disseminate to pupils and parents directly. To reduce the administrative burden on schools and as agreed by the ethics committee, parental consent for the intervention schools was opt-in and for the control schools was opt-out.
Three classes from each school participated in the trial, with students from control and intervention schools completing online questionnaires after recruitment (baseline questionnaires) and again approximately 12 months after baseline. The questionnaires included assessment of knowledge and attitudes about DOHaD concepts, and reported measures of dietary quality and physical activity. The LifeLab team provided support to the teachers to administer the process, but the students completed the questionnaires independently online. A written script was used to explain the process to the students to ensure consistency across control and intervention schools.
Participants
At a cluster level, all 81 secondary state schools/academies in Southampton and Hampshire were eligible for participation. At an individual level, there were no exclusion criteria for pupils as the teaching programme was planned for this age range and was differentiated for ability. Support was provided for students who required more input (e.g. English as an additional language).
Recruitment
Schools with which we had previous contact were approached for this pilot trial, and were asked to allocate three ‘middle ability’ classes to participate in the trial (~90 pupils). We approached schools in groups of six, and the first six schools we approached were keen to be recruited; no schools declined. To minimise loss of pupils to follow-up, pupil lists for each participating class were requested, so that missing participants at each stage could be identified and asked to complete the questionnaires. Recruitment was completed and schools randomised in December 2012. The first participant completed the baseline questionnaire in October 2013 and the last in July 2014, with the intervention schools attending LifeLab between January and March 2014. All participants had completed the 12 month follow-up questionnaire by July 2015.
Randomisation
Prior to randomisation, no matching of schools took place. The six schools were randomised in one block. Each school was considered to be a single cluster and randomised accordingly. To ensure allocation concealment, randomisation was conducted off-site, with researchers unaware of the procedure, ensuring that prediction of allocation would not be possible. It was conducted by a statistician at the MRC Lifecourse Epidemiology Unit (LEU) with no knowledge of the schools in question, using computer-generated sequences.
Statistical methods
Summary statistics (chi-squared tests, rank-sum test, and t-tests) were used to examine differences between groups. A formal cluster analysis was not possible due to the small number of schools. Categorical outcome variables were dichotomised and Poisson regression with robust variance18 was used to obtain prevalence rate ratios (PRRs) for the outcome in relation to the intervention, adjusted for baseline values, gender and Index of Deprivation Affecting Children (IDACI) score.19 The IDACI score is obtained from home postcode and indicates the level of deprivation of the area in which the child lives, with higher scores indicating greater deprivation. Adjustment for this was considered important to account for differences between the schools. Additionally, we used principal components analysis on the baseline reported dietary data to derive a summary dietary quality score.20 Multiple regression was used to compare the dietary quality scores at follow-up between the intervention and control groups, adjusting for baseline dietary quality score, gender and IDACI score.
Ethics Approval and Research Governance
The study was approved by the Research Ethics Committee of the Faculty of Social, Human, and Mathematical Sciences, University of Southampton (ERG reference: 8019). The research sponsor was the University of Southampton.
The intervention
The intervention comprised:
Teacher professional development (PD) – a one-day training course, explaining the research foundations of LifeLab and the student modules.
A two-week module of work for Year 9 school students (13-14yr olds), linked to the National Curriculum for Science in England, encompassing school-based pre- and post-visit lessons.
A hands-on practical day visit to LifeLab in the Southampton Centre for Biomedical Research at University Hospital Southampton, held during the module. At this visit, students experienced various ways to measure health, including assessing carotid artery blood flow and structure using ultrasound, measuring body composition, performing lung function tests and measuring grip strength and hamstring flexibility. They were also able to extract their own DNA and carry out gel electrophoresis experiments.
The long-term implications of the students’ current diet and lifestyle on their health and an introduction to DOHaD concepts were linked both to the hands-on practical activities at LifeLab and to the school-based activities. This ensured consistency, maximising opportunities for students to engage with these messages in a variety of ways.
Data Management
Data were collected via an online questionnaire (hosted by the University of Southampton), downloaded via a dedicated computer and stored on a University server. All data were kept in accordance with the Data Protection Act, the University of Southampton Data protection policy and with the protocols of the MRC LEU.
Results
The six randomised schools had different characteristics. The randomisation resulted in the control arm having three schools with a more deprived profile. For example, the average percentage of children eligible for free school meals at any time in the previous 6 years for the control schools was 37.6% (range 28.4-55.2) but for the intervention schools was lower at 22.8% (range 11.2-44.8).
Only five parents in the intervention arm did not opt-in and no parents in the control arm opted out, so it is unlikely that there was a difference in the two arms as a result of the two consent procedures used.
Participant Flow
Consort Diagram (see Supplementary Figure S1)
Baseline Data
Baseline data was collected on 392 students. Some loss to follow-up occurred due to students moving schools (6% of students at 12mo follow-up) and from student absences (9%), resulting in complete baseline and follow-up data from 333 students (85%).
For a comparison of students in the intervention and control groups at recruitment, see supplementary Table S1. Students in the control group generally lived in more deprived areas and assessed their lifestyles and diets as less healthy than those in the intervention group. The mean age at recruitment was 13.8 years, with the control group being slightly younger than the intervention group. There were no differences between those followed-up and those not in terms of gender or age at baseline, but those not seen at follow-up had higher IDACI scores and tended to live in more deprived circumstances than those who remained in the study (p=0.006).
Outcomes
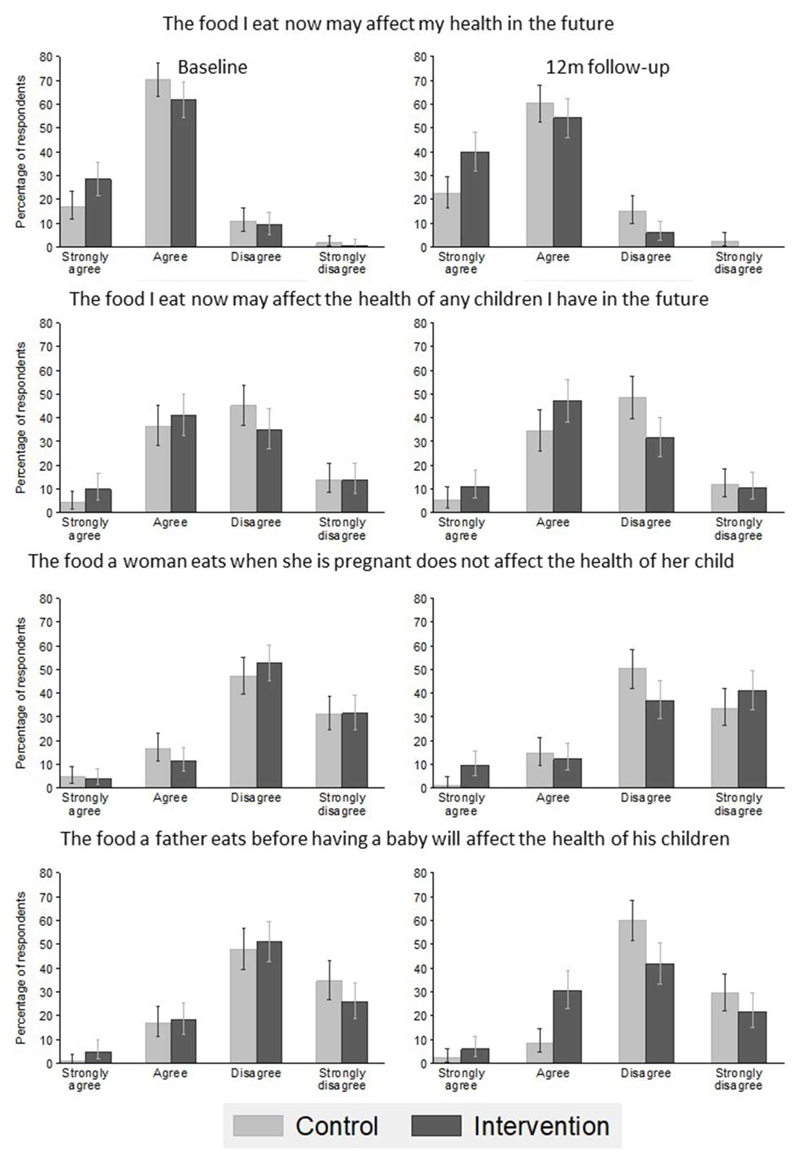
Analysis of students’ responses showed that, at 12 months, intervention students had greater understanding than control students of DOHaD concepts and the influences of health behaviours on their long term health and that of their children (Figure 1 and Table 1). At the twelve month follow-up, intervention students were nearly twice as likely to suggest that the answer to the question ‘At what age do you think our nutrition starts to affect our future health?’ was ‘Before birth’. Similarly they showed increased understanding of: how the food they eat affects their future health; that the food a woman eats when she is pregnant affects the health of her child; that the food they eat now may affect the health of any children they have in the future; and that the food a father eats before having a baby will affect the health of his children. However, although this change in knowledge and understanding of DOHaD concepts was maintained over 12 months, this was not translated into sustained behaviour change as shown by the lack of difference in diet and exercise levels between the intervention and control groups (Table 1). Furthermore, simply increasing the students’ knowledge did not influence their own perception of whether it was important for them to eat healthily now.
Figure 1.
Histograms showing percentage of LifeLab students agreeing with statements about the effects of diet on long-term health (n=333)
Table 1.
| Question | Outcome response | Adjusted PRR1 | (95%CI) | P-value |
|---|---|---|---|---|
| At what age do you think our nutrition starts to affect our future health? | Before birth | 1.87 | (1.42,2.45) | <0.001 |
| The food I eat now may affect my health in the future | Strongly agree or agree | 1.19 | (1.08,1.32) | <0.001 |
| The food a father eats before having a baby will affect the health of his children | Strongly agree or agree | 4.05 | (2.34,7.01) | <0.001 |
| It is not important for me to eat healthy food now | Strongly disagree or disagree | 1.19 | (0.79,1.79) | 0.4 |
| How many times per week do you do exercise which makes you out of breath? | Once a day or more | 0.79 | (0.49,1.27) | 0.3 |
| How often do you take long low level exercise (e.g. long walks, long swim)? | Once a day or more | 0.73 | (0.49,1.09) | 0.1 |
| Adjusted Beta1,2 | (95%CI) | P-value | ||
| Prudent diet score (SD) | -0.08 | (-0.24,0.09) | 0.4 |
Table to show prevalence rate ratios (PRR) of reporting the outcome at 12 month follow-up, adjusted for baseline response, sex and deprivation score, and results of the regression analysis of the prudent diet score
Adjusted for baseline value, sex and IDACI score
Beta expresses the change in prudent diet score in SD units associated with the intervention
Discussion
Main findings
This study builds on previous feasibility work showing a change in knowledge and attitudes in teenagers following the LifeLab programme.17 Here, we carried out a pilot cluster-randomised control trial. Significantly, we have shown it is possible to translate DOHaD concepts into an interactive hands-on educational intervention designed to engage students with the science behind health messages and enable them to understand the consequences of current health behaviours on their own and their future children’s health, and that this knowledge is retained 12 months later. What was apparent however, was that this alone was not sufficient for the students to apply this knowledge and act to improve their health behaviours. LifeLab provides a key motivational opportunity which leads to increased understanding of DOHaD concepts and sustained change in knowledge with the potential to initiate behaviour change, but to turn this into sustained behaviour change, additional personalised support is essential.
Strengths and limitations
This study demonstrates that schools could successfully be recruited to a cluster randomised trial. The follow-up rate was high at 85%, showing engagement from both study arms.
Schools were randomly allocated to control or intervention arm following recruitment. As demonstrated in this study, randomisation with low numbers can result in imbalances between the two trial arms. Students in the control schools came from more disadvantaged neighbourhoods, and reported poorer health and health behaviours than those in the intervention schools. The latter is potentially an interesting confounder; how does the perception of health affect engagement with the intervention? Does assessing one’s lifestyle and diet as less healthy represent a more negative perception of lifestyle and health or genuinely a more sophisticated judgement of a less healthy lifestyle and diet? This is an area for consideration through the process evaluation during the full trial. However, our analysis adjusted for deprivation and also took account of the baseline levels of the measures being assessed. This may not have accounted fully for the imbalance in the randomisation, nonetheless marked improvements were seen in the knowledge acquired by students in the intervention schools, but not in those from control schools. Notably, the difference seen between the results for knowledge and those for reported behaviour indicates that we have largely taken account of biases resulting from baseline differences.
Engaging adolescents with the science behind health messages, and empowering them to take ownership of and act on knowledge to support their future health, and that of their future children, is eminently translatable to different settings. Both LENScience (New Zealand) and LifeLab are being delivered in other ways; LENScience has been adapted for Pacific Island nations without specialised resources and Early LifeLab now delivers these concepts to younger children in primary schools.
Conclusion
The six schools in this pilot trial represented students from a range of backgrounds, including some who were quite disadvantaged. The effects observed on knowledge were, however, consistent with those observed in our feasibility work.17
Knowledge is easier to acquire than to act upon; embedding behaviour change is challenging and while LifeLab offers a contextualised programme of interactive activities for the students, more work after the LifeLab experience, and in collaboration with teachers, is required to improve health behaviours in line with their knowledge. Nonetheless, acquiring new knowledge is a first step in behaviour change and LifeLab shows promise as part of a more extensive intervention to improve behaviours. We have since expanded on the intervention, capturing this moment of motivation but including an additional element of inviting the students to commit to behaviour change pledges reinforced with tailored PD for school teachers in techniques to support behaviour change in their students, aligned with the ‘Healthy Conversation Skills’ ethos.21 We are therefore conducting a larger cluster-randomised trial of more than 30 schools22 to evaluate the impact of this enhanced intervention.
Supplementary Material
Acknowledgements
We thank the participating students, their teachers and schools and the LifeLab staff for contributions to this project. Ken Cox provided computer support for the data management.
Funding
This work was supported by the BUPA Foundation. KWT and MAH are supported by the National Institute for Health Research through the NIHR Southampton Biomedical Research Centre. KMG is supported by the UK Medical Research Council (MC_UU_12011/4), the National Institute for Health Research (as an NIHR Senior Investigator (NF-SI-0515-10042) and through the NIHR Southampton Biomedical Research Centre) and the European Union's Erasmus+ Capacity-Building ENeASEA Project and Seventh Framework Programme (FP7/2007-2013), projects EarlyNutrition and ODIN under grant agreement numbers 289346 and 613977. MAH and DL are supported by the British Heart Foundation, HD and LB are supported by Wessex Heartbeat and HMI is supported by the UK Medical Research Council.
Disclaimer
This report is independent research funded in part by the National Institute for Health Research Biomedical Research Centre Funding Scheme. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health or other funders.
Footnotes
Competing Interests
KMG has received reimbursement for speaking at conferences sponsored by nutrition companies, and is part of an academic consortium that has received research funding from Abbott Nutrition, Nestec and Danone. The University of Southampton has received an unrestricted donation from Danone Nutricia to support LifeLab’s work with schools
References
- 1.Wang, Mortality GBD, Causes of Death C Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scarborough P, Bhatnagar P, Wickramasinghe KK, et al. The economic burden of ill health due to diet, physical inactivity, smoking, alcohol and obesity in the UK: an update to 2006-07 NHS costs. J Public Health (Oxf) 2011;33(4):527–35. doi: 10.1093/pubmed/fdr033. [DOI] [PubMed] [Google Scholar]
- 3.Murray CJ, Lopez AD. Measuring the global burden of disease. N Engl J Med. 2013;369(5):448–57. doi: 10.1056/NEJMra1201534. [DOI] [PubMed] [Google Scholar]
- 4.Barker DJP. Mothers, Babies and health in later life. Edinburgh: Churchill Livingstone; 1998. [Google Scholar]
- 5.Eriksson JG, Forsen T, Tuomilehto J, et al. Early growth and coronary heart disease in later life: longitudinal study. BMJ. 2001;322(7292):949–53. doi: 10.1136/bmj.322.7292.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Godfrey KM, Gluckman PD, Hanson MA. Developmental origins of metabolic disease: life course and intergenerational perspectives. Trends Endocrinol Metab. 2010;21(4):199–205. doi: 10.1016/j.tem.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 7.Gluckman PD, Hanson MA, Bateson P, et al. Towards a new developmental synthesis: adaptive developmental plasticity and human disease. Lancet. 2009;373(9675):1654–7. doi: 10.1016/S0140-6736(09)60234-8. [DOI] [PubMed] [Google Scholar]
- 8.Barker M, Lawrence WT, Skinner TC, et al. Constraints on food choices of women in the UK with lower educational attainment. Public Health Nutr. 2008;11(12):1229–37. doi: 10.1017/S136898000800178X. [DOI] [PubMed] [Google Scholar]
- 9.Schagdarsurengin U, Steger K. Epigenetics in male reproduction: effect of paternal diet on sperm quality and offspring health. Nat Rev Urol. 2016;13(10):584–95. doi: 10.1038/nrurol.2016.157. [DOI] [PubMed] [Google Scholar]
- 10.Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: a foundation for future health. Lancet. 2012;379(9826):1630–40. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- 11.Baird J, Cooper C, Margetts BM, et al. Changing health behaviour of young women from disadvantaged backgrounds: evidence from systematic reviews. Proc Nutr Soc. 2009;68(2):195–204. doi: 10.1017/S0029665109001050. [DOI] [PubMed] [Google Scholar]
- 12.Borzekowski DL. Considering children and health literacy: a theoretical approach. Pediatrics. 2009;124(Suppl 3):S282–8. doi: 10.1542/peds.2009-1162D. [DOI] [PubMed] [Google Scholar]
- 13.Nutbeam D. Getting evidence into policy and practice to address health inequalities. Health Promot Int. 2004;19(2):137–40. doi: 10.1093/heapro/dah201. [DOI] [PubMed] [Google Scholar]
- 14.Tang KC, Nutbeam D, Aldinger C, et al. Schools for health, education and development: a call for action. Health Promot Int. 2009;24(1):68–77. doi: 10.1093/heapro/dan037. [DOI] [PubMed] [Google Scholar]
- 15.Bay JL, Mora HA, Sloboda DM, et al. Adolescent understanding of DOHaD concepts: a school-based intervention to support knowledge translation and behaviour change. J Dev Orig Health Dis. 2012;3(6):469–82. doi: 10.1017/S2040174412000505. [DOI] [PubMed] [Google Scholar]
- 16.Bennett J, Lubben F, Hogarth S. Bringing Science to Life: A Synthesis of the Research Evidence on the Effects of Context-Based and STS Approaches to Science Teaching. Science Education. 2007;91(3):347–70. [Google Scholar]
- 17.Grace M, Woods-Townsend K, Griffiths J, et al. A science-based approach to developing teenagers' views on their health and the health of their future children. Health Education. 2012;112:543–59. [Google Scholar]
- 18.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Government CaL, editor. DfCLG. English indices of deprivation 2015. 2015. [Google Scholar]
- 20.Crozier SR, Inskip HM, Barker ME, et al. Development of a 20-item food frequency questionnaire to assess a 'prudent' dietary pattern among young women in Southampton. Eur J Clin Nutr. 2010;64(1):99–104. doi: 10.1038/ejcn.2009.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lawrence W, Black C, Tinati T, et al. 'Making every contact count': Evaluation of the impact of an intervention to train health and social care practitioners in skills to support health behaviour change. J Health Psychol. 2016;21(2):138–51. doi: 10.1177/1359105314523304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Woods-Townsend K, Bagust L, Barker M, et al. Engaging teenagers in improving their health behaviours and increasing their interest in science (Evaluation of LifeLab Southampton): study protocol for a cluster randomized controlled trial. Trials. 2015;16:372. doi: 10.1186/s13063-015-0890-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.